Pathophysiology of Doxorubicin-Mediated Cardiotoxicity
Abstract
1. Introduction
2. Major Pathogenetic Mechanisms of DIC
2.1. DNA Instability and Topoisomerase Inhibition
2.2. Oxidative Stress
2.3. Autophagy
2.4. Inflammation
2.5. Apoptosis and Ferroptosis
3. Role of Sirtuins in DIC
4. Role of Natural Products in DIC
Therapeutic Attempts to Reduce DIC
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CATI | Catalase |
| DICJ | Doxorubicin-induced cardiotoxicity |
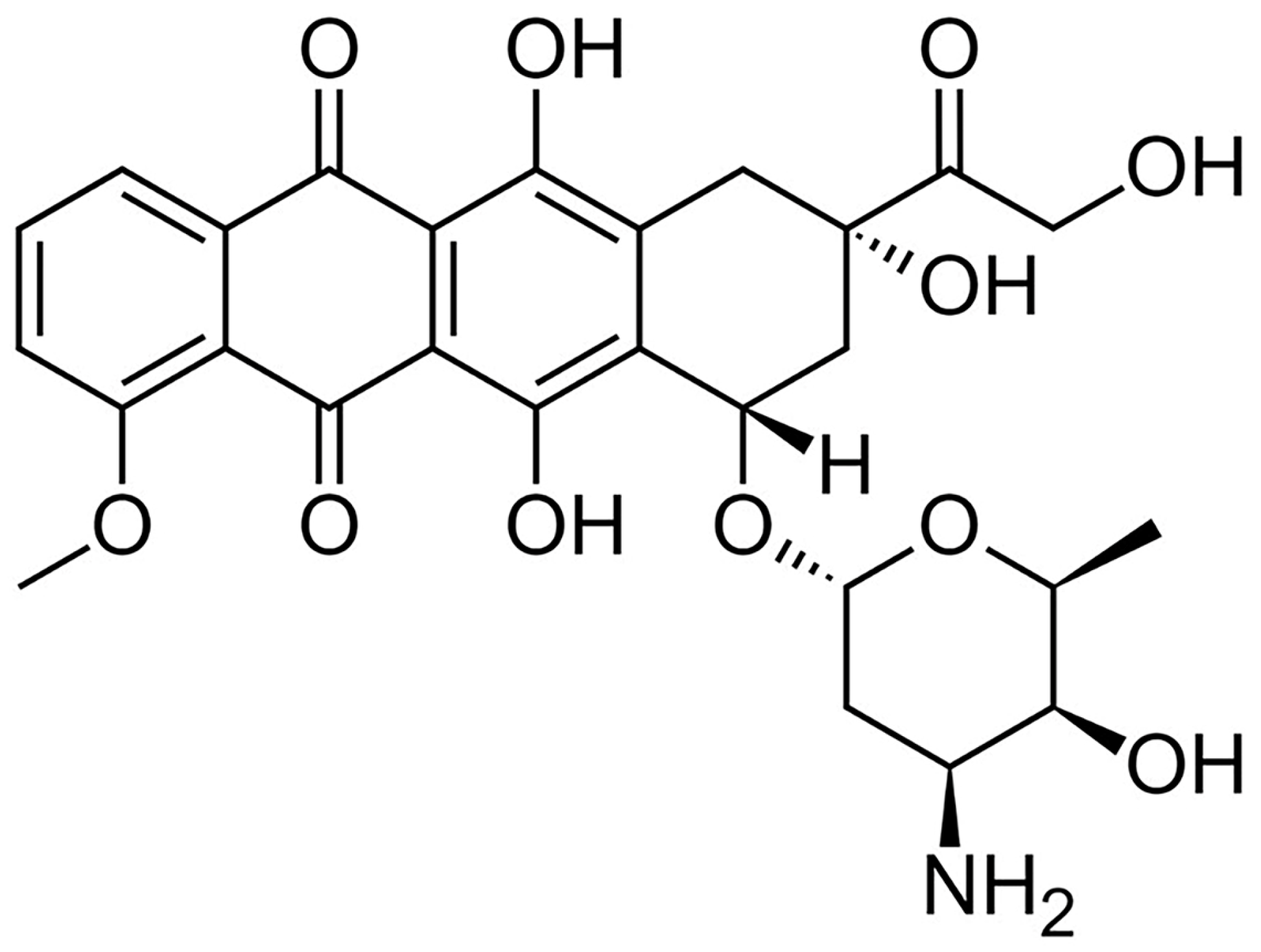
| DOX | Doxorubicin |
| ER | Endoplasmic reticulum |
| GPx4 | Glutathione peroxidase 4 |
| IL | Interleukin |
| MnSOD | Manganese superoxide dismutase |
| NLRP3 | Nod-like receptor thermal protein domain-associated protein 3 |
| NO | Nitric oxide |
| NOX | NADH oxidase |
| RBP | RNA-binding protein |
| RES | Resveratrol |
| ROS | Reactive oxygen species |
| SIRT | Sirtuins |
| TLR | Toll-like receptor |
| YAP | Yes-associated protein |
References
- Cardinale, D.; Colombo, A.; Bacchiani, G.; Tedeschi, I.; Meroni, C.A.; Veglia, F.; Civelli, M.; Lamantia, G.; Colombo, N.; Curigliano, G.; et al. Early detection of anthracycline cardiotoxicity and improvement with heart failure therapy. Circulation 2015, 131, 1981–1988. [Google Scholar] [CrossRef]
- Hudson, M.M.; Ness, K.K.; Gurney, J.G.; Mulrooney, D.A.; Chemaitilly, W.; Krull, K.R.; Green, D.M.; Armstrong, G.T.; Nottage, K.A.; Jones, K.E.; et al. Clinical ascertainment of health outcomes among adults treated for childhood cancer. JAMA 2013, 309, 2371–2381. [Google Scholar] [CrossRef]
- Li, D.L.; Hill, J.A. Cardiomyocyte autophagy and cancer chemotherapy. J. Mol. Cell. Cardiol. 2014, 71, 54–61. [Google Scholar] [CrossRef]
- Lyon, A.R.; López-Fernández, T.; Couch, L.S.; Asteggiano, R.; Aznar, M.C.; Bergler-Klein, J.; Boriani, G.; Cardinale, D.; Cordoba, R.; Cosyns, B.; et al. 2022 ESC Guidelines on cardio-oncology developed in collaboration with the European Hematology Association (EHA), the European Society for Therapeutic Radiology and Oncology (ESTRO) and the International Cardio-Oncology Society (IC-OS). Eur. Heart J. 2022, 43, 4229–4361. [Google Scholar] [CrossRef]
- Drafts, B.C.; Twomley, K.M.; D’Agostino, R.; Lawrence, J.; Avis, N.; Ellis, L.R.; Thohan, V.; Jordan, J.; Melin, S.A.; Torti, F.M.; et al. Low to moderate dose anthracycline-based chemotherapy is associated with early noninvasive imaging evidence of subclinical cardiovascular disease. JACC Cardiovasc. Imaging 2013, 6, 877–885. [Google Scholar] [CrossRef]
- Luminari, S.; Montanini, A.; Caballero, D.; Bologna, S.; Notter, M.; Dyer, M.J.S.; Chiappella, A.; Briones, J.; Petrini, M.; Barbato, A.; et al. Nonpegylated liposomal doxorubicin (MyocetTM) combination (R-COMP) chemotherapy in elderly patients with diffuse large B-cell lymphoma (DLBCL): Results from the phase II EUR018 trial. Ann. Oncol. Off. J. Eur. Soc. Med. Oncol. 2010, 21, 1492–1499. [Google Scholar] [CrossRef]
- Mukku, R.B.; Fonarow, G.C.; Watson, K.E.; Ajijola, O.A.; Depasquale, E.C.; Nsair, A.; Baas, A.S.; Deng, M.C.; Yang, E.H. Heart Failure Therapies for End-Stage Chemotherapy-Induced Cardiomyopathy. J. Card. Fail. 2016, 22, 439–448. [Google Scholar] [CrossRef]
- Curigliano, G.; Cardinale, D.; Dent, S.; Criscitiello, C.; Aseyev, O.; Lenihan, D.; Cipolla, C.M. Cardiotoxicity of anticancer treatments: Epidemiology, detection, and management. CA. Cancer J. Clin. 2016, 66, 309–325. [Google Scholar] [CrossRef]
- Zamorano, J.L.; Lancellotti, P.; Muñoz, D.R.; Aboyans, V.; Asteggiano, R.; Galderisi, M.; Habib, G.; Lenihan, D.J.; Lip, G.Y.H.; Lyon, A.R.; et al. 2016 ESC Position Paper on cancer treatments and cardiovascular toxicity developed under the auspices of the ESC Committee for Practice Guidelines: The Task Force for cancer treatments and cardiovascular toxicity of the European Society of Cardiology (ESC). Eur. Heart J. 2016, 37, 2768–2801. [Google Scholar] [CrossRef]
- Linders, A.N.; Dias, I.B.; Fernández, L.T.; Tocchetti, C.G.; Bomer, N.; Van der Meer, P. A review of the pathophysiological mechanisms of doxorubicin-induced cardiotoxicity and aging. npj Aging 2024, 10, 9. [Google Scholar] [CrossRef]
- Belger, C.; Abrahams, C.; Imamdin, A.; Lecour, S. Doxorubicin-induced cardiotoxicity and risk factors. Int. J. Cardiol. Heart Vasc. 2024, 50, 101332. [Google Scholar] [CrossRef]
- Picano, E. Sustainability of medical imaging. BMJ 2004, 328, 578–580. [Google Scholar] [CrossRef]
- Upshaw, J.N.; Finkelman, B.; Hubbard, R.A.; Smith, A.M.; Narayan, H.K.; Arndt, L.; Domchek, S.; DeMichele, A.; Fox, K.; Shah, P.; et al. Comprehensive Assessment of Changes in Left Ventricular Diastolic Function With Contemporary Breast Cancer Therapy. JACC Cardiovasc. Imaging 2020, 13, 198–210. [Google Scholar] [CrossRef]
- Caiati, C.; Argentiero, A.; Forleo, C.; Favale, S.; Lepera, M.E. Predictors of Exercise Capacity in Dilated Cardiomyopathy with Focus on Pulmonary Venous Flow Recorded with Transesophageal Eco-Doppler. J. Clin. Med. 2021, 10, 5954. [Google Scholar] [CrossRef]
- Demissei, B.G.; Hubbard, R.A.; Zhang, L.; Smith, A.M.; Sheline, K.; McDonald, C.; Narayan, V.; Domchek, S.M.; DeMichele, A.; Shah, P.; et al. Changes in Cardiovascular Biomarkers with Breast Cancer Therapy and Associations with Cardiac Dysfunction. J. Am. Heart Assoc. 2020, 9, e014708. [Google Scholar] [CrossRef]
