Aloe vera―An Extensive Review Focused on Recent Studies
Abstract
1. Introduction
2. Aloe vera Mill
3. Pharmacological Activities
3.1. Aloe vera Anti-Inflammatory Activity
3.2. Aloe vera Antioxidant Activity
3.3. Aloe vera Antibacterial Activity
| Activity | Ref. | ||
|---|---|---|---|
| Anti-inflammatory activity | [70] | ||
| In vitro against human glioblastoma/astrocytoma cells (U373 MG) | NF-κB phosphorylation inhibition | ||
| In vivo on Wistar albino rats | Lysosomal membrane stabilization; downregulation of TNF-α and COX-2 gene expression | [71] | |
| In vitro evaluation of protein denaturation and stabilization of RBC membrane In vivo by rat paw edema model | In vitro: IC50 = 218.9 ± 15.6 μg/mL (protein denaturation); IC50 = 275.9 ± 19.1 μg/mL (stabilization of RBC membrane) In vivo: AST and ALT levels decreased by around 44.5% and 41.8%, respectively | [72] | |
| Antioxidant activity | |||
| In vitro reducing power and DPPH radical scavenging activity | EC50 = 249,316 µg/mL: reducing power activity (methanol extract); IC50 = 54.0 µg/mL in DPPH assay (aqueous extract) | [3] | |
| Antimicrobial activity | |||
| In vitro activity against Gram-positive and Gram-negative bacteria | Ethanol extract: IZD = 23.33 mm (B. cereus) IZD = 22.33 mm (S. pyogenes) IZD = 23.00 mm (P. aeruginosa) IZD = 22.66 mm (K. pneumoniae) Methanol extract: IZD = 22.33 mm (B. cereus) IZD = 15.00 mm (S. pyogenes) IZD = 10.66 mm (P. aeruginosa) IZD = 14.00 mm (K. pneumoniae) | [80] | |
| In vitro studies against M. tuberculosis H37Rv strains (ATCC 27294) | AV = 50 μg/mL ETH = 6.25 μg/mL AV + ETH = 12.5 μg/mL PAS: 3.12 μg/mL = AV + PAS: 25 μg/mL AV + ETH + PAS = 12.5 μg/mL | [84] | |
| In vitro studies against MRSA | 3-hydroxy-1-(1,7-dihydroxy-3,6-dimethoxynaphthalen-2-yl)-propan-1-one obtained from AV: MIC90 = 48 ± 4 mg/L | [91] | |
| In vitro studies against fungi and bacteria | Aqueous extract Fungi: IZD = 0.33 ± 0.12 mm (A. chevalieri) IZD = 0.27 ± 0.06 mm (T. funiculosus) IZD = 0.57 ± 0.40 mm (P. funiculosum) Bacteria: IZD = 0.47 ± 0.25 mm (Shigella sp.) Ethanolic extract Fungi: IZD = 1.00 ± 0.50 mm (A. chevalieri) IZD = 0.13 ± 0.12 mm (T. funiculosus) IZD = 0.20 ± 0.10 mm (P. funiculosum) Bacteria: IZD = 0.17 ± 0.06 mm (Shigella sp.) | [92] |
3.4. Aloe vera Antifungal Activity
3.5. Aloe vera Antiparasitic Activity
3.6. Aloe vera Antiviral Activity
3.7. Aloe vera Immunomodulatory Activity
3.8. Aloe vera Anticancer Activity
3.9. Aloe vera Radioprotective Effects
3.10. Aloe vera and Hepatoprotection and Renoprotection
3.11. Cardioprotective Effects of Aloe vera
3.12. Aloe vera and Skin Disorders
| Activity | Ref. | ||
|---|---|---|---|
| Wound healing | In vivo studies in Rattus norvegicus Wistar strain rats | AV quickened the healing process in second-degree burn wounds | [173] |
| In vivo acceleration of wound healing after topical application of AV gel in Wistar rats | AV increased fibroblasts and TGF-β gene expression | [175] | |
| Comparison of burn healing outcomes between silver sulfadiazine and AV in second- and third-degree burn wounds in both animals and humans | Time to healing benefitted those burns on which AV was used | [176] | |
| In vivo induced deep second-degree burns in adult female albino rats | Topical AV promoted burn wound healing, with wounds healing faster and better than with intradermal injection of mesenchymal stem cells | [177] | |
| In vivo studies in deep second-degree burn wound healing in male Sprague Dawley rats | Both oral and topical applications of AV demonstrated beneficial effects by boosting the growth factors and antioxidant status of skin tissue | [178] | |
| In vitro scratch assay in wound healing using HaCaTs and HDFs; the expression of Nrf2 and its associated genes was also analyzed by quantitative RT-PCR | The extracellular vesicles isolated from AV peels activated the antioxidant mechanisms and wound-healing process via Nrf2 activation and enhanced the migration ability of HaCaTs and HDFs | [180] | |
| Acne vulgaris | Randomized, double-blind, prospective trial | Combination of topical AV and tretinoin greatly improved mild to moderate acne vulgaris with respect to tretinoin and placebo | [187] |
| In vitro assay against P. acnes by the agar diffusion method | AV’s antibacterial activity against P. acnes: IZD = 8.8. mm (at 2.5% concentration) IZD = 9.8 mm (at 5% concentration) IZD = 12.9 mm (at 10% concentration) | [188] | |
| Alopecia areata | In vitro drug release study for the prevention of microbial growth at the scalp during the treatment of alopecia areata | Topical AV gel loaded with finasteride–garlic oil–NTFS provided sustained and targeted drug delivery with increased encapsulation efficiency, nontoxicity, non-irritancy, and significant inhibition of the microbial zone of the said bacterial colony and more effectively treated the alopecia areata | [192] |
| Psoriasis | In vitro studies in human keratinocyte cell line HaCaTs using the CCK-8 assay; ELISA and Western blotting used to study the abundance of IL-8 and IL-12 in TNF-α-incubated culture medium and APS-treated HaCaT cells, respectively | APS significantly diminished TNF-α-stimulated HaCaT cell proliferation dose-dependently; it also increased the expression levels of IL-8-12 in response to TNF-α | [195] |
| Frostbite | In vitro and in vivo experiments and clinical trials using AV preparations | “Dermaide” Aloe cream (AV gel) is a topical inhibitor of thromboxane and reverses progressive ischemia and preserves the dermal microcirculation of cells | [201] |
3.13. Aloe vera in Gastrointestinal Disorders
3.14. Aloe vera in Metabolic, Neurological, and Endocrine Diseases
3.15. Prebiotic and Probiotic Effects of Involvement of Aloe vera with the Gut Microbiota
3.16. Aloe vera Activity in Dentistry and Oral Cavity Disorders
4. Aloe vera in Cosmetics and Sanitizers
5. Aloe vera as a Preservative for Foods
6. Composition of Aloe vera and Studies on the Single Components (Commercially Available)
6.1. Anthraquinones and Anthrones
6.1.1. Aloe-Emodin
6.1.2. Emodin
6.1.3. Aloin
6.1.4. Rhein
| Cancer Type | Cell Lines | Aloin Activity | Ref. |
|---|---|---|---|
| Oral Squamous Cell Carcinoma (OSCC) | CAL-27 | Promotes apoptosis and autophagy downregulation of p62 protein expression; upregulates Beclin-1 and LC3-I/LC3-II protein expression; blocks AKT/mTOR pathway activation | [353] |
| Gastric Cancer | HGC-27 | Induces apoptosis by downregulating expressions of High Mobility Group Box 1 (HMGB1) and RAGE, inhibiting HMGB1 release, and suppressing rhHMGB1-induced activation of AKT/mTOR-P70S6K and ERK-P90RSK-CREB signaling pathways | [354] |
| Gastric Cancer | HGC-27 and BGC-823 | Inhibits the proliferation and migration of gastric cancer cells by regulating NOX2-ROS-mediated pro-survival signal pathways | [355] |
| Gastric Cancer | NCI-N87 | Induces cell apoptosis and regulates the PI3K/AKT signaling pathway | [356] |
| Gastric Cancer | MGC-803 | Promotes apoptosis through the miR-5683/HMGB1 axis | [357] |
| Breast Cancer | T47D (estrogen receptor-positive) and MDA-MB-231 (triple negative) | Autophagy suggested as one of the mechanistic modes of aloin cytotoxicity through genetic mutations in p53 | [358] |
| Melanoma | A375 | Promotes cell apoptosis by downregulating HMGB1 expression at the transcriptional level, preventing its translocation to the cytoplasm and interaction with TLR4, which indeed blocks HMGB1-mediated ERK activation | [360] |
| Hepatocellular Carcinoma | HepG2 and Bel-7402 | In association with metformin: —increased antiproliferative effect via PI3K/AKT/mTOR-mediated apoptosis and autophagy —enhanced the expression of Beclin-1, LC3-II, and ATG8 and downregulated P62 | [361] |
| Colorectal Cancer | LoVo, SW620, and Caco2 (in vitro); six-week-old male NU/NU nude mice (in vivo) | In combination with CPT-11: —enhanced the antitumor activity of CPT-11 —reduced cell viability and induced apoptosis, both in vitro and in vivo —upregulated miRNA-133b and downregulated the IGF1R and its downstream MEK/ERK and PI3K/AKT/mTOR pathways | [362] |
6.1.5. Chrysophanol
6.2. Glycosides
6.2.1. Glycosylated Chromones
Aloesin
Aloeresin A
6.2.2. Glycosylated Pyran-2-Ones
6.3. Coumarins and Isocoumarins
6.4. Aloe vera Polysaccharides (APs)
Acemannan
7. Studies on Nanoparticles, Phytosomes, and Liposomes Containing Aloe vera
8. Metabolism of Aloe vera
9. Valorization
10. Toxicity Concerns of Aloe vera
11. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Sánchez-Machado, D.I.; López-Cervantes, J.; Sendón, R.; Sanches-Silva, A. Aloe vera: Ancient Knowledge with New Frontiers. Trends Food Sci. Technol. 2017, 61, 94–102. [Google Scholar] [CrossRef]
- Martínez-Burgos, W.J.; Serra, J.L.; Marsiglia, F.R.M.; Montoya, P.; Sarmiento-Vásquez, Z.; Marin, O.; Gallego-Cartagena, E.; Paternina-Arboleda, C.D. Aloe vera: From Ancient Knowledge to the Patent and Innovation Landscape—A review. S. Afr. J. Bot. 2022, 147, 993–1006. [Google Scholar] [CrossRef]
- Manye, S.J.; Saleh, J.S.; Ishaya, H.B.; Chiroma, S.M.; Attah, M.O.O.; Dibal, N.I. Phytochemical Screening and in-vitro Antioxidant Activities of Aqueous and Methanol Extracts of Aloe vera. Pharmacol. Research-Modern Chin. Med. 2023, 8, 100291. [Google Scholar] [CrossRef]
- Wagan, M.A.; Miano, T.F.; Nizamani, B.; Shar, H.A.; Wagan, M.K.; Wagan, F.A. Influence of Sunlight on Growth and Yield of Aloe vera Plant. Am. J. Biosci. Bioeng. 2022, 10, 84–88. [Google Scholar]
- Soni, S.; Noor, U.; Amiri, E.; Gupta, E. Novel Importance of Herbs and Their Effects on Human Health. In Immune-Boosting Nutraceuticals for Better Human Health; Apple Academic Press: Palm Bay, FL, USA, 2024; pp. 29–46. ISBN 9781003371069. [Google Scholar]
- Khan, A.H. Aloe vera (Aloe barbadensis Miller) and Its Natural Ingredients: A Mini Review. Phytopharmacol. Res. J. 2022, 1, 49–55. [Google Scholar]
- Kumar, R.; Singh, A.K.; Gupta, A.; Bishayee, A.; Pandey, A.K. Therapeutic potential of Aloe vera—A Miracle Gift of Nature. Phytomedicine 2019, 60, 152996. [Google Scholar] [CrossRef] [PubMed]
- Maenthaisong, R.; Chaiyakunapruk, N.; Niruntraporn, S.; Kongkaew, C. The Efficacy of Aloe vera Used for Burn Wound Healing: A Systematic Review. Burns 2007, 33, 713–718. [Google Scholar] [CrossRef] [PubMed]
- Akram, M.; Thiruvengadam, M.; Zainab, R.; Daniyal, M.; Bankole, M.M.; Rebezov, M.; Sharaiati, M.A.; Okuskhanova, E. Herbal medicine for the management of laxative activity. Curr. Pharm. Biotechnol. 2022, 23, 1269–1283. [Google Scholar] [CrossRef] [PubMed]
- Riaz, S.; Hussain, S.; Syed, S.K.; Anwar, R. Chemical Characteristics and Therapeutic Potentials of Aloe vera. RADS J. Biol. Res. Appl. Sci. 2021, 12, 160–166. [Google Scholar]
- Arora, R.; Babbar, R.; Kaur, R.; Rana, P. An Insight into the Potential of Natural Products as Anti-inflammatory Agents: A Systematic Review. In Manufacturing Technologies and Production Systems; CRC Press: Boca Raton, FL, USA, 2024; pp. 152–162. ISBN 9781003367161. [Google Scholar]
- Rengasamy, K.R.; Mahomoodally, M.F.; Joaheer, T.; Zhang, Y. A Systematic Review of Traditionally Used Herbs and Animal-derived Products as Potential Analgesics. Curr. Neuropharmacol. 2021, 19, 553–588. [Google Scholar] [CrossRef]
- Budai, M.M.; Varga, A.; Milesz, S.; Tozser, J.; Benko, S. Aloe vera Downregulates LPS-induced Inflammatory Cytokine Production and Expression of NLRP3 Inflammasome in Human Macrophages. Mol. Immunol. 2013, 56, 471–479. [Google Scholar] [CrossRef] [PubMed]
- Hęś, M.; Dziedzic, K.; Górecka, D.; Jędrusek-Golińska, A.; Gujska, E. Aloe vera (L.) Webb.: Natural sources of antioxidants—A review. Plant. Foods Hum. Nutr. 2019, 74, 255–265. [Google Scholar] [CrossRef] [PubMed]
- Inyang, M.; Ofem, O.E. Acute and Chronic Aloe barbadensis Miller gel mediates antiulcerogenic and Gastric Anti-secretory Effects Via Histaminergic H2 Receptors. Eur. J. Biomed. Pharm. Sci. 2016, 3, 107–111. [Google Scholar]
- Danish, P.; Ali, Q.; Hafeez, M.; Malik, A. Antifungal and Antibacterial Activity of Aloe vera Plant Extract. Biol. Clin. Sci. Res. J. 2020, 4, 1–8. [Google Scholar] [CrossRef]
- Gao, Y.; Kuok, K.I.; Jin, Y.; Wang, R. Biomedical Applications of Aloe vera. Crit. Rev. Food Sci. Nutr. 2019, 59, S244–S256. [Google Scholar] [CrossRef] [PubMed]
- Erhabor, J.O.; Idu, M. Aphrodisiac Potentials of the Ethanol Extract of Aloe barbadensis Mill. Root in Male Wistar Rats. BMC Compl. Altern. Med. 2017, 17, 360. [Google Scholar] [CrossRef] [PubMed]
- Catalano, A. COVID-19: Could Irisin Become the Handyman Myokine of the 21st Century? Coronaviruses 2020, 1, 32–41. [Google Scholar] [CrossRef]
- Sabbaghzadegan, S.; Golsorkhi, H.; Soltani, M.H.; Kamalinejad, M.; Bahrami, M.; Kabir, A.; Dadmehr, M. Potential Protective Effects of Aloe vera Gel on Cardiovascular Diseases: A Mini-review. Phytother. Res. 2021, 35, 6101–6113. [Google Scholar] [CrossRef] [PubMed]
- Sajjad, A.; Subhani Sajjad, S. Aloe vera: An Ancient Herb for Modern Dentistry—A Literature Review. J. Dent. Surg. 2014, 2014, 210463. [Google Scholar] [CrossRef]
- Pentapati, K.C.; Siddiq, H.; Abhinav, T.N. Aloe vera and Oral Health: A Systematic Review. Pharmacol. Studies Nat. Oral Care 2023, in press. [Google Scholar] [CrossRef]
- Poorkazemi, D.; Shafaroudi, A.M.; Nasiri, P.; Aarabi, M.; Sabet, J.M. Evaluation of Aloe vera as a Natural Pharmaceutic in Mouthwashes: A Narrative Review. Jundish. J. Nat. Pharm. Prod. 2022, 17, e122155. [Google Scholar] [CrossRef]
- Duane, B.; Yap, T.; Neelakantan, P.; Anthonappa, R.; Bescos, R.; McGrath, C.; McCullough, M.; Brookes, Z. Mouthwashes: Alternatives and Future Directions. Int. Dent. J. 2023, 73, S89–S97. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Bansal, K.; Bajpai, M. The Role of Different Medicinal Herbs in Treatment of Polycystic Ovary Syndrome: A Review. Nat. Prod. J. 2024, 14, 68–76. [Google Scholar] [CrossRef]
- Nagi, R.; Patil, D.J.; Rakesh, N.; Jain, S.; Sahu, S. Natural Agents in the Management of Oral Mucositis in Cancer Patients-systematic Review. J. Oral Biol. Craniofac. Res. 2018, 8, 245–254. [Google Scholar] [CrossRef] [PubMed]
- Mahboubi, M. Aloe vera (Aloe barbadensis) Usage in the Middle East: Applications for Gastroesophageal Reflux. In Ancient and Traditional Foods, Plants, Herbs and Spices used in the Middle East; CRC Press: Boca Raton, FL, USA, 2023; pp. 105–115. ISBN 9781003243472. [Google Scholar]
- Sousa, H.M.P.; Dias, J.O.D.S.B.; de Queiroz, P.V.A.; de Sousa Sá, W.R.; de Azevedo Sousa, W.L.; Sousa, I.J.O. Aplicação da Aloe vera l. No Tratamento de Gastrite. Res. Soc. Dev. 2022, 11, e53011730316. [Google Scholar] [CrossRef]
- Maiuolo, J.; Musolino, V.; Gliozzi, M.; Carresi, C.; Scarano, F.; Nucera, S.; Scicchitano, M.; Oppedisano, F.; Bosco, F.; Macri, R.; et al. Involvement of the Intestinal Microbiota in the Appearance of Multiple Sclerosis: Aloe vera and Citrus bergamia as Potential Candidates for Intestinal Health. Nutrients 2022, 14, 2711. [Google Scholar] [CrossRef] [PubMed]
- Alesci, A.; Lauriano, E.R.; Fumia, A.; Irrera, N.; Mastrantonio, E.; Vaccaro, M.; Gangemi, S.; Santini, A.; Cicero, N.; Pergolizzi, S. Relationship between Immune Cells, Depression, Stress, and Psoriasis: Could the Use of Natural Products Be Helpful? Molecules 2022, 27, 1953. [Google Scholar] [CrossRef] [PubMed]
- Al-Salman, N.T.S.; Al-Gharawi, J.K. The Effect of Locally Extracted Aloe vera Oil on the Productive Performance of ISA Brown Laying Hens. IOP Conf. Ser. Earth Environ. Sci. 2023, 1225, 012041. [Google Scholar] [CrossRef]
- Zolghadri, S.; Bahrami, A.; Hassan Khan, M.T.; Munoz-Munoz, J.; Garcia-Molina, F.; Garcia-Canovas, F.; Saboury, A.A. A Comprehensive Review on Tyrosinase Inhibitors. J. Enzym. Inhib. Med. Chem. 2019, 34, 279–309. [Google Scholar] [CrossRef]
- Svitina, H.; Swanepoel, R.; Rossouw, J.; Netshimbupfe, H.; Gouws, C.; Hamman, J. Treatment of skin disorders with aloe materials. Curr. Pharm. Des. 2019, 25, 2208–2240. [Google Scholar] [CrossRef]
- Genesi, B.P.; de Melo Barbosa, R.; Severino, P.; Rodas, A.C.D.; Yoshida, C.M.P.; Mathor, M.B.; Lopes, P.S.; Viseras, C.; Souto, E.B.; da Silva, C.F. Aloe vera and Copaiba Oleoresin-loaded Chitosan Films for Wound Dressings: Microbial Permeation, Cytotoxicity, and in vivo Proof of Concept. Int. J. Pharm. 2023, 634, 122648. [Google Scholar] [CrossRef] [PubMed]
- Hattingh, A.; Laux, J.-P.; Willers, C.; Hamman, J.; Steyn, D.; Hamman, H. In Vitro Wound Healing Effects of Combinations of Aloe vera Gel with Different Extracts of Bulbine frutescens. S. Afr. J. Bot. 2023, 158, 254–264. [Google Scholar] [CrossRef]
- ValizadehKaji, B.; Fakhri, N. Postharvest Application of Aloe vera Gel and Thymol Enhances Shelf-life of Duke Cherries via Altering Physiochemical Parameters. Chem. Biol. Technol. Agricult. 2023, 10, 85. [Google Scholar] [CrossRef]
- Harahap, Y.E.; Tanjung, I.F.; Shaharani, A.; Syahfitri, W.W. Growth Response of Tomato (Solanum lycopersicum) to the Combination of Aloe vera and Tauge (Flammulina velutipes) Extract. Biofarm J. Ilm. Pert. 2023, 19, 1–6. [Google Scholar] [CrossRef]
- Sahoo, D.K.; Jena, S.; Mohanty, P.; Biswal, H.S.; Gowd, K.H. Probing the Photostability of Avobenzone with N-acetylcysteine Using UV Spectroscopy, Computational Studies and Integration into Aloe vera Gel. J. Photochem. Photobiol. A 2024, 447, 115196. [Google Scholar] [CrossRef]
- Laux, A.; Gouws, C.; Hamman, J.H. Aloe vera Gel and Whole Leaf Extract: Functional and Versatile Excipients for Drug Delivery? Expert Opin. Drug Deliv. 2019, 16, 1283–1285. [Google Scholar] [CrossRef] [PubMed]
- Gerber, W.; Steyn, D.; Kotzé, A.; Svitina, H.; Weldon, C.; Hamman, J. Permeation enhancement Effects of Leaf Materials from Different Aloe Species on In Vitro and Ex Vivo Nasal Epithelial Models. J. Herbmed Pharmacol. 2020, 9, 355–365. [Google Scholar] [CrossRef]
- Kirby-Smith, C.; Steenekamp, J.; Steyn, D.; Haasbroek-Pheiffer, A.; Hamman, H.; Hamman, J. Intranasal Insulin Delivery: Microparticle Formulations Consisting of Aloe vera Polysaccharides for Advanced Delivery across Excised Olfactory and Respiratory Nasal Epithelial Tissues. Appl. Sci. 2023, 13, 4822. [Google Scholar] [CrossRef]
- Javed, S. Aloe vera Gel in Food, Health Products, and Cosmetics Industry. Studies Nat. Prod. Chem. 2014, 41, 261–285. [Google Scholar] [CrossRef]
- Wijesundara, W.M.A.S.; Adikari, A.M.J.B. Development of Aloe vera (Aloe barbadensis Miller) Incorporated Drinking Yoghurt. Int. J. Sci. Res. Publ. 2017, 7, 334–342. [Google Scholar]
- Kahramanoğlu, İ.; Chen, C.; Chen, J.; Wan, C. Chemical Constituents, Antimicrobial Activity, and Food Preservative Characteristics of Aloe vera Gel. Agronomy 2019, 9, 831. [Google Scholar] [CrossRef]
- Kumar, S.; Kalita, S.; Das, A.; Kumar, P.; Singh, S.; Katiyar, V.; Mukherjee, A. Aloe vera: A Contemporary Overview on Scope and Prospects in Food Preservation and Packaging. Prog. Org. Coat. 2022, 166, 106799. [Google Scholar] [CrossRef]
- Khan, R.U.; Naz, S.; De Marzo, D.; Dimuccio, M.M.; Bozzo, G.; Tufarelli, V.; Losacco, C.; Ragni, M. Aloe vera: A Sustainable Green Alternative to Exclude Antibiotics in Modern Poultry Production. Antibiotics 2023, 12, 44. [Google Scholar] [CrossRef] [PubMed]
- Bachheti, A.; Bachheti, R.K.; Abate, L.; Husen, A. Current Status of Aloe-based Nanoparticle Fabrication, Characterization and Their Application in Some Cutting-Edge Areas. S. Afr. J. Bot. 2022, 147, 1058–1069. [Google Scholar] [CrossRef]
- Farooq, A.; Niaz, B.; Saeed, F.; Afzaal, M.; Armghan Khalid, M.; Raza, M.A.; Al Jbawi, E. Exploring the Potential of Aloe vera Gel-based Coating for Shelf Life Extension and Quality Preservation of Tomato. Int. J. Food Prop. 2023, 26, 2909–2923. [Google Scholar] [CrossRef]
- Jithendra, P.; Annamalai, D.; Ebrahim, H.A.; Ibrahim, A.M.; El-Sherbiny, M.; Rajam, A.M.; EL-Nablaway, M.; Mohamed, J.M.M. Bioassessment of the Inflammatory Response of Macrophages to Collagen-chitosan Scaffold Blended with Aloe vera. Biomass Convers. Biorefin. 2023; in press. [Google Scholar] [CrossRef]
