Organ-Specific Endothelial Dysfunction Following Total Body Irradiation Exposure
Abstract
1. Introduction
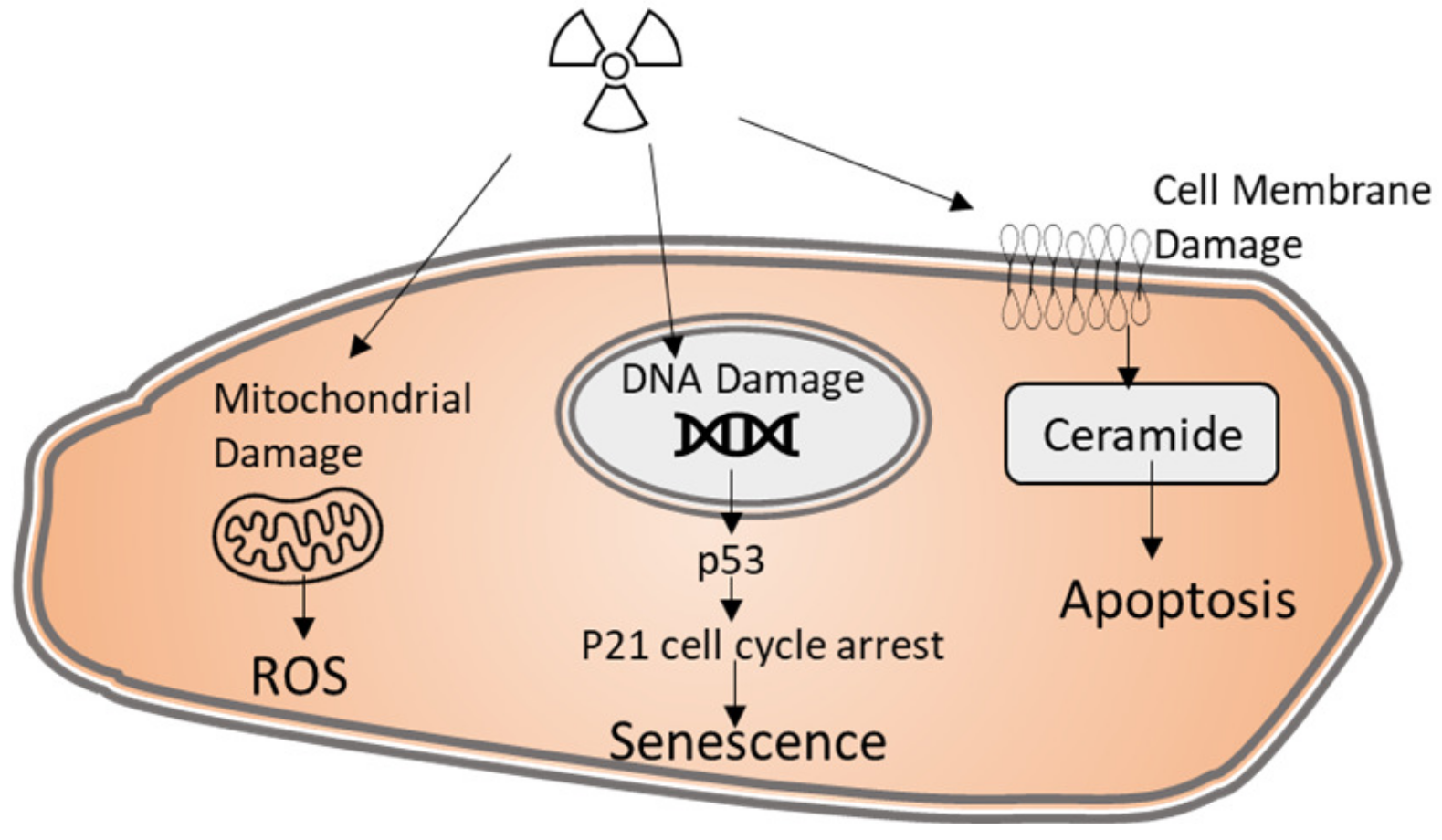
2. Radiation-Induced Endothelial Cell Injury
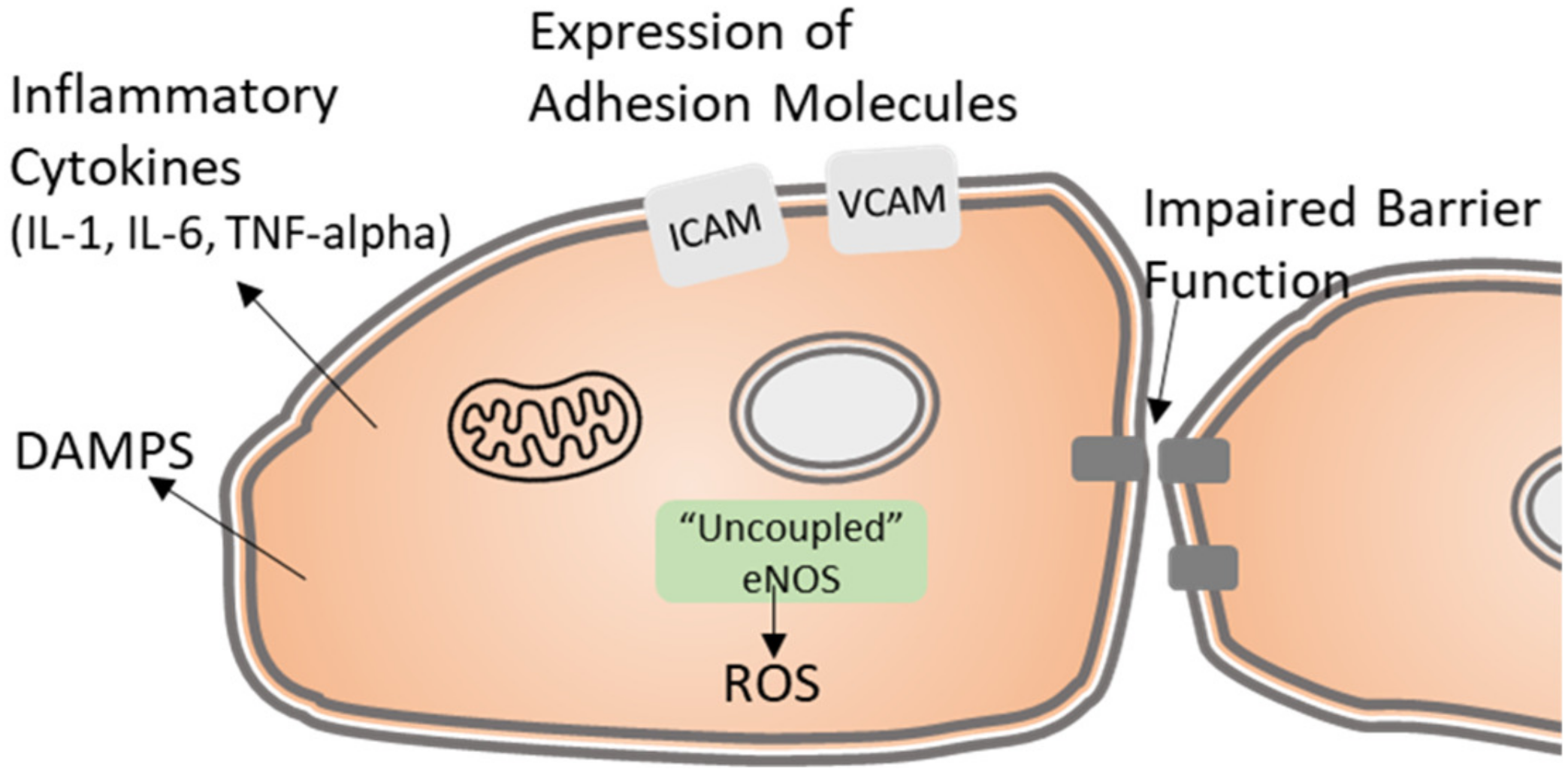
3. Radiation-Induced Endothelial Functional Alterations
4. Hematologic Acute Radiation Syndrome (H-ARS)
5. Gastrointestinal Acute Radiation Syndrome (GI-ARS)
6. Late Responding Organs
7. Radiation Enteropathy
8. Radiation-Induced Lung Injury
9. Heart Disease
10. Radiation Nephropathy
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Satyamitra, M.M.; DiCarlo, A.L.; Taliaferro, L. Understanding the Pathophysiology and Challenges of Development of Medical Countermeasures for Radiation-Induced Vascular/Endothelial Cell Injuries: Report of a NIAID Workshop, August 20, 2015. Radiat. Res. 2016, 186, 99–111. [Google Scholar] [CrossRef] [PubMed]
- Venkatesulu, B.P.; Mahadevan, L.S.; Aliru, M.L.; Yang, X.; Bodd, M.H.; Singh, P.K.; Yusuf, S.W.; Abe, J.-I.; Krishnan, S. Radiation-Induced Endothelial Vascular Injury: A Review of Possible Mechanisms. JACC Basic Transl. Sci. 2018, 3, 563–572. [Google Scholar] [CrossRef] [PubMed]
- Belzile-Dugas, E.; Eisenberg, M.J. Radiation-Induced Cardiovascular Disease: Review of an Underrecognized Pathology. J. Am. Heart Assoc. 2021, 10, e021686. [Google Scholar] [CrossRef] [PubMed]
- MacVittie, T.J.; Farese, A.M.; Parker, G.A.; Bennett, A.W.; Jackson, W.E., 3rd. Acute Radiation-induced Lung Injury in the Non-human Primate: A Review and Comparison of Mortality and Co-morbidities Using Models of Partial-body Irradiation with Marginal Bone Marrow Sparing and Whole Thorax Lung Irradiation. Health Phys. 2020, 119, 559–587. [Google Scholar] [CrossRef]
- Kusunoki, Y.; Hayashi, T. Long-lasting alterations of the immune system by ionizing radiation exposure: Implications for disease development among atomic bomb survivors. Int. J. Radiat. Biol. 2008, 84, 1–14. [Google Scholar] [CrossRef]
- Baselet, B.; Sonveaux, P.; Baatout, S.; Aerts, A. Pathological effects of ionizing radiation: Endothelial activation and dysfunction. Cell. Mol. Life Sci. 2019, 76, 699–728. [Google Scholar] [CrossRef]
- Wijerathne, H.; Langston, J.C.; Yang, Q.; Sun, S.; Miyamoto, C.; Kilpatrick, L.E.; Kiani, M.F. Mechanisms of radiation-induced endothelium damage: Emerging models and technologies. Radiother. Oncol. 2021, 158, 21–32. [Google Scholar] [CrossRef]
- Hooper, A.T.; Butler, J.M.; Nolan, D.J.; Kranz, A.; Iida, K.; Kobayashi, M.; Kopp, H.-G.; Shido, K.; Petit, I.; Yanger, K.; et al. Engraftment and Reconstitution of Hematopoiesis Is Dependent on VEGFR2-Mediated Regeneration of Sinusoidal Endothelial Cells. Cell Stem Cell 2009, 4, 263–274. [Google Scholar] [CrossRef]
- Doan, P.L.; Russell, J.L.; Himburg, H.A.; Helms, K.; Harris, J.R.; Lucas, J.; Holshausen, K.C.; Meadows, S.K.; Daher, P.; Jeffords, L.B.; et al. Tie2+ Bone Marrow Endothelial Cells Regulate Hematopoietic Stem Cell Regeneration Following Radiation Injury. Stem Cells 2013, 31, 327–337. [Google Scholar] [CrossRef]
- Paris, F.; Fuks, Z.; Kang, A.; Capodieci, P.; Juan, G.; Ehleiter, D.; Haimovitz-Friedman, A.; Cordon-Cardo, C.; Kolesnick, R. Endothelial Apoptosis as the Primary Lesion Initiating Intestinal Radiation Damage in Mice. Science 2001, 293, 293–297. [Google Scholar] [CrossRef]
- Rotolo, J.A.; Fong, C.S.; Bodo, S.; Nagesh, P.K.; Fuller, J.; Sharma, T.; Piersigilli, A.; Zhang, Z.; Fuks, Z.; Singh, V.K.; et al. Anti-ceramide single-chain variable fragment mitigates radiation GI syndrome mortality independent of DNA repair. JCI Insight 2021, 6, e145380. [Google Scholar] [CrossRef]
- Rotolo, J.; Stancevic, B.; Zhang, J.; Hua, G.; Fuller, J.; Yin, X.; Haimovitz-Friedman, A.; Kim, K.; Qian, M.; Cardó-Vila, M.; et al. Anti-ceramide antibody prevents the radiation gastrointestinal syndrome in mice. J. Clin. Investig. 2012, 122, 1786–1790. [Google Scholar] [CrossRef]
