Older Adults’ Exposure to Food Media Induced Unhealthy Eating during the COVID-19 Omicron Lockdown? Exploring Negative Emotions and Associated Literacy and Efficacy on Shanghainese
Abstract
1. Introduction
2. Literature Review
2.1. Food-Evoked Negative Emotions
2.2. Food Literacy
2.3. Health Consciousness
2.4. Eating Self-Efficacy
2.5. Potential Interaction
3. Materials and Methods
3.1. Research Design
3.2. Procedure
3.3. Measurements
3.4. Data Processing
4. Results
4.1. Descriptive Statistics
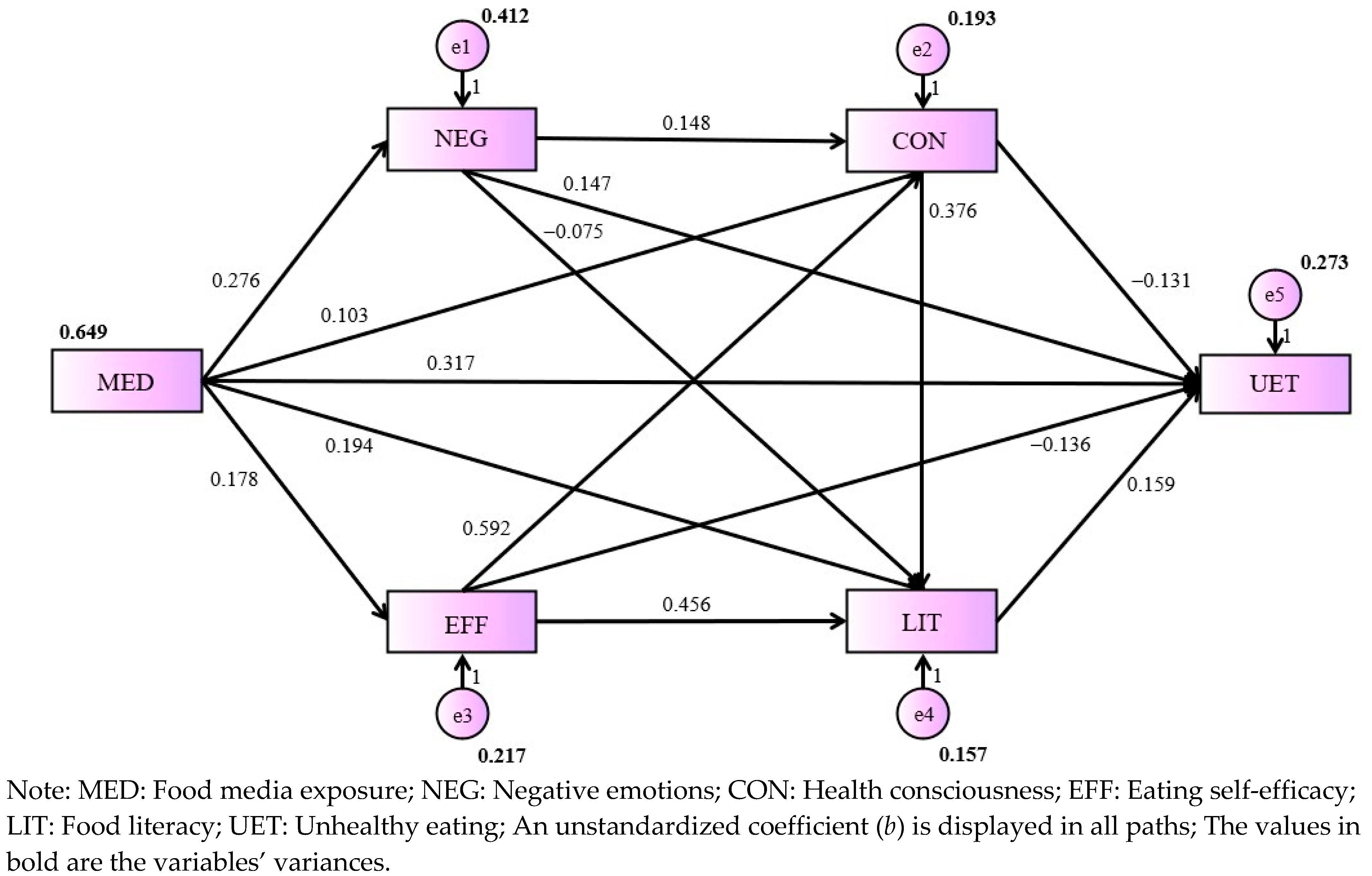
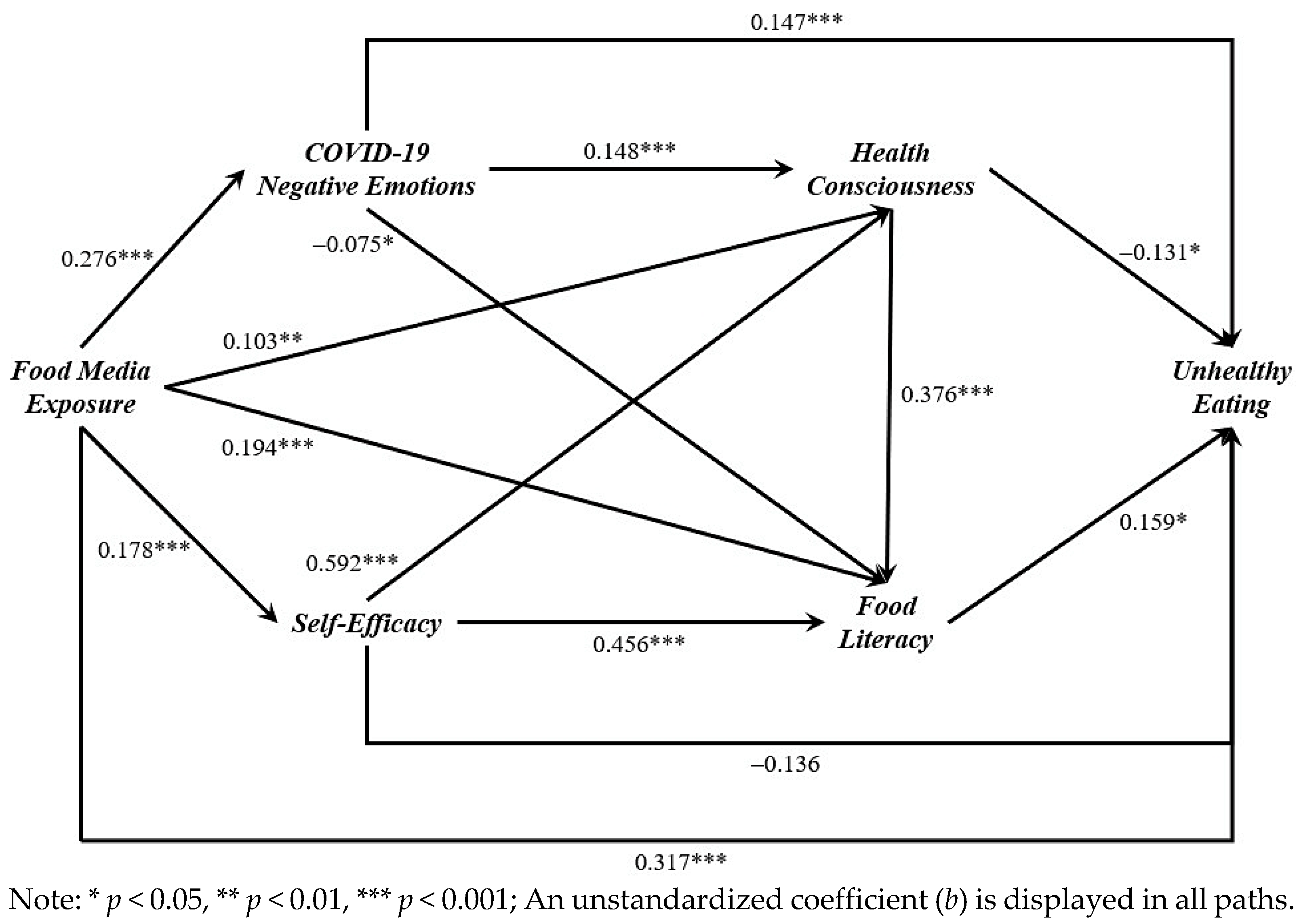
4.2. Evaluation of Main Effects
5. Discussion
5.1. Interpretation of Findings
5.2. Practical Implications
5.3. Limitations and Future Directions
6. Conclusions
Supplementary Materials
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Variable | Frequency | Percent |
|---|---|---|
| Gender | ||
| Female | 205 | 51.3% |
| Male | 195 | 48.8% |
| Age | ||
| 50–60 | 376 | 94.0% |
| 61–70 | 22 | 5.5% |
| 71–80 | 1 | 0.3% |
| 81–90 | 1 | 0.3% |
| Highest education | ||
| Under a high school diploma | 8 | 2.0% |
| High school diploma | 88 | 22.0% |
| Bachelor’s degree | 254 | 63.5% |
| Master’s degree | 39 | 9.8% |
| Doctorate | 11 | 2.8% |
| Employment status | ||
| No work | 55 | 13.8% |
| Work less than half-time | 13 | 3.3% |
| Work half-time | 23 | 5.8% |
| Work more than half-time but not full-time | 22 | 5.5% |
| Work full time | 287 | 71.8% |
| Monthly income in RMB | ||
| 1500 and below (≤USD 207.56) | 1 | 0.3% |
| 1501–2000 (USD 207.70–276.75) | 0 | 0.0% |
| 2001–3000 (USD 276.89–415.12) | 3 | 0.8% |
| 3001–5000 (USD 415.26–691.87) | 32 | 8.0% |
| 5001–8000 (USD 692.01–1106.99) | 111 | 27.8% |
| 8001–12,000 (USD 1107.13–1660.49) | 102 | 25.5% |
| 12,001–20,000 (USD 1660.63–2767.48) | 87 | 21.8% |
| More than 20,000 (>USD 2767.48) | 64 | 16.0% |
| Income changed due to COVID-19 | ||
| A lot less | 14 | 3.5% |
| A little less | 141 | 35.3% |
| No change | 219 | 54.8% |
| A little more | 22 | 5.5% |
| A lot more | 4 | 1.0% |
| Body mass index | ||
| Underweight | 44 | 11.0% |
| Normal weight | 240 | 60.0% |
| Overweight | 100 | 25.0% |
| Obesity | 16 | 4.0% |
References
- Hall, B.J.; Li, G.; Chen, W.; Shelley, D.; Tang, W. Prevalence of depression, anxiety, and suicidal ideation during the Shanghai 2022 Lockdown: A cross-sectional study. J. Affect. Disord. 2023, 330, 283–290. [Google Scholar] [CrossRef] [PubMed]
- Di Renzo, L.; Gualtieri, P.; Pivari, F.; Soldati, L.; Attinà, A.; Cinelli, G.; Leggeri, C.; Caparello, G.; Barrea, L.; Scerbo, F.; et al. Eating habits and lifestyle changes during COVID-19 lockdown: An Italian survey. J. Transl. Med. 2020, 18, 229. [Google Scholar] [CrossRef] [PubMed]