- De Matteis, V.; Cascione, M.; Costa, D.; Martano, S.; Manno, D.; Cannavale, A.; Mazzotta, S.; Paladini, F.; Martino, M.; Rinaldi, R. Aloe vera Silver Nanoparticles Addition in Chitosan Films: Improvement of Physicochemical Properties for Eco-friendly Food Packaging Material. J. Mater. Res. Technol. 2023, 24, 1015–1033. [Google Scholar] [CrossRef]
- Singha, P.S.; Ghosh, R.; Firdaus, S.B.; Ghosh, D. Effects of Biofertilizers in Improving the Growth and Development of the Traditional Medicinal Plant Aloe vera L. (Aloe barbadensis Miller). Curr. Tradit. Med. 2024, 10, 97–108. [Google Scholar] [CrossRef]
- Tanaka, M.; Yamada, M.; Toida, T.; Iwatsuki, K. Safety Evaluation of Supercritical Carbon Dioxide Extract of Aloe vera Gel. J. Food Sci. 2012, 77, T2–T9. [Google Scholar] [CrossRef] [PubMed]
- Sehgal, I.; Winters, W.D.; Scott, M.; David, A.; Gillis, G.; Stoufflet, T.; Nair, A.; Kousoulas, K. Toxicologic Assessment of a Commercial Decolorized Whole Leaf Aloe vera Juice, Lily of the Desert Filtered Whole Leaf Juice with Aloesorb. J. Toxicol. 2013, 2013, 802453. [Google Scholar] [CrossRef]
- Guo, X.; Mei, N. Aloe vera: A Review of Toxicity and Adverse Clinical Effects. J. Environ. Sci. Health C 2016, 34, 77–96. [Google Scholar] [CrossRef] [PubMed]
- Boudreau, M.D.; Mellick, P.W.; Olson, G.R.; Felton, R.P.; Thorn, B.T.; Beland, F.A. Clear Evidence of Carcinogenic Activity by a Whole-leaf Extract of Aloe barbadensis Miller (Aloe vera) in F344/n Rats. Toxicol. Sci. 2013, 131, 26–39. [Google Scholar] [CrossRef] [PubMed]
- Boudreau, M.D.; Mellick, P.W.; Olson, G.R.; Felton, R.P.; Thorn, B.T.; Beland, F.A. Toxicology and carcinogenesis studies of a nondecolorized [corrected] whole leaf extract of Aloe barbadensis Miller (Aloe vera) in F344/N rats and B6C3F1 mice (drinking water study). Natl. Toxicol. Program. Tech. Rep. Ser. 2013, 577, 1–266, Correction in Natl. Toxicol. Program. Tech. Rep. Ser. 2013, 577, 1. [Google Scholar] [PubMed]
- Bernstein, N.; Akram, M.; Yaniv-Bachrach, Z.; Daniyal, M. Is It Safe to Consume Traditional Medicinal Plants During Pregnancy? Phytother. Res. 2021, 35, 1908–1924. [Google Scholar] [CrossRef] [PubMed]
- Chopra, L. Photo-degradation of Dyes and Drugs Using Aloe vera Synthesized Zinc Oxide Nanoparticles—A Review. Mater. Today Proc. 2023, 72, 1613–1617. [Google Scholar] [CrossRef]
- Heng, H.C.; Zulfakar, M.H.; Ng, P.Y. Pharmaceutical Applications of Aloe vera. Indon. J. Pharm. 2018, 29, 101. [Google Scholar] [CrossRef]
- Gupta, A.; Rawat, S. Clinical Importance of Aloe vera. Res. J. Top. Cosmetic Sci. 2017, 8, 30–39. [Google Scholar] [CrossRef]
- Deshpande, G.; Shinde, P.; Patil, S.; Pawar, S.; Dhamdhere, P. Aloe vera Plant Diseases Detection. Int. J. Res. Eng. Sci. Manag. 2022, 5, 197–199. [Google Scholar]
- Giannakoudakis, D.A.; Hosseini-Bandegharaei, A.; Tsafrakidou, P.; Triantafyllidis, K.S.; Kornaros, M.; Anastopoulos, I. Aloe vera Waste Biomass-Based Adsorbents for the Removal of Aquatic Pollutants: A Review. J. Environ. Manag. 2018, 227, 354–364. [Google Scholar] [CrossRef]
- Jangra, A.; Sharma, G.; Sihag, S.; Chhokar, V. The Dark Side of Miracle Plant-Aloe vera: A review. Mol. Biol. Rep. 2022, 49, 5029–5040. [Google Scholar] [CrossRef] [PubMed]
- Jadhav, A.S.; Patil, O.A.; Kadam, S.V.; Bhutkar, M.A. Review on Aloe vera is Used in Medicinal Plant. Asian J. Res. Pharm. Sci. 2020, 10, 26–30. [Google Scholar] [CrossRef]
- Maan, A.A.; Nazir, A.; Khan, M.K.I.; Ahmad, T.; Zia, R.; Murid, M.; Abrar, M. The Therapeutic Properties and Applications of Aloe vera: A review. J. Herb. Med. 2018, 12, 1–10. [Google Scholar] [CrossRef]
- Kumar, S.; Yadav, J.P. Ethnobotanical and Pharmacological Properties of Aloe vera: A Review. J. Med. Plants Res. 2014, 48, 1387–1398. [Google Scholar]
- Surjushe, A.; Vasani, R.; Saple, D.G. Aloe vera: A short review. Ind. J. Dermatol. 2008, 53, 163. [Google Scholar] [CrossRef] [PubMed]
- Sharma, P.; Kharkwal, A.C.; Kharkwal, H.; Abdin, M.Z.; Varma, A. A Review on pharmacological properties of Aloe vera. Int. J. Pharm. Sci. Rev. Res. 2014, 29, 31–37. [Google Scholar]
- Radha, M.H.; Laxmipriya, N.P. Evaluation of Biological Properties and Clinical Effectiveness of Aloe vera: A Systematic Review. J. Tradit. Complement. Med. 2015, 5, 21–26. [Google Scholar] [CrossRef] [PubMed]
- Tornero-Martínez, A.; Silva-Lucero, M.D.C.; Sampedro, E.C.; Ramón-Gallegos, E.; Pérez-Cruz, C.; Pérez-Grijalva, B.; Mora-Escobedo, R. Aloe vera and Fermented Extracts Exhibit an Anti-Inflammatory Effect on Human Glioblastoma/Astrocytoma U373 MG Cells. Plant Foods Hum. Nutr. 2022, 77, 37–43. [Google Scholar] [CrossRef] [PubMed]
- Paul, S.; Modak, D.; Chattaraj, S.; Nandi, D.; Sarkar, A.; Roy, J.; Chaudhuri, T.K.; Bhattacharjee, S. Aloe vera Gel Homogenate Shows Anti-inflammatory Activity through Lysosomal Membrane Stabilization and Downregulation of TNF-α and Cox-2 Gene Expressions in Inflammatory Arthritic Animals. Futur. J. Pharm. Sci. 2021, 7, 12. [Google Scholar] [CrossRef]
- Babu, S.; Noor, A. Aloe barbadensis Miller Peptide/Polypeptide Fraction Alleviates Inflammation through Inhibition of Proinflammatory Cytokines and Mediators in Vitro and in Rats with Freund’s Adjuvant-Induced Hind Paw Edema. Asian. Pac. J. Trop. Biomed. 2019, 9, 524. [Google Scholar] [CrossRef]
- Rauwald, H.W.; Maucher, R.; Dannhardt, G.; Kuchta, K. Dihydroisocoumarins, Naphthalenes, and Further Polyketides from Aloe vera and A. plicatilis: Isolation, Identification and their 5-LOX/COX-1 Inhibiting Potency. Molecules 2021, 26, 4223. [Google Scholar] [CrossRef]
- Peng, S.Y.; Norman, J.; Curtin, G.; Corrier, D.; McDaniel, H.R.; Busbee, D. Decreased Mortality of Norman Murine Sarcoma in Mice Treated with the Immunomodulator, Acemannan. Mol. Biother. 1991, 3, 79–87. [Google Scholar] [PubMed]
- Malek Hosseini, A.; Rostam Khani, M.; Abdi, S.; Abdi, S.; Sharifi, N. Comparison of Aloe vera Gel Dressing with Conventional Dressing on Pressure Ulcer Pain Reduction: A Clinical Trial. BMC Res. Notes 2024, 17, 25. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Xu, J.; Hu, Q. Evaluation of Antioxidant Potential of Aloe vera (Aloe barbadensis Miller) Extracts. J. Agric. Food Chem. 2003, 51, 7788–7791. [Google Scholar] [CrossRef] [PubMed]
- Nejatzadeh-Barandozi, F. Antibacterial activities and antioxidant capacity of Aloe vera. Org. Med. Chem. Lett. 2013, 3, 5. [Google Scholar] [CrossRef] [PubMed]
- Pop, R.M.; Puia, I.C.; Puia, A.; Chedea, V.S.; Levai, A.M.; Bocsan, I.C.; Buzoianu, A.D. Pot Aloe vera Gel–a Natural Source of Antioxidants. Not. Bot. Horti Agrobot. Cluj Napoca 2022, 50, 12732. [Google Scholar] [CrossRef]
- Neththrika, G.T.C.; Gunathilaka, M.D.T.L. Dillenia retusa (Godapara) and Aloe vera (Komarika) as a Promising Antimicrobial Agent Against Skin Infections: A Mini-Review. Sri Lankan J. Appl. Sci. 2023, 2, 5–15. Available online: https://sljoas.uwu.ac.lk/index.php/sljoas/article/view/63 (accessed on 10 January 2024).
- Lawrence, R.; Tripathi, P.; Jeyakumar, E. Isolation, Purification and Evaluation of Antibacterial Agents from Aloe vera. Braz. J. Microbiol. 2009, 40, 906–915. [Google Scholar] [CrossRef]
- Cellini, L.; Di Bartolomeo, S.; Di Campli, E.; Genovese, S.; Locatelli, M.; Di Giulio, M. In Vitro Activity of Aloe vera Inner Gel against Helicobacter pylori Strains. Lett. Appl. Microbiol. 2014, 59, 43–48. [Google Scholar] [CrossRef]
- Rawat, A.; Saxena, A. Short Review on Composition and Medicinal Applications of Aloe-vera. AIP Conf. Proc. 2023, 2735, 030007. [Google Scholar] [CrossRef]
- Yahya, R.; Al-Rajhi, A.M.H.; Alzaid, S.Z.; Al Abboud, M.A.; Almuhayawi, M.S.; Al Jaouni, S.K.; Selim, S.; Ismail, K.S.; Abdelghany, T.M. Molecular Docking and Efficacy of Aloe vera Gel Based on Chitosan Nanoparticles against Helicobacter pylori and Its Antioxidant and Anti-Inflammatory Activities. Polymers 2022, 14, 2994. [Google Scholar] [CrossRef]
- Azal, S.; Zodape, G.V. Effect of Aloe vera Extract and Second Line Anti-Tuberculosis Drugs on Mycobacterium Tuberculosis Strain-H37Rv. Saudi J. Med. Pharm. Sci. 2023, 9, 214–219. [Google Scholar] [CrossRef]
- Mawarti, H.; Rajin, M.; Khusniyah, Z.; Asumta, Z.; Wijayanti, C.D.W. Aloe vera and its Potency as Antituberculosis against Strains of Mycobacterium tuberculosis that Is Resistant to Some Tuberculosis Drugs. Bali Med. J. 2022, 11, 1879–1883. [Google Scholar] [CrossRef]
- Bhavani, G.D.; Rathod, T.; Parveen, N.; Tirupathi, P.; Dharavattu, P.; Sekhar, V.S.S.K.; Sharma, D.; Utkarsh, K. Assessment of the Antimicrobial Effectiveness of Herbal Root Canal Irrigants (Propolis, Triphala, and Aloe vera) and Chlorhexidine against Enterococcus faecalis. Cureus 2023, 15, e41628. [Google Scholar] [CrossRef]
- Pozzi, C.; Ferrari, S.; Cortesi, D.; Luciani, R.; Stroud, R.M.; Catalano, A.; Costi, M.P.; Mangani, S. The structure of Enterococcus faecalis Thymidylate Synthase Provides Clues about Folate Bacterial Metabolism. Acta Crystallogr. D Biol. Crystallogr. 2012, 68, 1232–1241. [Google Scholar] [CrossRef] [PubMed]
- Arsene, M.M.J.; Viktorovna, P.I.; Sergei, G.V.; Hajjar, F.; Vyacheslavovna, Y.N.; Vladimirovna, Z.A.; Aleksandrovna, V.E.; Nikolayevich, S.A.; Sachivkina, N. Phytochemical Analysis, Antibacterial and Antibiofilm Activities of Aloe vera Aqueous Extract against Selected Resistant Gram-Negative Bacteria Involved in Urinary Tract Infections. Fermentation 2022, 8, 626. [Google Scholar] [CrossRef]
- Ahmad, B.; Khan, M.I.; Naeem, M.A.; Alhodaib, A.; Fatima, M.; Amami, M.; Al-Abbad, E.A.; Kausar, A.; Alwadai, N.; Nazir, A.; et al. Green Synthesis of NiO Nanoparticles Using Aloe vera gel Extract and Evaluation of Antimicrobial Activity. Mater. Chem. Phys. 2022, 288, 126363. [Google Scholar] [CrossRef]
- Arshad, H.; Saleem, M.; Pasha, U.; Sadaf, S. Synthesis of Aloe vera-conjugated Silver Nanoparticles for Use against Multidrug-Resistant Microorganisms. Electron. J. Biotechnol. 2022, 55, 55–64. [Google Scholar] [CrossRef]
- Kong, W.-S.; Li, J.; Liu, X.; Mi, Q.-L.; Chen, J.-H.; Li, X.-M.; Yang, G.-Y.; Hu, Q.-F.; Li, T.; Yang, Y.-K. A new naphthalene derivative from Aloe vera and its antibacterial activity. China J. Chin. Mater. Med. 2017, 42, 3761–3763. [Google Scholar] [CrossRef]
- Alghamdi, A.; Alshehri, W.; Sajer, B.; Ashkan, M.; Ashy, R.; Gashgari, R.; Hakmi, H. Biological Activities and GC-MS Analysis of Aloe vera and Opuntia ficus-indica Extracts. J. Chem. 2023, 2023, 6504505. [Google Scholar] [CrossRef]
- Sinicropi, M.S.; Baldino, N.; Ceramella, J.; Iacopetta, D.; Scali, E.; Basile, G.; Saturnino, C.; Catalano, A. Opuntia ficus indica (L.) Mill. An Ancient Plant Source of Nutraceuticals. Curr. Top. Med. Chem. 2022, 22, 1736–1749. [Google Scholar] [CrossRef]
- Khursheed, A.; Rather, M.A.; Jain, V.; Wani, A.R.; Rasool, S.; Nazir, R.; Malik, N.A.; Majid, S.A. Plant Based Natural Products as Potential Ecofriendly and Safer Biopesticides: A Comprehensive Overview of Their Advantages Over Conventional Pesticides, Limitations and Regulatory Aspects. Microb. Pathog. 2022, 173 Pt A, 105854. [Google Scholar] [CrossRef]
- Das, S.; Mishra, B.; Gill, K.; Ashraf, M.S.; Singh, A.K.; Sinha, M.; Sharma, S.; Xess, I.; Dalal, K.; Singh, T.P.; et al. Isolation and Characterization of Novel Protein with Anti-fungal and Anti-inflammatory Properties from Aloe vera Leaf Gel. Int. J. Biol. Macromol. 2011, 48, 38–43. [Google Scholar] [CrossRef] [PubMed]
- Bernardes, I.; Rodrigues, M.P.F.; Bacelli, G.K.; Munin, E.; Alves, L.P.; Costa, M.S. Aloe vera Extract Reduces Both Growth and Germ Tube Formation by Candida albicans. Mycoses 2012, 55, 257–261. [Google Scholar] [CrossRef] [PubMed]
- Thaweboon, S.; Thaweboon, B. Assessment of Antifungal Activity of Aloe vera Toothpaste against Candida albicans. IOP Conf. Ser. Mater. Sci. Eng. 2020, 761, 012007. [Google Scholar] [CrossRef]
- Añibarro-Ortega, M.; Pinela, J.; Barros, L.; Ćirić, A.; Silva, S.P.; Coelho, E.; Mocan, A.; Calhelha, R.C.; Soković, M.; Coimbra, M.A.; et al. Compositional Features and Bioactive Properties of Aloe vera leaf (Fillet, Mucilage, and Rind) and Flower. Antioxidants 2019, 8, 444. [Google Scholar] [CrossRef]
- Añibarro-Ortega, M.; Pinela, J.; Ćirić, A.; Lopes, E.; Molina, A.K.; Calhelha, R.C.; Soković, M.; Ferreira, O.; Ferreira, I.C.F.R.; Barros, L. Extraction of Aloesin from Aloe vera Rind using Alternative Green Solvents: Process Optimization and Biological Activity Assessment. Biology 2021, 10, 951. [Google Scholar] [CrossRef] [PubMed]
- Dinesh, D.; Murugan, K.; Madhiyazhagan, P.; Panneerselvam, C.; Mahesh Kumar, P.; Nicoletti, M.; Jiang, W.; Benelli, G.; Chandramohan, B.; Suresh, U. Mosquitocidal and Antibacterial Activity of Green-synthesized Silver Nanoparticles from Aloe vera Extracts: Towards an Effective Tool against the Malaria Vector Anopheles stephensi? Parasitol. Res. 2015, 114, 1519–1529. [Google Scholar] [CrossRef] [PubMed]
- Adebayo, N.S.; Motunrayo, O. Evaluation of Antiplasmodial Potential of Aloe barbadensis and Allium sativum on Plasmodium berghei-Infected Mice. J. Med. Plants Res. 2018, 12, 320–324. [Google Scholar] [CrossRef]
- Mørkve, Å.W.; Sitienei, J.; Van den Bergh, G. A Qualitative Case Study of Community Experiences with Tungiasis in High Prevalence Villages of Bungoma County, Kenya: “The Whole Body Aches and the Jiggers are Torturing Me!”. PLoS Negl. Trop. Dis. 2023, 17, e0011304. [Google Scholar] [CrossRef]
- Feldmeier, H.; Kehr, J.D.; Heukelbach, J. A Plant-based Repellent Protects against Tunga penetrans Infestation and Sand Flea Disease. Acta Trop. 2006, 99, 126–136. [Google Scholar] [CrossRef]
- Suzuki, K.; Kamiya, Y.; Smith, C.; Kaneko, S.; Ongaya, A.; Amukoye, E. Protocol for a Randomized Control Trial for Tungiasis Treatment in Homa Bay County, Kenya: Dimeticone versus Sodium Carbonate. Meth. Protocols 2023, 6, 12. [Google Scholar] [CrossRef]
- Pyne, N.; Bhattacharya, I.; Paul, S. Therapeutic Potential of Indian Medicinal Plants against Leishmania donovani: A Review. Proc.Indian Natl. Sci. Acad. 2023, 89, 1–14. [Google Scholar] [CrossRef]
- Dutta, A.; Sarkar, D.; Gurib-Fakim, A.; Mandal, C.; Chatterjee, M. In Vitro and In Vivo Activity of Aloe vera Leaf Exudate in Experimental Visceral Leishmaniasis. Parasitol. Res. 2008, 102, 1235–1242. [Google Scholar] [CrossRef] [PubMed]
- Richard, K.; Andrae-Marobela, K.; Tietjen, I. An Ethnopharmacological Survey of Medicinal Plants Traditionally Used by the BaKalanga People of the Tutume Subdistrict in Central Botswana to Manage HIV/AIDS, HIV-associated Conditions, and Other Health Conditions. J. Ethnopharmacol. 2023, 316, 116759. [Google Scholar] [CrossRef] [PubMed]
- Españo, E.; Kim, J.; Kim, J.-K. Utilization of Aloe Compounds in Combatting Viral Diseases. Pharmaceuticals 2022, 15, 599. [Google Scholar] [CrossRef] [PubMed]
- Saoo, K.; Miki, H.; Ohmori, M.; Winters, W.D. Antiviral Activity of Aloe Extracts against Cytomegalovirus. Phytother. Res. 1996, 10, 348–350. [Google Scholar] [CrossRef]
- Choi, J.-G.; Lee, H.; Kim, Y.S.; Hwang, Y.-H.; Oh, Y.-C.; Lee, B.; Moon, K.M.; Cho, W.-K.; Ma, J.Y. Aloe vera and its Components Inhibit Influenza A Virus-Induced Autophagy and Replication. Am. J. Chin. Med. 2019, 47, 1307–1324. [Google Scholar] [CrossRef]
- Gansukh, E.; Gopal, J.; Paul, D.; Muthu, M.; Kim, D.-H.; Oh, J.-W.; Chun, S. Ultrasound Mediated Accelerated Anti-influenza Activity of Aloe vera. Sci. Rep. 2018, 8, 17782. [Google Scholar] [CrossRef] [PubMed]
- Rezazadeh, F.; Moshaverinia, M.; Motamedifar, M.; Alyaseri, M. Assessment of Anti HSV-1 Activity of Aloe vera Gel Extract: An In Vitro Study. J. Dent. 2016, 17, 49–54. [Google Scholar] [PubMed] [PubMed Central]
- Sun, Z.; Yu, C.; Wang, W.; Yu, G.; Zhang, T.; Zhang, L.; Zhang, J.; Wei, K. Aloe Polysaccharides Inhibit Influenza A Virus Infection-A Promising Natural Anti-flu. Drug. Front. Microbiol. 2018, 9, 2338. [Google Scholar] [CrossRef]
- Ng, Y.C.; Kim, Y.W.; Ryu, S.; Lee, A.; Lee, J.-S.; Song, M.J. Suppression of Norovirus by Natural Phytochemicals from Aloe vera and Eriobotryae folium. Food Control 2017, 73, 1362–1370. [Google Scholar] [CrossRef]
- Lin, L.-T.; Hsu, W.-C.; Lin, C.-C. Antiviral Natural Products and Herbal Medicines. J. Tradit. Complementary Med. 2014, 4, 24–35. [Google Scholar] [CrossRef] [PubMed]
- Iacopetta, D.; Ceramella, J.; Catalano, A.; Saturnino, C.; Pellegrino, M.; Mariconda, A.; Longo, P.; Sinicropi, M.S.; Aquaro, S. COVID-19 at a Glance: An Up-to-date overview on Variants, Drug Design and Therapies. Viruses 2022, 14, 573. [Google Scholar] [CrossRef]
- Ceramella, J.; Iacopetta, D.; Sinicropi, M.S.; Andreu, I.; Mariconda, A.; Saturnino, C.; Giuzio, F.; Longo, P.; Aquaro, S.; Catalano, A. Drugs for COVID-19: An Update. Molecules 2022, 27, 8562. [Google Scholar] [CrossRef] [PubMed]
- Catalano, A.; Iacopetta, D.; Ceramella, J.; Di Maio, A.C.; Basile, G.; Giuzio, F.; Bonomo, M.G.; Aquaro, S.; Walsh, T.J.; Sinicropi, M.S.; et al. Are Nutraceuticals Effective in COVID-19 and Post-COVID Prevention and Treatment? Foods 2022, 11, 2884. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.A.; Al-Balushi, K. Combating COVID-19: The Role of Drug Repurposing and Medicinal Plants. J. Infect. Public Health 2021, 14, 495–503. [Google Scholar] [CrossRef] [PubMed]
- Ul Qamar, M.T.; Alqahtani, S.M.; Alamri, M.A.; Chen, L.L. Structural basis of SARS-CoV-2 3CL(pro) and anti-COVID-19 drug discovery from medicinal plants. J. Pharm. Anal. 2020, 10, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Yagi, A. Exploratory Approaches for the Use of Aloe for Covid-19 Treatment: Prevention and Mitigation Effect. J. Diabetes Res. Rev. Rep. 2020, 2, 1–6. [Google Scholar] [CrossRef]
- Mpiana, P.T.; Ngbolua, K.-T.-N.; Tshibangu, D.S.T.; Kilembe, J.T.; Gbolo, B.Z.; Mwanangombo, D.T.; Inkoto, C.L.; Lengbiye, E.M.; Mbadiko, C.M.; Matondo, A.; et al. Aloe vera (L.) Burm. F. as a Potential Anti-COVID-19 Plant: A Mini-review of Its Antiviral Activity. Eur. J. Med. Plants 2020, 31, 86–93. [Google Scholar] [CrossRef]
- Vidoni, C.; Fuzimoto, A.; Ferraresi, A.; Isidoro, C. Targeting Autophagy with Natural Products to Prevent SARS-CoV-2 Infection. J. Tradit. Complement. Med. 2022, 12, 55–68. [Google Scholar] [CrossRef]
- Nyagumbo, E.; Pote, W.; Shopo, B.; Nyirenda, T.; Chagonda, I.; Mapaya, R.J.; Maunganidze, F.; Mavengere, W.N.; Mawere, C.; Mutasa, I.; et al. Medicinal Plants Used for the Management of Respiratory Diseases in Zimbabwe: Review and Perspectives Potential Management of COVID-19. Phys. Chem. Earth 2022, 128, 103232. [Google Scholar] [CrossRef]
- Anwar, N.; Ahmed, N.Z.; Fathima, A.F.; Khan, A.A. Analytical review of Tiryāq-i-Wabāī-A Unani Panacea for the Control of COVID-19. J. Herb. Med. 2023, 39, 100653. [Google Scholar] [CrossRef] [PubMed]
- Nirala, R.K.; Raj, P.; Anjana, K.; Mandal, K.G. A Review on Immunomodulatory Activity of Amla and Aloe vera. J. Pharmacogn. Phytochem. 2020, 9, 2014–2016. [Google Scholar]
- Im, S.A.; Lee, Y.R.; Lee, Y.H.; Lee, M.K.; Park, Y.I.; Lee, S.; Kim, K.; Lee, C.K. In vivo Evidence of the Immunomodulatory Activity of Orally Administered Aloe vera gel. Arch. Pharm. Res. 2010, 33, 451–456. [Google Scholar] [CrossRef] [PubMed]
- Madan, J.; Sharma, A.K.; Inamdar, N.; Rao, H.S.; Singh, R. Immunomodulatory Properties of Aloe vera Gel in Mice. Int, J. Green Pharm. 2008, 2, 152–154. [Google Scholar]
- López, Z.; Femenia, A.; Núñez-Jinez, G.; Salazar Zúñiga, M.N.; Cano, M.E.; Espino, T.; Knauth, P. In Vitro Immunomodulatory Effect of Food Supplement from Aloe vera. Evid. Based Complement. Altern. Med. 2019, 2019, 5961742. [Google Scholar] [CrossRef] [PubMed]
- Mosayebi, G.; Ghazavi, A.; Aghili, B.; Mirshafiei, A. Immunomodulating Activity of Aloe vera in Animal Model of Multiple Sclerosis. J. Arak Univ. Med. Sci. 2009, 12, 109–115. Available online: http://jams.arakmu.ac.ir/article-1-388-en.html (accessed on 7 July 2024).
