Genotoxicity Comparison between Morinda citrifolia Fruit and Seed Substances
Abstract
1. Introduction
2. Materials and Methods
2.1. Chemicals and Reagents
2.2. Preparation of Noni Fruit and Seed Substances/Samples
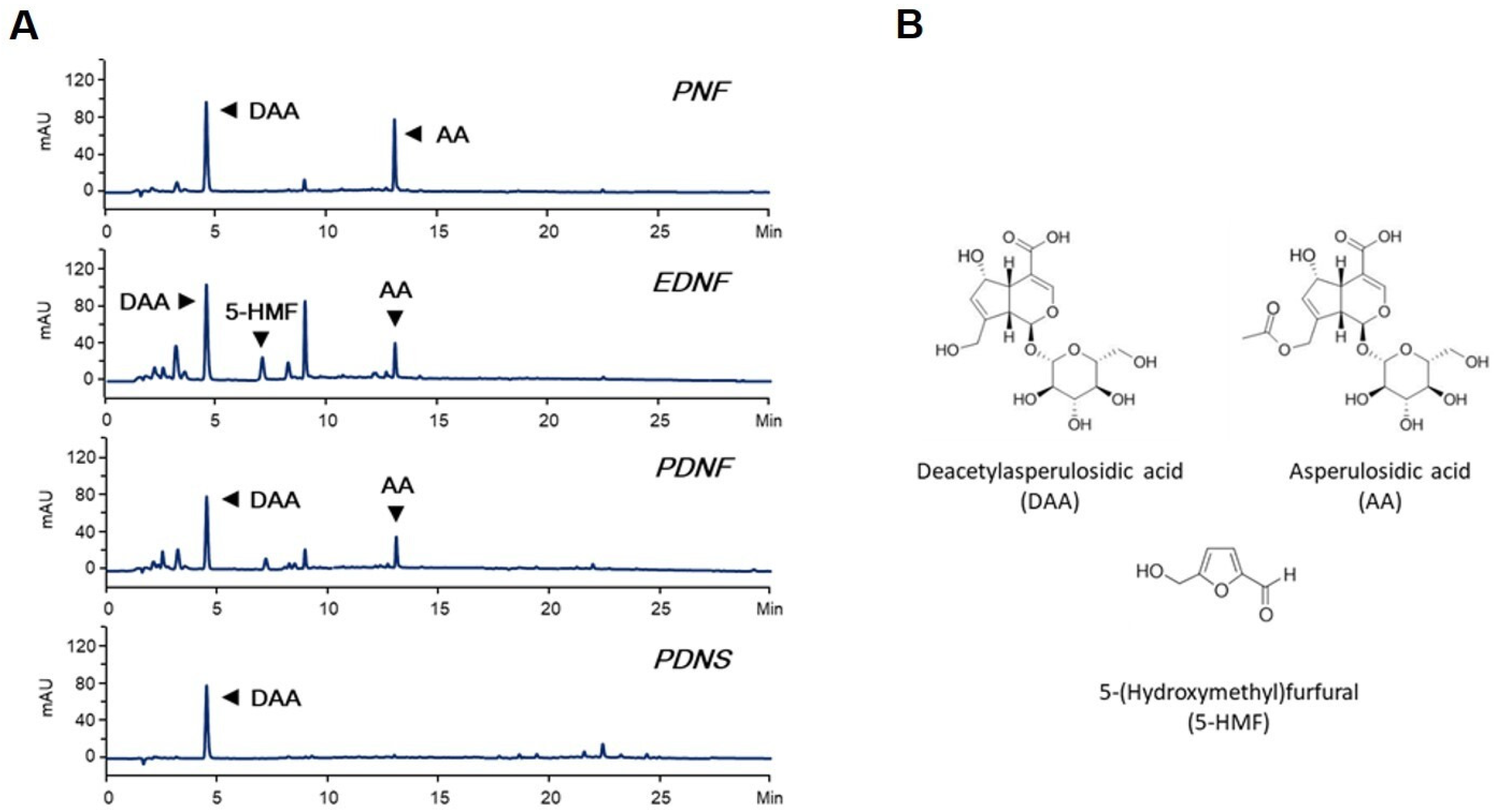
2.3. Chromatographic Analysis
2.4. Animals
2.5. Genotixicity Tests
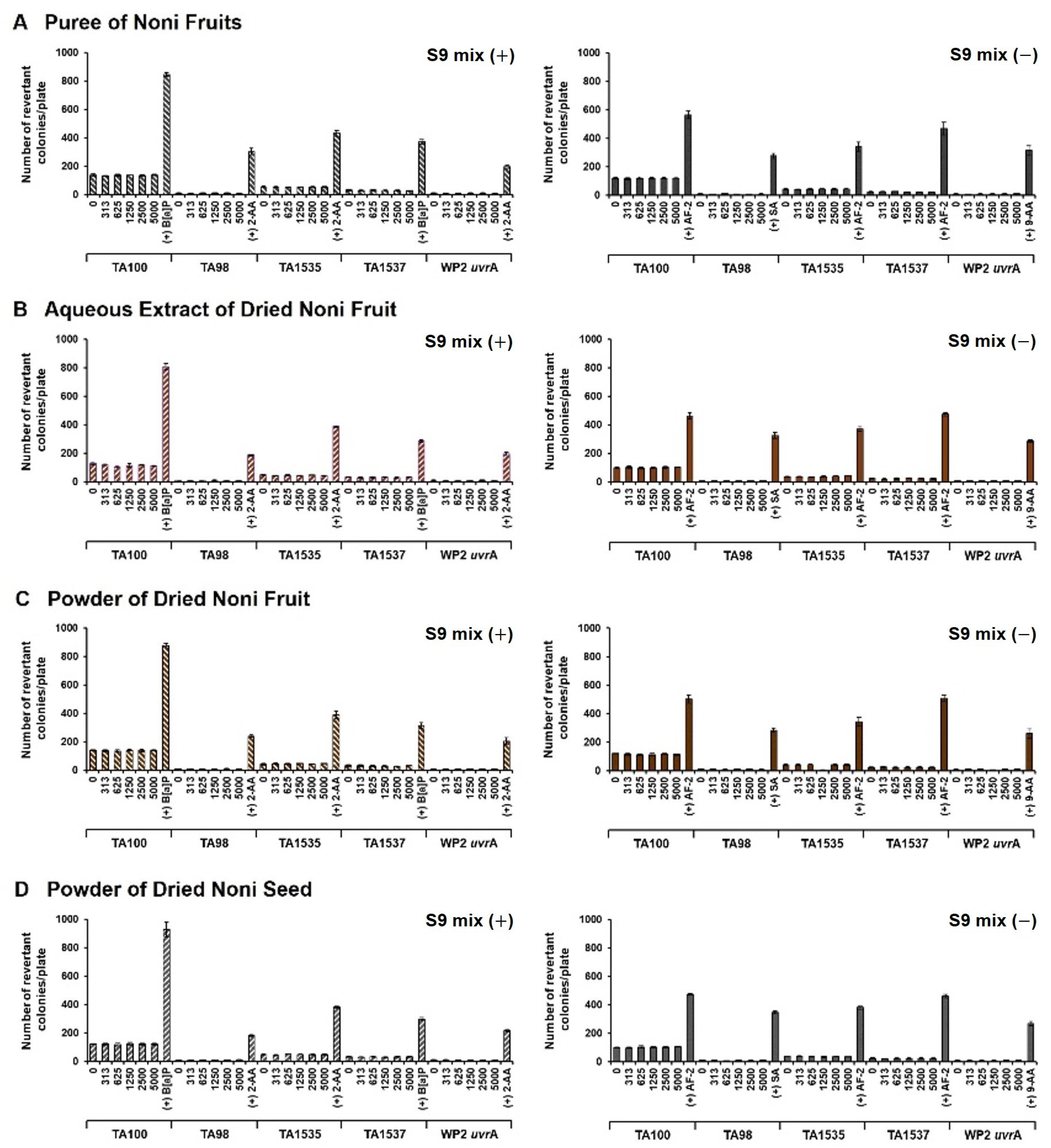
2.5.1. Ames Test
2.5.2. Chromosomal Aberration Test
2.5.3. Micronucleus Test
3. Results
3.1. Phytochemical Analysis
3.2. Ames Test
3.3. Chromosomal Aberration Test
3.4. In Vivo Micronucleus Test
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Chan-Blanco, Y.; Vaillant, F.; Perez, A.M.; Reynes, M.; Brillouet, J.-M.; Brat, P. The noni fruit (Morinda citrifolia L.): A review of agricultural research, nutritional and therapeutic properties. J. Food Compos. Anal. 2006, 19, 645–654. [Google Scholar] [CrossRef]
- Almeida, E.S.; De Oliveira, D. Properties and applications of Morinda Citrofolia (Noni): A review. Compr. Rev. Food Sci. Food. Saf. 2019, 18, 883–909. [Google Scholar] [CrossRef] [PubMed]
- Lachenmeier, K.; Musshoff, F.; Madea, B.; Reusch, H.; Lachenmeier, D. Authentication of Noni (Morinda citrifolia) Juice. Dtsch. Lebensm. 2006, 102, 58–61. [Google Scholar]
