MWB_Analyzer: An Automated Embedded System for Real-Time Quantitative Analysis of Morphine Withdrawal Behaviors in Rodents
Abstract
1. Introduction
- (1)
- Multi-angle video and full-scene audio capture via an edge computing platform for comprehensive data acquisition;
- (2)
- Real-time data reduction algorithms that significantly lower processing loads while preserving critical information;
- (3)
- Created and published a dataset of morphine withdrawal behavior video clips in rats for future research;
- (4)
- Enhanced behavioral recognition accuracy and objectivity through an improved YOLO-based framework and signal processing methods;
- (5)
- A more objective scoring protocol was used to score morphine withdrawal behavior to assess the degree of morphine addiction.
2. Materials and Methods
2.1. Animals and Drugs
2.2. Hardware Design and System Integration
2.3. Video Capture and External Trigger Synchronization
2.4. Motion Segment Filtering and Camera Angle Selection
2.5. Wet-Dog Shakes and Scratching Behavior Recognition
2.6. Lateral Behavior Recognition
2.7. Audio Recognition of Teeth Chattering Based on Mel Spectrogram and ResNet-SE
3. Results
3.1. Analysis of Withdrawal Behavior Recognition Metrics
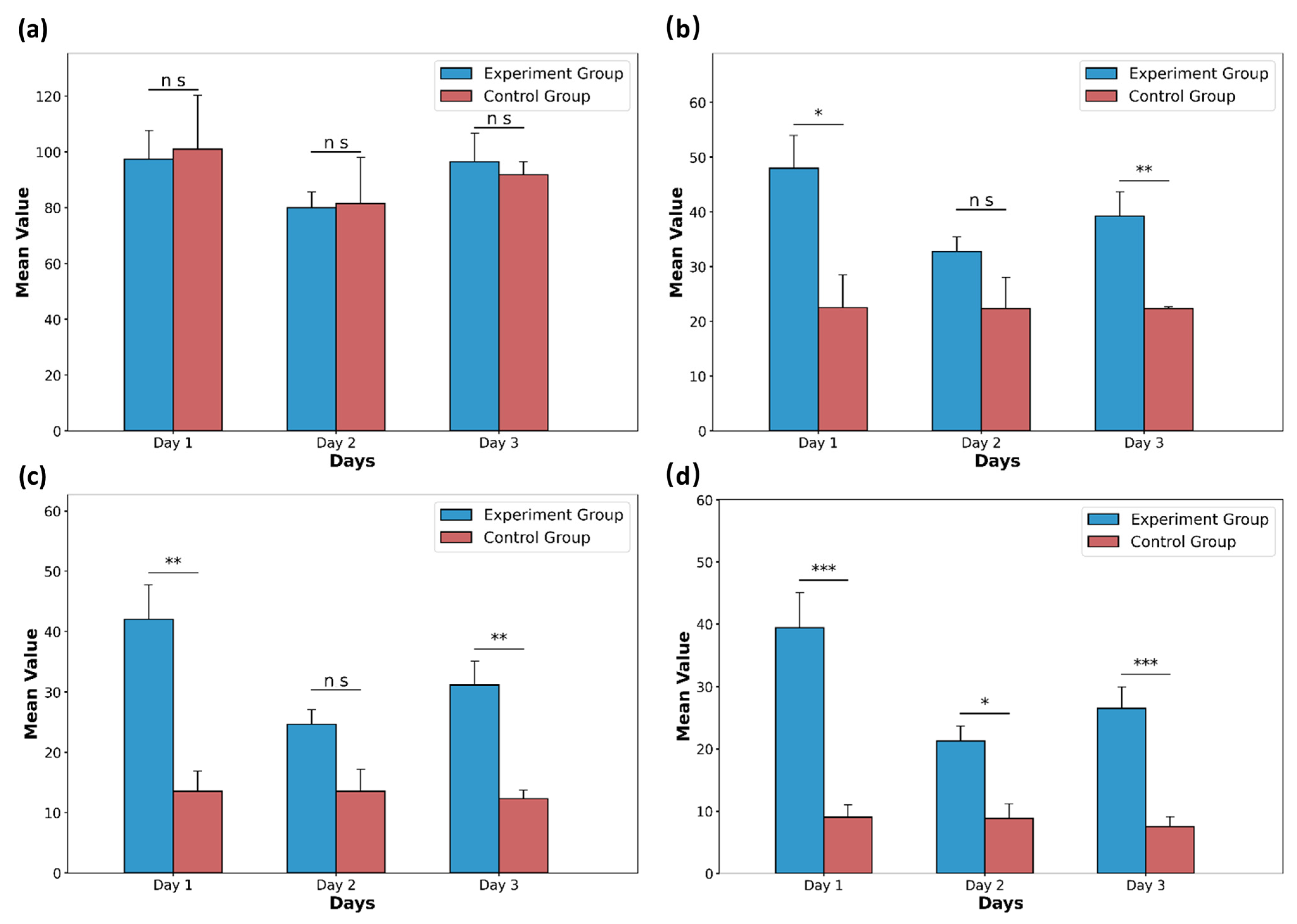
3.2. Exploring Behavioral Assessment Schemes for Morphine Addiction
3.3. Comprehensive Scoring Results Based on Our Proposed Evaluation Scheme
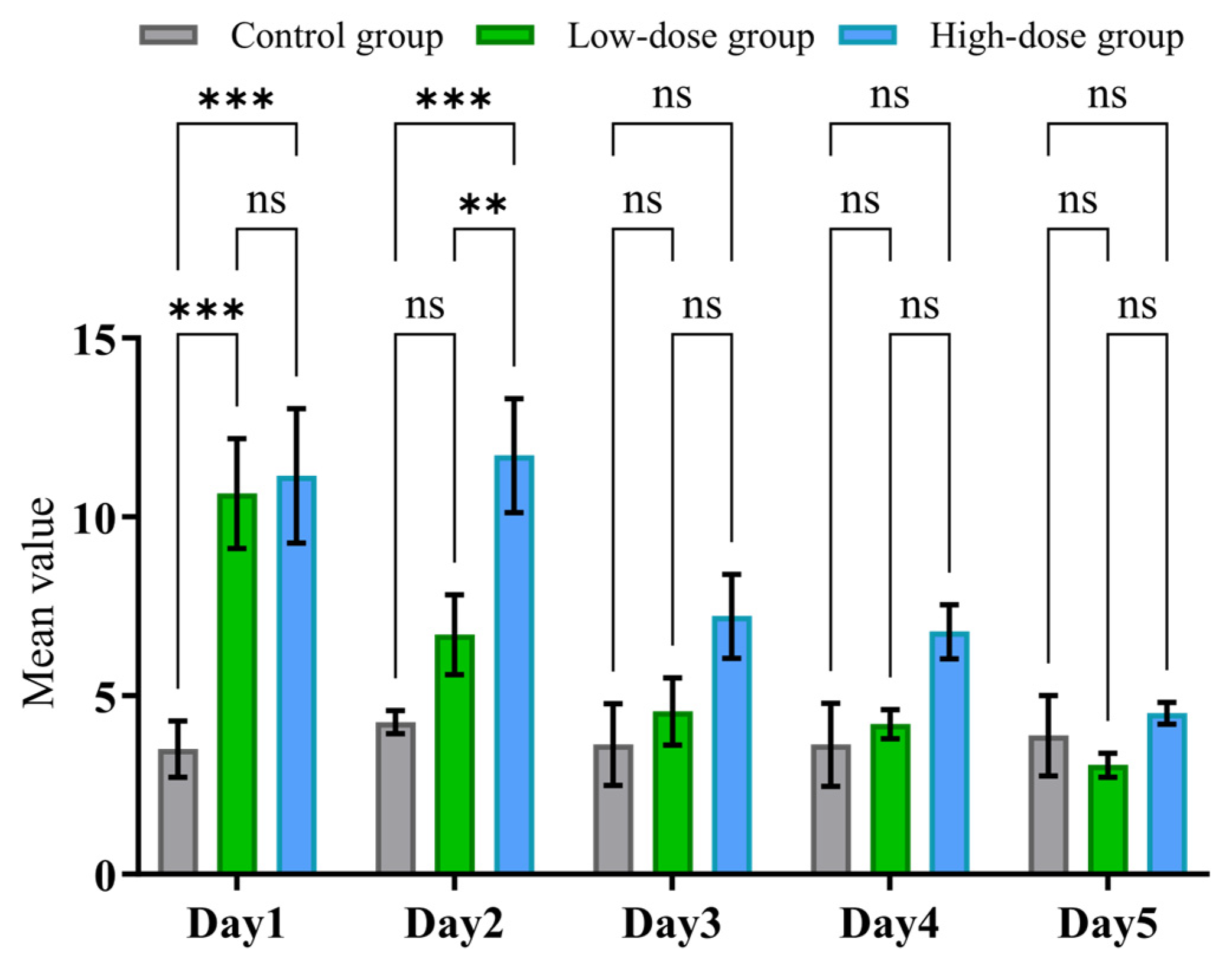
3.4. Experimental Study on Withdrawal Behaviors at Different Morphine Doses
3.5. Summary and Implications
4. Discussion
- (1)
- Easy Integration into Standard Workflows: MWB_Analyzer combines multi-angle video and full-scene audio capture in a fully automated manner. Its decentralized design (based on three compact Orange Pi units) requires no technical expertise for setup or operation. Once installed, the system runs autonomously, providing synchronized behavioral recordings without disrupting normal experimental procedures.
