A Survey of Analytical Techniques for Noroviruses
Abstract
1. Introduction
2. Ligand-Based Detection Techniques
2.1. Ligands
2.1.1. Histo-Blood Group Antigens
2.1.2. Porcine Gastric Mucin
2.1.3. Antibody
2.1.4. Aptamers
2.2. Immune Electron Microscopy (IEM)
2.3. Immunoassays
2.3.1. Immune Adherence Hemagglutination Assay (IAHA)
2.3.2. Radio-Immunoassays (RIA)
2.3.3. Enzyme Immunoassays (EIA)
2.3.4. Immuno-Chromatography (ICG)
2.3.5. Western Blot
3. Nucleic Acid-Based Techniques
3.1. Real-Time Reverse Transcription-Polymerase Chain Reaction (RT-PCR)
3.2. Isothermal Amplification Methods
3.3. Nucleic Acid Based Methods to Assess HuNoV Infectivity
4. Biosensors
4.1. Optical Biosensors
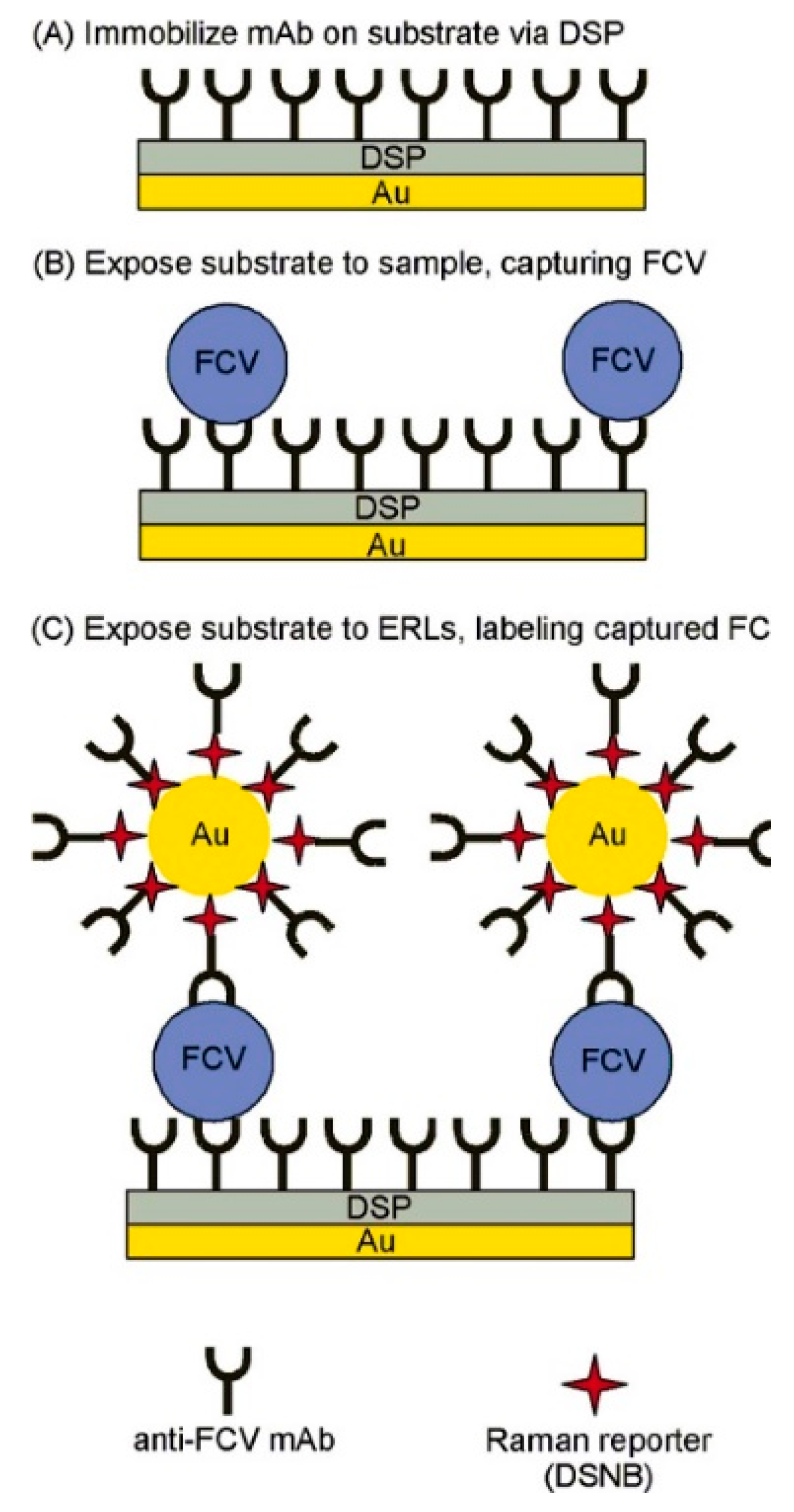
4.1.1. Surface Enhanced Raman Scattering (SERS)
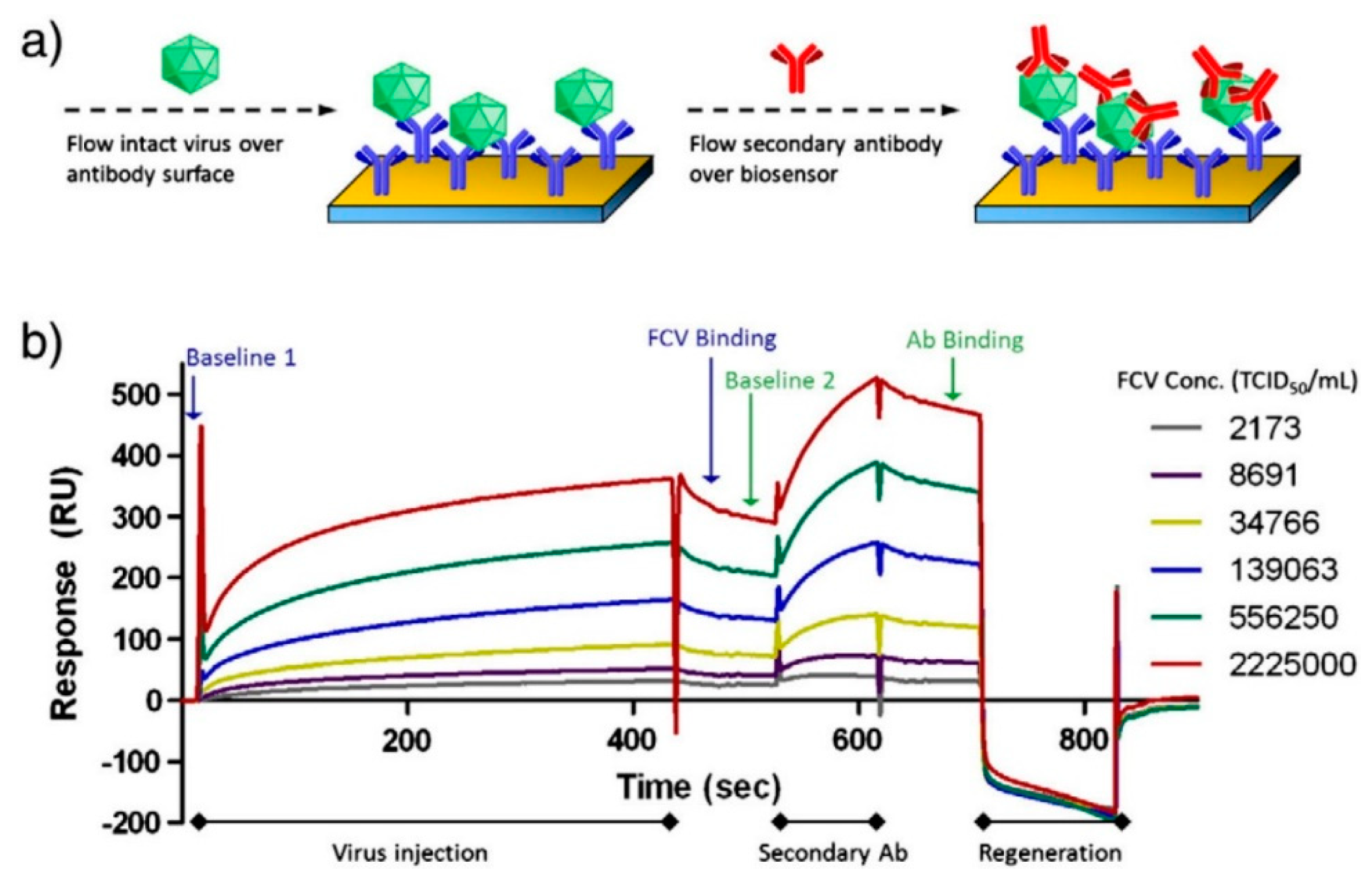
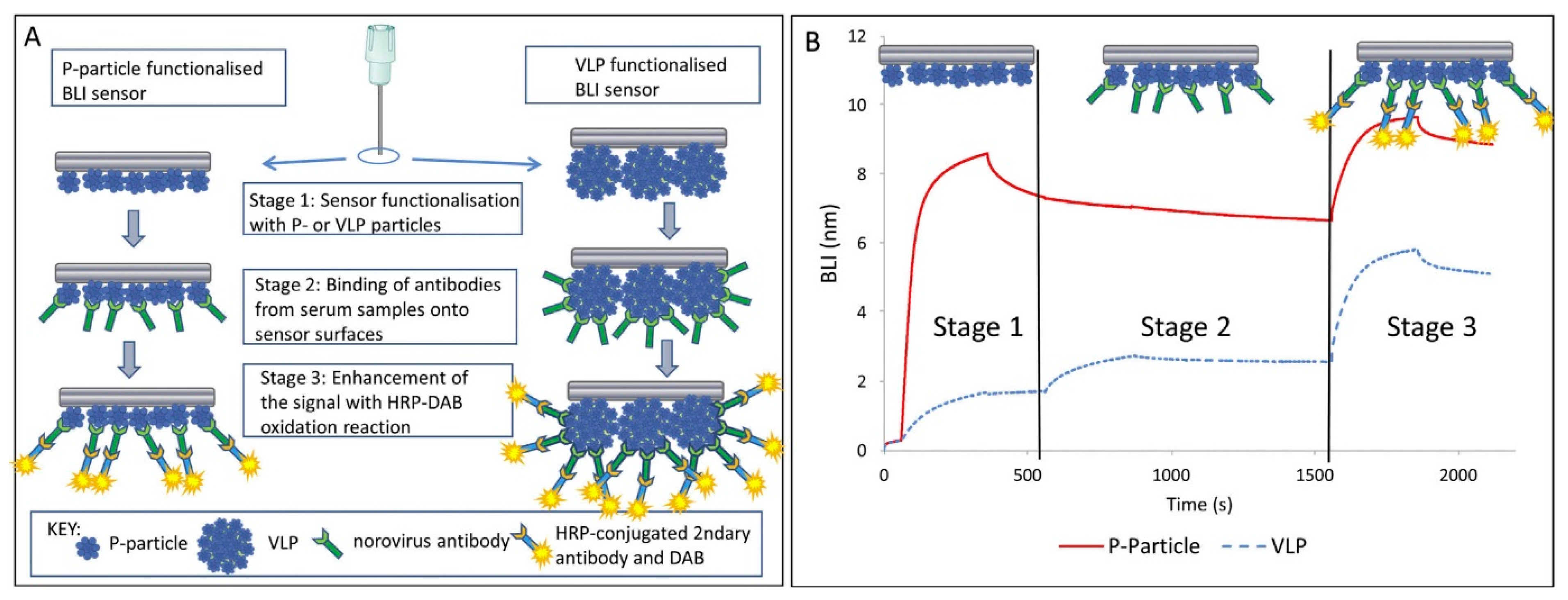
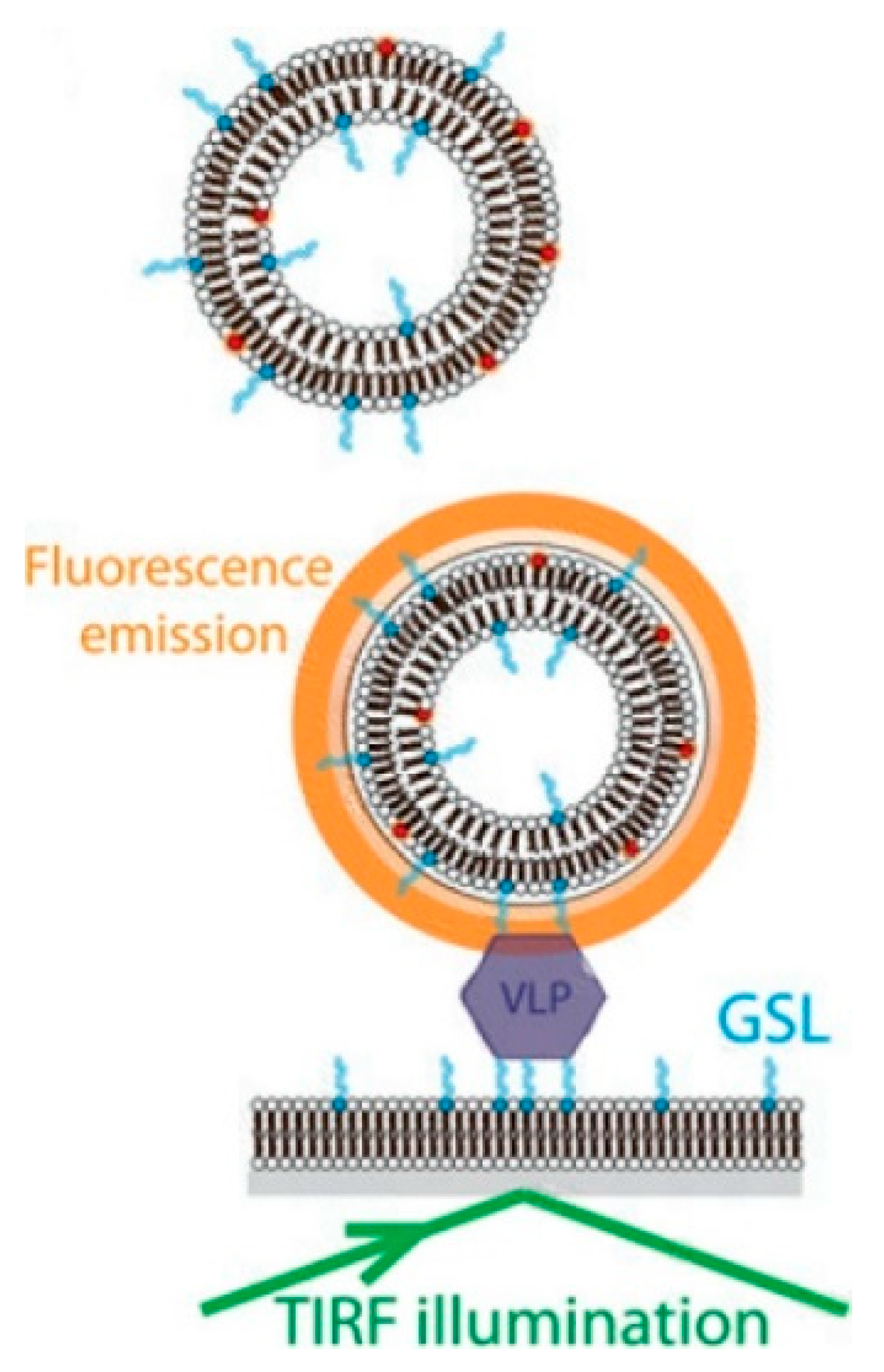
4.1.2. Surface Plasmon Resonance (SPR)
4.1.3. Other Optical Biosensor Methods
4.2. Electrochemical Biosensors
4.3. Piezoelectric Biosensors
5. Microarray
6. Omics-Based Approaches and Other Detection Methods
7. Future Perspective
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Hall, A.J. Noroviruses: The perfect human pathogens? J. Infect. Dis. 2012, 205, 1622–1624. [Google Scholar] [CrossRef] [PubMed]
- Scharff, R.L. Economic burden from health losses due to foodborne illness in the United States. J. Food Prot. 2012, 75, 123–131. [Google Scholar] [CrossRef] [PubMed]
- Rönnqvist, M.; Maunula, L. Noroviruses on surfaces: Detection, persistence, disinfection and role in environmental transmission. Future Virol. 2016, 11, 207–217. [Google Scholar] [CrossRef]
- Atmar, R.L. Noroviruses: State of the art. Food Environ. Virol. 2010, 2, 117–126. [Google Scholar] [CrossRef]
- Richards, G.P.; Watson, M.A.; Meade, G.K.; Hovan, G.L.; Kingsley, D.H. Resilience of norovirus GII. 4 to freezing and thawing: Implications for virus infectivity. Food Environ. Virol. 2012, 4, 192–197. [Google Scholar] [CrossRef]
- Lawley, R.; Curtis, L.; Davis, J. The Food Safety Hazard Guidebook, 2nd ed.; Royal Society of Chemistry: Cambridge, UK, 2012; pp. 148–149. [Google Scholar]
- Seitz, S.R.; Leon, J.S.; Schwab, K.J.; Lyon, G.M.; Dowd, M.; McDaniels, M.; Abdulhafid, G.; Fernandez, M.L.; Lindesmith, L.C.; Baric, R.S. Norovirus infectivity in humans and persistence in water. Appl. Environ. Microbiol. 2011, 77, 6884–6888. [Google Scholar] [CrossRef]
- D'Souza, D.H.; Sair, A.; Williams, K.; Papafragkou, E.; Jean, J.; Moore, C.; Jaykus, L. Persistence of caliciviruses on environmental surfaces and their transfer to food. Int. J. Food Microbiol. 2006, 108, 84–91. [Google Scholar] [CrossRef]
- Lamhoujeb, S.; Fliss, I.; Ngazoa, S.E.; Jean, J. Evaluation of the persistence of infectious human noroviruses on food surfaces by using real-time nucleic acid sequence-based amplification. Appl. Environ. Microbiol. 2008, 74, 3349–3355. [Google Scholar] [CrossRef]
- FAO/WHO (Food and Agriculture Organization of the United Nations/World Health Organization). Viruses in food: Scientific advice to support risk management activities. In Microbiological Risk Assessment Series No. 14; FAO/WHO: Rome, Italy, 2008; p. 151. [Google Scholar]
- Vinjé, J. Advances in laboratory methods for detection and typing of norovirus. J. Clin. Microbiol. 2015, 53, 373–381. [Google Scholar] [CrossRef]
- Moore, M.D.; Goulter, R.M.; Jaykus, L.-A. Human norovirus as a foodborne pathogen: Challenges and developments. Annu. Rev. Food Sci. Technol. 2015, 6, 411–433. [Google Scholar] [CrossRef]
- Zheng, D.P.; Ando, T.; Fankhauser, R.L.; Beard, R.S.; Glass, R.I.; Monroe, S.S. Norovirus classification and proposed strain nomenclature. Virology 2006, 346, 312–323. [Google Scholar] [CrossRef] [PubMed]
- Karst, S.M. Pathogenesis of noroviruses, emerging RNA viruses. Viruses 2010, 2, 748–781. [Google Scholar] [CrossRef] [PubMed]
- Debbink, K.; Lindesmith, L.C.; Baric, R.S. The state of norovirus vaccines. Clin. Infect. Dis. 2014, 58, 1746–1752. [Google Scholar] [CrossRef] [PubMed]
- Kou, B.; Crawford, S.E.; Ajami, N.J.; Czako, R.; Neill, F.H.; Tanaka, T.N.; Kitamoto, N.; Palzkill, T.G.; Estes, M.K.; Atmar, R.L. Characterization of cross-reactive norovirus-specific monoclonal antibodies. Clin. Vaccine Immunol. 2015, 22, 160–167. [Google Scholar] [CrossRef] [PubMed]
- Chames, P.; Van Regenmortel, M.; Weiss, E.; Baty, D. Therapeutic antibodies: Successes, limitations and hopes for the future. Br. J. Pharmacol. 2009, 157, 220–233. [Google Scholar] [CrossRef] [PubMed]
- Escudero-Abarca, B.I.; Suh, S.H.; Moore, M.D.; Dwivedi, H.P.; Jaykus, L.-A. Selection, characterization and application of nucleic acid aptamers for the capture and detection of human norovirus strains. PLoS ONE 2014, 9, e106805. [Google Scholar] [CrossRef]
- Lakhin, A.; Tarantul, V.; Gening, L. Aptamers: Problems, solutions and prospects. Acta Nat. 2013, 5, 34–43. [Google Scholar] [CrossRef]
- Marionneau, S.; Cailleau-Thomas, A.; Rocher, J.; Le Moullac-Vaidye, B.; Ruvoën, N.; Clément, M.; Le Pendu, J. ABH and Lewis histo-blood group antigens, a model for the meaning of oligosaccharide diversity in the face of a changing world. Biochimie 2001, 83, 565–573. [Google Scholar] [CrossRef]
- Tian, P.; Engelbrektson, A.; Mandrell, R. Two-log increase in sensitivity for detection of norovirus in complex samples by concentration with porcine gastric mucin conjugated to magnetic beads. Appl. Environ. Microbiol. 2008, 74, 4271–4276. [Google Scholar] [CrossRef]
- Kimoto-Nira, H.; Yamasaki, S.; Sasaki, K.; Moriya, N.; Takenaka, A.; Suzuki, C. New lactic acid bacterial strains from traditional Mongolian fermented milk products have altered adhesion to porcine gastric mucin depending on the carbon source. Anim. Sci. J. 2015, 86, 325–332. [Google Scholar] [CrossRef]
- Tan, M.; Jiang, X. Histo-blood group antigens: A common niche for norovirus and rotavirus. Expert Rev. Mol. Med. 2014, 16, e5. [Google Scholar] [CrossRef] [PubMed]
- Shirato, H. Norovirus and histo-blood group antigens. Jpn. J. Infect. Dis. 2011, 64, 95–103. [Google Scholar] [PubMed]
- Han, L.; Kitov, P.I.; Kitova, E.N.; Tan, M.; Wang, L.; Xia, M.; Jiang, X.; Klassen, J.S. Affinities of recombinant norovirus P dimers for human blood group antigens. Glycobiology 2013, 23, 276–285. [Google Scholar] [CrossRef] [PubMed]
- Tian, P.; Bates, A.H.; Jensen, H.M.; Mandrell, R. Norovirus binds to blood group A-like antigens in oyster gastrointestinal cells. Lett. Appl. Microbiol. 2006, 43, 645–651. [Google Scholar] [CrossRef]
- Harrington, P.R.; Vinjé, J.; Moe, C.L.; Baric, R.S. Norovirus capture with histo-blood group antigens reveals novel virus-ligand interactions. J. Virol. 2004, 78, 3035–3045. [Google Scholar] [CrossRef]
- Huang, P.; Farkas, T.; Zhong, W.; Tan, M.; Thornton, S.; Morrow, A.L.; Jiang, X. Norovirus and histo-blood group antigens: Demonstration of a wide spectrum of strain specificities and classification of two major binding groups among multiple binding patterns. J. Virol. 2005, 79, 6714–6722. [Google Scholar] [CrossRef]
- Tan, M.; Xia, M.; Chen, Y.; Bu, W.; Hegde, R.S.; Meller, J.; Li, X.; Jiang, X. Conservation of carbohydrate binding interfaces—Evidence of human HBGA selection in norovirus evolution. PLoS ONE 2009, 4, e5058. [Google Scholar] [CrossRef]
- Tan, M.; Jiang, X. Norovirus and its histo-blood group antigen receptors: An answer to a historical puzzle. Trends Microbiol. 2005, 13, 285–293. [Google Scholar] [CrossRef]