- Motshakeri, M.; Ghazali, H.M. Nutritional, Phytochemical and Commercial Quality of Noni Fruit: A Multi-Beneficial Gift from Nature. Trends Food Sci. Technol. 2015, 45, 118–129. [Google Scholar] [CrossRef]
- Brown, A.C. Anticancer Activity of Morinda citrifolia (Noni) Fruit: A Review. Phytother. Res. 2012, 26, 1427–1440. [Google Scholar] [CrossRef]
- Pawlus, A.D.; Kinghorn, A.D. Review of the Ethnobotany, Chemistry, Biological Activity and Safety of the Botanical Dietary Supplement Morinda citrifolia (noni). J. Pharm. Pharmacol. 2010, 59, 1587–1609. [Google Scholar] [CrossRef]
- Potterat, O.; Hamburger, M. Morinda citrifolia (Noni) fruit-phytochemistry, pharmacology, safety. Planta Med. 2007, 73, 191–199. [Google Scholar] [CrossRef]
- Hong, Y.H.; Yi, Y.S.; Han, S.Y.; Aziz, N.; Kim, H.G.; Park, S.H.; Hossain, M.A.; Baik, K.S.; Choi, S.Y.; Lee, J.; et al. Morinda citrifolia noni water extract enhances innate and adaptive immune responses in healthy mice, ex vivo, and in vitro. Phytother. Res. 2019, 33, 676–689. [Google Scholar] [CrossRef]
- Kustiarini, D.A.; Nishigaki, T.; Kanno, H. Effects of Morinda citrifolia on Rheumatoid Arthritis in SKG Mice. Biol. Pharm. Bull. 2019, 42, 496–500. [Google Scholar] [CrossRef]