- (2)
- Substantial Reduction in Manual Workload Through Automation: The system leverages automatic data filtering and prioritization of key views (e.g., top view for locomotion, side view for postural signs) to reduce redundant data by over 95%. This optimization significantly lowers the computational load, allowing real-time behavior recording and analysis to be performed efficiently on compact edge devices. By automating both data acquisition and analysis, MWB_Analyzer minimizes the need for manual scoring and video review, enabling researchers to obtain objective results with minimal hands-on effort.
- (3)
- Enhanced Objectivity and Reproducibility: MWB_Analyzer achieves high classification accuracy (over 94% for video-based and 92% for audio-based detection of withdrawal behaviors) using a refined machine learning model. Unlike traditional scales such as Gellert and Holtzman [37], the system eliminates subjective judgment, ensuring consistent and unbiased assessments across experiments and operators. This is especially valuable for detecting subtle dose–response differences that might be missed in manual scoring. The system’s real-time analysis and precise behavior recognition facilitate more reliable dose–response evaluations, improved standardization across studies, and higher throughput for preclinical drug screening. By reducing human variability, MWB_Analyzer strengthens the statistical power of pharmacodynamic assessments and enhances confidence in drug efficacy and safety evaluations.
- (4)
- Broad Applicability and Flexibility: While optimized for morphine withdrawal, the system’s modular design allows easy adaptation to other models of dependence (e.g., fentanyl, alcohol). Its architecture also supports studies on drug delivery methods, pharmacokinetics, and systemic effects, making it a versatile tool for a wide range of preclinical research applications.
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Zhuang, Y.W.; Wang, Y.; He, B.Q.; He, X.H.; Zhou, X.E.; Guo, S.M.; Rao, Q.D.; Yang, J.Q.; Liu, J.Y.; Zhou, Q.T.; et al. Molecular recognition of morphine and fentanyl by the human μ-opioid receptor. Cell 2022, 185, 4361–4375.E19. [Google Scholar] [CrossRef] [PubMed]
- Del Vecchio, G.; Spahn, V.; Stein, C. Novel Opioid Analgesics and Side Effects. ACS Chem. Neurosci. 2017, 8, 1638–1640. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association (Ed.) Diagnostic and Statistical Manual of Mental Disorders; American Psychiatric Association Publishing: Washington, DC, USA, 2013; Volume 21, pp. 591–643. [Google Scholar]
- Centers for Disease Control and Prevention. U.S. overdose deaths in 2021 increased half as much as in 2020—But are still up 15%. Natl. Cent. Health Stat. 2022, 16, 2022. [Google Scholar]
- Koob, G.F.; Maldonado, R.; Stinus, L. Neural Substrates of Opiate Withdrawal. Trends Neurosci. 1992, 15, 186–191. [Google Scholar] [CrossRef] [PubMed]
- Monroe, S.C.; Radke, A.K. Opioid withdrawal: Role in addiction and neural mechanisms. Psychopharmacology 2023, 240, 1417–1433. [Google Scholar] [CrossRef]
- Koob, G.F.; Volkow, N.D. Neurocircuitry of addiction. Neuropsychopharmacology 2010, 35, 217–238. [Google Scholar] [CrossRef]
- Baker, T.B.; Japuntich, S.J.; Hogle, J.M.; McCarthy, D.E.; Curtin, J.J. Pharmacologic and behavioral withdrawal from addictive drugs. Curr. Dir. Psychol. Sci. 2006, 15, 232–236. [Google Scholar] [CrossRef]
- Manglik, A.; Kruse, A.C.; Kobilka, T.S.; Thian, F.S.; Mathiesen, J.M.; Sunahara, R.K.; Pardo, L.; Weis, W.I.; Kobilka, B.K.; Granier, S. Crystal structure of the μ-opioid receptor bound to a morphinan antagonist. Nature 2012, 485, 321–326. [Google Scholar] [CrossRef]