- Singh, B.K.; Leuthold, M.M.; Hansman, G.S. Human noroviruses’ fondness for histo-blood group antigens. J. Virol. 2015, 89, 2024–2040. [Google Scholar] [CrossRef]
- Jones, M.K.; Watanabe, M.; Zhu, S.; Graves, C.L.; Keyes, L.R.; Grau, K.R.; Gonzalez-Hernandez, M.B.; Iovine, N.M.; Wobus, C.E.; Vinjé, J.; et al. Enteric bacteria promote human and mouse norovirus infection of B cells. Science 2014, 346, 755–759. [Google Scholar] [CrossRef]
- Miura, T.; Sano, D.; Suenaga, A.; Yoshimura, T.; Fuzawa, M.; Nakagomi, T.; Nakagomi, O.; Okabe, S. Histo-blood group antigen-like substances of human enteric bacteria as specific adsorbents for human noroviruses. J. Virol. 2013, 87, 9441–9451. [Google Scholar] [CrossRef] [PubMed]
- Almand, E.A.; Moore, M.D.; Jaykus, L.-A. Characterization of human norovirus binding to gut-associated bacterial ligands. BMC Res. Notes 2019, 12, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Shirato, H.; Ogawa, S.; Ito, H.; Sato, T.; Kameyama, A.; Narimatsu, H.; Xiaofan, Z.; Miyamura, T.; Wakita, T.; Ishii, K. Noroviruses distinguish between type 1 and type 2 histo-blood group antigens for binding. J. Virol. 2008, 82, 10756–10767. [Google Scholar] [CrossRef]
- Abdulhalim, I.; Zourob, M.; Lakhtakia, A. Surface plasmon resonance for biosensing: A mini-review. Electromagnetics 2008, 28, 214–242. [Google Scholar] [CrossRef]
- Huang, P.; Xia, M.; Tan, M.; Zhong, W.; Wei, C.; Wang, L.; Morrow, A.; Jiang, X. Spike protein VP8* of human rotavirus recognizes histo-blood group antigens in a type-specific manner. J. Virol. 2012, 86, 4833–4843. [Google Scholar] [CrossRef] [PubMed]
- Nasir, W. Studies on Interactions of Norovirus Capsid Protein with Fucosylated Glycans and Galactosylceramide as Soluble and Membrane Bound Ligands. Ph.D. Thesis, University of Gothenburg, Gothenburg, Sweden, 2014. [Google Scholar]
- Rydell, G.E.; Dahlin, A.B.; Hook, F.; Larson, G. QCM-D studies of human norovirus VLPs binding to glycosphingolipids in supported lipid bilayers reveal strain-specific characteristics. Glycobiology 2009, 19, 1176–1184. [Google Scholar] [CrossRef]
- Nilsson, J.; Rydell, G.E.; Le Pendu, J.; Larson, G. Norwalk virus-like particles bind specifically to A, H and difucosylated Lewis but not to B histo-blood group active glycosphingolipids. Glycoconj. J. 2009, 26, 1171–1180. [Google Scholar] [CrossRef]
- Shang, J.; Piskarev, V.E.; Xia, M.; Huang, P.; Jiang, X.; Likhosherstov, L.M.; Novikova, O.S.; Newburg, D.S.; Ratner, D.M. Identifying human milk glycans that inhibit norovirus binding using surface plasmon resonance. Glycobiology 2013, 23, 1491–1498. [Google Scholar] [CrossRef]
- Rydell, G.E.; Nilsson, J.; Rodriguez-Diaz, J.; Ruvoën-Clouet, N.; Svensson, L.; Le Pendu, J.; Larson, G. Human noroviruses recognize sialyl Lewis x neoglycoprotein. Glycobiology 2009, 19, 309–320. [Google Scholar] [CrossRef]
- Celli, J.; Gregor, B.; Turner, B.; Afdhal, N.H.; Bansil, R.; Erramilli, S. Viscoelastic properties and dynamics of porcine gastric mucin. Biomacromolecules 2005, 6, 1329–1333. [Google Scholar] [CrossRef]
- Turner, B.S.; Bhaskar, K.R.; Hadzopoulou-Cladaras, M.; LaMont, J.T. Cysteine-rich regions of pig gastric mucin contain von Willebrand factor and cystine knot domains at the carboxyl terminal. Biochim. Biophys. Acta Gene Struct. Expr. 1999, 1447, 77–92. [Google Scholar] [CrossRef]
- Hong, Z.; Chasan, B.; Bansil, R.; Turner, B.S.; Bhaskar, K.R.; Afdhal, N.H. Atomic force microscopy reveals aggregation of gastric mucin at low pH. Biomacromolecules 2005, 6, 3458–3466. [Google Scholar] [CrossRef] [PubMed]
- Lindesmith, L.C.; Debbink, K.; Swanstrom, J.; Vinjé, J.; Costantini, V.; Baric, R.S.; Donaldson, E.F. Monoclonal antibody-based antigenic mapping of norovirus GII. 4-2002. J. Virol. 2012, 86, 873–883. [Google Scholar] [CrossRef] [PubMed]
- Tan, M.; Jiang, X. Norovirus gastroenteritis, carbohydrate receptors, and animal models. PLoS Pathog. 2010, 6, e1000983. [Google Scholar] [CrossRef]
- Tian, P.; Jiang, X.; Zhong, W.; Jensen, H.M.; Brandl, M.; Bates, A.H.; Engelbrektson, A.L.; Mandrell, R. Binding of recombinant norovirus like particle to histo-blood group antigen on cells in the lumen of pig duodenum. Res. Vet. Sci. 2007, 83, 410–418. [Google Scholar] [CrossRef] [PubMed]
- Tian, P.; Brandl, M.; Mandrell, R. Porcine gastric mucin binds to recombinant norovirus particles and competitively inhibits their binding to histo-blood group antigens and Caco-2 cells. Lett. Appl. Microbiol. 2005, 41, 315–320. [Google Scholar] [CrossRef]
- Tian, P.; Yang, D.; Jiang, X.; Zhong, W.; Cannon, J.; Burkhardt Iii, W.; Woods, J.; Hartman, G.; Lindesmith, L.; Baric, R.S. Specificity and kinetics of norovirus binding to magnetic bead-conjugated histo-blood group antigens. J. Appl. Microbiol. 2010, 109, 1753–1762. [Google Scholar] [CrossRef]
- Wang, Y.; Ye, Z.; Ying, Y. New trends in impedimetric biosensors for the detection of foodborne pathogenic bacteria. Sensors 2012, 12, 3449–3471. [Google Scholar] [CrossRef]
- Byrne, B.; Stack, E.; Gilmartin, N.; O’Kennedy, R. Antibody-based sensors: Principles, problems and potential for detection of pathogens and associated toxins. Sensors 2009, 9, 4407–4445. [Google Scholar] [CrossRef]
- Shiota, T.; Okame, M.; Takanashi, S.; Khamrin, P.; Takagi, M.; Satou, K.; Masuoka, Y.; Yagyu, F.; Shimizu, Y.; Kohno, H. Characterization of a broadly reactive monoclonal antibody against norovirus genogroups I and II: Recognition of a novel conformational epitope. J. Virol. 2007, 81, 12298–12306. [Google Scholar] [CrossRef]
- Kitamoto, N.; Tanaka, T.; Natori, K.; Takeda, N.; Nakata, S.; Jiang, X.; Estes, M.K. Cross-reactivity among several recombinant calicivirus virus-like particles (VLPs) with monoclonal antibodies obtained from mice immunized orally with one type of VLP. J. Clin. Microbiol. 2002, 40, 2459–2465. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Crawford, S.E.; Ajami, N.; Parker, T.D.; Kitamoto, N.; Natori, K.; Takeda, N.; Tanaka, T.; Kou, B.; Atmar, R.L.; Estes, M.K. Mapping broadly reactive Norovirus genogroup I and II monoclonal antibodies. Clin. Vaccine Immunol. 2015, 22, 168–177. [Google Scholar] [CrossRef] [PubMed]
- Kou, B.; Huang, W.; Neill, F.H.; Palzkill, T.; Estes, M.K.; Atmar, R.L. Norovirus Antigen Detection with a Combination of Monoclonal and Single-Chain Antibodies. J. Clin. Microbiol. 2015, 53, 3916–3918. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Hurwitz, A.M.; Huang, W.; Kou, B.; Estes, M.K.; Atmar, R.L.; Palzkill, T. Identification and Characterization of Single-Chain Antibodies that Specifically Bind GI Noroviruses. PLoS ONE 2017, 12, e0170162. [Google Scholar] [CrossRef]
- Zheng, L.; Wang, W.; Liu, J.; Chen, X.; Li, S.; Wang, Q.; Huo, Y.; Qin, C.; Shen, S.; Wang, M. Characterization of a Norovirus-specific monoclonal antibody that exhibits wide spectrum binding activities. J. Med. Virol. 2018, 90, 671–676. [Google Scholar] [CrossRef]
- Cortez-Retamozo, V.; Backmann, N.; Senter, P.D.; Wernery, U.; De Baetselier, P.; Muyldermans, S.; Revets, H. Efficient cancer therapy with a nanobody-based conjugate. Cancer Res. 2004, 64, 2853–2857. [Google Scholar] [CrossRef]
- Doerflinger, S.Y.; Tabatabai, J.; Schnitzler, P.; Farah, C.; Rameil, S.; Sander, P.; Koromyslova, A.; Hansman, G.S. Development of a Nanobody-Based Lateral Flow Immunoassay for Detection of Human Norovirus. mSphere 2016, 1, e00216–e00219. [Google Scholar] [CrossRef]
- Koromyslova, A.D.; Hansman, G.S. Nanobodies targeting norovirus capsid reveal functional epitopes and potential mechanisms of neutralization. PLoS Pathog. 2017, 13, e1006636. [Google Scholar] [CrossRef]