- Chang, A.; Schulz, P.J.; Jiao, W.; Liu, M.T. Obesity-related communication in digital Chinese news from mainland China, Hong Kong, and Taiwan: Automated content analysis. JMIR Public Health Surveill. 2021, 7, e26660. [Google Scholar] [CrossRef]
- Bonaccio, M.; Costanzo, S.; Bracone, F.; Gialluisi, A.; Di Castelnuovo, A.; Ruggiero, E.; Esposito, S.; Olivieri, M.; Persichillo, M.; Cerletti, C.; et al. Psychological distress resulting from the COVID-19 confinement is associated with unhealthy dietary changes in two Italian population-based cohorts. Eur. J. Nutr. 2022, 61, 1491–1505. [Google Scholar] [CrossRef] [PubMed]
- Jiao, W.; Xiang, Y.T.; Chang, A. Are foods from the COVID-19 pandemic lockdown low in nutrients? An analysis of Chinese psychological distress effects. Nutrients 2022, 14, 4702. [Google Scholar] [CrossRef] [PubMed]
- Bakaloudi, D.R.; Jeyakumar, D.T.; Jayawardena, R.; Chourdakis, M. The impact of COVID-19 lockdown on snacking habits, fast-food and alcohol consumption: A systematic review of the evidence. Clin. Nutr. 2022, 41, 3038–3045. [Google Scholar] [CrossRef] [PubMed]
- Sidor, A.; Rzymski, P. Dietary choices and habits during COVID-19 lockdown: Experience from Poland. Nutrients 2020, 12, 1657. [Google Scholar] [CrossRef] [PubMed]
- Elisabeth, A.L.; Karlen, S.B.; Magkos, F. The effect of COVID-19-related lockdowns on diet and physical activity in older adults: A systematic review. Aging Dis. 2021, 12, 1935–1947. [Google Scholar] [CrossRef]
- Paderno, A.; Schreiber, A.; Grammatica, A.; Raffetti, E.; Tomasoni, M.; Gualtieri, T.; Taboni, S.; Zorzi, S.; Lombardi, D.; Deganello, A.; et al. Smell and taste alterations in COVID-19: A cross-sectional analysis of different cohorts. Int. Forum Allergy Rhinol. 2020, 10, 955–962. [Google Scholar] [CrossRef]
- Chen, Y.; Klein, S.L.; Garibaldi, B.T.; Li, H.; Wu, C.; Osevala, N.M.; Li, T.; Margolick, J.B.; Pawelec, G.; Leng, S.X. Aging in COVID-19: Vulnerability, immunity and intervention. Ageing Res. Rev. 2021, 65, 101205. [Google Scholar] [CrossRef]
- Lu, G.; Zhang, Y.; Zhang, H.; Ai, J.; He, L.; Yuan, X.; Bao, S.; Chen, X.; Wang, H.; Cai, J.; et al. Geriatric risk and protective factors for serious COVID-19 outcomes among older adults in Shanghai Omicron wave. Emerg. Microbes Infect. 2022, 11, 2045–2054. [Google Scholar] [CrossRef]