- Sverrisdóttir, E.; Lund, T.M.; Olesen, A.E.; Drewes, A.M.; Christrup, L.L.; Kreilgaard, M. A review of morphine and morphine-6-glucuronide’s pharmacokinetic–pharmacodynamic relationships in experimental and clinical pain. Eur. J. Pharm. Sci. 2015, 74, 45–62. [Google Scholar] [CrossRef]
- Vinks, A.A.; Punt, N.C.; Menke, F.; Kirkendall, E.; Butler, D.; Duggan, T.J.; Cortezzo, D.E.; Kiger, S.; Dietrich, T.; Spencer, P.; et al. Electronic Health Record-Embedded Decision Support Platform for Morphine Precision Dosing in Neonates. Clin. Pharmacol. Ther. 2020, 107, 186–194. [Google Scholar] [CrossRef]
- Weiss, F.; Ciccocioppo, R.; Parsons, L.H.; Katner, S.; Liu, X.; Zorrilla, E.P.; Valdez, G.R.; Ben-Shahar, O.; Angeletti, S.; Richter, R.R. Compulsive drug-seeking behavior and relapse—Neuroadaptation, stress, and conditioning factors. Biol. Basis Cocaine Addict. 2001, 937, 1–26. [Google Scholar] [CrossRef]
- Kutlu, M.G.; Gould, T.J. Effects of drugs of abuse on hippocampal plasticity and hippocampus-dependent learning and memory: Contributions to development and maintenance of addiction. Learn. Mem. 2016, 23, 515–533. [Google Scholar] [CrossRef] [PubMed]
- Werner, C.T.; Mitra, S.; Auerbach, B.D.; Wang, Z.J.; Martin, J.A.; Stewart, A.F.; Gobira, P.H.; Iida, M.; An, C.N.; Cobb, M.M.; et al. Neuroadaptations in the dorsal hippocampus underlie cocaine seeking during prolonged abstinence. Proc. Natl. Acad. Sci. USA 2020, 117, 26460–26469. [Google Scholar] [CrossRef]
- Meye, F.J.; Trusel, M.; Soiza-Reilly, M.; Mameli, M. Neural circuit adaptations during drug withdrawal—Spotlight on the lateral habenula. Pharmacol. Biochem. Behav. 2017, 162, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Burgdorf, C.E.; Schierberl, K.C.; Lee, A.S.; Fischer, D.K.; Van Kempen, T.A.; Mudragel, V.; Huganir, R.L.; Milner, T.A.; Glass, M.J.; Rajadhyaksha, A.M. Extinction of Contextual Cocaine Memories Requires Cav1.2 within D1R-Expressing Cells and Recruits Hippocampal Cav1.2-Dependent Signaling Mechanisms. J. Neurosci. 2017, 37, 11894–11911. [Google Scholar] [CrossRef]
- Lu, T.S.; Li, X.; Zheng, W.; Kuang, C.Y.; Wu, B.Y.; Liu, X.X.; Xue, Y.X.; Shi, J.; Lu, L.; Han, Y. Vaccines to Treat Substance Use Disorders: Current Status and Future Directions. Pharmaceutics 2024, 16, 84. [Google Scholar] [CrossRef] [PubMed]
- Haile, C.N.; Baker, M.D.; Sanchez, S.A.; Arteaga, C.A.L.; Duddupudi, A.L.; Cuny, G.D.; Norton, E.B.; Kosten, T.R.; Kosten, T.A. An Immunconjugate Vaccine Alters Distribution and Reduces the Antinociceptive, Behavioral and Physiological Effects of Fentanyl in Male and Female Rats. Pharmaceutics 2022, 14, 2290. [Google Scholar] [CrossRef] [PubMed]
- Moser, P.; Wolinsky, T.; Castagné, V.; Duxon, M. Current approaches and issues in non-clinical evaluation of abuse and dependence. J. Pharmacol. Toxicol. Methods 2011, 63, 160–167. [Google Scholar] [CrossRef]
- Zhu, J.; Ning, K.; Liu, B. Investigation and appraisal of non-clinical drug dependence in new drug development. J. China Pharm. Univ. 2008, 39, 373–375. [Google Scholar]
- Richardson, L.; Mammel, M.; Milloy, M.J.; Hayashi, K. Employment Cessation, Long Term Labour Market Engagement and HIV Infection Risk Among People Who Inject Drugs in an Urban Canadian Setting. Aids Behav. 2019, 23, 3267–3276. [Google Scholar] [CrossRef]
- Center for Drug Evaluation and Research. Technical Guidelines for Non-Clinical Drug Dependence Studies; Center for Drug Evaluation and Research: Silver Spring, MD, USA, 2022.
