Salmonella Risk Assessment in Poultry Meat from Farm to Consumer in Korea
Abstract
1. Introduction
2. Materials and Methods
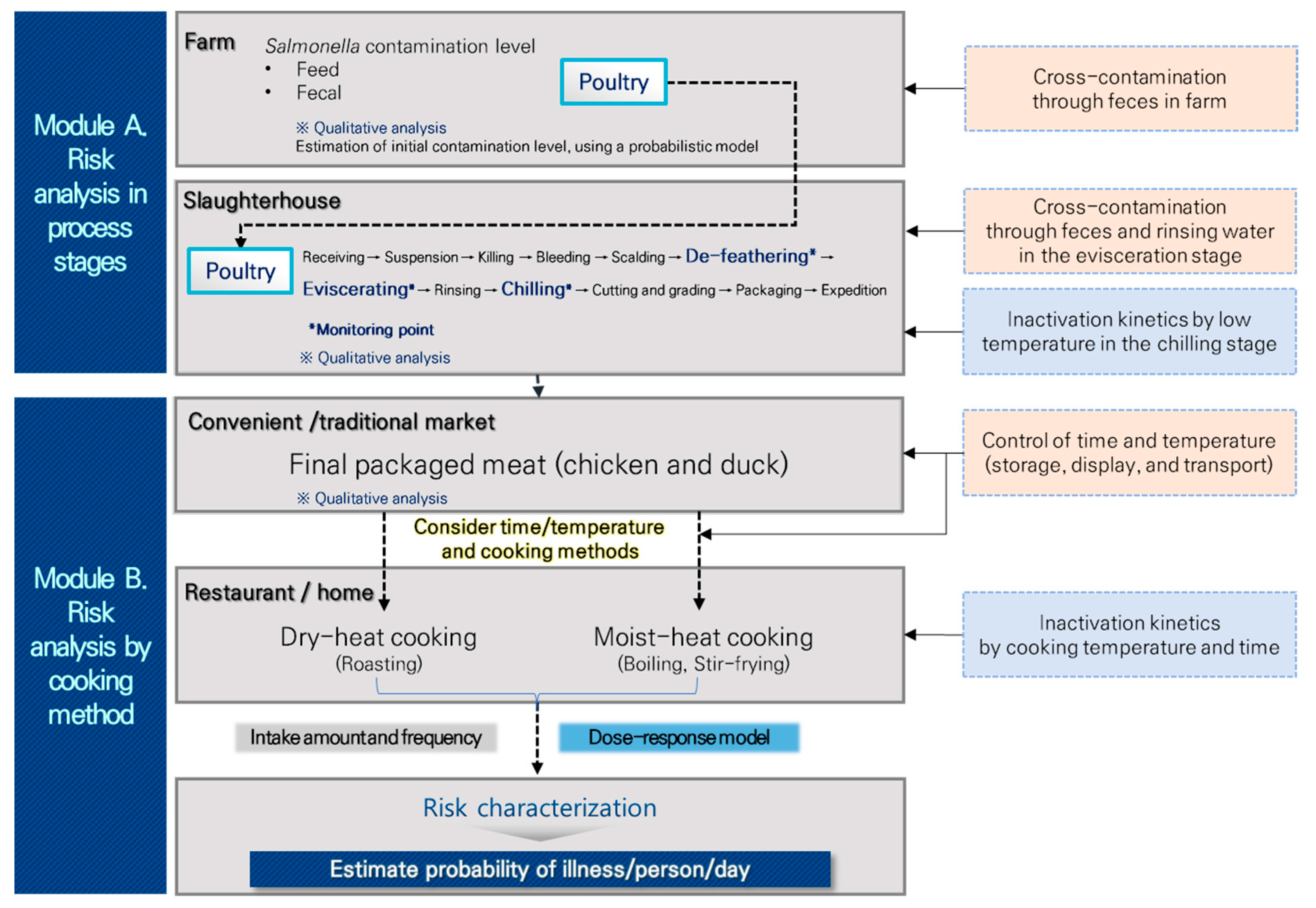
2.1. Model Overview
2.2. Salmonella Prevalence in Poultry
2.3. Preparation of Salmonella Inoculum
2.4. Predictive Models Development
2.5. Reduction of Salmonella by Cooking
2.6. Consumption Data for Chicken and Duck by Cooking Methods
2.7. Distribution Temperature and Time
2.8. The Characterization of Risk Based on Dose-Response Model
2.9. Statistics
3. Results
3.1. Salmonella Prevalence in Poultry during the Production Stage
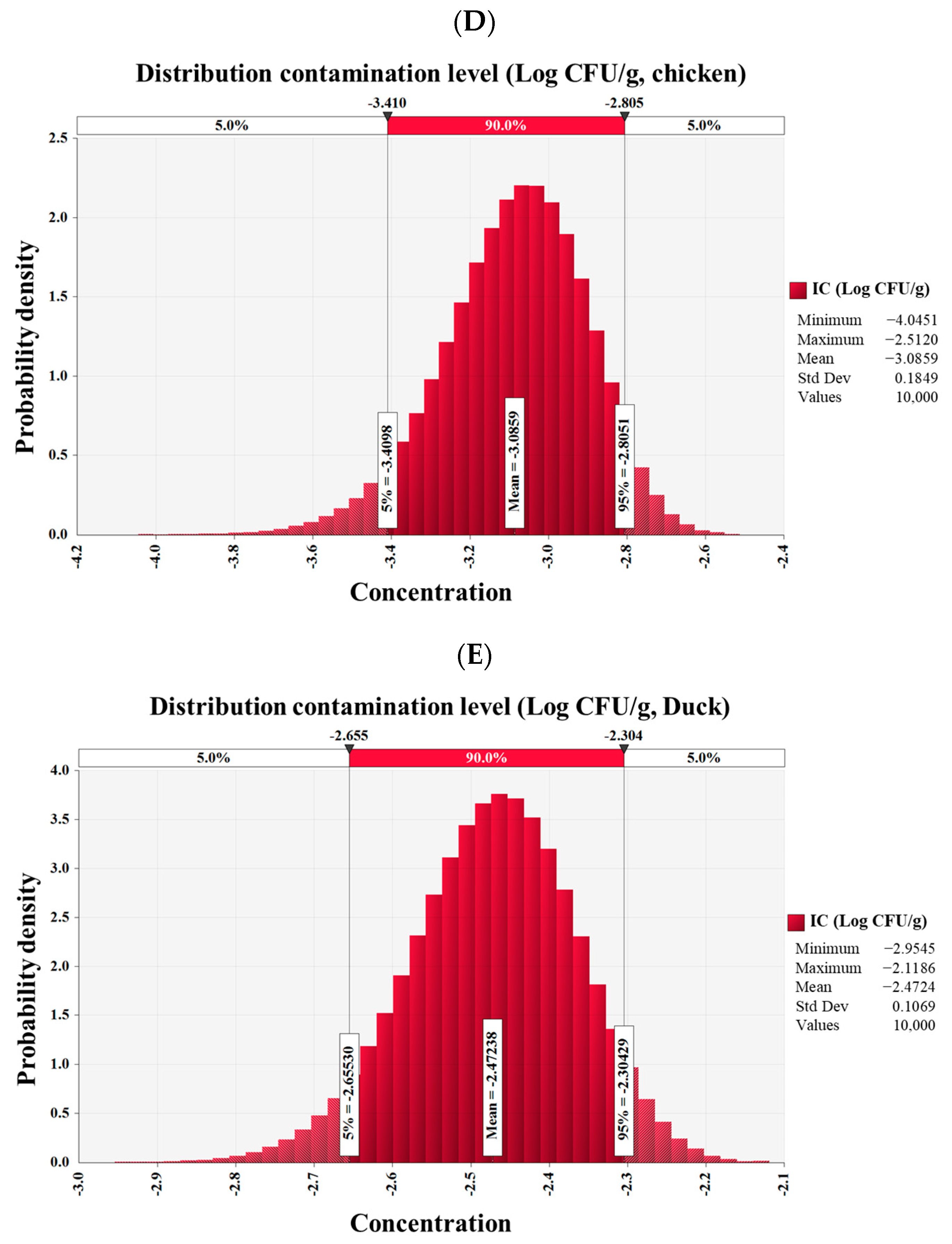
3.2. Salmonella Prevalence in Poultry at the Distribution Stage
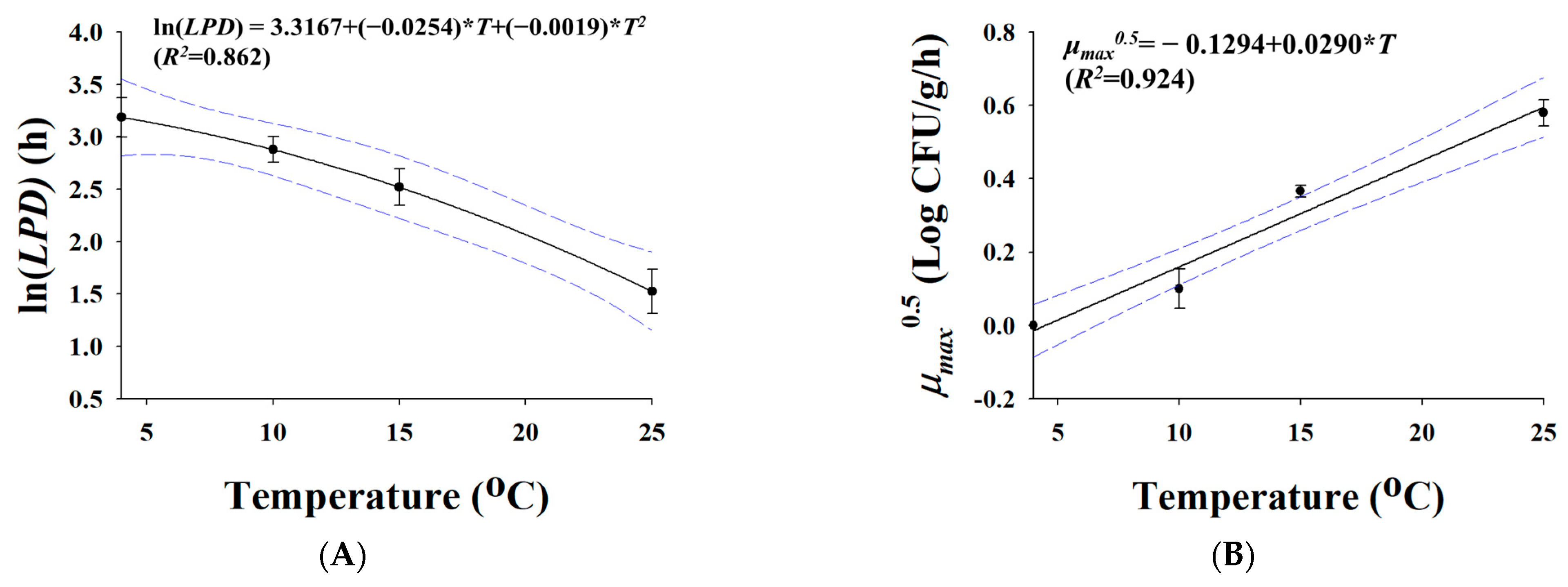
3.3. Predictive Models
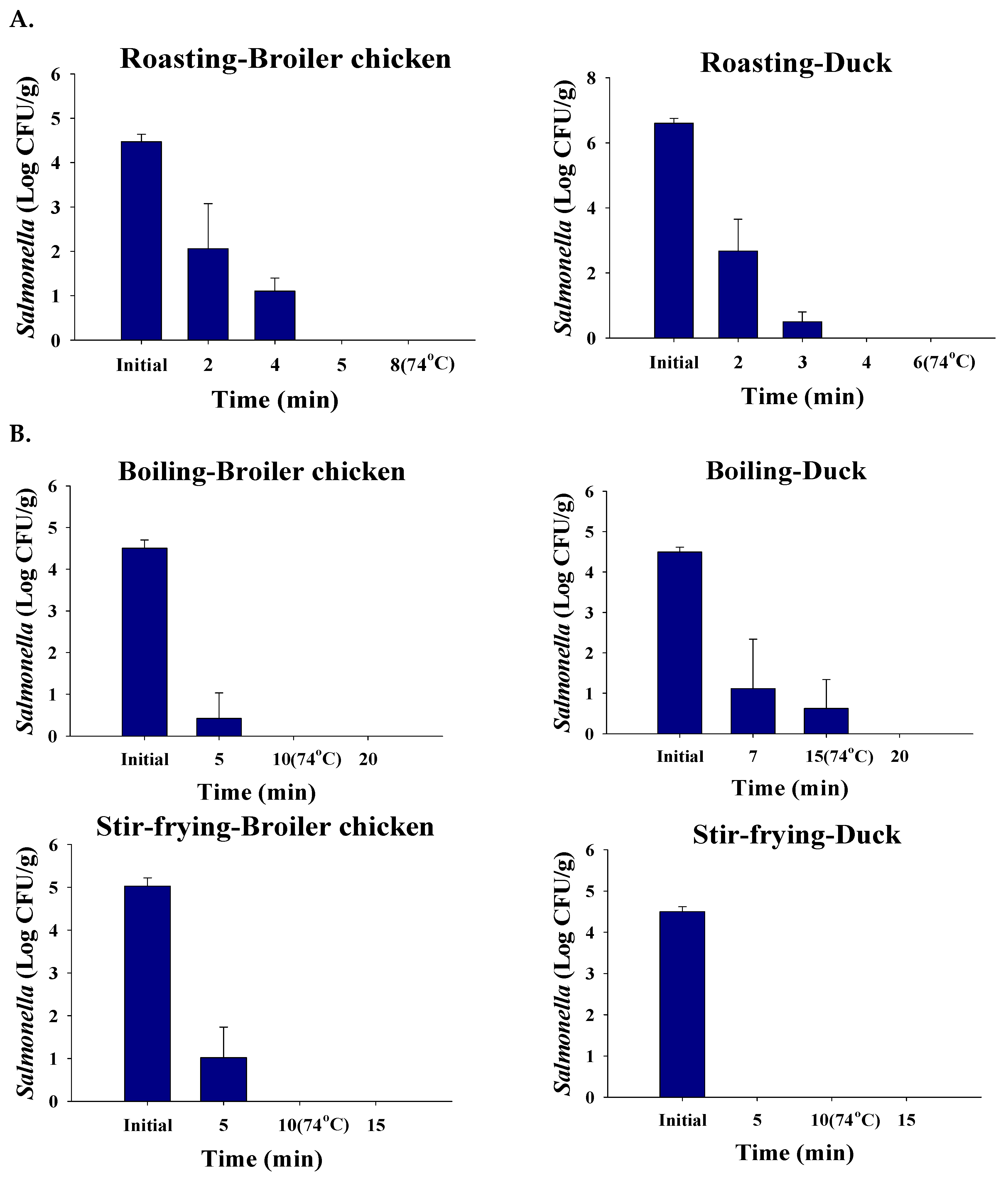
3.4. Effects of Cooking Methods on Reducing Salmonella Cell Counts
3.5. Consumption and Cooking Method Ratios in Republic of Korea
3.6. Time and Temperature of Distribution
3.7. Dose-Response Model
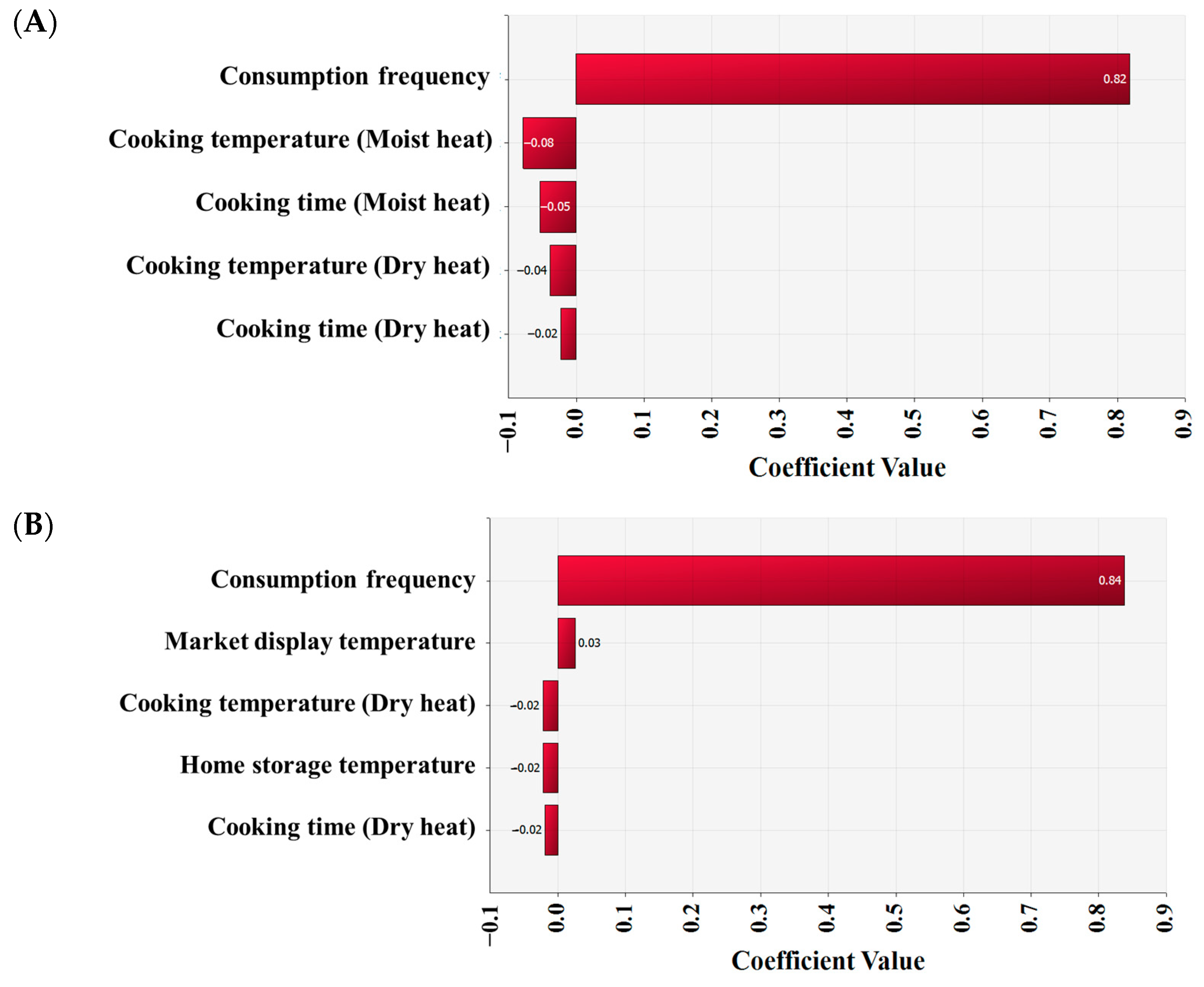
3.8. Simulation and Risk Assessment
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Chen, H.M.; Wang, Y.; Su, L.H.; Chiu, C.H. Nontyphoid Salmonella infection: Microbiology, clinical features, and antimicrobial therapy. Pediatr Neonatol. 2013, 54, 147–152. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.E.; Lee, Y.J. Molecular characterization of antimicrobial resistant non-typhoidal Salmonella from poultry industries in Korea. Ir. Vet. J. 2017, 70, 20. [Google Scholar] [CrossRef]
- European Food Safety Authority and the European Centre for Disease Prevention and Control (EFSA & ECDC). The European Union One Health 2021 Zoonoses Report. EFSA J. 2022, 20, 7666. [Google Scholar] [CrossRef]