- Rafii, S.; Butler, J.M.; Ding, B.-S. Angiocrine functions of organ-specific endothelial cells. Nature 2016, 529, 316–325. [Google Scholar] [CrossRef]
- Nolan, D.J.; Ginsberg, M.; Israely, E.; Palikuqi, B.; Poulos, M.G.; James, D.; Ding, B.-S.; Schachterle, W.; Liu, Y.; Rosenwaks, Z.; et al. Molecular Signatures of Tissue-Specific Microvascular Endothelial Cell Heterogeneity in Organ Maintenance and Regeneration. Dev. Cell 2013, 26, 204–219. [Google Scholar] [CrossRef]
- Aird, W.C. Endothelial Cell Heterogeneity. Cold Spring Harb. Perspect. Med. 2012, 2, a006429. [Google Scholar] [CrossRef]
- Vilenchik, M.M.; Knudson, A.G. Endogenous DNA double-strand breaks: Production, fidelity of repair, and induction of cancer. Proc. Natl. Acad. Sci. USA 2003, 100, 12871–12876. [Google Scholar] [CrossRef]
- Bakkenist, C.J.; Kastan, M.B. DNA damage activates ATM through intermolecular autophosphorylation and dimer dissociation. Nature 2003, 421, 499–506. [Google Scholar] [CrossRef]
- Eriksson, D.; Stigbrand, T. Radiation-induced cell death mechanisms. Tumour Biol. 2010, 31, 363–372. [Google Scholar] [CrossRef]
- Jackson, J.G.; Post, S.M.; Lozano, G. Regulation of tissue- and stimulus-specific cell fate decisions by p53 in vivo. J. Pathol. 2011, 223, 127–137. [Google Scholar] [CrossRef]
- Lee, C.-L.; Blum, J.M.; Kirsch, D.G. Role of p53 in regulating tissue response to radiation by mechanisms independent of apoptosis. Transl. Cancer Res. 2013, 2, 412–421. [Google Scholar] [PubMed]
- Lee, C.-L.; Moding, E.J.; Cuneo, K.C.; Li, Y.; Sullivan, J.M.; Mao, L.; Washington, I.; Jeffords, L.B.; Rodrigues, R.C.; Ma, Y.; et al. p53 Functions in Endothelial Cells to Prevent Radiation-Induced Myocardial Injury in Mice. Sci. Signal. 2012, 5, ra52. [Google Scholar] [CrossRef] [PubMed]
- Panganiban, R.A.M.; Mungunsukh, O.; Day, R.M. X-irradiation induces ER stress, apoptosis, and senescence in pulmonary artery endothelial cells. Int. J. Radiat. Biol. 2013, 89, 656–667. [Google Scholar] [CrossRef] [PubMed]
- Nagane, M.; Yasui, H.; Kuppusamy, P.; Yamashita, T.; Inanami, O. DNA damage response in vascular endothelial senescence: Implication for radiation-induced cardiovascular diseases. J. Radiat. Res. 2021, 62, 564–573. [Google Scholar] [CrossRef]
- Lowe, D.; Raj, K. Premature aging induced by radiation exhibits pro-atherosclerotic effects mediated by epigenetic activation ofCD44 expression. Aging Cell 2014, 13, 900–910. [Google Scholar] [CrossRef]
- Rodemann, H.P.; Blaese, M.A. Responses of Normal Cells to Ionizing Radiation. Semin. Radiat. Oncol. 2007, 17, 81–88. [Google Scholar] [CrossRef]
- Haimovitz-Friedman, A.; Kan, C.C.; Ehleiter, D.; Persaud, R.S.; McLoughlin, M.; Fuks, Z.; Kolesnick, R.N. Ionizing radiation acts on cellular membranes to generate ceramide and initiate apoptosis. J. Exp. Med. 1994, 180, 525–535. [Google Scholar] [CrossRef]
- Oskouian, B.; Saba, J.D. Cancer Treatment Strategies Targeting Sphingolipid Metabolism. Adv. Exp. Med. Biol. 2010, 688, 185–205. [Google Scholar] [CrossRef]
- Kolesnick, R.; Fuks, Z. Radiation and ceramide-induced apoptosis. Oncogene 2003, 22, 5897–5906. [Google Scholar] [CrossRef]
- Santana, P.; Peña, L.A.; Haimovitz-Friedman, A.; Martin, S.; Green, D.; McLoughlin, M.; Cordon-Cardo, C.; Schuchman, E.H.; Fuks, Z.; Kolesnick, R. Acid Sphingomyelinase–Deficient Human Lymphoblasts and Mice Are Defective in Radiation-Induced Apoptosis. Cell 1996, 86, 189–199. [Google Scholar] [CrossRef]
- Peña, L.A.; Fuks, Z.; Kolesnick, R.N. Radiation-induced apoptosis of endothelial cells in the murine central nervous system: Protection by fibroblast growth factor and sphingomyelinase deficiency. Cancer Res. 2000, 60, 321–327. [Google Scholar]
- Paris, F.; Grassmé, H.; Cremesti, A.; Zager, J.; Fong, Y.; Haimovitz-Friedman, A.; Fuks, Z.; Gulbins, E.; Kolesnick, R. Natural Ceramide Reverses Fas Resistance of Acid Sphingomyelinase (-/-)Hepatocytes. J. Biol. Chem. 2001, 276, 8297–8305. [Google Scholar] [CrossRef] [PubMed]