- Lerner, A.; Klein, M. Dependence, withdrawal and rebound of CNS drugs: An update and regulatory considerations for new drugs development. Brain Commun. 2019, 1, fcz025. [Google Scholar] [CrossRef]
- Marsden, J.; White, M.; Annand, F.; Burkinshaw, P.; Carville, S.; Eastwood, B.; Kelleher, M.; Knight, J.; O’Connor, R.; Tran, A.; et al. Medicines associated with dependence or withdrawal: A mixed-methods public health review and national database study in England. Lancet Psychiatry 2019, 6, 935–950. [Google Scholar] [CrossRef]
- Bluthenthal, R.N.; Simpson, K.; Ceasar, R.C.; Zhao, J.; Wenger, L.; Kral, A.H. Opioid withdrawal symptoms, frequency, and pain characteristics as correlates of health risk among people who inject drugs. Drug Alcohol Depend. 2020, 211, 107932. [Google Scholar] [CrossRef]
- Tarazi, D.; Maynes, J.T. Impact of Opioids on Cellular Metabolism: Implications for Metabolic Pathways Involved in Cancer. Pharmaceutics 2023, 15, 2225. [Google Scholar] [CrossRef]
- Antoine, D.; Singh, P.K.; Tao, J.Y.; Roy, S. Neonatal Morphine Results in Long-Lasting Alterations to the Gut Microbiome in Adolescence and Adulthood in a Murine Model. Pharmaceutics 2022, 14, 1879. [Google Scholar] [CrossRef]
- Danielewski, M.; Zielińska, S.; Merwid-Ląd, A.; Szandruk-Bender, M.; Słupski, W.; Włodarczyk, M.; Sozański, T.; Ziółkowski, P.; Szeląg, A.; Nowak, B. Sanguinarine-Chelerythrine from Coptis chinensis Offers Analgesic and Anti-Inflammatory Effects Without Gastrotoxicity. Pharmaceutics 2025, 17, 323. [Google Scholar] [CrossRef]
- Castro, N.C.F.; Silva, I.S.; Cartágenes, S.C.; Fernandes, L.M.P.; Ribera, P.C.; Barros, M.A.; Prediger, R.D.; Fontes-Júnior, E.A.; Maia, C.S.F. Morphine Perinatal Exposure Induces Long-Lasting Negative Emotional States in Adult Offspring Rodents. Pharmaceutics 2022, 14, 29. [Google Scholar] [CrossRef]
- Kudla, L.; Bugno, R.; Podlewska, S.; Szumiec, L.; Wiktorowska, L.; Bojarski, A.J.; Przewlocki, R. Comparison of an Addictive Potential of μ-Opioid Receptor Agonists with G Protein Bias: Behavioral and Molecular Modeling Studies. Pharmaceutics 2022, 14, 55. [Google Scholar] [CrossRef]
- Jin, T.L.; Duan, F. Rat Behavior Observation System Based on Transfer Learning. IEEE Access 2019, 7, 62152–62162. [Google Scholar] [CrossRef]
- Spragg, S.D.S. Morphine addiction in chimpanzees. Comp. Psychol. Monogr. 1940, 15, 132. [Google Scholar]
- Ahmed, S.H. Trying to make sense of rodents’ drug choice behavior. Prog. Neuro-Psychopharmacol. Biol. Psychiatry 2018, 87, 3–10. [Google Scholar] [CrossRef] [PubMed]
- Francis, D.L.; Schneider, C. Jumping after naloxone precipitated withdrawal of chronic morphine in the rat. Br. J. Pharmacol. 1971, 41, 424P–425P. [Google Scholar]
- Collier, H.O.J.; Schneider, C.; Francis, D.L. Modification of Morphine Withdrawal by Drugs Interacting with Humoral Mechanisms—Some Contradictions and Their Interpretation. Nature 1972, 237, 220–223. [Google Scholar] [CrossRef]
- Shiffman, S.; West, R.J.; Gilbert, D.G. Recommendation for the assessment of tobacco craving and withdrawal in smoking cessation trials. Nicotine Tob. Res. 2004, 6, 599–614. [Google Scholar] [CrossRef]