- Li, J.; Niu, D.; Zhang, Y.; Zeng, X.A. Physicochemical properties, antioxidant and antiproliferative activities of polysaccharides from Morinda citrifolia L. (Noni) based on different extraction methods. Int. J. Biol. Macromol. 2020, 150, 114–121. [Google Scholar] [CrossRef]
- Inada, A.C.; Figueiredo, P.S.; Dos Santos-Eichler, R.A.; Freitas, K.C.; Hiane, P.A.; De Castro, A.P.; Guimarães, R.C.A. Morinda citrifolia Lin (Noni) and its potential in obesity-related metabolic dysfunction. Nutrients 2017, 9, 540. [Google Scholar] [CrossRef] [PubMed]
- Assi, A.R.; Darwis, Y.; Abdulbaqi, I.M.; Khan, A.A.; Vuanghao, L.; Laghari, M.H. Morinda citrifolia (Noni): A Comprehensive Review on Its Industrial Uses, Pharmacological Activities, and Clinical Trials. Arab. J. Chem. 2017, 10, 691–707. [Google Scholar] [CrossRef]
- Torres, M.A.O.; de Fátima Braga Magalhães, I.; Mondêgo-Oliveira, R.; de Sá, J.C.; Rocha, A.L.; Abreu-Silva, A.L. One Plant, Many Uses: A Review of the Pharmacological Applications of Morinda citrifolia. Phytother. Res. 2017, 31, 971–979. [Google Scholar] [CrossRef] [PubMed]
- ECSC. Opinion of the Scientific Committee on Food on Tahitian Noni Juice European Commission Scientific Committee on Food; ECSC: Brussels, Belgium, 2003.
