Health Hazards Associated with Exposure to Endosulfan: A Mini-Review
Abstract
1. Introduction
2. Structure and Chemical Properties of Endosulfan
3. History, Global Distribution, and Regulatory Control of Endosulfan Use
4. Toxicity of Endosulfan and Associated Health Hazards in Various Organisms
5. Routes of Entry into the Human Body and Sources of Exposure
6. Endosulfan Tissue Distribution and Excretion in Humans
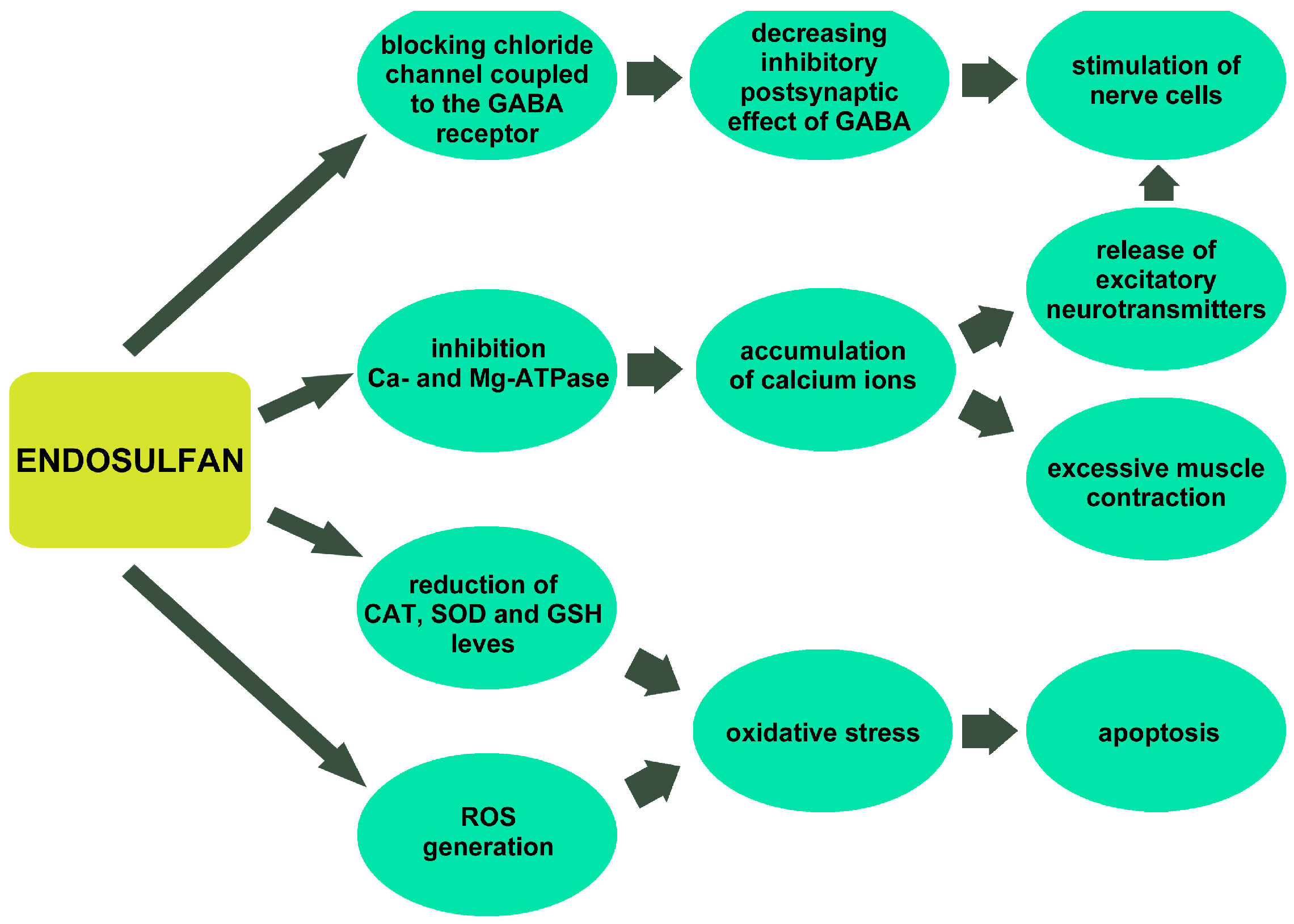
7. Mechanisms of Endosulfan Toxicity
8. Endosulfan Neurotoxicity in Humans
9. Endosulfan Genotoxicity
10. The Effect of Endosulfan on the Reproductive System and Fetal Development
11. Endosulfan and Cancers in Humans
12. Endosulfan and the Cardiovascular System
13. Other Endosulfan Effects on Human Health
14. Endosulfan Acute Poisoning and Its Treatment
15. Towards Safer Alternatives to Endosulfan
16. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AChE | Acetylcholinesterase |
| ACTH | Adrenocorticotropic hormone |
| ALS | Amyotrophic lateral sclerosis |
| ALT | Alanine aminotransferase |
| AST | Aspartate aminotransferase |
| BMI | Body mass index |
| CAT | Catalase |
| CNS | Central nervous system |
| COP5 | Fifth meeting of the Conference of the Parties |
| DIC | Disseminated intravascular coagulation |
| EPA | Environmental Protection Agency |
| EU | European Union |
| GABA | γ-aminobutyric acid |
| GH | Growth hormone |
| GSH | Glutathione |
| GST | Glutathione-S-transferase |
| HUVEC | Human umbilical vein endothelial cells |
| IL | Interleukin |
| LC50 | Lethal concentration 50% |
| LD50 | Median lethal dose |
| LH | Luteinizing hormone |
| MN | Micronuclei |
| NOEL | No Observed Effect Level |
| NTD | Neural tube defects |
| PBMC | Peripheral blood mononuclear cells |
| POPs | Stockholm Convention on Persistent Organic Pollutants |
| ROS | Reactive oxygen species |
| SCE | Sister chromatid exchanges |
| SCG | Single-cell gel electrophoresis |
| SOD | Superoxide dismutase |
| TSH | Thyroid-stimulating hormone |
| WHO | World Health Organization |
References