- Gellert, V.F.; Holtzman, S.G. Development and maintenance of morphine tolerance and dependence in the rat by scheduled access to morphine drinking solutions. J. Pharmacol. Exp. Ther. 1978, 205, 536–546. [Google Scholar] [CrossRef]
- Maldonado, R.; Negus, S.; Koob, G. Precipitation of morphine withdrawal syndrome in rats by administration of mu-, delta-and kappa-selective opioid antagonists. Neuropharmacology 1992, 31, 1231–1241. [Google Scholar] [CrossRef]
- Moayeri, A.; Mehdizadeh, R.; Karimi, E.; Aidy, A.; Ghaneialvar, H.; Abbasi, N. Thymol Nanopolymer Synthesis and Its Effects on Morphine Withdrawal Syndrome in Comparison with Clonidine in Rats. Front. Behav. Neurosci. 2022, 16, 843951. [Google Scholar] [CrossRef]
- Quintanilla, M.E.; Morales, P.; Santapau, D.; Ávila, A.; Ponce, C.; Berrios-Cárcamo, P.; Olivares, B.; Gallardo, J.; Ezquer, M.; Herrera-Marschitz, M.; et al. Chronic Voluntary Morphine Intake Is Associated with Changes in Brain Structures Involved in Drug Dependence in a Rat Model of Polydrug Use. Int. J. Mol. Sci. 2023, 24, 17081. [Google Scholar] [CrossRef]
- Halbout, B.; Hutson, C.; Agrawal, S.; Springs, Z.A.; Ostlund, S.B. Differential effects of acute and prolonged morphine withdrawal on motivational and goal-directed control over reward-seeking behaviour. Addict. Biol. 2024, 29, e13393. [Google Scholar] [CrossRef] [PubMed]
- López-Cano, M.; Font, J.; Aso, E.; Sahlholm, K.; Cabré, G.; Giraldo, J.; De Koninck, Y.; Hernando, J.; Llebaria, A.; Fernández-Dueñas, V.; et al. Remote local photoactivation of morphine produces analgesia without opioid-related adverse effects. Br. J. Pharmacol. 2023, 180, 958–974. [Google Scholar] [CrossRef] [PubMed]
- Srivastav, A.K.; Mishra, M.K.; Lillard, J.W.; Singh, R. Transforming Pharmacogenomics and CRISPR Gene Editing with the Power of Artificial Intelligence for Precision Medicine. Pharmaceutics 2025, 17, 555. [Google Scholar] [CrossRef] [PubMed]
- Yang, S.; Hu, X.; Zhu, J.; Zheng, B.; Bi, W.; Wang, X.; Wu, J.; Mi, Z.; Wu, Y. Aspects and Implementation of Pharmaceutical Quality by Design from Conceptual Frameworks to Industrial Applications. Pharmaceutics 2025, 17, 623. [Google Scholar] [CrossRef]
- Serrano, D.R.; Luciano, F.C.; Anaya, B.J.; Ongoren, B.; Kara, A.; Molina, G.; Ramirez, B.I.; Sánchez-Guirales, S.A.; Simon, J.A.; Tomietto, G.; et al. Artificial Intelligence (AI) Applications in Drug Discovery and Drug Delivery: Revolutionizing Personalized Medicine. Pharmaceutics 2024, 16, 1328. [Google Scholar] [CrossRef]
- El-Tanani, M.; Satyam, S.M.; Rabbani, S.A.; El-Tanani, Y.; Aljabali, A.A.A.; Al Faouri, I.; Rehman, A. Revolutionizing Drug Delivery: The Impact of Advanced Materials Science and Technology on Precision Medicine. Pharmaceutics 2025, 17, 375. [Google Scholar] [CrossRef] [PubMed]
- Albayati, N.; Talluri, S.R.; Dholaria, N.; Michniak-Kohn, B. AI-Driven Innovation in Skin Kinetics for Transdermal Drug Delivery: Overcoming Barriers and Enhancing Precision. Pharmaceutics 2025, 17, 188. [Google Scholar] [CrossRef]