- Mohammed, T.; Singh, M.; Tiu, J.G.; Kim, A.S. Etiology and management of hypertension in patients with cancer. Cardio-Oncol. Lond. Engl. 2021, 7, 14. [Google Scholar] [CrossRef]
- Qiu, S.; Zhou, T.; Qiu, B.; Zhang, Y.; Zhou, Y.; Yu, H.; Zhang, J.; Liu, L.; Yuan, L.; Yang, G.; et al. Risk Factors for Anthracycline-Induced Cardiotoxicity. Front. Cardiovasc. Med. 2021, 8, 736854. [Google Scholar] [CrossRef]
- Volkova, M.; Russell, R. Anthracycline Cardiotoxicity: Prevalence, Pathogenesis and Treatment. Curr. Cardiol. Rev. 2011, 7, 214–220. [Google Scholar] [CrossRef]
- Gewirtz, D. A critical evaluation of the mechanisms of action proposed for the antitumor effects of the anthracycline antibiotics adriamycin and daunorubicin. Biochem. Pharmacol. 1999, 57, 727–741. [Google Scholar] [CrossRef]
- Cagel, M.; Grotz, E.; Bernabeu, E.; Moretton, M.A.; Chiappetta, D.A. Doxorubicin: Nanotechnological overviews from bench to bedside. Drug Discov. Today 2017, 22, 270–281. [Google Scholar] [CrossRef]
- Kciuk, M.; Gielecińska, A.; Mujwar, S.; Kołat, D.; Kałuzińska-Kołat, Ż.; Celik, I.; Kontek, R. Doxorubicin-An Agent with Multiple Mechanisms of Anticancer Activity. Cells 2023, 12, 659. [Google Scholar] [CrossRef]
- Jean, S.R.; Tulumello, D.V.; Riganti, C.; Liyanage, S.U.; Schimmer, A.D.; Kelley, S.O. Mitochondrial Targeting of Doxorubicin Eliminates Nuclear Effects Associated with Cardiotoxicity. ACS Chem. Biol. 2015, 10, 2007–2015. [Google Scholar] [CrossRef]
- Doroshow, J.H.; Locker, G.Y.; Myers, C.E. Enzymatic defenses of the mouse heart against reactive oxygen metabolites: Alterations produced by doxorubicin. J. Clin. Investig. 1980, 65, 128–135. [Google Scholar] [CrossRef]
- Sun, X.; Zhou, L.; Han, Y.; Yang, Q.; Li, X.; Xin, B.; Chi, M.; Wang, Y.; Guo, C. Scutellarin Attenuates Doxorubicin-Induced Cardiotoxicity by Inhibiting Myocardial Fibrosis, Apoptosis and Autophagy in Rats. Chem. Biodivers. 2023, 20, e202200450. [Google Scholar] [CrossRef]
- Pugazhendhi, A.; Edison, T.N.J.I.; Velmurugan, B.K.; Jacob, J.A.; Karuppusamy, I. Toxicity of Doxorubicin (Dox) to different experimental organ systems. Life Sci. 2018, 200, 26–30. [Google Scholar] [CrossRef]
- Yang, F.; Teves, S.S.; Kemp, C.J.; Henikoff, S. Doxorubicin, DNA torsion, and chromatin dynamics. Biochim. Et Biophys. Acta (BBA)—Rev. Cancer 2014, 1845, 84–89. [Google Scholar] [CrossRef]
- Renu, K.; Abilash, V.G.; P.B., T.P.; Arunachalam, S. Molecular mechanism of doxorubicin-induced cardiomyopathy—An update. Eur. J. Pharmacol. 2018, 818, 241–253. [Google Scholar] [CrossRef]
- Nedělníková, A.; Stadlbauer, P.; Otyepka, M.; Kührová, P.; Paloncýová, M. Atomistic Insights Into Interaction of Doxorubicin With DNA: From Duplex to Nucleosome. J. Comput. Chem. 2025, 46, e70035. [Google Scholar] [CrossRef] [PubMed]
- Zhu, W.; Yang, W.; Sun, G.; Huang, J. RNA-binding protein quaking: A multifunctional regulator in tumour progression. Ann. Med. 2025, 57, 2443046. [Google Scholar] [CrossRef] [PubMed]
- Songbo, M.; Lang, H.; Xinyong, C.; Bin, X.; Ping, Z.; Liang, S. Oxidative stress injury in doxorubicin-induced cardiotoxicity. Toxicol. Lett. 2019, 307, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Saleh, M.F.; Elsayad, M.E.; Goda, A.E. Mitigation of doxorubicin-induced cardiotoxicity by dichloroacetate: Potential roles of restoration of PGC-1α/SIRT3 signaling and suppression of oxidative stress and apoptosis. Eur. Rev. Med. Pharmacol. Sci. 2021, 25, 6573–6584. [Google Scholar] [CrossRef] [PubMed]
- Doroshow, J.H.; Davies, K.J. Redox cycling of anthracyclines by cardiac mitochondria. II. Formation of superoxide anion, hydrogen peroxide, and hydroxyl radical. J. Biol. Chem. 1986, 261, 3068–3074. [Google Scholar]
- Sangomla, S.; Saifi, M.A.; Khurana, A.; Godugu, C. Nanoceria ameliorates doxorubicin induced cardiotoxicity: Possible mitigation via reduction of oxidative stress and inflammation. J. Trace Elem. Med. Biol. 2018, 47, 53–62. [Google Scholar] [CrossRef]
- Pecoraro, M.; Pala, B.; Di Marcantonio, M.C.; Muraro, R.; Marzocco, S.; Pinto, A.; Mincione, G.; Popolo, A. Doxorubicin-induced oxidative and nitrosative stress: Mitochondrial connexin 43 is at the crossroads. Int. J. Mol. Med. 2020, 46, 1197–1209. [Google Scholar] [CrossRef] [PubMed]
- Mukhopadhyay, P.; Rajesh, M.; Bátkai, S.; Kashiwaya, Y.; Haskó, G.; Liaudet, L.; Szabó, C.; Pacher, P. Role of superoxide, nitric oxide, and peroxynitrite in doxorubicin-induced celldeath in vivo and in vitro. Am. J. Physiol. Heart Circ. Physiol. 2009, 296, H1466–H1483. [Google Scholar] [CrossRef] [PubMed]
- Li, D.L.; Wang, Z.V.; Ding, G.; Tan, W.; Luo, X.; Criollo, A.; Xie, M.; Jiang, N.; May, H.; Kyrychenko, V.; et al. Doxorubicin Blocks Cardiomyocyte Autophagic Flux by Inhibiting Lysosome Acidification. Circulation 2016, 133, 1668–1687. [Google Scholar] [CrossRef]
- Podyacheva, E.; Danilchuk, M.; Toropova, Y. Molecular mechanisms of endothelial remodeling under doxorubicin treatment. Biomed. Pharmacother. Biomed. Pharmacother. 2023, 162, 114576. [Google Scholar] [CrossRef]
- Ma, K.; Xu, Q.; Wang, S.; Zhang, W.; Liu, M.; Liang, S.; Zhu, H.; Xu, N. Nuclear accumulation of Yes-Associated Protein (YAP) maintains the survival of doxorubicin-induced senescent cells by promoting survivin expression. Cancer Lett. 2016, 375, 84–91. [Google Scholar] [CrossRef]