- Majumder, R.; Das, C.K.; Mandal, M. Lead Bioactive Compounds of Aloe vera as Potential Anticancer Agent. Pharmacol. Res. 2019, 148, 104416. [Google Scholar] [CrossRef] [PubMed]
- Tong, X.; Li, M.; Li, D.; Lao, C.; Chen, J.; Xu, W.; Du, J.; Zhang, M.; Yang, X.; Li, J. Aloe vera Gel Extract: Safety Evaluation for Acute and Chronic Oral Administration in Sprague-Dawley Rats and Anticancer Activity in Breast and Lung Cancer Cells. J. Ethnopharmacol. 2021, 280, 114434. [Google Scholar] [CrossRef] [PubMed]
- Majumder, R.; Parida, P.; Paul, S.; Basak, P. In vitro and in Silico Study of Aloe vera Leaf Extract against Human Breast Cancer. Nat. Prod. Res. 2020, 34, 2363–2366. [Google Scholar] [CrossRef]
- Shalabi, M.; Khilo, K.; Zakaria, M.M.; Elsebaei, M.G.; Abdo, W.; Awadin, W. Anticancer Activity of Aloe vera and Calligonum comosum Extracts Separetely on Hepatocellular Carcinoma Cells. Asian Pac. J. Trop. Biomed. 2015, 5, 375–381. [Google Scholar] [CrossRef]
- Karpagam, T.; Firdous, J.; Priya, S.; Varalakshmi, B.; Gomathi, S.; Geetha, S.; Muhamad, N. Anti-cancer Activity of Aloe vera Ethanolic Leaves Extract against in Vitro Cancer Cells. Res. J. Pharm. Technol. 2019, 12, 2167–2170. [Google Scholar] [CrossRef]
- Akev, N.; Candoken, E.; Kuruca, S.E. Comparative Study on the Anticancer Drug Potential of a Lectin Purified from Aloe vera and Aloe-Emodin. Asian Pac. J. Cancer Prev. 2020, 21, 99–106. [Google Scholar] [CrossRef]
- De Carvalho Lima, E.N.; Barros Martins, G.L.; Diaz, R.S.; Schechter, M.; Piqueira, J.R.C.; Justo, J.F. Effects of Carbon Nanomaterials and Aloe vera on Melanomas—Where Are We? Recent Updates. Pharmaceutics 2022, 14, 2004. [Google Scholar] [CrossRef] [PubMed]
- Sinha, L.; Satyapal, G.K.; Kumar, S. Aloe vera-A Medicinal Plant as Potential Therapeutic Agents for Liver Cancer. Front. Med. Chem. 2023, 10, 281–289. [Google Scholar]
- Ferreira, A.S.; Macedo, C.; Silva, A.M.; Delerue-Matos, C.; Costa, P.; Rodrigues, F. Natural Products for the Prevention and Treatment of Oral Mucositis—A Review. Int. J. Mol. Sci. 2022, 23, 4385. [Google Scholar] [CrossRef] [PubMed]
- Gao, Y.; Jiang, T.; Mei, S.; Zhang, S.; Zhu, C.; Sun, Y. Meta-analysis of Aloe vera for the Prevention and Treatment of Chemotherapy-induced Phlebitis. Int. J. Clin. Exp. Med. 2016, 9, 9642–9650. [Google Scholar]
- Chiu, C.C.; Hsiao, Y.W.; Wen, Y.C.; Chang, T.Y.; Chen, S.H.; Jaing, T.H. Aloe vera Gel for Prevention of Chemotherapy-induced Hyperpigmentation: Four Case Reports. Medicine 2023, 102, e34037. [Google Scholar] [CrossRef] [PubMed]
- Raj, S.; Manchanda, R.; Bhandari, M.; Alam, M.S. Review on Natural Bioactive Products as Radioprotective Therapeutics: Present and Past Perspective. Curr. Pharm. Biotechnol. 2022, 23, 1721–1738. [Google Scholar] [CrossRef]
- Kumar, S.; Tiku, A.B. Immunomodulatory Potential of Acemannan (polysaccharide from Aloe vera) against Radiation Induced Mortality in Swiss Albino Mice. Food Agric. Immunol. 2016, 27, 72–86. [Google Scholar] [CrossRef]
- Bala, S.; Chugh, N.A.; Bansal, S.C.; Garg, M.L.; Koul, A. Protective Role of Aloe vera against X-ray Induced Testicular Dysfunction. Andrologia 2017, 49, 12697. [Google Scholar] [CrossRef]
- Bala, S.; Chugh, N.A.; Bansal, S.C.; Garg, M.L.; Koul, A. Radiomodulatory Effects of Aloe vera on Hepatic and Renal Tissues of X-ray Irradiated Mice. Mut. Res. 2018, 811, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Farid, A.; Haridyy, H.; Ashraf, S.; Ahmed, S.; Safwat, G. Aloe vera Gel as a Stimulant for Mesenchymal Stem Cells Differentiation and a Natural Therapy for Radiation Induced Liver Damage. J. Radiat. Res. Appl. Sci. 2022, 15, 270–278. [Google Scholar] [CrossRef]
- Kim, S.H.; Cheon, H.J.; Yun, N.; Oh, S.T.; Shin, E.; Shim, K.S.; Lee, S.M. Protective Effect of a Mixture of Aloe vera and Silybum marianum against Carbon Tetrachloride-induced Acute Hepatotoxicity and Liver Fibrosis. J. Pharmacol. Sci. 2009, 109, 119–127. [Google Scholar] [CrossRef]
- Aladejana, E.B.; Aladejana, A.E. Hepatoprotective Activities of Polyherbal Formulations: A Systematic Review. J. Med. Plants Econ. Dev. 2023, 7, 206. [Google Scholar] [CrossRef]
- Gupta, V.K.; Siddiqi, N.J.; Ojha, A.K.; Sharma, B. Hepatoprotective effect of Aloe vera against cartap- and malathion-induced toxicity in Wistar rats, J. Cell. Physiol. 2019, 234, 18329–18343. [Google Scholar] [CrossRef] [PubMed]
- Al-Abbassi, L.M.; Sharba, I.R.; Al-Hatemy, K.T. Study the Protective Effect of Aloe vera Gel Extract against Hepatotoxicity after Treated with Azathioprine in Adult Rats. AIP Conf. Proc. 2023, 2475, 020010. [Google Scholar] [CrossRef]
- Bhatt, S.; Virani, S.; Sharma, M.; Kumar, H.; Saxena, K.K. Evaluation of Hepatoprotective Activity of Aloe vera in Acute Viral Hepatitis. Int. J. Pharm. Sci. Res. 2014, 5, 2479. [Google Scholar] [CrossRef]
- Handayani, S.; Aprilia, D.; Nisa, K.; Rosyida, V.T.; Wulanjati, M.P.; Windarsih, A.; Darsih, C.; Frediansyah, A.; Haryanti, S. A Mini-Review: Possible Mechanisms of Hepatoprotective Effect of Aloe vera Gel. Indones. J. Cancer Chemoprevent. 2021, 12, 170–179. [Google Scholar] [CrossRef]
- Kumar, A.; Zechariah, J.; Ramchandra, S.A.J.; Tripathi, P. Study on Aloe vera Leaves Farming in Rajasthan. Pharma. Innov. J. 2022, 11, 289–291. [Google Scholar]
- Virani, S.; Bhatt, S.; Saini, M.A.N.I.S.H.; Saxena, K. Aloe vera attenuates gentamicin-induced nephrotoxicity in Wistar albino rats: Histopathological and biochemical changes. Asian J. Pharm. Clin. Res. 2016, 9, 113–117. [Google Scholar]
- Iftkhar, A.; Hasan, I.J.; Sarfraz, M.; Jafri, L.; Ashraf, M.A. Nephroprotective Effect of the Leaves of Aloe barbadensis (Aloe vera) against Toxicity Induced by Diclofenac Sodium in Albino Rabbits. West Indian Med. J. 2015, 64, 462–467. [Google Scholar] [CrossRef] [PubMed]
- Chatterjee, P.; Mukherjee, A.; Nandy, S. Protective Effects of the Aqueous Leaf Extract of Aloe barbadensis on Gentamicin and Cisplatin–induced Nephrotoxic Rats. Asian Pac. J. Trop. Biomed. 2012, 2, S1754–S1763. [Google Scholar] [CrossRef]
- El-Shafie, M.; Elmasry, H.G.; Elsadek, M.F.B.; AlMajwal, A.M. Curative Effect of Orally Consumed Aloe vera Juice on Ochratoxin A-Induced Nephrotoxicity in Rats. Prog. Nutr. 2015, 17, 128–136. [Google Scholar]
- Ahmed, A.; Khan, H.A.; Haq, R.M.A.U.; Naz, A.; Awan, S.J.; Shuaib, M.; Badar, R. Protective Effects of Aloe vera Gel Ethanolic Extract Against Streptozotocin-induced Hepato-pancreatic Toxicity in Female Albino Rats. J. Pharm. Res. Int. 2022, 34, 13–24. [Google Scholar] [CrossRef]
- Ceramella, J.; De Maio, A.C.; Basile, G.; Facente, A.; Scali, E.; Andreu, I.; Sinicropi, M.S.; Iacopetta, D.; Catalano, A. Phytochemicals Involved in Mitigating Silent Toxicity Induced by Heavy Metals. Foods 2024, 13, 978. [Google Scholar] [CrossRef]
- Kaithwas, G.; Dubey, K.; Pillai, K.K. Effect of Aloe vera (Aloe barbadensis Miller) Gel on Doxorubicin-induced Myocardial Oxidative Stress and Calcium Overload in Albino Rats. Ind. J. Exp. Biol. 2011, 49, 260–268. [Google Scholar]
- Yang, Y.; Yang, M.; Ai, F.; Huang, C. Cardioprotective Effect of Aloe vera Biomacromolecules Conjugated with Selenium Trace Element on Myocardial Ischemia-Reperfusion Injury in Rats. Biol. Trace Elem. Res. 2017, 177, 345–352. [Google Scholar] [CrossRef]
- Wasim, A.; Saif, A.; Pratap, S.A. A Comprehensive Review of Aloe vera: Health Benefits, Mechanisms of Action and Future Perspectives. Int. J. Res. Dev. Technol. 2023, 1, 1–18. Available online: http://ijrdt.com/index.php/files/article/view/81 (accessed on 7 July 2024).
- Kumar, V.; Kumar, N.; Singh, G. Natural Products and Derivatives Applied for Skin Care: An Updated Review. Curr. Tradit. Med. 2024, 10, 18–30. [Google Scholar] [CrossRef]
- Hekmatpou, D.; Mehrabi, F.; Rahzani, K.; Aminiyan, A. The Effect of Aloe vera Clinical Trials on Prevention and Healing of Skin Wound: A Systematic Review. Iran. J. Med. Sci. 2019, 44, 1–9. [Google Scholar] [PubMed] [PubMed Central]
- Kloter, E.; Albanese, F.; Schweighoffer, R.; Wolf, U. Phytotherapy in paediatric skin disorders-a systematic literature review. Compl. Ther. Med. 2023, 74, 102942. [Google Scholar] [CrossRef] [PubMed]
- Pegu, A.J.; Sharma, M.A. Review on Aloe vera. Int. J. Trend Sci. Res. Dev. 2019, 3, 35–40. Available online: https://www.ijtsrd.com/papers/ijtsrd23541.pdf (accessed on 7 July 2024). [CrossRef]
- Fox, L.T.; du Plessis, J.; Gerber, M.; van Zyl, S.; Boneschans, B.; Hamman, J.H. In Vivo Skin Hydration and Anti-erythema Effects of Aloe vera, Aloe ferox and Aloe marlothii Gel Materials after Single and Multiple Applications. Pharmacogn. Mag. 2014, 10 (Suppl. S2), S392–S403. [Google Scholar] [CrossRef] [PubMed]
- Rathee, P.; Kumar, S.; Kumar, D.; Kumari, B.; Yadav, S.S. Skin hyperpigmentation and its treatment with herbs: An alternative method. Future J. Pharm. Sci. 2021, 7, 132. [Google Scholar] [CrossRef]
- Mikayoulou, M.; Mayr, F.; Temml, V.; Pandian, A.; Vermaak, I.; Chen, W.; Komane, B.; Stuppner, H.; Viljoen, A. Anti-tyrosinase Activity of South African Aloe Species and Isolated Compounds Plicataloside and Aloesin. Fitoterapia 2021, 150, 104828. [Google Scholar] [CrossRef] [PubMed]
- Arbab, S.; Ullah, H.; Weiwei, W.; Wei, X.; Ahmad, S.U.; Wu, L.; Zhang, J. Comparative Study of Antimicrobial Action of Aloe vera and Antibiotics against Different Bacterial Isolates from Skin Infection. Vet. Med. Sci. 2021, 7, 2061–2067. [Google Scholar] [CrossRef]
- Liang, J.; Cui, L.; Li, J.; Guan, S.; Zhang, K.; Li, J. Aloe vera: A Medicinal Plant Used in Skin Wound Healing. Tissue Eng. Part B Rev. 2021, 27, 455–474. [Google Scholar] [CrossRef]
- Łopuszyńska, I.; Adamowicz, D.; Rudziński, P.; Wosińska, A.; Meliksetian, A.; Pazik, D.; Kosecka, K.; Cieślik, A.; Jargieło, A.; Kosieradzka, K. Medicinal Plants in Burns Treatment–A Systematic Review. J. Educat. Health Sport 2023, 45, 122–135. [Google Scholar] [CrossRef]
- Aulia, L.; Pane, Y.S. Effect of Aloe vera Extract in Post-burn Skin Repair in Rats. F1000Research 2022, 11, 168. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.; Alfonso, A.R.; Gordon, A.J.; Kwong, J.; Lin, L.J.; Chiu, E.S. Second-degree Burns and Aloe vera: A Meta-Analysis and Systematic Review. Adv. Skin Wound Care 2022, 35, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Takzaree, N.; Hadjiakhondi, A.; Hassanzadeh, G.; Rouini, M.R.; Manayi, A.; Zolbin, M.M. Transforming Growth Factor-β (TGF-β) Activation in Cutaneous Wounds after Topical Application of Aloe vera gel. Can. J. Physiol. Pharm. 2016, 94, 1285–1290. [Google Scholar] [CrossRef] [PubMed]
- Levin, N.J.; Erben, Y.; Li, Y.; Brigham, T.J.; Bruce, A.J. A Systematic Review and Meta-Analysis Comparing Burn Healing Outcomes between Silver Sulfadiazine and Aloe vera. Cureus 2022, 14, e30815. [Google Scholar] [CrossRef] [PubMed]
- Imbarak, N.; Abdel-Aziz, H.I.; Farghaly, L.M.; Hosny, S. Effect of Mesenchymal Stem Cells versus Aloe vera on Healing of Deep Second-Degree Burn. Stem Cell Investig. 2021, 8, 12. [Google Scholar] [CrossRef] [PubMed]
- Atiba, A.; Abdo, W.; Ali, E.; Abd-Elsalam, M.; Amer, M.; Abdel Monsef, A.; Taha, R.; Antar, S.; Mahmoud, A. Topical and Oral Applications of Aloe vera Improve Healing of Deep Second-Degree Burns in Rats via Modulation of Growth Factors. Biomarkers 2022, 27, 608–617. [Google Scholar] [CrossRef] [PubMed]
- Mustafa, W.W.; Moahammed, S.S. Experimental Investigation on the Oral and Topical Application of Aloe vera in Wound Care. J. Pharm. Neg. Res. 2022, 13, 442–450. [Google Scholar] [CrossRef]
- Kim, M.K.; Choi, Y.C.; Cho, S.H.; Choi, J.S.; Cho, Y.W. The Antioxidant Effect of Small Extracellular Vesicles Derived from Aloe vera Peels for Wound Healing. Tissue Eng. Regen. Med. 2021, 18, 561–571. [Google Scholar] [CrossRef] [PubMed]
- Chelu, M.; Musuc, A.M.; Popa, M.; Calderon Moreno, J. Aloe vera-based Hydrogels for Wound Healing: Properties and Therapeutic Effects. Gels 2023, 9, 539. [Google Scholar] [CrossRef] [PubMed]
- Rayate, A.; Nagoba, B.S.; Mumbre, S.S.; Mavani, H.B.; Gavkare, A.; Deshpande, A.S. Current Scenario of Traditional Medicines in Management of Diabetic Foot Ulcers: A Review. World J. Diabetes 2023, 14, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Worasakwutiphong, S.; Termwattanaphakdee, T.; Kamolhan, T.; Phimnuan, P.; Sittichokechaiwut, A.; Viyoch, J. Evaluation of the Safety and Healing Potential of a Fibroin-Aloe Gel Film for the Treatment of Diabetic Foot Ulcers. J. Wound Care 2021, 30, 1020–1028. [Google Scholar] [CrossRef]
- Jamiyanti, A.; Pahria, T.; Nursiswati, N. Topical Effects of Aloe vera in Healing Diabetic Foot Ulcers: A Protocol of Systematic Review. Mal. J. Med. Health Sci. 2023, 19, 355–359. [Google Scholar] [CrossRef]
- Yoshida, C.M.; Pacheco, M.S.; de Moraes, M.A.; Lopes, P.S.; Severino, P.; Souto, E.B.; da Silva, C.F. Effect of Chitosan and Aloe vera Extract Concentrations on the Physicochemical Properties of Chitosan Biofilms. Polymers 2021, 13, 1187. [Google Scholar] [CrossRef]
- Chauhan, P.N.; Sharma, A.; Rasheed, H.; Mathur, H.; Sharma, P. Treatment Opportunities and Technological Progress Prospective for Acne vulgaris. Curr. Drug Deliv. 2022, 19, 1037–1048. [Google Scholar] [CrossRef] [PubMed]
- Hajheidari, Z.; Saeedi, M.; Morteza-Semnani, K.; Soltani, A. Effect of Aloe vera Topical Gel Combined with Tretinoin in Treatment of Mild and Moderate Acne Vulgaris: A Randomized, Double-Blind, Prospective Trial. J. Dermatol. Treat. 2013, 25, 123–129. [Google Scholar] [CrossRef] [PubMed]
- Bilal, M.; Lubis, M.S.; Yuniarti, R.; Nasution, H.M. Formulation of Anti-Acne Extract Aloe vera (Aloe vera (L.) Burm. f.) Inhibiting the Activity of Propionibacterium acnes. Int. J. Health Pharm. 2023, 3, 241–248. [Google Scholar] [CrossRef]
- Pratt, C.H.; King, L.E.; Messenger, A.G.; Christiano, A.M.; Sundberg, J.P. Alopecia Areata. Nat. Rev. Dis. Primers 2017, 3, 17011. [Google Scholar] [CrossRef]
- Wang, E.; Lee, J.S.; Hee, T.H. Is Propionibacterium Acnes Associated with Hair Casts and Alopecia? Int. J. Trichol. 2012, 4, 93–97. [Google Scholar] [CrossRef]
- El Zawahry, M.; Hegazy, M.R.; Helal, M. Use of Aloe in Treating Leg Ulcers and Dermatoses. Int. J. Dermatol. 1973, 12, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Hosny, K.M.; Rizg, W.Y.; Alhakamy, N.A.; Alamoudi, A.J.; Mushtaq, R.Y.; Safhi, A.Y. Utilization of Nanotechnology and Experimental Design in Development and Optimization of Aloe vera Gel Loaded with Finasteride–Garlic Oil–Nanotransfersomes. J. Drug Deliv. Sci. Technol. 2022, 68, 103130. [Google Scholar] [CrossRef]
- Sonkodi, B. Psoriasis, Is It a Microdamage of Our “Sixth Sense”? A Neurocentric View. Int. J. Mol. Sci. 2022, 23, 11940. [Google Scholar] [CrossRef]
- Miroddi, M.; Navarra, M.; Calapai, F.; Mancari, F.; Giofre, S.V.; Gangemi, S.; Calapai, G. Review of Clinical Pharmacology of Aloe vera L. in the Treatment of Psoriasis. Phytother Res. 2015, 29, 648–655. [Google Scholar] [CrossRef]
- Leng, H.; Pu, L.; Xu, L.; Shi, X.; Ji, J.; Chen, K. Effects of Aloe Polysaccharide, a Polysaccharide Extracted from Aloe vera, on TNF-α-induced HaCaT Cell Proliferation and the Underlying Mechanism in Psoriasis. Mol. Med. Rep. 2018, 18, 3537–3543. [Google Scholar] [CrossRef] [PubMed]
- Niculet, E.; Radaschin, D.S.; Nastase, F.; Draganescu, M.; Baroiu, L.; Miulescu, M.; Arbune, M.; Tatu, A.L. Influence of phytochemicals in induced psoriasis (Review). Exp. Ther. Med. 2020, 20, 3421–3424. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.V.; Banwell, P.E.; Roberts, A.H.N.; McGrouther, D.A. Frostbite: Pathogenesis and Treatment. J. Trauma Inj. Infect. Crit. Care 2000, 48, 171–178. [Google Scholar] [CrossRef] [PubMed]
- Murphy, J.; Endorf, F.W.; Winters, M.K.; Rogers, C.; Walter, E.; Neumann, N.; Weber, L.; Lacey, A.M.; Punjabi, G.; Nygaard, R.M. Bleeding complications in patients with severe frostbite injury. J. Burn Care Res. 2023, 44, 745–750. [Google Scholar] [CrossRef]
- Patel, P.; Handa, M.; Jain, K.; Shukla, R. Recent pharmaceutical engineered approaches as prophylaxis and management of frostbite. J. Drug Deliv. Sci. Technol. 2022, 76, 103838. [Google Scholar] [CrossRef]
- Davis, A.; Sinopoli, B.; Mann, N.; Stenbit, A.E. A photographic case of frostbite treated with delayed hyperbaric oxygen therapy. High Altitude Med. Biol. 2022, 23, 194–197. [Google Scholar] [CrossRef] [PubMed]
- Feily, A.; Namazi, M. Aloe vera in dermatology: A Brief Review. G. Ital. Dermatol. Venereol. Organo Uff. Soc. Ital. Dermatol. Sifilogr. 2009, 144, 85–91. [Google Scholar] [PubMed]