- Świerczek, A.; Batko, D.; Wyska, E. The Role of Pharmacometrics in Advancing the Therapies for Autoimmune Diseases. Pharmaceutics 2024, 16, 1559. [Google Scholar] [CrossRef]
- Negrete, S.B.; Arai, H.; Natsume, K.; Shibata, T. Multi-view image-based behavior classification of wet-dog shake in Kainate rat model. Front. Behav. Neurosci. 2023, 17, 1148549. [Google Scholar] [CrossRef]
- Yu, H.S.; Xiong, J.W.; Ye, A.Y.; Li Cranfill, S.; Cannonier, T.; Gautam, M.; Zhang, M.; Bilal, R.; Park, J.E.; Xue, Y.J.; et al. Scratch-AID, a deep learning-based system for automatic detection of mouse scratching behavior with high accuracy. eLife 2022, 11, e84042. [Google Scholar] [CrossRef] [PubMed]
- Shih, Y.H.; Ke, T.C.; Lin, M.T.; Young, M.S. Sensor system for enhanced detection of locomotion and standing behavior in rats. IEEE Sens. J. 2008, 8, 357–364. [Google Scholar] [CrossRef]
- Kernan, W.J.; Mullenix, P.J.; Hopper, D.L. Pattern-Recognition of Rat Behavior. Pharmacol. Biochem. Behav. 1987, 27, 559–564. [Google Scholar] [CrossRef]
- Arai, H.; Shigemoto, M.; Natsume, K. Detection of the change in characteristics of self-grooming by the neural network in the latent period of the Rat Kainate Epilepsy model. Sice J. Control Meas. Syst. Integr. 2022, 15, 64–70. [Google Scholar] [CrossRef]
- Nath, T.; Mathis, A.; Chen, A.C.; Patel, A.; Bethge, M.; Mathis, M.W. Using DeepLabCut for 3D markerless pose estimation across species and behaviors. Nat. Protoc. 2019, 14, 2152–2176. [Google Scholar] [CrossRef] [PubMed]
- Li, W.; Liu, M.; Liu, H.; Guo, T.; Wang, T.; Tang, H.; Sebe, N. GraphMLP: A graph MLP-like architecture for 3D human pose estimation. Pattern Recognit. 2025, 158, 110925. [Google Scholar] [CrossRef]
- Cao, Z.; Hidalgo, G.; Simon, T.; Wei, S.E.; Sheikh, Y. OpenPose: Realtime Multi-Person 2D Pose Estimation Using Part Affinity Fields. IEEE Trans. Pattern Anal. Mach. Intell. 2021, 43, 172–186. [Google Scholar] [CrossRef] [PubMed]
- Fang, Q.; Xu, Z.H.; Hu, M.X.; Zeng, Q.Y.; Liu, C.J.; Chen, Q.J. SPGformer: Serial-Parallel Hybrid GCN-Transformer with Graph-Oriented Encoder for 2-D-to-3-D Human Pose Estimation. IEEE Trans. Instrum. Meas. 2024, 73, 8003015. [Google Scholar] [CrossRef]
- Yin, Y.F.; Liu, M.; Zhu, Q.G.; Zhang, S.S.; Hussien, N.A.; Fan, Y. Multibranch Attention Graph Convolutional Networks for 3-D Human Pose Estimation. IEEE Trans. Instrum. Meas. 2023, 72, 2520412. [Google Scholar] [CrossRef]
- Hu, Y.J.; Ferrario, C.R.; Maitland, A.D.; Ionides, R.B.; Ghimire, A.; Watson, B.; Iwasaki, K.; White, H.; Xi, Y.T.; Zhou, J.; et al. LabGym: Quantification of user-defined animal behaviors using learning-based holistic assessment. Cell Rep. Methods 2023, 3, 100415. [Google Scholar] [CrossRef]
- Hassan, R.; See, C.P.; Sreenivasan, S.; Mansor, S.M.; Müller, C.P.; Hassan, Z. Mitragynine Attenuates Morphine Withdrawal Effects in Rats—A Comparison with Methadone and Buprenorphine. Front. Psychiatry 2020, 11, 411. [Google Scholar] [CrossRef]
- Piczak, K.J. ESC: Dataset for environmental sound classification. In Proceedings of the 23rd ACM International Conference on Multimedia, Brisbane, Australia, 26–30 October 2015; pp. 1015–1018. [Google Scholar]