- Koromyslova, A.D.; Hansman, G.S. Nanobody binding to a conserved epitope promotes norovirus particle disassembly. J. Virol. 2015, 89, 2718–2730. [Google Scholar] [CrossRef]
- Ma, D.; Shen, L.; Wu, K.; Diehnelt, C.W.; Green, A.A. Low-cost detection of norovirus using paper-based cell-free systems and synbody-based viral enrichment. Synth. Biol. 2018, 3, ysy018. [Google Scholar] [CrossRef]
- Gupta, N.; Lainson, J.C.; Belcher, P.E.; Shen, L.; Mason, H.S.; Johnston, S.A.; Diehnelt, C.W. Cross-reactive synbody affinity ligands for capturing diverse noroviruses. Anal. Chem. 2017, 89, 7174–7181. [Google Scholar] [CrossRef] [PubMed]
- Wang, P.; Yang, Y.; Hong, H.; Zhang, Y.; Cai, W.; Fang, D. Aptamers as therapeutics in cardiovascular diseases. Curr. Med. Chem. 2011, 18, 4169–4174. [Google Scholar] [CrossRef] [PubMed]
- Darmostuk, M.; Rimpelova, S.; Gbelcova, H.; Ruml, T. Current approaches in SELEX: An update to aptamer selection technology. Biotechnol. Adv. 2015, 33, 1141–1161. [Google Scholar] [CrossRef] [PubMed]
- Giamberardino, A.; Labib, M.; Hassan, E.M.; Tetro, J.A.; Springthorpe, S.; Sattar, S.A.; Berezovski, M.V.; DeRosa, M.C. Ultrasensitive norovirus detection using DNA aptasensor technology. PLoS ONE 2013, 8, e79087. [Google Scholar] [CrossRef]
- Kitajima, M.; Wang, N.; Tay, M.Q.; Miao, J.; Whittle, A.J. Development of a MEMS-based electrochemical aptasensor for norovirus detection. Micro Nano Lett. 2016, 11, 582–585. [Google Scholar] [CrossRef]
- Weerathunge, P.; Ramanathan, R.; Torok, V.A.; Hodgson, K.; Xu, Y.; Goodacre, R.; Behera, B.K.; Bansal, V. Ultrasensitive colorimetric detection of murine norovirus using NanoZyme aptasensor. Anal. Chem. 2019, 91, 3270–3276. [Google Scholar] [CrossRef]
- Weng, X.; Neethirajan, S. Aptamer-based fluorometric determination of norovirus using a paper-based microfluidic device. Microchim. Acta 2017, 184, 4545–4552. [Google Scholar] [CrossRef]
- Moore, M.D.; Escudero-Abarca, B.I.; Suh, S.H.; Jaykus, L.-A. Generation and characterization of nucleic acid aptamers targeting the capsid P domain of a human norovirus GII. 4 strain. J. Biotechnol. 2015, 209, 41–49. [Google Scholar] [CrossRef]
- Schilling, K.B.; DeGrasse, J.; Woods, J.W. The influence of food matrices on aptamer selection by SELEX (systematic evolution of ligands by exponential enrichment) targeting the norovirus P-Domain. Food Chem. 2018, 258, 129–136. [Google Scholar] [CrossRef]
- Adler, J.L.; Zickl, R. Winter vomiting disease. J. Infect. Dis. 1969, 119, 668–673. [Google Scholar] [CrossRef]
- Kapikian, A.Z.; Wyatt, R.G.; Dolin, R.; Thornhill, T.S.; Kalica, A.R.; Chanock, R.M. Visualization by immune electron microscopy of a 27-nm particle associated with acute infectious nonbacterial gastroenteritis. J. Virol. 1972, 10, 1075–1081. [Google Scholar] [CrossRef] [PubMed]
- Glass, R.I.; Noel, J.; Ando, T.; Fankhauser, R.; Belliot, G.; Mounts, A.; Parashar, U.D.; Bresee, J.S.; Monroe, S.S. The epidemiology of enteric caliciviruses from humans: A reassessment using new diagnostics. J. Infect. Dis. 2000, 181, S254–S261. [Google Scholar] [CrossRef] [PubMed]
- ITO, M.; TAGAYA, I. Immune adherence hemagglutination test as a new sensitive method for titration of animal virus antigens and antibodies. Jpn. J. Med Sci. Biol. 1966, 19, 109–126. [Google Scholar] [CrossRef] [PubMed]
- Kapikian, A.Z.; Greenberg, H.B.; Cline, W.L.; Kalica, A.R.; Wyatt, R.G.; James, H.D.; Lloyd, N.L.; Chanock, R.M.; Ryder, R.W.; Kim, H.W. Prevalence of antibody to the Norwalk agent by a newly developed immune adherence hemagglutination assay. J. Med. Virol. 1978, 2, 281–294. [Google Scholar] [CrossRef]
- Lamhoujeb, S. Human Noroviruses: Characterization, Detection, and Evaluation of Their Persistence in Foods and on Food-contact Surfaces. Ph.D. Thesis, Université Laval, Québec, Canada, 2008. [Google Scholar]
- Atmar, R.L.; Estes, M.K. Diagnosis of noncultivatable gastroenteritis viruses, the human caliciviruses. Clin. Microbiol. Rev. 2001, 14, 15–37. [Google Scholar] [CrossRef]
- Atmar, R.L.; Englund, J.A. Laboratory methods for the diagnosis of viral diseases. In Viral Infections of Humans: Epidemiology and Control, 4th ed.; Atmar, R.L., Kaslow, R.A., Eds.; Plenum Publishing Corporation: New York, NY, USA, 1997; pp. 59–82. [Google Scholar]
- Greenberg, H.B.; Wyatt, R.G.; Valdesuso, J.; Kalica, A.R.; London, W.T.; Chanock, R.M.; Kapikian, A.Z. Solid-phase microtiter radioimmunoassay for detection of the Norwalk strain of acute nonbacterial, epidemic gastroenteritis virus and its antibodies. J. Med. Virol. 1978, 2, 97–108. [Google Scholar] [CrossRef]
- O’Farrell, B. Evolution in lateral flow–Based immunoassay systems. In Lateral Flow Immunoassay; Wong, R., Tse, H., Eds.; Humana Press: New York, NY, USA, 2009; pp. 1–33. [Google Scholar]
- Rackoff, L.A.; Bok, K.; Green, K.Y.; Kapikian, A.Z. Epidemiology and evolution of rotaviruses and noroviruses from an archival WHO Global Study in Children (1976–79) with implications for vaccine design. PLoS ONE 2013, 8, e59394. [Google Scholar] [CrossRef]
- Jiang, X.; Wang, M.; Graham, D.Y.; Estes, M.K. Expression, self-assembly, and antigenicity of the Norwalk virus capsid protein. J. Virol. 1992, 66, 6527–6532. [Google Scholar] [CrossRef]
- Okhuysen, P.C.; Jiang, X.; Ye, L.; Johnson, P.C.; Estes, M.K. Viral shedding and fecal IgA response after Norwalk virus infection. J. Infect. Dis. 1995, 171, 566–569. [Google Scholar] [CrossRef]
- Robilotti, E.; Deresinski, S.; Pinsky, B.A. Norovirus. Clin. Microbiol. Rev. 2015, 28, 134–164. [Google Scholar] [CrossRef]
- Kirby, A.; Gurgel, R.Q.; Dove, W.; Vieira, S.C.F.; Cunliffe, N.A.; Cuevas, L.E. An evaluation of the RIDASCREEN and IDEIA enzyme immunoassays and the RIDAQUICK immunochromatographic test for the detection of norovirus in faecal specimens. J. Clin. Virol. 2010, 49, 254–257. [Google Scholar] [CrossRef] [PubMed]
- Morillo, S.G.; Luchs, A.; Cilli, A.; Ribeiro, C.D.; Calux, S.J.; Carmona, R.C.C.; Timenetsky, M.C.S.T. Norovirus 3rd generation kit: An improvement for rapid diagnosis of sporadic gastroenteritis cases and valuable for outbreak detection. J. Virol. Methods 2011, 173, 13–16. [Google Scholar] [CrossRef] [PubMed]
- Sakamaki, N.; Ohiro, Y.; Ito, M.; Makinodan, M.; Ohta, T.; Suzuki, W.; Takayasu, S.; Tsuge, H. Bioluminescent enzyme immunoassay for the detection of norovirus capsid antigen. Clin. Vaccine Immunol. 2012, 19, 1949–1954. [Google Scholar] [CrossRef] [PubMed]
- Shigemoto, N.; Tanizawa, Y.; Matsuo, T.; Sakamaki, N.; Ohiro, Y.; Takayasu, S.; Fukuda, S. Clinical evaluation of a bioluminescent enzyme immunoassay for detecting norovirus in fecal specimens from patients with acute gastroenteritis. J. Med. Virol. 2014, 86, 1219–1225. [Google Scholar] [CrossRef]
- Suzuki, W.; Ohiro, Y.; Tsukagoshi, H.; Kimura, H. Evaluation of Norovirus Detection Method Based on a Newly Developed Bioluminescent Enzyme Immunoassay (BLEIA) System. Kansenshogaku Zasshi J. Jpn. Assoc. Infect. Dis. 2015, 89, 230–236. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ambert-Balay, K.; Pothier, P. Evaluation of 4 immunochromatographic tests for rapid detection of norovirus in faecal samples. J. Clin. Virol. 2013, 56, 278–282. [Google Scholar] [CrossRef]
- Hagström, A.E.; Garvey, G.; Paterson, A.S.; Dhamane, S.; Adhikari, M.; Estes, M.K.; Strych, U.; Kourentzi, K.; Atmar, R.L.; Willson, R.C. Sensitive detection of norovirus using phage nanoparticle reporters in lateral-flow assay. PLoS ONE 2015, 10, e0126571. [Google Scholar] [CrossRef]