- Decorte, P.; Cuykx, I.; Teunissen, L.; Poels, K.; Smits, T.; Pabian, S.; van Royen, K.; De Backer, C. “Everywhere you look, you’ll find food”: Emerging adult perspectives toward the food media landscape. Ecol. Food Nutr. 2022, 61, 273–303. [Google Scholar] [CrossRef] [PubMed]
- Renström, E.A.; Bäck, H. Emotions during the COVID-19 pandemic: Fear, anxiety, and anger as mediators between threats and policy support and political actions. J. Appl. Soc. Psychol. 2021, 51, 861–877. [Google Scholar] [CrossRef]
- Ahorsu, D.K.; Lin, C.Y.; Imani, V.; Saffari, M.; Griffiths, M.D.; Pakpour, A.H. The Fear of COVID-19 Scale: Development and initial validation. Int. J. Ment. Health Addict. 2022, 20, 1537–1545. [Google Scholar] [CrossRef]
- Sim, S.; Wiwanitkit, V. Food contamination, food safety and COVID-19 outbreak. J. Health Res. 2021, 35, 463–466. [Google Scholar] [CrossRef]
- Kaneko, D.; Toet, A.; Brouwer, A.M.; Kallen, V.; Van Erp, J.B.F. Methods for evaluating emotions evoked by food experiences: A literature review. Front. Psychol. 2018, 9, 316974. [Google Scholar] [CrossRef] [PubMed]
- Naja, F.; Hamadeh, R. Nutrition amid the COVID-19 pandemic: A multi-level framework for action. Eur. J. Clin. Nutr. 2020, 74, 1117–1121. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.T.; Li, R.T.; Sun, X.J.; Peng, M.; Li, X. Social media exposure, psychological distress, emotion regulation, and depression during the COVID-19 outbreak in community samples in China. Front. Psychiatry 2021, 12, 644899. [Google Scholar] [CrossRef]
- McAtamney, K.; Mantzios, M.; Egan, H.; Wallis, D.J. Emotional eating during COVID-19 in the United Kingdom: Exploring the roles of alexithymia and emotion dysregulation. Appetite 2021, 161, 105120. [Google Scholar] [CrossRef]
- Camilleri, G.M.; Méjean, C.; Kesse-Guyot, E.; Andreeva, V.A.; Bellisle, F.; Hercberg, S.; Péneau, S. The associations between emotional eating and consumption of energy-dense snack foods are modified by sex and depressive symptomatology. J. Nutr. 2014, 144, 1264–1273. [Google Scholar] [CrossRef]
- Lopez-Cepero, A.; Frisard, C.F.; Lemon, S.C.; Rosal, M.C. Association between emotional eating, energy-dense foods and overeating in Latinos. Eat. Behav. 2019, 33, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Vidgen, H.A.; Gallegos, D. Defining food literacy and its components. Appetite 2014, 76, 50–59. [Google Scholar] [CrossRef] [PubMed]
- Poelman, M.P.; Dijkstra, S.C.; Sponselee, H.; Kamphuis, C.B.M.; Battjes-Fries, M.C.E.; Gillebaart, M.; Seidell, J.C. Towards the measurement of food literacy with respect to healthy eating: The development and validation of the self perceived food literacy scale among an adult sample in the Netherlands. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 54. [Google Scholar] [CrossRef] [PubMed]
