Music Is Served: How Acoustic Interventions in Hospital Dining Environments Can Improve Patient Mealtime Wellbeing
Abstract
1. Introduction
1.1. Background
1.1.1. Visual Meal Environment Aesthetics
1.1.2. Acoustic Meal Environments
1.1.3. Mealtime Music
1.2. Objectives
- Identify and resolve issues in the existing acoustic environment of a common dining area of a hospital ward.
- Explore how improvements to the acoustic eating environment, including music playback, affects patients’ mealtime experience, behaviour, and food intake.
- Examine various musical genres and their appropriateness for eating situations in hospital settings.
2. Materials and Methods
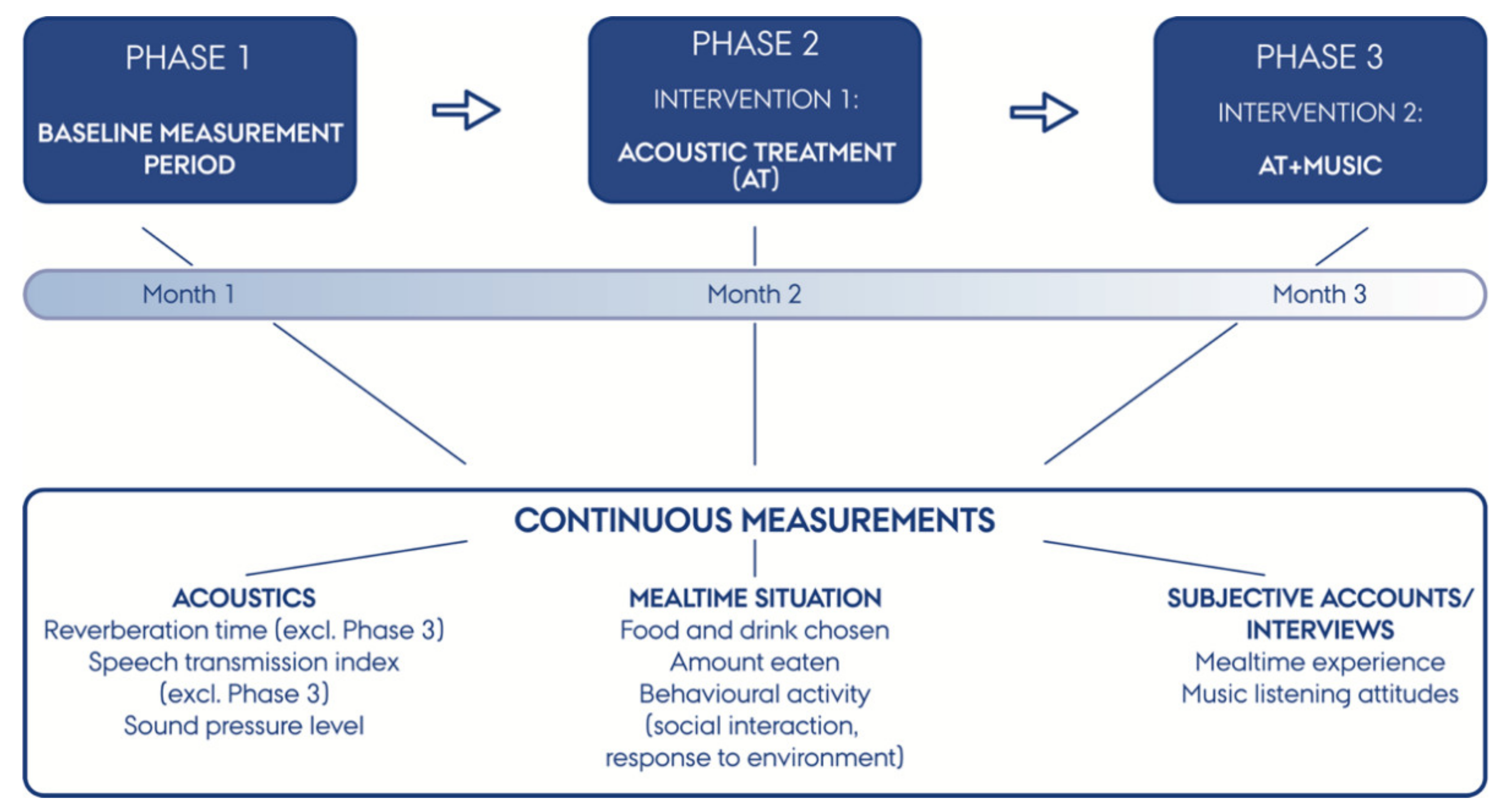
2.1. Design
2.1.1. Room Acoustics Analysis, Treatment, and Wall Panel Design
2.1.2. Music Selection (Phase 3 Only)
2.1.3. Participants
2.1.4. Meal Procedure
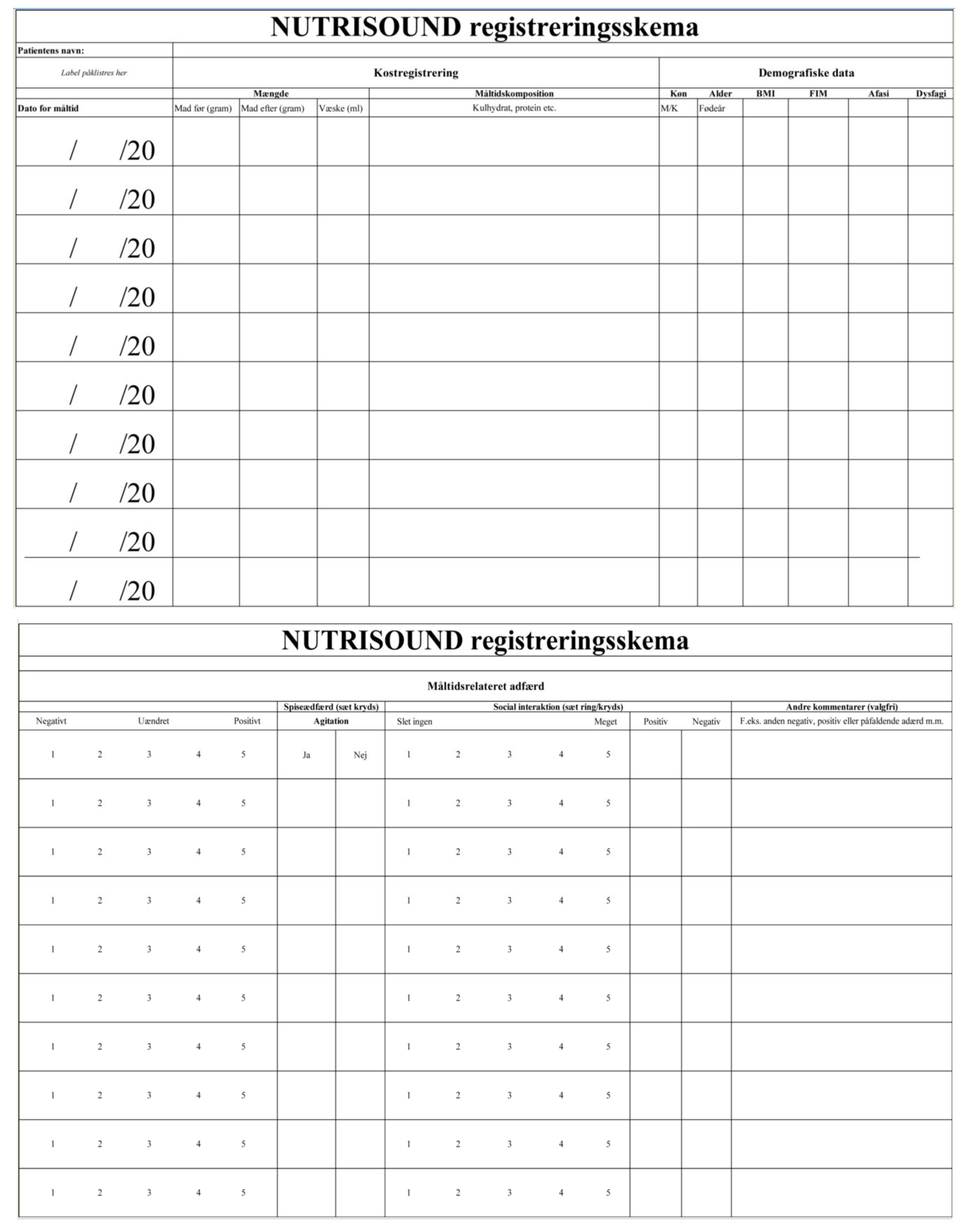
2.2. Data Collection
2.2.1. Overall Sound Pressure Level
2.2.2. Patient Food Intake and Mealtime Behaviour
2.2.3. Patient and Staff Interviews
2.3. Data Analysis
2.3.1. Sound Pressure Levels
2.3.2. Mealtime Observations
2.3.3. Qualitative Interviews
3. Results
3.1. Sound Pressure Levels
3.2. Mealtime Observations
3.3. Qualitative Interviews
3.3.1. Acoustic Panels Enhance Inter-Patient and Staff Communication
I think there is a big difference in the sound […] I could clearly hear that it was easier to talk at the table…There is less “ringing” in the room […] I think you are much better able to hear what is being said around the whole table. You are taking part more. Because it is not ringing in the same way in there. It is just calmer […] You can almost feel it the moment you enter, even when you don’t speak, it is as if there is just better acoustics. It is just kind of better in a way […] it is a nice place to be (project nurse).
Before, it was just a bad room in which to move plates and cutlery around, but I don’t think this makes as much noise anymore […] it has also led to us speaking softer. When we’re standing at the buffet, we have not spoken so loudly I don’t think … It has this calming atmosphere (project nurse).
3.3.2. Acoustic Panels Enhance Physical Environment Aesthetics and Promotes “Cosiness” and Pleasantness
We are just sitting, you know, like “hospital”, and “older people”, and “it’s a bit sad” and it’s a “serious illness” […] Recovery should be a cosy place where you feel at home, because you have to be there for a long time (Participant 06, Phase 1).
