Healthier Lifestyles Attenuated Association of Single or Mixture Exposure to Air Pollutants with Cardiometabolic Risk in Rural Chinese Adults
Abstract
1. Introduction
2. Methods
2.1. Study Design and Participants
2.2. Assessment of Air Pollution and the Air Pollution Score
2.3. Assessment of Cardiometabolic Risk
2.4. Assessment of the Healthy Lifestyle Score
2.5. Statistical Analysis
3. Results
3.1. Basic Characteristics of the Study Population
3.2. Associations of Single Air Pollution and the Air Pollution Score with Cardiometabolic Risk
3.3. Associations of the Lifestyle Score with Cardiometabolic Risk
3.4. Associations of Air Pollutants and the Air Pollution Score with Cardiometabolic Risk by Lifestyle Factors
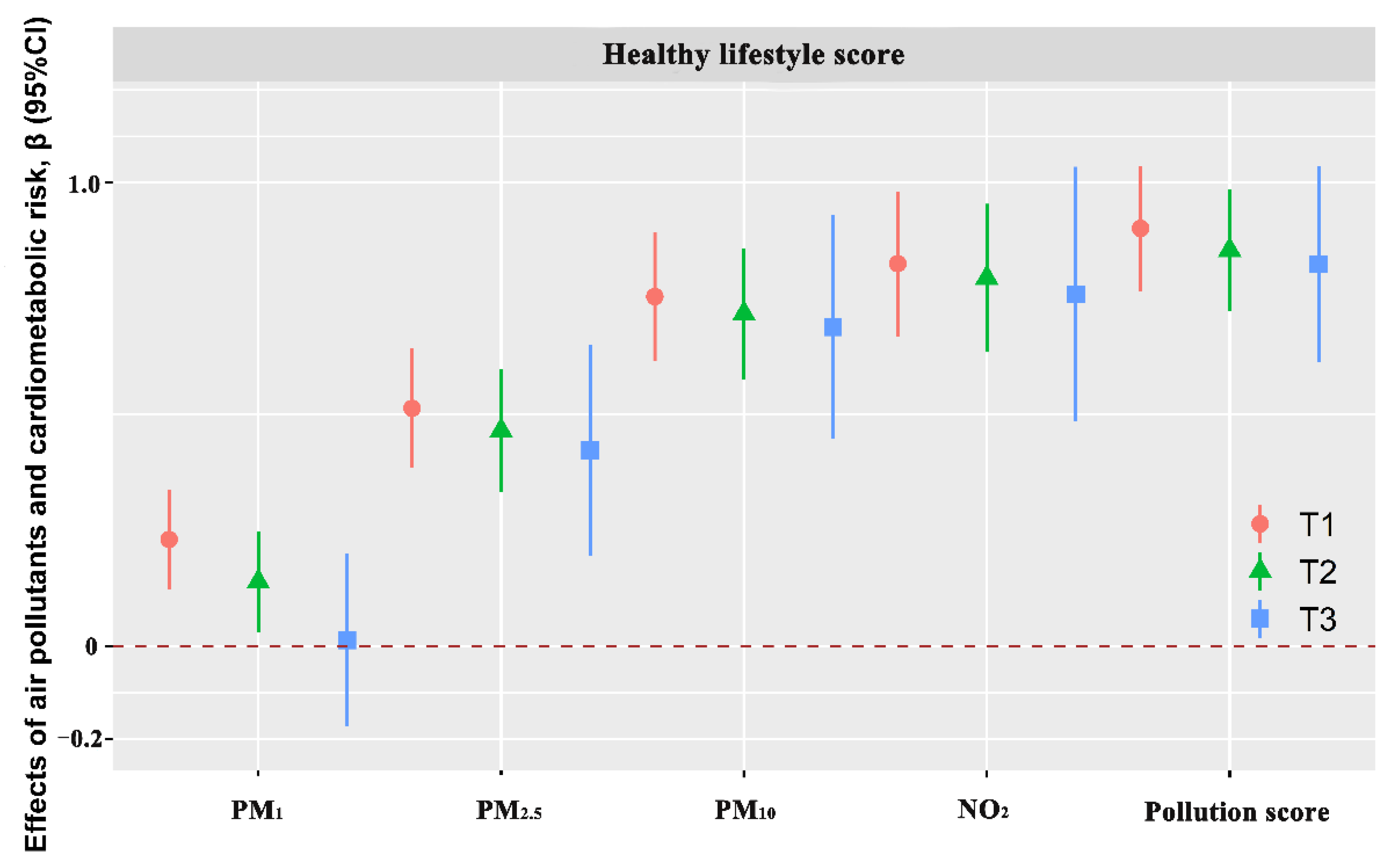
3.5. Interactive Effect of the Lifestyle Score and Air Pollution on Cardiometabolic Risk
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cardiovascular Diseases (CVDs) 2021. Available online: https://www.who.int/en/news-room/fact-sheets/detail/cardiovascular-diseases-(cvds) (accessed on 11 June 2021).