- She, G.; Du, J.-C.; Wu, W.; Pu, T.-T.; Zhang, Y.; Bai, R.-Y.; Zhang, Y.; Pang, Z.-D.; Wang, H.-F.; Ren, Y.-J.; et al. Hippo pathway activation mediates chemotherapy-induced anti-cancer effect and cardiomyopathy through causing mitochondrial damage and dysfunction. Theranostics 2023, 13, 560–577. [Google Scholar] [CrossRef]
- Takaguri, A.; Akihiro, O.; Sasano, J.; Satoh, K. Involvement of Yes-associated protein 1 (YAP1) in doxorubicin-induced cytotoxicity in H9c2 cardiac cells. Cell Biol. Int. 2020, 44, 873–881. [Google Scholar] [CrossRef]
- Aman, Y.; Schmauck-Medina, T.; Hansen, M.; Morimoto, R.I.; Simon, A.K.; Bjedov, I.; Palikaras, K.; Simonsen, A.; Johansen, T.; Tavernarakis, N.; et al. Autophagy in healthy aging and disease. Nat. Aging 2021, 1, 634–650. [Google Scholar] [CrossRef] [PubMed]
- Xiao, B.; Hong, L.; Cai, X.; Mei, S.; Zhang, P.; Shao, L. The true colors of autophagy in doxorubicin-induced cardiotoxicity (Review). Oncol. Lett. 2019, 18, 2165–2172. [Google Scholar] [CrossRef] [PubMed]
- Yin, J.; Guo, J.; Zhang, Q.; Cui, L.; Zhang, L.; Zhang, T.; Zhao, J.; Li, J.; Middleton, A.; Carmichael, P.L.; et al. Doxorubicin-induced mitophagy and mitochondrial damage is associated with dysregulation of the PINK1/parkin pathway. Toxicol. Vitro Int. J. Publ. Assoc. BIBRA 2018, 51, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Varela-López, A.; Battino, M.; Navarro-Hortal, M.D.; Giampieri, F.; Forbes-Hernández, T.Y.; Romero-Márquez, J.M.; Collado, R.; Quiles, J.L. An update on the mechanisms related to cell death and toxicity of doxorubicin and the protective role of nutrients. Food Chem. Toxicol. Int. J. Publ. Br. Ind. Biol. Res. Assoc. 2019, 134, 110834. [Google Scholar] [CrossRef]
- Abdullah, C.S.; Alam, S.; Aishwarya, R.; Miriyala, S.; Bhuiyan, M.A.N.; Panchatcharam, M.; Pattillo, C.B.; Orr, A.W.; Sadoshima, J.; Hill, J.A.; et al. Doxorubicin-induced cardiomyopathy associated with inhibition of autophagic degradation process and defects in mitochondrial respiration. Sci. Rep. 2019, 9, 2002. [Google Scholar] [CrossRef]
- Toda, N.; Sato, T.; Muraoka, M.; Lin, D.; Saito, M.; Li, G.; Song, Q.-C.; Yanagisawa, T.; Yamauchi, M. Doxorubicin induces cardiomyocyte death owing to the accumulation of dysfunctional mitochondria by inhibiting the autophagy fusion process. Free Radic. Biol. Med. 2023, 195, 47–57. [Google Scholar] [CrossRef]
- Li, X.; Wang, X.; Wang, B.; Chi, W.; Li, Z.; Zhang, M.; Shen, Y.; Liu, X.; Lu, Y.; Liu, Y. Dihydromyricetin protects against Doxorubicin-induced cardiotoxicity through activation of AMPK/mTOR pathway. Phytomedicine Int. J. Phytother. Phytopharm. 2022, 99, 154027. [Google Scholar] [CrossRef]
- Abdel-Daim, M.M.; Kilany, O.E.; Khalifa, H.A.; Ahmed, A.A.M. Allicin ameliorates doxorubicin-induced cardiotoxicity in rats via suppression of oxidative stress, inflammation and apoptosis. Cancer Chemother. Pharmacol. 2017, 80, 745–753. [Google Scholar] [CrossRef]
- Bagchi, A.K.; Malik, A.; Akolkar, G.; Jassal, D.S.; Singal, P.K. Endoplasmic Reticulum Stress Promotes iNOS/NO and Influences Inflammation in the Development of Doxorubicin-Induced Cardiomyopathy. Antioxidants 2021, 10, 1897. [Google Scholar] [CrossRef]
- Yarmohammadi, F.; Karbasforooshan, H.; Hayes, A.W.; Karimi, G. Inflammation suppression in doxorubicin-induced cardiotoxicity: Natural compounds as therapeutic options. Naunyn. Schmiedebergs Arch. Pharmacol. 2021, 394, 2003–2011. [Google Scholar] [CrossRef]
- Ye, S.; Su, L.; Shan, P.; Ye, B.; Wu, S.; Liang, G.; Huang, W. LCZ696 Attenuated Doxorubicin-Induced Chronic Cardiomyopathy Through the TLR2-MyD88 Complex Formation. Front. Cell Dev. Biol. 2021, 9, 654051. [Google Scholar] [CrossRef] [PubMed]
- Wei, S.; Ma, W.; Li, X.; Jiang, C.; Sun, T.; Li, Y.; Zhang, B.; Li, W. Involvement of ROS/NLRP3 Inflammasome Signaling Pathway in Doxorubicin-Induced Cardiotoxicity. Cardiovasc. Toxicol. 2020, 20, 507–519. [Google Scholar] [CrossRef]
- Ye, B.; Shi, X.; Xu, J.; Dai, S.; Xu, J.; Fan, X.; Han, B.; Han, J. Gasdermin D mediates doxorubicin-induced cardiomyocyte pyroptosis and cardiotoxicity via directly binding to doxorubicin and changes in mitochondrial damage. Transl. Res. J. Lab. Clin. Med. 2022, 248, 36–50. [Google Scholar] [CrossRef]
- Lan, Y.; Wang, Y.; Huang, K.; Zeng, Q. Heat Shock Protein 22 Attenuates Doxorubicin-Induced Cardiotoxicity via Regulating Inflammation and Apoptosis. Front. Pharmacol. 2020, 11, 257. [Google Scholar] [CrossRef]
- Xu, A.; Deng, F.; Chen, Y.; Kong, Y.; Pan, L.; Liao, Q.; Rao, Z.; Xie, L.; Yao, C.; Li, S.; et al. NF-κB pathway activation during endothelial-to-mesenchymal transition in a rat model of doxorubicin-induced cardiotoxicity. Biomed. Pharmacother. Biomedecine Pharmacother. 2020, 130, 110525. [Google Scholar] [CrossRef]
- Avagimyan, A.A.; Mkrtchyan, L.H.; Gevorkyan, A.A.; Kononchuk, N.B.; Kakturskiy, L.V.; Djndoyan, Z.T. Relationship between Chemotherapy and Atrial Fibrillation: Clinical Case. Ration. Pharmacother. Cardiol. 2021, 17, 785–791. [Google Scholar] [CrossRef]
- Cerasuolo, F.A.; Gambardella, J.; Santulli, G.; Fiordelisi, A.; Wang, X.; Prevete, N.; Sommella, E.; Avvisato, R.; Buonaiuto, A.; Altobelli, G.G.; et al. Macrophages participate in doxorubicin-induced cardiac damage. Vascul. Pharmacol. 2024, 155, 107309. [Google Scholar] [CrossRef]