- Ministry of Food and Drug Safety (MFDS). Food Safety Korea. 2022. Available online: https://www.foodsafetykorea.go.kr/portal/healthyfoodlife/foodPoisoningStat.do?menu_no=3724&menu_grp=MENU_NEW02 (accessed on 12 October 2022).
- Lee, H.; Yoon, Y. Etiological agents implicated in foodborne illness worldwide. Food Sci. Anim. Resour. 2021, 41, 1–7. [Google Scholar] [CrossRef]
- Yang, X.; Wu, Q.; Zhang, J.; Huang, J.; Chen, L.; Wu, S.; Zeng, H.; Wang, J.; Chen, M.; Wu, H.; et al. Prevalence, bacterial load, and antimicrobial resistance of Salmonella serovars isolated from retail meat and meat products in China. Front. Microbiol. 2019, 10, 2019. [Google Scholar] [CrossRef]
- Yang, X.; Wu, Q.; Huang, J.; Wu, S.; Zhang, J.; Chen, L.; Wei, X.; Ye, Y.; Li, Y.; Wang, J.; et al. Prevalence and characterization of Salmonella isolated from raw vegetables in China. Food Control. 2020, 109, 106915. [Google Scholar] [CrossRef]
- Abd-Elghany, S.M.; Fathy, T.M.; Zakaria, A.I.; Imre, K.; Morar, A.; Herman, V.; Pascalau, R.; Smuleac, L.; Morar, D.; Imre, M.; et al. Prevalence of multidrug-resistant Salmonella enterica serovars in buffalo meat in Egypt. Foods 2022, 11, 2924. [Google Scholar] [CrossRef]
- Zhu, J.; Wang, Y.; Song, X.; Cui, S.; Xu, H.; Yang, B.; Huang, J.; Liu, G.; Chen, Q.; Zhou, G.; et al. Prevalence and quantification of Salmonella contamination in raw chicken carcasses at the retail in China. Food Control. 2014, 44, 198–202. [Google Scholar] [CrossRef]
- Tîrziu, E.; Lazar, R.; Sala, C.; Nichita, I.; Morar, A.; Seres, M.; Imre, K. Salmonella in raw chicken meat from the Romanian seaside: Frequency of isolation and antibiotic resistance. J. Food Prot. 2015, 78, 1003–1006. [Google Scholar] [CrossRef]
- Nauman, K.; Jaspal, M.H.; Asghar, B.; Manzoor, A.; Akhter, K.H.; Ali, U.; Ali, S.; Nasir, J.; Sohaib, M.; Badar, I.H. Effect of different packaging atmosphere on microbiological shelf life, physicochemical attributes, and sensory characteristics of chilled poultry fillets. Food Sci. Anim. Resour. 2022, 42, 153–174. [Google Scholar] [CrossRef]