- Alwan, A.; MacLean, D.R.; Riley, L.M.; D’Espaignet, E.T.; Mathers, C.D.; Stevens, G.A.; Bettcher, D. Monitoring and surveillance of chronic non-communicable diseases: Progress and capacity in high-burden countries. Lancet 2010, 376, 1861–1868. [Google Scholar] [CrossRef]
- Song, C.; He, J.; Wu, L.; Jin, T.; Chen, X.; Li, R.; Ren, P.; Zhang, L.; Mao, H. Health burden attributable to ambient PM2.5 in China. Environ. Pollut. 2017, 223, 575–586. [Google Scholar] [CrossRef] [PubMed]
- Long, Y.; Wang, J.; Wu, K.; Zhang, J. Population Exposure to Ambient PM2.5 at the Subdistrict Level in China. Int. J. Environ. Res. Public Health 2018, 15, 2683. [Google Scholar] [CrossRef]
- Alexeeff, S.E.; Liao, N.S.; Liu, X.; Eeden, S.K.V.D.; Sidney, S. Long-Term PM2.5 Exposure and Risks of Ischemic Heart Disease and Stroke Events: Review and Meta-Analysis. J. Am. Hear. Assoc. 2021, 10, e016890. [Google Scholar] [CrossRef] [PubMed]
- Pan, M.; Li, S.; Tu, R.; Li, R.; Liu, X.; Chen, R.; Yu, S.; Mao, Z.; Huo, W.; Yin, S.; et al. Associations of solid fuel use and ambient air pollution with estimated 10-year atherosclerotic cardiovascular disease risk. Environ. Int. 2021, 157, 106865. [Google Scholar] [CrossRef]
- Tu, R.; Hou, J.; Liu, X.; Li, R.; Dong, X.; Pan, M.; Yin, S.; Hu, K.; Mao, Z.; Huo, W.; et al. Low socioeconomic status aggravated associations of exposure to mixture of air pollutants with obesity in rural Chinese adults: A cross-sectional study. Environ. Res. 2020, 194, 110632. [Google Scholar] [CrossRef]
- Liu, X.; Zhou, M.; Yu, C.; Zhang, Z.-J. Age-Period-Cohort Analysis of Type 2 Diabetes Mortality Attributable to Particulate Matter Pollution in China and the U.S. J. Diabetes Res. 2020, 2020, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Mao, S.; Li, S.; Wang, C.; Liu, Y.; Li, N.; Liu, F.; Huang, S.; Liu, S.; Lu, Y.; Mao, Z.; et al. Is long-term PM1 exposure associated with blood lipids and dyslipidemias in a Chinese rural population? Environ. Int. 2020, 138, 105637. [Google Scholar] [CrossRef]
- Li, N.; Chen, G.; Liu, F.; Mao, S.; Liu, Y.; Hou, Y.; Lu, Y.; Liu, S.; Wang, C.; Xiang, H.; et al. Associations of long-term exposure to ambient PM1 with hypertension and blood pressure in rural Chinese population: The Henan rural cohort study. Environ. Int. 2019, 128, 95–102. [Google Scholar] [CrossRef]
- Li, N.; Chen, G.; Liu, F.; Mao, S.; Liu, Y.; Liu, S.; Mao, Z.; Lu, Y.; Wang, C.; Guo, Y.; et al. Associations between long-term exposure to air pollution and blood pressure and effect modifications by behavioral factors. Environ. Res. 2020, 182, 109109. [Google Scholar] [CrossRef]
- Hou, J.; Liu, X.; Tu, R.; Dong, X.; Zhai, Z.; Mao, Z.; Huo, W.; Chen, G.; Xiang, H.; Guo, Y.; et al. Long-term exposure to ambient air pollution attenuated the association of physical activity with metabolic syndrome in rural Chinese adults: A cross-sectional study. Environ. Int. 2020, 136, 105459. [Google Scholar] [CrossRef] [PubMed]