- Caiati, C.; Jirillo, E. The Immune System, An Arrow into the Heart. Principles of Cardioimmunology, An Emerging Branch in Medicine. Curr. Vasc. Pharmacol. 2025, 23, 162–171. [Google Scholar] [CrossRef]
- Kitakata, H.; Endo, J.; Ikura, H.; Moriyama, H.; Shirakawa, K.; Katsumata, Y.; Sano, M. Therapeutic Targets for DOX-Induced Cardiomyopathy: Role of Apoptosis vs. Ferroptosis. Int. J. Mol. Sci. 2022, 23, 1414. [Google Scholar] [CrossRef]
- Zhu, J.; Zhang, X.; Xie, H.; Wang, Y.; Zhang, X.; Lin, Z. Cardiomyocyte Stim1 Deficiency Exacerbates Doxorubicin Cardiotoxicity by Magnification of Endoplasmic Reticulum Stress. J. Inflamm. Res. 2021, 14, 3945–3958. [Google Scholar] [CrossRef]
- Jiang, X.; Stockwell, B.R.; Conrad, M. Ferroptosis: Mechanisms, biology and role in disease. Nat. Rev. Mol. Cell Biol. 2021, 22, 266–282. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhou, L.; Du, B.; Liu, Y.; Xing, J.; Guo, S.; Li, L.; Chen, H. Protection against Doxorubicin-Related Cardiotoxicity by Jaceosidin Involves the Sirt1 Signaling Pathway. Oxid. Med. Cell. Longev. 2021, 2021, 9984330. [Google Scholar] [CrossRef]
- Tai, P.; Chen, X.; Jia, G.; Chen, G.; Gong, L.; Cheng, Y.; Li, Z.; Wang, H.; Chen, A.; Zhang, G.; et al. WGX50 mitigates doxorubicin-induced cardiotoxicity through inhibition of mitochondrial ROS and ferroptosis. J. Transl. Med. 2023, 21, 823. [Google Scholar] [CrossRef] [PubMed]
- Hirschhorn, T.; Stockwell, B.R. The development of the concept of ferroptosis. Free Radic. Biol. Med. 2019, 133, 130–143. [Google Scholar] [CrossRef]
- Zhuang, S.; Ma, Y.; Zeng, Y.; Lu, C.; Yang, F.; Jiang, N.; Ge, J.; Ju, H.; Zhong, C.; Wang, J.; et al. METTL14 promotes doxorubicin-induced cardiomyocyte ferroptosis by regulating the KCNQ1OT1-miR-7-5p-TFRC axis. Cell Biol. Toxicol. 2023, 39, 1015–1035. [Google Scholar] [CrossRef]
- Kawalec, P.; Martens, M.D.; Field, J.T.; Mughal, W.; Caymo, A.M.; Chapman, D.; Xiang, B.; Ghavami, S.; Dolinsky, V.W.; Gordon, J.W. Differential impact of doxorubicin dose on cell death and autophagy pathways during acute cardiotoxicity. Toxicol. Appl. Pharmacol. 2022, 453, 116210. [Google Scholar] [CrossRef] [PubMed]
- Matsushima, S.; Sadoshima, J. The role of sirtuins in cardiac disease. Am. J. Physiol. Heart Circ. Physiol. 2015, 309, H1375–H1389. [Google Scholar] [CrossRef]
- Wang, Y.; Li, Y.; Ding, H.; Li, D.; Shen, W.; Zhang, X. The Current State of Research on Sirtuin-Mediated Autophagy in Cardiovascular Diseases. J. Cardiovasc. Dev. Dis. 2023, 10, 382. [Google Scholar] [CrossRef]
- Hao, J.; Xi, Y.; Jiao, L.; Wen, X.; Wu, R.; Chang, G.; Sun, F.; Wei, C.; Li, H. Exogenous hydrogen sulfide inhibits the senescence of cardiomyocytes through modulating mitophagy in rats. Cell. Signal. 2022, 100, 110465. [Google Scholar] [CrossRef]
- Zhang, Q.; Zhang, Y.; Xie, B.; Liu, D.; Wang, Y.; Zhou, Z.; Zhang, Y.; King, E.; Tse, G.; Liu, T. Resveratrol activation of SIRT1/MFN2 can improve mitochondria function, alleviating doxorubicin-induced myocardial injury. Cancer Innov. 2023, 2, 253–264. [Google Scholar] [CrossRef]
- Li, S.; Zhu, Z.; Xue, M.; Yi, X.; Liang, J.; Niu, C.; Chen, G.; Shen, Y.; Zhang, H.; Zheng, J.; et al. Fibroblast growth factor 21 protects the heart from angiotensin II-induced cardiac hypertrophy and dysfunction via SIRT1. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2019, 1865, 1241–1252. [Google Scholar] [CrossRef] [PubMed]
- Ren, B.; Feng, J.; Yang, N.; Guo, Y.; Chen, C.; Qin, Q. Ginsenoside Rg3 attenuates angiotensin II-induced myocardial hypertrophy through repressing NLRP3 inflammasome and oxidative stress via modulating SIRT1/NF-κB pathway. Int. Immunopharmacol. 2021, 98, 107841. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Zhang, X.; Wang, S.; Shen, A.; Xu, T.; Hou, Y.; Gao, S.; Xie, Y.; Zeng, Y.; Chen, J.; et al. PARP-2 mediates cardiomyocyte aging and damage induced by doxorubicin through SIRT1 Inhibition. Apoptosis Int. J. Program. Cell Death 2024, 29, 816–834. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Huang, C.; Hou, Y.; Jiang, S.; Zhang, Y.; Wang, S.; Chen, J.; Lai, J.; Wu, L.; Duan, H.; et al. Research progress on the role and mechanism of Sirtuin family in doxorubicin cardiotoxicity. Phytomedicine 2024, 129, 155673. [Google Scholar] [CrossRef]
- Fu, Q.; Pan, H.; Tang, Y.; Rong, J.; Zheng, Z. MiR-200a-3p Aggravates DOX-Induced Cardiotoxicity by Targeting PEG3 Through SIRT1/NF-κB Signal Pathway. Cardiovasc. Toxicol. 2021, 21, 302–313. [Google Scholar] [CrossRef]
- Sun, Z.; Lu, W.; Lin, N.; Lin, H.; Zhang, J.; Ni, T.; Meng, L.; Zhang, C.; Guo, H. Dihydromyricetin alleviates doxorubicin-induced cardiotoxicity by inhibiting NLRP3 inflammasome through activation of SIRT1. Biochem. Pharmacol. 2020, 175, 113888. [Google Scholar] [CrossRef]
- Zhai, J.; Tao, L.; Zhang, S.; Gao, H.; Zhang, Y.; Sun, J.; Song, Y.; Qu, X. Calycosin ameliorates doxorubicin-induced cardiotoxicity by suppressing oxidative stress and inflammation via the sirtuin 1-NOD-like receptor protein 3 pathway. Phytother. Res. PTR 2020, 34, 649–659. [Google Scholar] [CrossRef]