- Mansilla, S.; Bataller, M. Mechanisms of Drug-Induced Mitotic Catastrophe in Cancer Cells. Curr. Pharm. Des. 2010, 16, 69–78. [Google Scholar] [CrossRef]
- Martins, I.; Galluzzi, L.; Kroemer, G. Hormesis, cell death and aging. Aging 2011, 3, 821–828. [Google Scholar] [CrossRef]
- Leach, J.K.; Van Tuyle, G.; Lin, P.S.; Schmidt-Ullrich, R.; Mikkelsen, R.B. Ionizing radiation-induced, mitochondria-dependent generation of reactive oxygen/nitrogen. Cancer Res 2001, 61, 3894–3901. [Google Scholar]
- Baselet, B.; Driesen, R.B.; Coninx, E.; Belmans, N.; Sieprath, T.; Lambrichts, I.; De Vos, W.H.; Baatout, S.; Sonveaux, P.; Aerts, A. Rosiglitazone Protects Endothelial Cells from Irradiation-Induced Mitochondrial Dysfunction. Front. Pharmacol. 2020, 11, 268. [Google Scholar] [CrossRef]
- Hellweg, C.E. The Nuclear Factor κB pathway: A link to the immune system in the radiation response. Cancer Lett. 2015, 368, 275–289. [Google Scholar] [CrossRef]
- Goebeler, M.; Gillitzer, R.; Kilian, K.; Utzel, K.; Bröcker, E.-B.; Rapp, U.R.; Ludwig, S. Multiple signaling pathways regulate NF-κB–dependent transcription of the monocyte chemoattractant protein-1 gene in primary endothelial cells. Blood J. Am. Soc. Hematol. 2001, 97, 46–55. [Google Scholar] [CrossRef]
- Kim, I.; Moon, S.-O.; Kim, S.H.; Kim, H.J.; Koh, Y.S.; Koh, G.Y. Vascular Endothelial Growth Factor Expression of Intercellular Adhesion Molecule 1 (ICAM-1), Vascular Cell Adhesion Molecule 1 (VCAM-1), and E-selectin through Nuclear Factor-κB Activation in Endothelial Cells. J. Biol. Chem. 2001, 276, 7614–7620. [Google Scholar] [CrossRef]
- Soroush, F.; Tang, Y.; Zaidi, H.M.; Sheffield, J.B.; Kilpatrick, L.E.; Kiani, M.F. PKCδ inhibition as a novel medical countermeasure for radiation-induced vascular damage. FASEB J. 2018, 32, fj201701099. [Google Scholar] [CrossRef]
- Soroush, F.; Zhang, T.; King, D.J.; Tang, Y.; Deosarkar, S.; Prabhakarpandian, B.; Kilpatrick, L.E.; Kiani, M.F. A novel microfluidic assay reveals a key role for protein kinase C δ in regulating human neutrophil–endothelium interaction. J. Leukoc. Biol. 2016, 100, 1027–1035. [Google Scholar] [CrossRef]
- Claesson-Welsh, L.; Dejana, E.; McDonald, D.M. Permeability of the Endothelial Barrier: Identifying and Reconciling Controversies. Trends Mol. Med. 2020, 27, 314–331. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.P.; Frei, A.C.; Narayanan, J.; Gasperetti, T.; Veley, D.; Amjad, A.; Albano, K.; Fish, B.L.; Himburg, H.A. Brain-derived neurotrophic factor promotes immune reconstitution following radiation injury via activation of bone marrow mesenchymal stem cells. PLoS ONE 2021, 16, e0259042. [Google Scholar] [CrossRef]
- Jagtap, J.; Audi, S.; Razeghi-Kondelaji, M.H.; Fish, B.L.; Hansen, C.; Narayan, J.; Gao, F.; Sharma, G.; Parchur, A.K.; Banerjee, A.; et al. A rapid dynamic in vivo near-infrared fluorescence imaging assay to track lung vascular permeability after acute radiation injury. Am. J. Physiol. Cell. Mol. Physiol. 2021, 320, L436–L450. [Google Scholar] [CrossRef]
- Kouam, P.N.; Rezniczek, G.A.; Adamietz, I.A.; Bühler, H. Ionizing radiation increases the endothelial permeability and the transendothelial migration of tumor cells through ADAM10-activation and subsequent degradation of VE-cadherin. BMC Cancer 2019, 19, 958. [Google Scholar] [CrossRef]
- Sharma, P.; Templin, T.; Grabham, P. Short term effects of gamma radiation on endothelial barrier function: Uncoupling of PECAM-1. Microvasc. Res. 2013, 86, 11–20. [Google Scholar] [CrossRef]
- Otterson, M.F.; Nie, L.; Schmidt, J.L.; Link, B.J.; Jovanovic, N.; Lyros, O.; Rafiee, P. EUK-207 protects human intestinal microvascular endothelial cells (HIMEC) against irradiation-induced apoptosis through the Bcl2 pathway. Life Sci. 2012, 91, 771–782. [Google Scholar] [CrossRef]
- Mahmood, J.; Jelveh, S.; Calveley, V.; Zaidi, A.; Doctrow, S.R.; Hill, R.P. Mitigation of radiation-induced lung injury by genistein and EUK-207. Int. J. Radiat. Biol. 2011, 87, 889–901. [Google Scholar] [CrossRef]
