Inactivation of Aerosolized Hepatitis A Viral Droplets on Food Contact Surfaces by Ultraviolet-Light-Emitting Diodes at 255 nm and 279 nm
Abstract
1. Introduction
2. Materials and Methods
2.1. Animal Cell Culture as Hosts
2.2. Propagation of HAV
2.3. Aerosolization of HAV Droplets on Discs
2.4. Aerosolized HAV Deposit Treatments with UV-C LED (255 nm or 279 nm) on Stainless-Steel and Glass Discs
2.5. Hepatitis A Virus Recovery
2.6. HAV Infectious Plaque Assay
2.7. Dose Calculation of UV-C at 255 nm and 279 nm
2.8. Statistical Analysis of Recovered HAV
3. Results
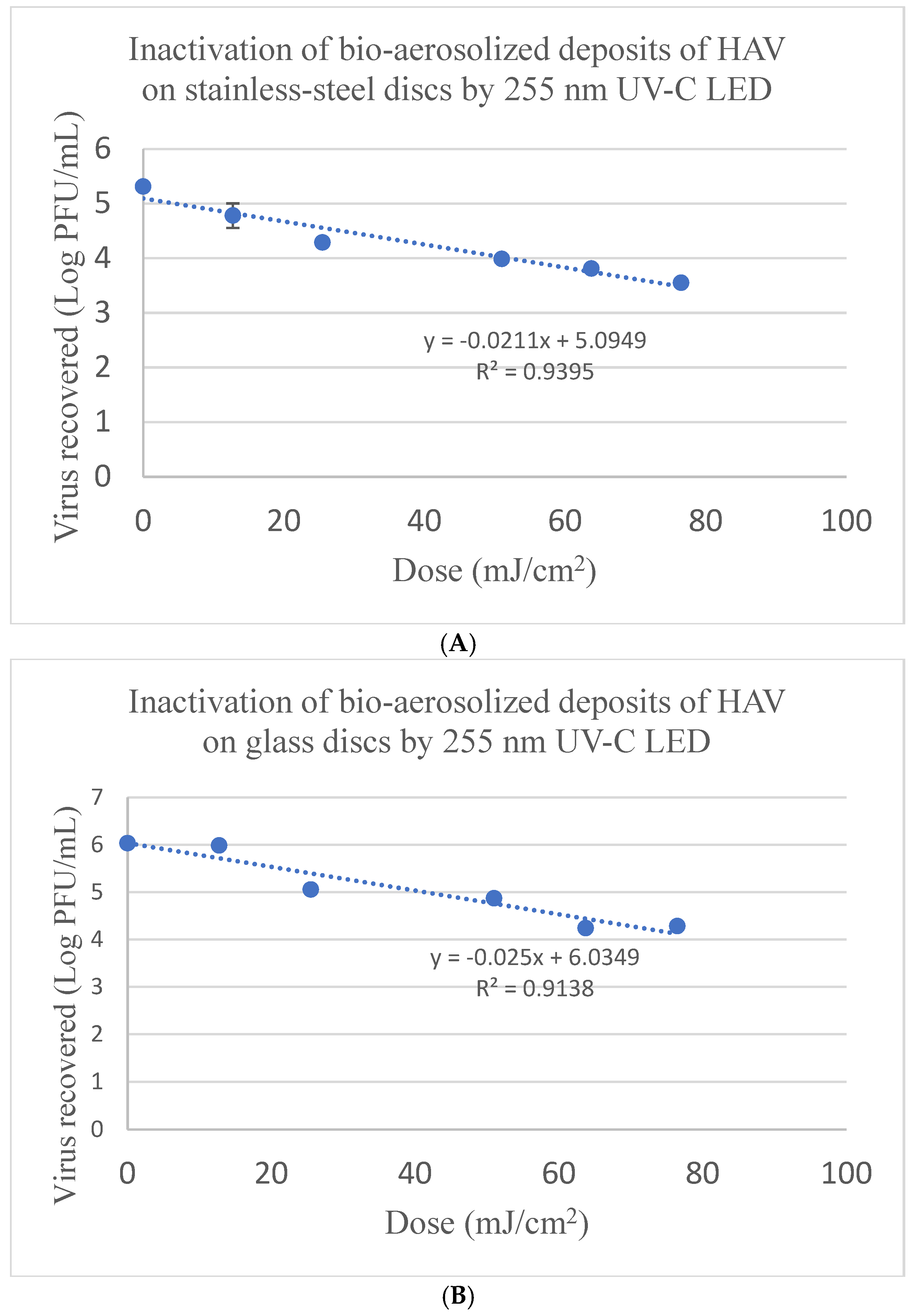
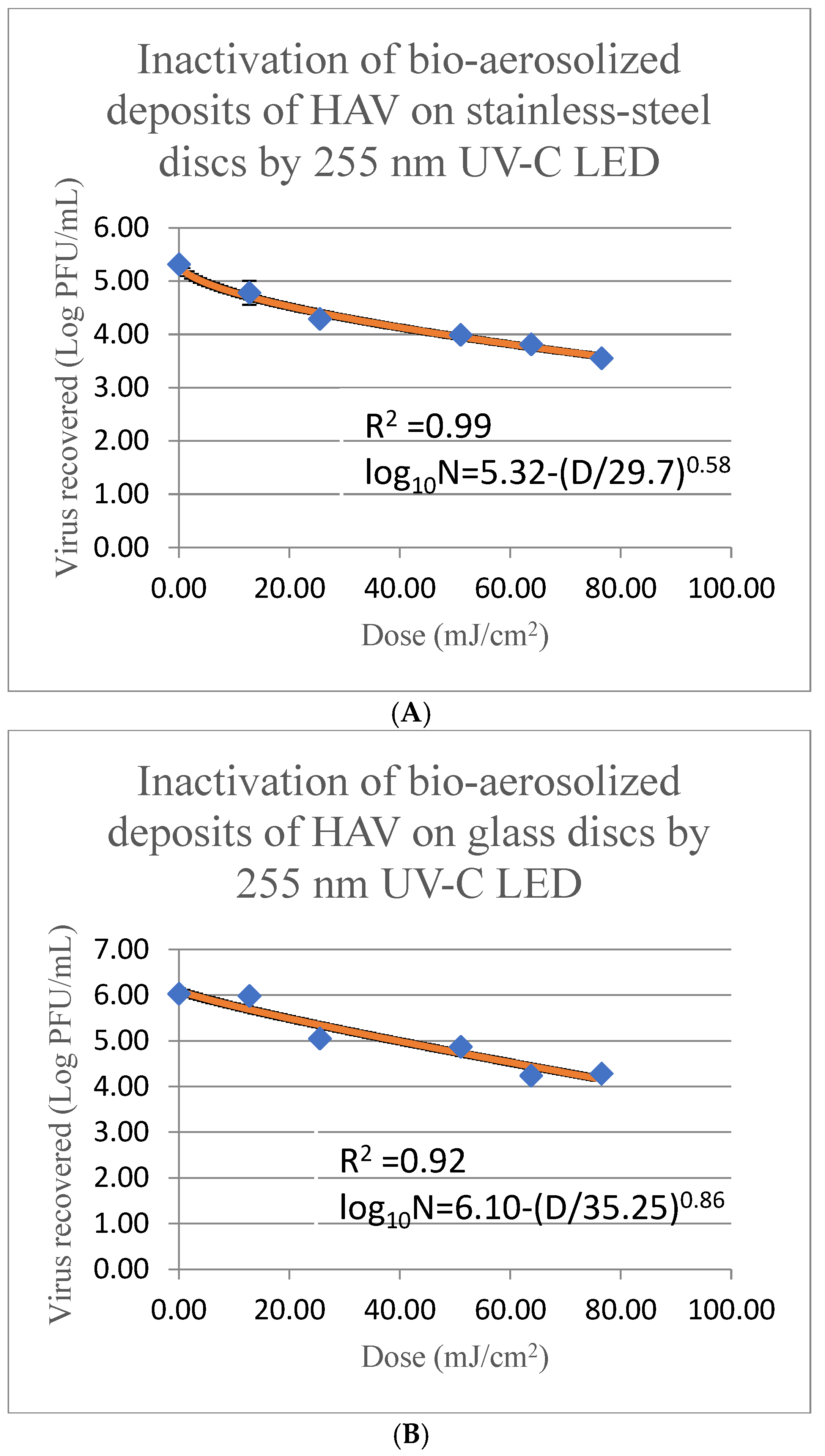
3.1. Bioaerosol Deposited HAV Inactivation on Stainless-Steel Discs by a 255 nm UV-C LED System
3.2. Bioaerosol Deposited HAV Inactivation on Glass Discs by a 255 nm UV-C LED System
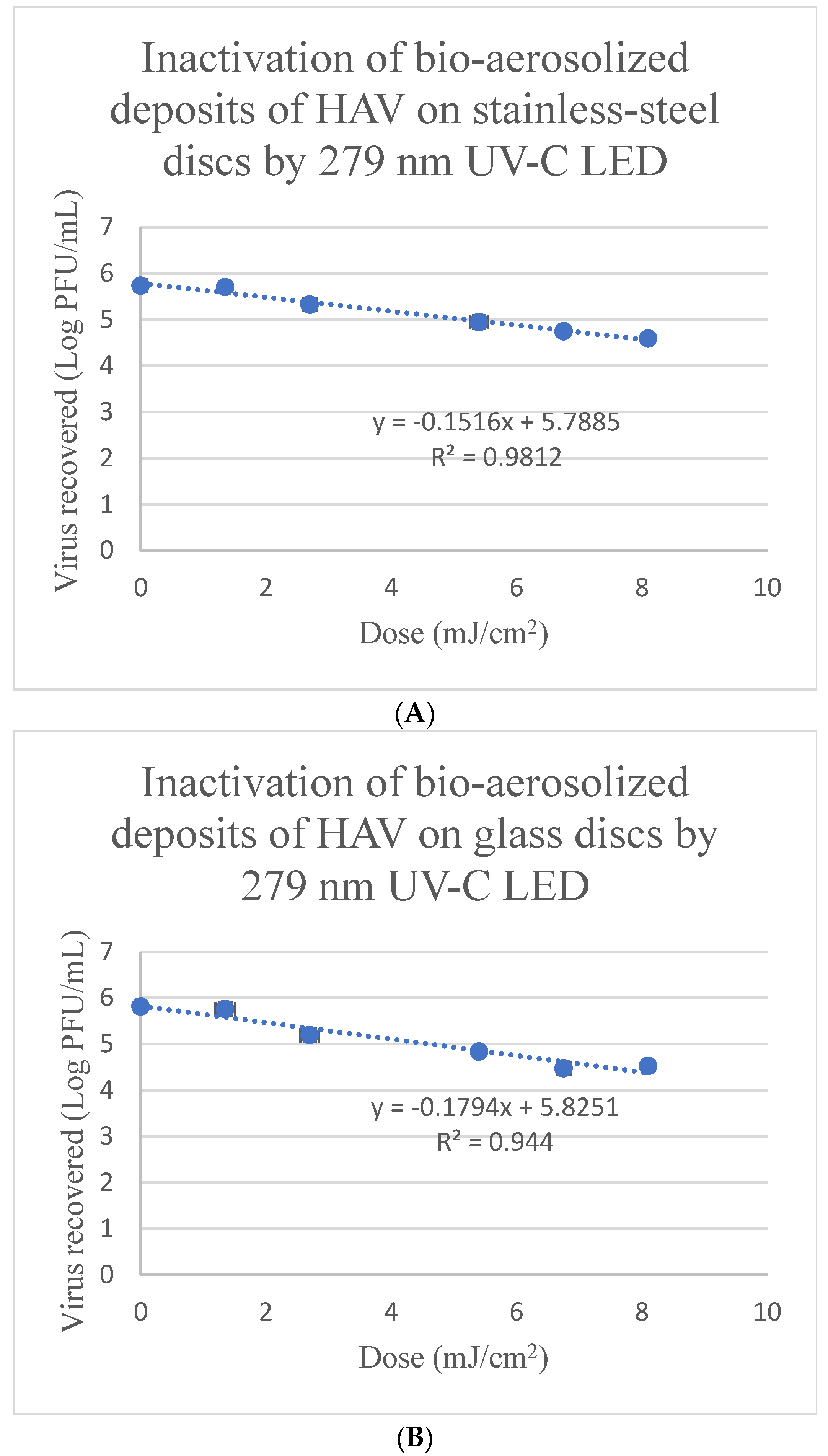
3.3. Inactivation of Bioaerosol Deposited HAV on Stainless-Steel Discs by a 279 nm UV-C LED System