- Zhang, C.; Feng, Y.; Qu, S.; Wei, X.; Zhu, H.; Luo, Q.; Liu, M.; Chen, G.; Xiao, X. Resveratrol attenuates doxorubicin-induced cardiomyocyte apoptosis in mice through SIRT1-mediated deacetylation of p53. Cardiovasc. Res. 2011, 90, 538–545. [Google Scholar] [CrossRef]
- Wang, W.; Zhong, X.; Fang, Z.; Li, J.; Li, H.; Liu, X.; Yuan, X.; Huang, W.; Huang, Z. Cardiac sirtuin1 deficiency exacerbates ferroptosis in doxorubicin-induced cardiac injury through the Nrf2/Keap1 pathway. Chem. Biol. Interact. 2023, 377, 110469. [Google Scholar] [CrossRef]
- Wu, S.; Lan, J.; Li, L.; Wang, X.; Tong, M.; Fu, L.; Zhang, Y.; Xu, J.; Chen, X.; Chen, H.; et al. Sirt6 protects cardiomyocytes against doxorubicin-induced cardiotoxicity by inhibiting P53/Fas-dependent cell death and augmenting endogenous antioxidant defense mechanisms. Cell Biol. Toxicol. 2023, 39, 237–258. [Google Scholar] [CrossRef]
- Tang, X.; Chen, X.-F.; Chen, H.-Z.; Liu, D.-P. Mitochondrial Sirtuins in cardiometabolic diseases. Clin. Sci. 2017, 131, 2063–2078. [Google Scholar] [CrossRef]
- Zhao, L.; Qi, Y.; Xu, L.; Tao, X.; Han, X.; Yin, L.; Peng, J. MicroRNA-140-5p aggravates doxorubicin-induced cardiotoxicity by promoting myocardial oxidative stress via targeting Nrf2 and Sirt2. Redox Biol. 2018, 15, 284–296. [Google Scholar] [CrossRef] [PubMed]
- Sun, W.; Liu, C.; Chen, Q.; Liu, N.; Yan, Y.; Liu, B. SIRT3: A New Regulator of Cardiovascular Diseases. Oxid. Med. Cell. Longev. 2018, 2018, 7293861. [Google Scholar] [CrossRef]
- LI, H.; Zhang, M.; Wang, Y.; Gong, K.; Yan, T.; Wang, D.; Meng, X.; Yang, X.; Chen, Y.; Han, J.; et al. Daidzein alleviates doxorubicin-induced heart failure via the SIRT3/FOXO3a signaling pathway. Food Funct. 2022, 13, 9576–9588. [Google Scholar] [CrossRef]
- Coelho, A.R.; Martins, T.R.; Couto, R.; Deus, C.; Pereira, C.V.; Simões, R.F.; Rizvanov, A.A.; Silva, F.; Cunha-Oliveira, T.; Oliveira, P.J.; et al. Berberine-induced cardioprotection and Sirt3 modulation in doxorubicin-treated H9c2 cardiomyoblasts. Biochim. Biophys. Acta Mol. Basis Dis. 2017, 1863, 2904–2923. [Google Scholar] [CrossRef]
- Tomczyk, M.M.; Cheung, K.G.; Xiang, B.; Tamanna, N.; Teixeira, A.L.F.; Agarwal, P.; Kereliuk, S.M.; Spicer, V.; Lin, L.; Treberg, J.; et al. Mitochondrial Sirtuin-3 (SIRT3) Prevents Doxorubicin-Induced Dilated Cardiomyopathy by Modulating Protein Acetylation and Oxidative Stress. Circ. Heart Fail. 2022, 15, e008547. [Google Scholar] [CrossRef]
- Zhang, J.; Li, W.; Xue, S.; Gao, P.; Wang, H.; Chen, H.; Hong, Y.; Sun, Q.; Lu, L.; Wang, Y.; et al. Qishen granule attenuates doxorubicin-induced cardiotoxicity by protecting mitochondrial function and reducing oxidative stress through regulation of Sirtuin3. J. Ethnopharmacol. 2024, 319, 117134. [Google Scholar] [CrossRef]
- Zhong, Z.; Gao, Y.; Zhou, J.; Wang, F.; Zhang, P.; Hu, S.; Wu, H.; Lou, H.; Chi, J.; Lin, H.; et al. Inhibiting mir-34a-5p regulates doxorubicin-induced autophagy disorder and alleviates myocardial pyroptosis by targeting Sirt3-AMPK pathway. Biomed. Pharmacother. 2023, 168, 115654. [Google Scholar] [CrossRef]
- Li, Y.; Zhou, Y.; Wang, F.; Chen, X.; Wang, C.; Wang, J.; Liu, T.; Li, Y.; He, B. SIRT4 is the last puzzle of mitochondrial sirtuins. Bioorg. Med. Chem. 2018, 26, 3861–3865. [Google Scholar] [CrossRef]
- Lang, A.; Piekorz, R.P. Novel role of the SIRT4-OPA1 axis in mitochondrial quality control. Cell Stress 2017, 2, 1–3. [Google Scholar] [CrossRef]
- Lang, A.; Anand, R.; Altinoluk-Hambüchen, S.; Ezzahoini, H.; Stefanski, A.; Iram, A.; Bergmann, L.; Urbach, J.; Böhler, P.; Hänsel, J.; et al. SIRT4 interacts with OPA1 and regulates mitochondrial quality control and mitophagy. Aging 2017, 9, 2163–2189. [Google Scholar] [CrossRef] [PubMed]
- He, L.; Wang, J.; Yang, Y.; Zou, P.; Xia, Z.; Li, J. SIRT4 Suppresses Doxorubicin-Induced Cardiotoxicity by Regulating the AKT/mTOR/Autophagy Pathway. Toxicology 2022, 469, 153119. [Google Scholar] [CrossRef] [PubMed]
- Pei, Z.; Ma, L.; Li, Y.; Yang, J.; Yang, Q.; Yao, W.; Li, S. CoQ10 Improves Myocardial Damage in Doxorubicin-Induced Heart Failure in C57BL/6 Mice. Front. Biosci. Landmark Ed. 2022, 27, 244. [Google Scholar] [CrossRef]
- Li, X.; Liu, L.; Li, T.; Liu, M.; Wang, Y.; Ma, H.; Mu, N.; Wang, H. SIRT6 in Senescence and Aging-Related Cardiovascular Diseases. Front. Cell Dev. Biol. 2021, 9, 641315. [Google Scholar] [CrossRef]
- Han, D.; Wang, Y.; Wang, Y.; Dai, X.; Zhou, T.; Chen, J.; Tao, B.; Zhang, J.; Cao, F. The Tumor-Suppressive Human Circular RNA CircITCH Sponges miR-330-5p to Ameliorate Doxorubicin-Induced Cardiotoxicity Through Upregulating SIRT6, Survivin, and SERCA2a. Circ. Res. 2020, 127, e108–e125. [Google Scholar] [CrossRef] [PubMed]
- Peng, K.; Zeng, C.; Gao, Y.; Liu, B.; Li, L.; Xu, K.; Yin, Y.; Qiu, Y.; Zhang, M.; Ma, F.; et al. Overexpressed SIRT6 ameliorates doxorubicin-induced cardiotoxicity and potentiates the therapeutic efficacy through metabolic remodeling. Acta Pharm. Sin. B 2023, 13, 2680–2700. [Google Scholar] [CrossRef]
- Wang, S.; Zhang, X.; Hou, Y.; Zhang, Y.; Chen, J.; Gao, S.; Duan, H.; Gu, S.; Yu, S.; Cai, Y. SIRT6 activates PPARα to improve doxorubicin-induced myocardial cell aging and damage. Chem. Biol. Interact. 2024, 392, 110920. [Google Scholar] [CrossRef]
- Lagunas-Rangel, F.A. SIRT7 in the aging process. Cell. Mol. Life Sci. 2022, 79, 297. [Google Scholar] [CrossRef]