- Gao, F.; Fish, B.L.; Szabo, A.; Doctrow, S.R.; Kma, L.; Molthen, R.C.; Moulder, J.E.; Jacobs, E.R.; Medhora, M. Short-Term Treatment with a SOD/Catalase Mimetic, EUK-207, Mitigates Pneumonitis and Fibrosis after Single-Dose Total-Body or Whole-Thoracic Irradiation. Radiat. Res. 2012, 178, 468–480. [Google Scholar] [CrossRef]
- Rabender, C.S.; Mezzaroma, E.; Yakovlev, V.A.; Mauro, A.G.; Bonaventura, A.; Abbate, A.; Mikkelsen, R.B. Mitigation of Radiation-Induced Lung and Heart Injuries in Mice by Oral Sepiapterin after Irradiation. Radiat. Res. 2021, 195, 463–473. [Google Scholar] [CrossRef]
- Itkin, T.; Gur-Cohen, S.; Spencer, J.A.; Schajnovitz, A.; Ramasamy, S.K.; Kusumbe, A.P.; Ledergor, G.; Jung, Y.; Milo, I.; Poulos, M.G.; et al. Distinct bone marrow blood vessels differentially regulate haematopoiesis. Nature 2016, 532, 323–328. [Google Scholar] [CrossRef]
- Ramalingam, P.; Butler, J.M.; Poulos, M.G. Vascular Regulation of Hematopoietic Stem Cell Homeostasis, Regeneration, and Aging. Curr. Stem Cell Rep. 2021, 7, 194–203. [Google Scholar] [CrossRef] [PubMed]
- Kunisaki, Y.; Frenette, P.S. Influences of vascular niches on hematopoietic stem cell fate. Int. J. Hematol. 2014, 99, 699–705. [Google Scholar] [CrossRef] [PubMed]
- Shirota, T.; Tavassoli, M. Alterations of bone marrow sinus endothelium induced by ionizing irradiation: Implications in the homing of intravenously transplanted marrow cells. Blood cells 1992, 18, 197–214. [Google Scholar]
- Li, X.-M.; Hu, Z.; Jorgenson, M.L.; Wingard, J.R.; Slayton, W.B. Bone marrow sinusoidal endothelial cells undergo nonapoptotic cell death and are replaced by proliferating sinusoidal cells in situ to maintain the vascular niche following lethal irradiation. Exp. Hematol. 2008, 36, 1143–1156.e3. [Google Scholar] [CrossRef]
- Huang, W.; Yang, Y.; Sun, Z.; Zeng, X. Early Radiation-induced Bone Marrow Injury: Serial MR Imaging During Initial 4 Weeks After Irradiation. Acad. Radiol. 2009, 16, 733–738. [Google Scholar] [CrossRef]
- Chen, Q.; Liu, Y.; Jeong, H.-W.; Stehling, M.; Dinh, V.V.; Zhou, B.; Adams, R.H. Apelin+ Endothelial Niche Cells Control Hematopoiesis and Mediate Vascular Regeneration after Myeloablative Injury. Cell Stem Cell 2019, 25, 768–783.e6. [Google Scholar] [CrossRef]
- Cary, L.; Noutai, D.; Salber, R.; Fadiyimu, O.; Gross, A.; Almeida-Porada, G.; Kidane, Y.; Whitnall, M. Bone Marrow Endothelial Cells Influence Function and Phenotype of Hematopoietic Stem and Progenitor Cells after Mixed Neutron/Gamma Radiation. Int. J. Mol. Sci. 2019, 20, 1795. [Google Scholar] [CrossRef]
- Poulos, M.G.; Guo, P.; Kofler, N.M.; Pinho, S.; Gutkin, M.C.; Tikhonova, A.; Aifantis, I.; Frenette, P.S.; Kitajewski, J.; Rafii, S.; et al. Endothelial Jagged-1 Is Necessary for Homeostatic and Regenerative Hematopoiesis. Cell Rep. 2013, 4, 1022–1034. [Google Scholar] [CrossRef]
- Himburg, H.A.; Muramoto, G.G.; Daher, P.; Meadows, S.K.; Russell, J.L.; Doan, P.; Chi, J.-T.; Salter, A.B.; Lento, W.E.; Reya, T.; et al. Pleiotrophin regulates the expansion and regeneration of hematopoietic stem cells. Nat. Med. 2010, 16, 475–482. [Google Scholar] [CrossRef]
- Himburg, H.A.; Yan, X.; Doan, P.L.; Quarmyne, M.; Micewicz, E.; McBride, W.; Chao, N.J.; Slamon, D.J.; Chute, J.P. Pleiotrophin mediates hematopoietic regeneration via activation of RAS. J. Clin. Investig. 2014, 124, 4753–4758. [Google Scholar] [CrossRef]
- Doan, P.L.; Himburg, H.A.; Helms, K.; Russell, J.L.; Fixsen, E.; Quarmyne, M.; Harris, J.R.; Deoliviera, D.; Sullivan, J.M.; Chao, N.J.; et al. Epidermal growth factor regulates hematopoietic regeneration after radiation injury. Nat. Med. 2013, 19, 295–304. [Google Scholar] [CrossRef] [PubMed]
- Piryani, S.O.; Kam, A.Y.F.; Vu, U.T.; Chao, N.J.; Doan, P.L. CCR5 Signaling Promotes Murine and Human Hematopoietic Regeneration following Ionizing Radiation. Stem Cell Rep. 2019, 13, 76–90. [Google Scholar] [CrossRef]