3.4. Inactivation of Bioaerosol Deposited HAV on Glass Discs with a 279 nm UV-C LED System
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Stuart, D.I.; Ren, J.; Wang, X.; Rao, Z.; Fry, E.E. Hepatitis A Virus Capsid Structure. Cold Spring Harb. Perspect. Med. 2019, 9, a031807. [Google Scholar] [CrossRef] [PubMed]
- Sattar, S.A.; Jason, T.; Bidawid, S.; Farber, J. Foodborne spread of hepatitis A: Recent studies on virus survival, transfer and inactivation. Can. J. Infect. Dis. Med. Microbiol. 2000, 11, 159–163. [Google Scholar] [CrossRef] [PubMed]
- Yi, M.; Lemon, S.M. Replication of subgenomic hepatitis A virus RNAs expressing firefly luciferase is enhanced by mutations associated with adaptation of virus to growth in cultured cells. J. Virol. 2002, 76, 1171–1180. [Google Scholar] [CrossRef]
- Hussain, Z.; Das, B.C.; Husain, S.A.; Asim, M.; Chattopadhyay, S.; Malik, A.; Poovorawan, Y.; Theamboonlers, A.; Kar, P. Hepatitis A viral genotypes and clinical relevance: Clinical and molecular characterization of hepatitis A virus isolates from northern India. Hepatol. Res. Off. J. Jpn. Soc. Hepatol. 2005, 32, 16–24. [Google Scholar] [CrossRef] [PubMed]
- Kaddoura, M.; Allaham, R.; Abubakar, A.; Ezzeddine, A.; Barakat, A.; Mala, P.; Zaraket, H. Hepatitis A virus genotype IB outbreak among internally displaced persons, Syria. Emerg. Infect. Dis. 2020, 26, 369. [Google Scholar] [CrossRef]
- Vaughan, G.; Rossi, L.M.G.; Forbi, J.C.; Paula, V.S.; Purdy, M.A.; Xia, G.; Khudyakov, Y.E. Hepatitis A virus: Host interactions, molecular epidemiology and evolution. Infect. Genet. Evol. 2014, 21, 227–243. [Google Scholar] [CrossRef]
- Shin, E.C.; Jeong, S.H. Natural History, Clinical Manifestations, and Pathogenesis of Hepatitis A. Cold Spring Harb. Perspect. Med. 2018, 8, a031708. [Google Scholar] [CrossRef]
- Foster, M.A.; Hofmeister, M.G.; Kupronis, B.A.; Lin, Y.; Xia, G.L.; Yin, S.; Teshale, E. Increase in Hepatitis A Virus Infections—United States, 2013–2018. MMWR. Morb. Mortal. Wkly. Rep. 2019, 68, 413–415. [Google Scholar] [CrossRef]
- Ridpath, A.; Reddy, V.; Layton, M.; Misener, M.; Scaccia, A.; Starr, D.M.; Stavinsky, F.; Varma, J.K.; Waechter, H.; Zucker, J.R.M.; et al. Hepatitis A Cases Among Food Handlers: A Local Health Department Response-New York City, 2013. J. Public Heal. Manag. Pr. 2017, 23, 571–576. [Google Scholar] [CrossRef]
- Pradhan, A.K.; Pang, H.; Mishra, A. Foodborne disease outbreaks associated with organic foods: Animal and plant products. In Safety and Practice for Organic Food; Academic Press: Cambridge, MA, USA, 2019; pp. 135–150. [Google Scholar]
- Centers for Disease Control and Prevention (CDC). Hepatitis A. Available online: https://www.cdc.gov/hepatitis-a/index.html (accessed on 2 November 2024).