- Ren, X.; Li, M.; Xu, C.; Cui, K.; Feng, Z.; Fu, Y.; Zhang, J.; Liao, M. Prevalence and molecular characterization of Salmonella enterica isolates throughout an integrated broiler supply chain in China. Epidemiol. Infect. 2016, 144, 2989–2999. [Google Scholar] [CrossRef]
- Sohail, M.N.; Rathnamma, D.; Priya, S.C.; Isloor, S.; Naryanaswamy, H.D.; Ruban, S.W.; Veeregowda, B.M. Salmonella from farm to table: Isolation, characterization, and antimicrobial resistance of Salmonella from commercial broiler supply chain and its environment. Biomed Res. Int. 2021, 2021, 3987111. [Google Scholar] [CrossRef] [PubMed]
- Lakins, D.G.; Alvarado, C.Z.; Thompson, L.D.; Brashears, M.T.; Brooks, J.C.; Brashears, M.M. Reduction of Salmonella Enteritidis in shell eggs using directional microwave technology. Pout. Sci. 2008, 87, 985–991. [Google Scholar] [CrossRef]
- Davis, A.L.; Curtis, P.A.; Conner, D.E.; McKee, S.R.; Kerth, L.K. Validation of cooking methods using shell eggs inoculated with Salmonella serotypes Enteritidis and Heidelberg. Poult. Sci. 2008, 87, 1637–1642. [Google Scholar] [CrossRef] [PubMed]
- Savi, G.D.; Bortolotto, T.; Simoes, L.R.; Barichello, T. Elimination of Salmonella enterica serovar Typhimurium in artificially contaminated eggs through correct cooking and frying procedures. Food Sci. Technol. 2011, 31, 492–496. [Google Scholar] [CrossRef]
- Lee, J.; Lee, H.; Lee, S.; Kim, S.; Ha, J.; Choi, Y.; Oh, H.; Kim, Y.; Lee, Y.; Yoon, K.S.; et al. Quantitative microbial risk assessment for Campylobacter jejuni in ground meat products in Korea. Food Sci. Anim. Resour. 2019, 39, 565–575. [Google Scholar] [CrossRef]