- Menezes, R.G.; Qadir, T.F.; Moin, A.; Fatima, H.; Hussain, S.A.; Madadin, M.; Pasha, S.B.; Al Rubaish, F.A.; Senthilkumaran, S. Endosulfan poisoning: An overview. J. Forensic Leg. Med. 2017, 51, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Murali, M.; Shivanandappa, T. Endosulfan causes oxidative stress in the liver and brain that involves inhibition of NADH dehydrogenase and altered antioxidant enzyme status in rat. Ecotoxicol. Environ. Saf. 2022, 239, 113593. [Google Scholar] [CrossRef] [PubMed]
- Milesi, M.M.; Durando, M.; Lorenz, V.; Gastiazoro, M.P.; Varayoud, J. Postnatal exposure to endosulfan affects uterine development and fertility. Mol. Cell. Endocrinol. 2020, 511, 110855. [Google Scholar] [CrossRef]
- Karn, S.K.; Upadhyay, A.; Kumar, A. Biomonitoring of endosulfan toxicity in human. Biocell 2022, 46, 1771–1777. [Google Scholar] [CrossRef]
- National Center for Biotechnology Information. PubChem Compound Summary for CID 3224, Endosulfan. Available online: https://pubchem.ncbi.nlm.nih.gov/compound/Endosulfan (accessed on 19 May 2025).
- Essandoh, Y.E.; Steiniche, T.; Xia, C.; Romanak, K.; Ogwang, J.; Mutegeki, R.; Wasserman, M.; Venier, M. Tracking toxic chemical exposure in Uganda: Insights from silicone wristbands. Environ. Res. 2025, 277, 121522. [Google Scholar] [CrossRef]
- Sosan, M.B.; Adeleye, A.O.; Oyekunle, J.A.O.; Udah, O.; Oloruntunbi, P.M.; Daramola, M.O.; Saka, W.T. Dietary risk assessment of organochlorine pesticide residues in maize-based complementary breakfast food products in Nigeria. Heliyon 2020, 6, e05803. [Google Scholar] [CrossRef] [PubMed]
- Sathishkumar, P.; Mohan, K.; Ramu Ganesan, A.; Govarthanan, M.; Rahim Mohd Yusoff, A.; Long Gu, F. Persistence, toxicological effect and ecological issues of endosulfan–A review. J. Hazrd. Mater. 2021, 416, 125779. [Google Scholar] [CrossRef]
- Sivakamasundari, K.; Smitha, M.V. Analysis on the causes for using endosulfan in agriculture by induced fuzzy cognitive maps (IFCM). MEMES 2017, 1, 21–38. Available online: https://researchjournalsmesmampad.edu.in/assets/15541917484.%20M.V.Smitha.pdf (accessed on 19 May 2025).