[…] I think that if [the pictures] had not been there, then it would have been very hospital-like. Because there are completely white walls in there. And these pictures are fantastic. The blueberries and the cabbage and the apple. The colours, and then the mere size of them […] It seems cosy, you are almost… it grabs you, the room “hugs” you […] The colours, the deep, red apple and those blueberries and the cabbage, yes, it is a little intoxicating, because of the size. Yes, it is cosy, very cosy (Participant 15, Phase 3).
3.3.3. Music Enhances the Physical Environment, Prolongs Meal Duration, and the Social Aspects of the Meal Activity
I definitely think there are more conversations now. We talk about ‘this one, we know this one’, and ‘this one is by so-and-so’ […] And I think that the chatter is going better […] there was a melody from a gymnastics show I had seen, that I really liked. Then I told the others about that experience I had had with that piece of music. In that way the music leads us onto some other topics than we normally talk about (Participant 14, Phase 3).
[…] it is nice that there is background music […] we did not choose each other. In that way, it is nice that there is also music. Then you have something to naturally talk about […] it has definitely generated conversations about the music (Participant 11, Phase 3).
I think it [the music] does that you take longer to eat. Because you are sitting and eating and enjoying […] The way that we eat the food. It is better digested than when we just quickly go in and eat and go back to our rooms. So, we sit and listen to the music and then enjoy (Participant 12, Phase 3).
They have been sitting in there much longer. That has really been thought-provoking […] It was this thing where they would have a cup of coffee and talk a little. It was much more a cosy atmosphere after the meal […] and some of them actually eat more. It’s more this thing of where they grab a piece of fruit or a piece of bread with the coffee (project nurse).
3.3.4. Patient and Staff Views on Music in Hospital Settings
4. Discussion
4.1. Acoustic Panels Enhance Inter-Patient and Staff Communication
4.2. Nutritional Observations
4.3. Acoustic Panels Enhance Physical Environment Aesthetics and Promotes “Cosiness” and Pleasantness
4.4. Music Enhances the Physical Environment, Prolongs Meal Duration and the Social Aspects of the Meal Activity
4.5. Patient and Staff Views on Music in Hospital Settings
4.6. Limitations
4.7. Implications
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Baseline Empty Room | Phase 2 Acoustic Treatment Empty Room | ||||
|---|---|---|---|---|---|
| Frequency | RT20 (s) | STI | Frequency | RT20 (s) | STI |
| 0.604 | 0.676 | ||||
| 63 Hz | 1.63 | 63 Hz | 1.73 | ||
| 125 Hz | 0.33 | 125 Hz | 0.30 | ||
| 250 Hz | 0.70 | 250 Hz | 0.59 | ||
| 500 Hz | 0.53 | 500 Hz | 0.50 | ||
| 1 kHz | 0.79 | 1 kHz | 0.87 | ||
| 2 kHz | 1.27 | 2 kHz | 0.73 | ||
| 4 kHz | 1.11 | 4 kHz | 0.76 | ||
| 8 kHz | 0.84 | 8 kHz | 0.60 | ||
| Eating experience |
| Please describe your physical and mental state before, during and after the lunch meal. |
| Commensality |
| What does commensality mean to you? |
| Are you more used to eating alone or with others? |
| How do you feel about the social aspect in relation to eating? |
| Is conversation during mealtime something you prefer? |
| The environment |
| Is there anything specific to the dining room that you have noticed and/or that is important to your eating experience? |
| How is the dining room engaging your senses? |
| Are some senses engaged more than others? |
| Do you notice the sound in the dining room? |
| Is it relevant to your eating experience? |
| Music listening practices and attitude towards sound in general |
| What is your relationship to sound and music in general? |
| Do you often think about sound/music in your surroundings? |
| Do you listen to music a lot in your daily life? |
| Are you easily distracted or annoyed by sound/noise? |
| Would you expect to encounter music at a place such as this? |
References
- World Health Organization (WHO). Essential Nutrition Actions—Mainstreaming Nutrition through the Life-Course; World Health Organization: Geneva, Switzerland, 2019. [Google Scholar]
- The European Nutrition for Health Alliance. STOP Disease-Related Malnutrition and Diseases Due to Malnutrition! The European Nutrition for Health Alliance: Prague, Czech Republic, 2009. [Google Scholar]
- World Health Organization (WHO). Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 25 March 2021).