- Vakili, M.; Ahmadipour, S.; Rahmani, P. Concise Review: Herbal Remedies and Herbal Plants for Constipation in Children. Biomed. Res. Ther. 2018, 5, 2260–2267. [Google Scholar] [CrossRef]
- Ma, Q.; Wang, C.Z.; Sawadogo, W.R.; Bian, Z.X.; Yuan, C.S. Herbal Medicines for Constipation and Phytochemical Comparison of Active Components. Am. J. Chin. Med. 2022, 50, 723–732. [Google Scholar] [CrossRef]
- Yu, M.; Kong, X.Y.; Chen, T.T.; Zou, Z.M. In Vivo Metabolism Combined Network Pharmacology to Identify Anti-constipation Constituents in Aloe barbadensis Mill. J. Ethnopharmacol. 2024, 319, 117200. [Google Scholar] [CrossRef]
- Varpe, B.D.; Kulkarni, A.A.; Mali, A.S. Aloe vera Compositions Used for Medicinal Applications: A Patent Review (2013-till 2020). Recent Pat. Food Nutr. Agric. 2021, 12, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Panahi, Y.; Khedmat, H.; Valizadegan, G.; Mohtashami, R.; Sahebkar, A. Efficacy and Safety of Aloe vera Syrup for the Treatment of Gastroesophageal Reflux Disease: A Pilot Randomized Positive-Controlled Trial. J. Tradit. Chin. Med. 2015, 35, 632–636. [Google Scholar] [CrossRef] [PubMed]
- Mahboubi, M. Aloe vera (Aloe barbadensis) Gel for the Management of Gastroesophageal Reflux Disease (GERD). Nat. Prod. J. 2021, 11, 13–20. [Google Scholar] [CrossRef]
- Fong-Jaén, F.; Smit, I.; Setshedi, M.; Engel, M.E. Consumption of Aloe to Improve Health Outcomes in Adults with Irritable Bowel Syndrome: A Systematic Review and Meta-analysis. South Afr. Gastroenterol. Rev. 2022, 20, 13–21. [Google Scholar]
- Wal, A.; Srivastava, A.; Verma, N.; Pandey, S.S.; Tyagi, S. The Role of Nutraceutical Supplements in the Treatment of Irritable Bowel Syndrome: A Mini Review. Curr. Pediatr. Rev. 2024, 20, 66–75. [Google Scholar] [CrossRef] [PubMed]
- Zhu, M.; Yang, M.; Song, Y.; Xu, H.; Xu, J.; Yue, N.N.; Zhang, Y.; Tian, C.; Shi, R.; Liang, Y.; et al. Exploring the Efficacy of Herbal Medicinal Products as Oral Therapy for Inflammatory Bowel Disease. Biomed. Pharmacother. 2023, 165, 115266. [Google Scholar] [CrossRef] [PubMed]
- Di Maio, A.C.; Basile, G.; Iacopetta, D.; Catalano, A.; Ceramella, J.; Cafaro, D.; Saturnino, C.; Sinicropi, M.S. The Significant Role of Nutraceutical Compounds in Ulcerative Colitis Treatment. Curr. Med. Chem. 2022, 29, 4216–4234. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.H.; Eom, J.Y.; Kim, H.J.; Seo, W.; Kwun, H.J.; Kim, D.K.; Kim, J.; Cho, Y.E. Aloe-derived Nanovesicles Attenuate Inflammation and Enhance Tight Junction Proteins for Acute Colitis Treatment. Biomat. Sci. 2023, 11, 5490–5501. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.J.; Huang, X.J.; Shi, X.D.; Chen, H.H.; Cui, S.W.; Nie, S.P. Protective Effect of Three Glucomannans from Different Plants against DSS Induced Colitis in Female BALB/c Mice. Food Funct. 2019, 10, 1928–1939. [Google Scholar] [CrossRef]
- Zhang, D.; Zhou, X.; Zhang, K.; Yu, Y.; Cui, S.W.; Nie, S. Glucomannan from Aloe vera Gel Maintains Intestinal Barrier Integrity via Mitigating Anoikis Mediated by Nrf2-Mitochondria Axis. Int. J. Biol. Macromol. 2023, 235, 123803. [Google Scholar] [CrossRef]
- Liu, C.; Hu, B.; Cheng, Y.; Guo, Y.; Yao, W.; Qian, H. In-depth Analysis of the Mechanisms of Aloe Polysaccharides on Mitigating Subacute Colitis in Mice via Microbiota Informatics. Carbohydr. Polym. 2021, 265, 118041. [Google Scholar] [CrossRef] [PubMed]
- Ismaeil, H.; Abdo, W.; Amer, S.; Tahoun, A.; Massoud, D.; Zanaty, E.; Bin-Jumah, M.; Mahmoud, A.M. Ameliorative Effect of Heat-Killed Lactobacillus plantarum L.137 and/or Aloe vera against Colitis in Mice. Processes 2020, 8, 225. [Google Scholar] [CrossRef]
- Langmead, L.; Feakins, R.M.; Goldthorpe, S.; Holt, H.; Tsironi, E.; De Silva, A.; Jewell, D.P.; Rampton, D.S. Randomized, Double-blind, Placebo-controlled Trial of Oral Aloe vera Gel for Active Ulcerative Colitis. Aliment. Pharmacol. Ther. 2004, 19, 739–747. [Google Scholar] [CrossRef] [PubMed]
- Babalola, W.O.; Ofusori, D.A.; Awoniran, P.; Falana, B.A. Aloe vera Gel Attenuates Acetic Acid-Induced Ulcerative Colitis in Adult Male Wistar Rats. Toxicol. Rep. 2022, 9, 640–646. [Google Scholar] [CrossRef] [PubMed]
- Naini, M.A.; Zargari-Samadnejad, A.; Mehrvarz, S.; Tanideh, R.; Ghorbani, M.; Dehghanian, A.; Hasanzarrini, M.; Banaee, F.; Hosseinabadi, O.K.; Iraji, A. Anti-inflammatory, Antioxidant, and Healing-promoting Effects of Aloe vera Extract in the Experimental Colitis in Rats. Evid. Based. Complement. Altern. Med. 2021, 2021, 9945244. [Google Scholar] [CrossRef] [PubMed]
- Shakib, Z.; Shahraki, N.; Razavi, B.M.; Hosseinzadeh, H. Aloe vera as an Herbal Medicine in the Treatment of Metabolic Syndrome: A Review. Phytother. Res. 2019, 33, 2649–2660. [Google Scholar] [CrossRef] [PubMed]
- Vieira, R.; Souto, S.B.; Sanchez-Lopez, E.; Machado, A.L.; Severino, P.; Jose, S.; Santini, A.; Fortuna, A.; Garcia, M.L.; Silva, A.M.; et al. Sugar-Lowering Drugs for Type 2 Diabetes Mellitus and Metabolic Syndrome-Review of Classical and New Compounds: Part-I. Pharmaceuticals 2019, 12, 152. [Google Scholar] [CrossRef] [PubMed]
- Deora, N.; Venkatraman, K. Aloe vera in Diabetic Dyslipidemia: Improving Blood Glucose and Lipoprotein Levels In Pre-clinical and Clinical Studies. J. Ayurveda Integr. Med. 2022, 13, 100675. [Google Scholar] [CrossRef]
- Bunyapraphatsara, N.; Yongchaiyudha, S.; Rungpitarangsi, V.; Chokechaijaroenporn, O. Antidiabetic activity of Aloe vera L. juice II. Clinical Trial in Diabetes Mellitus Patients in Combination with Glibenclamide. Phytomed. Int. J. Phytother. Phytopharm. 1996, 3, 245–248. [Google Scholar] [CrossRef]
- Tanaka, M.; Misawa, E.; Ito, Y.; Habara, N.; Nomaguchi, K.; Yamada, M.; Toida, T.; Hayasawa, H.; Takase, M.; Inagaki, M.; et al. Identification of Five Phytosterols from Aloe vera Gel as Anti-Diabetic Compounds. Biol. Pharm. Bull. 2006, 29, 1418–1422. [Google Scholar] [CrossRef]
- Devaraj, S.; Yimam, M.; Brownell, L.A.; Jialal, I.; Singh, S.; Jia, Q. Effects of Aloe vera Supplementation in Subjects with Prediabetes/Metabolic Syndrome. Metab. Syndr. Relat. Disord. 2013, 11, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Foadoddini, M.; Alinejad Mofrad, S. Effect of Aloe vera Extract on Depression in People with Prediabetes. Mod. Care J. 2020, 17, e100927. [Google Scholar] [CrossRef]
- Maurya, A.K.; Amrita, B.Y.; Pandey, D.K. To Examine Antidepressant Impact of Aloe vera and Fluoxetine in Mice. Eur. J. Mol. Clin. Med. 2021, 8, 3612–3619. [Google Scholar]
- Haghani, F.; Arabnezhad, M.-R.; Mohammadi, S.; Ghaffarian-Bahraman, A. Aloe vera and Streptozotocin-Induced Diabetes Mellitus. Rev. Bras. Farm. 2022, 32, 174–187. [Google Scholar] [CrossRef]
- Tabatabaei, S.R.F.; Ghaderi, S.; Bahrami-Tapehebur, M.; Farbood, Y.; Rashno, M. Aloe vera Gel Improves Behavioral Deficits and Oxidative Status in Streptozotocin-induced Diabetic Rats. Biomed. Pharmacother. 2017, 96, 279–290. [Google Scholar] [CrossRef] [PubMed]
- Tabatabaei, S.R.F.; Ghaderi, S.; Bahrami-Tapehebur, M.; Farbood, Y.; Rashno, M. Corrigendum to “Aloe vera Gel Improves Behavioral Deficits and Oxidative Status in Streptozotocin-induced Diabetic Rats”. Biomed. Pharmacother. 2023, 165, 115063. [Google Scholar] [CrossRef]
- Firempong, C.K.; Addo-Fordjour, P.; Komlaga, G.; Ameyaw, Y.; Nirvana, N.O.; Frederick, K.; Yaw, A.A. Ethnobotanical Study of Medicinal Plants Used to Treat HIV, Cancer and Diabetes in Some Communities of Ashanti Region, Ghana. J. Herb. Med. 2023, 39, 100648. [Google Scholar] [CrossRef]
- Prasannaraja, C.; Kamalanathan, A.S.; Vijayalakshmi, M.A.; Venkataraman, K. A Dipyrrole Derivative from Aloe vera Inhibits an Anti-diabetic Drug Target Dipeptidyl Peptidase (DPP)-IV in Vitro. Prep. Biochem. Biotechnol. 2020, 50, 511–520. [Google Scholar] [CrossRef] [PubMed]
- Irani, P.S.; Ranjbar, H.; Mehdipour-Rabori, R.; Torkaman, M.; Amirsalari, S.; Alazmani-Noode, F. The Effect of Aloe vera on the Healing of Diabetic Foot Ulcer: A Randomized, Double-blind Clinical Trial. Curr. Drug Discov. Technol. 2023, in press. [Google Scholar] [CrossRef]
- Derrien, M.; Alvarez, A.S.; de Vos, W.M. The Gut Microbiota in the First Decade of Life. Trends Microbiol. 2019, 27, 997–1010. [Google Scholar] [CrossRef]
- Liu, C.; Du, P.; Cheng, Y.; Guo, Y.; Hu, B.; Yao, W.; Zhu, X.; Qian, H. Study on Fecal Fermentation Characteristics of Aloe Polysaccharides in vitro and their Predictive Modeling. Carbohydr. Polym. 2021, 256, 117571. [Google Scholar] [CrossRef] [PubMed]
- Gullón, B.; Gullón, P.; Tavaria, F.; Alonso, J.L.; Pintado, M. In vitro Assessment of the Prebiotic Potential of Aloe vera Mucilage and its Impact on the Human Microbiota. Food Funct. 2015, 6, 525–531. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, S.; Noor, A.; Tariq, M.; Zaidi, A. Functional Improvement of Synbiotic Yogurt Enriched with Lacticaseibacillus rhamnosus and Aloe vera Gel Using the Response Surface Method. Food Prod. Process. Nutr. 2023, 5, 38. [Google Scholar] [CrossRef]
- Dobson, R.; Giovannoni, G. Multiple sclerosis–A review. Eur. J. Neurol. 2019, 26, 27–40. [Google Scholar] [CrossRef] [PubMed]
- Chen, Z.; Lv, Y.; Xu, H.; Deng, L. Herbal Medicine, Gut Microbiota, and COVID-19. Front. Pharmacol. 2021, 12, 646560. [Google Scholar] [CrossRef] [PubMed]
- Najmi, N.; Megantara, I.; Andriani, L.; Goenawan, H.; Lesmana, R. Importance of Gut Microbiome Regulation for the Prevention and Recovery Process after SARS-CoV-2 Respiratory Viral Infection. Biomed. Rep. 2022, 16, 25. [Google Scholar] [CrossRef] [PubMed]
- Soleymani, S.; Naghizadeh, A.; Karimi, M.; Zarei, A.; Mardi, R.; Kordafshari, G.; Esmaealzadeh, N.; Zargaran, A. COVID-19: General Strategies for Herbal Therapies. J. Evid. Based Integr. Med. 2022, 27, 2515690X211053641. [Google Scholar] [CrossRef] [PubMed]
- Mondal, P.; Sindhu, R.; Nimmy, P.; Bharathwaj, V.V.; Damodhar, D.; Sathiyapriya, S.; Prabu, L.; Mohan, M.R. Role of Aloe vera and its Clinical Efficiency on Dental Caries: A Systematic Review. Int. J. Mod. Dev. Eng. Sci. 2022, 1, 85–89. [Google Scholar]
- Iacopetta, D.; Ceramella, J.; Catalano, A.; D’Amato, A.; Lauria, G.; Saturnino, C.; Andreu, I.; Longo, P.; Sinicropi, M.S. Diarylureas: New Promising Small Molecules against Streptococcus mutans for the Treatment of Dental Caries. Antibiotics 2023, 12, 112. [Google Scholar] [CrossRef]
- Fani, M.; Kohanteb, J. Inhibitory Activity of Aloe vera Gel on Some Clinically Isolated Cariogenic and Periodontopathic Bacteria. J. Oral Sci. 2012, 54, 15–21. [Google Scholar] [CrossRef]
- Al-Abdullah, A.; Edris, S.; Abu Hasna, A.; de Carvalho, L.S.; Al-Nahlawi, T. The Effect of Aloe vera and Chlorhexidine as Disinfectants on the Success of Selective Caries Removal Technique: A Randomized Controlled Trial. Int. J. Dent. 2022, 2022, 9474677. [Google Scholar] [CrossRef] [PubMed]
- Wardhana, Y.W.; Warya, S.; Trisnawaty, A. Formulation of Toothpaste Gel Containing Mixture of Aloe vera (Aloe barbadensis Mill.) and Red Betel (Piper crocatum) Extract in Prevention of Dental Caries. J. Pharm. Sci. Res. 2017, 9, 2172–2174. [Google Scholar]
- Pattnaik, N.; Mohanty, R.; Satpathy, A.; Nayak, R.; Shamim, R.; Praharaj, A.K. Aloe vera Mouthwashes Can Be a Natural Alternative to Chemically Formulated Ones—A Randomized-Controlled Trial. J. Taibah Univ. Med. Sci. 2022, 17, 424–432. [Google Scholar] [CrossRef] [PubMed]
- Nisha, D.S.; Biju, S.; Kalappurakkal, R.; Kirubakaran, R. Efficacy of Aloe vera and Probiotic Mouthwashes vs Fluoride Mouthwash on Streptococcus mutans in Plaque Around Brackets of Orthodontic Patients: A Randomized Clinical Trial. Angle Orthodontist. 2023; in press. [Google Scholar] [CrossRef]
- Naghsh, N.; Moghareabed, A.; Nematnejad, M.; Yaghini, J.; Sadeghi, S.M. A Comparative Evaluation of the Antimicrobial Effect of Chamomile, Aloe vera-Green Tea, and Chlorhexidine Mouthwashes on Some Oral Bacterial Species. Dent. Res. J. 2023, 20, 70. [Google Scholar] [CrossRef]
- Soares, I.M.V.; Fernandes, G.V.D.O.; Cavalcante, L.C.; Leite, Y.K.P.D.C.; Bezerra, D.D.O.; Carvalho, M.A.M.D.; Carvalho, C.M.R.S. The Influence of Aloe vera with Mesenchymal Stem Cells from Dental Pulp on Bone Regeneration: Characterization and Treatment of Non-critical Defects of the Tibia in Rats. J. Appl. Oral Sci. 2019, 27, e20180103. [Google Scholar] [CrossRef] [PubMed]
- Tariq, R.; Khurshid, Z.; Farooqui, W.A.; Adanir, N. Anti-bacterial Efficacy of Aloe vera against E. faecalis as Compared to Other Intracanal Medicaments: A Systematic Review and Meta-analysis. Saudi Dent. J. 2023, 35, 451–467. [Google Scholar] [CrossRef] [PubMed]
- Ghasemi, N.; Behnezhad, M.; Asgharzadeh, M.; Zeinalzadeh, E.; Kafil, H.S. Antibacterial Properties of Aloe vera on Intracanal Medicaments against Enterococcus faecalis Biofilm at Different Stages of Development. Int. J. Dent. 2020, 2020, 8855277. [Google Scholar] [CrossRef]
- Babaee, N.; Zabihi, E.; Mohseni, S.; Moghadamnia, A.A. Evaluation of the therapeutic effects of Aloe vera gel on minor recurrent aphthous stomatitis. Dent. Res. J. 2012, 9, 381–385. [Google Scholar] [PubMed] [PubMed Central]
- Salehi, B.; Lopez-Jornet, P.; Pons-Fuster López, E.; Calina, D.; Sharifi-Rad, M.; Ramírez-Alarcón, K.; Forman, K.; Fernández, M.; Martorell, M.; Setzer, W.N.; et al. Plant-derived Bioactives in Oral Mucosal Lesions: A Key Emphasis to Curcumin, Lycopene, Chamomile, Aloe vera, Green Tea and Coffee Properties. Biomolecules 2019, 9, 106. [Google Scholar] [CrossRef]
- Jeevitha, T.; Deepa, K.; Michael, A. In Vitro Study on the Anti-microbial Efficacy of Aloe vera against Candida albicans. Afr. J. Microbiol. Res. 2018, 12, 930–937. [Google Scholar] [CrossRef]
- Rezvaninejad, R.; Rezvaninejad, R.; Ashoorian, M.J.; Talebi, M. Comparison of Effect of Aloe vera Gel and Nystatin on Candida Species: An In Vitro Study. Jundishapur J. Health Sci. 2022, 14, e122029. [Google Scholar] [CrossRef]
- Pouyafard, A.; Jabbaripour, N.; Jafari, A.A.; Owlia, F. Investigating the Anti-fungal Activity of Different Concentrations of Aloe vera in Candida albicans Infection under In Vitro Conditions. J. Adv. Med. Biomed. Res. 2023, 31, 268–274. [Google Scholar] [CrossRef]
- Chen, X.; Xie, H.; Guo, J. Drug Treatment for Oral Submucous Fibrosis: An Update. BMC Oral Health 2023, 23, 748. [Google Scholar] [CrossRef]
- Nigam, S.; Saxena, R.; Singh, S.; Jain, R.; Thomas, S. Comparative Evaluation of Aloe vera, Curcumin, and Lycopene in Oral Submucous Fibrosis Patients–A Randomized Controlled Trial. J. Precis. Oncol. 2023, 3, 35–39. [Google Scholar] [CrossRef]
- Daly, B.J.M.; Sharif, M.O.; Jones, K.; Worthington, H.V.; Beattie, A. Local Interventions for the Management of Alveolar Osteitis (Dry Socket). Cochrane Database Syst. Rev. 2022, 2022, CD006968. [Google Scholar] [CrossRef] [PubMed]
- Alhalabi, N.R.; Jaafo, M.H.; Mourad, R.; Alkhouli, M.; Al-Nerabieah, Z. The Effectiveness of Intra-alveolar Aloe vera Extract Powder on Reducing the Incidence of Dry Socket after Tooth Extraction: A Randomized Controlled Clinical Trial. Oral Surg. 2023, 16, 195–200. [Google Scholar] [CrossRef]
- Mansouri, P.; Haghighi, M.; Beheshtipour, N.; Ramzi, M. The Effect of Aloe vera Solution on Chemotherapy-induced Stomatitis in Clients with Lymphoma and Leukemia: A Randomized Controlled Clinical Trial. Int. J. Community Based Nurs. Midwifery 2016, 4, 119–126. [Google Scholar] [PubMed]
- Karbasizade, S.; Ghorbani, F.; Ghasemi Darestani, N.; Mansouri-Tehrani, M.M.; Kazemi, A.H. Comparison of Therapeutic Effects of Statins and Aloe vera Mouthwash on Chemotherapy Induced Oral Mucositis. Int. J. Physiol. Pathophysiol. Pharmacol. 2021, 13, 110–116. [Google Scholar] [PubMed] [PubMed Central]
- Alkhouli, M.; Laflouf, M.; Alhaddad, M. Efficacy of Aloe-vera Use for Prevention of Chemotherapy-induced Oral Mucositis in Children with Acute Lymphoblastic Leukemia: A Randomized Controlled Clinical Trial. Compr. Child Adolesc. Nurs. 2021, 44, 49–62. [Google Scholar] [CrossRef]
- Sahebjamee, M.; Mansourian, A.; Hajimirzamohammad, M.; Zadeh, M.T.; Bekhradi, R.; Kazemian, A.; Manifar, S.; Ashnagar, S.; Doroudgar, K. Comparative Efficacy of Aloe vera and Benzydamine Mouthwashes on Radiation-induced Oral Mucositis: A Triple-Blind, Randomised, Controlled Clinical Trial. Oral Health Prev. Dent. 2015, 13, 309–315. [Google Scholar] [CrossRef] [PubMed]
- Michalak, M. Plant Extracts as Skin Care and Therapeutic Agents. Int. J. Mol. Sci. 2023, 24, 15444. [Google Scholar] [CrossRef] [PubMed]