- Nauta, M.; Hill, A.; Rosenquist, H.; Brynestad, S.; Fetsch, A.; van der Logt, P.; Fazil, A.; Christensen, B.; Katsma, E.; Borck, B.; et al. A comparison of risk assessments on Campylobacter in broiler meat. Int. J. Food. Microbiol. 2009, 129, 107–123. [Google Scholar] [CrossRef] [PubMed]
- Whiting, R.C.; Buchanan, R.L. Development of a quantitative risk assessment model for Salmonella enteritidis in pasteurized liquid eggs. Int. J. Food Microbiol. 1997, 36, 111–125. [Google Scholar] [CrossRef]
- Jeong, J.; Chon, J.W.; Kim, H.; Song, K.Y.; Seo, K.H. Risk assessment for salmonellosis in chicken in South Korea: The effect of Salmonella concentration in chicken at retail. Korean J. Food Sci. An. 2018, 38, 1043–1054. [Google Scholar] [CrossRef]
- Ministry of Food and Drug Safety (MFDS). Food Code. 2022. Available online: https://www.mfds.go.kr/eng/brd/m_15/view.do?seq=72437 (accessed on 12 October 2022).
- Ministry of Food and Drug Safety (MFDS). Processing Standards and Ingredient Specifications for Livestock Products. Notice no. 2015–94, 12/16/2015. Available online: https://www.mfds.go.kr/eng/brd/m_15/view.do?seq=70016 (accessed on 12 October 2022).
- Baranyi, J.; Roberts, T.A. A dynamic approach to predicting bacterial growth in food. Int. J. Food Microbiol. 1994, 23, 277–294. [Google Scholar] [CrossRef]
- Park, S.Y.; Lim, J.H.; Lee, J.H.; Hwang, M.J.; Lee, J.S.; Choi, Y.M.; Lee, S.; Hwang, J.; Seo, D.W.; Nam, J.S. Changes in fat-soluble components (Fatty acids, vitamin A, and vitamin E) of different parts of chicken by different cooking methods. J. Korean. Soc. Food. Sci. Nutr. 2017, 46, 1257–1264. [Google Scholar] [CrossRef]
- Son, J.Y.; Kang, K.O. Effect of an oil-water fryer on quality properties of deep frying oil used for chicken. Korean J. Food Cook Sci. 2012, 28, 443–450. [Google Scholar] [CrossRef]