- Ljungqvist, O.; van Gossum, A.; Sanz, M.L.; de Man, F. The European fight against malnutrition. Clin. Nutr. 2009, 29, 149–150. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, E.; Ferguson, M.; Banks, M.; Batterham, M.; Bauer, J.; Capra, S.; Isenring, E. Malnutrition and poor food intake are associated with prolonged hospital stay, frequent readmissions, and greater in-hospital mortality: Results from the Nutrition Care Day Survey 2010. Clin. Nutr. 2012, 32, 737–745. [Google Scholar] [CrossRef] [PubMed]
- Sundhedsstyrelsen. Oplæg om Ernæringsindsatser for den ældre Medicinsk Patient; Sundhedsstyrelsen: Copenhagen, Denmark, 2017. [Google Scholar]
- Vizzini, A.R.D.; Aranda-Michel, J.M.D. Nutritional support in head injury. Nutrition 2011, 27, 129–132. [Google Scholar] [CrossRef]
- Wang, X.; Dong, Y.; Han, X.; Qi, X.-Q.; Huang, C.-G.; Hou, L.-J. Nutritional support for patients sustaining traumatic brain injury: A systematic review and meta-analysis of prospective studies. PLoS ONE 2013, 8, e58838. [Google Scholar] [CrossRef]
- Erdman, J.; Oria, M.; Pillsbury, L. Nutrition in Clinical Practice Guidelines for Traumatic Brain Injury. In Nutrition and Traumatic Brain Injury; Improving Acute and Subacute Health Outcomes in Military Personnel; The National Academies Press: Washington, DC, USA, 2011; Volume 26. [Google Scholar]
- Krakau, K.B.S.; Hansson, A.B.S.; Karlsson, T.M.D.P.D.; de Boussard, C.N.M.D.P.D.; Tengvar, C.M.D.P.D.; Borg, J.M.D.P.D. Nutritional treatment of patients with severe traumatic brain injury during the first six months after injury. Nutrition 2007, 23, 308–317. [Google Scholar] [CrossRef]
- Carney, N.A.; Ghajar, J. Guidelines for the management of severe traumatic brain injury. Introd. J. Neurotrauma 2007, 24 (Suppl. S1), S1–S2. [Google Scholar] [CrossRef]
- Aadal, L.; Mortensen, J.; Nielsen, J.F. Weight reduction after severe brain injury: A challenge during the rehabilitation course. J. Neurosci. Nurs. 2015, 47, 85–90. [Google Scholar] [CrossRef]
- Mosselman, M.J.; Kruitwagen, C.L.J.J.; Schuurmans, M.J.; Hafsteinsdóttir, T.B. Malnutrition and risk of malnutrition in patients with stroke: Prevalence during hospital stay. J. Neurosci. Nurs. 2013, 45, 194–204. [Google Scholar] [CrossRef]
- Burgos, R.; Bretón, I.; Cereda, E.; Desport, J.C.; Dziewas, R.; Genton, L.; Gomes, F.; Jésus, P.; Leischker, A.; Muscaritoli, M.; et al. ESPEN guideline clinical nutrition in neurology. Clin. Nutr. 2018, 37, 354–396. [Google Scholar] [CrossRef] [PubMed]
- Chapple, L.S.; Deane, A.M.; Heyland, D.K.; Lange, K.; Kranz, A.J.; Williams, L.T.; Chapman, M.J. Energy and protein deficits throughout hospitalization in patients admitted with a traumatic brain injury. Clin. Nutr. 2016, 35, 1315–1322. [Google Scholar] [CrossRef]
- Feo, R.; Kitson, A.; Conroy, T. How fundamental aspects of nursing care are defined in the literature: A scoping review. J. Clin. Nurs. 2018, 27, 2189–2229. [Google Scholar] [CrossRef]
- Feo, R.; Conroy, T.; Jangland, E.; Muntlin Athlin, Å.; Brovall, M.; Parr, J.; Blomberg, K.; Kitson, A. Towards a standardised definition for fundamental care: A modified Delphi study. J. Clin. Nurs. 2018, 27, 2285–2299. [Google Scholar] [CrossRef] [PubMed]
- Henderson, V. The concept of nursing. J. Adv. Nurs. 2006, 53, 21–31. [Google Scholar] [CrossRef]
- Jefferies, D.; Johnson, M.; Ravens, J. Nurturing and nourishing: The nurses’ role in nutritional care. J. Clin. Nurs. 2011, 20, 317–330. [Google Scholar] [CrossRef] [PubMed]
- Kitson, A.; Conroy, T.; Wengström, Y.; Profetto-McGrath, J.; Robertson-Malt, S. Defining the fundamentals of care. Int. J. Nurs. Pract. 2010, 16, 423–434. [Google Scholar] [CrossRef]
- Joanna Briggs Institute. Effectiveness of interventions for under nourished older inpatients in the hospital setting. Aust. Nurs. J. 2007, 15, 28–31. [Google Scholar]