- Cichocki, M. HIV prevention and testing. In Living with HIV: A Patient’s Guide, 2nd ed.; Cichocki, M., Ed.; McFarland & Company Inc.: Jefferson, NC, USA, 2017. [Google Scholar]
- Tamminen, K.; Huhti, L.; Koho, T.; Lappalainen, S.; Hytönen, V.P.; Vesikari, T.; Blazevic, V. A comparison of immunogenicity of norovirus GII-4 virus-like particles and P-particles. Immunology 2012, 135, 89–99. [Google Scholar] [CrossRef]
- Hayashi, Y.; Ando, T.; Utagawa, E.; Sekine, S.; Okada, S.; Yabuuchi, K.; Miki, T.; Ohashi, M. Western blot (immunoblot) assay of small, round-structured virus associated with an acute gastroenteritis outbreak in Tokyo. J. Clin. Microbiol. 1989, 27, 1728–1733. [Google Scholar] [CrossRef]
- Jiang, X.; Graham, D.Y.; Wang, K.; Estes, M.K. Norwalk virus genome cloning and characterization. Science 1990, 250, 1580–1583. [Google Scholar]
- Anonymous. Microbiology of Food and Animal Feed—Horizontal Method for Determination of Hepatitis A Virus and Norovirus in Food Using Real-Time RT-PCR—Part 1: Method for Quantification; ISO/TS 15216-1:2017; International Organization for Standardization (ISO): Geneva, Switzerland, 2017. [Google Scholar]
- Anonymous. Microbiology of the Food Chain—Horizontal Method for Determination of Hepatitis A Virus and Norovirus Using Real-Time RT-PCR—Part 2: Method for Detection; ISO 15216-2:2019; International Organization for Standardization (ISO): Geneva, Switzerland, 2019. [Google Scholar]
- Alexander, T.A. Development of methodology based on commercialized SERS-active substrates for rapid discrimination of Poxviridae virions. Anal. Chem. 2008, 80, 2817–2825. [Google Scholar] [CrossRef] [PubMed]
- Farkas, T.; Singh, A.; Le Guyader, F.S.; La Rosa, G.; Saif, L.; McNeal, M. Multiplex real-time RT-PCR for the simultaneous detection and quantification of GI, GII and GIV noroviruses. J. Virol. Methods 2015, 223, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Stals, A.; Baert, L.; Botteldoorn, N.; Werbrouck, H.; Herman, L.; Uyttendaele, M.; Van Coillie, E. Multiplex real-time RT-PCR for simultaneous detection of GI/GII noroviruses and murine norovirus 1. J. Virol. Methods 2009, 161, 247–253. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Fang, L.; Shi, X.; Zhang, H.; Li, Y.; Lin, Y.; Qiu, Y.; Chen, Q.; Li, H.; Zhou, L. Simultaneous detection of five enteric viruses associated with gastroenteritis by use of a PCR assay: A single real-time multiplex reaction and its clinical application. J. Clin. Microbiol. 2014, 52, 1266–1268. [Google Scholar] [CrossRef]
- Claas, E.C.; Mazzulli, T.; Topin, F. Performance of the xTAGR Gastrointestinal Pathogen Panel, a Multiplex Molecular Assay for Simultaneous Detection of Bacterial, Viral, and Parasitic Causes of Infectious Gastroenteritis. J. Microbiol. Biotechnol. 2013, 23, 1041–1045. [Google Scholar] [CrossRef]
- Pang, X. Detection and laboratory diagnosis of noroviruses. In The Norovirus: Features, Detection, and Prevention of Foodborne Disease; Chan, P.K.S., Kwan, H.S., Chan, M.C.W., Eds.; Academic Press: Cambridge, MA, USA, 2017; pp. 109–129. [Google Scholar]
- Moore, C.; Clark, E.; Gallimore, C.; Corden, S.; Gray, J.; Westmoreland, D. Evaluation of a broadly reactive nucleic acid sequence based amplification assay for the detection of noroviruses in faecal material. J. Clin. Virol. 2004, 29, 290–296. [Google Scholar] [CrossRef]
- Fukuda, S.; Sasaki, Y.; Kuwayama, M.; Miyazaki, K. Simultaneous Detection and Genogroup-Screening Test for Norovirus Genogroups I and II from Fecal Specimens in Single Tube by Reverse Transcription-Loop-Mediated Isothermal Amplification Assay. Microbiol. Immunol. 2007, 51, 547–550. [Google Scholar] [CrossRef]
- Moore, M.D.; Jaykus, L.-A. Development of a recombinase polymerase amplification assay for detection of epidemic human noroviruses. Sci. Rep. 2017, 7, 40244. [Google Scholar] [CrossRef]
- Jeon, S.B.; Seo, D.J.; Oh, H.; Kingsley, D.H.; Choi, C. Development of one-step reverse transcription loop-mediated isothermal amplification for norovirus detection in oysters. Food Control 2017, 73, 1002–1009. [Google Scholar] [CrossRef]
- Luo, J.; Xu, Z.; Nie, K.; Ding, X.; Guan, L.; Wang, J.; Xian, Y.; Wu, X.; Ma, X. Visual detection of norovirus genogroup ii by reverse transcription loop-mediated isothermal amplification with hydroxynaphthol blue dye. Food Environ. Virol. 2014, 6, 196–201. [Google Scholar] [CrossRef]
- Manuel, C.S.; Moore, M.D.; Jaykus, L.-A. Predicting human norovirus infectivity-Recent advances and continued challenges. Food Microbiol. 2018, 76, 337–345. [Google Scholar] [CrossRef] [PubMed]
- Knight, A.; Li, D.; Uyttendaele, M.; Jaykus, L.-A. A critical review of methods for detecting human noroviruses and predicting their infectivity. Crit. Rev. Microbiol. 2013, 39, 295–309. [Google Scholar] [CrossRef] [PubMed]
- Kostela, J.; Ayers, M.; Nishikawa, J.; McIntyre, L.; Petric, M.; Tellier, R. Amplification by long RT-PCR of near full-length norovirus genomes. J. Virol. Methods 2008, 149, 226–230. [Google Scholar] [CrossRef] [PubMed]
- Seo, K.; Lee, J.E.; Lim, M.Y.; Ko, G. Effect of temperature, pH, and NaCl on the inactivation kinetics of murine norovirus. J. Food Prot. 2012, 75, 533–540. [Google Scholar] [CrossRef]
- Sánchez, G.; Elizaquível, P.; Aznar, R. Discrimination of infectious hepatitis A viruses by propidium monoazide real-time RT-PCR. Food Environ. Virol. 2012, 4, 21–25. [Google Scholar] [CrossRef]
- Kim, S.; Ko, G. Using propidium monoazide to distinguish between viable and nonviable bacteria, MS2 and murine norovirus. Lett. Appl. Microbiol. 2012, 55, 182–188. [Google Scholar] [CrossRef]
- Randazzo, W.; López-Gálvez, F.; Allende, A.; Aznar, R.; Sánchez, G. Evaluation of viability PCR performance for assessing norovirus infectivity in fresh-cut vegetables and irrigation water. Int. J. Food Microbiol. 2016, 229, 1–6. [Google Scholar] [CrossRef]
- Aboubakr, H.A.; Parra, F.S.; Collins, J.; Bruggeman, P.; Goyal, S.M. Ìn situ inactivation of human norovirus GII. 4 by cold plasma: Ethidium monoazide (EMA)-coupled RT-qPCR underestimates virus reduction and fecal material suppresses inactivation. Food Microbiol. 2020, 85, 103307. [Google Scholar] [CrossRef]
- Moore, M.D.; Bobay, B.G.; Mertens, B.; Jaykus, L.-A. Human norovirus aptamer exhibits high degree of target conformation-dependent binding similar to that of receptors and discriminates particle functionality. Msphere 2016, 1, e00216–e00298. [Google Scholar] [CrossRef]
- Nuanualsuwan, S.; Cliver, D.O. Pretreatment to avoid positive RT-PCR results with inactivated viruses. J. Virol. Methods 2002, 104, 217–225. [Google Scholar] [CrossRef]
- Yang, Y.; Griffiths, M.W. Enzyme treatment reverse transcription-PCR to differentiate infectious and inactivated F-specific RNA phages. Appl. Environ. Microbiol. 2014, 80, 3334–3340. [Google Scholar] [CrossRef]
- Cannon, J.L.; Vinjé, J. Histo-blood group antigen assay for detecting noroviruses in water. Appl. Environ. Microbiol. 2008, 74, 6818–6819. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dancho, B.A.; Chen, H.; Kingsley, D.H. Discrimination between infectious and non-infectious human norovirus using porcine gastric mucin. Int. J. Food Microbiol. 2012, 155, 222–226. [Google Scholar] [CrossRef] [PubMed]