- Arisekar, U.; Jeya Shakila, R.; Shalini, R.; Jeyasekaran, G. Pesticides contamination in the Thamirabarani, a perennial river in peninsular India: The first report on ecotoxicological and human health risk assessment. Chemosphere 2021, 267, 129251. [Google Scholar] [CrossRef]
- Sharma, N.; Kumar, A.; Singh, S.; Kumar, S.; Joshi, R. Multi-residue determination of pesticides in vegetables and assessment of human health risks in Western Himalayan region of India. Environ. Monit. Assess. 2022, 194, 332. [Google Scholar] [CrossRef]
- Bonvoisin, T.; Utyasheva, L.; Knipe, D.; Gunnell, D.; Eddleston, M. Suicide by pesticide poisoning in India: A review of pesticide regulations and their impact on suicide trends. BMC Public Health 2020, 20, 251. [Google Scholar] [CrossRef] [PubMed]
- Ben Mukiibi, S.; Nyanzi, S.A.; Kwetegyeka, J.; Olisah, C.; Taiwo, A.M.; Mubiru, E.; Tebandeke, E.; Matovu, H.; Odongo, S.; Abayi, J.J.M.; et al. Organochlorine pesticide residues in Uganda’s honey as a bioindicator of environmental contamination and reproductive health implications to consumers. Ecotoxicol. Environ. Saf. 2021, 214, 112094. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, R.; Raghavan, S.C. Molecular mechanism of Endosulfan action in mammals. J. Biosci. 2017, 42, 149–153. [Google Scholar] [CrossRef]
- Coskun, R.; Gundogan, K.; Tanriverdi, F.; Guven, M.; Sungur, M. Effects of endosulfan intoxication on pituitary functions. Clin. Toxicol. 2012, 50, 441–443. [Google Scholar] [CrossRef]
- Saiyed, H.; Dewan, A.; Bhatnagar, V.; Shenoy, U.; Shenoy, R.; Rajmohan, H.; Patel, K.; Kashyap, R.; Kulkarni, P.; Rajan, B.; et al. Effect of endosulfan on male reproductive development. Environ. Health Perspect. 2003, 111, 1958–1962. [Google Scholar] [CrossRef]
- Ren, A.; Qiu, X.; Jin, L.; Ma, J.; Li, Z.; Zhang, L.; Zhu, H.; Finnell, R.H.; Zhu, T. Association of selected persistent organic pollutants in the placenta with the risk of neural tube defects. Proc. Natl. Acad. Sci. USA 2011, 108, 12770–12775. [Google Scholar] [CrossRef] [PubMed]
- Pathak, R.; Suke, S.G.; Ahmed, T.; Ahmed, R.S.; Tripathi, A.K.; Guleria, K.; Sharma, C.S.; Makhijani, S.D.; Banerjee, B.D. Organochlorine pesticide residue levels and oxidative stress in preterm delivery cases. Hum. Exp. Toxicol. 2010, 29, 351–358. [Google Scholar] [CrossRef] [PubMed]
- Tyagi, V.; Garg, N.; Mustafa, M.D.; Banerjee, B.D.; Guleria, K. Organochlorine pesticide levels in maternal blood and placental tissue with reference to preterm birth: A recent trend in North Indian population. Environ. Monit. Assess. 2015, 187, 471. [Google Scholar] [CrossRef]
- Yadla, M.; Yanala, S.R.; Parvithina, S.; Chennu, K.K.; Annapindi, N.; Vishnubhotla, S. Acute kidney injury in endosulfan poisoning. Saudi J. Kidney Dis. Transpl. 2013, 24, 592–593. [Google Scholar] [CrossRef]
- Thammineni, K.L.; Thakur, G.K.; Banerjee, B.D.; Kaur, N. Breast adipose tissue level of organochlorine pesticides as a risk factor in breast cancer: A cross sectional study in North Indian females. Chemosphere 2025, 377, 144339. [Google Scholar] [CrossRef]
- Sharma, S.; Malhotra, L.; Mukherjee, P.; Kaur, N.; Krishanlata, T.; Srikanth, C.V.; Mishra, V.; Banerjee, B.D.; Ethayathulla, A.S.; Sharma, R.S. Putative interactions between transthyretin and endosulfan II and its relevance in breast cancer. Int. J. Biol. Macromol. 2023, 235, 123670. [Google Scholar] [CrossRef] [PubMed]
- Sasikala, S.; Minu Jenifer, M.; Velavan, K.; Sakthivel, M.; Sivasamy, R.; Fenwick Antony, E.R. Predicting the relationship between pesticide genotoxicity and breast cancer risk in South Indian women in in vitro and in vivo experiments. Sci. Rep. 2023, 13, 9712. [Google Scholar] [CrossRef]
- Kiyani, R.; Dehdashti, B.; Heidari, Z.; Sharafi, S.M.; Mahmoodzadeh, M.; Amin, M.M. Biomonitoring of organochlorine pesticides and cancer survival: A population-based study. Environ. Sci. Pollut. Res. Int. 2023, 30, 37357–37369. [Google Scholar] [CrossRef]
- Moon, J.M.; Chun, B.J. Acute endosulfan poisoning: A retrospective study. Hum. Exp. Toxicol. 2009, 28, 309–316. [Google Scholar] [CrossRef] [PubMed]