- Sinicropi, M.S.; Iacopetta, D.; Ceramella, J.; Catalano, A.; Mariconda, A.; Pellegrino, M.; Saturnino, C.; Longo, P.; Aquaro, S. Triclosan: A Small Molecule with Controversial Roles. Antibiotics 2022, 11, 735. [Google Scholar] [CrossRef] [PubMed]
- Sethi, A.; Kaur, T.; Malhotra, S.K.; Gambhir, M.L. Moisturizers: The Slippery Road. Indian J. Dermatol. 2016, 61, 279–287. [Google Scholar] [CrossRef] [PubMed]
- Mawazi, S.M.; Ann, J.; Othman, N.; Khan, J.; Alolayan, S.O.; Al Thagfan, S.S.; Kaleemullah, M. A Review of Moisturizers; History, Preparation, Characterization and Applications. Cosmetics 2022, 9, 61. [Google Scholar] [CrossRef]
- Daverey, A.; Dutta, K. COVID-19: Eco-friendly Hand Hygiene for Human and Environmental Safety. J. Environ. Chem. Eng. 2021, 9, 104754. [Google Scholar] [CrossRef]
- Booq, R.Y.; Alshehri, A.A.; Almughem, F.A.; Zaidan, N.M.; Aburayan, W.S.; Bakr, A.A.; Kabli, S.H.; Alshaya, H.A.; Alsuabeyl, M.S.; Alyamani, E.J.; et al. Formulation and Evaluation of Alcohol-Free Hand Sanitizer Gels to Prevent the Spread of Infections during Pandemics. Int. J. Environ. Res. Public Health 2021, 18, 6252. [Google Scholar] [CrossRef] [PubMed]
- Valverde, J.M.; Valero, D.; Martínez-Romero, D.; Guillén, F.; Castillo, S.; Serrano, M. Novel Edible Coating Based on Aloe vera Gel to Maintain Table Grape Quality and Safety. J. Agric. Food Chem. 2005, 53, 7807–7813. [Google Scholar] [CrossRef]
- Martínez-Romero, D.; Zapata, P.J.; Guillén, F.; Paladines, D.; Castillo, S.; Valero, D.; Serrano, M. The Addition of Rosehip Oil to Aloe gels Improves their Properties as Postharvest Coatings for Maintaining Quality in Plum. Food Chem. 2017, 217, 585–592. [Google Scholar] [CrossRef]
- Nicolau-Lapena, I.; Colas-Meda, P.; Alegre, I.; Aguilo-Aguayo, I.; Muranyi, P.; Vinas, I. Aloe vera Gel: An Update on its Use as a Functional Edible Coating to Preserve Fruits and Vegetables. Prog. Org. Coat. 2021, 151, 106007. [Google Scholar] [CrossRef]
- Hasan, M.U.; Riaz, R.; Malik, A.U.; Khan, A.S.; Anwar, R.; Rehman, R.N.U.; Ali, S. Potential of Aloe vera Gel Coating for Storage Life Extension and Quality Conservation of Fruits and Vegetables: An Overview. J. Food Biochem. 2021, 45, e13640. [Google Scholar] [CrossRef] [PubMed]
- Hassanpour, H. Effect of Aloe vera Gel Coating on Antioxidant Capacity, Antioxidant Enzyme Activities and Decay in Raspberry Fruit. LWT 2015, 60, 495–501. [Google Scholar] [CrossRef]
- Partoazar, A.; Afrasiabi, S.; Ghasemzadeh, F.; Ghazi-Khansari, M.; Dallal, M.M.S. Antimicrobial Activity of Zeolite/Zinc Oxide Nanocomposite Containing Aloe vera Gel against Shigella spp. and Its Durability Effects on Strawberries. BioNanoScience 2023, 13, 2096–2102. [Google Scholar] [CrossRef]
- Hassan, H.S.; EL-Hefny, M.; Ghoneim, I.M.; El-Lahot, M.S.R.A.; Akrami, M.; Al-Huqail, A.A.; Ali, H.M.; Abd-Elkader, D.Y. Assessing the Use of Aloe vera Gel Alone and in Combination with Lemongrass Essential Oil as a Coating Material for Strawberry Fruits: HPLC and EDX Analyses. Coatings 2022, 12, 489. [Google Scholar] [CrossRef]
- Ahmad, F.; Muhammad, A.; Hashmi, M.S.; Ahmad, A.; Alam, S.; Din, K.U.; Siyab, A. Pre-storage Calcium Chloride and Aloe vera Gel Coatings Mitigate Internal Browning and Senescence Scald in ‘Conference’ Pears. Sci. Horticult. 2024, 325, 112684. [Google Scholar] [CrossRef]
- Soltan Dallal, M.M.; Karimaei, S.; Hajighasem, M.; Hashemi, S.J.; Rahimi Foroushani, A.; Ghazi-Khansari, M.; Partoazar, A. Evaluation of Zinc Oxide Nanocomposite with Aloe vera Gel for Packaging of Chicken Fillet against Salmonella typhi and Salmonella para typhi A. Food Sci. Nutr. 2023, 11, 5882–5889. [Google Scholar] [CrossRef]
- Kouser, F.; Kumar, S.; Bhat, H.F.; Hassoun, A.; Bekhit, A.E.-D.A.; Bhat, Z.F. Aloe barbadensis Based Bioactive Edible Film Improved Lipid Stability and Microbial Quality of the Cheese. Foods 2023, 12, 229. [Google Scholar] [CrossRef]
- Kaur, N.; Somasundram, C.; Razali, Z.; Mourad, A.H.I.; Hamed, F.; Ahmed, Z.F. Aloe vera/Chitosan-Based Edible Film with Enhanced Antioxidant, Antimicrobial, Thermal, and Barrier Properties for Sustainable Food Preservation. Polymers 2024, 16, 242. [Google Scholar] [CrossRef]
- Sánchez, M.; González-Burgos, E.; Iglesias, I.; Gómez-Serranillos, M.P. Pharmacological update properties of Aloe vera and its major active constituents. Molecules 2020, 25, 1324. [Google Scholar] [CrossRef]
- Choi, S.W.; Chung, M.-H. A Review on the Relationship between Aloe vera Components and their Biologic Effects. Semin. Integr. Med. 2003, 1, 53–62. [Google Scholar] [CrossRef]
- Babu, S.N.; Noor, A. Bioactive Constituents of the Genus Aloe and their Potential Therapeutic and Pharmacological Applications: A Review. J. Appl. Pharm. Sci. 2020, 10, 133–145. [Google Scholar] [CrossRef]
- Ni, Y.; Turner, D.; Yates, K.M.; Tizard, I. Isolation and Characterization of Structural Components of Aloe vera L. Leaf Pulp. Int. Immunopharmacol. 2004, 4, 1745–1755. [Google Scholar] [CrossRef]
- Dagne, E.; Bisrat, D.; Viljoen, A.; Van Wyk, B.E. Chemistry of Aloe species. Curr. Org. Chem. 2000, 4, 1055–1078. [Google Scholar] [CrossRef]
- Sadiq, U.; Gill, H.; Chandrapala, J. Temperature and pH Stability of Anthraquinones from Native Aloe vera Gel, Spray-Dried and Freeze-Dried Aloe vera Powders during Storage. Foods 2022, 11, 1613. [Google Scholar] [CrossRef] [PubMed]
- Lv, L.; Yang, Q.Y.; Zhao, Y.; Yao, C.S.; Sun, Y.; Yang, E.J.; Fang, W.S. BACE1 (β-secretase) Inhibitory Chromone Glycosides from Aloe vera and Aloe nobilis. Planta Med. 2008, 74, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Eshun, K.; He, Q. Aloe vera: A Valuable Ingredient for the Food, Pharmaceutical and Cosmetic Industries—A Review. Crit. Rev. Food Sci. Nutr. 2004, 44, 91–96. [Google Scholar] [CrossRef]
- Lanka, S. A Review on Aloe vera-the Wonder Medicinal Plant. J. Drug Deliv. Ther. 2018, 8, 94–99. [Google Scholar] [CrossRef]
- Meadows, T.P. Aloe as a Humectant in New Skin Preparations. Cosmet. Toilet. 1980, 95, 51–56. [Google Scholar]
- Ahmed, M.; Hussain, F. Chemical Composition and Biochemical Activity of Aloe vera (Aloe barbadensis Miller) Leaves. Int. J. Chem. Biochem. Sci. 2013, 3, 29–33. [Google Scholar]
- Sohag, A.A.M.; Hossain, M.T.; Rahaman, M.A.; Rahman, P.; Hasan, M.S.; Das, R.C.; Khan, M.K.; Sikder, M.H.; Alam, M.; Uddin, M.J.; et al. Molecular Pharmacology and Therapeutic Advances of the Pentacyclic Triterpene Lupeol. Phytomedicine 2022, 99, 154012. [Google Scholar] [CrossRef]
- Darzi, S.; Paul, K.; Leitan, S.; Werkmeister, J.A.; Mukherjee, S. Immunobiology and Application of Aloe vera-based Scaffolds in Tissue Engineering. Int. J. Mol. Sci. 2021, 22, 1708. [Google Scholar] [CrossRef] [PubMed]
- Sabeh, F.; Wright, T.; Norton, S. Isozymes of Superoxide Dismutase from Aloe Vera. Enzym. Protein 1996, 49, 212–221. [Google Scholar] [CrossRef]
- Nalimu, F.; Oloro, J.; Kahwa, I.; Ogwang, P.E. Review on the Phytochemistry and Toxicological Profiles of Aloe vera and Aloe ferox. Futur. J. Pharm. Sci. 2021, 7, 145. [Google Scholar] [CrossRef]
- Friedman, M.; Xu, A.; Lee, R.; Nguyen, D.N.; Phan, T.A.; Hamada, S.M.; Panchel, R.; Tam, C.C.; Kim, J.H.; Cheng, L.W.; et al. Pathogenic protozoa, bacteria, and fungi and the relationship to structure. Molecules 2020, 25, 3101. [Google Scholar] [CrossRef]
- Malik, E.M.; Muller, C.E. Anthraquinones as pharmacological tools and drugs. Med. Res. Rev. 2016, 36, 705–748. [Google Scholar] [CrossRef] [PubMed]
- Parvez, M.K.; Al-Dosari, M.S.; Alam, P.; Rehman, M.; Alajmi, M.F.; Alqahtani, A.S. The anti-hepatitis B virus therapeutic potential of anthraquinones derived from Aloe vera. Phytother. Res. 2019, 33, 2960–2970. [Google Scholar] [CrossRef] [PubMed]
- Maheshwari, N.; Sharma, M.C. Anticancer properties of some selected plant phenolic compounds: Future leads for therapeutic development. J. Herb. Med. 2023, 42, 100801. [Google Scholar] [CrossRef]
- Nowak-Perlak, M.; Bromke, M.A.; Ziółkowski, P.; Woźniak, M. The Comparison of the Efficiency of Emodin and Aloe-emodin in Photodynamic Therapy. Int. J. Mol. Sci. 2022, 23, 6276. [Google Scholar] [CrossRef] [PubMed]
- Sulaiman, C.; George, B.P.; Balachandran, I.; Abrahamse, H. Photoactive Herbal Compounds: A Green Approach to Photodynamic Therapy. Molecules 2022, 27, 5084. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Zeng, Y.; Liu, Y.; You, L.; Yin, X.; Fu, J.; Ni, J. Aloe-emodin: A Review of its Pharmacology, Toxicity, and Pharmacokinetics. Phytother. Res. 2021, 34, 270–281. [Google Scholar] [CrossRef] [PubMed]
- Shang, H.; Guo, J.; Wang, P.; Li, L.; Tian, Y.; Li, X.; Zou, Z. Design, Synthesis and Anti-inflammatory Evaluation of Aloe-emodin Derivatives as Potential Modulators of Akt, NF-κB and JNK Signaling Pathways. Eur. J. Med. Chem. 2022, 238, 114511. [Google Scholar] [CrossRef] [PubMed]
- Su, Z.-L.; Hang, P.-Z.; Hu, J.; Zheng, Y.-Y.; Sun, H.-Q.; Guo, J.; Liu, K.-Y.; Du, Z.-M. Aloe-emodin Exerts Cholesterol-lowering Effects by Inhibiting Proprotein Convertase Subtilisin/kexin Type 9 in Hyperlipidemic Rats. Acta Pharmacol. Sin. 2020, 41, 1085–1092. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.; Liu, H.; Yang, D.; He, F.; Yuan, Y.; Guo, J.; Hu, J.; Yu, J.; Yan, X.; Wang, S.; et al. Aloe-Emodin Attenuates Myocardial Infarction and Apoptosis Via Up-Regulating MiR-133 Expression. Pharmacol. Res. 2019, 146, 104315. [Google Scholar] [CrossRef]
- Chen, Y.; Feng, B.; Yuan, Y.; Hu, J.; Zhao, W.; Jiang, H.; Li, W.; Fan, Z.; Du, Z. Aloe Emodin Reduces Cardiac Inflammation Induced by a High-Fat Diet through the TLR4 Signaling Pathway. Mediat. Inflamm. 2020, 2020, 6318520. [Google Scholar] [CrossRef] [PubMed]
- Sapkota, M.; Shrestha, S.K.; Yang, M.; Park, Y.R.; Soh, Y. Aloe-emodin Inhibits Osteogenic Differentiation and Calcification of Mouse Vascular Smooth Muscle Cells. Eur. J. Pharmacol. 2019, 865, 172772. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Su, Z.; Sun, H.; Zhao, W.; Chen, X.; Hang, P.; Zhu, W.; Du, Z. Aloe-emodin Relieves High-fat diet Induced QT Prolongation via MiR-1 Inhibition and IK1 Up-regulation in Rats. Cell. Physiol. Biochem. 2017, 43, 1961–1973. [Google Scholar] [CrossRef] [PubMed]
- Seker Karatoprak, G.; Kupeli Akkol, E.; Yucel, C.; Bahadir Acikara, O.; Sobarzo-Sanchez, E. Advances in Understanding the Role of Aloe Emodin and Targeted Drug Delivery Systems in Cancer. Oxid Med. Cell Longev. 2022, 2022, 7928200. [Google Scholar] [CrossRef] [PubMed]
- Trybus, W.; Krol, T.; Trybus, E.; Stachurska, A.; Kopacz-Bednarska, A.; Krol, G. Induction of Mitotic Catastrophe in Human Cervical Cancer Cells after Administration of Aloe-emodin. Anticancer Res. 2018, 38, 2037–2044. [Google Scholar] [CrossRef] [PubMed]
- Tabolacci, C.; Cordella, M.; Turcano, L.; Rossi, S.; Lentini, A.; Mariotti, S.; De Maria, R. Aloe-emodin Exerts a Potent Anticancer and Immunomodulatory Activity on BRAF-mutated Human Melanoma Cells. Eur. J. Pharmacol. 2015, 762, 283–292. [Google Scholar] [CrossRef] [PubMed]
- Stringaro, A.; Serra, S.; Gori, A.; Calcabrini, A.; Colone, M.; Dupuis, M.L.; Spadaro, F.; Cecchetti, S.; Vitali, A. Peptide-Mediated Targeted Delivery of Aloe-emodin as Anticancer Drug. Molecules 2022, 27, 4615. [Google Scholar] [CrossRef]
- Iacopetta, D.; Ceramella, J.; Baldino, N.; Sinicropi, M.S.; Catalano, A. Targeting Breast Cancer: An Overlook on Current Strategies. Int. J. Mol. Sci. 2023, 24, 3643. [Google Scholar] [CrossRef] [PubMed]
- Sanders, B.; Ray, A.M.; Goldberg, S.; Clark, T.; McDaniel, H.R.; Atlas, S.E.; Farooqi, A.; Konefal, J.; Lages, L.C.; Lopez, J.; et al. Anti-cancer Effects of Aloe-emodin: A Systematic Review. J. Clin. Transl. Res. 2017, 3, 283–296. [Google Scholar] [CrossRef]
- Liu, K.; Park, C.; Li, S.; Lee, K.W.; Liu, H.; He, L.; Soung, N.K.; Ahn, J.S.; Bode, A.M.; Dong, Z. Aloe-emodin Suppresses Prostate Cancer by Targeting the mTOR Complex 2. Carcinogenesis 2012, 33, 1406–1411. [Google Scholar] [CrossRef] [PubMed]
- Kuo, P.-L.; Lin, T.-C.; Lin, C.-C. The antiproliferative activity of aloe-emodin is through p53-dependent and p21-dependent apoptotic pathway in human hepatoma cell lines. Life Sci. 2002, 71, 1879–1892. [Google Scholar] [CrossRef] [PubMed]
- Chang, X.; Zhao, J.; Tian, F.; Jiang, Y.; Lu, J.; Ma, J.; Liu, K. Aloe-emodin Suppresses Esophageal Cancer Cell TE1 Proliferation by Inhibiting AKT and ERK Phosphorylation. Oncol. Lett. 2016, 12, 2232–2238. [Google Scholar] [CrossRef]
- Zhang, J.; Guo, L.; Zhang, Q.; Liu, K.; Dong, Z. Aloe Emodin Suppresses EGF-induced Neoplastic Cell Transformation by Inhibiting the ERK/MSK1 and AKT/GSK3β Signaling Pathways. Mol. Med. Rep. 2018, 18, 5215–5220. [Google Scholar] [CrossRef]
- Meng, X.; An, X.; Zhou, L.; Fu, B.; Jia, L. The Isomers, Aloe-emodin and Emodin, Possess Differential Inhibitory Activities Against CYP1B1 Enzyme. Steroids 2022, 185, 109055. [Google Scholar] [CrossRef]
- Su, J.; Chen, S.; Xiao, J.; Feng, Z.; Hu, S.; Su, Q.; Chen, Q.; Chen, D. Aloe-emodin Ameliorates Cecal Ligation and Puncture-Induced Sepsis. Int. J. Mol. Sci. 2023, 24, 11972. [Google Scholar] [CrossRef]
- Furkan, M.; Alam, M.T.; Rizvi, A.; Khan, K.; Ali, A.; Naeem, A. Aloe emodin, an Anthroquinone from Aloe vera acts as an Anti Aggregatory Agent to the Thermally Aggregated Hemoglobin. Spectrochim. Acta Part A Mol. Biomol. Spectrosc. 2017, 179, 188–193. [Google Scholar] [CrossRef]
- Gallo, V.; Arienzo, A.; Iacobelli, S.; Iacobelli, V.; Antonini, G. Gal-3BP in Viral Infections: An Emerging Role in Severe Acute Respiratory Syndrome Coronavirus 2. Int. J. Mol. Sci. 2022, 23, 7314. [Google Scholar] [CrossRef]
- Li, S.W.; Yang, T.C.; Lai, C.C.; Huang, S.H.; Liao, J.M.; Wan, L.; Lin, Y.J.; Lin, C.W. Antiviral Activity of Aloe-emodin against Influenza A virus via Galectin-3 up-regulation. Eur. J. Pharm. 2014, 738, 125–132. [Google Scholar] [CrossRef] [PubMed]
- Zeng, H.J.; Liu, Z.; Hu, G.Z.; Qu, L.B.; Yang, R. Investigation on the Binding of Aloe-emodin with Tyrosinase by Spectral Analysis and Molecular Docking. Spectrochim. Acta Mol. Biomol. Spectrosc. 2019, 211, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Ma, W.P.; Liu, C.C.; Li, J.; Hao, M.; Ji, Y.H.; Zeng, X.Y. The Effects of Aloe Emodin-mediated Antimicrobial Photodynamic Therapy on Drug-sensitive and Resistant Candida albicans. Photochem. Photobiol. Sci. 2020, 19, 485–494. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.; Cao, T.; Li, Y.; Hu, Y.; Yang, H.; Yin, S. Synthesized Derivatives of Aloe-emodin as Proliferation Inhibitors for Human Breast Adenocarcinoma, Human Nonsmall Cell Lung Carcinoma, and Human Cervix Carcinoma. Chem. Nat. Compd. 2020, 56, 30–33. [Google Scholar] [CrossRef]
- Chen, R.; Wang, S.; Zhang, J.; Chen, M.; Wang, Y. Aloe-emodin Loaded Solid Lipid Nanoparticles: Formulation Design and In Vitro Anti-cancer Study. Drug Deliv. 2015, 22, 666–674. [Google Scholar] [CrossRef] [PubMed]
- Vath, P.; Wamer, W.G.; Falvey, D.E. Photochemistry and Phototoxicity of Aloe Emodin. Photochem. Photobiol. 2002, 75, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Younes, M.; Aggett, P.; Aguilar, F.; Crebelli, R.; Filipič, M.; Frutos, M.J.; Galtier, P.; Gott, D.; Gundert-Remy, U.; Kuhnle, G.G.; et al. Safety of hydroxyanthracene derivatives for use in food. EFSA J. 2018, 16, e05090. Available online: https://efsa.onlinelibrary.wiley.com/doi/epdf/10.2903/j.efsa.2018.5090 (accessed on 7 July 2024). [PubMed]
- Quan, Y.; Gong, L.; He, J.; Zhou, Y.; Liu, M.; Cao, Z.; Li, Y.; Peng, C. Aloe emodin induces hepatotoxicity by activating NF-κB inflammatory pathway and P53 apoptosis pathway in zebrafish. Toxicol. Lett. 2019, 306, 66–79. [Google Scholar] [CrossRef] [PubMed]
- Galli, C.L.; Cinelli, S.; Ciliutti, P.; Melzi, G.; Marinovich, M. Aloe-emodin, a hydroxyanthracene derivative, is not genotoxic in an in vivo comet test. Regul. Toxicol. Pharmacol. 2021, 124, 104967. [Google Scholar] [CrossRef]
- Dong, X.; Fu, J.; Yin, X.; Cao, S.; Li, X.; Lin, L.; Huyiligeqi; Ni, J. Emodin: A Review of its Pharmacology, Toxicity and Pharmacokinetics. Phytother. Res. 2016, 30, 1207–1218. [Google Scholar] [CrossRef]
- Li, Q.; Gao, J.; Pang, X.; Chen, A.; Wang, Y. Molecular Mechanisms of Action of Emodin: As an Anti-cardiovascular Disease Drug. Front. Pharmacol. 2020, 11, 559607. [Google Scholar] [CrossRef] [PubMed]
- Luo, N.; Fang, J.; Wei, L.; Sahebkar, A.; Little, P.J.; Xu, S.; Luo, C.; Li, G. Emodin in Atherosclerosis Prevention: Pharmacological Actions and Therapeutic Potential. Eur. J. Pharmacol. 2021, 890, 173617. [Google Scholar] [CrossRef] [PubMed]
