NGS Techniques Reveal a High Diversity of RNA Viral Pathogens and Papillomaviruses in Fresh Produce and Irrigation Water
Abstract
1. Introduction
2. Materials and Methods
2.1. Organic Food and Water Samples
2.2. Viral Concentration and Nucleic Acid Extraction
2.3. Viral Quantification
LOD Determination
2.4. Target Enrichment Sequencing (TES)
2.4.1. Sequence-Independent, Single-Primer Amplification (SISPA)
2.4.2. Library Construction
2.4.3. Capture of Viral Sequences by VirCapSeq-VERT Capture Panel
2.4.4. TES Bioinformatic Processing
2.5. Amplicon Deep Sequencing (ADS)
2.5.1. Amplicon Generation
2.5.2. ADS Bioinformatic Processing
3. Results
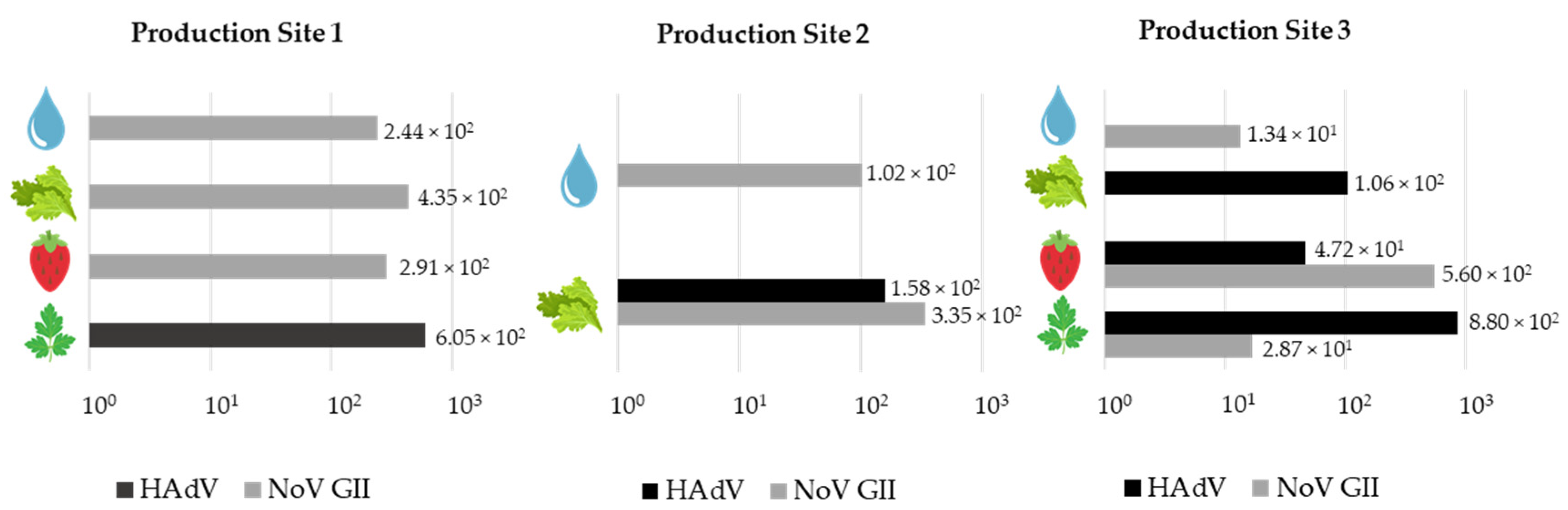
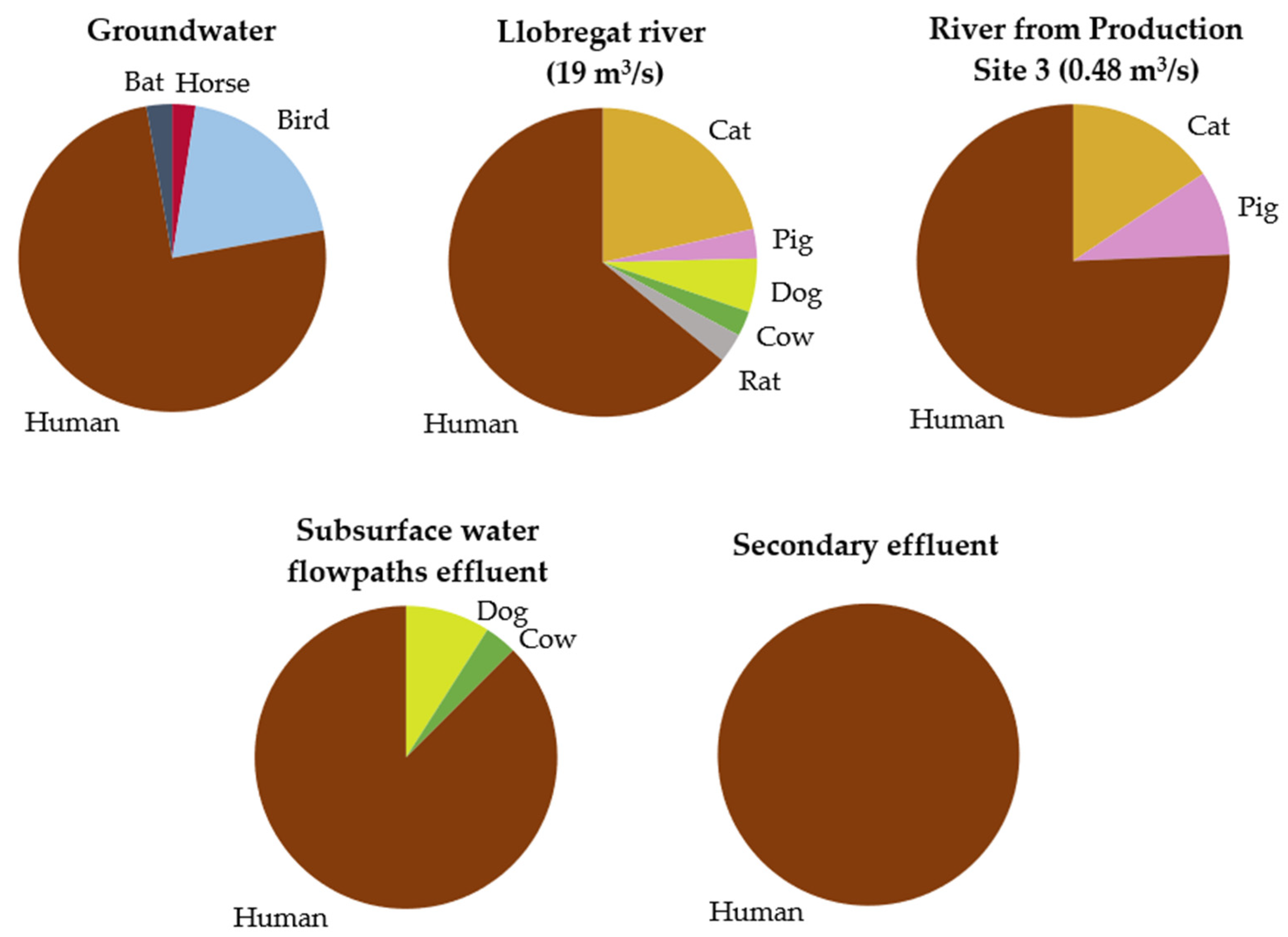
3.1. Virus Quantification in Irrigation Water and Organic Food
3.2. Virome of Irrigation Water and Organic Food Using TES
3.3. Diversity of NoV and HPV Sequencing in Irrigation Water and Organic Food Using ADS
4. Discussion
5. Conclusions
- The fresh fruits and vegetables cultured in the analyzed organic farms show a high frequency of viral contamination, and the contaminating viruses are also detected in river water and tertiary effluents from subsurface water flow paths used in irrigation, indicating that they are common circulating pathogens.