- Vakhrusheva, O.; Smolka, C.; Gajawada, P.; Kostin, S.; Boettger, T.; Kubin, T.; Braun, T.; Bober, E. Sirt7 increases stress resistance of cardiomyocytes and prevents apoptosis and inflammatory cardiomyopathy in mice. Circ. Res. 2008, 102, 703–710. [Google Scholar] [CrossRef]
- Araki, S.; Izumiya, Y.; Rokutanda, T.; Ianni, A.; Hanatani, S.; Kimura, Y.; Onoue, Y.; Senokuchi, T.; Yoshizawa, T.; Yasuda, O.; et al. Sirt7 Contributes to Myocardial Tissue Repair by Maintaining Transforming Growth Factor-β Signaling Pathway. Circulation 2015, 132, 1081–1093. [Google Scholar] [CrossRef]
- Yamamura, S.; Izumiya, Y.; Araki, S.; Nakamura, T.; Kimura, Y.; Hanatani, S.; Yamada, T.; Ishida, T.; Yamamoto, M.; Onoue, Y.; et al. Cardiomyocyte Sirt (Sirtuin) 7 Ameliorates Stress-Induced Cardiac Hypertrophy by Interacting with and Deacetylating GATA4. Hypertens. Dallas Tex 1979 2020, 75, 98–108. [Google Scholar] [CrossRef]
- Sun, M.; Zhai, M.; Zhang, N.; Wang, R.; Liang, H.; Han, Q.; Jia, Y.; Jiao, L. MicroRNA-148b-3p is involved in regulating hypoxia/reoxygenation-induced injury of cardiomyocytes in vitro through modulating SIRT7/p53 signaling. Chem. Biol. Interact. 2018, 296, 211–219. [Google Scholar] [CrossRef]
- Ghosh, S.; Liu, B.; Zhou, Z. Resveratrol activates SIRT1 in a Lamin A-dependent manner. Cell Cycle Georget. Tex 2013, 12, 872–876. [Google Scholar] [CrossRef] [PubMed]
- Cao, D.; Wang, M.; Qiu, X.; Liu, D.; Jiang, H.; Yang, N.; Xu, R.-M. Structural basis for allosteric, substrate-dependent stimulation of SIRT1 activity by resveratrol. Genes Dev. 2015, 29, 1316–1325. [Google Scholar] [CrossRef]
- Chang, C.; Meikle, T.G.; Drummond, C.J.; Yang, Y.; Conn, C.E. Comparison of cubosomes and liposomes for the encapsulation and delivery of curcumin. Soft Matter 2021, 17, 3306–3313. [Google Scholar] [CrossRef]
- Luo, G.; Jian, Z.; Zhu, Y.; Zhu, Y.; Chen, B.; Ma, R.; Tang, F.; Xiao, Y. Sirt1 promotes autophagy and inhibits apoptosis to protect cardiomyocytes from hypoxic stress. Int. J. Mol. Med. 2019, 43, 2033–2043. [Google Scholar] [CrossRef]
- Kong, C.-Y.; Guo, Z.; Song, P.; Zhang, X.; Yuan, Y.-P.; Teng, T.; Yan, L.; Tang, Q.-Z. Underlying the Mechanisms of Doxorubicin-Induced Acute Cardiotoxicity: Oxidative Stress and Cell Death. Int. J. Biol. Sci. 2022, 18, 760–770. [Google Scholar] [CrossRef] [PubMed]
- Wu, B.; You, S.; Qian, H.; Wu, S.; Lu, S.; Zhang, Y.; Sun, Y.; Zhang, N. The role of SIRT2 in vascular-related and heart-related diseases: A review. J. Cell. Mol. Med. 2021, 25, 6470–6478. [Google Scholar] [CrossRef]
- Chen, L.; Sun, X.; Wang, Z.; Chen, M.; He, Y.; Zhang, H.; Han, D.; Zheng, L. Resveratrol protects against doxorubicin-induced cardiotoxicity by attenuating ferroptosis through modulating the MAPK signaling pathway. Toxicol. Appl. Pharmacol. 2024, 482, 116794. [Google Scholar] [CrossRef]
- Zhang, Y.; Wang, L.; Meng, L.; Cao, G.; Wu, Y. Sirtuin 6 overexpression relieves sepsis-induced acute kidney injury by promoting autophagy. Cell Cycle Georget. Tex 2019, 18, 425–436. [Google Scholar] [CrossRef]
- Magrone, T.; Jirillo, E. Immunity to Tuberculosis and Novel Therapeutic Strategies. Clin. Immunol. Endocr. Metab. Drugs 2014, 1, 46–60. [Google Scholar] [CrossRef]
- Arrigoni, R.; Ballini, A.; Jirillo, E.; Santacroce, L. Current View on Major Natural Compounds Endowed with Antibacterial and Antiviral Effects. Antibiotics 2024, 13, 603. [Google Scholar] [CrossRef]
- Jiang, K.; Bai, Y.; Hou, R.; Chen, G.; Liu, L.; Ciftci, O.N.; Farag, M.A.; Liu, L. Advances in dietary polyphenols: Regulation of inflammatory bowel disease (IBD) via bile acid metabolism and the gut-brain axis. Food Chem. 2025, 472, 142932. [Google Scholar] [CrossRef]
- Arrigoni, R.; Cammarota, F.; Porro, R.; Cantore, S.; Dioguardi, M.; Cazzolla, A.P.; De Leonardis, F.; Polimeno, L.; Zerman, N.; Di Cosola, M.; et al. Natural Bioactive Compounds against Oxidative Stress: Dietary Polyphenols Strike Back. Endocr. Metab. Immune Disord. Drug Targets 2023, 23, 764–776. [Google Scholar] [CrossRef]
- Li, G.; Liu, Q.; Gao, T.; Li, J.; Zhang, J.; Chen, O.; Cao, C.; Mao, M.; Xiao, M.; Zhang, X.; et al. Resveratrol and FGF1 Synergistically Ameliorates Doxorubicin-Induced Cardiotoxicity via Activation of SIRT1-NRF2 Pathway. Nutrients 2022, 14, 4017. [Google Scholar] [CrossRef]
- Syahputra, R.A.; Harahap, U.; Dalimunthe, A.; Nasution, M.P.; Satria, D. The Role of Flavonoids as a Cardioprotective Strategy against Doxorubicin-Induced Cardiotoxicity: A Review. Molecules 2022, 27, 1320. [Google Scholar] [CrossRef] [PubMed]
- Yu, W.; Sun, H.; Zha, W.; Cui, W.; Xu, L.; Min, Q.; Wu, J. Apigenin Attenuates Adriamycin-Induced Cardiomyocyte Apoptosis via the PI3K/AKT/mTOR Pathway. Evid.-Based Complement. Altern. Med. ECAM 2017, 2017, 2590676. [Google Scholar] [CrossRef]
- Ma, Y.; Yang, L.; Ma, J.; Lu, L.; Wang, X.; Ren, J.; Yang, J. Rutin attenuates doxorubicin-induced cardiotoxicity via regulating autophagy and apoptosis. Biochim. Biophys. Acta BBA Mol. Basis Dis. 2017, 1863, 1904–1911. [Google Scholar] [CrossRef]
- Priya, L.B.; Baskaran, R.; Huang, C.-Y.; Padma, V.V. Neferine ameliorates cardiomyoblast apoptosis induced by doxorubicin: Possible role in modulating NADPH oxidase/ROS-mediated NFκB redox signaling cascade. Sci. Rep. 2017, 7, 12283. [Google Scholar] [CrossRef]