- Afolayan, O.T.; Webb, C.C.; Cannon, J.L. Evaluation of a Porcine Gastric Mucin and RNase A Assay for the Discrimination of Infectious and Non-infectious GI. 1 and GII. 4 Norovirus Following Thermal, Ethanol, or Levulinic Acid Plus Sodium Dodecyl Sulfate Treatments. Food Environ. Virol. 2016, 8, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Chen, H. Evaluation of the porcine gastric mucin binding assay for high-pressure-inactivation studies using murine norovirus and tulane virus. Appl. Environ. Microbiol. 2015, 81, 515–521. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Cho, Y.-H.; Jee, Y.; Ko, G. Immunomagnetic separation combined with real-time reverse transcriptase PCR assays for detection of norovirus in contaminated food. Appl. Environ. Microbiol. 2008, 74, 4226–4230. [Google Scholar] [CrossRef] [PubMed]
- Tung, G.; Macinga, D.; Arbogast, J.; Jaykus, L.A. Efficacy of commonly used disinfectants for inactivation of human noroviruses and its surrogates. J. Food Prot. 2010, 76, 1210–1217. [Google Scholar] [CrossRef]
- Saylan, Y.; Erdem, Ö.; Ünal, S.; Denizli, A. An alternative medical diagnosis method: Biosensors for virus detection. Biosensors 2019, 9, 65. [Google Scholar] [CrossRef]
- Driskell, J.D.; Kwarta, K.M.; Lipert, R.J.; Porter, M.D.; Neill, J.D.; Ridpath, J.F. Low-level detection of viral pathogens by a surface-enhanced Raman scattering based immunoassay. Anal. Chem. 2005, 77, 6147–6154. [Google Scholar] [CrossRef]
- Fan, C.; Hu, Z.; Riley, L.K.; Purdy, G.A.; Mustapha, A.; Lin, M. Detecting Food-and Waterborne Viruses by Surface-Enhanced Raman Spectroscopy. J. Food Sci. 2010, 75, M302–M307. [Google Scholar] [CrossRef]
- Zhang, Z.; Li, S.; Tian, Z.; Li, J.; Chuanxian, W. Immunochromatographic detection method of norovirus Raman microprobe labeling. CN105759028A, 13 July 2016. [Google Scholar]
- Takemura, K.; Adegoke, O.; Takahashi, N.; Kato, T.; Li, T.-C.; Kitamoto, N.; Tanaka, T.; Suzuki, T.; Park, E.Y. Versatility of a localized surface plasmon resonance-based gold nanoparticle-alloyed quantum dot nanobiosensor for immunofluorescence detection of viruses. Biosens. Bioelectron. 2017, 89, 998–1005. [Google Scholar] [CrossRef] [PubMed]
- Nasrin, F.; Chowdhury, A.D.; Takemura, K.; Lee, J.; Adegoke, O.; Deo, V.K.; Abe, F.; Suzuki, T.; Park, E.Y. Single-step detection of norovirus tuning localized surface plasmon resonance-induced optical signal between gold nanoparticles and quantum dots. Biosens. Bioelectron. 2018, 122, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Heo, N.S.; Oh, S.Y.; Ryu, M.Y.; Baek, S.H.; Park, T.J.; Choi, C.; Huh, Y.S.; Park, J.P. Affinity peptide-guided plasmonic biosensor for detection of noroviral protein and human norovirus. Biosens. Bioelectron. Eng. 2019, 24, 318–325. [Google Scholar] [CrossRef]
- Takemura, K.; Lee, J.; Suzuki, T.; Hara, T.; Abe, F.; Park, E.Y. Ultrasensitive detection of norovirus using a magnetofluoroimmunoassay based on synergic properties of gold/magnetic nanoparticle hybrid nanocomposites and quantum dots. Sens. Actuators B Chem. 2019, 296, 126672. [Google Scholar] [CrossRef]
- Yakes, B.J.; Papafragkou, E.; Conrad, S.M.; Neill, J.D.; Ridpath, J.F.; Burkhardt, W., 3rd; Kulka, M.; Degrasse, S.L. Surface plasmon resonance biosensor for detection of feline calicivirus, a surrogate for norovirus. Int. J. Food Microbiol. 2013, 162, 152–158. [Google Scholar] [CrossRef]
- Kim, D.; Lee, H.-M.; Oh, K.-S.; Ki, A.Y.; Protzman, R.A.; Kim, D.; Choi, J.-S.; Kim, M.J.; Kim, S.H.; Vaidya, B. Exploration of the metal coordination region of concanavalin A for its interaction with human norovirus. Biomaterials 2017, 128, 33–43. [Google Scholar] [CrossRef]
- Ashiba, H.; Sugiyama, Y.; Wang, X.; Shirato, H.; Higo-Moriguchi, K.; Taniguchi, K.; Ohki, Y.; Fujimaki, M. Detection of norovirus virus-like particles using a surface plasmon resonance-assisted fluoroimmunosensor optimized for quantum dot fluorescent labels. Biosens. Bioelectron. 2017, 93, 260–266. [Google Scholar] [CrossRef]
- Han, Z.; Chen, L.; Weng, Q.; Zhou, Y.; Wang, L.; Li, C.; Chen, J. Silica-coated gold nanorod@ CdSeTe ternary quantum dots core/shell structure for fluorescence detection and dual-modal imaging. Sens. Actuators B Chem. 2018, 258, 508–516. [Google Scholar] [CrossRef]
- Bally, M.; Graule, M.; Parra, F.; Larson, G.; Höök, F. A virus biosensor with single virus-particle sensitivity based on fluorescent vesicle labels and equilibrium fluctuation analysis. Biointerphases 2013, 8, 4. [Google Scholar] [CrossRef]
- Connelly, J.T.; Kondapalli, S.; Skoupi, M.; Parker, J.S.; Kirby, B.J.; Baeumner, A.J. Micro-total analysis system for virus detection: Microfluidic pre-concentration coupled to liposome-based detection. Anal. Bioanal. Chem. 2012, 402, 315–323. [Google Scholar] [CrossRef]
- Zhao, Z.; Zhang, J.; Xu, M.-L.; Liu, Z.-P.; Wang, H.; Liu, M.; Yu, Y.-Y.; Sun, L.; Zhang, H.; Wu, H.-Y. A rapidly new-typed detection of norovirus based on F0F1-ATPase molecular motor biosensor. Biotechnol. Bioprocess Eng. 2016, 21, 128–133. [Google Scholar] [CrossRef]
- Kim, B.; Chung, K.W.; Lee, J.H. Non-stop aptasensor capable of rapidly monitoring norovirus in a sample. J. Pharm. Biomed. Anal. 2018, 152, 315–321. [Google Scholar] [CrossRef]
- Auer, S.; Azizi, L.; Faschinger, F.; Blazevic, V.; Vesikari, T.; Gruber, H.J.; Hytönen, V.P. Stable immobilisation of His-tagged proteins on BLI biosensor surface using cobalt. Sens. Actuators B Chem. 2017, 243, 104–113. [Google Scholar] [CrossRef]
- Auer, S.; Koho, T.; Uusi-Kerttula, H.; Vesikari, T.; Blazevic, V.; Hytönen, V.P. Rapid and sensitive detection of norovirus antibodies in human serum with a biolayer interferometry biosensor. Sens. Actuators B Chem. 2015, 221, 507–514. [Google Scholar] [CrossRef]
- Dong, X.; Broglie, J.; Tang, Y.; Yang, L. Evaluation of Bio-Layer Interferometric Biosensors for Label-Free Rapid Detection of Norovirus Using Virus like Particles. J. Anal. Bioanal. Tech. 2016, 7, 2. [Google Scholar] [CrossRef]
- Chakkarapani, S.K.; Sun, Y.; Kang, S.H. Ultrasensitive norovirus nanoimmunosensor based on concurrent axial super-localization of ellipsoidal point spread function by 3D light sheet microscopy. Sens. Actuators B Chem. 2019, 284, 81–90. [Google Scholar] [CrossRef]
- Adegoke, O.; Seo, M.-W.; Kato, T.; Kawahito, S.; Park, E.Y. An ultrasensitive SiO2-encapsulated alloyed CdZnSeS quantum dot-molecular beacon nanobiosensor for norovirus. Biosens. Bioelectron. 2016, 86, 135–142. [Google Scholar] [CrossRef]
- Yasuura, M.; Fujimaki, M. Detection of extremely low concentrations of biological substances using near-field illumination. Sci. Rep. 2016, 6, 1–7. [Google Scholar] [CrossRef]
- Kim, J.H.; Park, J.E.; Lin, M.; Kim, S.; Kim, G.H.; Park, S.; Ko, G.; Nam, J.M. Sensitive, Quantitative Naked-Eye Biodetection with Polyhedral Cu Nanoshells. Adv. Mater. 2017, 29, 1702945. [Google Scholar] [CrossRef]
- Khoris, I.M.; Takemura, K.; Lee, J.; Hara, T.; Abe, F.; Suzuki, T.; Park, E.Y. Enhanced colorimetric detection of norovirus using in-situ growth of Ag shell on Au NPs. Biosens. Bioelectron. 2019, 126, 425–432. [Google Scholar] [CrossRef]
- Chand, R.; Neethirajan, S. Microfluidic platform integrated with graphene-gold nano-composite aptasensor for one-step detection of norovirus. Biosens. Bioelectron. 2017, 98, 47–53. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Morita, M.; Takemura, K.; Park, E.Y. A multi-functional gold/iron-oxide nanoparticle-CNT hybrid nanomaterial as virus DNA sensing platform. Biosens. Bioelectron. 2018, 102, 425–431. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.; Takemura, K.; Kato, C.N.; Suzuki, T.; Park, E.Y. Binary nanoparticle graphene hybrid structure-based highly sensitive biosensing platform for norovirus-like particle detection. ACS Appl. Mater. Interfaces 2017, 9, 27298–27304. [Google Scholar] [CrossRef] [PubMed]