- In this study, irrigation water is the most probable source of the viral pathogens, primarily NoV and HPV, detected in food. All pathogens were detected in some types of irrigation water, such as river water or treated wastewater, indicating that are potential sources of contamination. However, virus infectivity potential was not analyzed in this study.
- A wide diversity of cutaneous HPV was detected in fresh produce and a wider diversity of HPV was identified in more polluted water samples, such as river and treated wastewater samples. HPV-8, a high-risk type associated with SCC, was found in treated wastewater.
- The three methodologies used for the analysis of viral contamination of irrigation water and organic food are useful and produce different types of information: (a) qPCR is a highly sensitive quantitative and specific technique, (b) TES shows the presence of relatively abundant viral pathogens present in irrigation water, including unexpected viral pathogens and potentially zoonotic strains, and (c) ADS provides higher sensitivity for the identification of viral types or variants in viral groups that contaminate food and water.
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Hess, T.; Sutcliffe, C. The Exposure of a Fresh Fruit and Vegetable Supply Chain to Global Water-Related Risks. Water Int. 2018, 43, 746–761. [Google Scholar] [CrossRef]
- Balali, G.I.; Yar, D.D.; Afua Dela, V.G.; Adjei-Kusi, P. Microbial Contamination, an Increasing Threat to the Consumption of Fresh Fruits and Vegetables in Today’s World. Int. J. Microbiol. 2020, 2020, 3029295. [Google Scholar] [CrossRef]
- Septembre-Malaterre, A.; Remize, F.; Poucheret, P. Fruits and Vegetables, as a Source of Nutritional Compounds and Phytochemicals: Changes in Bioactive Compounds during Lactic Fermentation. Food Res. Int. 2018, 104, 86–99. [Google Scholar] [CrossRef] [PubMed]
- Mir, S.A.; Shah, M.A.; Mir, M.M.; Dar, B.N.; Greiner, R.; Roohinejad, S. Microbiological Contamination of Ready-to-Eat Vegetable Salads in Developing Countries and Potential Solutions in the Supply Chain to Control Microbial Pathogens. Food Control 2018, 85, 235–244. [Google Scholar] [CrossRef]
- Fernandez-Cassi, X.; Timoneda, N.; Gonzales-Gustavson, E.; Abril, J.F.; Bofill-Mas, S.; Girones, R. A Metagenomic Assessment of Viral Contamination on Fresh Parsley Plants Irrigated with Fecally Tainted River Water. Int. J. Food Microbiol. 2017, 257, 80–90. [Google Scholar] [CrossRef] [PubMed]
- Callejón, R.M.; Rodríguez-Naranjo, M.I.; Ubeda, C.; Hornedo-Ortega, R.; Garcia-Parrilla, M.C.; Troncoso, A.M. Reported Foodborne Outbreaks Due to Fresh Produce in the United States and European Union: Trends and Causes. Foodborne Pathog. Dis. 2015, 12, 32–38. [Google Scholar] [CrossRef]
- Shaheen, M.N.F.; Elmahdy, E.M.; Chawla-Sarkar, M. Quantitative PCR-Based Identification of Enteric Viruses Contaminating Fresh Produce and Surface Water Used for Irrigation in Egypt. Environ. Sci. Pollut. Res. 2019, 26, 21619–21628. [Google Scholar] [CrossRef]
- Iwu, C.D.; Okoh, A.I. Preharvest Transmission Routes of Fresh Produce Associated Bacterial Pathogens with Outbreak Potentials: A Review. Int. J. Environ. Res. Public Health 2019, 16, 4407. [Google Scholar] [CrossRef]
- Garcia, B.C.B.; Dimasupil, M.A.A.Z.; Vital, P.G.; Widmer, K.W.; Rivera, W.L. Fecal Contamination in Irrigation Water and Microbial Quality of Vegetable Primary Production in Urban Farms of Metro Manila, Philippines. J. Environ. Sci. Health 2015, 50, 734–743. [Google Scholar] [CrossRef]
- Park, S.; Szonyi, B.; Gautam, R.; Nightingale, K.; Anciso, J.; Ivanek, R. Risk Factors for Microbial Contamination in Fruits and Vegetables at the Preharvest Level: A Systematic Review. J. Food Prot. 2012, 75, 2055–2081. [Google Scholar] [CrossRef]
- Wei, X.; Hou, S.; Pan, X.; Xu, C.; Li, J.; Yu, H.; Chase, J.; Atwill, E.R.; Li, X.; Chen, K.; et al. Microbiological Contamination of Strawberries from U-Pick Farms in Guangzhou, China. Int. J. Environ. Res. Public Health 2019, 16, 4910. [Google Scholar] [CrossRef]
- Rodrigues, C.; da Silva, A.L.B.R.; Dunn, L.L. Factors Impacting the Prevalence of Foodborne Pathogens in Agricultural Water Sources in the Southeastern United States. Water 2020, 12, 51. [Google Scholar] [CrossRef]
- Gil, M.I.; Selma, M.V.; Suslow, T.; Jacxsens, L.; Uyttendaele, M.; Allende, A. Pre- and Postharvest Preventive Measures and Intervention Strategies to Control Microbial Food Safety Hazards of Fresh Leafy Vegetables. Crit. Rev. Food Sci. Nutr. 2015, 55, 453–468. [Google Scholar] [CrossRef] [PubMed]
- Pachepsky, Y.; Shelton, D.R.; McLain, J.E.T.; Patel, J.; Mandrell, R.E. Irrigation Waters as a Source of Pathogenic Microorganisms in Produce. A Review. Adv. Agron. 2011, 113, 73–138. [Google Scholar] [CrossRef]
- Machado-Moreira, B.; Richards, K.; Brennan, F.; Abram, F.; Burgess, C.M. Microbial Contamination of Fresh Produce: What, Where, and How? Compr. Rev. Food Sci. Food Saf. 2019, 18, 1727–1750. [Google Scholar] [CrossRef]
- Gobeil, A.; Maherani, B.; Lacroix, M. Norovirus Elimination on the Surface of Fresh Foods. Crit. Rev. Food Sci. Nutr. 2020. [Google Scholar] [CrossRef]
- Gonzales-Gustavson, E.; Rusiñol, M.; Medema, G.; Calvo, M.; Girones, R. Quantitative Risk Assessment of Norovirus and Adenovirus for the Use of Reclaimed Water to Irrigate Lettuce in Catalonia. Water Res. 2019, 153, 91–99. [Google Scholar] [CrossRef] [PubMed]