- Centers for Disease Control and Prevention (CDC). Estimates of Foodborne Illness in the United States. Available online: https://www.cdc.gov/foodborneburden/index.html#:~:text=CDC%20estimates%2048%20million%20people,known%20pathogens%20and%20unspecified%20agents (accessed on 1 November 2024).
- Enkirch, T.; Eriksson, R.; Persson, S.; Schmid, D.; Aberle, S.W.; Löf, E.; Ederth, J.L. Hepatitis A outbreak linked to imported frozen strawberries by sequencing. Eurosurveillance 2018, 23, 1800528. [Google Scholar]
- Sharma, A.; Singh, A.; Pendyala, B.; Balamurugan, S.; Patras, A. Inactivation of Deposited Bioaerosols on Food Contact Surfaces with UV-C Light Emitting Diode Devices. Appl. Environ. Microbiol. 2024, 91, e01093-24. [Google Scholar] [CrossRef] [PubMed]
- Tellier, R.; Li, Y.; Cowling, B.J. Recognition of aerosol transmission of infectious agents: A commentary. BMC Infect. Dis. 2019, 19, 101. [Google Scholar] [CrossRef] [PubMed]
- Pereira, A.R.; Braga, D.F.; Vassal, M.; Gomes, I.B.; Simões, M. Ultraviolet C irradiation: A promising approach for the disinfection of public spaces? Sci. Total Environ. 2023, 879, 163007. [Google Scholar] [CrossRef]
- Corson, E.; Pendyala, B.; Patras, A.; D’Souza, D.H. Inactivation of hepatitis A virus, feline calicivirus, and Tulane virus on Formica coupons using ultraviolet light technologies. Heliyon 2024, 10, e25201. [Google Scholar] [CrossRef]
- Polen, B.; Pendyala, B.; Patras, A.; D’Souza, D.H. Inactivation of Hepatitis A Virus and Feline Calicivirus on Model Food Contact Surfaces by Ultraviolet Light (UV-C) Systems. Foods 2024, 13, 2892. [Google Scholar] [CrossRef]
- Hadi, J.; Dunowska, M.; Wu, S.; Brightwell, G. Control Measures for SARS-CoV-2: A Review on Light-Based Inactivation of Single-Stranded RNA Viruses. Pathogens 2020, 9, 737. [Google Scholar] [CrossRef]
- Tseng, C.C.; Li, C.S. Inactivation of virus-containing aerosols by ultraviolet germicidal irradiation. Aerosol Sci. Technol. 2005, 39, 1136–1142. [Google Scholar] [CrossRef]
- Liang, J.J.; Liao, C.C.; Chang, C.S.; Lee, C.Y.; Chen, S.Y.; Huang, S.B.; Lu, K.M. The effectiveness of far-ultraviolet (UVC) light prototype devices with different wavelengths on disinfecting SARS-CoV-2. Appl. Sci. 2021, 11, 10661. [Google Scholar] [CrossRef]
- Joshi, S.S.; Dice, L.; Ailavadi, S.; D’Souza, D.H. Antiviral Effects of Quillaja saponaria Extracts Against Human Noroviral Surrogates. Food. Environ. Virol. 2023, 15, 167–175. [Google Scholar] [CrossRef]
- Choi, J.M.; D’Souza, D.H. Inactivation of Tulane virus and feline calicivirus by aqueous ozone. J. Food Sci. 2023, 88, 4218–4229. [Google Scholar] [CrossRef]
- Sharma, A.; Mahmoud, H.; Pendyala, B.; Balamurugan, S.; Patras, A. UV-C inactivation of microorganisms in droplets on food contact surfaces using UV-C light-emitting diode devices. Front. Food Sci. Technol. 2023, 3, 1182765. [Google Scholar] [CrossRef]