- Hartwell, H.J.; Shepherd, P.A.; Edwards, J.S.A.; Johns, N. What do patients value in the hospital meal experience? Appetite 2016, 96, 293–298. [Google Scholar] [CrossRef]
- Holst, M.; Beermann, T.; Mortensen, M.N.; Skadhauge, L.B.; Køhler, M.; Lindorff-Larsen, K.; Rasmussen, H.H. Optimizing protein and energy intake in hospitals by improving individualized meal serving, hosting and the eating environment. Nutrition 2017, 34, 14–20. [Google Scholar] [CrossRef]
- Beck, M.; Martinsen, B.; Poulsen, I.; Birkelund, R. Mealtimes in a neurological ward: A phenomenological-hermeneutic study. J. Clin. Nurs. 2016, 25, 1614–1623. [Google Scholar] [CrossRef]
- Beck, M.; Birkelund, R.; Poulsen, I.; Martinsen, B. Hospital meals are existential asylums to hospitalized people with a neurological disease: A phenomenological-hermeneutical explorative study of the meaningfulness of mealtimes. Nurs. Open 2019, 6, 626–634. [Google Scholar] [CrossRef] [PubMed]
- Perry, L.; Hamilton, S.; Williams, J.; Jones, S. Nursing Interventions for Improving Nutritional Status and Outcomes of Stroke Patients: Descriptive Reviews of Processes and Outcomes: Nursing Nutritional Interventions for Stroke Patients. Worldviews Evid. Based Nurs. 2013, 10, 17–40. [Google Scholar] [CrossRef]
- The Danish National Board of Health. A Guide for Doctors, Nurses, Healthcare Assistants, Auxiliary Nurses and Clinical Dietitians—Screening and Treatment of Patients at Nutritional Risk; The Danish National Board of Health: Copenhagen, Denmark, 2008. [Google Scholar]
- Olsen, T.D.; Fisker, A.M. Madens rum—Handler patienternes spiseoplevelse ikke også om arkitekturen omkring måltidet? Tidsskr. Forsk. I Sygd. Og Samf. 2011, 8, 75–85. [Google Scholar] [CrossRef]
- Meiselman, H.L. Dimensions of the meal. J. Foodserv. 2008, 19, 13–21. [Google Scholar] [CrossRef]
- Nijs, K.A.N.D.; de Graaf, C.; Kok, F.J.; van Staveren, W.A. Effect of family style mealtimes on quality of life, physical performance, and body weight of nursing home residents: Cluster randomised controlled trial. BMJ 2006, 332, 1180–1184. [Google Scholar] [CrossRef] [PubMed]
- Hartwell, H.; Shepherd, P.; Edwards, J. Effects of a hospital ward eating environment on patients’ mealtime experience: A pilot study. Nutr. Diet. 2013, 70. [Google Scholar] [CrossRef]
- Paquet, C.; St-Arnaud-McKenzie, D.; Ma, Z.; Kergoat, M.-J.; Ferland, G.; Dubé, L. More than just not being alone: The number, nature, and complementarity of meal-time social interactions influence food intake in hospitalized elderly patients. Gerontologist 2008, 48, 603–611. [Google Scholar] [CrossRef] [PubMed]
- McLaren-Hedwards, T.; D’Cunha, K.; Elder-Robinson, E.; Smith, C.; Jennings, C.; Marsh, A.; Young, A. Effect of communal dining and dining room enhancement interventions on nutritional, clinical and functional outcomes of patients in acute and sub-acute hospital, rehabilitation and aged-care settings: A systematic review. Nutr. Diet. 2021, 1–29. [Google Scholar] [CrossRef]
- Mathey, M.-F.A.M.; Vanneste, V.G.G.; de Graaf, C.; de Groot, L.C.; van Staveren, W.A. Health Effect of Improved Meal Ambiance in a Dutch Nursing Home: A 1-Year Intervention Study. Prev. Med. 2001, 32, 416–423. [Google Scholar] [CrossRef]
- Justesen, L. Hospitable Meal in Hospitals: Co-creation a Passion for Food with Patients. Ph.D. Thesis, Aalborg University, Aalborg, Denmark, 2015. [Google Scholar]
- Baptiste, F.; Egan, M.; Dubouloz-Wilner, C.J. Geriatric rehabilitation patients’ perceptions of unit dining locations. Can. Geriatr. J. 2014, 17, 38–44. [Google Scholar] [CrossRef][Green Version]
- Justesen, L.; Gyimóthy, S.; Mikkelsen, B.E. Hospitality within hospital meals—Socio-material assemblages. J. Foodserv. Bus. Res. 2016, 19, 255–271. [Google Scholar] [CrossRef]
- Ståhlberg-Aalto, F. The Aesthetics and Architecture of Care Environments: A Q Methodological Study of Ten Care Environments in Japan and the European Countries of Finland, Sweden, the UK, France and Austria; Aalto University, School of Arts, Design and Architecture: Helsinki, Finland, 2019. [Google Scholar]