- Dicaprio, E.; Purgianto, A.; Li, J. Effects of Abiotic and Biotic Stresses on the Internalization and Dissemination of Human Norovirus Surrogates in Growing Romaine. Appl. Environ. Microbiol. 2015, 81, 4791–4800. [Google Scholar] [CrossRef] [PubMed]
- Koo, H.L.; Ajami, N.; Atmar, R.L.; DuPont, H.L. Noroviruses: The Leading Cause of Gastroenteritis Worldwide. Discov. Med. 2010, 10, 61–70. [Google Scholar]
- Newell, D.G.; Koopmans, M.; Verhoef, L.; Duizer, E.; Aidara-Kane, A.; Sprong, H.; Opsteegh, M.; Langelaar, M.; Threfall, J.; Scheutz, F.; et al. Food-Borne Diseases—The Challenges of 20 Years Ago Still Persist While New Ones Continue to Emerge. Int. J. Food Microbiol. 2010, 139, S3–S15. [Google Scholar] [CrossRef]
- Martínez-Puchol, S.; Rusiñol, M.; Fernández-Cassi, X.; Timoneda, N.; Itarte, M.; Andrés, C.; Antón, A.; Abril, J.F.; Girones, R.; Bofill-Mas, S. Characterisation of the Sewage Virome: Comparison of NGS Tools and Occurrence of Significant Pathogens. Sci. Total Environ. 2020, 713, 136604. [Google Scholar] [CrossRef]
- Rusiñol, M.; Martínez-Puchol, S.; Timoneda, N.; Fernández-Cassi, X.; Pérez-Cataluña, A.; Fernández-Bravo, A.; Moreno-Mesonero, L.; Moreno, Y.; Alonso, J.L.; Figueras, M.J.; et al. Metagenomic Analysis of Viruses, Bacteria and Protozoa in Irrigation Water. Int. J. Hyg. Environ. Health 2020, 224, 113440. [Google Scholar] [CrossRef] [PubMed]
- Iaconelli, M.; Petricca, S.; Della Libera, S.; Di Bonito, P.; La Rosa, G. First Detection of Human Papillomaviruses and Human Polyomaviruses in River Waters in Italy. Food Environ. Virol. 2015, 7, 309–315. [Google Scholar] [CrossRef]
- La Rosa, G.; Fratini, M.; Accardi, L.; D’Oro, G.; Della Libera, S.; Muscillo, M.; Di Bonito, P. Mucosal and Cutaneous Human Papillomaviruses Detected in Raw Sewages. PLoS ONE 2013, 8, e52391. [Google Scholar] [CrossRef]
- Di Bonito, P.; Della Libera, S.; Petricca, S.; Iaconelli, M.; Sanguinetti, M.; Graffeo, R.; Accardi, L.; La Rosa, G. A Large Spectrum of Alpha and Beta Papillomaviruses Are Detected in Human Stool Samples. J. Gen. Virol. 2015, 96, 607–613. [Google Scholar] [CrossRef] [PubMed]
- Di Cola, G.; Fantilli, A.C.; Pisano, M.B.; Ré, V.E. Foodborne Transmission of Hepatitis A and Hepatitis E Viruses: A Literature Review. Int. J. Food Microbiol. 2021, 338, 108986. [Google Scholar] [CrossRef] [PubMed]
- EFSA BIOHAZ Panel. Scientific Opinion on the Guidance on the Requirements for the Development of Microbiological Criteria. EFSA J. 2017, 15, 5052. [Google Scholar] [CrossRef]
- EU C163. Guidance Document on Addressing Microbiological Risks in Fresh Fruits and Vegetables at Primary Production through Good Hygiene. Off. J. Eur. Union. 2017, 163, 1–40. [Google Scholar]
- Rusiñol, M.; Hundesa, A.; Cárdenas-Youngs, Y.; Fernández-Bravo, A.; Pérez-Cataluña, A.; Moreno-Mesonero, L.; Moreno, Y.; Calvo, M.; Alonso, J.L.; Figueras, M.J.; et al. Microbiological Contamination of Conventional and Reclaimed Irrigation Water: Evaluation and Management Measures. Sci. Total Environ. 2020, 710, 136298. [Google Scholar] [CrossRef] [PubMed]
- Girones, R.; Ferrús, M.A.; Alonso, J.L.; Rodriguez-Manzano, J.; Calgua, B.; de Abreu Corrêa, A.; Hundesa, A.; Carratala, A.; Bofill-Mas, S. Molecular Detection of Pathogens in Water—The Pros and Cons of Molecular Techniques. Water Res. 2010, 44, 4325–4339. [Google Scholar] [CrossRef]
- Gerba, C.P.; Goyal, S.M.; LaBelle, R.L.; Bodgan, G.F. Failure of Indicator Bacteria to Reflect the Occurrence of Enteroviruses in Marine Waters. Am. J. Public Health 1979, 69, 1116–1119. [Google Scholar] [CrossRef]
- Pusch, D.; Oh, D.Y.; Wolf, S.; Dumke, R.; Schröter-Bobsin, U.; Höhne, M.; Röske, I.; Schreier, E. Detection of Enteric Viruses and Bacterial Indicators in German Environmental Waters. Arch. Virol. 2005, 150, 929–947. [Google Scholar] [CrossRef] [PubMed]
- Savichtcheva, O.; Okabe, S. Alternative Indicators of Fecal Pollution: Relations with Pathogens and Conventional Indicators, Current Methodologies for Direct Pathogen Monitoring and Future Application Perspectives. Water Res. 2006, 40, 2463–2476. [Google Scholar] [CrossRef] [PubMed]
- Allard, A.; Vantarakis, A. Adenoviruses. Glob. Water Pathog. Proj. 2017. [Google Scholar] [CrossRef]
- Verani, M.; Federigi, I.; Donzelli, G.; Cioni, L.; Carducci, A. Human Adenoviruses as Waterborne Index Pathogens and Their Use for Quantitative Microbial Risk Assessment. Sci. Total Environ. 2019, 651, 1469–1475. [Google Scholar] [CrossRef] [PubMed]
- Hewitt, J.; Greening, G.E.; Leonard, M.; Lewis, G.D. Evaluation of Human Adenovirus and Human Polyomavirus as Indicators of Human Sewage Contamination in the Aquatic Environment. Water Res. 2013, 47, 6750–6761. [Google Scholar] [CrossRef]
- Albinana-Gimenez, N.; Miagostovich, M.P.; Calgua, B.; Huguet, J.M.; Matia, L.; Girones, R. Analysis of Adenoviruses and Polyomaviruses Quantified by QPCR as Indicators of Water Quality in Source and Drinking-Water Treatment Plants. Water Res. 2009, 43, 2011–2019. [Google Scholar] [CrossRef]
- International Organization for Standardization. ISO 15216-1. Microbiology of the Food Chain—Horizontal Method for Determination of Hepatitis A Virus and Norovirus in Food Using Real-Time RT-PCR—Part 1: Method for Quantification. Available online: https://www.iso.org/standard/65681.html (accessed on 8 April 2021).