- Baldelli, G.; Aliano, M.P.; Amagliani, G.; Magnani, M.; Brandi, G.; Pennino, C.; Schiavano, G.F. Airborne microorganism inactivation by a UV-C LED and ionizer-based continuous sanitation air (CSA) system in train environments. Int. J. Environ. 2022, 19, 1559. [Google Scholar] [CrossRef] [PubMed]
- Balamurugan, S.; Zaidi, M.; Arvaj, L.; Pendyala, B.; Gabriel, M.; Farber, J.M.; Sasges, M.; Patras, A. Modeling the UV-C Inactivation Kinetics and Determination of Fluence Required for Incremental Inactivation of Cronobacter spp. J. Food Prot. 2022, 85, 1625–1634. [Google Scholar] [CrossRef] [PubMed]
- Bozkurt, H.; D’Souza, D.H.; Davidson, P.M. Thermal Inactivation Kinetics of Human Norovirus Surrogates and Hepatitis A Virus in Turkey Deli Meat. Appl. Environ. Microbiol. 2015, 81, 4850–4859. [Google Scholar] [CrossRef]
- Nunayon, S.S.; Wang, M.; Zhang, H.H.; Lai, A.C. Evaluating the efficacy of a rotating upper-room UVC-LED irradiation device in inactivating aerosolized Escherichia coli under different disinfection ranges, air mixing, and irradiation conditions. J. Hazard. Mater. 2022, 440, 129791. [Google Scholar] [CrossRef] [PubMed]
- Kim, D.K.; Kang, D.H. UVC LED Irradiation Effectively Inactivates Aerosolized Viruses, Bacteria, and Fungi in a Chamber-Type Air Disinfection System. Appl. Environ. Microbiol. 2018, 84, 00918–00944. [Google Scholar] [CrossRef]
- McDevitt, J.J.; Rudnick, S.N.; Radonovich, L.J. Aerosol susceptibility of influenza virus to UV-C light. Appl. Environ. Microbiol. 2012, 78, 1666–1669. [Google Scholar] [CrossRef]
- Biasin, M.; Bianco, A.; Pareschi, G.; Cavalleri, A.; Cavatorta, C.; Fenizia, C.; Clerici, M. UV-C irradiation is highly effective in inactivating SARS-CoV-2 replication. Sci. Rep. 2021, 11, 6260. [Google Scholar]
- Inagaki, H.; Saito, A.; Sugiyama, H.; Okabayashi, T.; Fujimoto, S. Rapid inactivation of SARS-CoV-2 with deep-UV LED irradiation. Emerg. Microbes Infect. 2020, 9, 1744–1747. [Google Scholar] [CrossRef]
- Jureka, A.S.; Williams, C.G.; Basler, C.F. Pulsed broad-spectrum UV light effectively inactivates SARS-CoV-2 on multiple surfaces and N95 material. Viruses 2021, 13, 460. [Google Scholar] [CrossRef]
- Fischer, R.J.; Port, J.R.; Holbrook, M.G.; Yinda, K.C.; Creusen, M.; Ter Stege, J.; Munster, V.J. UV-C light completely blocks aerosol transmission of highly contagious SARS-CoV-2 variants WA1 and Delta in hamsters. Environ. Sci. Technol. 2022, 56, 12424–12430. [Google Scholar] [CrossRef] [PubMed]
- Wanguyun, A.P.; Oishi, W.; Sano, D. Sensitivity Evaluation of Enveloped and Non-enveloped Viruses to Ethanol Using Machine Learning: A Systematic Review. Food Environ. Virol. 2024, 16, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Wassenaar, T.M.; Jun, S.; Robeson, M.; Ussery, D.W. Comparative genomics of hepatitis A virus, hepatitis C virus, and hepatitis E virus provides insights into the evolutionary history of Hepatovirus species. Microbiologyopen 2020, 2, 973. [Google Scholar] [CrossRef] [PubMed]