- Trybus, W.; Król, T.; Trybus, E.; Kopacz-Bednarska, A.; Król, G.; Karpowicz, E. Changes in the Lysosomal System of Cervical Cancer Cells Induced by Emodin Action. Anticancer Res. 2017, 37, 6087–6096. [Google Scholar] [CrossRef] [PubMed]
- Liu, A.; Chen, H.; Wei, W.; Ye, S.; Liao, W.; Gong, J.; Jiang, Z.; Wang, L.; Lin, S. Antiproliferative and Antimetastatic Effects of Emodin on Human Pancreatic Cancer. Oncol. Rep. 2011, 26, 81–89. [Google Scholar] [CrossRef] [PubMed]
- Akkol, E.K.; Tatlı, I.I.; Karatoprak, G.Ş.; Ağar, O.T.; Yücel, Ç.; Sobarzo-Sánchez, E.; Capasso, R. Is Emodin with Anticancer Effects Completely Innocent? Two Sides of the Coin. Cancers 2021, 13, 2733. [Google Scholar] [CrossRef] [PubMed]
- Ceramella, J.; Iacopetta, D.; Franchini, A.; De Luca, M.; Saturnino, C.; Andreu, I.; Sinicropi, M.S.; Catalano, A. A Look at the Importance of Chirality in Drug Activity: Some Significative Examples. Appl. Sci. 2022, 12, 10909. [Google Scholar] [CrossRef]
- Cardarelli, M.; Rouphael, Y.; Pellizzoni, M.; Colla, G.; Lucini, L. Profile of Bioactive Secondary Metabolites and Antioxidant Capacity of Leaf Exudates from Eighteen Aloe Species. Ind. Crops Prod. 2017, 108, 44–51. [Google Scholar] [CrossRef]
- Wamer, W.G.; Vath, P.; Falvey, D.E. In Vitro Studies on the Photobiological Properties of Aloe Emodin and Aloin A. Free Radic. Biol. Med. 2003, 34, 233–242. [Google Scholar] [CrossRef]
- Park, M.-Y.; Kwon, H.-J.; Sung, M.-K. Evaluation of Aloin and Aloe-emodin as Anti-inflammatory Agents in Aloe by Using Murine Macrophages. Biosci. Biotechnol. Biochem. 2009, 73, 828–832. [Google Scholar] [CrossRef]
- Liu, F.W.; Liu, F.C.; Wang, Y.R.; Tsai, H.I.; Yu, H.P. Aloin protects skin fibroblasts from heat stress-induced oxidative stress damage by regulating the oxidative defense system. PLoS ONE 2015, 10, e0143528. [Google Scholar] [CrossRef]
- Wan, L.; Zhang, L.; Fan, K.; Wang, J. Aloin Promotes A549 Cell Apoptosis via the Reactive Oxygen Species Mitogen Activated Protein Kinase Signaling Pathway and p53 Phosphorylation. Mol. Med. Rep. 2017, 16, 5759–5768. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Wu, J.J.; Xia, J.; Wan, Y.; Xu, J.F.; Zhang, L.; Liu, D.; Chen, L.; Tang, F.; Ao, H.; et al. Can Aloin Develop to Medicines or Healthcare Products? Biomed. Pharmacother. 2022, 153, 113421. [Google Scholar] [CrossRef] [PubMed]
- Chang, R.Y.; Zhou, R.; Qi, X.; Wang, J.; Wu, F.; Yang, W.L.; Zhang, W.N.; Sun, T.; Li, Y.X.; Yu, J.Q. Protective Effects of Aloin on Oxygen and Glucose Deprivation-Induced Injury in PC12 Cells. Brain Res. Bull. 2016, 121, 75–83. [Google Scholar] [CrossRef] [PubMed]
- Pengjam, Y.; Madhyastha, H.; Madhyastha, R.; Yamaguchi, Y.; Nakajima, Y.; Maruyama, M. NF-κB Pathway Inhibition by Anthrocyclic Glycoside Aloin Is Key Event in Preventing Osteoclastogenesis in RAW264.7 Cells. Phytomedicine 2016, 23, 417–428. [Google Scholar] [CrossRef] [PubMed]
- Pengjam, Y.; Madhyastha, H.; Madhyastha, R.; Yamaguchi, Y.; Nakajima, Y.; Maruyama, M. Anthraquinone Glycoside Aloin Induces Osteogenic Initiation of MC3T3-E1 Cells: Involvement of MAPK Mediated Wnt and Bmp Signaling. Biomol. Ther. 2016, 24, 123. [Google Scholar] [CrossRef] [PubMed]
- Xiao, J.; Chen, S.; Chen, Y.; Su, J. The Potential Health Benefits of Aloin from Genus Aloe. Phytother. Res. 2022, 36, 873–890. [Google Scholar] [CrossRef] [PubMed]
- Boudreau, M.D.; Olson, G.R.; Tryndyak, V.P.; Bryant, M.S.; Felton, R.P.; Beland, F.A. From the Cover: Aloin, a Component of the Aloe vera Plant Leaf, Induces Pathological Changes and Modulates the Composition of Microbiota in the Large Intestines of F344/N Male Rats. Toxicol. Sci. 2017, 158, 302–318. [Google Scholar] [CrossRef] [PubMed]
- Ma, Y.; Tang, T.; Sheng, L.; Wang, Z.; Tao, H.; Zhang, Q.; Qi, Z. Aloin Suppresses Lipopolysaccharide-induced Inflammation by Inhibiting JAK1-STAT1/3 Activation and ROS Production in RAW264.7 Cells. Int. J. Mol. Med. 2018, 42, 1925–1934. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.; Xiang, X.; Zhang, Y.; Tian, Z.; Wang, L. Aloin Promotes Oral Squamous Cell Carcinoma Cell Apoptosis and Autophagy through Akt/mTOR Pathway. Qual. Assur. Safety Crops Foods 2022, 14, 58–65. [Google Scholar] [CrossRef]
- Tao, H.; Tang, T.; Wang, S.; Wang, Z.; Ma, Y.; Cai, T.; Cheng, X.; Qi, S.; Zhang, Y.; Qi, Z. The molecular mechanisms of Aloin Induce Gastric Cancer Cells Apoptosis by Targeting High Mobility Group Box 1. Drug Des Devel Ther. 2019, 13, 1221–1231. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Tang, T.; Wang, S.; Cai, T.; Tao, H.; Zhang, Q.; Qi, S.; Qi, Z. Aloin Inhibits the Proliferation and Migration of Gastric Cancer Cells by Regulating NOX2–ROS-mediated Pro-Survival Signal Pathways. Drug Des. Dev. Ther. 2020, 14, 145–155. [Google Scholar] [CrossRef]
- Gao, J.; Yang, S.; Xie, G.; Pan, J.; Zhu, F. Integrating Network Pharmacology and Experimental Verification to Explore the Pharmacological Mechanisms of Aloin Against Gastric Cancer. Drug Des. Dev. Ther. 2022, 16, 1947–1961. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Wu, X.; Ge, F.; Cheng, J.; Cheng, Z.; Qi, Z. Aloin Induces Gastric Cancer Cell Apoptosis via the miR-5683/HMGB1 Signal Axis. Nat. Prod. Commun. 2023, 18, 1934578X231168759. [Google Scholar] [CrossRef]
- Ahmed, E.K.; El-Gendy, A.K.; El-Tantawi, H.; El-Rouby, M.N.; Said, M.M.; Ghanem, H.M.; Esmat, A.Y. Autophagy in Antitumor Activity of Aloin for Breast Cancer Cells Compared with Doxorubicin. Ind. J. Exp. Biol. 2023, 61, 252–264. [Google Scholar] [CrossRef]
- Mani, S.; Swargiary, G.; Gulati, S.; Gupta, S.; Jindal, D. Molecular Docking and ADMET Studies to Predict the Anti-breast Cancer Effect of Aloin by Targeting Estrogen and Progesterone Receptors. Mat. Today Proc. 2023, 80, 2378–2384. [Google Scholar] [CrossRef]
- Li, P.; Ren, K.; Liang, Y.; Liu, J.; Liang, Z.; Zhang, Y. Aloin Promotes Cell Apoptosis by Targeting HMGB1-TLR4-ERK Axis in Human Melanoma Cells. EXCLI J. 2020, 19, 641–651. [Google Scholar] [CrossRef]
- Sun, R.; Zhai, R.; Ma, C.; Miao, W. Combination of Aloin and Metformin Enhances the Antitumor Effect by Inhibiting the Growth and Invasion and Inducing Apoptosis and Autophagy in Hepatocellular Carcinoma through PI3K/AKT/mTOR Pathway. Cancer Med. 2020, 9, 1141–1151. [Google Scholar] [CrossRef] [PubMed]
- Jassi, C.; Kuo, W.W.; Chang, Y.C.; Wang, T.F.; Li, C.C.; Ho, T.J.; Hsieh, D.J.Y.; Kuo, C.H.; Chen, M.C.; Huang, C.Y. Aloin and CPT-11 Combination Activates miRNA-133b and Downregulates IGF1R-PI3K/AKT/mTOR and MEK/ERK Pathways to inhibit colorectal cancer progression. Biomed. Pharmacother. 2023, 169, 115911. [Google Scholar] [CrossRef]
- Patel, K.; Patel, D.K. Medicinal Importance, Pharmacological Activities, and Analytical Aspects of Aloin: A Concise Report. J. Acute Dis. 2013, 2, 262–269. [Google Scholar] [CrossRef]
- Lewis, D.S.; Ho, J.; Wills, S.; Kawall, A.; Sharma, A.; Chavada, K.; Ebert, M.C.C.J.C.; Evoli, S.; Singh, A.; Rayalam, S. Aloin Isoforms (A and B) Selectively Inhibits Proteolytic and Deubiquitinating Activity of Papain Like Protease (PLpro) of SARS-CoV-2 In Vitro. Sci. Rep. 2022, 12, 2145. [Google Scholar] [CrossRef]
- Mitra, S.S.; Ghorai, M.; Nandy, S.; Mukherjee, N.; Kumar, M.; Radha Ghosh, A.; Jha, N.K.; Proćków, J.; Dey, A. Barbaloin: An Amazing Chemical from the ‘Wonder Plant’ with Multidimensional Pharmacological Attributes. Naunyn-Schmiedeb. Arch. Pharmacol. 2022, 395, 1525–1536. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Bai, R.; Huang, J.; Gao, Y.; Yun, X.; Haji, A.A. Barbaloin Attenuates Pulmonary Fibrosis through TGF-β1/Smads/p38 Pathway. J. Pharm. Pharmacol. 2022, 74, 1160–1169. [Google Scholar] [CrossRef] [PubMed]
- Wang, N.; Gan, G.; Yang, J.; Wang, L. Barbaloin Promotes Osteogenic Differentiation of Human Bone Marrow Mesenchymal Stem Cells: Involvement of Wnt/β-Catenin Signaling Pathway. Curr. Med. Chem. 2022, 29, 6100–6111. [Google Scholar] [CrossRef] [PubMed]
- Omer, A.B.; Afzal, O.; Altamimi, A.S.; Patil, S.; Alghamdi, S.A.; Alghamdi, A.M.; Alzarea, S.I.; Almalki, W.H.; Kazmi, I. Neuroprotective Effect of Barbaloin on Streptozotocin-Induced Cognitive Dysfunction in Rats via Inhibiting Cholinergic and Neuroinflammatory Cytokines Pathway—TNF-α/IL-1β/IL-6/NF-κB. ACS Omega 2023, 8, 8110–8118. [Google Scholar] [CrossRef] [PubMed]
- Cao, Z.Z.; Tian, Y.J.; Hao, J.; Zhang, P.H.; Liu, Z.P.; Jiang, W.Z.; Zeng, M.L.; Zhang, P.P.; Ma, J.H. Barbaloin Inhibits Ventricular Arrhythmias in Rabbits by Modulating Voltage-gated Ion Channels. Acta Pharmacol. Sin. 2017, 39, 357–370. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Wang, H.; Yang, F. Barbaloin Treatment Contributes to the Rebalance of Glucose and Lipid Homeostasis of Gestational Diabetes Mellitus Mice. Dose-Response Publ. Int. Hormesis Soc. 2020, 18, 1559325820984910. [Google Scholar] [CrossRef]
- Alhadrami, H.A.; Sayed, A.M.; Hassan, H.M.; Rateb, M.E. Aloin A Inhibits SARS CoV-2 Replication by Targeting its Binding with ACE2-Evidence from Modeling-supported Molecular Dynamics Simulation. J. Biomol. Struct. Dynam. 2023, 41, 11647–11656. [Google Scholar] [CrossRef] [PubMed]
- Matos, F.L.; Duarte, E.L.; Muniz, G.S.; Milán-Garcés, E.A.; Coutinho, K.; Lamy, M.T.; da Cunha, A.R. Spectroscopic Characterization of Different Protonation/Deprotonation States of Barbaloin in Aqueous Solution. Spectrochim. Acta A Mol. Biomol. Spectrosc. 2023, 286, 122020. [Google Scholar]
- Feng, Y.; Qiao, H.; Liu, H.; Wang, J.; Tang, H. Exploration of the mechanism of aloin ameliorates of combined allergic rhinitis and asthma syndrome based on network pharmacology and experimental validation. Front. Pharmacol. 2023, 14, 1218030. [Google Scholar] [CrossRef]
- Xu, X.; Lv, H.; Xia, Z.; Fan, R.; Zhang, C.; Wang, Y.; Wang, D. Rhein Exhibits Antioxidative Effects Similar to Rhubarb in a Rat Model of Traumatic Brain Injury. BMC Compl. Altern. Med. 2017, 17, 140. [Google Scholar] [CrossRef]
- Zeng, J.Y.; Wang, Y.; Miao, M.; Bao, X.R. The Effects of Rhubarb for the Treatment of Diabetic Nephropathy in Animals: A Systematic Review and Meta-analysis. Front. Pharmacol. 2021, 12, 602816. [Google Scholar] [CrossRef] [PubMed]
- Fang, J.Y.; Huang, T.H.; Chen, W.J.; Aljuffali, I.A.; Hsu, C.Y. Rhubarb Hydroxyanthraquinones Act as Antiobesity Agents to Inhibit Adipogenesis and Enhance Lipolysis. Biomed. Pharmacother. 2022, 146, 112497. [Google Scholar] [CrossRef] [PubMed]
- Liudvytska, O.; Kolodziejczyk-Czepas, J. A Review on Rhubarb-derived Substances as Modulators of Cardiovascular Risk Factors—A Special Emphasis on Anti-obesity Action. Nutrients 2022, 14, 2053. [Google Scholar] [CrossRef] [PubMed]
- Espinosa, A.; Paz-Y-Miño-C, G.; Santos, Y.; Ma, H.; Nadeau, M.; Seeram, N.P.; Rowley, D.C. Anti-amebic Effects of Chinese rhubarb (Rheum palmatum) Leaves’ Extract, the Anthraquinone Rhein and Related Compounds. Heliyon 2020, 6, e03693. [Google Scholar] [CrossRef] [PubMed]
- Khattak, A.K.; Hassan, S.M.; Mughal, S.S. General Overview of Phytochemistry and Pharmacological Potential of Rheum palmatum (Chinese rhubarb). Innovare J. Ayurvedic Sci. 2020, 8, 5–9. [Google Scholar] [CrossRef]
- Xiang, H.; Zuo, J.; Guo, F.; Dong, D. What We Already Know About Rhubarb: A Comprehensive Review. Chin. Med. 2020, 15, 88. [Google Scholar] [CrossRef] [PubMed]
- Gao, F.; Zhong, H.Y.; Chen, K.X.; Dong, L.L.; Lin, M.S.; Du, H.L. Mechanism of Combined Treatment of Rhein and Emodin in Rhubarb for Ulcerative Colitis. China J. Chin. Materia Medica 2022, 47, 4148–4155. [Google Scholar] [CrossRef]
- Cheng, Y.; Zhang, H.; Qu, L.; He, Y.; Routledge, M.N.; Yun Gong, Y.; Qiao, B. Identification of Rhein as the Metabolite Responsible for Toxicity of Rhubarb Anthraquinones. Food Chem. 2020, 331, 127363. [Google Scholar] [CrossRef] [PubMed]
- Su, S.; Wu, J.; Gao, Y.; Luo, Y.; Yang, D.; Wang, P. The Pharmacological Properties of Chrysophanol, the Recent Advances. Biomed. Pharmacother. 2020, 125, 110002. [Google Scholar] [CrossRef]
- Lu, J.; Miao, Z.; Jiang, Y.; Xia, W.; Wang, X.; Shi, Y.; Ni, L.; Li, S.; Xiao, J.; Sheng, S.; et al. Chrysophanol Prevents IL-1β-Induced Inflammation and ECM Degradation in Osteoarthritis via the Sirt6/NF-κB and Nrf2/NF-κB Axis. Biochem. Pharmacol. 2023, 208, 115402. [Google Scholar] [CrossRef]
- Ahmad, W.; Ansari, M.A.; Alsayari, A.; Almaghaslah, D.; Wahab, S.; Alomary, M.N.; Jamal, Q.M.S.; Khan, F.A.; Ali, A.; Alam, P.; et al. In Vitro, Molecular Docking and In Silico ADME/Tox Studies of Emodin and Chrysophanol against Human Colorectal and Cervical Carcinoma. Pharmaceuticals 2022, 15, 1348. [Google Scholar] [CrossRef] [PubMed]
- Hsu, P.-C.; Hsu, C.-C.; Hsia, Y.-J.; Kuo, C.-Y. Chrysophanol Suppresses Cell Growth via mTOR/PPAR-α Regulation and ROS Accumulation in Cultured Human Tongue Squamous Carcinoma SAS Cells. Curr. Issues Mol. Biol. 2022, 44, 1528–1538. [Google Scholar] [CrossRef] [PubMed]
- Zhao, X.; Qiao, D.; Guan, D.; Wang, K.; Cui, Y. Chrysophanol Ameliorates Hemin-Induced Oxidative Stress and Endoplasmic Reticulum Stress by Regulating MicroRNA-320-5p/Wnt3a Pathway in HT22 Cells. Oxidative Med. Cell. Longev. 2022, 2022, 9399658. [Google Scholar] [CrossRef] [PubMed]
- Jadaun, K.S.; Mehan, S.; Sharma, A.; Siddiqui, E.M.; Kumar, S.; Alsuhaymi, N. Neuroprotective Effect of Chrysophanol as a PI3K/AKT/mTOR Signaling Inhibitor in an Experimental Model of Autologous Blood-induced Intracerebral Hemorrhage. Curr. Med. Sci. 2022, 42, 249–266. [Google Scholar] [CrossRef] [PubMed]
- Jiang, F.; Jiang, J.; He, W.; Dong, G.; Xu, N.; Meng, L.; Zhao, Y.; Wang, M.; Tan, S.; Shi, Y.; et al. Chrysophanol Alleviates Acute Lung Injury Caused by Klebsiella pneumoniae Infection by Inhibiting Pro-inflammatory Cytokine Production. Phytother. Res. 2023; in press. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Tang, H.; Song, J.; Long, J.; Zhang, L.; Li, X. Chrysophanol: A Review of its Pharmacology, Toxicity and Pharmacokinetics. J. Pharm. Pharmacol. 2019, 71, 1475–1487. [Google Scholar] [CrossRef] [PubMed]
- Yusuf, M.A.; Singh, B.N.; Sudheer, S.; Kharwar, R.N.; Siddiqui, S.; Abdel-Azeem, A.M.; Fraceto, L.F.; Dashora, K.; Gupta, V.K. Chrysophanol: A natural anthraquinone with multifaceted biotherapeutic potential. Biomolecules 2019, 9, 68. [Google Scholar] [CrossRef]
- Gu, M.; Zhou, Y.; Liao, N.; Wei, Q.; Bai, Z.; Bao, N.; Zhu, Y.; Zhang, H.; Gao, L.; Cheng, X. Chrysophanol, a Main Anthraquinone from Rheum palmatum L. (rhubarb), Protects against Renal Fibrosis by Suppressing NKD2/NF-κB Pathway. Phytomedicine 2022, 105, 154381. [Google Scholar] [CrossRef] [PubMed]
- Liu, X.; Zhang, X.; Chen, J.; Song, D.; Zhang, C.; Chen, R.; Xu, R.; Jiang, W.; Li, L. Chrysophanol Facilitates Long-Term Neurological Recovery through Limiting Microglia-mediated Neuroinflammation after Ischemic Stroke in Mice. Int. Immunopharmacol. 2022, 112, 109220. [Google Scholar] [CrossRef]
- Amen, Y.; Elsbaey, M.; Othman, A.; Sallam, M.; Shimizu, K. Naturally Occurring Chromone Glycosides: Sources, Bioactivities, and Spectroscopic Features. Molecules 2021, 26, 7646. [Google Scholar] [CrossRef]
- Handayani, S.; Ni’maturrohmah, D.; Indrianingsih, A.W.; Nisa, K.; Windarsih, A.; Darsih, C.; Sefrienda, A.R.; Suryani, A.E.; Haryanti, S. Molecular Docking Study of Aloesin and Its Derivatives as Potential Antiaging Agents. In Proceedings of the 1st International Conference for Health Research–BRIN (ICHR 2022), Jakarta, Indonesia, 23–24 November 2022; Atlantis Press: Amsterdam, The Netherlands, 2023; pp. 288–299. [Google Scholar] [CrossRef]
- Ro, J.Y.; Lee, B.C.; Kim, J.Y.; Chung, Y.J.; Chung, M.H.; Lee, S.K.; Jo, T.H.; Kim, K.H.; Park, Y.I. Inhibitory Mechanism of aloe single component (Alprogen) on mediator release in guinea pig lung mast cells activated with specific antigen-antibody reactions. J. Pharmacol. Exp. Ther. 2000, 292, 114–121. [Google Scholar] [PubMed]
- Ogidi, O.I.; Enenebeaku, U.E. Medicinal Potentials of Aloe vera (Aloe barbadensis Miller): Technologies for the Production of Therapeutics. In Sustainable Utilization and Conservation of Africa’s Biological Resources and Environment; Springer Nature: Singapore, 2023; pp. 295–321. [Google Scholar]
- Pillai, A.R.; Revathi, K.; Mahendra, J.; Sundaravalli, K. Effect of Alprogen as Compared to Subantimicrobial Dose of Doxycycline on Salivary Collagenases. Ann. Rom. Soc. Cell Biol. 2020, 24, 1138–1144. Available online: http://annalsofrscb.ro/index.php/journal/article/view/10188 (accessed on 7 July 2024).