- Bartsch, C.; Höper, D.; Mäde, D.; Johne, R. Analysis of Frozen Strawberries Involved in a Large Norovirus Gastroenteritis Outbreak Using Next Generation Sequencing and Digital PCR. J. Food Microbiol. 2018, 76, 390–395. [Google Scholar] [CrossRef] [PubMed]
- Mäde, D.; Trübner, K.; Neubert, E.; Höhne, M.; Johne, R. Detection and Typing of Norovirus from Frozen Strawberries Involved in a Large-Scale Gastroenteritis Outbreak in Germany. Food Environ. Virol. 2013, 5, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Schrader, C.; Schielke, A.; Ellerbroek, L.; Johne, R. PCR Inhibitors—Occurrence, Properties and Removal. J. Appl. Microbiol. 2012, 113, 1014–1026. [Google Scholar] [CrossRef]
- Scherer, K.; Johne, R.; Schrader, C.; Ellerbroek, L.; Schulenburg, J.; Klein, G. Comparison of Two Extraction Methods for Viruses in Food and Application in a Norovirus Gastroenteritis Outbreak. J. Virol. Methods 2010, 169, 22–27. [Google Scholar] [CrossRef]
- Aw, T.G.; Wengert, S.; Rose, J.B. Metagenomic Analysis of Viruses Associated with Field-Grown and Retail Lettuce Identifies Human and Animal Viruses. Int. J. Food Microbiol. 2016, 223, 50–56. [Google Scholar] [CrossRef] [PubMed]
- Park, E.J.; Kim, K.H.; Abell GC, J.; Kim, M.S.; Roh, S.W.; Bae, J.W. Metagenomic Analysis of the Viral Communities in Fermented Foods. Appl. Environ. Microbiol. 2011, 77, 1284–1291. [Google Scholar] [CrossRef] [PubMed]
- Zhang, W.; Li, L.; Deng, X.; Kapusinszky, B.; Delwart, E. What Is for Dinner? Viral Metagenomics of US Store Bought Beef, Pork, and Chicken. Virology 2014, 468–470, 303–310. [Google Scholar] [CrossRef]
- Nieuwenhuijse, D.F.; Koopmans, M.P.G. Metagenomic Sequencing for Surveillance of Food- and Waterborne Viral Diseases. Front. Microbiol. 2017, 8, 230. [Google Scholar] [CrossRef]
- Aarestrup, F.M.; Brown, E.W.; Detter, C.; Gerner-Smidt, P.; Gilmour, M.W.; Harmsen, D.; Hendriksen, R.S.; Hewson, R.; Heymann, D.L.; Johansson, K.; et al. Integrating Genome-Based Informatics to Modernize Global Disease Monitoring, Information Sharing, and Response. Emerg. Infect. Dis. 2012, 18. [Google Scholar] [CrossRef]
- Desdouits, M.; Wacrenier, C.; Ollivier, J.; Schaeffer, J.; Le Guyader, F.S. A Targeted Metagenomics Approach to Study the Diversity of Norovirus GII in Shellfish Implicated in Outbreaks. Viruses 2020, 12, 978. [Google Scholar] [CrossRef] [PubMed]
- Filipa-Silva, A.; Parreira, R.; Martínez-Puchol, S.; Bofill-Mas, S.; Barreto Crespo, M.T.; Nunes, M. The Unexplored Virome of Two Atlantic Coast Fish: Contribution of Next-Generation Sequencing to Fish Virology. Foods 2020, 9, 1634. [Google Scholar] [CrossRef] [PubMed]
- Strubbia, S.; Schaeffer, J.; Besnard, A.; Wacrenier, C.; Le Mennec, C.; Garry, P.; Desdouits, M.; Le Guyader, F.S. Metagenomic to Evaluate Norovirus Genomic Diversity in Oysters: Impact on Hexamer Selection and Targeted Capture-Based Enrichment. Int. J. Food Microbiol. 2020, 323, 108588. [Google Scholar] [CrossRef]
- Rosani, U.; Shapiro, M.; Venier, P.; Allam, B. A Needle in a Haystack: Tracing Bivalve-Associated Viruses in High-Throughput Transcriptomic Data. Viruses 2019, 11, 205. [Google Scholar] [CrossRef]
- Oshiki, M.; Miura, T.; Kazama, S.; Segawa, T.; Ishii, S.; Hatamoto, M.; Yamaguchi, T.; Kubota, K.; Iguchi, A.; Tagawa, T.; et al. Microfluidic PCR Amplification and MiSeq Amplicon Sequencing Techniques for High-Throughput Detection and Genotyping of Human Pathogenic RNA Viruses in Human Feces, Sewage, and Oysters. Front. Microbiol. 2018, 9, 830. [Google Scholar] [CrossRef]
- Imamura, S.; Kanezashi, H.; Goshima, T.; Haruna, M.; Okada, T.; Inagaki, N.; Uema, M.; Noda, M.; Akimoto, K. Next-Generation Sequencing Analysis of the Diversity of Human Noroviruses in Japanese Oysters. Foodborne Pathog. Dis. 2017, 14, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Chiapponi, C.; Pavoni, E.; Bertasi, B.; Baioni, L.; Scaltriti, E.; Chiesa, E.; Cianti, L.; Losio, M.N.; Pongolini, S. Isolation and Genomic Sequence of Hepatitis A Virus from Mixed Frozen Berries in Italy. Food Environ. Virol. 2014, 6, 202–206. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Yang, Z.; Mammel, M.; Papafragkou, E.; Hida, K.; Elkins, C.A.; Kulka, M. Application of Next Generation Sequencing toward Sensitive Detection of Enteric Viruses Isolated from Celery Samples as an Example of Produce. Int. J. Food Microbiol. 2017, 261, 73–81. [Google Scholar] [CrossRef] [PubMed]
- Toscano, A.; Marzo, A.; Milani, M.; Cirelli, G.L.; Barbagallo, S. Comparison of Removal Efficiencies in Mediterranean Pilot Constructed Wetlands Vegetated with Different Plant Species. Ecol. Eng. 2015, 75, 155–160. [Google Scholar] [CrossRef]
- Ribot, M.; Bernal, S.; Nikolakopoulou, M.; Vaessen, T.N.; Cochero, J.; Gacia, E.; Sorolla, A.; Argerich, A.; Sabater, F.; Isnard, M.; et al. Enhancement of Carbon and Nitrogen Removal by Helophytes along Subsurface Water Flowpaths Receiving Treated Wastewater. Sci. Total Environ. 2017, 599–600, 1667–1676. [Google Scholar] [CrossRef]
- Bofill-Mas, S.; Albinana-Gimenez, N.; Clemente-Casares, P.; Hundesa, A.; Rodriguez-Manzano, J.; Allard, A.; Calvo, M.; Girones, R. Quantification and Stability of Human Adenoviruses and Polyomavirus JCPyV in Wastewater Matrices. Appl. Environ. Microbiol. 2006, 72, 7894–7896. [Google Scholar] [CrossRef]