- Health Canada’s Guidance on Safe Cooking and Handling Labelling for Raw Ground Meat and Raw Ground Poultry. Available online: https://www.canada.ca/content/dam/hc-sc/migration/hc-sc/fn-an/alt_formats/pdf/legislation/guide-ld/guide-cook-cuiss-meat-viand-eng.pdf (accessed on 15 October 2022).
- Korea Disease Control and Prevention Agency (KDCA). 2016 Korea National Health and Nutrition Examination Survey (KNHNES). Korea. 2018. Available online: https://knhanes.kdca.go.kr/knhanes/sub03/sub03_02_05.do (accessed on 15 October 2021).
- Jung, H.K. Consumer Survey and Hazard Analysis for the Improvement of Food Hygiene and Safety in Purchase. Master’s Thesis, Korea University, Seoul, Korea, August 2011. [Google Scholar]
- Park, M.S.; Bahk, G.J. Current state for temperature management of cold and frozen food transportation vehicles in Jeonbuk province. J. Food Hyg. Saf. 2017, 32, 107–113. [Google Scholar] [CrossRef]
- Lee, H.; Kim, K.; Choi, K.H.; Yoon, Y. Quantitative microbial risk assessment for Staphylococcus aureus in natural and processed cheese in Korea. J. Dairy Sci. 2015, 98, 5931–5945. [Google Scholar] [CrossRef]
- Teunis, P.F.; Nagelkerke, N.J.; Haas, C.N. Dose response models for infectious gastroenteritis. Risk Anal. 1999, 19, 1251–1260. [Google Scholar] [CrossRef]
- Sanaa, M.; Coroller, L.; Cerf, O. Risk assessment of listeriosis linked to the consumption of two soft cheeses made from raw milk: Camembert of Normandy and Brie of Meaux. Risk Anal. 2004, 24, 389–399. [Google Scholar] [CrossRef] [PubMed]
- Vose, D.J. Risk analysis in relation to the importation and exportation of animal products. Rev. Sci. Tech. 1997, 16, 17–29. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Salmonella. 2022. Available online: https://www.cdc.gov/salmonella/index.html (accessed on 12 October 2022).