- Budiastutik, I.; Subagio, W.H.; Kartasurya, I.M.; Widjanarko, B.; Kartini, A.; Soegiyanto, B.; Suhartono, S. The Effect of Aloe vera on Fasting Blood Glucose Levels in Pre-diabetes and Type 2 Diabetes Mellitus: A Systematic Review and Meta-analysis. J. Pharm. Pharmacogn. Res. 2022, 10, 737–747. [Google Scholar] [CrossRef]
- Aljulifi, M.Z. Paradigm on Complementary and Alternative Medicine and Type 2 Diabetes. In Type 2 Diabetes-From Diagnosis to Effective Management; Chlup, R., Ed.; InTechOpen: London, UK, 2023. [Google Scholar] [CrossRef]
- Yu, L.; McGarry, S.; Cruickshank, D.; Jensen, G.S. Rapid increase in immune surveillance and expression of NKT and γδT cell activation markers after consuming a nutraceutical supplement containing Aloe vera gel, extracts of Poria cocos and rosemary. A randomized placebo-controlled cross-over trial. PLoS ONE 2023, 18, e0291254. [Google Scholar] [CrossRef] [PubMed]
- Choi, S.; Park, Y.I.; Lee, S.K.; Kim, J.E.; Chung, M.H. Aloesin Inhibits Hyperpigmentation Induced by UV Radiation. Clin. Exp. Dermatol. 2002, 27, 513–515. [Google Scholar] [CrossRef] [PubMed]
- Jones, K.; Hughes, J.; Hong, M.; Jia, Q.; Orndorff, S. Modulation of Melanogenesis by Aloesin: A Competitive Inhibitor of Tyrosinase. Pigment Cell Res. 2002, 15, 335–340. [Google Scholar] [CrossRef]
- Wahedi, H.M.; Jeong, M.; Chae, J.K.; Do, S.G.; Yoon, H.; Kim, S.Y. Aloesin from Aloe vera Accelerates Skin Wound Healing by Modulating MAPK/Rho and Smad Signaling Pathways in vitro and in vivo. Phytomedicine 2017, 28, 19–26. [Google Scholar] [CrossRef]
- Yimam, M.; Brownell, L.; Jia, Q. Aloesin as a Medical Food Ingredient for Systemic Oxidative Stress of Diabetes. World J. Diabetes 2015, 6, 1097–1107. [Google Scholar] [CrossRef] [PubMed]
- Zhang, G.; Li, R.; Wu, X.; Li, M. Natural Product Aloesin Significantly Inhibits Spore Germination and Appressorium Formation in Magnaporthe oryzae. Microorganisms 2023, 11, 2395. [Google Scholar] [CrossRef]
- Yagi, A.; Kanbara, T.; Morinobut, N. Inhibition of Mushroom-Tyrosinase by Aloe Extract. Planta Med. 1987, 53, 515–517. [Google Scholar] [CrossRef]
- Nautiyal, A.; Wairkar, S. Management of Hyperpigmentation: Current Treatments and Emerging Therapies. Pigment Cell Melanoma Res. 2021, 34, 1000–1014. [Google Scholar] [CrossRef] [PubMed]
- Lee, K.Y.; Park, J.H.; Chung, M.H.; Park, Y.I.; Kim, K.W.; Lee, Y.J.; Lee, S.K. Aloesin Up-regulates Cyclin E/CDK2 Kinase Activity via Inducing the Protein Levels of Cyclin E, CDK2, and CDC25A in SK-HEP-1 Cells. Biochem. Mol. Biol. Int. 1997, 41, 285–292. [Google Scholar] [CrossRef] [PubMed]
- Yimam, M.; Zhao, J.; Corneliusen, B.; Pantier, M.; Brownell, L.A.; Jia, Q. UP780, a Chromone-enriched Aloe Composition Improves Insulin Sensitivity. Metab. Syndr. Rel. Disord. 2013, 11, 267–275. [Google Scholar] [CrossRef] [PubMed]
- Yimam, M.; Zhao, J.; Corneliusen, B.; Pantier, M.; Brownell, L.; Jia, Q. Blood Glucose Lowering Activity of Aloe Based Composition, UP780, in alloxan Induced Insulin Dependent Mouse Diabetes Model. Diabetol. Metab. Syndr. 2014, 6, 61. [Google Scholar] [CrossRef] [PubMed]
- Yimam, M.; Brownell, L.; Jia, Q. In vivo safety evaluation of UP780, a standardized Composition of Aloe Chromone Aloesin Formulated with an Aloe vera Inner Leaf Fillet. Regul. Toxicol. Pharmacol. 2014, 69, 390–397. [Google Scholar] [CrossRef] [PubMed]
- Yimam, M.; Zhao, J.; Tseng-Crank, J.; Brownell, L.; Devaraj, S.; Jialal, R.; Jialal, I.; Rockwood, J.; Ma, W.; Padmapriya, A.; et al. A Novel Standardized Chromone Extract (UP780) from Aloe Regulated Adiponectin Production and Improved Insulin Resistance. Planta Med. 2008, 74, SL78. [Google Scholar] [CrossRef]
- Abouelela, M.E.; Assaf, H.K.; Abdelhamid, R.A.; Elkhyat, E.S.; Sayed, A.M.; Oszako, T.; Belbahri, L.; El Zowalaty, A.E.; Abdelkader, M.S.A. Identification of Potential SARS-CoV-2 Main Protease and Spike Protein Inhibitors from the Genus Aloe: An in silico Study for Drug Development. Molecules 2021, 26, 1767. [Google Scholar] [CrossRef] [PubMed]
- Yagi, A.; Kabash, A.; Mizuno, K.; Moustafa, S.; Khalifa, T.; Tsuji, H. Radical Scavenging Glycoprotein Inhibiting Cyclooxygenase-2 and Thromboxane A2 Synthase from Aloe vera gel. Planta Med. 2003, 69, 269–271. [Google Scholar] [CrossRef] [PubMed]
- Yagi, A.; Kabash, A.; Okamura, N.; Haraguchi, H.; Moustafa, S.M.; Khalifa, T.I. Antioxidant, Free Radical Scavenging and Anti-inflammatory Effects of Aloesin Derivatives in Aloe vera. Planta Med. 2002, 68, 957–960. [Google Scholar] [CrossRef]
- Breaud, C.; Lallemand, L.; Mares, G.; Mabrouki, F.; Bertolotti, M.; Simmler, C.; Greff, S.; Mauduit, M.; Herbette, G.; Garayev, E.; et al. LC-MS Based Phytochemical Profiling towards the Identification of Antioxidant Markers in Some Endemic Aloe Species from Mascarene Islands. Antioxidants 2022, 12, 50. [Google Scholar] [CrossRef]
- Roshni, J.; Ahmad, S.F.; Wani, A.; Ahmed, S.S. Multi-Target Effect of Aloeresin-A against Bacterial and Host Inflammatory Targets Benefits Contact Lens-Related Keratitis: A Multi-Omics and Quantum Chemical Investigation. Molecules 2023, 28, 6955. [Google Scholar] [CrossRef] [PubMed]
- Deora, N.; Venkatraman, K. Lipase Activity Inhibited by Aloenin A: Glycoside from Aloe vera (L.) Burm. f.—In vitro and Molecular Docking Studies. J. Mol. Recognit. 2023, 36, e3002. [Google Scholar] [CrossRef] [PubMed]
- Bendjedid, S.; Benouchenne, D. In Silico Studies for Assessing Physicochemical, Pharmacokinetic and Cytotoxic Properties of Bioactive Molecules Identified by LC-MS in Aloe vera Leaf Extracts. S. Afr. J. Bot. 2023, 157, 75–81. [Google Scholar] [CrossRef]
- Rahman, M.S.; Islam, R.; Rana, M.M.; Spitzhorn, L.-S.; Rahman, M.S.; Adjaye, J.; Asaduzzaman, S.M. Characterization of Burn Wound Healing Gel Prepared from Human Amniotic Membrane and Aloe vera Extract. BMC Complement. Altern. Med. 2019, 19, 115. [Google Scholar] [CrossRef]
- Rehman, N.U.; Hussain, H.; Khiat, M.; Khan, H.Y.; Abbas, G.; Green, I.R.; Al-Harrasi, A. Bioactive Chemical Constituents from the Resin of Aloe vera. Z. Nat. B 2017, 72, 955–958. [Google Scholar] [CrossRef]
- Khan, I.; Mohanta, T.K.; Ihsan, N.; Halim, S.A.; Khan, A.; Rehman, N.U.; Khan, F.; Khalid, A.; Abdalla, A.N.; Karim, N.; et al. Antiamnesic Effects of Feralolide Isolated from Aloe vera Resin Miller against Learning Impairments Induced in Mice. Antioxidants 2023, 12, 161. [Google Scholar] [CrossRef]
- Shaji, D.; Suzuki, R.; Yamamoto, S.; Orihashi, D.; Kurita, N. Natural Inhibitors for Severe Acute Respiratory Syndrome Coronavirus 2 Main Protease from Moringa oleifera, Aloe vera, and Nyctanthes arbor-tristis: Molecular Docking and ab Initio Fragment Molecular Orbital Calculations. Struct. Chem. 2022, 33, 1771–1788. [Google Scholar] [CrossRef] [PubMed]
- Minjares-Fuentes, J.R.; Femenia, A.; Comas-Serra, F.; Rodríguez-González, V.M. Compositional and Structural Features of the Main Bioactive Polysaccharides Present in the Aloe vera Plant. J. AOAC Int. 2018, 101, 1711–1719. [Google Scholar] [CrossRef]
- Liu, C.; Cui, Y.; Pi, F.; Cheng, Y.; Guo, Y.; Qian, H. Extraction, Purification, Structural Characteristics, Biological Activities and Pharmacological Applications of Acemannan, a Polysaccharide from Aloe vera: A Review. Molecules 2019, 24, 1554. [Google Scholar] [CrossRef]
- Leung, M.Y.; Liu, C.; Zhu, L.F.; Hui, Y.Z.; Yu, B.; Fung, K.P. Chemical and Biological Characterization of a Polysaccharide Biological Response Modifier from Aloe vera L. var. chinensis (Haw.) Berg. Glycobiology 2004, 14, 501–510. [Google Scholar] [CrossRef]
- Im, S.A.; Kim, J.W.; Kim, H.S.; Park, C.S.; Shin, E.; Do, S.G.; Park, Y.I.; Lee, C.K. Prevention of Azoxymethane/Dextran Sodium Sulfate-Induced Mouse Colon Carcinogenesis by Processed Aloe vera Gel. Int. Immunopharmacol. 2016, 40, 428–435. [Google Scholar] [CrossRef] [PubMed]
- Kang, M.-C.; Kim, S.Y.; Kim, Y.T.; Kim, E.-A.; Lee, S.-H.; Ko, S.-C.; Wijesinghe, W.; Samarakoon, K.W.; Kim, Y.-S.; Cho, J.H.; et al. In vitro and in vivo antioxidant activities of polysaccharide purified from Aloe vera (Aloe barbadensis) gel. Carbohydr. Polym. 2014, 99, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Du, P.; Guo, Y.; Xie, Y.; Yu, H.; Yao, W.; Cheng, Y.; Qian, H. Extraction, Characterization of Aloe polysaccharides and the In-Depth Analysis of its Prebiotic Effects on Mice Gut Microbiota. Carbohydr. Polym. 2021, 261, 117874. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.; Hua, H.; Zhu, H.; Cheng, Y.; Guo, Y.; Yao, W.; Qian, H. Aloe Polysaccharides Ameliorate Acute Colitis in Mice via Nrf2/HO-1 Signaling Pathway and Short-chain Fatty Acids Metabolism. Int. J. Biol. Macromol. 2021, 31, 804–812. [Google Scholar] [CrossRef] [PubMed]
- Cui, Y.; Ye, Q.; Wang, H.; Li, Y.; Yao, W.; Qian, H. Hepatoprotective Potential of Aloe vera Polysaccharides against Chronic Alcohol-induced Hepatotoxicity in Mice. J. Sci. Food Agric. 2014, 94, 1764–1771. [Google Scholar] [CrossRef] [PubMed]
- Wei, J.; Zhang, C.; Tang, X.; Huang, J.; Liu, H.; He, Y.; Zhu, R.; Gao, J. Synergistic protection of combined Aronia melanocarpa Elliot anthocyanins with aloe polysaccharides inhibits alcoholic liver injury in mice. Food Biosci. 2023, 55, 102938. [Google Scholar] [CrossRef]
- Shi, X.D.; Yin, J.Y.; Zhang, L.J.; Li, O.Y.; Huang, X.J.; Nie, S.P. Studies on Polysaccharides from Leaf Skin of Aloe barbadensis Miller: Part II. Structural Characteristics and Molecular Properties of Two Lower Molecular Weight Fractions. Food Hydrocoll. 2019, 86, 50–61. [Google Scholar] [CrossRef]
- Aranda-Cuevas, B.; Tamayo-Cortez, J.; y Vargas, L.V.; Islas-Flores, I.; Arana-Argáez, V.; Solís-Pereira, S.; Cuevas-Glory, L.; Méndez, C.H.H. Assessment of the Immunomodulatory Effect of Aloe vera Polysaccharides Extracts on Macrophages Functions. Emir. J. Food Agric. 2020, 32, 408–416. [Google Scholar] [CrossRef]
- Pugh, N.; Ross, S.A.; ElSohly, M.A.; Pasco, D.S. Characterization of Aloeride, a New High-molecular-weight Polysaccharide from Aloe vera with Potent Immunostimulatory Activity. J. Agricult. Food Chem. 2001, 49, 1030–1034. [Google Scholar] [CrossRef]
- Femenia, A.; Garcia-Pascual, P.; Simal, S.; Rossello, C. Effects of heat treatment and dehydration on bioactive polysaccharide acemannan and cell wall polymers from Aloe barbadensis Miller. Carbohyd. Polym. 2003, 51, 397–405. [Google Scholar] [CrossRef]
- Minjares-Fuentes, R.; Rodriguez-Gonzalez, V.M.; Gonzalez-Laredo, R.F.; Eim, V.; Gonzalez-Centeno, M.R.; Femenia, A. Effect of Different Drying Procedures on the Bioactive Polysaccharide Acemannan from Aloe vera (Aloe barbadensis Miller). Carbohydr. Polym. 2017, 168, 327–336. [Google Scholar] [CrossRef] [PubMed]
- Quezada, M.P.; Salinas, C.; Gotteland, M.; Cardemil, L. Acemannan and Fructans from Aloe vera (Aloe barbadensis Miller) Plants as Novel Prebiotics. J. Agric. Food Chem. 2017, 65, 10029–10039. [Google Scholar] [CrossRef] [PubMed]
- Chokboribal, J.; Tachaboonyakiat, W.; Sangvanich, P.; Ruangpornvisuti, V.; Jettanacheawchankit, S.; Thunyakitpisal, P. Deacetylation Affects the Physical Properties and Bioactivity of Acemannan, an Extracted Polysaccharide from Aloe vera. Carbohydr. Pol. 2015, 133, 556–566. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Niu, Y.; Qin, S.; Ma, G. A new biomaterial derived from Aloe vera—Acemannan from basic studies to clinical application. Pharmaceutics 2023, 15, 1913. [Google Scholar] [CrossRef] [PubMed]
- Comas-Serra, F.; Estrada, P.; Minjares-Fuentes, R.; Femenia, A. Evaluation of Acemannan in Different Commercial Beverages Containing Aloe vera (Aloe barbadensis Miller) Gel. Gels 2023, 9, 552. [Google Scholar] [CrossRef] [PubMed]
- Tippayawat, P.; Phromviyo, N.; Boueroy, P.; Chompoosor, A. Green Synthesis of Silver Nanoparticles in Aloe vera Plant Extract Prepared by a Hydrothermal Method and Their Synergistic Antibacterial Activity. PeerJ 2016, 4, e2589. [Google Scholar] [CrossRef] [PubMed]
- Chandran, S.P.; Chaudhary, M.; Pasricha, R.; Ahmad, A.; Sastry, M. Synthesis of Gold Nanotriangles and Silver Nanoparticles Using Aloe vera Plant Extract. Biotechnol. Progr. 2006, 22, 577–583. [Google Scholar] [CrossRef] [PubMed]
- Logaranjan, K.; Raiza, A.J.; Gopinath, S.C.; Chen, Y.; Pandia, K. Shape- and Size-controlled Synthesis of Silver Nanoparticles Using Aloe vera Plant Extract and their Antimicrobial Activity. Nanoscale Res. Lett. 2016, 11, 520. [Google Scholar] [CrossRef]
- Mamatha, G.; Rajulu, A.V.; Madhukar, K. In Situ Generation of Bimetallic Nanoparticles In Cotton Fabric Using Aloe vera Leaf Extract as Reducing Agent. J. Nat. Fibers 2018, 17, 1121–1129. [Google Scholar] [CrossRef]
- Sohal, J.K.; Saraf, A.; Shukla, K.; Shrivastava, M. Determination of Antioxidant Potential of Biochemically Synthesized Silver Nanoparticles Using Aloe vera Gel Extract. Plant Sci. Today 2019, 6, 208–217. [Google Scholar] [CrossRef]
- Zhou, Q.; Lv, J.; Ren, Y.; Chen, J.; Gao, D.; Lu, Z.; Wang, C. A Green in Situ Synthesis of Silver Nanoparticles on Cotton Fabrics Using Aloe vera Leaf Extraction for Durable Ultraviolet Protection and Antibacterial Activity. Text. Res. J. 2016, 87, 2407–2419. [Google Scholar] [CrossRef]
- Gupta, S.; Tejavath, K.K. Catalytic Reduction of Organic Dyes with Green Synthesized Silver Nanoparticles Using Aloe vera Leaf Extract. J. Nanosci. Nanoeng. Appl. 2019, 9, 9–21. [Google Scholar] [CrossRef]
- Kamala Nalini, S.P.; Vijayaraghavan, K. Green Synthesis of Silver and Gold Nanoparticles Using Aloe vera Gel and Determining its Antimicrobial Properties on Nanoparticle Impregnated Cotton Fabric. J. Nanotechnol. Res. 2020, 2, 42–50. [Google Scholar] [CrossRef]
- Vyas, Y.; Rana, S. Antioxidant Activity and Biogenic Synthesis of Selenium Nanoparticles Using The Leaf Extract of Aloe vera. Int. J. Curr. Pharm. Res. 2017, 9, 147–152. [Google Scholar] [CrossRef]
- Fardsadegh, B.; Jafarizadeh-Malmiri, H. Aloe vera Leaf Extract Mediated Green Synthesis of Selenium Nanoparticles and Assessment of their In Vitro Antimicrobial Activity Against Spoilage Fungi and Pathogenic Bacteria Strains. Green Process Synth. 2019, 8, 399–407. [Google Scholar] [CrossRef]
- Srujana, S.; Anjamma, M.; Alimuddin Singh, B.; Dhakar, R.C.; Natarajan, S.; Hechhu, R. A Comprehensive Study on the Synthesis and Characterization of TiO2 Nanoparticles Using Aloe vera Plant Extract and Their Photocatalytic Activity against MB Dye. Adsorpt. Sci. Technol. 2022, 2022, 7244006. [Google Scholar] [CrossRef]
- Gowri, S.; Gandhi, R.R.; Senthil, S.; Suresh, J.; Sundrarajan, M. Enhancing Antimicrobial Activity of Biotemplated TiO2 Nanoparticles Using Aloe vera Plant Extract. J. Bionanosci. 2016, 10, 181–190. [Google Scholar] [CrossRef]
- Vijay Kumar, P.P.N.; Shameem, U.; Kollu, P.; Kalyani, R.L.; Pammi, S.V.N. Green Synthesis of Copper Oxide Nanoparticles Using Aloe vera Leaf Extract and Its Antibacterial Activity Against Fish Bacterial Pathogens. BioNanoScience 2015, 5, 135–139. [Google Scholar] [CrossRef]
- Sharma, S.; Kumar, K. Aloe-vera Leaf Extract as a Green Agent for the Synthesis of CuO Nanoparticles Inactivating Bacterial Pathogens and Dye. J. Dispersion Sci. Technol. 2020, 42, 1950–1962. [Google Scholar] [CrossRef]
- Ramírez, O.; Pomareda, F.; Olivares, B.; Huang, Y.L.; Zavala, G.; Carrasco-Rojas, J.; Álvarez, S.; Leiva-Sabadini, C.; Hidalgo, V.; Romo, P.; et al. Aloe vera Peel-derived Nanovesicles Display Anti-inflammatory Properties and Prevent Myofibroblast Differentiation. Phytomedicine 2024, 122, 155108. [Google Scholar] [CrossRef]
- Valizadeh, A.; Darvishi, M.H.; Amani, A.; Zarchi, A.A.K. Design and Development of Novel Formulation of Aloe vera Nanoemulsion Gel Contained Erythromycin for Topical Antibacterial Therapy: In Vitro and In Vivo Assessment. J. Drug Deliv. Sci. Technol. 2022, 74, 103519. [Google Scholar] [CrossRef]
- Wu, Y.-Y.; Zhang, J.-H.; Gao, J.-H.; Li, Y.-S. Aloe-emodin (AE) Nanoparticles Suppresses Proliferation and Induces Apoptosis in Human Lung Squamous Carcinoma via ROS Generation in Vitro and in Vivo. Biochem. Biophys. Res. Commun. 2017, 490, 601–607. [Google Scholar] [CrossRef] [PubMed]
- Murugesan, M.P.; Ratnam, M.V.; Mengitsu, Y.; Kandasamy, K. Evaluation of Anti-cancer Activity of Phytosomes Formulated from Aloe vera extract. Mater. Today Proc. 2021, 42, 631–636. [Google Scholar] [CrossRef]