- Steils, N.; Obaidalahe, Z. “Social food”: Food literacy co-construction and distortion on social media. Food Policy 2020, 95, 101932. [Google Scholar] [CrossRef]
- Melki, J.; Tamim, H.; Hadid, D.; Farhat, S.; Makki, M.; Ghandour, L.; Hitti, E. Media exposure and health behavior during pandemics: The mediating effect of perceived knowledge and fear on compliance with COVID-19 prevention measures. Health Commun. 2022, 37, 586–596. [Google Scholar] [CrossRef] [PubMed]
- Hong, H. An extension of the extended parallel process model (EPPM) in television health news: The influence of health consciousness on individual message processing and acceptance. Health Commun. 2011, 26, 343–353. [Google Scholar] [CrossRef] [PubMed]
- Lapointe, L.; Ramaprasad, J.; Vedel, I. Creating health awareness: A social media enabled collaboration. Health Technol. 2014, 4, 43–57. [Google Scholar] [CrossRef]
- Igbinoba, A.O.; Soola, E.O.; Omojola, O.; Odukoya, J.; Adekeye, O.; Salau, O.P. Women’s mass media exposure and maternal health awareness in Ota, Nigeria. Cogent Soc. Sci. 2020, 6, 1766260. [Google Scholar] [CrossRef]
- Dutta, M.J. Health information processing from television: The role of health orientation. Health Commun. 2007, 21, 1–9. [Google Scholar] [CrossRef]
- Divine, R.L.; Lepisto, L. Analysis of the healthy lifestyle consumer. J. Consum. Mark. 2005, 22, 275–283. [Google Scholar] [CrossRef]
- Hartmann, C.; Siegrist, M.; van der Horst, K. Snack frequency: Associations with healthy and unhealthy food choices. Public Health Nutr. 2013, 16, 1487–1496. [Google Scholar] [CrossRef]
- Jiao, W.; Liu, M.T.; Schulz, P.J.; Chang, A. Impacts of self-efficacy on food and dietary choices during the first COVID-19 lockdown in China. Foods 2022, 11, 2668. [Google Scholar] [CrossRef]
- Fitzgerald, A.; Heary, C.; Kelly, C.; Nixon, E.; Shevlin, M. Self-efficacy for healthy eating and peer support for unhealthy eating are associated with adolescents’ food intake patterns. Appetite 2013, 63, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Churchill, S.; Good, A.; Pavey, L. Promoting the avoidance of high-calorie snacks. The role of temporal message framing and eating self-efficacy. Appetite 2014, 80, 131–136. [Google Scholar] [CrossRef] [PubMed]
- Diotaiuti, P.; Valente, G.; Mancone, S.; Corrado, S.; Bellizzi, F.; Falese, L.; Langiano, E.; Vilarino, G.T.; Andrade, A. Effects of cognitive appraisals on perceived self-efficacy and distress during the COVID-19 lockdown: An empirical analysis based on structural equation modeling. Int. J. Environ. Res. Public Health 2023, 20, 5294. [Google Scholar] [CrossRef]