- Hwang, H.J.; Ryu, M.Y.; Park, C.Y.; Ahn, J.; Park, H.G.; Choi, C.; Ha, S.-D.; Park, T.J.; Park, J.P. High sensitive and selective electrochemical biosensor: Label-free detection of human norovirus using affinity peptide as molecular binder. Biosens. Bioelectron. 2017, 87, 164–170. [Google Scholar] [CrossRef] [PubMed]
- Nakano, M.; Hisajima, T.; Mao, L.; Suehiro, J. Electrical detection of norovirus capsid using dielectrophoretic impedance measurement method. In Proceedings of the Sensors, Taipei, Taiwan, 28–31 October 2012; pp. 1–4. [Google Scholar]
- Hong, S.A.; Kwon, J.; Kim, D.; Yang, S. A rapid, sensitive and selective electrochemical biosensor with concanavalin A for the preemptive detection of norovirus. Biosens. Bioelectron. 2015, 64, 338–344. [Google Scholar] [CrossRef] [PubMed]
- Baek, S.H.; Kim, M.W.; Park, C.Y.; Choi, C.-S.; Kailasa, S.K.; Park, J.P.; Park, T.J. Development of a rapid and sensitive electrochemical biosensor for detection of human norovirus via novel specific binding peptides. Biosens. Bioelectron. 2019, 123, 223–229. [Google Scholar] [CrossRef]
- Xiang, L.; Wang, Z.; Liu, Z.; Weigum, S.E.; Yu, Q.; Chen, M.Y. Inkjet-printed flexible biosensor based on graphene field effect transistor. IEEE Sens. J. 2016, 16, 8359–8364. [Google Scholar] [CrossRef]
- Han, Z.; Weng, Q.; Lin, C.; Yi, J.; Kang, J. Development of CdSe–ZnO Flower-Rod Core-Shell Structure Based Photoelectrochemical Biosensor for Detection of Norovirous RNA. Sensors 2018, 18, 2980. [Google Scholar] [CrossRef]
- Velusamy, V.; Arshak, K.; Korostynska, O.; Oliwa, K.; Adley, C. An overview of foodborne pathogen detection: In the perspective of biosensors. Biotechnol. Adv. 2010, 28, 232–254. [Google Scholar] [CrossRef]
- Arora, P.; Sindhu, A.; Kaur, H.; Dilbaghi, N.; Chaudhury, A. An overview of transducers as platform for the rapid detection of foodborne pathogens. Appl. Microbiol. Biotechnol. 2013, 97, 1829–1840. [Google Scholar] [CrossRef]
- Driskell, J.D.; Zhu, Y.; Kirkwood, C.D.; Zhao, Y.; Dluhy, R.A.; Tripp, R.A. Rapid and sensitive detection of rotavirus molecular signatures using surface enhanced Raman spectroscopy. PLoS ONE 2010, 5, e10222. [Google Scholar] [CrossRef] [PubMed]
- Shanmukh, S.; Jones, L.; Driskell, J.; Zhao, Y.; Dluhy, R.; Tripp, R.A. Rapid and sensitive detection of respiratory virus molecular signatures using a silver nanorod array SERS substrate. Nano Lett. 2006, 6, 2630–2636. [Google Scholar] [CrossRef] [PubMed]
- Mattison, K.; Corneau, N.; Berg, I.; Bosch, A.; Duizer, E.; Gutiérrez-Aguirre, I.; L’Homme, Y.; Lucero, Y.; Luo, Z.; Martyres, A. Development and validation of a microarray for the confirmation and typing of norovirus RT-PCR products. J. Virol. Methods 2011, 173, 233–250. [Google Scholar] [CrossRef] [PubMed]
- Huang, W.; Samanta, M.; Crawford, S.E.; Estes, M.K.; Neill, F.H.; Atmar, R.L.; Palzkill, T. Identification of human single-chain antibodies with broad reactivity for noroviruses. Protein Eng. Des. Sel. 2014, 27, 339–349. [Google Scholar] [CrossRef]
- de Rougemont, A.; Ruvoen-Clouet, N.; Simon, B.; Estienney, M.; Elie-Caille, C.; Aho, S.; Pothier, P.; Le Pendu, J.; Boireau, W.; Belliot, G. Qualitative and quantitative analysis of the binding of GII.4 norovirus variants onto human blood group antigens. J. Virol. 2011, 85, 4057–4070. [Google Scholar] [CrossRef]
- Helmerhorst, E.; Chandler, D.J.; Nussio, M.; Mamotte, C.D. Real-time and label-free bio-sensing of molecular interactions by surface plasmon resonance: A laboratory medicine perspective. Clin. Biochem. Rev. 2012, 33, 161. [Google Scholar]
- Ahmed, S.R.; Takemeura, K.; Li, T.-C.; Kitamoto, N.; Tanaka, T.; Suzuki, T.; Park, E.Y. Size-controlled preparation of peroxidase-like graphene-gold nanoparticle hybrids for the visible detection of norovirus-like particles. Biosens. Bioelectron. 2017, 87, 558–565. [Google Scholar] [CrossRef]
- Han, K.N.; Choi, J.-S.; Kwon, J. Three-dimensional paper-based slip device for one-step point-of-care testing. Sci. Rep. 2016, 6, 1–7. [Google Scholar] [CrossRef]
- Lee, S.; Ahn, S.; Chakkarapani, S.K.; Kang, S.H. Supersensitive Detection of the Norovirus Immunoplasmon by 3D Total Internal Reflection Scattering Defocus Microscopy with Wavelength-Dependent Transmission Grating. ACS Sens. 2019, 4, 2515–2523. [Google Scholar] [CrossRef]
- Altintas, Z.; Gittens, M.; Pocock, J.; Tothill, I.E. Biosensors for waterborne viruses: Detection and removal. Biochimie 2015, 115, 144–154. [Google Scholar] [CrossRef]
- Caygill, R.L.; Blair, G.E.; Millner, P.A. A review on viral biosensors to detect human pathogens. Anal. Chim. Acta 2010, 681, 8–15. [Google Scholar] [CrossRef] [PubMed]
- Dixon, M.C. Quartz crystal microbalance with dissipation monitoring: Enabling real-time characterization of biological materials and their interactions. J. Biomol. Tech. JBT 2008, 19, 151. [Google Scholar] [PubMed]
- Kuznetsov, Y.G.; McPherson, A. Atomic force microscopy in imaging of viruses and virus-infected cells. Microbiol. Mol. Biol. Rev. 2011, 75, 268–285. [Google Scholar] [CrossRef] [PubMed]
- Bally, M.; Rydell, G.E.; Zahn, R.; Nasir, W.; Eggeling, C.; Breimer, M.E.; Svensson, L.; Hook, F.; Larson, G. Norovirus GII.4 virus-like particles recognize galactosylceramides in domains of planar supported lipid bilayers. Angew. Chem. Int. Ed. Engl. 2012, 51, 12020–12024. [Google Scholar] [CrossRef] [PubMed]
- Selvaratnam, T. Optimization and characterization of a centrally functionalized quartz crystal microbalance sensor surface for Norovirus detection. Master’s Thesis, KTH Royal Institute of Technology, Stockholm, Sweden, 2015. [Google Scholar]
- Neumann, F.; Madaboosi, N.; Hernández-Neuta, I.; Salas, J.; Ahlford, A.; Mecea, V.; Nilsson, M. QCM mass underestimation in molecular biotechnology: Proximity ligation assay for norovirus detection as a case study. Sens. Actuators B Chem. 2018, 273, 742–750. [Google Scholar] [CrossRef]
- Aybeke, E.N.; Belliot, G.; Lemaire-Ewing, S.; Estienney, M.; Lacroute, Y.; Pothier, P.; Bourillot, E.; Lesniewska, E. HS-AFM and SERS Analysis of Murine Norovirus Infection: Involvement of the Lipid Rafts. Small 2017, 13, 1600918. [Google Scholar] [CrossRef]
- Cuellar, J.; Meinhoevel, F.; Hoehne, M.; Donath, E. Size and mechanical stability of norovirus capsids depend on pH: A nanoindentation study. J. Gen. Virol. 2010, 91, 2449–2456. [Google Scholar] [CrossRef]
- Kostrzynska, M.; Bachand, A. Application of DNA microarray technology for detection, identification, and characterization of food-borne pathogens. Can. J. Microbiol. 2006, 52, 1–8. [Google Scholar] [CrossRef]
- Chou, C.-C.; Lee, T.-T.; Chen, C.-H.; Hsiao, H.-Y.; Lin, Y.-L.; Ho, M.-S.; Yang, P.-C.; Peck, K. Design of microarray probes for virus identification and detection of emerging viruses at the genus level. BMC Bioinform. 2006, 7, 232. [Google Scholar] [CrossRef]
- Wang, D.; Coscoy, L.; Zylberberg, M.; Avila, P.C.; Boushey, H.A.; Ganem, D.; DeRisi, J.L. Microarray-based detection and genotyping of viral pathogens. Proc. Natl. Acad. Sci. USA 2002, 99, 15687–15692. [Google Scholar] [CrossRef]
- Pagotto, F.; Corneau, N.; Mattison, K.; Bidawid, S. Development of a DNA microarray for the simultaneous detection and genotyping of noroviruses. J. Food Prot. 2008, 71, 1434–1441. [Google Scholar] [CrossRef] [PubMed]
- Acton, Q.A. Norovirus: New Insights for the Healthcare Professional, 2012 ed.; eBooks, USA; ScholarlyEditions, 2012. [Google Scholar]