- Da Silva, A.K.; Le Saux, J.C.; Parnaudeau, S.; Pommepuy, M.; Elimelech, M.; Le Guyader, F.S. Evaluation of Removal of Noroviruses during Wastewater Treatment, Using Real-Time Reverse Transcription-PCR: Different Behaviors of Genogroups I and II. Appl. Environ. Microbiol. 2007, 73, 7891–7897. [Google Scholar] [CrossRef] [PubMed]
- Svraka, S.; Duizer, E.; Vennema, H.; De Bruin, E.; Van Der Veer, B.; Dorresteijn, B.; Koopmans, M. Etiological Role of Viruses in Outbreaks of Acute Gastroenteritis in The Netherlands from 1994 through 2005. J. Clin. Microbiol. 2007, 45, 1389–1394. [Google Scholar] [CrossRef]
- Hoehne, M.; Schreier, E. Detection of Norovirus Genogroup I and II by Multiplex Real-Time RT-PCR Using a 3′-Minor Groove Binder-DNA Probe. BMC Infect. Dis. 2006, 6, 69. [Google Scholar] [CrossRef] [PubMed]
- Loisy, F.; Atmar, R.L.; Guillon, P.; Le Cann, P.; Pommepuy, M.; Le Guyader, F.S. Real-Time RT-PCR for Norovirus Screening in Shellfish. J. Virol. Methods 2005, 123, 1–7. [Google Scholar] [CrossRef]
- Kageyama, T.; Kojima, S.; Shinohara, M.; Uchida, K.; Fukushi, S.; Hoshino, F.B.; Takeda, N.; Katayama, K. Broadly Reactive and Highly Sensitive Assay for Norwalk-like Viruses Based on Real-Time Quantitative Reverse Transcription-PCR. J. Clin. Microbiol. 2003, 41, 1548–1557. [Google Scholar] [CrossRef]
- Jothikumar, N.; Cromeans, T.L.; Robertson, B.H.; Meng, X.J.; Hill, V.R. A Broadly Reactive One-Step Real-Time RT-PCR Assay for Rapid and Sensitive Detection of Hepatitis E Virus. J. Virol. Methods 2006, 131, 65–71. [Google Scholar] [CrossRef]
- Fernandez-Cassi, X.; Timoneda, N.; Martínez-Puchol, S.; Rusiñol, M.; Rodriguez-Manzano, J.; Figuerola, N.; Bofill-Mas, S.; Abril, J.F.; Girones, R. Metagenomics for the Study of Viruses in Urban Sewage as a Tool for Public Health Surveillance. Sci. Total. Environ. 2018, 618, 870–880. [Google Scholar] [CrossRef]
- Fernandez-Cassi, X.; Rusiñol, M.; Martínez-Puchol, S. Viral Concentration and Amplification from Human Serum Samples Prior to Application of Next-Generation Sequencing Analysis. Methods Mol. Biol. 2018, 1838, 173–188. [Google Scholar] [CrossRef] [PubMed]
- Hjelmsø, M.H.; Mollerup, S.; Jensen, R.H.; Pietroni, C.; Lukjancenko, O.; Schultz, A.C.; Aarestrup, F.M.; Hansen, A.J. Metagenomic Analysis of Viruses in Toilet Waste from Long Distance Flights—A New Procedure for Global Infectious Disease Surveillance. PLoS ONE 2019, 14, e0210368. [Google Scholar] [CrossRef]
- Briese, T.; Kapoor, A.; Mishra, N.; Jain, K.; Kumar, A.; Jabado, O.J.; Ian Lipkina, W. Virome Capture Sequencing Enables Sensitive Viral Diagnosis and Comprehensive Virome Analysis. MBio 2015, 6, e01491-15. [Google Scholar] [CrossRef] [PubMed]
- Vilsker, M.; Moosa, Y.; Nooij, S.; Fonseca, V.; Ghysens, Y.; Dumon, K.; Pauwels, R.; Alcantara, L.C.; Vanden Eynden, E.; Vandamme, A.-M.; et al. Genome Detective: An Automated System for Virus Identification from High-Throughput Sequencing Data. Bioinformatics 2019, 35, 871–873. [Google Scholar] [CrossRef] [PubMed]
- Benson, D.A.; Clark, K.; Karsch-Mizrachi, I.; Lipman, D.J.; Ostell, J.; Sayers, E.W. GenBank. Nucleic Acids Res. 2015, 43, D30–D35. [Google Scholar] [CrossRef]
- Altschul, S.F.; Gish, W.; Miller, W.; Myers, E.W.; Lipman, D.J. Basic Local Alignment Search Tool. J. Mol. Biol. 1990, 215, 403–410. [Google Scholar] [CrossRef]
- Kearse, M.; Moir, R.; Wilson, A.; Stones-Havas, S.; Cheung, M.; Sturrock, S.; Buxton, S.; Cooper, A.; Markowitz, S.; Duran, C.; et al. Geneious Basic: An Integrated and Extendable Desktop Software Platform for the Organization and Analysis of Sequence Data. Bioinformatics 2012, 28, 1647–1649. [Google Scholar] [CrossRef]
- Chhabra, P.; de Graaf, M.; Parra, G.I.; Chan, M.C.W.; Green, K.; Martella, V.; Wang, Q.; White, P.A.; Katayama, K.; Vennema, H.; et al. Updated Classification of Norovirus Genogroups and Genotypes. J. Gen. Virol. 2019, 100, 1393–1406. [Google Scholar] [CrossRef]
- Chhabra, P.; de Graaf, M.; Parra, G.I.; Chan, M.C.W.; Green, K.; Martella, V.; Wang, Q.; White, P.A.; Katayama, K.; Vennema, H.; et al. Corrigendum: Updated Classification of Norovirus Genogroups and Genotypes. J. Gen. Virol. 2020, 101, 893. [Google Scholar] [CrossRef]
- Kroneman, A.; Vennema, H.; Deforche, K.; Avoort, H.; Peñaranda, S.; Oberste, M.S.; Vinjé, J.; Koopmans, M. An Automated Genotyping Tool for Enteroviruses and Noroviruses. J. Clin. Virol. 2011, 51, 121–125. [Google Scholar] [CrossRef]
- Kitajima, M.; Oka, T.; Haramoto, E.; Takeda, N.; Katayama, K.; Katayama, H. Seasonal Distribution and Genetic Diversity of Genogroups I, II, and IV Noroviruses in the Tamagawa River, Japan. Environ. Sci. Technol. 2010, 44, 7116–7122. [Google Scholar] [CrossRef]
- Aw, T.G.; Gin, K.Y.H.; Oon, L.L.E.; Chen, E.X.; Woo, C.H. Prevalence and Genotypes of Human Noroviruses in Tropical Urban Surface Waters and Clinical Samples in Singapore. Appl. Environ. Microbiol. 2009, 75, 4984–4992. [Google Scholar] [CrossRef]
- Forslund, O.; Ly, H.; Higgins, G. Improved Detection of Cutaneous Human Papillomavirus DNA by Single Tube Nested “hanging Droplet” PCR. J. Virol. Methods 2003, 110, 129–136. [Google Scholar] [CrossRef]
- De Roda Husman, A.M.; Walboomers, J.M.M.; Van den Brule, A.J.C.; Meijer, C.J.L.M.; Snijders, P.J.F. The Use of General Primers GP5 and GP6 Elongated at Their 3′ Ends with Adjacent Highly Conserved Sequences Improves Human Papillomavirus Detection by PCR. J. Gen. Virol. 1995, 76, 1057–1062. [Google Scholar] [CrossRef] [PubMed]