- Van Kampen, H.S. The principle of consistency and the cause and function of behaviour. Behav. Process. 2019, 159, 42–54. [Google Scholar] [CrossRef] [PubMed]
- Hoque, M.Z.; Alam, M.N.; Nahid, K.A. Health consciousness and its effect on perceived knowledge, and belief in the purchase intent of liquid milk: Consumer insights from an emerging market. Foods 2018, 7, 150. [Google Scholar] [CrossRef]
- Anderson, E.S.; Winett, R.A.; Wojcik, J.R. Social-cognitive determinants of nutrition behavior among supermarket food shoppers: A structural equation analysis. Health Psychol. 2000, 19, 479–486. [Google Scholar] [CrossRef]
- Mai, R.; Hoffmann, S. Taste lovers versus nutrition fact seekers: How health consciousness and self-efficacy determine the way consumers choose food products. J. Consum. Behav. 2012, 11, 316–328. [Google Scholar] [CrossRef]
- Rimal, R.N. Closing the knowledge-behavior gap in health promotion: The mediating role of self-efficacy. Health Commun. 2000, 12, 219–237. [Google Scholar] [CrossRef]
- Cha, E.; Kim, K.H.; Lerner, H.M.; Dawkins, C.R.; Bello, M.K.; Umpierrez, G.; Dunbar, S.B. Health literacy, self-efficacy, food label use, and diet in young adults. Am. J. Health Behav. 2014, 38, 331–339. [Google Scholar] [CrossRef] [PubMed]
- De Backer, C.; Teunissen, L.; Cuykx, I.; Decorte, P.; Pabian, S.; Gerritsen, S.; Matthys, C.; Al Sabbah, H.; Van Royen, K.; Corona Cooking Survey Study Group. An evaluation of the COVID-19 pandemic and perceived social distancing policies in relation to planning, selecting, and preparing healthy meals: An observational study in 38 countries worldwide. Front. Nutr. 2020, 7, 621726. [Google Scholar] [CrossRef]
- Grunert, K.G.; Janssen, M.; Nyland Christensen, R.; Teunissen, L.; Cuykx, I.; Decorte, P.; Reisch, L.A. “Corona Cooking”: The interrelation between emotional response to the first lockdown during the COVID-19 pandemic and cooking attitudes and behaviour in Denmark. Food Qual. Prefer. 2022, 96, 104425. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Zhang, W.; Chen, S. Shanghai’s life-saving efforts against the current omicron wave of the COVID-19 pandemic. Lancet 2022, 399, 2011–2012. [Google Scholar] [CrossRef] [PubMed]
- Giles, J.; Lei, X.; Wang, G.; Wang, Y.; Zhao, Y. One country, two systems: Evidence on retirement patterns in China. J. Pension Econ. Financ. 2023, 22, 188–210. [Google Scholar] [CrossRef] [PubMed]