- Yu, C.; Wales, S.Q.; Mammel, M.K.; Hida, K.; Kulka, M. Optimizing a custom tiling microarray for low input detection and identification of unamplified virus targets. J. Virol. Methods 2016, 234, 54–64. [Google Scholar] [CrossRef] [PubMed]
- Brinkman, N.E.; Fout, G.S. Development and evaluation of a generic tag array to detect and genotype noroviruses in water. J. Virol. Methods 2009, 156, 8–18. [Google Scholar] [CrossRef] [PubMed]
- Quiñones, B.; Lee, B.G.; Martinsky, T.J.; Yambao, J.C.; Haje, P.K.; Schena, M. Sensitive Genotyping of Foodborne-Associated Human Noroviruses and Hepatitis A Virus Using an Array-Based Platform. Sensors 2017, 17, 2157. [Google Scholar] [CrossRef]
- Won, Y.J.; Lee, S.G.; Paik, S.Y.; Lyoo, K.S. Development of an oligonucleotide-based microarray for the detection of foodborne viruses. J. Consum. Prot. Food Saf. 2019, 14, 287–291. [Google Scholar] [CrossRef]
- Gyawali, P.; KC, S.; Beale, D.J.; Hewitt, J. Current and Emerging Technologies for the Detection of Norovirus from Shellfish. Foods 2019, 8, 187. [Google Scholar] [CrossRef]
- Fumian, T.M.; Fioretti, J.M.; Lun, J.H.; dos Santos, I.A.; White, P.A.; Miagostovich, M.P. Detection of norovirus epidemic genotypes in raw sewage using next generation sequencing. Environ. Int. 2019, 123, 282–291. [Google Scholar] [CrossRef]
- Strubbia, S.; Phan, M.V.; Schaeffer, J.; Koopmans, M.; Cotten, M.; Le Guyader, F.S. Characterization of Norovirus and Other Human Enteric Viruses in Sewage and Stool Samples Through Next-Generation Sequencing. Food Environ. Virol. 2019, 11, 400–409. [Google Scholar] [CrossRef]
- Imamura, S.; Haruna, M.; Goshima, T.; Kanezashi, H.; Okada, T.; Akimoto, K. Application of next-generation sequencing to investigation of norovirus diversity in shellfish collected from two coastal sites in Japan from 2013 to 2014. Jpn. J. Vet. Res. 2016, 64, 113–122. [Google Scholar]
- Trauger, S.A.; Junker, T.; Siuzdak, G. Investigating viral proteins and intact viruses with mass spectrometry. In Modern Mass Spectrometry; Schalley, C.A., Ed.; Springer: Berlin/Heidelberg, Germany, 2003; pp. 265–282. [Google Scholar]
- Colquhoun, D.R.; Schwab, K.J.; Cole, R.N.; Halden, R.U. Detection of norovirus capsid protein in authentic standards and in stool extracts by matrix-assisted laser desorption ionization and nanospray mass spectrometry. Appl. Environ. Microbiol. 2006, 72, 2749–2755. [Google Scholar] [CrossRef]
- Hellberg, R.S.; Li, F.; Sampath, R.; Yasuda, I.J.; Carolan, H.E.; Wolfe, J.M.; Brown, M.K.; Alexander, R.C.; Williams-Hill, D.M.; Martin, W.B. Rapid detection and differentiation of human noroviruses using RT-PCR coupled to electrospray ionization mass spectrometry. Food Microbiol. 2014, 44, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Goodridge, L.; Goodridge, C.; Wu, J.; Griffiths, M.; Pawliszyn, J. Isoelectric point determination of norovirus virus-like particles by capillary isoelectric focusing with whole column imaging detection. Anal. Chem. 2004, 76, 48–52. [Google Scholar] [CrossRef] [PubMed]
- Moore, M.D.; Mertens, B.S.; Jaykus, L.-A. Alternative In Vitro Methods for the Determination of Viral Capsid Structural Integrity. J. Vis. Exp. 2017, 129, e56444. [Google Scholar] [CrossRef] [PubMed]
| Method | Cost | Time | Sensitivity | Specificity | Detection Limit | Advantages | Disadvantages |
|---|---|---|---|---|---|---|---|
| Electron microscopy (EM) | High | 15 min 1 | Low | Low | 106 viral particles/mL stool | Fast; capable of visually observation of viral morphology | Low sensitivity and specificity; laborious and expensive operation (including the requirement of trained personnel) |
| Enzyme-linked immunosorbent assay (ELISA) | Medium | 60~90 min 1 | 31.6%~92.0% | 65.3%~100.0% | 104~106 viral particles/mL stool | Cheap reagent; long shelf-life; widely available | Measurement of enzyme activity may be complex and the enzyme activity may be affected by plasma constituents |
| Immunochromatography (ICG) | Medium | 15 min | 17.0%~83.0% | 87.5%~100.0% | NA | Fast; long shelf life (12~24 months); ease of use; relatively low cost and relative ease in manufacturing | Varied performance |
| Real time RT-qPCR | High | 40 min~3 h (with pre-extracted nucleic acid) | High | High | Around 10~100 gc/g sample | High sensitivity and specificity | Reagent-intensive; requirement of specific equipment |
| Biosensor | High | Short (Varied) | High | High | Varied | Potentials for point-of-care diagnostics | Sample preparation; matrix effects and system integration |
| Bioreceptor | Availability | Cost 1 | Component | Specificity | Sensitivity | Advantages | Disadvantages | Reference |
|---|---|---|---|---|---|---|---|---|
| Monoclonal antibody | Some are commercially available; some are currently available in research laboratories | Varied | large (~150 kDa) multimeric proteins | High | Medium | High specificity and selectivity | Produced from animal systems, more expensive; the binding conditions cannot be modulated; heat sensitive and binding irreversible; limited shelf-life | [16,17] |
| Aptamer | Available in some research laboratories; can be synthesized commercially upon request | $6–16/nmol 2 | DNA oligonucleotide, single strand | High | Medium | Chemical synthesis; the binding conditions can be modulated; heat stable and recoverable; less expensive; long shelf-life | Rapid degradation of aptamers by nucleases in biological media or in blood; time- and labor-consuming; may also bind to molecules with a similar structure; require purified target molecules for generation | [18,19] |
| Porcine gastric mucin (PGM) | Easily available commercially | $3.84/g 3 | Type A, H type 1 and Lewis b HBGA, other carbohydrates as well as protein (20%) | Low | High | Low cost, easily available, and broad reactivity | Low specificity, since it can also bind to other microbes; PGM also contains another broadly recognized receptor-sialic acid | [20,21,22] |
| Histo-blood group antigens (HBGAs) | Difficult to obtain since only one company produces HBGAs, and it′s possibly backordered | ~ $260/mg 4 | ABH, secretor and Lewis antigens | Low | High | Commercially available; bind to all NoVs except for a few genotypes | Low specificity, since they can also bind to other viruses and bacteria, including Rotavirus and rabbit hemorrhagic disease virus | [20] |
| Biosensor Method | Target | Platform | Detection Material | Ligand Chosen | Sample Type | Detection Time | Linear Range | Detection Limit | Specificity | Reference |
|---|---|---|---|---|---|---|---|---|---|---|
| SERS | FCV | Functionalized gold chips | AuNP | mAb | Cell culture | N/A | 1.0 × 106~2.5 × 108 viruses/mL | 1 × 106 viruses/mL (or ~70 captured viruses) | N/A | [129] |
| SERS | MNV | Gold coated silicon wafers | Gold substrate | N/A | Mixture virus strains | N/A | N/A | Titer of 100 | N/A | [130] |
| SERS- ICG | NoV VP1 protein | Polyethylene polyvinyl chloride base strip | Colloidal gold | Antibody | Centrifuged fecal specimen | ~15 min | 3~150 ng/mL detection range | 0.5 ng/mL | Good | [131] |
| LSPR-based fluorescence | NoV VLPs | NP solution | AuNP and QDs | Antibody | N/A | ~5 min | 10~100 pg/mL | 0.4 pg/mL | N/A | [132] |
| LSPR-induced optical sensor | NoV VLPs and HuNoV | Liquid | CdSeTeS QDs/AuNP nanocomposite | Antibody | NoV VLPs and clinically isolated NoV | Response time 1 min | 10 fg/mL~1 ng/mL NoV VLPs and 100~100,000 copies/mL | 12.1 fg/mL NoV VLPs and 95 copies/mL clinically isolated HuNoV | Superior | [133] |