- Bussmann, R.W.; Hennig, L.; Giannis, A.; Ortwein, J.; Kutchan, T.M.; Feng, X. Anthraquinone Content in Noni (Morinda citrifolia L.). Evid. Based Complement. Alternat. Med. 2013, 2013, 208378. [Google Scholar] [CrossRef] [PubMed]
- EFSA. Opinion on the Safety of Tahitian Noni® ‘Morinda citrifolia (noni) Fruit Puree and Concentrate’ as a Novel Food Ingredient. EFSA J. 2009, 7, 998. [Google Scholar]
- West, B.J.; Berrio, L.F. Tahitian Noni Juice Is Not Hepatotoxic. Rev. Esp. Enferm. Dig. 2007, 99, 737–738, author reply 738. [Google Scholar] [CrossRef] [PubMed][Green Version]
- West, B.J.; Su, C.X.; Jensen, C.J. Hepatotoxicity and Subchronic Toxicity Tests of Morinda citrifolia (noni) Fruit. J. Toxicol. Sci. 2009, 34, 581–585. [Google Scholar] [CrossRef]
- West, B.J.; White, L.D.; Jensen, C.J.; Palu, A.K. A Double-Blind Clinical Safety Study of noni Fruit Juice. Pac. Health Dialog. 2009, 15, 21–32. [Google Scholar]
- Westendorf, J.; Effenberger, K.; Iznaguen, H.; Basar, S. Toxicological and Analytical Investigations of Noni (Morinda citrifolia) Fruit Juice. J. Agric. Food Chem. 2007, 55, 529–537. [Google Scholar] [CrossRef]
- Estevam dos Santos, P.; Carmem Monte Egito, L.; Batistuzzo de Medeiros, S.R.; Agnez-Lima, L.F. Genotoxicity Induced by Eugenia Caryophyllata Infusion. J. Toxicol. Environ. Health A. 2008, 71, 439–444. [Google Scholar] [CrossRef]
- Rolim, L.A.D.M.M.; Macêdo, M.F.S.; Sisenando, H.A.; Napoleão, T.H.; Felzenszwalb, I.; Aiub, C.A.F.; Coelho, L.C.B.B.; Medeiros, S.R.B.; Paiva, P.M.G. Genotoxicity Evaluation of Moringa oleifera Seed Extract and Lectin. J. Food Sci. 2011, 76, T53–T58. [Google Scholar] [CrossRef] [PubMed]
- Zan, M.A.; Ferraz, A.B.F.; Richter, M.F.; Picada, J.N.; de Andrade, H.H.R.; Lehmann, M.; Dihl, R.R.; Nunes, E.; Semedo, J.; Da Silva, J. In Vivo Genotoxicity Evaluation of an Artichoke (Cynara Scolymus L.) Aqueous Extract. J. Food Sci. 2013, 78, T367–T371. [Google Scholar] [CrossRef] [PubMed]
- Inoue, K.; Yoshida, M.; Takahashi, M.; Fujimoto, H.; Shibutani, M.; Hirose, M.; Nishikawa, A. Carcinogenic Potential of Alizarin and Rubiadin, Components of Madder Color, in a Rat Medium-Term Multi-Organ Bioassay. Cancer Sci. 2009, 100, 2261–2267. [Google Scholar] [CrossRef] [PubMed]
- NTP. NTP Technical Report on the Toxicology and Carcinogenesis Studies of Anthraquinone (CAS No. 84-65–1) in F344/N Rats and B6C3F1 Mice (Feed Studies). Natl Toxicol. Program Tech. Rep. Ser. 2005, 494, 1–358. [Google Scholar]
- Kiathevest, K.; Goto, M.; Sasaki, M.; Pavasant, P.; Shotipruk, A. Extraction and Concentration of Anthraquinones from Roots of Morinda citrifolia by Non-Ionic Surfactant Solution. Sep. Purif. Technol. 2009, 66, 111–117. [Google Scholar] [CrossRef]
- Mariann Garner-Wizard, S.H.; Hoots, D.; Robbins, S.; Van De Walle, G. Genotoxicity of Noni Juice Associated with the Occurrence of Hydroxyanthraquinones. Am. Bot. Council. 2007, 324, 020171–020324. [Google Scholar]
- Franchi, L.P.; Guimarães, N.G.; De Andrade, L.R.; De Andrade, H.; Lehmann, M.; Dihl, R.; Cunha, K. Antimutagenic and antirecombinagenic activities of noni fruit juice in somatic cells of Drosophila melanogaster. An. Da Acad. Bras. De Cienc. 2013, 85, 585–594. [Google Scholar] [CrossRef][Green Version]
- Miao, W.G.; Tang, C.; Ye, Y.; Quinn, R.J.; Feng, Y. Traditional Chinese medicine extraction method by ethanol delivers drug-like molecules. Chin. J. Nat. Med. 2019, 17, 713–720. [Google Scholar] [CrossRef]
- OECD. Health Effects Test No. 471: Bacterial Reverse Mutation Test. In Guideline for the Testing of Chemicals; Section 4; Organization for Economic Cooperation and Development: Paris, France, 1997. [Google Scholar]
- OECD. Health Effects Test No. 473: In Vitro Mammalian Chromosome Aberration Test. In Guideline for the Testing of Chemicals; Section 4; Organization for Economic Cooperation and Development: Paris, France, 2016. [Google Scholar]
- OECD. Health Effects Test No. 474: Mammalian Erythrocyte Micronucleus Test. In Guideline for the Testing of Chemicals; Section 4; Organization for Economic Cooperation and Development: Paris, France, 2016. [Google Scholar]
- MFDS. Guidelines for Toxicity Tests of Pharmaceuticals. No. 2017-71; Ministry of Food and Drug Safety: Cheongju, Korea, 2017.