- Lankston, L.; Cusack, P.; Fremantle, C.; Isles, C. Visual art in hospitals: Case studies and review of the evidence. J. R. Soc. Med. 2010, 103, 490–499. [Google Scholar] [CrossRef]
- Wilson, C.; Bungay, H.; Munn-Giddings, C.; Boyce, M. Healthcare professionals’ perceptions of the value and impact of the arts in healthcare settings: A critical review of the literature. Int. J. Nurs. Stud. 2016, 56, 90–101. [Google Scholar] [CrossRef]
- Nanda, U.; Eisen, S.; Zadeh, R.S.; Owen, D. Effect of visual art on patient anxiety and agitation in a mental health facility and implications for the business case. J. Psychiatr. Ment. Health Nurs. 2011, 18, 386–393. [Google Scholar] [CrossRef]
- Fuchs, H. Applied Acoustics: Concepts, Absorbers, and Silencers for Acoustical Comfort and Noise Control; Springer: Berlin, Germany, 2013. [Google Scholar]
- Eurich, B.; Klenzner, T.; Oehler, M. Impact of room acoustic parameters on speech and music perception among participants with cochlear implants. Hear. Res. 2019, 377, 122–132. [Google Scholar] [CrossRef]
- Knudsen, V.O. The Hearing of Speech in Auditoriums. J. Acoust. Soc. Am. 1929, 1, 30. [Google Scholar] [CrossRef]
- Zacharov, N. Sensory Evaluation of Sound; CRC Press, Taylor & Francis Group: Boca Raton, FL, USA, 2019. [Google Scholar]
- Cox, T.J.; D’Antonio, P. Acoustic Absorbers and Diffusers: Theory, Design and Application, 3rd ed.; Taylor & Francis: Boca Raton, FL, USA, 2017. [Google Scholar]
- Xyrichis, A.; Wynne, J.; Mackrill, J.; Rafferty, A.M.; Carlyle, A. Noise pollution in hospitals. BMJ 2018, 363, k4808. [Google Scholar] [CrossRef]
- Liu, H.; Ma, H.; Kang, J.; Wang, C. The speech intelligibility and applicability of the speech transmission index in large spaces. Appl. Acoust. 2020, 167, 107400. [Google Scholar] [CrossRef]
- Ministry of Transport, Building, and Housing. Executive Order on Building Regulations 2018 (BR18). Title Number: BSo2000-00353. 2018. Available online: https://www.retsinformation.dk/eli/lta/2019/1399 (accessed on 25 October 2021).
- DS 490:2018: Lydklassifikation af Boliger = Sound Classification of Dwellings; Fonden Dansk Standard: Copenhagen, Denmark, 2018.
- Gebauer, L.; Vuust, P. Music Interventions in Health Care: White Paper, 1. Oplag. ed.; Danish Sound Innovation Network: Kongens, Lyngby, 2014. [Google Scholar]
- Bonde, L.O.; Theorell, T. Music and Public Health: A Nordic Perspective; Springer International Publishing AG: Cham, Switzerland, 2018. [Google Scholar]
- Topf, M. Hospital noise pollution: An environmental stress model to guide research and clinical interventions. J. Adv. Nurs. 2000, 31, 520–528. [Google Scholar] [CrossRef] [PubMed]
- Busch-Vishniac, I.J.; West, J.E.; Barnhill, C.; Hunter, T.; Orellana, D.; Chivukula, R. Noise levels in Johns Hopkins Hospital. J. Acoust. Soc. Am. 2005, 118, 3629–3645. [Google Scholar] [CrossRef] [PubMed]
- Joseph, A.; Ulrich, R. Sound Control for Improved Outcomes in Healthcare Settings. Cent. Health Des. 2007, 4, 1–15. [Google Scholar]
- Spence, C.; Keller, S. Medicines Melodies: On the Costs & Benefits of Music, Soundscapes, & Noise in Healthcare Settings. Music Med. 2019, 11, 211–225. [Google Scholar]
- Joseph, E.B.; Mehazabeen, H.; Monisha, U. Noise pollution in hospitals—A study of public perception. Noise Health 2020, 22, 28–33. [Google Scholar]
- Aaron, J.N.; Carlisle, C.C.; Carskadon, M.A.; Meyer, T.J.; Hill, N.S.; Millman, R.P. Environmental noise as a cause of sleep disruption in an intermediate respiratory care unit. Sleep 1996, 19, 707–710. [Google Scholar] [CrossRef]
- Veljovic, F.; Burak, S.; Begic, E.; Masic, I. Noise Effect on Blood Pressure and Heart Rate—Regression Analysis in Service of Prediction. Acta Inform. Med. 2019, 27, 162–166. [Google Scholar] [CrossRef]