| Plasmonic biosensor | NoV capsid and HuNoV | LSPR layer | AuNP | Affinity peptide | NoV capsid protein and HuNoV | N/A | 10~105 copies/mL | 0.1 ng/mL NoV capsid protein in culture media and 9.9 copies/mL HuNoV | High | [134] |
| LSPR-amplified fluorescence assisted by magnetic field | NoV VLPs and HuNoV | Liquid | AuNP/MNP hybrid nanocomposites and CdSeS QDs | GII antibody | NoV VLPs in feces and feces containing HuNoV | N/A | 1 pg/mL to 5 ng/mL NoV VLPs; 102~107 RNA copies/mL GII isolated clinical HuNoV | 0.48 pg/mL NoV VLPs in feces; 84~934 copies/mL GII HuNoV | High | [135] |
| SPR | FCV | Au sensor chip | Thin gold layer | Antibody | Purified cell culture lysates or spiked oyster matrices | <15 min | 3 × 104~106 TCID50 FCV/mL | 104 TCID50 FCV/mL | N/A | [136] |
| SPR | HuNoV (GII.4) | Au sensor chip | Polyacrylate beads | Con A | Spiked lettuce, strawberries, and milk | 15 min | N/A | up to 10 RT-PCR units/mL | N/A | [137] |
| SPR-assisted fluorescence | NoV VLPs | Al film on polystyrene substrate | CdSe-ZnS-based quantum dot fluorescent dye | mAb and pAb | N/A | N/A | 0.01~1 ng/mL | 0.01 ng/mL (or 100 VLPs) | N/A | [138] |
| Fluorescence | NoV GII RNA | Liquid | AuNR@CdSeTe QDs | MB containing 20 bp complementary to NV RNA | Purified and mixed virus RNA | N/A | 2~18 copies/mL | 1.2 copies/mL | High | [139] |
| Fluorescence | Single NoV VLP (GII.4) | Lipid bilayer coated glass-bottom microtiter wells | Rhodamine-labeled lipid vesicle | H type 1 GSL | N/A | <2 h | 12~200 fM | 16 fM (single-molecule) | High | [140] |
| Fluorescence | FCV | Fabricated nanoporous membranes in glass microchannels | Protein A superparamagnetic beads and fluorescent liposomes | mAb and pAb | Purified and dialyzed virus | Within 2.5 h | N/A | 1.6 × 105 PFU/mL | N/A | [141] |
| Fluorescence | Single strand NoV RNA | 96 well plates | Fluorescent F0F1-ATPase molecular motor containing ε-subunit antibody-streptomycin-biotin-probe | NoV RNA probe | Extracted RNA | Within 1 h | N/A | 0.005 ng/mL | High | [142] |
| Fluorescence | NoV capsid protein | Paper-based microfluidic platform | MWCNT or GO | Aptamer | Spiked mussel samples | ~10 min | 13 ng/mL to 13 μg/mL | 3.3~4.4 ng center dot per mL | High | [70] |
| Chemiluminescence | NoV GII capsid | Magnetic NP solution | GO/Fe3O4 nanocomposite | Modified aptamer | Tap water and artificial urine | 30 min incubation time | 0.16–10 μg/mL | 80 ng/mL (in tap water) | High | [143] |
| BLI | NoV antibody | Octet BLI sensor | Co(III)-NTA | Avidin and His-tagged NVLPs | Human serum samples | 10–15 min oxidation time | N/A | N/A | N/A | [144] |
| BLI | NoV antibody | Octet BLI sensor | Ni-NTA | NoV VLPs or NoV P-particles | Human serum samples | 10-20 min with pre-functionalized sensors | N/A | Dilutions up to 1:100,000 | N/A | [145] |
| BLI | NoV VLPs (GI.1 and GII.4) | Needle-shaped sensor | N/A | Antibodies | N/A | 2 min | 10~20 μg/mL | 5 μg/mL | N/A | [146] |
| 3D dual-view light sheet microscopy based | NoV GI capsid | Gold nanoarray on glass wafer | AuNS and AgNP | Antibody | NoV capsid spiked lettuce leaf | N/A | 7.8 zM~240 aM | 7.8 zM | Signal slightly increase towards other antigens | [147] |
| Photoluminescence based biosensor | NoV GII RNA | 96-well plate | SiO2-coated CdZnSeS QD | Molecular beacon | Buffer and human serum | 3 min hybridization time | 2~16 copies/mL in buffer and 0~8 copies/mL in human serum | 8.2 gc/mL in human serum and 9.3 gc/mL in buffer | high | [148] |
| Near-field illumination biosensor assisted by external magnetic field | NoV VLPs | Liquid cell | Magnetic bead and polystyrene bead | Antibody | Contaminated water | N/A | N/A | 40 particles per 100 mu l in contaminated water | N/A | [149] |
| Nake-eye biosensor | HuNoV | Dot-blotting | Polyhedral Cu nanoshell deposited AuNPs | Antibody | Stool | Signal generation time 10 min | 2.7 × 103~2.7 × 105 copies | 2700 copies NoV in clinical stool samples | High | [150] |
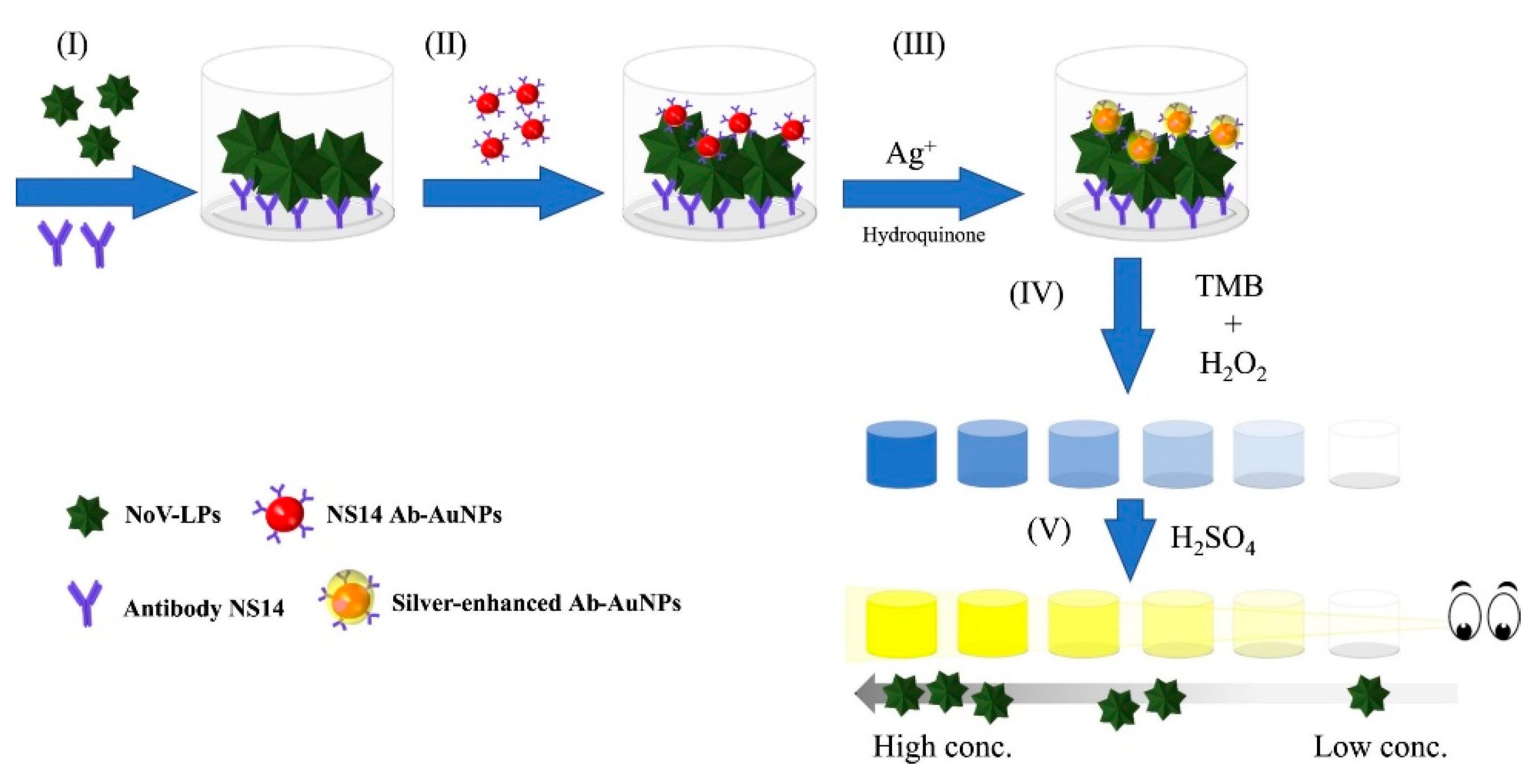
| Silver-enhanced nanozyme-based colorimetric immunoassay | NoV VLP and GII.4 feces | Microtiter plate | Au/Ag NPs | GII antibody | Human feces | N/A | 10~105 pg/mL NoV VLP ; 10~104 and 102~105 copies/mL fecal solution for NoV GII.3 and GII.4, respectively | 10.8 pg/mL NoV VLP; 13.2~16.3 gc/mL fecal NoV GII.3 and GII.4 (or 132~163 gc/g feces) | High | [151] |
| Colorimetric NanoZyme aptasensor | MNV | Liquid | AuNP | AG3 Aptamer | Cell culture in presence of matrix | 10 min | 200−10,000 viruses/mL, or 1320−19,800 viruses/mL, or 3300−33,000 viruses/mL | 200 viruses/mL (experimental) and 30 viruses/mL (calculated) | High | [69] |
| Electrochemical | GII NoV VLPs | PDMS microfluidic chip | GRP-AuNPs composite modified carbon electrode | Aptamer | Spiked blood samples and samples with other interferences | N/A | 100 pM~3.5 nM | 100 pM | High | [152] |
| Electrochemical | NoV RNA | Planar Pt-IDE | Au/iron-oxide MNP-decorated CNT | Probe RNA | N/A | N/A | 1 pM~10 nM | 8.8 pM | High | [153] |
| Electrochemical | NoV VLPs | Pt-IDE | Au/MNP-decorated GRPs | Antibody | N/A | N/A | 0.1 pg/mL~1 ng/mL | 1.16 pg/mL | High | [154] |
| Electrochemical | NoV capsid proteins or HuNoV | Three-electrode cell | Au electrode | Affinity peptide | Spiked fetal bovine serum | N/A | 0.01~1000 μg/mL NoV capsid proteins; 1~103 or 103~106 NoV | 99.8 nM for NoV capsid proteins and 7.8 copies/mL for HuNoV | Varied | [155] |
| Electrochemical | NoV capsid | Chromium IDE fabricated glass substrate | Chromium IDE | N/A | Recombinant NoV capsid | 5 min | N/A | 2.5 ng/mL | N/A | [156] |
| Voltammetric electrochemical | NoV (GII.4) | PDMS bonded glass substrate | Au electrode | Con A and NoV antibodies | Lettuce | 1 h | 102 and 106 copies/mL | 60 copies/mL | 98% | [157] |
| Electrochemical | FCV | Fabricated nanoporous membranes in glass microchannels | Protein A superparamagnetic beads and electrochemical liposomes | mAb and pAb | Purified and dialyzed virus | 2.5 h | N/A | 3.2 × 106 PFU/mL | N/A | [141] |
| Electrochemical | MNV | Fabricated silicon substrate | Au working electrode | Aptamer AG3 | Cell culture | N/A | 10~104 PFU/mL | 10 PFU/mL | N/A | [68] |
| Electrochemical | MNV | SPE | AuNP | Aptamer AG3 | Cell culture | 60 min | 20~120 aM (ca. 360~2170 viral particles) | 10 aM (~180 virus particles) | Not high | [67] |
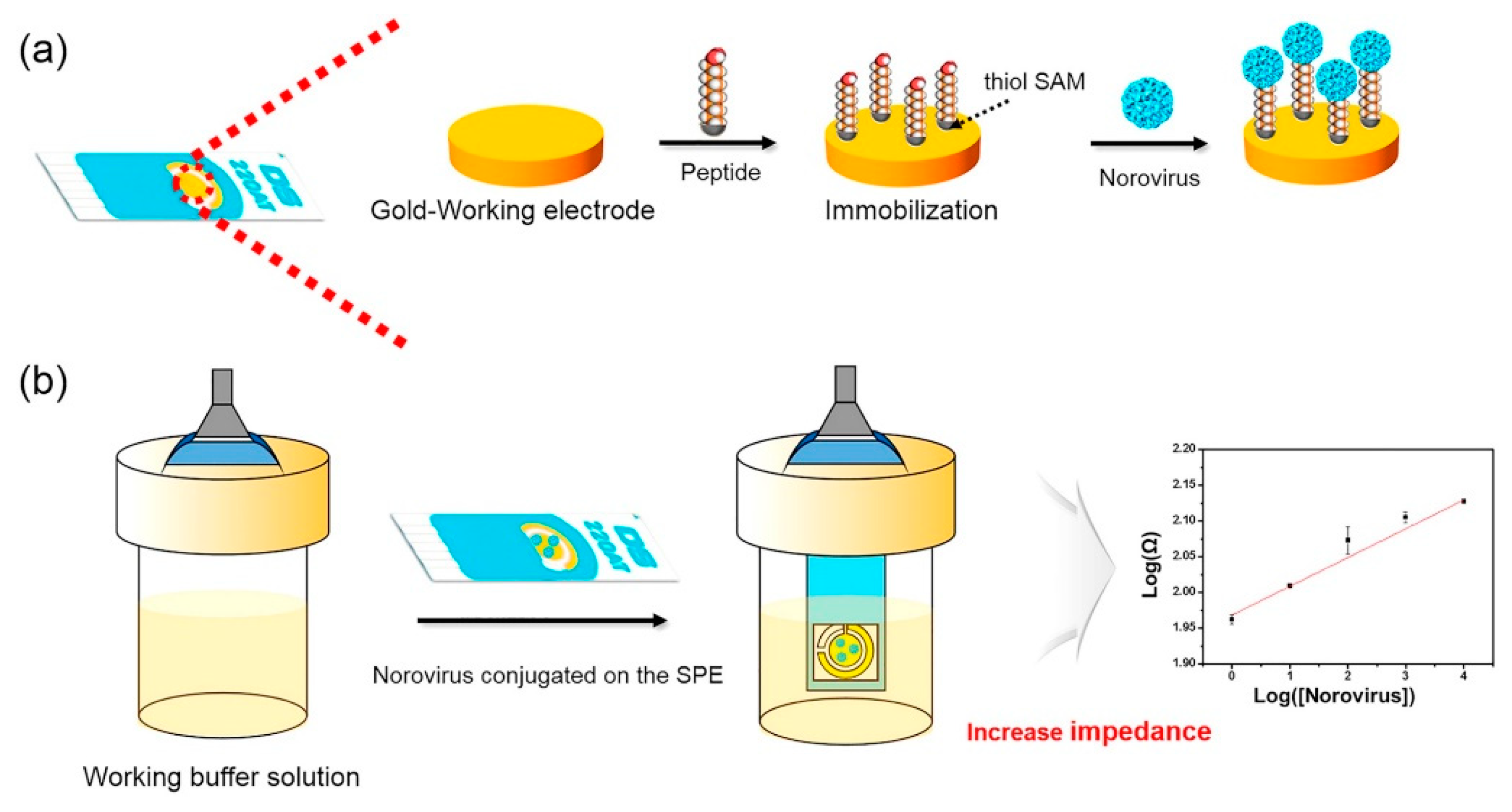
| Impedance electrochemical | HuNoV GII.4 | SPE | Au electrode | NoroBP-nonFoul (FlexL)2 peptide | Clinical HuNoV | Within 30 min | 0 to 104 copies/mL HuNoV GII.4; 10 to 105 copies/mL extracted NoV from oysters | 1.78 gc/mL HuNoV GII.4 and 2.47 gc/mL NoV from oysters | High | [158] |
| Field effect transistor based | NoV VLPs | Kapton films | Inkjet-printed graphene materials | Antibody | NoV VLPs | N/A | 0.1 to 100 μg/mL NoV VLPs | ~0.1 μg/mL | N/A | [159] |
| Photoelectrochemical | NoV RNA | An electrochemical workstation | CdSe–ZnO | DNA probe | Spiked diluted serum | N/A | 0~5.10 nM NoV RNA | 0.50 nM | N/A | [160] |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, L.; Moore, M.D. A Survey of Analytical Techniques for Noroviruses. Foods 2020, 9, 318. https://doi.org/10.3390/foods9030318
Liu L, Moore MD. A Survey of Analytical Techniques for Noroviruses. Foods. 2020; 9(3):318. https://doi.org/10.3390/foods9030318
Chicago/Turabian StyleLiu, Lingling, and Matthew D. Moore. 2020. "A Survey of Analytical Techniques for Noroviruses" Foods 9, no. 3: 318. https://doi.org/10.3390/foods9030318
APA StyleLiu, L., & Moore, M. D. (2020). A Survey of Analytical Techniques for Noroviruses. Foods, 9(3), 318. https://doi.org/10.3390/foods9030318