- Mottram, S.; Peat, G.; Thomas, E.; Wilkie, R.; Croft, P. Patterns of pain and mobility limitation in older people: Cross-sectional findings from a population survey of 18,497 adults aged 50 years and over. Qual. Life Res. 2008, 17, 529–539. [Google Scholar] [CrossRef] [PubMed]
- Ma, J.F.; Xin, X.Y.; Liang, L.; Liu, L.H.; Fang, R.; Zhang, Y.J.; Wang, D.Y.; Fahn, S.; Tang, H.D.; Chen, S.D. Restless legs syndrome in Chinese elderly people of an urban suburb in Shanghai: A community-based survey. Parkinsonism Relat. Disord. 2012, 18, 294–298. [Google Scholar] [CrossRef]
- Yang, F.; Gu, D.; Mitnitski, A. Frailty and life satisfaction in Shanghai older adults: The roles of age and social vulnerability. Arch. Gerontol. Geriatr. 2016, 67, 68–73. [Google Scholar] [CrossRef] [PubMed]
- Xiao, Y.; Miao, S.; Zhang, Y.; Xie, B.; Wu, W. Exploring the associations between neighborhood greenness and level of physical activity of older adults in shanghai. J. Transp. Health 2022, 24, 101312. [Google Scholar] [CrossRef]
- Glynn, S.M.; Ruderman, A.J. The development and validation of an Eating Self-Efficacy Scale. Cogn. Ther. Res. 1986, 10, 403–420. [Google Scholar] [CrossRef]
- Weihrauch, A.; Huang, S.C. Portraying humans as machines to promote health: Unintended risks, mechanisms, and solutions. J. Mark. 2021, 85, 184–203. [Google Scholar] [CrossRef]
- Williams, J.; Mackinnon, D.P. Resampling and distribution of the product methods for testing indirect effects in complex models. Struct. Equ. Modeling 2008, 15, 23–51. [Google Scholar] [CrossRef] [PubMed]
- Schulz, P.J.; Fitzpatrick, M.A.; Hess, A.; Sudbury-Riley, L.; Hartung, U. Effects of eHealth literacy on general practitioner consultations: A mediation analysis. J. Med. Internet Res. 2017, 19, e166. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Health promotion by social cognitive means. Health Educ. Behav. 2004, 31, 143–164. [Google Scholar] [CrossRef] [PubMed]
- Jiao, W.; Chang, A. Unhealthy aging? Featuring older people in television food commercials in China. Int. J. Nurs. Sci. 2020, 7, S67–S73. [Google Scholar] [CrossRef]
- Parvanta, S.A.; Brown, J.D.; Du, S.; Zimmer, C.R.; Zhao, X.; Zhai, F. Television use and snacking behaviors among children and adolescents in China. J. Adolesc. Health 2010, 46, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Jiao, W.; Chang, A.; Ho, M.; Lu, Q.; Liu, M.T.; Schulz, P.J. Predicting and empowering health for generation Z by comparing health information seeking and digital health literacy: Cross-sectional questionnaire study. J. Med. Internet Res. 2023, 25, e47595. [Google Scholar] [CrossRef]