- Kim, M.S.; Lim, T.H.; Jang, J.H.; Lee, D.H.; Kim, B.Y.; Kwon, J.H.; Choi, S.W.; Noh, J.Y.; Hong, Y.H.; Lee, S.B.; et al. Prevalence and antimicrobial resistance of Salmonella species isolated from chicken meats produced by different integrated broiler operations in Korea. Poult. Sci. 2012, 91, 2370–2375. [Google Scholar] [CrossRef]
- Nauta, M.; van Der Fels-Klerx, I.; Havelaar, A. A poultry-processing model for quantitative microbiological risk assessment. Risk Anal. 2005, 25, 85–98. [Google Scholar] [CrossRef]
- Rose, N.; Beaudeau, F.; Drouin, P.; Toux, J.Y.; Rose, V.; Colin, P. Risk factors for Salmonella enterica subsp. enterica contamination in French broiler-chicken flocks at the end of the rearing period. Prev. Vet. Med. 1999, 39, 265–277. [Google Scholar] [CrossRef]
- Marin, C.; Lainez, M. Salmonella detection in feces during broiler rearing and after live transport to the slaughterhouse. Poult. Sci. 2009, 88, 1999–2005. [Google Scholar] [CrossRef]
- McCrea, B.; Tonooka, K.; Van Worth, C.; Boggs, C.; Atwill, E.; Scharader, J. Prevalence of Campylobacter and Salmonella species on farm after transport, and at processing in specialty market poultry. Poult. Sci. 2006, 85, 136–143. [Google Scholar] [CrossRef]
- Xiao, X.; Wang, W.; Zhang, J.; Liao, M.; Rainwater, C.; Yang, H.; Li, Y. A quantitative risk assessment model of Salmonella contamination for the yellow-feathered broiler chicken supply chain in China. Food Control. 2021, 121, 107612. [Google Scholar] [CrossRef]
- Berrang, M.E.; Buhr, R.J.; Cason, J.A.; Dickens, J.A. Microbiological consequences of skin removal prior to evisceration of broiler carcasses. Poult. Sci. 2002, 81, 134–138. [Google Scholar] [CrossRef]
- Collineau, L.; Chapman, B.; Bao, X.; Sivapathasundaram, B.; Carson, C.A.; Fazil, A.; Reid-Smith, R.J.; Smith, B.A. A farm-to-fork quantitative risk assessment model for Salmonella Heidelberg resistant to third-generation cephalosporins in broiler chickens in Canada. Int. J. Food Microbiol. 2020, 330, 108559. [Google Scholar] [CrossRef]
- Andre, A.; Arief, I.I.; Apriantini, A.; Jayanegara, A.; Budiman, C. Antimicrobial activity of propolis extract and their application as a natural preservative in livestock products: A meta-analysis. Food Sci. Anim. Resour. 2022, 42, 280–294. [Google Scholar] [CrossRef]
- Nastasijevic, I.; Lakicevic, B.; Petrovic, Z. Cold chain management in meat storage, distribution and retail: A review. IOP Conf. Ser. Earth Environ. Sci. 2017, 85, 012022. [Google Scholar] [CrossRef]
- Hadjicharalambous, C.; Grispoldi, L.; Chalias, T.; Cenci-Goga, B. A quantitative risk assessment of Listeria monocytogenes from prevalence and concentration data: Application to a traditional ready to eat (RTE) meat product. Int. J. Food Microbiol. 2022, 379, 109843. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention (CDC). Salmonella Outbreak Linked to Raw Frozen Breaded Stuffed Chicken Products. Available online: https://www.cdc.gov/salmonella/enteritidis-06-21/index.html. (accessed on 15 October 2022).
- Dogan, O.B.; Clarke, J.; Mattos, F.; Wang, B. A quantitative microbial risk assessment model of Campylobacter in broiler chickens: Evaluating processing interventions. Food Control. 2019, 100, 97–110. [Google Scholar] [CrossRef]

| Temperature (°C) | |||||
|---|---|---|---|---|---|
| 4 | 10 | 15 | 25 | ||
| Kinetic parameters | μmax | −0.02 ± 0.01 | 0.01 ± 0.02 | 0.13 ± 0.02 | 0.34 ± 0.07 |
| LPD | 25.03 ± 8.03 | 18.06 ± 3.93 | 12.79 ± 3.85 | 4.79 ± 1.53 | |
| N0 | 3.0 ± 0.1 | 3.4 ± 0.7 | 3.5 ± 0.8 | 3.5 ± 0.6 | |
| R2 | 0.825 ± 0.084 | 0.551 ± 0.324 | 0.967 ± 0.026 | 0.959 ± 0.013 | |
| Input Model | Unit | Variable | Formula | Reference |
|---|---|---|---|---|
| PRODUCT | ||||
| Pathogen contamination level | ||||
| Salmonella prevalence | PR | = RiskBeta(6, 266) for broiler chicken = RiskBeta(17, 190) for duck | This research; [33] | |
| Level of initial contamination | CFU/g | C | = −LN(1 − PR)/25g | [32] |
| Log CUF/g | IC | = LOG(C) | ||
| TRANSPORTATION | ||||
| Time | h | Timetrans | = RiskPert(0.5, 4, 9) | Personal communication a |
| Temperature | °C | Temptrans | = RiskUniform(2.12, 12.54) | [23] |
| Growth | h0 | = Average(LPD × growth rate), Fixed 0.7967 | This research; [23] | |
| Log CFU/g | Y0 | = Average(Y0i), Fixed 3.4 | This research; [23] | |
| Log CFU/g | Yend | = Average(Yendi), Fixed 5.8 | This research; [23] | |