- Karatas, A.D.; Aygun, D.; Baydin, A. Characteristics of endosulfan poisoning: A study of 23 cases. Singap. Med. J. 2006, 47, 1030–1032. [Google Scholar]
- Liu, Z.; Ding, X.; Zhang, B.; Pang, Y.; Wang, Y.; Xu, D.; Wang, H. Endosulfan promotes cell growth, migration and invasion via CCL5/CCR5 axis in MCF-7 cells. Ecotoxicol. Environ. Saf. 2024, 288, 117344. [Google Scholar] [CrossRef]
- Wang, Y.; Guo, Y.; Hu, Y.; Sun, Y.; Xu, D. Endosulfan triggers epithelial-mesenchymal transition via PTP4A3-mediated TGF-β signaling pathway in prostate cancer cells. Sci. Total Environ. 2020, 731, 139234. [Google Scholar] [CrossRef] [PubMed]
- Weber, J.; Halsall, C.J.; Muir, D.; Teixeira, C.; Small, J.; Solomon, K.; Hermanson, M.; Hung, H.; Bidleman, T. Endosulfan, a global pesticide: A review of its fate in the environment and occurrence in the Arctic. Sci. Total Environ. 2010, 408, 2966–2984. [Google Scholar] [CrossRef]
- Jayaraj, R.; Megha, P.; Sreedev, P. Organochlorine pesticides, their toxic effects on living organisms and their fate in the environment. Interdiscip. Toxicol. 2016, 9, 90–100. [Google Scholar] [CrossRef]
- Wan, M.T.; Kuo, J.N.; Buday, C.; Schroeder, G.; Van Aggelen, G.; Pasternak, J. Toxicity of alpha-, beta-, (alpha + beta)-endosulfan and their formulated and degradation products to Daphnia magna, Hyalella azteca, Oncorhynchus mykiss, Oncorhynchus kisutch, and biological implications in streams. Environ. Toxicol. Chem. 2005, 24, 1146–1154. [Google Scholar] [CrossRef]
- Vorkamp, K.; Rigét, F.F.; Bossi, R.; Sonne, C.; Dietz, R. Endosulfan, short-chain chlorinated paraffins (sccps) and octachlorostyrene in wildlife from greenland: Levels, trends and methodological challenges. Arch. Environ. Contam. Toxicol. 2017, 73, 542–551. [Google Scholar] [CrossRef] [PubMed]
- Kataoka, R.; Takagi, K. Biodegradability and biodegradation pathways of endosulfan and endosulfan sulfate. Appl. Microbiol. Biotechnol. 2013, 97, 3285–3292. [Google Scholar] [CrossRef]
- Stewart, D.K.; Cairns., K.G. Endosulfan persistence in soil and uptake by potato tubers. J. Agric. Food Chem. 1974, 22, 984–986. [Google Scholar] [CrossRef] [PubMed]
- Aktar, M.W.; Sengupta, D.; Chowdhury, A. Impact of pesticides use in agriculture: Their benefits and hazards. Interdiscip. Toxicol. 2009, 2, 1–12. [Google Scholar] [CrossRef]
- Rosales Landeros, C.; Barrera Díaz, C.E.; Bilyeu, B. Dissemination of endosulfan into the environment. In Persistent Organic Pollutants; IntechOpen: New York, NY, USA, 2019. [Google Scholar] [CrossRef]
- Liu, W.; Gan, J.J.; Lee, S.; Kabashima, J.N. Phase distribution of synthetic pyrethroids in runoff and stream water. Environ. Toxicol. Chem. 2004, 23, 7–11. [Google Scholar] [CrossRef]
- Stockholm Convention on Persistent Organic Pollutants. Endosulfan Added to the List of Persistent Organic Pollutants to Be Eliminated Worldwide; United Nations Environment Programme: Geneva, Switzerland, 2011; Available online: https://chm.pops.int (accessed on 18 April 2025).
- European Parliament and Council. Regulation (EU) No 649/2012 concerning the export and import of hazardous chemicals. Off. J. Eur. Union 2012, L201, 60–106. [Google Scholar]
- European Parliament and Council. Regulation (EU) 2019/1021 on persistent organic pollutants. Off. J. Eur. Union 2019, L169, 45–77. [Google Scholar]
- Stockholm Convention Secretariat. Listing of Endosulfan in Annex A to the Stockholm Convention on Persistent Organic Pollutants; United Nations Environment Programme: Geneva, Switzerland, 2011. [Google Scholar]
- Lubick, N. Environment. Endosulfan’s exit: U.S. EPA pesticide review leads to a ban. Science 2010, 328, 1466. [Google Scholar] [CrossRef] [PubMed]
- Shamma, S.; Hussein, M.A.; El-Nahrery, E.M.A.; Shahat, A.; Shoeib, T.; Abdelnaser, A. Leveraging machine learning in precision medicine to unveil organochlorine pesticides as predictive biomarkers for thyroid dysfunction. Sci. Rep. 2025, 15, 12501. [Google Scholar] [CrossRef]
- Agency for Toxic Substances and Disease Registry (ATSDR). Toxicological Profile for Endosulfan; Draft for Public Comment; Department of Health and Human Services, Public Health Service: Atlanta, GA, USA, 2015. Available online: https://www.atsdr.cdc.gov/ToxProfiles/tp41.pdf (accessed on 20 May 2025).