- Maron, D.M.; Ames, B.N. Revised Methods for the Salmonella Mutagenicity Test. Mutat. Res. 1983, 113, 173–215. [Google Scholar] [CrossRef]
- Ishidate, M.; Sofuni, T. The In Vitro Chromosomal Aberration Test Using Chinese Hamster Lung (CHL) Fibroblast Cells in Culture. Prog. Muation Res. 1985, 5, 427–432. [Google Scholar]
- Erexson, G.L. Lack of In Vivo Clastogenic Activity of Grape Seed and Grape Skin Extracts in a Mouse Micronucleus Assay. Food Chem. Toxicol. 2003, 41, 347–350. [Google Scholar] [CrossRef]
- Hayashi, M.; Sofuni, T.; Ishidate, M. An Application of Acridine Orange Fluorescent Staining to the Micronucleus Test. Mutat. Res. 1983, 120, 241–247. [Google Scholar] [CrossRef]
- Kirkland, D.J.; Mahon, G.A.T. Statistical Evaluation of Mutagenicity Test Data: UKEMS Sub-Committee on Guidelines for Mutagenicity Testing; Part III; Cambridge University Press: Cambridge, UK, 1989. [Google Scholar]
- Deng, S.; West, B.J.; Jensen, C.J. A Quantitative Comparison of Phytochemical Components in Global noni Fruits and Their Commercial Products. Food Chem. 2010, 122, 267–270. [Google Scholar] [CrossRef]
- Deng, S.; West, B.J. Thin layer Chromatography Methods for Rapid Identity Testing of Morinda citrifolia L. (Noni) Fruit and Leaf. Adv. J. Food Sci. Tech. 2010, 2, 298–302. [Google Scholar]
- Sofuni, T. Data Book of Chromosomal Aberration Test In Vitro. Revised Edition 1998; Life-science Information Center Ltd.: Tokyo, Japan, 1999. [Google Scholar]
- Westendorf, J.; Poginsky, B.; Marquardt, H.; Groth, G.; Marquardt, H. The Genotoxicity of Lucidin, a Natural Component of Rubia Tinctorum L., and Lucidinethylether, a Component of Ethanolic Rubia Extracts. Cell Biol. Toxicol. 1988, 4, 225–239. [Google Scholar] [CrossRef]
- Ames, B.N.; McCann, J.; Yamasaki, E. Methods for Detecting Carcinogens and Mutagens with the Salmonella/Mammalian-Microsome Mutagenicity Test. Mutat. Res. 1975, 31, 347–364. [Google Scholar] [CrossRef]
- West, B.J.; Su, C.X.; Jensen, C.J. Prenatal toxicity test of Morinda citrifolia (noni) fruit. J. Toxicol. Sci. 2008, 33, 647–649. [Google Scholar] [CrossRef][Green Version]
- Fenech, M. Cytokinesis-Block Micronucleus Cytome Assay. Nat. Protoc. 2007, 2, 1084–1104. [Google Scholar] [CrossRef]
- Murgia, E.; Ballardin, M.; Bonassi, S.; Rossi, A.M.; Barale, R. Validation of Micronuclei Frequency in Peripheral Blood Lymphocytes as Early Cancer Risk Biomarker in a Nested Case–Control Study. Mutat. Res. 2008, 639, 27–34. [Google Scholar] [CrossRef]
- Bonassi, S.; Znaor, A.; Ceppi, M.; Lando, C.; Chang, W.P.; Holland, N.; Kirsch-Volders, M.; Zeiger, E.; Ban, S.; Barale, R.; et al. An Increased Micronucleus Frequency in Peripheral Blood Lymphocytes Predicts the Risk of Cancer in Humans. Carcinogenesis 2007, 28, 625–631. [Google Scholar] [CrossRef]
- Witt, K.L.; Knapton, A.; Wehr, C.M.; Hook, G.J.; Mirsalis, J.; Shelby, M.D.; MacGregor, J.T. Micronucleated Erythrocyte Frequency in Peripheral Blood of B6C3F(1) Mice from Short-Term, Prechronic, and Chronic Studies of the NTP Carcinogenesis Bioassay Program. Environ. Mol. Mutagen. 2000, 36, 163–194. [Google Scholar] [CrossRef]
- Hovhannisyan, G.G. Fluorescence In Situ Hybridization in Combination with the Comet Assay and Micronucleus Test in Genetic Toxicology. Mol. Cytogenet. 2010, 3, 17. [Google Scholar] [CrossRef] [PubMed]