| ln(q) | = LN(1/(EXP(h0) − 1)) | This research; [23] | ||
| Growth rate | Log CFU/g/h | GRtrans | = IF(Temptrans > 4.46207, (0.0294 × (Temptrans − 4.46207))2, 0) | This research; [23] |
| Level of Salmonella | Log CFU/g | C1 | = IC + 1/(1 + EXP(−ln(q))) × (1 − (10 −|Y0−Yend|/LN(10))) × GRtrans × Timetrans | This research; [23] |
| MARKET | ||||
| Market storage | ||||
| Time | h | Timemark-st | = RiskUniform(0, 24) | Personal communication |
| Temperature | °C | Tempmark-st | = RiskPert(−2, 2, 5) | Personal communication |
| Growth | h0 | = Average(LPD × growth rate), Fixed 0.7967 | This research; [23] | |
| Log CFU/g | Y0 | = Average(Y0i), Fixed 3.4 | This research; [23] | |
| Log CFU/g | Yend | = Average(Yendi), Fixed 5.8 | This research; [23] | |
| ln(q) | = LN(1/(EXP(h0) − 1)) | This research; [23] | ||
| Growth rate | Log CFU/g/h | GRmark-st | = IF(Tempmark-st > 4.46207, (0.0294 × (Tempmark-st − 4.46207))2, 0) | This research; [23] |
| Level of Salmonella | Log CFU/g | C2 | = C1 + 1/(1 + EXP(−ln(q)))×(1 − (10 −|Y0−Yend|/LN(10))) × GRmark-st × Timemark-st | This research; [23] |
| Market display | ||||
| Time | h | Timemark-dis | = RiskPert(0, 24, 48) | Personal communication |
| Temperature | °C | Tempmark-dis | = RiskUniform(−2, 10) | Personal communication |
| Growth | h0 | = Average(LPD × growth rate), Fixed 0.7967 | This research; [23] | |
| Log CFU/g | Y0 | = Average(Y0i), Fixed 3.4 | This research; [23] | |
| Log CFU/g | Yend | = Average(Yendi), Fixed 5.8 | This research; [23] | |
| ln(q) | = LN(1/(EXP(h0) − 1)) | This research; [23] | ||
| Growth rate | Log CFU/g/h | GRmark-dis | = IF(Tempmark-dis > 4.46207, (0.0294 × (Tempmark-dis − 4.46207))2, 0) | This research; [23] |
| Level of Salmonella | Log CFU/g | C3 | = C2 + 1/(1 + EXP(−ln(q)))×(1 − (10 −|Y0−Yend|/LN(10))) × GRmark-dis × Timemark-dis | This research; [23] |
| TRANSPORTATION (vehicle) | ||||
| Time | h | Timeveh | = RiskUniform(0.325, 1.643) | [28] |
| Temperature | °C | Tempveh | = RiskPert(10, 18, 25) | [28] |
| Growth | h0 | = Average(LPD × growth rate), Fixed 0.7967 | This research; [23] | |
| Log CFU/g | Y0 | = Average(Y0i), Fixed 3.4 | This research; [23] | |
| Log CFU/g | Yend | = Average(Yendi), Fixed 5.8 | This research; [23] | |
| ln(q) | = LN(1/(EXP(h0) − 1)) | This research; [23] | ||
| Growth rate | Log CFU/g/h | GRveh | = IF(Tempveh > 4.46207, (0.0294 × (Tempveh − 4.46207))2, 0) | This research; [23] |
| Level of Salmonella | Log CFU/g | C4 | = C3 + 1/(1 + EXP(−ln(q)))×(1 − (10 −|Y0−Yend|/LN(10))) × GRveh × Timeveh | This research; [23] |
| HOME | ||||
| Storage | ||||
| Time | h | Timehome | = RiskUniform(0, 72) | Personal communication |
| Temperature | °C | Temphome | = RiskLogLogistic(−29.283, 33.227, 26.666, RiskTruncate(−5, 20)) | [30] |
| Growth | h0 | = Average(LPD × growth rate), Fixed 0.7967 | This research; [23] | |
| Log CFU/g | Y0 | = Average(Y0i), Fixed 3.4 | This research; [23] | |
| Log CFU/g | Yend | = Average(Yendi), Fixed 5.8 | This research; [23] | |
| ln(q) | = LN(1/(EXP(h0) − 1)) | This research; [23] | ||
| Growth rate | Log CFU/g/h | GRhome | = IF(Temphome > 4.46207, (0.0294 × (Temphome − 4.46207))2, 0) | This research; [23] |
| Level of Salmonella | Log CFU/g | C5 | = C4 + 1/(1 + EXP(−ln(q)))×(1 − (10 −|Y0−Yend|/LN(10))) × GRhome × Timehome | This research; [23] |
| CFU/g | C5CFU/g | = 10C5 | ||
| CONSUMPTION | ||||
| Daily consumption frequency for broiler chicken | % | ConFre | Fixed 13.7 | [27] b |
| CF(0) | = 1 − 13.7/100 | |||
| CF(1) | = 13.7/100 | |||
| CF | = RiskDiscrete({0, 1}, {CF(0), CF(1)}) | |||
| Daily consumption frequency for duck | % | ConFre | Fixed 1.8 | [27] |
| CF(0) | = 1 − 1.8/100 | |||
| CF(1) | = 1.8/100 | |||
| CF | = RiskDiscrete({0, 1}, {CF(0), CF(1)}) | |||
| COOKING METHOD—Broiler chicken | ||||
| Dry heat cooking | Cook(dry) | = 36/100 | [27] | |
| Moist heat cooking | Cook(moist) | = 64/100 | [27] | |
| Cook | = RiskDiscrete({1, 2}, {Cook(dry), Cook(moist)}) | |||
| Consumption at dry heat cooking | g | Consumpdry-cook | = RiskLognorm(158.26, 203.31, RiskShift(−3.7516), RiskTruncate(0, 1256.4)) | [27] |
| Consumption at moist heat cooking | g | Consumpmoist-cook | = RiskInvgauss(95.947, 101.63, RiskShift(−9.9848), RiskTruncate(0, 589.1)) | [27] |
| g | Consump | = IF(Cook = 1,Consumpdry-cook, Consumpmoist-cook) | ||
| Total consumption | g | Amount | = IF(CF = 0, 0, Consump) | |