- Winkler, I.G.; Barbier, V.; Nowlan, B.; Jacobsen, R.N.; Forristal, C.E.; Patton, J.T.; Magnani, J.L.; Lévesque, J.-P. Vascular niche E-selectin regulates hematopoietic stem cell dormancy, self renewal and chemoresistance. Nat. Med. 2012, 18, 1651–1657. [Google Scholar] [CrossRef]
- Himburg, H.A.; Termini, C.M.; Schlussel, L.; Kan, J.; Li, M.; Zhao, L.; Fang, T.; Sasine, J.P.; Chang, V.Y.; Chute, J.P. Distinct Bone Marrow Sources of Pleiotrophin Control Hematopoietic Stem Cell Maintenance and Regeneration. Cell Stem Cell 2018, 23, 370–381.e5. [Google Scholar] [CrossRef]
- Chute, J.P.; Muramoto, G.G.; Salter, A.B.; Meadows, S.K.; Rickman, D.W.; Chen, B.; Himburg, H.A.; Chao, N.J. Transplantation of vascular endothelial cells mediates the hematopoietic recovery and survival of lethally irradiated mice. Blood 2007, 109, 2365–2372. [Google Scholar] [CrossRef]
- Poulos, M.G.; Ramalingam, P.; Gutkin, M.C.; Llanos, P.; Gilleran, K.; Rabbany, S.Y.; Butler, J.M. Endothelial transplantation rejuvenates aged hematopoietic stem cell function. J. Clin. Investig. 2017, 127, 4163–4178. [Google Scholar] [CrossRef]
- Li, B.; Bailey, A.S.; Jiang, S.; Liu, B.; Goldman, D.C.; Fleming, W.H. Endothelial cells mediate the regeneration of hematopoietic stem cells. Stem Cell Res. 2010, 4, 17–24. [Google Scholar] [CrossRef]
- Piryani, S.O.; Jiao, Y.; Kam, A.Y.F.; Liu, Y.; Vo-Dinh, T.; Chen, B.J.; Chao, N.J.; Doan, P.L. Endothelial Cell-Derived Extracellular Vesicles Mitigate Radiation-Induced Hematopoietic Injury. Int. J. Radiat. Oncol Biol. Phys. 2019, 104, 291–301. [Google Scholar] [CrossRef]
- Kim, M.M.; Schlussel, L.; Zhao, L.; Himburg, H.A. Dickkopf-1 Treatment Stimulates Hematopoietic Regenerative Function in Infused Endothelial Progenitor Cells. Radiat. Res. 2019, 192, 53–62. [Google Scholar] [CrossRef]
- Zachman, D.K.; Leon, R.P.; Das, P.; Goldman, D.C.; Hamlin, K.L.; Guha, C.; Fleming, W.H. Endothelial cells mitigate DNA damage and promote the regeneration of hematopoietic stem cells after radiation injury. Stem Cell Res. 2013, 11, 1013–1021. [Google Scholar] [CrossRef][Green Version]
- Wang, J.; Boerma, M.; Fu, Q.; Hauer-Jensen, M. Significance of endothelial dysfunction in the pathogenesis of early and delayed radiation enteropathy. World J. Gastroenterol. 2007, 13, 3047–3055. [Google Scholar] [CrossRef]
- Gur-Cohen, S.; Itkin, T.; Chakrabarty, S.; Graf, C.; Kollet, O.; Ludin, A.; Golan, K.; Kalinkovich, A.; Ledergor, G.; Wong, E.; et al. PAR1 signaling regulates the retention and recruitment of EPCR-expressing bone marrow hematopoietic stem cells. Nat. Med. 2015, 21, 1307–1317. [Google Scholar] [CrossRef] [PubMed]
- Geiger, H.; Pawar, S.A.; Kerschen, E.J.; Nattamai, K.J.; Hernandez, I.; Liang, H.P.; Fernández, J.A.; Cancelas, J.A.; Ryan, M.A.; Kustikova, O.; et al. Pharmacological targeting of the thrombomodulin–activated protein C pathway mitigates radiation toxicity. Nat. Med. 2012, 18, 1123–1129. [Google Scholar] [CrossRef] [PubMed]
- Termini, C.M.; Pang, A.; Fang, T.; Roos, M.; Chang, V.Y.; Zhang, Y.; Setiawan, N.J.; Signaevskaia, L.; Li, M.; Kim, M.M.; et al. Neuropilin 1 regulates bone marrow vascular regeneration and hematopoietic reconstitution. Nat. Commun. 2021, 12, 6990. [Google Scholar] [CrossRef]
- MacVittie, T.J.; Farese, A.M.; Bennett, A.; Gelfond, D.; Shea-Donohue, T.; Tudor, G.; Booth, C.; McFarland, E.; Jackson, W., 3rd. The Acute Gastrointestinal Subsyndrome of the Acute Radiation Syndrome: A rhesus macaque model. Health Phys. 2012, 103, 411–426. [Google Scholar] [CrossRef]
- MacVittie, T.J.; Bennett, A.; Booth, C.; Garofalo, M.; Tudor, G.; Ward, A.; Shea-Donohue, T.; Gelfond, D.; McFarland, E.; Jackson, W., 3rd; et al. The Prolonged Gastrointestinal Syndrome in Rhesus Macaques: The relationship between gastrointestinal, hematopoietic, and delayed multi-organ sequelae following acute, potentially lethal, partial-body irradiation. Health Phys. 2012, 103, 427–453. [Google Scholar] [CrossRef]