- OECD. Principles on Good Laboratory Practice (as revised in 1997). In Document No. 1 ENV/MC/CHEM(98)17; Organization for Economic Cooperation and Development: Paris, France, 1998. [Google Scholar]
- Product Safety Labs. Guinea pig antigenicity study. In Tahitian Noni puree, Tahitian Noni juice, and Tahitian Noni concentrate; Eurofins Scientific, Inc.: East Brunswick, NJ, USA, 2000. [Google Scholar]
- Parra, V.; Lopez, A.G.; Ramos, A.R.; Ferrer, J.; González, V.; Penichet, M. Evaluación mutagénica de un extracto fluido con un menstruo etanólico Al 70 % de Teloxys ambrosioides L. Weber (apasote). Rev. Cuba. Plant. Med. 2000, 5, 102–105. [Google Scholar]
- Sehgal, I.; Winters, W.D.; Scott, M.; Kousoulas, K. An In Vitro and In Vivo Toxicologic Evaluation of a Stabilized Aloe Vera Gel Supplement Drink in Mice. Food Chem. Toxicol. 2013, 55, 363–370. [Google Scholar] [CrossRef] [PubMed]
- Verma, A.; Gupta, A.K.; Kumar, A.; Khan, P.K. Cytogenetic Toxicity of Aloe vera (a Medicinal Plant). Drug Chem. Toxicol. 2012, 35, 32–35. [Google Scholar] [CrossRef]
| PNF | EDNF | PDNF | PDNS | ||
|---|---|---|---|---|---|
| DAA | Rt (min) | 4.59 ± 0.05 | 4.56 ± 0.01 | 4.57 ± 0.02 | 4.53 ± 0.02 |
| Contents (mg/g) | 5.70 ± 0.01 | 9.44 ± 0.02 | 4.67 ± 0.01 | 4.13 ± 0.01 | |
| AA | Rt (min) | 13.06 ± 0.01 | 12.98 ± 0.02 | 13.07 ± 0.01 | _ |
| Contents (mg/g) | 5.20 ± 0.01 | 3.52 ± 0.01 | 2.19 ± 0.01 | _ | |
| 5-HMF | Rt (min) | _ | 7.08 ± 0.04 | _ | _ |
| Contents (mg/g) | _ | 3.23 ± 0.01 | _ | _ | |
| Drug | Dose (μg/mL) | Chromosomal Aberration | Numerical ab. | RICC (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Structural ab. | |||||||||||
| Chromatid Type | Chromosome Type | Gaps | Others | Total | |||||||
| ctb | cte | csb | cse | Gaps | Others | −Gaps | +Gaps | PP + ER | |||
| Treatment: 6 h treatment and 18 h recovery (−S9 mix) | |||||||||||
| PNF | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 |
| 1250 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 88 | |
| 2500 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 89 | |
| 5000 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 79 | |
| MMC | 0.1 | 9 | 32 | 4 | 0 | 1 | 0 | 45 23 **/22 | 46 | 0 | 72 |
| Treatment: 6 h treatment and 18 h recovery (+S9 mix) | |||||||||||
| PNF | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 100 |
| 1250 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 96 | |
| 2500 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 96 | |
| 5000 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 93 | |
| CPA | 5.0 | 5 | 42 | 1 | 0 | 1 | 0 | 48 25 */23 | 49 | 0 | 60 |
| Treatment: 24 h treatment and 0 h recovery (−S9 mix) | |||||||||||
| PNF | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 |
| 1250 | 0 | 0 | 2 | 0 | 0 | 0 | 2 | 2 | 0 | 86 | |
| 2500 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 84 | |
| 5000 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 78 | |
| MMC | 0.05 | 4 | 36 | 2 | 1 | 0 | 0 | 42 23 */19 | 42 | 0 | 63 |
| Drug | Dose (μg/mL) | Chromosomal Aberration | Numerical ab. | RICC (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Structural ab. | |||||||||||
| Chromatid Type | Chromosome Type | Gaps | Others | Total | |||||||
| ctb | cte | csb | cse | Gaps | Others | −Gaps | +Gaps | PP + ER | |||
| Treatment: 6 h treatment and 18 h recovery (−S9 mix) | |||||||||||