- Bofill-Mas, S.; Rusiñol, M.; Fernandez-Cassi, X.; Carratalà, A.; Hundesa, A.; Girones, R. Quantification of Human and Animal Viruses to Differentiate the Origin of the Fecal Contamination Present in Environmental Samples. Biomed. Res. Int. 2013, 2013. [Google Scholar] [CrossRef] [PubMed]
- Rusiñol, M.; Fernandez-Cassi, X.; Hundesa, A.; Vieira, C.; Kern, A.; Eriksson, I.; Ziros, P.; Kay, D.; Miagostovich, M.; Vargha, M.; et al. Application of Human and Animal Viral Microbial Source Tracking Tools in Fresh and Marine Waters from Five Different Geographical Areas. Water Res. 2014, 59, 119–129. [Google Scholar] [CrossRef]
- Rusiñol, M.; Girones, R. Summary of Excreted and Waterborne Viruses. Glob. Water Pathog. Proj. 2017. [Google Scholar] [CrossRef]
- Vieira, C.B.; de Abreu Corrêa, A.; de Jesus, M.S.; Luz, S.L.B.; Wyn-Jones, P.; Kay, D.; Vargha, M.; Miagostovich, M.P. Viruses Surveillance Under Different Season Scenarios of the Negro River Basin, Amazonia, Brazil. Food Environ. Virol. 2016, 8, 57–69. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, P.; Kozyra, I.; Lazic, S.; Bouwknegt, M.; Rutjes, S.; Willems, K.; Moloney, R.; de Roda Husman, A.M.; Kaupke, A.; Legaki, E.; et al. Harmonised Investigation of the Occurrence of Human Enteric Viruses in the Leafy Green Vegetable Supply Chain in Three European Countries. Food Environ. Virol. 2012, 4, 179–191. [Google Scholar] [CrossRef]
- Maunula, L.; Kaupke, A.; Vasickova, P.; Söderberg, K.; Kozyra, I.; Lazic, S.; van der Poel, W.H.M.; Bouwknegt, M.; Rutjes, S.; Willems, K.A.; et al. Tracing Enteric Viruses in the European Berry Fruit Supply Chain. Int. J. Food Microbiol. 2013, 167, 177–185. [Google Scholar] [CrossRef] [PubMed]
- Brassard, J.; Gagné, M.; Généreux, M.; Côté, C. Detection of Human Food-Borne and Zoonotic Viruses on Irrigated, Field-Grown Strawberries. Appl. Environ. Microbiol. 2012, 78, 3763–3766. [Google Scholar] [CrossRef] [PubMed]
- Baert, L.; Mattison, K.; Loisy-Hamon, F.; Harlow, J.; Martyres, A.; Lebeau, B.; Stals, A.; Van Coillie, E.; Herman, L.; Uyttendaele, M. Review: Norovirus Prevalence in Belgian, Canadian and French Fresh Produce: A Threat to Human Health? Int. J. Food Microbiol. 2011, 151, 261–269. [Google Scholar] [CrossRef]
- Cantalupo, P.G.; Calgua, B.; Zhao, G.; Hundesa, A.; Wier, A.D.; Katz, J.P.; Grabe, M.; Hendrix, R.W.; Girones, R.; Wang, D.; et al. Raw Sewage Harbors Diverse Viral Populations. MBio 2011, 2, e00180. [Google Scholar] [CrossRef]
- De Graaf, M.; Van Beek, J.; Vennema, H.; Podkolzin, A.T.; Hewitt, J.; Bucardo, F.; Templeton, K.; Mans, J.; Nordgren, J.; Reuter, G.; et al. Emergence of a Novel GII.17 Norovirus—End of the GII.4 Era? Eurosurveillance 2015, 20, 21178. [Google Scholar] [CrossRef]
- Le Guyader, F.S.; Mittelholzer, C.; Haugarreau, L.; Hedlund, K.O.; Alsterlund, R.; Pommepuy, M.; Svensson, L. Detection of Noroviruses in Raspberries Associated with a Gastroenteritis Outbreak. Int. J. Food Microbiol. 2004, 97, 179–186. [Google Scholar] [CrossRef]
- Ogorzaly, L.; Walczak, C.; Galloux, M.; Etienne, S.; Gassilloud, B.; Cauchie, H.M. Human Adenovirus Diversity in Water Samples Using a Next-Generation Amplicon Sequencing Approach. Food Environ. Virol. 2015, 7, 112–121. [Google Scholar] [CrossRef]
- Hamza, H.; Hamza, I.A. Oncogenic Papillomavirus and Polyomavirus in Urban Sewage in Egypt. Sci. Total Environ. 2018, 610–611, 1413–1420. [Google Scholar] [CrossRef]
- La Rosa, G.; Della Libera, S.; Petricca, S.; Iaconelli, M.; Briancesco, R.; Paradiso, R.; Semproni, M.; di Bonito, P.; Bonadonna, L. First Detection of Papillomaviruses and Polyomaviruses in Swimming Pool Waters: Unrecognized Recreational Water-Related Pathogens? J. Appl. Microbiol. 2015, 119, 1683–1691. [Google Scholar] [CrossRef]
- Houde, A.; Leblanc, D.; Poitras, E.; Ward, P.; Brassard, J.; Simard, C.; Trottier, Y.L. Comparative Evaluation of RT-PCR, Nucleic Acid Sequence-Based Amplification (NASBA) and Real-Time RT-PCR for Detection of Noroviruses in Fecal Material. J. Virol. Methods 2006, 135, 163–172. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Cassi, X.; Martínez-Puchol, S.; Silva-Sales, M.; Cornejo, T.; Bartolome, R.; Bofill-Mas, S.; Girones, R. Unveiling Viruses Associated with Gastroenteritis Using a Metagenomics Approach. Viruses 2020, 12, 1432. [Google Scholar] [CrossRef] [PubMed]
- Tohma, K.; Lepore, C.J.; Gao, Y.; Ford-Siltz, L.A.; Parra, G.I. Population Genomics of GII.4 Noroviruses Reveal Complex Diversification and New Antigenic Sites Involved in the Emergence of Pandemic Strains. MBio 2019, 10, e02202-19. [Google Scholar] [CrossRef]
- Maunula, L.; Roivainen, M.; Keränen, M.; Mäkela, S.; Söderberg, K.; Summa, M.; von Bonsdorff, C.H.; Lappalainen, M.; Korhonen, T.; Kuusi, M.; et al. Detection of Human Norovirus from Frozen Raspberries in a Cluster of Gastroenteritis Outbreaks. Eurosurveillance 2009, 14, 19435. [Google Scholar] [CrossRef] [PubMed]
- Jeong, H.S.; Jeong, A.; Cheon, D.S. Epidemiology of Astrovirus Infection in Children. Korean J. Pediatr. 2012, 55, 77–82. [Google Scholar] [CrossRef] [PubMed]
- Johnson, C.; Hargest, V.; Cortez, V.; Meliopoulos, V.A.; Schultz-Cherry, S. Astrovirus Pathogenesis. Viruses 2017, 9, 22. [Google Scholar] [CrossRef]
- Cordey, S.; Vu, D.L.; Schibler, M.; L’Huillier, A.G.; Brito, F.; Docquier, M.; Posfay-Barbe, K.M.; Petty, T.J.; Turin, L.; Zdobnov, E.M.; et al. Astrovirus MLB2, a New Gastroenteric Virus Associated with Meningitis and Disseminated Infection. Emerg. Infect. Dis. 2016, 22, 846–853. [Google Scholar] [CrossRef]