- Probst, C.; Jecht, M.; Gauss-Müller, V. Intrinsic signals for the assembly of hepatitis A virus particles: Role of structural proteins VP4 and 2A. J. Biol. Chem. 1999, 274, 4527–4531. [Google Scholar] [CrossRef]
- Guo, K.; Chen, C. Investigation of Far-UVC (222 nm) disinfection of bioaerosols deposited on surfaces with different material properties. J. Hazard. Mater. 2024, 465, 133358. [Google Scholar] [CrossRef]

| UV-C LED 255 nm | UV-C LED 279 nm | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Linear | Weibull | Linear | Weibull | |||||||
| HAV | D10-Value | R2 | δ | p | R2 | D10-Value | R2 | δ | p | R2 |
| SS | 47.39 ± 7.40 Ba | 0.94 | 29.69 ± 5.49 Ba | 0.58 | 0.99 | 6.60 ± 0.27 Aa | 0.98 | 6.67 ± 0.63 Aa | 1.04 | 0.98 |
| glass | 40.0 ± 2.94 Ba | 0.91 | 35.25 ± 15.01 Ba | 0.86 | 0.92 | 5.57 ± 0.74 Aa | 0.94 | 5.21 ± 1.25 Aa | 0.88 | 0.95 |
| Time (min) | 255 nm UV-C LED Dose (mJ/cm2) | 255 nm UV-C LED Reduction (log PFU/mL) | 279 nm UV-C LED Dose (mJ/cm2) | 279 nm UV-C LED Reduction (log PFU/mL) |
|---|---|---|---|---|
| 0 | 0 | 0 A | 0 | 0 A |
| 0.25 | 12.75 | 0.53 ± 0.22 A | 1.35 | 0.01 ± 0.15 A |
| 0.5 | 25.5 | 1.02 ± 0.04 B | 2.7 | 0.41 ± 0.15 B |
| 1.0 | 51.0 | 1.32 ± 0.04 C | 5.4 | 0.78 ± 0.03 C |
| 1.25 | 63.75 | 1.5 ± 0.02 CD | 6.75 | 0.98 ± 0.10 CD |
| 1.5 | 76.5 | 1.76 ± 0.05 D | 8.1 | 1.14 ± 0.09 D |
| Time (min) | 255 nm UV-C LED Dose (mJ/cm2) | 255 nm UV-C LED Reduction (log PFU/mL) | 279 nm UV-C LED Dose (mJ/cm2) | 279 nm UV-C LED Reduction (log PFU/mL) |
|---|---|---|---|---|
| 0 | 0 | 0 A | 0 | 0 A |
| 0.25 | 12.75 | 0.04 ± 0.05 A | 1.35 | 0.05 ± 0.15 A |
| 0.5 | 25.5 | 0.97 ± 0.03 B | 2.7 | 0.62 ± 0.15 B |
| 1.0 | 51.0 | 1.16 ± 0.08 B | 5.4 | 0.98 ± 0.03 BC |
| 1.25 | 63.75 | 1.79 ± 0.07 C | 6.75 | 1.34 ± 0.10 C |
| 1.5 | 76.5 | 1.75 ± 0.07 C | 8.1 | 1.29 ± 0.09 C |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polen, B.; Patras, A.; Pendyala, B.; D’Souza, D.H. Inactivation of Aerosolized Hepatitis A Viral Droplets on Food Contact Surfaces by Ultraviolet-Light-Emitting Diodes at 255 nm and 279 nm. Foods 2025, 14, 1899. https://doi.org/10.3390/foods14111899
Polen B, Patras A, Pendyala B, D’Souza DH. Inactivation of Aerosolized Hepatitis A Viral Droplets on Food Contact Surfaces by Ultraviolet-Light-Emitting Diodes at 255 nm and 279 nm. Foods. 2025; 14(11):1899. https://doi.org/10.3390/foods14111899
Chicago/Turabian StylePolen, Breanna, Ankit Patras, Brahmaiah Pendyala, and Doris H. D’Souza. 2025. "Inactivation of Aerosolized Hepatitis A Viral Droplets on Food Contact Surfaces by Ultraviolet-Light-Emitting Diodes at 255 nm and 279 nm" Foods 14, no. 11: 1899. https://doi.org/10.3390/foods14111899
APA StylePolen, B., Patras, A., Pendyala, B., & D’Souza, D. H. (2025). Inactivation of Aerosolized Hepatitis A Viral Droplets on Food Contact Surfaces by Ultraviolet-Light-Emitting Diodes at 255 nm and 279 nm. Foods, 14(11), 1899. https://doi.org/10.3390/foods14111899