- Silva, M.H.; Gammon, D. An assessment of the developmental, reproductive, and neurotoxicity of endosulfan. Birth Defects Res. B Dev. Reprod. Toxicol. 2009, 86, 1–28. [Google Scholar] [CrossRef]
- Gupta, P.K.; Murthy, R.C.; Chandra, S.V. Toxicity of endosulfan and manganese chloride: Cumulative toxicity rating. Toxicol. Lett. 1981, 7, 221–227. [Google Scholar] [CrossRef] [PubMed]
- Kumar, N.; Ambasankar, K.; Krishnani, K.K.; Gupta, S.K.; Bhushan, S.; Minhas, P.S. Acute toxicity, biochemical and histopathological responses of endosulfan in Chanos chanos. Ecotoxicol. Environ. Saf. 2016, 131, 79–88. [Google Scholar] [CrossRef] [PubMed]
- Kumari, U.; Singh, R.; Mazumder, S. Chronic endosulfan exposure impairs immune response rendering Clarias gariepinus susceptible to microbial infection. Aquat. Toxicol. 2017, 191, 42–49. [Google Scholar] [CrossRef]
- Capkin, E.; Altinok, I.; Karahan, S. Water quality and fish size affect toxicity of endosulfan, an organochlorine pesticide, to rainbow trout. Chemosphere 2006, 64, 1793–1800. [Google Scholar] [CrossRef] [PubMed]
- Nam, T.H.; Kim, L.; Jeon, H.J.; Kim, K.; Ok, Y.S.; Choi, S.D.; Lee, S.E. Biomarkers indicate mixture toxicities of fluorene and phenanthrene with endosulfan toward earthworm (Eisenia fetida). Environ. Geochem. Health 2017, 39, 307–317. [Google Scholar] [CrossRef]
- Uğurlu, P.; Satar, E.İ.; Ünlü, E. Toxic effects of commercial grade indoxacarb and endosulfan on Gammarus kischineffensis (Schellenberg, 1937) (Crustacea: Amphipoda). Chemosphere 2024, 360, 142387. [Google Scholar] [CrossRef]
- Oktay, C.; Goksu, E.; Bozdemir, N.; Soyuncu, S. Unintentional toxicity due to endosulfan: A case report of two patients and characteristics of endosulfan toxicity. Vet. Hum. Toxicol. 2003, 45, 318–320. [Google Scholar]
- Sanghi, R.; Pillai, M.K.; Jayalekshmi, T.R.; Nair, A. Organochlorine and organophosphorus pesticide residues in breast milk from Bhopal, Madhya Pradesh, India. Hum. Exp. Toxicol. 2003, 22, 73–76. [Google Scholar] [CrossRef]
- Jindal, A.; Sankhyan, N. Endosulfan poisoning resulting from skin exposure. Indian. J. Pediatr. 2012, 79, 1104. [Google Scholar] [CrossRef]
- Hayat, K.; Afzal, M.; Aqueel, M.A.; Ali, S.; Saeed, M.F.; Qureshi, A.K.; Ullah, M.I.; Khan, Q.M.; Naseem, M.T.; Ashfaq, U.; et al. Insecticide toxic effects and blood biochemical alterations in occupationally exposed individuals in Punjab, Pakistan. Sci. Total Environ. 2019, 655, 102–111. [Google Scholar] [CrossRef]
- Moon, J.W.; Moon, J.M.; Lee, B.K.; Roo, H.H. Prognostic predictors of endosulfan intoxication. J. Korean Soc. Emerg. Med. 2009, 20, 185–191. [Google Scholar]
- Kido, K.; Fujii, Y.; Kato, Y.; Ohta, C.; Koga, N.; Haraguchi, K. Concentrations and dietary exposure to persistent organic pollutants and naturally occurring halogenated contaminants in edible shrimp from Japanese coastal waters and the South China Sea. Chemosphere 2025, 375, 144226. [Google Scholar] [CrossRef]
- Ugranli, T.; Gungormus, E.; Kavcar, P.; Demircioglu, E.; Odabasi, M.; Sofuoglu, S.C.; Lammel, G.; Sofuoglu, A. POPs in a major conurbation in Turkey: Ambient air concentrations, seasonal variation, inhalation and dermal exposure, and associated carcinogenic risks. Environ. Sci. Pollut. Res. Int. 2016, 23, 22500–22512. [Google Scholar] [CrossRef] [PubMed]
- Hung, H.; Kallenborn, R.; Breivik, K.; Su, Y.; Brorström-Lundén, E.; Olafsdottir, K.; Thorlacius, J.M.; Leppänen, S.; Bossi, R.; Skov, H.; et al. Atmospheric monitoring of organic pollutants in the Arctic under the Arctic Monitoring and Assessment Programme (AMAP): 1993-2006. Sci. Total Environ. 2010, 408, 2854–2873. [Google Scholar] [CrossRef] [PubMed]
- Lee, I.; Eriksson, P.; Fredriksson, A.; Buratovic, S.; Viberg, H. Developmental neurotoxic effects of two pesticides: Behavior and neuroprotein studies on endosulfan and cypermethrin. Toxicology 2015, 335, 1–10. [Google Scholar] [CrossRef]