- Kapoor, A.; Li, L.; Victoria, J.; Oderinde, B.; Mason, C.; Pandey, P.; Zaidi, S.Z.; Delwart, E. Multiple Novel Astrovirus Species in Human Stool. J. Gen. Virol. 2009, 90, 2965–2972. [Google Scholar] [CrossRef]
- Gabbay, Y.B.; Leite, J.P.G.; Oliveira, D.S.; Nakamura, L.S.; Nunes, M.R.T.; Mascarenhas, J.D.A.P.; Heinemann, M.B.; Linhares, A.C. Molecular Epidemiology of Astrovirus Type 1 in Belém, Brazil, as an Agent of Infantile Gastroenteritis, over a Period of 18 Years (1982–2000): Identification of Two Possible New Lineages. Virus Res. 2007, 129, 166–174. [Google Scholar] [CrossRef]
- Rivadulla, E.; Romalde, J.L. A Comprehensive Review on Human Aichi Virus. Virol. Sin. 2020, 35, 501–516. [Google Scholar] [CrossRef] [PubMed]
- Reuter, G.; Boros, Á.; Pankovics, P. Kobuviruses—A Comprehensive Review. Rev. Med. Virol. 2011, 21, 32–41. [Google Scholar] [CrossRef]
- Ambert-Balay, K.; Lorrot, M.; Bon, F.; Giraudon, H.; Kaplon, J.; Wolfer, M.; Lebon, P.; Gendrel, D.; Pothier, P. Prevalence and Genetic Diversity of Aichi Virus Strains in Stool Samples from Community and Hospitalized Patients. J. Clin. Microbiol. 2008, 46, 1252–1258. [Google Scholar] [CrossRef]
- Rosario, K.; Nilsson, C.; Lim, Y.W.; Ruan, Y.; Breitbart, M. Metagenomic Analysis of Viruses in Reclaimed Water. Environ. Microbiol. 2009, 11, 2806–2820. [Google Scholar] [CrossRef] [PubMed]
- Gerba, C.P.; Choi, C.Y. Role of Irrigation Water in Crop Contamination by Viruses. In Viruses in Foods; Springer: Boston, MA, USA, 2006; pp. 257–263. [Google Scholar] [CrossRef]
- Wei, J.; Jin, Y.; Sims, T.; Kniel, K.E. Internalization of Murine Norovirus 1 by Lactuca Sativa during Irrigation. Appl. Environ. Microbiol. 2011, 77, 2508–2512. [Google Scholar] [CrossRef] [PubMed]
- Reganold, J.P.; Wachter, J.M. Organic Agriculture in the Twenty-First Century. Nat. Plants 2016, 2, 15221. [Google Scholar] [CrossRef]
- Machado, D.C.; Maia, C.M.; Carvalho, I.D.; Da Silva, N.F.; Dantas Porfírio Borges Andre, M.C.; Serafini, Á.B. Microbiological Quality of Organic Vegetables Produced in Soil Treated with Different Types of Manure and Mineral Fertilizer. Brazilian J. Microbiol. 2006, 37, 538–544. [Google Scholar] [CrossRef]
- Grusenmeyer, D.C.; Cramer, T.N. Symposium: Manure Management. J. Dairy Sci. 1997, 80, 2651–2654. [Google Scholar] [CrossRef]
- Pell, A.N. Manure and Microbes: Public and Animal Health Problem? J. Dairy Sci. 1997, 80, 2673–2681. [Google Scholar] [CrossRef]
- Alegbeleye, O.O.; Singleton, I.; Sant’Ana, A.S. Sources and Contamination Routes of Microbial Pathogens to Fresh Produce during Field Cultivation: A Review. Food Microbiol. 2018, 73, 177–208. [Google Scholar] [CrossRef]
- Mawdsley, J.L.; Bardgett, R.D.; Merry, R.J.; Pain, B.F.; Theodorou, M.K. Pathogens in Livestock Waste, Their Potential for Movement through Soil and Environmental Pollution. Appl. Soil Ecol. 1995, 2, 1–15. [Google Scholar] [CrossRef]
- Duhaime, M.B.; Deng, L.; Poulos, B.T.; Sullivan, M.B. Towards Quantitative Metagenomics of Wild Viruses and Other Ultra-Low Concentration DNA Samples: A Rigorous Assessment and Optimization of the Linker Amplification Method. Environ. Microbiol. 2012, 14, 2526–2537. [Google Scholar] [CrossRef] [PubMed]
- Karlsson, O.E.; Belák, S.; Granberg, F. The Effect of Preprocessing by Sequence-Independent, Single-Primer Amplification (SISPA) on Metagenomic Detection of Viruses. Biosecur. Bioterror. Biodef. Strategy Pract. Sci. 2013, 11, S227–S234. [Google Scholar] [CrossRef]
- Li, J.; Pan, Y.Q.; Xu, Z.; Wang, Q.; Hang, D.; Shen, N.; Liu, M.; Zhang, C.; Abliz, A.; Deng, Q.; et al. Improved Detection of Human Papillomavirus Harbored in Healthy Skin with FAP6085/64 Primers. J. Virol. Methods 2013, 193, 633–638. [Google Scholar] [CrossRef] [PubMed]
- Akgül, B.; Cooke, J.C.; Storey, A. HPV-Associated Skin Disease. J. Pathol. 2006, 208, 165–175. [Google Scholar] [CrossRef] [PubMed]
- Hošnjak, L.; Komloš, K.F.; Kocjan, B.J.; Seme, K.; Poljak, M. Development of a Novel Multiplex Type-Specific Quantitative Realtime PCR for Detection and Differentiation of Infections with Human Papillomavirus Types HPV2, HPV27, and HPV57. Acta Dermatovenerol. APA 2016, 25, 65–71. [Google Scholar] [CrossRef]
- Yeni, F.; Alpas, H. Vulnerability of Global Food Production to Extreme Climatic Events. Food Res. Int. 2017, 96, 27–39. [Google Scholar] [CrossRef]
- Berger, C.N.; Sodha, S.V.; Shaw, R.K.; Griffin, P.M.; Pink, D.; Hand, P.; Frankel, G. Fresh Fruit and Vegetables as Vehicles for the Transmission of Human Pathogens. Environ. Microbiol. 2010, 12, 2385–2397. [Google Scholar] [CrossRef]
- Kokkinos, P.; Kozyra, I.; Lazic, S.; Söderberg, K.; Vasickova, P.; Bouwknegt, M.; Rutjes, S.; Willems, K.; Moloney, R.; de Roda Husman, A.M.; et al. Virological quality of irrigation water in leafy green vegetables and berry fruits production chains. Food Environ. Virol. 2017, 9, 72–78. [Google Scholar] [CrossRef]
| Irrigation Water | Lettuce | Strawberry | Parsley | |
|---|---|---|---|---|
| Production Site 1 | GW1.1 to GW1.4 | LET1.1 to LET1.4 | STR1.1 to STR1.8 | PAR1.1 to PAR1.4 |
| Production Site 2 | GW2.1 to GW2.4 | LET2.1 to LET2.4 | ||
| Production Site 3 | RIV3.1 to RIV3.4 | LET3.1 to LET3.4 | STR3.1 to STR3.4 | PAR3.1 to PAR3.4 |
| Llobregat river | LLRIV.1 and LLRIV.2 | |||
| Treated wastewater | SE and WFPE |
| HAdV | NoV GI | NoV GII | HEV | ||
|---|---|---|---|---|---|
| Llobregat river | LLRIV.1 | 3.47 × 104 | 6.36 × 103 | 1.33 × 104 | ND |
| LLRIV.2 | 5.99 × 103 | 1.01 × 104 | 4.75 × 104 | ND | |