- Wysocki, A.B. The effect of intermittent noise exposure on wound healing. Adv. Wound Care 1996, 9, 35. [Google Scholar] [PubMed]
- Morrison, W.E.; Haas, E.C.; Shaffner, D.H.; Garrett, E.S.; Fackler, J.C. Noise, stress, and annoyance in a pediatric intensive care unit. Crit. Care Med. 2003, 31, 113–119. [Google Scholar] [CrossRef] [PubMed]
- Chanda, M.L.; Levitin, D.J. The neurochemistry of music. Trends Cogn. Sci. 2013, 17, 179–193. [Google Scholar] [CrossRef] [PubMed]
- Johnson, R.; Taylor, C. Can playing pre-recorded music at mealtimes reduce the symptoms of agitation for people with dementia? Int. J. Ther. Rehabil. 2011, 18, 700–708. [Google Scholar] [CrossRef]
- Courtright, P.; Johnson, S.; Baumgartner, M.A.; Jordan, M.; Webster, J.C. Dinner music: Does it affect the behavior of psychiatric inpatients? J. Psychosoc. Nurs. Ment. Health Serv. 1990, 28, 37–40. [Google Scholar] [CrossRef]
- Goddaer, J.; Abraham, I.L. Effects of relaxing music on agitation during meals among nursing home residents with severe cognitive impairment. Arch. Psychiatr. Nurs. 1994, 8, 150–158. [Google Scholar] [CrossRef]
- Hicks-Moore, S.L. Relaxing Music at Mealtime in Nursing Homes: Effects on Agtated Patients with Dementia. J. Gerontol. Nurs. 2005, 31, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Ragneskog, H.; Kihlgren, M.; Karlsson, I.; Norberg, A. Dinner Music for Demented Patients: Analysis of Video-Recorded Observations. Clin. Nurs. Res. 1996, 5, 262–277. [Google Scholar] [CrossRef]
- Denney, A. Quiet music: An intervention for mealtime agitation? J. Gerontol. Nurs. 1997, 23, 16–23. [Google Scholar] [CrossRef]
- Ho, S.Y.; Lai, H.L.; Jeng, S.Y.; Tang, C.W.; Sung, H.C.; Chen, P.W. The effects of researcher-composed music at mealtime on agitation in nursing home residents with dementia. Arch. Psychiatr. Nurs. 2011, 25, e49–e55. [Google Scholar] [CrossRef]
- Richeson, N.E.; Neill, D.J. Therapeutic Recreation Music Intervention to Decrease Mealtime Agitation and Increase Food Intake in Older Adults with Dementia. Am. J. Recreat. Ther. 2004, 3, 37–41. [Google Scholar]
- Ragneskog, H.; Bråne, G.; Karlsson, I.; Kihlgren, M. Influence of Dinner Music on Food Intake and Symptoms Common in Dementia. Scand. J. Caring Sci. 1996, 10, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Thomas, D.W.; Smith, M. The Effect of Music on Caloric Consumption Among Nursing Home Residents with Dementia of the Alzheimer’s Type. Act. Adapt. Aging 2009, 33, 1–16. [Google Scholar] [CrossRef]
- Tan, X.; Yowler, C.J.; Super, D.M.; Fratianne, R.B. The Interplay of Preference, Familiarity and Psychophysical Properties in Defining Relaxation Music. J. Music Ther. 2012, 49, 150–179. [Google Scholar] [CrossRef] [PubMed]
- Wigram, T.; Grocke, D. Receptive Methods in Music Therapy: Techniques and Clinical Applications for Music Therapy Clinicians, Educators and Students; Jessica Kingsley Publishers: London, UK, 2007. [Google Scholar]
- Wärja, M.; Bonde, L.O. Music as Co-Therapist: Towards a Taxonomy of Music in Therapeutic Music and Imagery Work. Music Med. 2014, 6, 16–27. [Google Scholar] [CrossRef]
- Lund, H.N.; Bertelsen, L.R. “Musikstjernen”—En ny stjerne i psykiatrien. Dan. Musikterapi 2016, 13, 3–10. [Google Scholar]
- ISO. Acoustics—Measurement of room acoustic parameters. In Part 1: Performance Space (ISO Standard No. 3382-1:2009); ISO: Geneva, Switzerland, 2009. [Google Scholar]
- Hannibal, N.; Lund, H.N.; Bonde, L.O. Musiklyttepuder, Lydbøjler og Spillelister i Behandlingen af Psykiatriske Patienter. Musikterapi I Psykiatr. Online 2013, 8, 4–17. [Google Scholar] [CrossRef]
- Lund, H.N.; Bertelsen, L.R.; Bonde, L.O. Sound and Music Interventions in Psychiatry at Aalborg University Hospital. SoundEffects 2016, 6, 48–68. [Google Scholar] [CrossRef]
- MusiCure. MusiCure in Healthcare®-Developed through 25 Years of International Research for Hospitals Departments. Available online: https://musicure.com/ (accessed on 25 March 2021).