- Botella, B.; Crespo, J.; Rivas, A.; Cerrillo, I.; Olea-Serrano, M.F.; Olea, N. Exposure of women to organochlorine pesticides in Southern Spain. Environ. Res. 2004, 96, 34–40. [Google Scholar] [CrossRef]
- Fan, Y.; Bao, J.; Wu, Y.; Lou, X.; Chen, D.; Jiang, J.; Han, J.; Yang, Y.; Qiao, Y.; Hou, L.; et al. Affinity of endosulfan and HCB with human serum albumin affects serum concentrations in a general population. Emerg. Contam. 2025, 11, 100392. [Google Scholar] [CrossRef]
- Carreño, J.; Rivas, A.; Granada, A.; Jose Lopez-Espinosa, M.; Mariscal, M.; Olea, N.; Olea-Serrano, F. Exposure of young men to organochlorine pesticides in Southern Spain. Environ. Res. 2007, 103, 55–61. [Google Scholar] [CrossRef] [PubMed]
- Cabrera-Rodríguez, R.; Luzardo, O.P.; Almeida-González, M.; Boada, L.D.; Zumbado, M.; Henríquez-Hernández, L.A. Database of persistent organic pollutants in umbilical cord blood: Concentration of organochlorine pesticides, PCBs, BDEs and polycyclic aromatic hydrocarbons. Data Brief. 2019, 28, 104918. [Google Scholar] [CrossRef]
- Odongo, S.; Ssebugere, P.; Spencer, P.S.; Palmer, V.S.; Angues, R.V.; Mwaka, A.D.; Wasswa, J. Organochlorine pesticides and their markers of exposure in serum and urine of children from a nodding syndrome hotspot in northern Uganda, east Africa. Chemosphere 2024, 364, 143191. [Google Scholar] [CrossRef]
- Neild, G.H.; Viswanathan, S.; Jayakrishnan, K.S.; Vijan, V. Endosulfan and black urine. NDT Plus. 2011, 4, 353. [Google Scholar] [CrossRef]
- Silva, M.H. Investigating open access new approach methods (NAM) to assess biological points of departure: A case study with 4 neurotoxic pesticides. Curr. Res. Toxicol. 2024, 6, 100156. [Google Scholar] [CrossRef] [PubMed]
- Silva, M.H.; Beauvais, S.L. Human health risk assessment of endosulfan: Toxicology and hazard identification. Regul. Toxicol. Pharmacol. 2010, 56, 4–17. [Google Scholar] [CrossRef]
- van Melis, L.V.J.; Peerdeman, A.M.; Huiberts, E.H.W.; van Kleef, R.G.D.M.; de Groot, A.; Westerink, R.H.S. Effects of acute insecticide exposure on neuronal activity in vitro in rat cortical cultures. Neurotoxicology 2024, 102, 58–67. [Google Scholar] [CrossRef] [PubMed]
- Sohn, H.Y.; Kwon, C.S.; Kwon, G.S.; Lee, J.B.; Kim, E. Induction of oxidative stress by endosulfan and protective effect of lipid-soluble antioxidants against endosulfan-induced oxidative damage. Toxicol. Lett. 2004, 151, 357–365. [Google Scholar] [CrossRef]
- Ahmed, T.; Tripathi, A.K.; Ahmed, R.S.; Das, S.; Suke, S.G.; Pathak, R.; Chakraboti, A.; Banerjee, B.D. Endosulfan-induced apoptosis and glutathione depletion in human peripheral blood mononuclear cells: Attenuation by N-acetylcysteine. J. Biochem. Mol. Toxicol. 2008, 22, 299–304. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Zhang, L.; Ren, L.; Zhang, J.; Yu, Y.; Wang, J.; Duan, J.; Peng, C.; Sun, Z.; Zhou, X. Endosulfan inhibits proliferation through the Notch signaling pathway in human umbilical vein endothelial cells. Environ. Pollut. 2017, 221, 26–36. [Google Scholar] [CrossRef]
- Zervos, I.A.; Nikolaidis, E.; Lavrentiadou, S.N.; Tsantarliotou, M.P.; Eleftheriadou, E.K.; Papapanagiotou, E.P.; Fletouris, D.J.; Georgiadis, M.; Taitzoglou, I.A. Endosulfan-induced lipid peroxidation in rat brain and its effect on t-PA and PAI-1: Ameliorating effect of vitamins C and E. J. Toxicol. Sci. 2011, 36, 423–433. [Google Scholar] [CrossRef] [PubMed]
- Richardson, J.R.; Fitsanakis, V.; Westerink, R.H.S.; Kanthasamy, A.G. Neurotoxicity of pesticides. Acta Neuropathol. 2019, 138, 343–362. [Google Scholar] [CrossRef]
- Qi, S.Y.; Xu, X.L.; Ma, W.Z.; Deng, S.L.; Lian, Z.X.; Yu, K. Effects of organochlorine pesticide residues in maternal body on infants. Front. Endocrinol. 2022, 13, 890307. [Google Scholar] [CrossRef]