- Alberti, K.G.M.M.; Zimmet, P.; Shaw, J.; IDF Epidemiology Task Force Consensus Group. The metabolic syndrome—A new worldwide definition. Lancet 2005, 366, 1059–1062. [Google Scholar] [CrossRef]
- Hillier, T.A.; Rousseau, A.; Lange, C.; Lépinay, P.; Cailleau, M.; Novak, M.; Calliez, E.; Ducimetière, P.; Balkau, B. Practical way to assess metabolic syndrome using a continuous score obtained from principal components analysis. Diabetologia 2006, 49, 1528–1535. [Google Scholar] [CrossRef] [PubMed]
- DeBoer, M.D.; Gurka, M.J. Clinical utility of metabolic syndrome severity scores: Considerations for practitioners. Diabetes Metab. Syndr. Obes. Targets Ther. 2017, ume 10, 65–72. [Google Scholar] [CrossRef]
- Tu, R.; Hou, J.; Liu, X.; Li, R.; Dong, X.; Pan, M.; Mao, Z.; Huo, W.; Chen, G.; Guo, Y.; et al. Physical activity attenuated association of air pollution with estimated 10-year atherosclerotic cardiovascular disease risk in a large rural Chinese adult population: A cross-sectional study. Environ. Int. 2020, 140, 105819. [Google Scholar] [CrossRef]
- Liu, X.; Mao, Z.; Li, Y.; Wu, W.; Zhang, X.; Huo, W.; Yu, S.; Shen, L.; Li, L.; Tu, R.; et al. Cohort Profile: The Henan Rural Cohort: A prospective study of chronic non-communicable diseases. Int. J. Epidemiol. 2019, 48, 1756. [Google Scholar] [CrossRef]
- Chen, G.; Knibbs, L.D.; Zhang, W.; Li, S.; Cao, W.; Guo, J.; Ren, H.; Wang, B.; Wang, H.; Williams, G.; et al. Estimating spatiotemporal distribution of PM1 concentrations in China with satellite remote sensing, meteorology, and land use information. Environ. Pollut. 2018, 233, 1086–1094. [Google Scholar] [CrossRef]
- Chen, G.; Li, S.; Knibbs, L.D.; Hamm, N.A.S.; Cao, W.; Li, T.; Guo, J.; Ren, H.; Abramson, M.J.; Guo, Y. A machine learning method to estimate PM2.5 concentrations across China with remote sensing, meteorological and land use information. Sci. Total Environ. 2018, 636, 52–60. [Google Scholar] [CrossRef]
- Li, X.; Wang, M.; Song, Y.; Ma, H.; Zhou, T.; Liang, Z.; Qi, L. Obesity and the relation between joint exposure to ambient air pollutants and incident type 2 diabetes: A cohort study in UK Biobank. PLoS Med. 2021, 18, e1003767. [Google Scholar] [CrossRef]
- Joseph, J.J.; Tcheugui, J.B.E.; Effoe, V.S.; Hsueh, W.A.; Allison, M.A.; Golden, S.H. Renin-Angiotensin-Aldosterone System, Glucose Metabolism and Incident Type 2 Diabetes Mellitus: MESA. J. Am. Hear. Assoc. 2018, 7, e009890. [Google Scholar] [CrossRef]
- Wallace, T.M.; Levy, J.C.; Matthews, D.R. Use and Abuse of HOMA Modeling. Diabetes Care 2004, 27, 1487–1495. [Google Scholar] [CrossRef] [PubMed]
- Viitasalo, A.; Lakka, T.; Laaksonen, D.E.; Savonen, K.; Lakka, H.-M.; Hassinen, M.; Komulainen, P.; Tompuri, T.; Kurl, S.; Laukkanen, J.; et al. Validation of metabolic syndrome score by confirmatory factor analysis in children and adults and prediction of cardiometabolic outcomes in adults. Diabetologia 2014, 57, 940–949. [Google Scholar] [CrossRef] [PubMed]