| Treated wastewater | SE | 8.99 × 104 | 3.77 × 103 | ND | ND |
| WFPE | 1.88 × 105 | 9.49 × 103 | 6.64 × 102 | ND |
| Family | Genus | Species | Genogroup/ Genotype/ Serotype | Samples | |||||
|---|---|---|---|---|---|---|---|---|---|
| Contigs | Length (bp) | Nucleotide Identity (%) | Genome Coverage (%) | Sample Name | Site | ||||
| Astroviridae | Mamastrovirus | Mamastrovirus 1 | HAstV-1 | 2 | 429–435 | 98.60–99.07 | 6.3–6.4 | RIV3.1 | Production Site 3 |
| 1 | 551 | 98.19 | 8.1 | LLRIV.1 | Llobregat river | ||||
| HAstV-4 | 2 | 800–3071 | 92.10–93.62 | 11.9–45.7 | LLRIV.1 | Llobregat river | |||
| HAstV-5 | 1 | 2869 | 92.36 | 42.2 | RIV3.1 | Production Site 3 | |||
| 1 | 808 | 97.65 | 12.1 | WFPE | Treated wastewater | ||||
| Mamastrovirus 6 | AstV-MLB1 | 1 | 420 | 95.00 | 6.8 | LLRIV.1 | Llobregat river | ||
| AstV-MLB2 | 1 | 364 | 98.35 | 5.9 | LLRIV.1 | Llobregat river | |||
| Mamastrovirus 8 | HAstV-VA2 | 1 | 585 | 99.49 | 9.0 | LLRIV.1 | Llobregat river | ||
| Caliciviridae | Norovirus | Norwalk virus | NoV GI.1 | 1 | 524 | 90.15 | 6.8 | LLRIV.1 | Llobregat river |
| NoV GII.4 | 2 | 689–845 | 92.79–97.98 | 9.1–11.2 | LLRIV.1 | Llobregat river | |||
| NoV GII.17 | 1 | 282 | 97.28 | 3.8 | PAR3.2 | Production Site 3 | |||
| 2 | 632–717 | 95.66–98.58 | 8.4–9.5 | LLRIV.1 | Llobregat river | ||||
| Circoviridae | Cyclovirus | Human associated cyclovirus 6 | NG12 | 1 | 1541 | 81.00 | 85.9 | GW1.1 | Production Site 1 |
| 1 | 433 | 88.29 | 24.10 | SE | Treated wastewater | ||||
| Parvoviridae | Dependoparvovirus | Adeno-associated dependoparvovirus A | AAV2 | 1 | 124 | 95.97 | 2.7 | GW2.1 | Production Site 2 |
| 1 | 3040 | 97.27 | 64.9 | RIV3.1 | Production Site 3 | ||||
| 3 | 932–1216 | 96.46–98.39 | 19.9–26.0 | LLRIV.1 | Llobregat river | ||||
| 1 | 1438 | 96.45 | 30.7 | WFPE | Treated wastewater | ||||
| AAV6 | 1 | 682 | 79.71 | 14.6 | LLRIV.1 | Llobregat river | |||
| Bocaparvovirus | Human bocavirus 3 | Undetermined | 3 | 342–566 | 95.61–98.25 | 6.6–10.8 | LLRIV.1 | Llobregat river | |
| Picornaviridae | Kobuvirus | Aichivirus A | Aichi virus 1 | 4 | 348–724 | 94.31–99.42 | 4.2–8.8 | RIV3.1 | Production Site 3 |
| 5 | 404–952 | 95.79–97.56 | 4.9–11.5 | LLRIV.1 | Llobregat river | ||||
| Salivirus | Salivirus A | Undetermined | 3 | 683–1197 | 97.21–98.41 | 8.7–15.3 | RIV3.1 | Production Site 3 | |
| 2 | 459–552 | 97.67–98.04 | 5.9–7.0 | LLRIV.1 | Llobregat river | ||||
| 2 | 395–907 | 96.73–97.97 | 5–11.6 | SE | Treated wastewater | ||||
| 3 | 516–623 | 97.16–97.87 | 6.6–7.9 | WFPE | Treated wastewater | ||||
| Production Site 1 | Production Site 3 | Llobregat River | Treated Wastewater | ||||||
|---|---|---|---|---|---|---|---|---|---|
| STR1.1 | RIV3.1 | PAR3.1 | PAR3.2 | LLRIV.1 | LLRIV.2 | SE | WFPE | ||
| NoV GI | GI.4 | 17 | 1 | 10 | 98,699 | 3 | 15 | 59 | |
| GI.1 | 4 | 2 | 15 | 23,411 | 35,901 | ||||
| GI.2 | 8 | 28 | 2 | 2 | |||||
| GI.3 | 4 | 9 | 9500 | ||||||
| GI.5 | 2 | 12,021 | 475 | ||||||
| NoV GII | GII.4 | 1 | 3 | 9331 | 3 | 6 | |||
| GII.13 | 2 | 3 | 11 | 49,651 | 16 | ||||
| GII.2 | 2 | 16,933 | 4 | ||||||
| GII.17 | 52 | 1203 | |||||||
| GII.3 | 68 | ||||||||
 | |||||||||
| Production Site 3 | Llobregat River | Treated Wastewater | |||||||
|---|---|---|---|---|---|---|---|---|---|
| RIV3.1 | LET3.4 | PAR3.1 | PAR3.2 | LLRIV.1 | LLRIV.2 | SE | WFPE | ||
| HPV | HPV-92 | 1 | 2 | 14 | 6 | 39,158 | 15 | 3 | 16 |
| HPV-105 | 3 | 45 | 381,617 | 16 | 108 | 197 | 13 | 337,323 | |
| HPV-122 | 2 | 19 | 90 | 50 | 271,741 | 38 | 11 | 114 | |
| HPV-38 | 152,893 | 14 | 19 | 23 | 1161 | 8 | 7 | ||
| HPV-145 | 102,028 | 17 | 8 | 8 | 150 | 5 | 6 | ||
| HPV-177 | 16 | 10 | 3 | 10 | 20 | 8 | 28 | ||
| HPV-182 | 1 | 9 | 580 | 1 | 1 | 3 | 2 | ||
| HPV-37 | 101 | 45 | 8 | 9 | 90 | 19 | |||
| HPV-76 | 84 | 6 | 8 | 87,512 | 4 | 10 | |||
| HPV-96 | 2 | 1 | 145 | 4 | 1171 | ||||
| HPV-4 | 7 | 1 | 2 | 169,019 | 3 | ||||
| HPV-57 | 6 | 56 | 76,118 | 1 | |||||
| HPV-12 | 20 | 16 | 79 | 152,261 | 17 | 35 | |||
| HPV-8 | 321 | 1 | |||||||
| HPV-17 | 2 | 3 | |||||||
| HPV-196 | 49 | 1 | |||||||
| Other PV | BPV-7 | 1 | 1 | ||||||
| RnPV-2 | 17 | ||||||||
 | |||||||||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Itarte, M.; Martínez-Puchol, S.; Forés, E.; Hundesa, A.; Timoneda, N.; Bofill-Mas, S.; Girones, R.; Rusiñol, M. NGS Techniques Reveal a High Diversity of RNA Viral Pathogens and Papillomaviruses in Fresh Produce and Irrigation Water. Foods 2021, 10, 1820. https://doi.org/10.3390/foods10081820
Itarte M, Martínez-Puchol S, Forés E, Hundesa A, Timoneda N, Bofill-Mas S, Girones R, Rusiñol M. NGS Techniques Reveal a High Diversity of RNA Viral Pathogens and Papillomaviruses in Fresh Produce and Irrigation Water. Foods. 2021; 10(8):1820. https://doi.org/10.3390/foods10081820
Chicago/Turabian StyleItarte, Marta, Sandra Martínez-Puchol, Eva Forés, Ayalkibet Hundesa, Natàlia Timoneda, Sílvia Bofill-Mas, Rosina Girones, and Marta Rusiñol. 2021. "NGS Techniques Reveal a High Diversity of RNA Viral Pathogens and Papillomaviruses in Fresh Produce and Irrigation Water" Foods 10, no. 8: 1820. https://doi.org/10.3390/foods10081820
APA StyleItarte, M., Martínez-Puchol, S., Forés, E., Hundesa, A., Timoneda, N., Bofill-Mas, S., Girones, R., & Rusiñol, M. (2021). NGS Techniques Reveal a High Diversity of RNA Viral Pathogens and Papillomaviruses in Fresh Produce and Irrigation Water. Foods, 10(8), 1820. https://doi.org/10.3390/foods10081820