| COOKING METHOD—Duck | ||||
| Dry heat cooking | Cook(dry) | = 51/100 | [27] | |
| Moist heat cooking | Cook(moist) | = 49/100 | [27] | |
| Cook | = RiskDiscrete({1,2}, {Cook(dry), Cook(moist)}) | |||
| Consumption at dry heat cooking | g | Consumpdry-cook | = RiskLognorm(88.864, 60.024, RiskShift(−7.5199), RiskTruncate(0, 294.3)) | [27] |
| Consumption at moist heat cooking | g | Consumpmoist-cook | = RiskExpon(58.692, RiskShift(−0.75665), RiskTruncate(0, 461.7)) | [27] |
| g | Consump | = IF(Cook = 1, Consumpdry-cook, Consumpmoist-cook) | ||
| Total consumption | g | Amount | = IF(CF = 0, 0, Consump) | |
| REDUCTION—Broiler chicken | ||||
| Dry heat cooking | Reduce(dry) | = 36/100 | [27] | |
| Moist heat cooking | Reduce(moist) | = 64/100 | [27] | |
| Reduce | = RiskDiscrete({1, 2}, {Reduce(dry), Reduce(moist)}) | |||
| Reduce(dry)—dry heat cooking | ||||
| Cooking time | h | Timedry-cook | = RiskPert(0.08, 0.13, 0.25) | This research |
| Food temperature during cooking | °C | Tempdry-cook | = RiskPert(74 × 0.8, 74, 74 × 1.2) | This research; [20] |
| CFU/g | Reducedry-cook | = IF(AND(Tempdry-cook > 74, Timedry-cook > 0.13), 0, C5CFU/g × 0.01) | ||
| Reduce(moist)—moist heat cooking | ||||
| Cooking time | h | Timemoist-cook | = RiskPert(0.08, 0.17, 0.33) | This research |
| Food temperature during cooking | °C | Tempmoist-cook | = RiskPert(74 × 0.8, 74, 74 × 1.2) | This research; [20] |
| CFU/g | Reducemoist-cook | = IF(AND(Tempmoist-cook > 74, Timemoist-cook > 0.17), 0, C5CFU/g × 0.01) | ||
| Total reduction | CFU/g | Reduction | = IF({Reduce = 1, Reducedry-cook, Reducemoist-cook) | |
| Final concentration | CFU/g | C6 (Cooked) | = IF(CF = 0, 0, Reduction) | This research |
| REDUCTION—Duck | ||||
| Dry heat cooking | Reduce(dry) | = 51/100 | [27] | |
| Moist heat cooking | Reduce(moist) | = 49/100 | [27] | |
| Reduce | = RiskDiscrete({1, 2}, {Reduce(dry), Reduce(moist)}) | |||
| Reduce(dry)—dry heat cooking | ||||
| Cooking time | h | Timedry-cook | = RiskPert(0.03, 0.05, 0.1) | This research |
| Food temperature during cooking | °C | Tempdry-cook | = RiskPert(74 × 0.8, 74, 74 × 1.2) | This research; [20] |
| CFU/g | Reducedry-cook | = IF(AND(Tempdry-cook > 74, Timedry-cook > 0.05), 0, C5CFU/g × 0.01) | ||
| Reduce(moist)—moist heat cooking | ||||
| Cooking time | h | Timemoist-cook | = Riskpert(0.12, 0.25, 0.33) | This research |
| Food temperature during cooking | °C | Tempmoist-cook | = Riskpert(74 × 0.8, 74, 74 × 1.2) | This research; [20] |
| CFU/g | Reducemoist-cook | = IF(AND(Tempmoist-cook > 74, Timemoist-cook > 0.25), 0, C5CFU/g × 0.01) | ||
| Total reduction | CFU/g | Reduction | = IF({Reduce = 1, Reducedry-cook, Reducemoist-cook) | |
| Final concentration | CFU/g | C6 (Cooked) | = IF(CF = 0, 0, Reduction) | This research |
| DOSE-RESPONSE | ||||
| Salmonella amounts | CFU | D | = C6 × Amount | |
| Parameter of Beta-Poisson | α | Fixed, 0.89 | [31] | |
| β | Fixed, 4.4 × 105 | [31] | ||
| RISK | ||||
| Probability of illness/person/day | Risk | = 1 − (1 + D/β)−α | ||
| 50% | 90% | 95% | 99% | Mean | ||
|---|---|---|---|---|---|---|
| Chicken | Probability of illness/person/day applied cooking methods | 0 | 0 | 1.6 × 10−9 | 7.3 × 10−9 | 3.0 × 10−10 |
| Cooking methods not considered | 0 | 8.3 × 10−8 | 2.7 × 10−7 | 10.0 × 10−7 | 5.2 × 10−8 | |
| Duck | Probability of illness/person/day applied cooking methods | 0 | 0 | 0 | 1.5 × 10−9 | 8.8 × 10−11 |
| Cooking methods not considered | 0 | 0 | 0 | 4.1 × 10−7 | 1.4 × 10−8 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oh, H.; Yoon, Y.; Yoon, J.-W.; Oh, S.-W.; Lee, S.; Lee, H. Salmonella Risk Assessment in Poultry Meat from Farm to Consumer in Korea. Foods 2023, 12, 649. https://doi.org/10.3390/foods12030649
Oh H, Yoon Y, Yoon J-W, Oh S-W, Lee S, Lee H. Salmonella Risk Assessment in Poultry Meat from Farm to Consumer in Korea. Foods. 2023; 12(3):649. https://doi.org/10.3390/foods12030649
Chicago/Turabian StyleOh, Hyemin, Yohan Yoon, Jang-Won Yoon, Se-Wook Oh, Soomin Lee, and Heeyoung Lee. 2023. "Salmonella Risk Assessment in Poultry Meat from Farm to Consumer in Korea" Foods 12, no. 3: 649. https://doi.org/10.3390/foods12030649
APA StyleOh, H., Yoon, Y., Yoon, J.-W., Oh, S.-W., Lee, S., & Lee, H. (2023). Salmonella Risk Assessment in Poultry Meat from Farm to Consumer in Korea. Foods, 12(3), 649. https://doi.org/10.3390/foods12030649