- Yavuz, Y.; Yurumez, Y.; Kucuker, H.; Ela, Y.; Yuksel, S. Two cases of acute endosulfan toxicity. Clin. Toxicol. 2007, 45, 530–532. [Google Scholar] [CrossRef] [PubMed]
- Talbott, E.O.; Malek, A.M.; Arena, V.C.; Wu, F.; Steffes, K.; Sharma, R.K.; Buchanich, J.; Rager, J.R.; Bear, T.; Hoffman, C.A.; et al. Case-control study of environmental toxins and risk of amyotrophic lateral sclerosis involving the national ALS registry. Amyotroph. Lateral Scler. Frontotemporal. Degener. 2024, 25, 533–542. [Google Scholar] [CrossRef]
- Lu, Y.; Morimoto, K.; Takeshita, T.; Takeuchi, T.; Saito, T. Genotoxic effects of aendosulfan and b-endosulfan on human HepG2 cells. Environ. Health Perspect. 2000, 108, 559–561. [Google Scholar] [CrossRef] [PubMed]
- Li, D.; Liu, J.; Li, J. Genotoxic evaluation of the insecticide endosulfan based on the induced GADD153-GFP reporter gene expression. Environ. Monit. Assess. 2011, 176, 251–258. [Google Scholar] [CrossRef]
- Sebastian, R.; Raghavan, S.C. Induction of DNA damage and erroneous repair can explain genomic instability caused by endosulfan. Carcinogenesis 2016, 37, 929–940. [Google Scholar] [CrossRef] [PubMed]
- Sebastian, R.; Raghavan, S.C. Exposure to Endosulfan can result in male infertility due to testicular atrophy and reduced sperm count. Cell Death Discov. 2015, 1, 15020. [Google Scholar] [CrossRef]
- Milesi, M.M.; Alarcón, R.; Ramos, J.G.; Muñoz-de-Toro, M.; Luque, E.H.; Varayoud, J. Neonatal exposure to low doses of endosulfan induces implantation failure and disrupts uterine functional differentiation at the pre-implantation period in rats. Mol. Cell. Endocrinol. 2015, 401, 248–259. [Google Scholar] [CrossRef]
- Felisbino, K.; Milhorini, S.D.S.; Kirsten, N.; Bernert, K.; Schiessl, R.; Guiloski, I.C. Exposure to pesticides during pregnancy and the risk of neural tube defects: A systematic review. Sci. Total Environ. 2024, 913, 169317. [Google Scholar] [CrossRef]
- Kalra, S.; Dewan, P.; Batra, P.; Sharma, T.; Tyagi, V.; Banerjee, B.D. Organochlorine pesticide exposure in mothers and neural tube defects in offsprings. Reprod. Toxicol. 2016, 66, 56–60. [Google Scholar] [CrossRef]
- Attaullah, M.; Yousuf, M.J.; Shaukat, S.; Anjum, S.I.; Ansari, M.J.; Buneri, I.D.; Tahir, M.; Amin, M.; Ahmad, N.; Khan, S.U. Serum organochlorine pesticides residues and risk of cancer: A case-control study. Saudi J. Biol. Sci. 2018, 25, 1284–1290. [Google Scholar] [CrossRef]
- Kalinina, T.; Kononchuk, V.; Klyushova, L.; Gulyaeva, L. Effects of endocrine disruptors o,p’-Dichlorodiphenyltrichloroethane, p,p’-Dichlorodiphenyltrichloroethane, and Endosulfan on the expression of Estradiol-, Progesterone-, and Testosterone-responsive MicroRNAs and their target genes in MCF-7 cells. Toxics 2022, 10, 25. [Google Scholar] [CrossRef] [PubMed]
- Xu, D.; Liu, T.; Lin, L.; Li, S.; Hang, X.; Sun, Y. Exposure to endosulfan increases endothelial permeability by transcellular and paracellular pathways in relations to cardiovascular diseases. Environ. Pollut. 2017, 223, 111–119. [Google Scholar] [CrossRef]
- Wei, J.; Zhang, L.; Wang, J.; Guo, F.; Li, Y.; Zhou, X.; Sun, Z. Endosulfan inducing blood hypercoagulability and endothelial cells apoptosis via the death receptor pathway in Wistar rats. Toxicol. Res. 2015, 4, 1282–1288. [Google Scholar] [CrossRef]
- Zhang, B.; Liu, S.; Sun, Y.; Xu, D. Endosulfan induced kidney cell injury by modulating ACE2 through up-regulating miR-429 in HK-2 cells. Toxicology 2023, 484, 153392. [Google Scholar] [CrossRef]
- Caride, A.; Lafuente, A.; Cabaleiro, T. Endosulfan effects on pituitary12.hormone and both nitrosative and oxidative stress in pubertal malerats. Toxicol. Lett. 2010, 197, 106–112. [Google Scholar] [CrossRef]