- Winning, A.; Glymour, M.M.; McCormick, M.C.; Gilsanz, P.; Kubzansky, L.D. Psychological Distress Across the Life Course and Cardiometabolic Risk: Findings From the 1958 British Birth Cohort Study. J. Am. Coll. Cardiol. 2015, 66, 1577–1586. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Wu, W.; Mao, Z.; Huo, W.; Tu, R.; Qian, X.; Zhang, X.; Tian, Z.; Zhang, H.; Jiang, J.; et al. Prevalence and influencing factors of overweight and obesity in a Chinese rural population: The Henan Rural Cohort Study. Sci. Rep. 2018, 8, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Chinese Nutrition Society. Chinese Dietary Guidelines Summary (2016); People’s Medical Publishing House: Beijing, China, 2016; pp. 1–140. [Google Scholar]
- World Health Organization. International Guide for Monitoring Alcohol Consumption and Related Harm, 2000th ed.; WHO: Geneva, Switzerland, 2000; 51p. [Google Scholar]
- International Physical Activity Questionnaire: Short Last 7 Days Self-Administered Format 2005. Available online: http://www.ipaq.ki.se/downloads.htm (accessed on 26 October 2015).
- Xue, Y.; Yang, K.; Wang, B.; Liu, C.; Mao, Z.; Yu, S.; Li, X.; Wang, Y.; Sun, H.; Wang, C.; et al. Reproducibility and validity of an FFQ in the Henan Rural Cohort Study. Public Health Nutr. 2019, 23, 34–40. [Google Scholar] [CrossRef]
- Yuan, Y.-Q.; Li, F.; Wu, H.; Wang, Y.-C.; Chen, J.-S.; He, G.-S.; Li, S.-G.; Chen, B. Evaluation of the Validity and Reliability of the Chinese Healthy Eating Index. Nutrients 2018, 10, 114. [Google Scholar] [CrossRef]
- Li, Y.; Schoufour, J.; Wang, D.D.; Dhana, K.; Pan, A.; Liu, X.; Song, M.; Liu, G.; Shin, H.J.; Sun, Q.; et al. Healthy lifestyle and life expectancy free of cancer, cardiovascular disease, and type 2 diabetes: Prospective cohort study. BMJ 2020, 368, l6669. [Google Scholar] [CrossRef]
- Lv, J.; Yu, C.; Guo, Y.; Bian, Z.; Yang, L.; Chen, Y.; Tang, X.; Zhang, W.; Qian, Y.; Huang, Y.; et al. Adherence to Healthy Lifestyle and Cardiovascular Diseases in the Chinese Population. J. Am. Coll. Cardiol. 2017, 69, 1116–1125. [Google Scholar] [CrossRef]
- Keil, A.P.; Buckley, J.P.; O’Brien, K.M.; Ferguson, K.; Zhao, S.; White, A.J. A Quantile-Based g-Computation Approach to Addressing the Effects of Exposure Mixtures. Environ. Health Perspect. 2020, 128, 047004. [Google Scholar] [CrossRef]
- Wei, Y.; Zhang, J.J.; Li, Z.; Gow, A.; Chung, K.F.; Hu, M.; Sun, Z.; Zeng, L.; Zhu, T.; Jia, G.; et al. Chronic exposure to air pollution particles increases the risk of obesity and metabolic syndrome: Findings from a natural experiment in Beijing. FASEB J. 2016, 30, 2115–2122. [Google Scholar] [CrossRef]
- Hou, J.; Gu, J.; Liu, X.; Tu, R.; Dong, X.; Li, R.; Mao, Z.; Huo, W.; Chen, G.; Pan, M.; et al. Long-term exposure to air pollutants enhanced associations of obesity with blood pressure and hypertension. Clin. Nutr. 2021, 40, 1442–1450. [Google Scholar] [CrossRef] [PubMed]
- Eze, I.C.; Schaffner, E.; Fischer, E.; Schikowski, T.; Adam, M.; Imboden, M.; Tsai, M.; Carballo, D.; von Eckardstein, A.; Künzli, N.; et al. Long-term air pollution exposure and diabetes in a population-based Swiss cohort. Environ. Int. 2014, 70, 95–105. [Google Scholar] [CrossRef] [PubMed]