| EDNF | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 100 |
| 1162.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 93 | |
| 2325 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 88 | |
| 4650 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 57 | |
| MMC | 0.1 | 8 | 45 | 4 | 1 | 1 | 0 | 55 29 **/26 | 56 | 0 | 65 |
| Treatment: 6 h treatment and 18 h recovery (+S9 mix) | |||||||||||
| EDNF | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 |
| 1250 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 90 | |
| 2500 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 84 | |
| 5000 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 66 | |
| CPA | 5.0 | 9 | 43 | 3 | 1 | 1 | 1 | 57 30 */27 | 58 | 0 | 55 |
| Treatment: 24 h treatment and 0 h recovery (−S9 mix) | |||||||||||
| EDNF | 0 | 2 | 0 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 100 |
| 1085.5 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 95 | |
| 2175 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 87 | |
| 4350 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 57 | |
| MMC | 0.05 | 8 | 43 | 5 | 2 | 0 | 0 | 58 29 */29 | 58 | 0 | 60 |
| Drug | Dose (μg/mL) | Chromosomal Aberration | Numerical ab. | RICC (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Structural ab. | |||||||||||
| Chromatid Type | Chromosome Type | Gaps | Others | Total | |||||||
| ctb | cte | csb | cse | Gaps | Others | −Gaps | +Gaps | PP + ER | |||
| Treatment: 6 h treatment and 18 h recovery (−S9 mix) | |||||||||||
| PDNF | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 1 | 2 | 0 | 100 |
| 512.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 86 | |
| 1025 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 79 | |
| 2050 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 78 | |
| 4100 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 57 | |
| MMC | 0.1 | 7 | 35 | 3 | 2 | 0 | 0 | 47 24 **/23 | 47 | 0 | 66 |
| Treatment: 6 h treatment and 18 h recovery (+S9 mix) | |||||||||||
| PDNF | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 100 |
| 625 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 95 | |
| 1250 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 91 | |
| 2500 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 58 | |
| CPA | 5.0 | 5 | 39 | 2 | 0 | 0 | 0 | 46 23 */23 | 46 | 0 | 64 |
| Treatment: 24 h treatment and 0 h recovery (−S9 mix) | |||||||||||
| PDNF | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 2 | 0 | 100 |
| 275 | 0 | 0 | 0 | 0 | 2 | 0 | 0 | 2 | 0 | 84 | |
| 550 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 79 | |
| 1100 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 57 | |
| MMC | 0.05 | 6 | 40 | 2 | 0 | 0 | 0 | 48 24 */24 | 48 | 0 | 76 |
| Drug | Dose (μg/mL) | Chromosomal Aberration | Numerical ab. | RICC (%) | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Structural ab. | |||||||||||
| Chromatid Type | Chromosome Type | Gaps | Others | Total | |||||||
| ctb | cte | csb | cse | Gaps | Others | −Gaps | +Gaps | PP + ER | |||
| Treatment: 6 h treatment and 18 h recovery (−S9 mix) | |||||||||||
| PDNS | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 100 |
| 112.5 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 94 | |
| 225 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 70 | |