- Ghafarzadeh, M.; Eatemadi, A. Clinical Efficacy of Liposome-Encapsulated Aloe vera on Melasma Treatment during Pregnancy. J. Cosmet. Laser Ther. 2017, 19, 181–187. [Google Scholar] [CrossRef]
- Iacopetta, D.; Ceramella, J.; Catalano, A.; Scali, E.; Scumaci, D.; Pellegrino, M.; Aquaro, S.; Saturnino, C.; Sinicropi, M.S. Impact of Cytochrome P450 Enzymes on the Phase I Metabolism of Drugs. Appl. Sci. 2023, 13, 6045. [Google Scholar] [CrossRef]
- Singh, R.P.; Dhanalakshmi, S.; Rao, A.R. Chemomodulatory Action of Aloe vera on the Profiles of Enzymes Associated with Carcinogen Metabolism and Antioxidant Status Regulation in Mice. Phytomedicine 2000, 7, 209–219. [Google Scholar] [CrossRef] [PubMed]
- Juv, A.; Nilsen, O.G. Aloe vera Juice: IC50 and Dual Mechanistic Inhibition of CYP3A4 and CYP2D6. Phytother. Res. 2012, 26, 445–451. [Google Scholar] [CrossRef]
- Şen, A. Complementary Medicines Used in Ulcerative Colitis and Unintended Interactions with Cytochrome P450-dependent Drug-metabolizing Enzymes. Turk. J. Med. Sci. 2022, 52, 1425–1447. [Google Scholar] [CrossRef] [PubMed]
- Brandin, H.; Viitanen, E.; Myrberg, O.; Arvidsson, A.K. Effects of Herbal Medicinal Products and Food Supplements on Induction of CYP1A2, CYP3A4 and MDR1 in the Human Colon Carcinoma Cell Line LS180. Phytother. Res. 2007, 21, 239–244. [Google Scholar] [CrossRef]
- Vinson, J.A.; Al Kharrat, H.; Andreoli, L. Effect of Aloe vera Preparations on the Human Bioavailability of Vitamins C and E. Phytomedicine 2005, 12, 760–765. [Google Scholar] [CrossRef]
- Yang, M.S.; Yu, C.P.; Huang, C.Y.; Chao, P.D.L.; Lin, S.P.; Hou, Y.C. Aloe Activated P-glycoprotein and CYP3A: A Study on the Serum Kinetics of Aloe and its Interaction with Cyclosporine in Rats. Food Funct. 2017, 8, 315–322. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Mapa, M.S.; Sprando, R.L. Anthraquinones Inhibit Cytochromes P450 Enzyme Activity in Silico and in Vitro. J. Appl. Toxicol. 2021, 41, 1438–1445. [Google Scholar] [CrossRef] [PubMed]
- Hu, Y.H.; Quan, Z.Y.; Li, D.K.; Wang, C.Y.; Sun, Z.X. Inhibition of CYP3A4 Enhances Aloe-emodin Induced Hepatocyte Injury. Toxicol. In Vitro 2022, 79, 105276. [Google Scholar] [CrossRef] [PubMed]
- Kong, X.Y.; Chen, T.T.; Zhang, H.W.; Jia, H.M.; Yu, M.; Zou, Z.M. Characterization of the Metabolism of Aloin A/B and Aloesin in Rats Using Ultra-high performance Liquid Chromatography Coupled with Quadrupole Time-of-flight Mass Spectrometry. Biomed. Chromatog. 2022, 36, e5483. [Google Scholar] [CrossRef] [PubMed]
- Niu, C.; Ye, W.; Cui, X.; Sun, J.; Xiao, S.; Chen, G.; Bao, S.; Chen, R. UHPLC-MS/MS Method for the Quantification of Aloin-A in Rat Plasma and its Application to a Pharmacokinetic Study. J. Pharm. Biomed. Anal. 2020, 178, 112928. [Google Scholar] [CrossRef] [PubMed]
- Mueller, S.; Stopper, H.; Dekant, W. Biotransformation of the Antraquinones Emodin and Chrysophanol by Cytochrome P450 Enzymes. Drug Metab. Dispos. 1998, 26, 540–546. [Google Scholar] [PubMed]
- Semerel, J.; John, N.; Dehaen, W.; Fardim, P. Valorization of Aloe barbadensis Miller (Aloe vera) processing waste. J. Renew. Mater. 2023, 11, 1031–1061. [Google Scholar] [CrossRef]
- Solaberrieta, I.; Jiménez, A.; Garrigós, M.C. Valorization of Aloe vera Skin By-Products to Obtain Bioactive Compounds by Microwave-Assisted Extraction: Antioxidant Activity and Chemical Composition. Antioxidants 2022, 11, 1058. [Google Scholar] [CrossRef] [PubMed]
- Hossen, M.M.; Hossain, M.L.; Mitra, K.; Hossain, B.; Bithi, U.H.; Uddin, M.N. Phytochemicals and In-vitro Antioxidant Activity Analysis of Aloe vera by-products (skin) in Different Solvent Extract. J. Agric. Food Res. 2022, 10, 100460. [Google Scholar] [CrossRef]
- Martínez-Sánchez, A.; López-Cañavate, M.E.; Guirao-Martínez, J.; Roca, M.J.; Aguayo, E. Aloe vera Flowers, a Byproduct with Great Potential and Wide Application, Depending on Maturity Stage. Foods 2020, 9, 1542. [Google Scholar] [CrossRef]
- Guancha-Chalapud, M.A.; Serna-Cock, L.; Tirado, D.F. Aloe vera Rind Valorization to Improve the Swelling Capacity of Commercial Acrylic Hydrogels. Fibers 2022, 10, 73. [Google Scholar] [CrossRef]
- Elferjane, M.R.; Jovanović, A.A.; Milutinović, V.; Čutović, N.; Jovanović Krivokuća, M.; Marinković, A. From Aloe vera Leaf Waste to the Extracts with Biological Potential: Optimization of the Extractions, Physicochemical Characterization, and Biological Activities. Plants 2023, 12, 2744. [Google Scholar] [CrossRef] [PubMed]
- Brown, A.C. Liver Toxicity Related to Herbs and Dietary Supplements: Online Table of Case Reports. Part 2 of 5 Series. Food Chem. Toxicol. 2017, 107, 472–501. [Google Scholar] [CrossRef] [PubMed]
- Belfrage, B.; Malmström, R. Several Cases of Liver Affected by Aloe vera. Lakartidningen 2008, 105, 45. [Google Scholar] [PubMed]
- Kanat, O.; Ozet, A.; Ataergin, S. Aloe vera-induced acute toxic hepatitis in a healthy young man. Eur. J. Int. Med. 2006, 17, 589. [Google Scholar] [CrossRef] [PubMed]
- Rabe, C.; Musch, A.; Schirmacher, P.; Kruis, W.; Hoffmann, R. Acute Hepatitis Induced by an Aloe vera Preparation: A Case Report. World J. Gastroenterol. 2005, 11, 303. [Google Scholar] [CrossRef] [PubMed]
- Curciarello, J.; De Ortúzar, S.; Borzi, S.; Bosia, D. Severe acute hepatitis associated with intake of Aloe vera tea. Gastroenterol. Hepatol. 2008, 31, 436–438. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.N.; Kim, D.J.; Kim, Y.M.; Kim, B.H.; Sohn, K.M.; Choi, M.J.; Choi, Y.H. Aloe-Induced Toxic Hepatitis. J. Korean Med. Sci. 2010, 25, 492–495. [Google Scholar] [CrossRef] [PubMed]
- Bottenberg, M.M.; Wall, G.C.; Harvey, R.L.; Habib, S. Oral Aloe vera-induced Hepatitis. Ann. Pharmacother. 2007, 41, 1740–1743. [Google Scholar] [CrossRef]
- Parlati, L.; Voican, C.S.; Perlemuter, K.; Perlemuter, G. Aloe vera-Induced Acute Liver Injury: A Case Report and Literature Review. Clin. Res. Hepatol. Gastroenterol. 2017, 41, e39–e42. [Google Scholar] [CrossRef]
- Lee, J.; Lee, M.S.; Nam, K.W. Acute Toxic Hepatitis Caused by an Aloe vera Preparation in a Young Patient: A Case Report with a Literature Review. Korean J. Gastroenterol. 2014, 64, 54–58. [Google Scholar] [CrossRef] [PubMed]
- Lippert, A.; Renner, B. Herb–Drug Interaction in Inflammatory Diseases: Review of Phytomedicine and Herbal Supplements. J. Clin. Med. 2022, 11, 1567. [Google Scholar] [CrossRef] [PubMed]
- Kiliś-Pstrusińska, K.; Wiela-Hojeńska, A. Nephrotoxicity of Herbal Products in Europe—A Review of an Underestimated Problem. Int. J. Mol. Sci. 2021, 22, 4132. [Google Scholar] [CrossRef] [PubMed]
- Moosa, M.S. A Young Adult with Aloe vera-Induced Acute Liver Failure. S. Afr. Gastroenterol. Rev. 2023, 21, 1–3. [Google Scholar]
- Ahmed-Khan, M.A.; Hanif, M.; Nepal, N.; Jiffry, Z. S3672 The Price of Natural Healing: A Case of Aloe vera Associated Liver Injury. Off. J. Am. Coll. Gastroenterol. ACG 2023, 118, S2379–S2380. [Google Scholar] [CrossRef]
- Beik, A.; Joukar, S.; Najafipour, H. A Review on Plants and Herbal Components with Antiarrhythmic Activities and Their Interaction with Current Cardiac Drugs. J. Tradit. Complement. Med. 2020, 10, 275–287. [Google Scholar] [CrossRef] [PubMed]
- Kumar, P.; Verma, S.; Sigh, S.; Tiwari, S.; Khan, M.Y. Effect of Aloe vera (Aloe barbadensis) Gel Extract on Re-polarization State of Myocardium in Albino Rat. Afr. J. Pharm. Pharmacol. 2010, 4, 885–889. [Google Scholar]
- Villaescusa, L.; Zaragoza, C.; Zaragoza, F.; Tamargo, J. Herbal Medicines for the Treatment of Cardiovascular Diseases: Benefits and Risks–A Narrative Review. Int. J. Cardiol. 2023, 385, 44–52. [Google Scholar] [CrossRef]
- Loschi, F.; Faggian, M.; Sut, S.; Ferrarese, I.; Maccari, E.; Peron, G.; Dall’Acqua, S. Development of an LC–DAD–MS-Based Method for the Analysis of Hydroxyanthracene Derivatives in Food Supplements and Plant Materials. Molecules 2022, 27, 1932. [Google Scholar] [CrossRef]
- European Commission Draft COMMISSION REGULATION (EU). Amending Annex III to Regulation (EC) no 1925/2006 of the European Parliament and of the Council as Regards Apecies Containing Hydroxyanthracene Derivatives. 2020. Available online: https://eur-lex.europa.eu/eli/reg/2021/468/oj (accessed on 7 July 2024).
- Tinti, L.; Cicaloni, V.; Nezi, P.; Isoldi, G.; Etiope, P.; Barlozzini, B.; Pecorari, R.; Salvini, L. Hydroxyanthracene Derivates Citotoxicity: A Differential Evaluation between Single Molecule and Whole Plant Extract. Front. Plant Sci. 2023, 14, 1166075. [Google Scholar] [CrossRef]
- Baldi, A.; Sommella, E.; Campiglia, P.; Daglia, M. Aloe Gel-base Food Products: Chemical, Toxicological, and Regulatory Aspects. Regul. Toxicol. Pharmacol. 2021, 119, 104818. [Google Scholar] [CrossRef]
- Hayes, A.W.; Clemens, R.A.; Pressman, P. The Absence of Genotoxicity of a Mixture of Aloin A and B and a Commercial Aloe Gel Beverage. Toxicol. Mech. Methods 2022, 32, 385–394. [Google Scholar] [CrossRef] [PubMed]
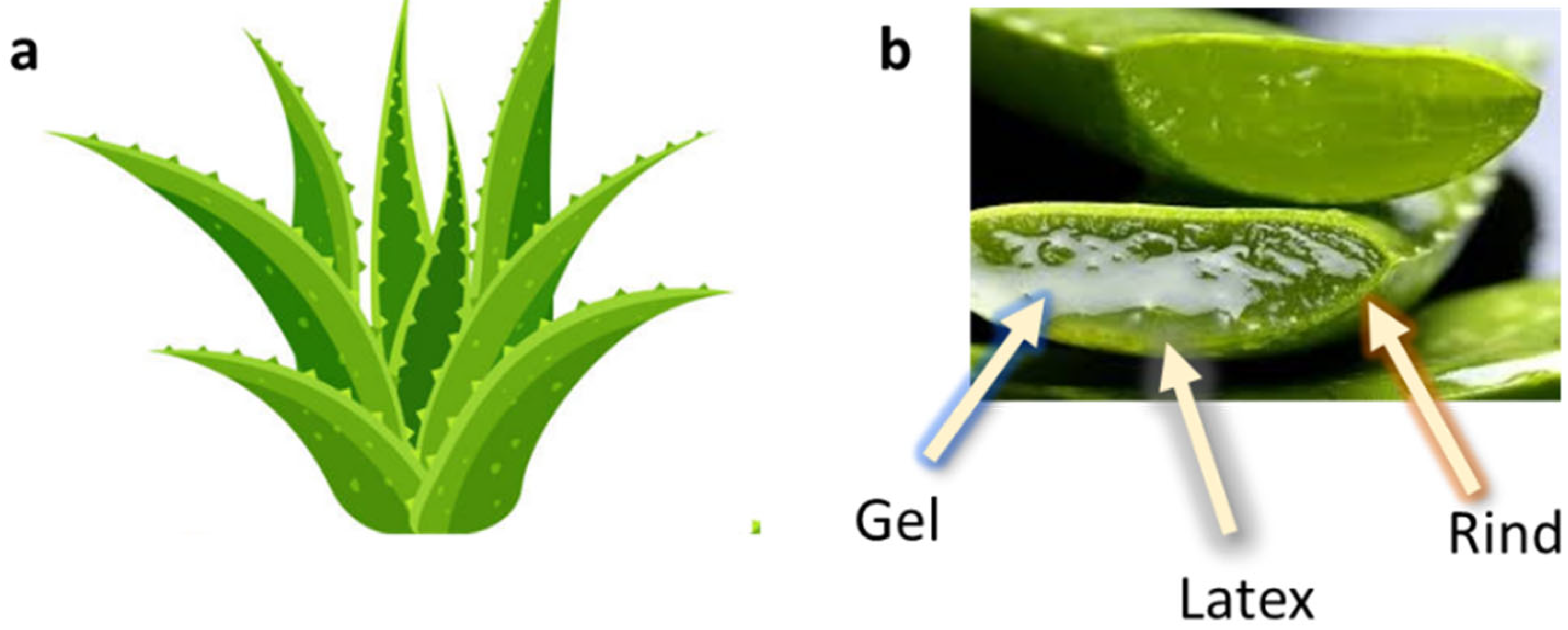
| Activity | Ref. | ||
|---|---|---|---|
| Antiviral activity | HCMV in cell culture | Diminution of DNA viral replication and plaque formation in HCMV-infected cells | [109] |
| Influenza A virus in MDCK cells | Reduction in influenza A virus replication and autophagy inhibition in MDCK cells. Reduced transcription and protein expression of M1, M2, and HA following AVE exposure, in a concentration-dependent manner. | [110] | |
| HSV-1 (Vero cells infected with HSV-1) | High reduction in PFU of HSV-1 with 5% concentration AV gel. | [112] | |
| H1N1 (female SPF BALB/c mice infected with PR8 (H1N1) | APS extracted from AV significantly ameliorated the clinical symptoms and the lung damage of female SPF BALB/c mice infected with PR8 (H1N1), and significantly reduced the virus loads and mortality. | [113] | |
| MNV1 | AV reduced MNV1 infectivity both on food vegetable surfaces and in liquid media. | [114] |
| Activity | Ref. | ||
|---|---|---|---|
| Gastroesophageal Reflux Disease (GERD) | Randomized clinical trial | AV syrup was safe and well tolerated and reduced the frequency of GERD symptoms | [206] |
| Five clinical studies on patients suffering from GERD | 10 mL AV gel syrup twice daily significantly eliminated GERD symptoms with no adverse effects, when compared with omeprazole or ranitidine | [207] | |
| Irritable Bowel Syndrome (IBS) | A systematic review and meta-analysis of randomized controlled trials, non-randomized controlled trials, retrospective and prospective cohort studies, and controlled before-and-after studies | Aloe-containing preparations were more effective than placebo in improving symptoms among all IBS subtypes, such as diarrhea-predominant IBS (IBS-D) and mixed-pattern IBS (IBS-M)) | [208] |
| Inflammatory Bowel Disease (IBD) | In vivo DSS-induced acute experimental colitis mouse model | AV-derived nanovesicles were able to attenuate inflammation and enhance tight junction proteins for acute colitis treatment | [212] |
| In vivo DSS-induced acute experimental colitis mouse model | Glucomannan protected mice from DSS-induced colitis, maintained intestinal barrier integrity by mitigating anoikis mediated by the Nrf2/mitochondria axis and reduced ROS levels by activating the Nrf2/Gpx2 cascade | [213,214] | |
| Subacute ulcerative colitis in healthy male C57BL/6 mice | APS was responsible for the anticolitic action, by alleviating colonic inflammation | [215] | |
| In vivo DSS-induced experimental colitis in 7-week-old male BALB/c mice | AV synergistically acted with heat-killed Lactobacillus plantarum L.137 (HK L.137) | [216] | |
| Ulcerative Colitis (UC) | Placebo-controlled, randomized, double-blind trial involving 44 UC patients, studying the effects of oral AV gel (200 mL/day) over a period of four weeks | UC patients receiving oral AV gel (200 mL/day) showed a significant reduction in clinical and histological disease activity scores (compared to placebo); no serious side effects were recorded | [217] |
| In vivo study on acetic acid-induced UC in adult male Wistar rats | AV gel significantly improved the clinical activity index and inflammation | [218] | |
| In vivo studies on 70 Sprague Dawley male rats | AV extract exhibited a therapeutic effect in TNBS-induced colitis; the oral route was less effective than the local and rectal ones | [219] |
| Structure | Name(s) | IUPAC Names | Ref. |
|---|---|---|---|
| ANTHRAQUINONES AND ANTHRONES | |||
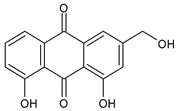 | Aloe-emodin | 1,8-Dihydroxy-3-hydroxymethyl-anthraquinone 3-Hydroxymethyl-chrysazin 1,8-Dihydroxy-3-hydroxymethyl-9,10-anthracenedione | [287] |
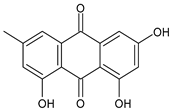 | Emodin | 1,3,8-Trihydroxy-6-methylanthraquinone 3-Hydroxy-6-methyl-chrysazin | [287] |
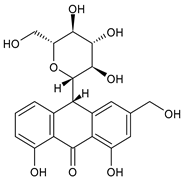 | Aloin A Barbaloin | (10S)-Glucopyranosyl–1,8–dihydroxy–3–(hydroxymethyl)–9(10H)–anthraquinone 10-C-β-D-Glucopyranosyl-1,8-dihydroxy-3-(hydroxymethyl)-9(10H)-anthracenone | [287] |
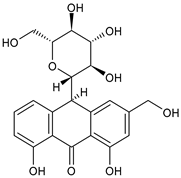 | Aloin B Isobarbaloin | (10R)-10-Glucopyranosyl-1,8-dihydroxy-3-(hydroxymethyl)-9(10H)-anthraquinone (10R)-10-Glucopyranosyl-1,8-dihydroxy-3-(hydroxymethyl)-9(10H)-anthracenone | [287] |
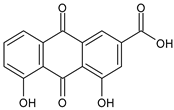 | Rhein Cassic acid Monorhein Rheic acid Rhubarb yellow | 4,5-Dihydroxy-9,10-dioxoanthracene-2-carboxylic acid 4,5-Dihydroxyanthraquinone-2-carboxylic acid 9,10-Dihydro-4,5-dihydroxy-9,10-dioxo-2-anthracenecarboxylic acid Chrysazin 3-carboxylic acid | [288] |
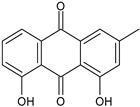 | Chrysophanol Chrysophanic acid | 1,8-Dihydroxy-3-methylanthraquinone-3-methylchrysazin | [131] |
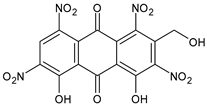 | Aloetic acid | 4,5-Dihydroxy-2-(hydroxymethyl)-1,3,6,8-tetranitroanthracene-9,10-dione | [64] |
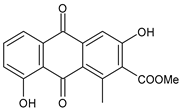 | Aloesaponarin I | Methyl-3,8-dihydroxy-1-methyl-9,10-dioxoanthracene-2-carboxylate | [131] |
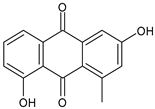 | Aloesaponarin II | 3,8-Dihydroxy-1-methylanthracene-9,10-dione 3,8-Dihydroxy-1-methyl-9,10-anthracenedione | [131] |
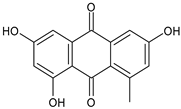 | Deoxyerythrolaccin | 1,3,6-Trihydroxy-8-methylanthracene-9,10-dione | [131] |
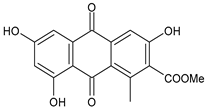 | Laccaic acid D-methylester | 3,6,8-Trihydroxy-1-methyl-9,10-dioxo-9,10-dihydroanthracene-2-carboxylic acid | [131] |
 | Helminthosporin | 1,5,8-Trihydroxy-3-methylanthracene-9,10-dione | [131] |
| GLYCOSIDES | |||
| Glycosylated Chromones | |||
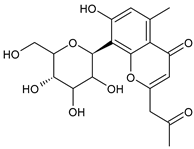 | Aloesin (formerly aloeresin B) | – | [287] |
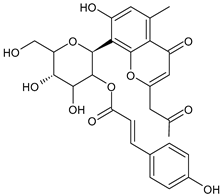 | Aloeresin A | – | [287] |
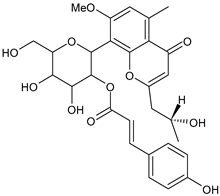 | Aloeresin D | – | [287] |
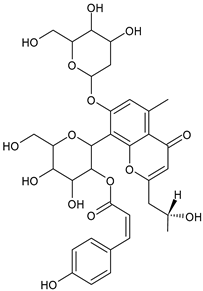 | Allo-aloeresin D | – | [289] |
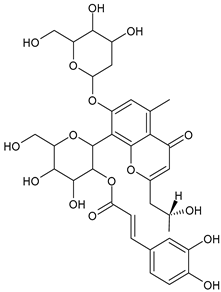 | Rebaichromone | – | [289] |
| Glycosylated pyran-2-ones | |||
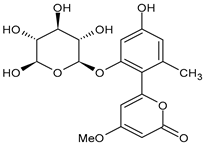 | Aloenin or Aloenin A | – | [287] |
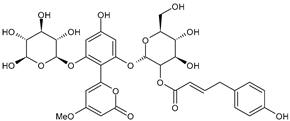 | Aloenin B | – | [287] |
| COUMARINS AND ISOCOUMARINS | |||
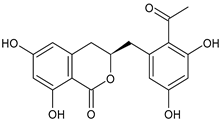 | Feralolide | 3R-3,4-dihydro-6,8-dihydroxy-3-(2′-acetyl-3′,5′-dihydroxyphenyl)- methylisocoumarin | [73] |
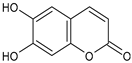 | Esculetin | 6,7-Dihydroxy-2H-1-benzopyran-2-one | [131] |
| POLISACCHARIDES | |||
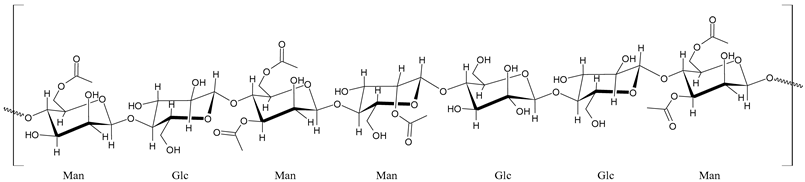 Acemannan | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Catalano, A.; Ceramella, J.; Iacopetta, D.; Marra, M.; Conforti, F.; Lupi, F.R.; Gabriele, D.; Borges, F.; Sinicropi, M.S. Aloe vera―An Extensive Review Focused on Recent Studies. Foods 2024, 13, 2155. https://doi.org/10.3390/foods13132155
Catalano A, Ceramella J, Iacopetta D, Marra M, Conforti F, Lupi FR, Gabriele D, Borges F, Sinicropi MS. Aloe vera―An Extensive Review Focused on Recent Studies. Foods. 2024; 13(13):2155. https://doi.org/10.3390/foods13132155
Chicago/Turabian StyleCatalano, Alessia, Jessica Ceramella, Domenico Iacopetta, Maria Marra, Filomena Conforti, Francesca R. Lupi, Domenico Gabriele, Fernanda Borges, and Maria Stefania Sinicropi. 2024. "Aloe vera―An Extensive Review Focused on Recent Studies" Foods 13, no. 13: 2155. https://doi.org/10.3390/foods13132155
APA StyleCatalano, A., Ceramella, J., Iacopetta, D., Marra, M., Conforti, F., Lupi, F. R., Gabriele, D., Borges, F., & Sinicropi, M. S. (2024). Aloe vera―An Extensive Review Focused on Recent Studies. Foods, 13(13), 2155. https://doi.org/10.3390/foods13132155