- Bloemsma, L.D.; Gehring, U.; Klompmaker, J.O.; Hoek, G.; Janssen, N.A.; Lebret, E.; Brunekreef, B.; Wijga, A.H. Green space, air pollution, traffic noise and cardiometabolic health in adolescents: The PIAMA birth cohort. Environ. Int. 2019, 131, 104991. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Fuertes, E.; Tiesler, C.M.; Birk, M.; Babisch, W.; Bauer, C.-P.; Koletzko, S.; von Berg, A.; Hoffmann, B.; Heinrich, J. The associations between traffic-related air pollution and noise with blood pressure in children: Results from the GINIplus and LISAplus studies. Int. J. Hyg. Environ. Health 2013, 217, 499–505. [Google Scholar] [CrossRef] [PubMed]
- Brook, R.D.; Rajagopalan, S.; Pope, C.A., 3rd; Brook, J.R.; Bhatnagar, A.; Diez-Roux, A.V.; Holguin, F.; Hong, Y.; Luepker, R.V.; Mittleman, M.A.; et al. Particulate Matter Air Pollution and Cardiovascular Disease: An update to the scientific statement from the american heart association. Circulation 2010, 121, 2331–2378. [Google Scholar] [CrossRef]
- Mendez, R.; Zheng, Z.; Fan, Z.; Rajagopalan, S.; Sun, Q.; Zhang, K. Exposure to fine airborne particulate matter induces macrophage infiltration, unfolded protein response, and lipid deposition in white adipose tissue. Am. J. Transl. Res. 2013, 5, 224–234. [Google Scholar]
- Thiering, E.; Cyrys, J.; Kratzsch, J.; Meisinger, C.; Hoffmann, B.; Berdel, D.; von Berg, A.; Koletzko, S.; Bauer, C.-P.; Heinrich, J. Long-term exposure to traffic-related air pollution and insulin resistance in children: Results from the GINIplus and LISAplus birth cohorts. Diabetologia 2013, 56, 1696–1704. [Google Scholar] [CrossRef]
- Nava, A. Atherosclerosis and inflammation. Arch. De Cardiol. De Mex. 2002, 72 (Suppl. S1), S153–S155. [Google Scholar]
- Yang, B.-Y.; Qian, Z.; Li, S.; Fan, S.; Chen, G.; Syberg, K.M.; Xian, H.; Wang, S.-Q.; Ma, H.; Chen, D.-H.; et al. Long-term exposure to ambient air pollution (including PM1) and metabolic syndrome: The 33 Communities Chinese Health Study (33CCHS). Environ. Res. 2018, 164, 204–211. [Google Scholar] [CrossRef]
- Zhang, J.; Nuebel, E.; Daley, G.Q.; Koehler, C.M.; Teitell, M.A. Metabolic Regulation in Pluripotent Stem Cells during Reprogramming and Self-Renewal. Cell Stem Cell 2012, 11, 589–595. [Google Scholar] [CrossRef]
- Kaali, S.; Jack, D.; Chillrud, S.N.; Owusu-Agyei, S.; Kinney, P.L.; Baccarelli, A.A.; Asante, K.P.; Lee, A.G.; Delimini, R.; Hu, L.; et al. Prenatal Household Air Pollution Alters Cord Blood Mononuclear Cell Mitochondrial DNA Copy Number: Sex-Specific Associations. Int. J. Environ. Res. Public Health 2019, 16, 26. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chang, S.-C.; Niu, R.; Liu, L.; Crabtree-Ide, C.R.; Zhao, B.; Shi, J.; Han, X.; Li, J.; Su, J.; et al. TP53 genetic polymorphisms, interactions with lifestyle factors and lung cancer risk: A case control study in a Chinese population. BMC Cancer 2013, 13, 607. [Google Scholar] [CrossRef] [PubMed]