- Lin, X.; Wang, Q.; Sun, S.; Xu, G.; Wu, Q.; Qi, M.; Bai, F.; Yu, J. Astragaloside IV promotes the eNOS/NO/cGMP pathway and improves left ventricular diastolic function in rats with metabolic syndrome. J. Int. Med. Res. 2020, 48, 300060519826848. [Google Scholar] [CrossRef]
- Afsar, T.; Razak, S.; Batoo, K.M.; Khan, M.R. Acacia hydaspica R. Parker prevents doxorubicin-induced cardiac injury by attenuation of oxidative stress and structural Cardiomyocyte alterations in rats. BMC Complement. Altern. Med. 2017, 17, 554. [Google Scholar] [CrossRef]
- Wang, M.; Zhang, J.; Zhao, M.; Liu, J.; Ye, J.; Xu, Y.; Wang, Z.; Ye, D.; Li, D.; Wan, J. Resolvin D1 Attenuates Doxorubicin-Induced Cardiotoxicity by Inhibiting Inflammation, Oxidative and Endoplasmic Reticulum Stress. Front. Pharmacol. 2021, 12, 749899. [Google Scholar] [CrossRef]
- Wan, Y.; Wang, J.; Xu, J.-F.; Tang, F.; Chen, L.; Tan, Y.-Z.; Rao, C.-L.; Ao, H.; Peng, C. Panax ginseng and its ginsenosides: Potential candidates for the prevention and treatment of chemotherapy-induced side effects. J. Ginseng Res. 2021, 45, 617–630. [Google Scholar] [CrossRef] [PubMed]
- Li, X.-R.; Cheng, X.-H.; Zhang, G.-N.; Wang, X.-X.; Huang, J.-M. Cardiac safety analysis of first-line chemotherapy drug pegylated liposomal doxorubicin in ovarian cancer. J. Ovarian Res. 2022, 15, 96. [Google Scholar] [CrossRef]
- Xing, M.; Yan, F.; Yu, S.; Shen, P. Efficacy and Cardiotoxicity of Liposomal Doxorubicin-Based Chemotherapy in Advanced Breast Cancer: A Meta-Analysis of Ten Randomized Controlled Trials. PLoS ONE 2015, 10, e0133569. [Google Scholar] [CrossRef]
- Norouzi, M.; Yathindranath, V.; Thliveris, J.A.; Kopec, B.M.; Siahaan, T.J.; Miller, D.W. Doxorubicin-loaded iron oxide nanoparticles for glioblastoma therapy: A combinational approach for enhanced delivery of nanoparticles. Sci. Rep. 2020, 10, 11292. [Google Scholar] [CrossRef]
- Kourek, C.; Touloupaki, M.; Rempakos, A.; Loritis, K.; Tsougkos, E.; Paraskevaidis, I.; Briasoulis, A. Cardioprotective Strategies from Cardiotoxicity in Cancer Patients: A Comprehensive Review. J. Cardiovasc. Dev. Dis. 2022, 9, 259. [Google Scholar] [CrossRef] [PubMed]
- McGowan, J.V.; Chung, R.; Maulik, A.; Piotrowska, I.; Walker, J.M.; Yellon, D.M. Anthracycline Chemotherapy and Cardiotoxicity. Cardiovasc. Drugs Ther. 2017, 31, 63–75. [Google Scholar] [CrossRef]
- Liesse, K.; Harris, J.; Chan, M.; Schmidt, M.L.; Chiu, B. Dexrazoxane Significantly Reduces Anthracycline-induced Cardiotoxicity in Pediatric Solid Tumor Patients: A Systematic Review. J. Pediatr. Hematol. Oncol. 2018, 40, 417–425. [Google Scholar] [CrossRef]
- van Dalen, E.C.; Caron, H.N.; Dickinson, H.O.; Kremer, L.C. Cardioprotective interventions for cancer patients receiving anthracyclines. Cochrane Database Syst. Rev. 2011, 2011, CD003917. [Google Scholar] [CrossRef]
- Tebbi, C.K.; London, W.B.; Friedman, D.; Villaluna, D.; De Alarcon, P.A.; Constine, L.S.; Mendenhall, N.P.; Sposto, R.; Chauvenet, A.; Schwartz, C.L. Dexrazoxane-associated risk for acute myeloid leukemia/myelodysplastic syndrome and other secondary malignancies in pediatric Hodgkin’s disease. J. Clin. Oncol. Off. J. Am. Soc. Clin. Oncol. 2007, 25, 493–500. [Google Scholar] [CrossRef] [PubMed]
- Oxnard, G.R.; Yang, J.C.-H.; Yu, H.; Kim, S.-W.; Saka, H.; Horn, L.; Goto, K.; Ohe, Y.; Mann, H.; Thress, K.S.; et al. TATTON: A multi-arm, phase Ib trial of osimertinib combined with selumetinib, savolitinib, or durvalumab in EGFR-mutant lung cancer. Ann. Oncol. 2020, 31, 507–516. [Google Scholar] [CrossRef] [PubMed]
- Beheshti, T.; Toroghi, M.; Hosseini, G.; Zarifian, A.; Shandiz, H.; Fazlinezhad, A. Carvedilol Administration Can Prevent Doxorubicin-Induced Cardiotoxicity: A Double-Blind Randomized Trial. Cardiology 2016, 134, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Neilan, T.G.; Quinaglia, T.; Onoue, T.; Mahmood, S.S.; Drobni, Z.D.; Gilman, H.K.; Smith, A.; Heemelaar, J.C.; Brahmbhatt, P.; Ho, J.S.; et al. Atorvastatin for Anthracycline-Associated Cardiac Dysfunction: The STOP-CA Randomized Clinical Trial. JAMA 2023, 330, 528–536. [Google Scholar] [CrossRef]
- Makhlin, I.; Demissei, B.G.; D’Agostino, R.; Hundley, W.G.; Baleanu-Gogonea, C.; Wilcox, N.S.; Chen, A.; Smith, A.M.; O’Connell, N.S.; Januzzi, J.L.; et al. Statins Do Not Significantly Affect Oxidative Nitrosative Stress Biomarkers in the PREVENT Randomized Clinical Trial. Clin. Cancer Res. Off. J. Am. Assoc. Cancer Res. 2024, 30, 2370–2376. [Google Scholar] [CrossRef]
- Gupta, S.K.; Garg, A.; Bär, C.; Chatterjee, S.; Foinquinos, A.; Milting, H.; Streckfuß-Bömeke, K.; Fiedler, J.; Thum, T. Quaking Inhibits Doxorubicin-Mediated Cardiotoxicity Through Regulation of Cardiac Circular RNA Expression. Circ. Res. 2018, 122, 246–254. [Google Scholar] [CrossRef]
- Li, K.; Jiang, K.-M.; Wang, Y.; Hu, F.; Zhu, X.-C.; Sun, C.-L.; Jin, L.; Liu, W.-T.; Lin, T.-T.; Li, M. Inhibition of NETs prevents doxorubicin-induced cardiotoxicity by attenuating IL-18-IFN-γ-Cx43 axis induced cardiac conduction abnormalities. Int. Immunopharmacol. 2025, 147, 114016. [Google Scholar] [CrossRef]