| 450 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 51 | |
| MMC | 0.1 | 6 | 41 | 6 | 2 | 1 | 0 | 55 27 **/28 | 56 | 0 | 71 |
| Treatment: 6 h treatment and 18 h recovery (+S9 mix) | |||||||||||
| PDNS | 0 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 100 |
| 525 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 82 | |
| 1050 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 69 | |
| 2100 | 0 | 1 | 0 | 0 | 0 | 0 | 1 | 1 | 0 | 57 | |
| CPA | 5.0 | 7 | 45 | 6 | 1 | 0 | 1 | 60 32 */28 | 60 | 0 | 63 |
| Treatment: 24 h treatment and 0 h recovery (−S9 mix) | |||||||||||
| PDNS | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 0 | 100 |
| 92.5 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 83 | |
| 185 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 66 | |
| 370 | 0 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | 0 | 55 | |
| MMC | 0.05 | 9 | 41 | 3 | 0 | 0 | 0 | 53 25 */28 | 53 | 0 | 83 |
| Drug | Dose (mg/kg/d) | Mortality (Dead/Total) | MNPCE/4000 PCEs (%, Mean ± S.D.) | PCE/(PCE + NCE) (%, Mean ± S.D.) |
|---|---|---|---|---|
| PNF | 0 | 0/5 | 0.07 ± 0.03 | 50.44 ± 0.91 |
| 500 | 0/5 | 0.06 ± 0.04 | 50.68 ± 0.43 | |
| 1000 | 0/5 | 0.03 ± 0.03 | 50.87 ± 0.36 | |
| 2000 | 0/5 | 0.02 ± 0.03 | 50.84 ± 0.43 | |
| CPA | 70 | 0/5 | 6.45 ± 0.31 * | 46.91 ± 0.72 * |
| Drug | Dose (mg/kg/d) | Mortality (Dead/Total) | MNPCE/4000 PCEs (%, Mean ± S.D.) | PCE/(PCE + NCE) (%, Mean ± S.D.) |
|---|---|---|---|---|
| EDNF | 0 | 0/5 | 0.05 ± 0.04 | 49.97 ± 0.67 |
| 500 | 0/5 | 0.05 ± 0.04 | 50.38 ± 1.07 | |
| 1000 | 0/5 | 0.04 ± 0.03 | 50.67 ± 0.59 | |
| 2000 | 0/5 | 0.04 ± 0.03 | 51.00 ± 0.56 | |
| CPA | 70 | 0/5 | 6.79 ± 0.27 * | 46.14 ± 0.58 * |
| Drug | Dose (mg/kg/d) | Mortality (Dead/Total) | MNPCE/4000 PCEs (%, Mean ± S.D.) | PCE/(PCE + NCE) (%, Mean ± S.D.) |
|---|---|---|---|---|
| PDNF | 0 | 0/5 | 0.04 ± 0.05 | 51.37 ± 0.71 |
| 500 | 0/5 | 0.07 ± 0.04 | 51.18 ± 0.61 | |
| 1000 | 0/5 | 0.06 ± 0.02 | 51.40 ± 0.28 | |
| 2000 | 0/5 | 0.03 ± 0.03 | 50.94 ± 0.36 | |
| CPA | 70 | 0/5 | 6.47 ± 0.28 * | 47.07 ± 0.99 * |
| Drug | Dose (mg/kg/d) | Mortality (Dead/Total) | MNPCE/4000 PCEs (%, Mean ± S.D.) | PCE/(PCE + NCE) (%, Mean ± S.D.) |
|---|---|---|---|---|
| PDNS | 0 | 0/5 | 0.06 ± 0.04 | 50.62 ± 0.41 |
| 500 | 0/5 | 0.05 ± 0.05 | 50.45 ± 1.27 | |
| 1000 | 0/5 | 0.06 ± 0.03 | 51.22 ± 0.45 | |
| 2000 | 0/5 | 0.05 ± 0.03 | 50.78 ± 0.65 | |
| CPA | 70 | 0/5 | 6.81 ± 0.26 * | 46.18 ± 1.26 * |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Shin, S.; Kim, J.S.; Park, M.K.; Bang, O.-S. Genotoxicity Comparison between Morinda citrifolia Fruit and Seed Substances. Foods 2022, 11, 1773. https://doi.org/10.3390/foods11121773
Shin S, Kim JS, Park MK, Bang O-S. Genotoxicity Comparison between Morinda citrifolia Fruit and Seed Substances. Foods. 2022; 11(12):1773. https://doi.org/10.3390/foods11121773
Chicago/Turabian StyleShin, Sarah, Ji Soo Kim, Myung Ku Park, and Ok-Sun Bang. 2022. "Genotoxicity Comparison between Morinda citrifolia Fruit and Seed Substances" Foods 11, no. 12: 1773. https://doi.org/10.3390/foods11121773
APA StyleShin, S., Kim, J. S., Park, M. K., & Bang, O.-S. (2022). Genotoxicity Comparison between Morinda citrifolia Fruit and Seed Substances. Foods, 11(12), 1773. https://doi.org/10.3390/foods11121773