- Song, Q.; Christiani, D.C.; Wang, X.; Ren, J. The Global Contribution of Outdoor Air Pollution to the Incidence, Prevalence, Mortality and Hospital Admission for Chronic Obstructive Pulmonary Disease: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2014, 11, 11822–11832. [Google Scholar] [CrossRef] [PubMed]
- WHO Global Air Quality Guidelines. Particulate Matter (PM2.5 and PM10), Ozone, Nitrogen Dioxide, Sulfur Dioxide and Carbon Monoxide; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Wu, F.; Wang, W.; Man, Y.B.; Chan, C.Y.; Liu, W.; Tao, S.; Wong, M.H. Levels of PM 2.5 /PM 10 and associated metal(loid)s in rural households of Henan Province, China. Sci. Total Environ. 2015, 512–513, 194–200. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Mo, J.; Weschler, C.J. Reducing Health Risks from Indoor Exposures in Rapidly Developing Urban China. Environ. Health Perspect. 2013, 121, 751–755. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Wang, Y.; Li, S.; Cao, W.; Ren, H.; Knibbs, L.D.; Abramson, M.J.; Guo, Y. Spatiotemporal patterns of PM10 concentrations over China during 2005–2016: A satellite-based estimation using the random forests approach. Environ. Pollut. 2018, 242, 605–613. [Google Scholar]

| Variable | Air pollution score | p | |||
|---|---|---|---|---|---|
| Q1 | Q2 | Q3 | Q4 | ||
| Age (years) | 55.3 (11.82) | 54.94 (12.30) | 52.59 (13.20) | 55.90 (11.52) | <0.001 a |
| Sex | <0.001 b | ||||
| Men | 3440 (41.84) | 3493 (41.09) | 3144 (38.12) | 2931 (33.81) | |
| Women | 4782 (58.16) | 5008 (58.91) | 5103 (61.88) | 5737 (66.19) | |
| Marital status | <0.001 b | ||||
| Married/cohabitation | 7422 (90.27) | 7693 (90.50) | 7506 (91.01) | 7715 (89.01) | |
| Unmarried/divorced/widowed | 800 (9.73) | 808 (9.50) | 741 (8.99) | 953 (10.99) | |
| Educational level | <0.001 b | ||||
| Elementary school or below | 3953 (48.08) | 3882 (45.67) | 2845 (34.50) | 3879 (44.75) | |
| Middle school | 3288 (39.99) | 3342 (39.31) | 3364 (40.79) | 3711 (42.81) | |
| High school or above | 981 (11.93) | 1277 (15.02) | 2038 (24.71) | 1078 (12.44) | |
| Personal averaged monthly income | <0.001 b | ||||
| <500 RMB | 3317 (40.34) | 2451 (28.83) | 2807 (34.04) | 3048 (35.16) | |
| 500–999 RMB | 2424 (29.48) | 2791 (32.83) | 2818 (34.17) | 3137 (36.19) | |
| ≥1000 RMB | 2481 (30.18) | 3259 (38.34) | 2622 (31.79) | 2483 (28.65) | |
| Current regular smokers | 1836 (22.33) | 1805 (21.23) | 1522 (18.46) | 1339 (15.45) | <0.001 b |
| Current regular drinking | 1422 (17.30) | 1486 (17.48) | 1719 (20.84) | 1628 (18.78) | <0.001 b |
| Physical activity | <0.001 b | ||||
| Low | 2242 (27.27) | 2228 (26.21) | 3225 (39.11) | 2769 (31.95) | |
| Moderate | 3583 (43.58) | 3479 (40.92) | 2443 (29.62) | 3370 (38.88) | |
| High | 2397 (29.15) | 2794 (32.87) | 2579 (31.27) | 2529 (29.18) | |
| Diet score | 19.71 (3.88) | 20.58 (4.20) | 21.99 (4.14) | 19.57 (4.13) | <0.001 a |
| BMI (kg/m2) | 24.23 (3.37) | 24.43 (3.54) | 25.35 (3.54) | 25.16 (3.48) | <0.001 a |
| WC (cm) | 80.85 (9.90) | 83.38 (10.29) | 85.99 (10.39) | 85.15 (9.84) | <0.001 a |