- Todorova, V.K.; Hsu, P.-C.; Wei, J.Y.; Lopez-Candales, A.; Chen, J.Z.; Su, L.J.; Makhoul, I. Biomarkers of inflammation, hypercoagulability and endothelial injury predict early asymptomatic doxorubicin-induced cardiotoxicity in breast cancer patients. Am. J. Cancer Res. 2020, 10, 2933–2945. [Google Scholar]
| Oxidative Stress | Interaction with mitochondrial DNA, and inhibition of the respiratory chain [31]; |
| Generation of ROS, alteration of the phospholipids of cell membranes, mitochondria, and ER, with myocardial damage [32]; | |
| Reduction of glutathione and CAT levels, with increase in oxidative stress [33]; DIC-mediated endothelial dysfunction with increased levels of endothelin-1, activation of type A and type B receptors, vasoconstriction, and release of NO, adrenomedullin, and prostacyclin [37] | |
| Autophagy | DOX-mediated increase in Beclin-1, p62, and microtubule-associated protein 1A/1B light chain 3 (LC3)-II/LC3-I levels, with damaged mitochondria removed by mitophagy [43]; |
| DOX-mediated abrogation of lysosome biosynthesis and catepsin activity, with autophagolysosomal accumulation, and impairment of autophagy [45]; DOX-induced inhibition of the fusion between autophagosomes and liposomes [46]; DOX-mediated enhancement of TLR9, and suppression of AMPK activation [47] | |
| Inflammation | DIC-induced release of pro-inflammatory cytokines through activation of TLR-4, NF-kB, and NLRP3 inflammasome [48,49,50]; |
| DOX-mediated transformation of smooth cardiac muscle cells into macrophage-like cells, with vascular wall low-grade inflammation and impairment of sarcoplasmic reticulum [55,56]; | |
| DOX-induced apoptosis of cardiomyocytes via release of catecholamines by infiltrating macrophages [57] | |
| Apoptosis/Ferroptosis | Decrease in the anti-apoptotic protein, Bcl-2, and increase in Bcl-2-associated X expression in DOX-treated cardiomyocytes, with increased mitochondrial permeability, cytochrome c release and caspase-3, thus leading to cardiomyocyte apoptosis [60]; |
| DOX-induced ferroptosis of cardiomyocytes by inactivation of GPx4 [62,63,64]; Overexpression of methyltransferase-like 14 with upregulation of transferrin receptors, and uptake of iron [65]; DOX-mediated ferroptosis by impairment of Forkhead Box O4 transcription, and high mobility group Box 1 nuclear translocation [66] |
| SIRT 1 | ROS generation and FOXO 1 deacetylation inhibition, with decrease in cardiac oxidative stress [71] |
| SIRT 1-mediated inhibition of NF-kB through deacetylation of the peroxisome proliferator-activated receptor gamma coactivator 1 alpha; SIRT 1/Liver kinase B1/AMPK pathway activation; inhibition of miR-200a 3p, respectively [72,75,79] | |
| Natural product (jaceosidin, calycosin, and dihydromyrecitin)-mediated activation of SIRT 1, with inhibition of NF-kB [76,77,94]; p53 protein acetylation decrease by resveratrol-activated SIRT 1, with attenuation of myocardial cell apoptosis [78]; SIRT 1-mediated activation of the Nrf2/Kelch-like associated protein, with reduction of ferroptosis, and DIC [79] | |
| SIRT 2 | FOXO3a and AMPK SIRT 2-mediated activation, respectively, with reduced release of ROS and mitigation of DIC [81,108] |
| SIRT 2 activation and improvement of DOX-mediated cardiac aging [65]; miR-140-5p inhibition with activation of the SIRT2/NRF2 antioxidant pathway [82] | |
| SIRT 3 | Natural product (RES, daidzein, tubeimoside, berberine, Qishen granules) and dichloroacetic acid-mediated upregulation of SIRT3, with improvement of DOX-induced mitochondrial dysfunction, ROS generation, and apoptosis [70,84,85,86,87,109] |
| miR-34-5p SIRT 3-mediated inhibition, with autophagic activity regulation, and protection from DIC [88] | |
| SIRT 3-induced inhibition of NLRP3 inflammasome, with autophagy regulation, and pyroptosis decrease [83] | |
| SIRT 4 | SIRT 4-mediated inhibition of fatty acid oxidation in muscles, with reduction of mitochondrial function [89] |
| Overexpression of SIRT 4 and interaction with optic atrophin 1, with regulation of autophagy and ROS generation; SIRT 4-mediated inhibition of DIC, with activation of the akt/mTOR pathway [92] | |
| SIRT 5 | Coenzyme Q 10-mediated overexpression of SIRT 5 and protection from DIC [93] |
| SIRT 6 | SIRT 6 overexpression by targeting miR-330-5p, with inhibition of ROS generation, apoptosis, and necrosis during DIC [80,95] |
| Enhancement of autophagy by SIRT 6-mediated acetylation and inhibition of SKG1 [110] | |
| SIRT 7 | SIRT 7-induced reduction of myocardial stress via deacetylation of p53 and GATA4; regulation of |
| autophagy and inhibition of miR-148-3p, respectively [83,98,100,101,102] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Arrigoni, R.; Jirillo, E.; Caiati, C. Pathophysiology of Doxorubicin-Mediated Cardiotoxicity. Toxics 2025, 13, 277. https://doi.org/10.3390/toxics13040277
Arrigoni R, Jirillo E, Caiati C. Pathophysiology of Doxorubicin-Mediated Cardiotoxicity. Toxics. 2025; 13(4):277. https://doi.org/10.3390/toxics13040277
Chicago/Turabian StyleArrigoni, Roberto, Emilio Jirillo, and Carlo Caiati. 2025. "Pathophysiology of Doxorubicin-Mediated Cardiotoxicity" Toxics 13, no. 4: 277. https://doi.org/10.3390/toxics13040277
APA StyleArrigoni, R., Jirillo, E., & Caiati, C. (2025). Pathophysiology of Doxorubicin-Mediated Cardiotoxicity. Toxics, 13(4), 277. https://doi.org/10.3390/toxics13040277