- Bours, M.J.L. Using mediators to understand effect modification and interaction. J. Clin. Epidemiol. 2023, 163, 117–121. [Google Scholar] [CrossRef]
| Variable | Mean | SD | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|---|
| 1: Food media exposure | 2.95 | 0.81 | 0.371 ** | 0.460 ** | 0.321 ** | 0.279 ** | 0.522 ** |
| 2: COVID-19 negative emotions | 3.04 | 0.73 | 0.187 ** | 0.313 ** | 0.153 ** | 0.316 ** | |
| 3: Food literacy | 3.65 | 0.61 | 0.631 ** | 0.645 ** | 0.239 ** | ||
| 4: Health consciousness | 3.86 | 0.57 | 0.581 ** | 0.107 * | |||
| 5: Eating self-efficacy | 4.07 | 0.51 | 0.065 | ||||
| 6: Unhealthy eating | 2.60 | 0.64 |
| Parameter | Estimate | 95% CI | p-Value | |
|---|---|---|---|---|
| Lower | Upper | |||
| 1: Food media exposure → Negative emotions → Unhealthy eating | 0.041 | 0.018 | 0.076 | <0.001 |
| 2: Food media exposure → Food literacy → Unhealthy eating | 0.031 | 0.002 | 0.070 | 0.036 |
| 3: Food media exposure → Health consciousness → Unhealthy eating | −0.013 | −0.038 | −0.001 | 0.036 |
| 4: Food media exposure → Emotional eating → Unhealthy eating | −0.024 | −0.059 | 0.000 | 0.047 |
| 5: Food media exposure → Negative emotions → Health consciousness → Food literacy → Unhealthy eating | 0.002 | 0.000 | 0.007 | 0.027 |
| 6: Food media exposure → Eating self-efficacy → Health consciousness → Food literacy → Unhealthy eating | 0.006 | 0.000 | 0.017 | 0.035 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Jiao, W. Older Adults’ Exposure to Food Media Induced Unhealthy Eating during the COVID-19 Omicron Lockdown? Exploring Negative Emotions and Associated Literacy and Efficacy on Shanghainese. Foods 2024, 13, 1797. https://doi.org/10.3390/foods13121797
Jiao W. Older Adults’ Exposure to Food Media Induced Unhealthy Eating during the COVID-19 Omicron Lockdown? Exploring Negative Emotions and Associated Literacy and Efficacy on Shanghainese. Foods. 2024; 13(12):1797. https://doi.org/10.3390/foods13121797
Chicago/Turabian StyleJiao, Wen. 2024. "Older Adults’ Exposure to Food Media Induced Unhealthy Eating during the COVID-19 Omicron Lockdown? Exploring Negative Emotions and Associated Literacy and Efficacy on Shanghainese" Foods 13, no. 12: 1797. https://doi.org/10.3390/foods13121797
APA StyleJiao, W. (2024). Older Adults’ Exposure to Food Media Induced Unhealthy Eating during the COVID-19 Omicron Lockdown? Exploring Negative Emotions and Associated Literacy and Efficacy on Shanghainese. Foods, 13(12), 1797. https://doi.org/10.3390/foods13121797