- Santos, A.J.M.; Lo, Y.-H.; Mah, A.T.; Kuo, C.J. The Intestinal Stem Cell Niche: Homeostasis and Adaptations. Trends Cell Biol. 2018, 28, 1062–1078. [Google Scholar] [CrossRef]
- Spadoni, I.; Pietrelli, A.; Pesole, G.; Rescigno, M. Gene expression profile of endothelial cells during perturbation of the gut vascular barrier. Gut Microbes 2016, 7, 540–548. [Google Scholar] [CrossRef]
- Schuller, B.W.; Binns, P.J.; Riley, K.J.; Ma, L.; Hawthorne, M.F.; Coderre, J.A. Selective irradiation of the vascular endothelium has no effect on the survival of murine intestinal crypt stem cells. Proc. Natl. Acad. Sci. USA 2006, 103, 3787–3792. [Google Scholar] [CrossRef]
- Williams, J.P.; Jackson, I.L.; Shah, J.R.; Czarniecki, C.W.; Maidment, B.W.; DiCarlo, A.L. Animal Models and Medical Countermeasures Development for Radiation-Induced Lung Damage: Report from an NIAID Workshop. Radiat. Res. 2012, 177, e0025–e0039. [Google Scholar] [CrossRef]
- Mehrvar, S.; Mostaghimi, S.; Camara, A.K.; Foomani, F.; Narayanan, J.; Fish, B.; Medhora, M.; Ranji, M. Three-dimensional vascular and metabolic imaging using inverted autofluorescence. J. Biomed. Opt. 2021, 26, 076002. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.N.; Wu, Q.; Mäder, M.; Fish, B.L.; Moulder, J.E.; Jacobs, E.R.; Medhora, M.; Molthen, R.C. Vascular Injury after Whole Thoracic X-Ray Irradiation in the Rat. Int. J. Radiat. Oncol. 2009, 74, 192–199. [Google Scholar] [CrossRef]
- Robbins, M.E.; Brunso-Bechtold, J.K.; Peiffer, A.M.; Tsien, C.I.; Bailey, J.E.; Marks, L.B. Imaging Radiation-Induced Normal Tissue Injury. Radiat. Res. 2012, 177, 449–466. [Google Scholar] [CrossRef] [PubMed]
- Farhood, B.; Aliasgharzadeh, A.; Amini, P.; Rezaeyan, A.; Tavassoli, A.; Motevaseli, E.; Shabeeb, D.; Musa, A.E.; Najafi, M. Mitigation of Radiation-Induced Lung Pneumonitis and Fibrosis Using Metformin and Melatonin: A Histopathological Study. Medicina 2019, 55, 417. [Google Scholar] [CrossRef]
- Graham, M.M.; Evans, M.L.; Dahlen, D.D.; Mahler, P.A.; Rasey, J.S. Pharmacological alteration of the lung vascular response to radiation. Int. J. Radiat. Oncol. Biol. Phys. 1990, 19, 329–339. [Google Scholar] [CrossRef]
- Klaus, R.; Niyazi, M.; Lange-Sperandio, B. Radiation-induced kidney toxicity: Molecular and cellular pathogenesis. Radiat. Oncol. 2021, 16, 43. [Google Scholar] [CrossRef]
- Gao, F.; Dong, W.; Liu, P.; Narayanan, J.; Fish, B.L.; Jacobs, E.R.; Medhora, M. Molecular Changes in miRNA in Irradiated Rat Kidneys: Role of miR-34a and its Vascular Targets in the Notch Pathway. Radiat. Res. 2021, 196, 611–622. [Google Scholar] [CrossRef]
- Unthank, J.L.; Miller, S.J.; Quickery, A.K.; Ferguson, E.L.; Wang, M.; Sampson, C.H.; Chua, H.L.; DiStasi, M.R.; Feng, H.; Fisher, A. Delayed effects of acute radiation exposure in a murine model of the H-ARS: Multiple-organ injury consequent to< 10 Gy total body irradiation. Health Phys. 2015, 109, 511. [Google Scholar]
- Unthank, J.L.; Ortiz, M.; Trivedi, H.; Pelus, L.M.; Sampson, C.H.; Sellamuthu, R.; Fisher, A.; Chua, H.L.; Plett, A.; Orschell, C.M.; et al. Cardiac and Renal Delayed Effects of Acute Radiation Exposure: Organ Differences in Vasculopathy, Inflammation, Senescence and Oxidative Balance. Radiat. Res. 2019, 191, 383–397. [Google Scholar] [CrossRef]
- Boerma, M.; Hauer-Jensen, M. Potential Targets for Intervention in Radiation-Induced Heart Disease. Curr. Drug Targets 2010, 11, 1405–1412. [Google Scholar] [CrossRef]
- Baker, J.E.; Fish, B.L.; Su, J.; Haworth, S.T.; Strande, J.L.; Komorowski, R.A.; Migrino, R.Q.; Doppalapudi, A.; Harmann, L.; Allen Li, X.; et al. 10 Gy total body irradiation increases risk of coronary sclerosis, degeneration of heart structure and function in a rat model. Int. J. Radiat. Biol. 2009, 85, 1089–1100. [Google Scholar] [CrossRef] [PubMed]