| SBP (mmHg) | 119.07 (17.52) | 124.77 (20.17) | 128.75 (19.78) | 126.97 (19.75) | <0.001 a |
| DBP (mmHg) | 73.03 (10.57) | 76.93 (11.37) | 80.69 (11.40) | 78.68 (11.42) | <0.001 a |
| FPG (mmol/L) | 5.27 (1.12) | 5.32 (1.28) | 5.64 (1.32) | 5.58 (1.42) | <0.001 a |
| TG (mmol/L) | 1.83 (1.14) | 1.56 (1.03) | 1.62 (1.08) | 1.59 (1.03) | <0.001 a |
| HDLC (mmol/L) | 1.37 (0.34) | 1.36 (0.33) | 1.30 (0.33) | 1.31 (0.33) | <0.001 a |
| INS (μIU/mL) | 13.10 (4.42) | 11.23 (5.12) | 8.58 (4.71) | 9.99 (5.18) | <0.001 a |
| Family history of CHD (Yes) | 802 (9.75) | 699 (8.45) | 472 (5.74) | 657 (7.58) | <0.001 b |
| Family history of Stroke (Yes) | 789 (9.60) | 801 (9.68) | 384 (4.67) | 773 (8.92) | <0.001 b |
| Family history of hypertension (Yes) | 1319 (16.04) | 1527 (17.96) | 1746 (21.17) | 1875 (21.63) | <0.001 b |
| Family history of T2DM (Yes) | 223 (2.71) | 271 (3.19) | 432 (5.24) | 481 (5.55) | <0.001 b |
| T2DM (Yes) | 800 (9.73) | 808 (9.50) | 741 (8.99) | 953 (10.99) | <0.001 b |
| Hypertension (Yes) | 435 (5.29) | 536 (6.31) | 781 (9.47) | 852 (9.83) | <0.001 b |
| Dyslipidemia (Yes) | 1569 (19.08) | 2351 (27.66) | 3181 (38.57) | 2915 (33.63) | <0.001 b |
| Air Pollutants | Line Regression β (95% CI) | ||
|---|---|---|---|
| Model 1 | Model 2 | Model 3 | |
| PM1 | 0.230 (0.159, 0.301) * | 0.217 (0.146, 0.288) * | 0.162 (0.091, 0.233) * |
| PM2.5 | 0.570 (0.484, 0.655) * | 0.550 (0.464, 0.635) * | 0.473 (0.388, 0.559) * |
| PM10 | 0.828 (0.736, 0.919) * | 0.807 (0.715, 0.899) * | 0.718 (0.627, 0.810) * |
| NO2 | 0.909 (0.806, 1.013) * | 0.888 (0.784, 0.991) * | 0.795 (0.691, 0.898) * |
| Air pollution score | 0.952 (0.866, 1.038) * | 0.933 (0.847, 1.020) * | 0.854 (0.768, 0.940) * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wu, X.; Liu, X.; Liao, W.; Dong, X.; Li, R.; Hou, J.; Mao, Z.; Huo, W.; Guo, Y.; Li, S.; et al. Healthier Lifestyles Attenuated Association of Single or Mixture Exposure to Air Pollutants with Cardiometabolic Risk in Rural Chinese Adults. Toxics 2022, 10, 541. https://doi.org/10.3390/toxics10090541
Wu X, Liu X, Liao W, Dong X, Li R, Hou J, Mao Z, Huo W, Guo Y, Li S, et al. Healthier Lifestyles Attenuated Association of Single or Mixture Exposure to Air Pollutants with Cardiometabolic Risk in Rural Chinese Adults. Toxics. 2022; 10(9):541. https://doi.org/10.3390/toxics10090541
Chicago/Turabian StyleWu, Xueyan, Xiaotian Liu, Wei Liao, Xiaokang Dong, Ruiying Li, Jian Hou, Zhenxing Mao, Wenqian Huo, Yuming Guo, Shanshan Li, and et al. 2022. "Healthier Lifestyles Attenuated Association of Single or Mixture Exposure to Air Pollutants with Cardiometabolic Risk in Rural Chinese Adults" Toxics 10, no. 9: 541. https://doi.org/10.3390/toxics10090541
APA StyleWu, X., Liu, X., Liao, W., Dong, X., Li, R., Hou, J., Mao, Z., Huo, W., Guo, Y., Li, S., Chen, G., & Wang, C. (2022). Healthier Lifestyles Attenuated Association of Single or Mixture Exposure to Air Pollutants with Cardiometabolic Risk in Rural Chinese Adults. Toxics, 10(9), 541. https://doi.org/10.3390/toxics10090541