- Wang, X.; Gao, M.; Tan, Y.; Li, Q.; Chen, J.; Lan, C.; Jiangtulu, B.; Wang, B.; Shen, G.; Yu, Y.; et al. Associations of dietary exposure to organochlorine pesticides from plant-origin foods with lipid metabolism and inflammation in women: A multiple follow-up study in North China. Bull. Environ. Contam. Toxicol. 2021, 107, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Ramaswamy, S.; Puri, G.D.; Rajeev, S. Endosulfan poisoning with intravascular hemolysis. J. Emerg. Med. 2008, 34, 295–297. [Google Scholar] [CrossRef]
- Jain, G.; Singh, D.K.; Yadav, G. Malignant hyperthermia in endosulfan poisoning. Toxicol. Int. 2012, 19, 74–76. [Google Scholar] [CrossRef]
- Sharma, R.K.; Kaul, A.; Gupta, A.; Bhadauria, D.; Prasad, N.; Jain, A.; Gurjar, M.; Rao, B.P. High anion gap refractory metabolic acidosis as a critical presentation of endosulfan poisoning. Indian J. Pharmacol. 2011, 43, 469–471. [Google Scholar] [CrossRef]
- Moses, V.; Peter, J.V. Acute intentional toxicity: Endosulfan and other organochlorines. Clin. Toxicol. 2010, 48, 539–544. [Google Scholar] [CrossRef]
- Moon, J.M.; Chun, B.J.; Lee, S.D. In-hospital outcomes and delayed neurologic sequelae of seizure-related endosulfan poisoning. Seizure 2017, 51, 43–49. [Google Scholar] [CrossRef] [PubMed]
- Boereboom, F.T.; van Dijk, A.; van Zoonen, P.; Meulenbelt, J. Nonaccidental endosulfan intoxication: A case report with toxicokinetic calculations and tissue concentrations. J. Toxicol. Clin. Toxicol. 1998, 36, 345–352. [Google Scholar] [CrossRef]
- Isman, M.B. Botanical insecticides, deterrents, and repellents in modern agriculture and an increasingly regulated world. Annu. Rev. Entomol. 2006, 51, 45–66. [Google Scholar] [CrossRef] [PubMed]
- Babendreier, D.; Koku Agboyi, L.; Beseh, P.; Osae, M.; Nboyine, J.; Ofori, S.E.K.; Frimpong, J.O.; Attuquaye Clottey, V.; Kenis, M. The efficacy of alternative, environmentally friendly plant protection measures for control of Fall Armyworm, Spodoptera Frugiperda, in Maize. Insects 2020, 11, 240. [Google Scholar] [CrossRef] [PubMed]
- Casida, J.E.; Quistad, G.B. Golden age of insecticide research: Past, present, or future? Annu. Rev. Entomol. 1998, 43, 1–16. [Google Scholar] [CrossRef]
- Dively, G.P.; Patton, T.; Barranco, L.; Kulhanek, K. Comparative efficacy of common active ingredients in organic insecticides against difficult to control insect pests. Insects 2020, 11, 614. [Google Scholar] [CrossRef]
- Aioub, A.A.A.; Ghosh, S.; AL-Farga, A.; Khan, A.N.; Bibi, R.; Elwakeel, A.M.; Nawaz, A.; Sherif, N.T.; Elmasry, S.A.; Ammar, E.E. Back to the origins: Biopesticides as promising alternatives to conventional agrochemicals. Eur. J. Plant Pathol. 2024, 169, 697–713. [Google Scholar] [CrossRef]
- Samada, L.H.; Tambunan, U.S.F. Biopesticides as promising alternatives to chemical pesticides: A review of their current and future status. OnLine J. Biol. Sci. 2020, 20, 66–76. [Google Scholar] [CrossRef]
- Nicholls, C.I.; Altieri, M.A.; Vazquez, L. Agroecology: Principles for the conversion and redesign of farming systems. J. Ecosys. Ecograph. 2016, S5, 010. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berdowska, A.; Bandurska, K. Health Hazards Associated with Exposure to Endosulfan: A Mini-Review. Toxics 2025, 13, 455. https://doi.org/10.3390/toxics13060455
Berdowska A, Bandurska K. Health Hazards Associated with Exposure to Endosulfan: A Mini-Review. Toxics. 2025; 13(6):455. https://doi.org/10.3390/toxics13060455
Chicago/Turabian StyleBerdowska, Agnieszka, and Katarzyna Bandurska. 2025. "Health Hazards Associated with Exposure to Endosulfan: A Mini-Review" Toxics 13, no. 6: 455. https://doi.org/10.3390/toxics13060455
APA StyleBerdowska, A., & Bandurska, K. (2025). Health Hazards Associated with Exposure to Endosulfan: A Mini-Review. Toxics, 13(6), 455. https://doi.org/10.3390/toxics13060455