- van Luijk, P.; Novakova-Jiresova, A.; Faber, H.; Schippers, J.M.; Kampinga, H.H.; Meertens, H.; Coppes, R.P. Radiation Damage to the Heart Enhances Early Radiation-Induced Lung Function Loss. Cancer Res. 2005, 65, 6509–6511. [Google Scholar] [CrossRef]
- Andrews, R.N.; Bloomer, E.G.; Olson, J.D.; Hanbury, D.B.; Dugan, G.O.; Whitlow, C.T.; Cline, J.M. Non-Human Primates Receiving High-Dose Total-Body Irradiation are at Risk of Developing Cerebrovascular Injury Years Postirradiation. Radiat. Res. 2020, 194, 277–287. [Google Scholar] [CrossRef]
- Wang, J.; Zheng, H.; Kulkarni, A.; Ou, X.; Hauer-Jensen, M. Regulation of early and delayed radiation responses in rat small intestine by capsaicin-sensitive nerves. Int. J. Radiat. Oncol. Biol. Phys. 2006, 64, 1528–1536. [Google Scholar] [CrossRef]
- Lee, C.-L.; Daniel, A.R.; Holbrook, M.; Brownstein, J.; Silva Campos, L.D.; Hasapis, S.; Ma, Y.; Borst, L.B.; Badea, C.T.; Kirsch, D.G. Sensitization of Vascular Endothelial Cells to Ionizing Radiation Promotes the Development of Delayed Intestinal Injury in Mice. Radiat. Res. 2019, 192, 258–266. [Google Scholar] [CrossRef]
- Richter, K.K.; Fink, L.M.; Hughes, B.M.; Sung, C.-C.; Hauer-Jensen, M. Is the loss of endothelial thrombomodulin involved in the mechanism of chronicity in late radiation enteropathy? Radiother. Oncol. 1997, 44, 65–71. [Google Scholar] [CrossRef]
- Richter, K.K.; Fink, L.M.; Hughes, B.M.; Shmaysani, H.M.; Sung, C.-C.; Hauer-Jensen, M. Differential effect of radiation on endothelial cell function in rectal cancer and normal rectum. Am. J. Surg. 1998, 176, 642–647. [Google Scholar] [CrossRef]
- Pathak, R.; Wang, J.; Garg, S.; Aykin-Burns, N.; Petersen, K.-U.; Hauer-Jensen, M. Recombinant Thrombomodulin (Solulin) Ameliorates Early Intestinal Radiation Toxicity in a Preclinical Rat Model. Radiat. Res. 2016, 186, 112–120. [Google Scholar] [CrossRef]
- Jang, H.; Kwak, S.-Y.; Park, S.; Kim, K.; Kim, Y.-H.; Na, J.; Kim, H.; Jang, W.-S.; Lee, S.-J.; Kim, M.J.; et al. Pravastatin Alleviates Radiation Proctitis by Regulating Thrombomodulin in Irradiated Endothelial Cells. Int. J. Mol. Sci. 2020, 21, 1897. [Google Scholar] [CrossRef]
- Sridharan, V.; Johnson, K.A.; Landes, R.D.; Cao, M.; Singh, P.; Wagoner, G.; Hayar, A.; Sprick, E.D.; Eveld, K.A.; Bhattacharyya, A.; et al. Sex-dependent effects of genetic upregulation of activated protein C on delayed effects of acute radiation exposure in the mouse heart, small intestine, and skin. PLoS ONE 2021, 16, e0252142. [Google Scholar] [CrossRef]
- Williams, J.P.; Brown, S.L.; Georges, G.E.; Hauer-Jensen, M.; Hill, R.P.; Huser, A.K.; Kirsch, D.G.; MacVittie, T.J.; Mason, K.A.; Medhora, M.M.; et al. Animal Models for Medical Countermeasures to Radiation Exposure. Radiat. Res. 2010, 173, 557–578. [Google Scholar] [CrossRef] [PubMed]
- Rubin, P.; Finkelstein, J.; Shapiro, D. Molecular biology mechanisms in the radiation induction of pulmonary injury syndromes: Interrelationship between the alveolar macrophage and the septal fibroblast. Int. J. Radiat. Oncol. Biol. Phys. 1992, 24, 93–101. [Google Scholar] [CrossRef] [PubMed]
- Ghosh, S.N.; Zhang, R.; Fish, B.L.; Semenenko, V.A.; Li, X.A.; Moulder, J.E.; Jacobs, E.R.; Medhora, M. Renin-Angiotensin System Suppression Mitigates Experimental Radiation Pneumonitis. Int. J. Radiat. Oncol. Biol. Phys. 2009, 75, 1528–1536. [Google Scholar] [CrossRef] [PubMed]
- Sharma, G.P.; Fish, B.L.; Frei, A.C.; Narayanan, J.; Gasperetti, T.; Scholler, D.; Pierce, L.; Szalewski, N.; Blue, N.; Medhora, M.; et al. Pharmacologic ACE-Inhibition Mitigates Radiation-Induced Pneumonitis by Suppressing ACE-Expressing Lung Myeloid Cells. Int. J. Radiat. Oncol. Biol. Phys. 2022, 113, 177–191. [Google Scholar] [CrossRef] [PubMed]
- Jacobson, J.R. Sphingolipids as a Novel Therapeutic Target in Radiation-Induced Lung Injury. Cell Biochem. Biophys. 2021, 79, 509–516. [Google Scholar] [CrossRef]