| Criterion | Baseline | Baseline + CBAM (Kernel = 3) | Baseline + CSPM (Kernel = 3) | Baseline + CSPM (Kernel = 7) | Baseline + CBAM (Kernel = 7) | RK3588 (Baseline + CSPM (Kernel = 3)) | |
|---|---|---|---|---|---|---|---|
| Grooming | Precision | 0.936 | 0.912 | 0.912 | 0.928 | 0.928 | 0.904 |
| Recall | 0.860 | 0.832 | 0.950 | 0.885 | 0.959 | 0.950 | |
| F1 | 0.897 | 0.870 | 0.931 | 0.906 | 0.943 | 0.926 | |
| Head-raising | Precision | 0.977 | 0.989 | 0.989 | 0.977 | 0.977 | 0.989 |
| Recall | 0.966 | 0.966 | 0.966 | 0.977 | 0.977 | 0.966 | |
| F1 | 0.971 | 0.977 | 0.977 | 0.977 | 0.977 | 0.977 | |
| Normal | Precision | 0.879 | 0.894 | 0.924 | 0.909 | 0.924 | 0.924 |
| Recall | 0.841 | 0.881 | 0.924 | 0.870 | 0.871 | 0.924 | |
| F1 | 0.859 | 0.887 | 0.924 | 0.889 | 0.897 | 0.924 | |
| Rearing | Precision | 0.915 | 0.872 | 0.894 | 0.809 | 0.830 | 0.851 |
| Recall | 0.977 | 0.854 | 1.000 | 1.000 | 1.000 | 1.000 | |
| F1 | 0.945 | 0.863 | 0.994 | 0.894 | 0.907 | 0.920 | |
| Genital licking | Precision | 0.831 | 0.803 | 0.958 | 0.887 | 0.972 | 0.958 |
| Recall | 0.952 | 0.934 | 0.919 | 0.984 | 0.896 | 0.932 | |
| F1 | 0.887 | 0.864 | 0.938 | 0.933 | 0.932 | 0.944 | |
| Wall-supported rearing | Precision | 0.990 | 0.930 | 0.990 | 1.000 | 1.000 | 0.990 |
| Recall | 0.961 | 0.949 | 0.961 | 0.926 | 0.943 | 0.943 | |
| F1 | 0.975 | 0.939 | 0.975 | 0.962 | 0.971 | 0.966 | |
| Face-washing | Precision | 0.769 | 0.821 | 0.872 | 0.821 | 0.821 | 0.872 |
| Recall | 0.909 | 0.914 | 0.829 | 0.842 | 0.914 | 0.791 | |
| F1 | 0.833 | 0.865 | 0.850 | 0.831 | 0.865 | 0.829 | |
| All | Top-1 | 0.918 | 0.901 | 0.942 | 0.923 | 0.938 | 0.936 |
| Types of Behavior | Scoring Method |
|---|---|
| Wet-dog shakes | 1 point each time recorded |
| Head-raising | 1 point each time recorded |
| Stereotypic behaviors | 0.5 point each time recorded |
| Teeth chattering | 2 points if it occurs every 5 min |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Zhang, M.; Li, Q.; Li, S.; Sun, B.; Wu, Z.; Liu, J.; Geng, X.; Chen, F. MWB_Analyzer: An Automated Embedded System for Real-Time Quantitative Analysis of Morphine Withdrawal Behaviors in Rodents. Toxics 2025, 13, 586. https://doi.org/10.3390/toxics13070586
Zhang M, Li Q, Li S, Sun B, Wu Z, Liu J, Geng X, Chen F. MWB_Analyzer: An Automated Embedded System for Real-Time Quantitative Analysis of Morphine Withdrawal Behaviors in Rodents. Toxics. 2025; 13(7):586. https://doi.org/10.3390/toxics13070586
Chicago/Turabian StyleZhang, Moran, Qianqian Li, Shunhang Li, Binxian Sun, Zhuli Wu, Jinxuan Liu, Xingchao Geng, and Fangyi Chen. 2025. "MWB_Analyzer: An Automated Embedded System for Real-Time Quantitative Analysis of Morphine Withdrawal Behaviors in Rodents" Toxics 13, no. 7: 586. https://doi.org/10.3390/toxics13070586
APA StyleZhang, M., Li, Q., Li, S., Sun, B., Wu, Z., Liu, J., Geng, X., & Chen, F. (2025). MWB_Analyzer: An Automated Embedded System for Real-Time Quantitative Analysis of Morphine Withdrawal Behaviors in Rodents. Toxics, 13(7), 586. https://doi.org/10.3390/toxics13070586