- Curle, L.; Keller, H. Resident interactions at mealtime: An exploratory study. Eur. J. Ageing 2010, 7, 189–200. [Google Scholar] [CrossRef] [PubMed]
- Charon, J.M. Symbolic Interactionism: An Introduction, an Interpretation, an Integration; Prentice-Hall Inc: Englewood Cliffs, NJ, USA, 1979. [Google Scholar]
- Kvale, S.; Brinkmann, S. Interview: Det Kvalitative Forskningsinterview som Håndværk, 3rd ed.; Hans Reitzel: Copenhagen, Denmark, 2018. [Google Scholar]
- Barnard, A.; McCosker, H.; Gerber, R. Phenomenography: A Qualitative Research Approach for Exploring Understanding in Health Care. Qual. Health Res. 1999, 9, 212–226. [Google Scholar] [CrossRef]
- Sjöström, B.; Dahlgren, L.O. Applying phenomenography in nursing research. J. Adv. Nurs. 2002, 40, 339–345. [Google Scholar] [CrossRef] [PubMed]
- MacDonald, R.A.R.; Kreutz, G.; Mitchell, L. Music, Health, and Wellbeing; Oxford University Press: Oxford, UK, 2013. [Google Scholar]
- Spence, C.; Reinoso-Carvalho, F.; Velasco, C.; Wang, Q.J. Extrinsic Auditory Contributions to Food Perception & Consumer Behaviour: An Interdisciplinary Review. Multisens. Res. 2019, 32, 275–318. [Google Scholar] [CrossRef]
- Crisinel, A.-S.; Cosser, S.; King, S.; Jones, R.; Petrie, J.; Spence, C. A bittersweet symphony: Systematically modulating the taste of food by changing the sonic properties of the soundtrack playing in the background. Food Qual. Prefer. 2012, 24, 201–204. [Google Scholar] [CrossRef]
- Caldwell, C.; Hibbert, S.A. Play that one again: The effect of music tempo on consumer behaviour in a restaurant. Eur. Adv. Consum. Res. 1999, 4, 58–62. [Google Scholar]
- Caldwell, C.; Hibbert, S.A. The influence of music tempo and musical preference on restaurant patrons’ behavior. Psychol. Mark. 2002, 19, 895–917. [Google Scholar] [CrossRef]
- Roballey, T.; McGreevy, C.; Rongo, R.R.; Schwantes, M.L.; Steger, P.J.; Wininger, M.A.; Gardner, E.B. The effect of music on eating behavior. Bull. Psychon. Soc. 1985, 23, 221–222. [Google Scholar] [CrossRef]
- Mathiesen, S.L.; Mielby, L.A.; Byrne, D.V.; Wang, Q.J. Music to eat by: A systematic investigation of the relative importance of tempo and articulation on eating time. Appetite 2020, 155, 104801. [Google Scholar] [CrossRef] [PubMed]

| Characteristics of Study Participants | Total | Phase 1 Baseline No Intervention | Phase 2 Acoustic Intervention | Phase 3 Acoustic Intervention + Music |
|---|---|---|---|---|
| Number of patients (overlapped from previous phase) | 17 | 7 | 11 (4) | 7 (4) |
| Male | 11 | 5 | 8 (3) | 4 (3) |
| Female | 6 | 2 | 3 (1) | 3 (1) |
| Mean age in years (SD) | 64.47 (9.19) | 67.29 (7.65) | 65.55 (8.29) | 60.50 (11.20) |
| Mean BMI (SD) | 28.33 (5.01) | 27.14 (3.02) | 30.13 (5.47) | 26.87 (8.03) |
| Mean FIM * (SD) | 99.35 (20.55) | 97.14 (21.82) | 96.43 (22.57) | 111.33 (12.66) |
| Mean no. of meals in the dining room (SD) | 10.35 (5.89) | 8.14 (5.64) | 5.73 (2.24) | 7.57 (3.69) |
| Mealtime observations | ||||
| Average food intake in grams (SD) | 334.96 (107.87) | 359.70 (99.83) | 338.50 (100.31) | |
| Average fluid intake in millilitres (SD) | 282.42 (60.89) | 327.61 (143.42) | 342.23 (89.32) | |
| Average response to interventions score (SD) | 3 | 4.52 (0.79) | 4.9 (0.30) | |
| Average social interaction score (SD) | 4.77 (0.95) | 4.30 (1.49) | 4.60 (0.84) | |
| Average sound pressure levels (SPL) | ||||
| Average sound pressure levels, dB(A) | 64.49 | 62.47 | 62.90 | |
| Average sound pressure levels, dB(C) | 67.85 | 65.53 | 66.70 | |
| Difference from baseline, dB(A) | −2.02 | −1.55 | ||
| Difference from baseline, dB(C) | −2.32 | −1.12 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mathiesen, S.L.; Aadal, L.; Uldbæk, M.L.; Astrup, P.; Byrne, D.V.; Wang, Q.J. Music Is Served: How Acoustic Interventions in Hospital Dining Environments Can Improve Patient Mealtime Wellbeing. Foods 2021, 10, 2590. https://doi.org/10.3390/foods10112590
Mathiesen SL, Aadal L, Uldbæk ML, Astrup P, Byrne DV, Wang QJ. Music Is Served: How Acoustic Interventions in Hospital Dining Environments Can Improve Patient Mealtime Wellbeing. Foods. 2021; 10(11):2590. https://doi.org/10.3390/foods10112590
Chicago/Turabian StyleMathiesen, Signe Lund, Lena Aadal, Morten Laulund Uldbæk, Peter Astrup, Derek Victor Byrne, and Qian Janice Wang. 2021. "Music Is Served: How Acoustic Interventions in Hospital Dining Environments Can Improve Patient Mealtime Wellbeing" Foods 10, no. 11: 2590. https://doi.org/10.3390/foods10112590
APA StyleMathiesen, S. L., Aadal, L., Uldbæk, M. L., Astrup, P., Byrne, D. V., & Wang, Q. J. (2021). Music Is Served: How Acoustic Interventions in Hospital Dining Environments Can Improve Patient Mealtime Wellbeing. Foods, 10(11), 2590. https://doi.org/10.3390/foods10112590