- Mathew, B.; Jacobson, J.R.; Berdyshev, E.; Huang, Y.; Sun, X.; Zhao, Y.; Gerhold, L.M.; Siegler, J.; Evenoski, C.; Wang, T.; et al. Role of sphingolipids in murine radiation-induced lung injury: Protection by sphingosine 1-phosphate analogs. FASEB J. 2011, 25, 3388–3400. [Google Scholar] [CrossRef]
- Fountain, M.D.; McLellan, L.A.; Smith, N.L.; Loughery, B.F.; Rakowski, J.T.; Tse, H.Y.; Hillman, G.G. Isoflavone-mediated radioprotection involves regulation of early endothelial cell death and inflammatory signaling in Radiation-Induced lung injury. Int. J. Radiat. Biol. 2020, 96, 245–256. [Google Scholar] [CrossRef]
- Schultz-Hector, S.; Trott, K.-R. Radiation-induced cardiovascular diseases: Is the epidemiologic evidence compatible with the radiobiologic data? Int. J. Radiat. Oncol. Biol. Phys. 2007, 67, 10–18. [Google Scholar] [CrossRef]
- Hayashi, T.; Morishita, Y.; Kubo, Y.; Kusunoki, Y.; Hayashi, I.; Kasagi, F.; Hakoda, M.; Kyoizumi, S.; Nakachi, K. Long-term effects of radiation dose on inflammatory markers in atomic bomb survivors. Am. J. Med. 2005, 118, 83–86. [Google Scholar] [CrossRef]
- Shimizu, Y.; Kodama, K.; Nishi, N.; Kasagi, F.; Suyama, A.; Soda, M.; Grant, E.J.; Sugiyama, H.; Sakata, R.; Moriwaki, H.; et al. Radiation exposure and circulatory disease risk: Hiroshima and Nagasaki atomic bomb survivor data, 1950-2003. BMJ 2010, 340, b5349. [Google Scholar] [CrossRef]
- Azizova, T.V.; Grigorieva, E.S.; Hunter, N.; Pikulina, M.V.; Moseeva, M.B. Risk of mortality from circulatory diseases in Mayak workers cohort following occupational radiation exposure. J. Radiol. Prot. 2015, 35, 517–538. [Google Scholar] [CrossRef]
- Sera, N.; Hida, A.; Imaizumi, M.; Nakashima, E.; Akahoshi, M. The Association Between Chronic Kidney Disease and Cardiovascular Disease Risk Factors in Atomic Bomb Survivors. Radiat. Res. 2013, 179, 46–52. [Google Scholar] [CrossRef]
- Jaenke, R.S.; Robbins, M.E.; Bywaters, T.; Whitehouse, E.; Rezvani, M.; Hopewell, J.W. Capillary endothelium. Target site of renal radiation injury. Lab. Investig. 1993, 68, 396–405. [Google Scholar]
- Obeidat, M.; Obeidat, M.; Ballermann, B.J. Glomerular endothelium: A porous sieve and formidable barrier. Exp. Cell Res. 2012, 318, 964–972. [Google Scholar] [CrossRef]
- Lawton, C.A.; Cohen, E.P.; Barber-Derus, S.W.; Murray, K.J.; Ash, R.C.; Casper, J.T.; Moulder, J.E. Late renal dysfunction in adult survivors of bone marrow transplantation. Cancer 1991, 67, 2795–2800. [Google Scholar] [CrossRef]
| Mitigator | Mechanism of Action | Refs. |
|---|---|---|
| PKCδ-TAT | Blocks upregulation of adhesion molecules | [7,39,40] |
| SOD Mimetics | Scavengers of ROS | [46,47,48] |
| Sepiapterin | Restores eNOS “coupling” and reduces ROS | [49] |
| ECs/Vesicles | Restores hematopoiesis and rescues H-ARS lethality | [65,66,67,68,69,70] |
| Anti-Sema3A | Blocks SEMA3A binding to Neuropilin-1 | [74] |
| APC | Corrects for thrombomodulin loss | [72,73,98,99] |
| ACE inhibitors | Reduces recruitment of inflammatory immune cells | [103,104] |
| Anti-ceramide | Blocks ceramide-mediated apoptotic death | [10,11,12] |
| S1P Analogs | Restores endothelial barrier function | [105,106] |
| Soy isoflavones | Promote clearance of damaged endothelium | [107] |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharma, G.P.; Himburg, H.A. Organ-Specific Endothelial Dysfunction Following Total Body Irradiation Exposure. Toxics 2022, 10, 747. https://doi.org/10.3390/toxics10120747
Sharma GP, Himburg HA. Organ-Specific Endothelial Dysfunction Following Total Body Irradiation Exposure. Toxics. 2022; 10(12):747. https://doi.org/10.3390/toxics10120747
Chicago/Turabian StyleSharma, Guru Prasad, and Heather A. Himburg. 2022. "Organ-Specific Endothelial Dysfunction Following Total Body Irradiation Exposure" Toxics 10, no. 12: 747. https://doi.org/10.3390/toxics10120747
APA StyleSharma, G. P., & Himburg, H. A. (2022). Organ-Specific Endothelial Dysfunction Following Total Body Irradiation Exposure. Toxics, 10(12), 747. https://doi.org/10.3390/toxics10120747





