Effects of Milk or Soy Milk Combined with Mild Resistance Exercise on the Muscle Mass and Muscle Strength in Very Old Nursing Home Residents with Sarcopenia
Abstract
:1. Introduction
2. Materials and Methods
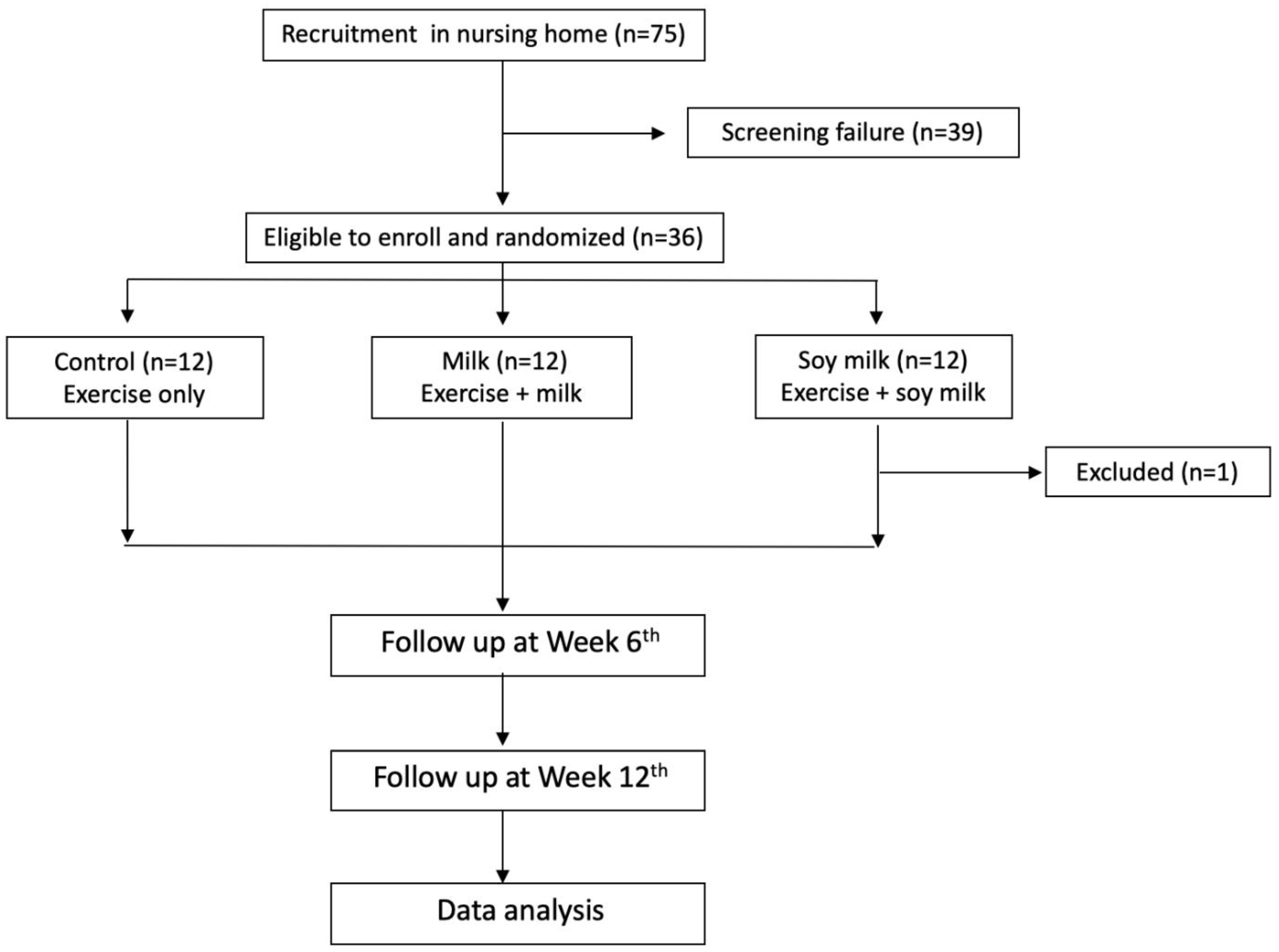
2.1. Study Design and Population
2.2. Data Collection
2.2.1. Sociodemographic Data
2.2.2. Anthropometric, Clinical, and Laboratory Data
2.2.3. Sarcopenic Index
2.2.4. Diet Assessment
2.3. Statistical Analysis
3. Results
3.1. General Characteristics and Clinical Data at the Baseline
3.2. Anthropometric Data and the Sarcopenic Index
3.3. Dietary Intake
4. Discussion
4.1. Nutritional Status and Inflammation Index in Nursing Home Residents
4.2. Effects of Exercise on the Sarcopenic Index
4.3. Effects of Exercise Combined with Milk and Soy Milk Supplementation on the Sarcopenic Index
4.4. Effects of Exercise Combined with Milk and Soy Milk Supplementation on IGF-1
4.5. Strengths and Limitations
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Shafiee, G.; Keshtkar, A.; Soltani, A.; Ahadi, Z.; Larijani, B.; Heshmat, R. Prevalence of sarcopenia in the world: A systematic review and meta- analysis of general population studies. J. Diabetes Metab. Disord. 2017, 16, 21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chien, M.-Y.; Huang, T.-Y.; Wu, Y.-T. Prevalence of Sarcopenia Estimated Using a Bioelectrical Impedance Analysis Prediction Equation in Community-Dwelling Elderly People in Taiwan. J. Am. Geriatr. Soc. 2008, 56, 1710–1715. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Landi, F.; Schneider, S.M.; Zúñiga, C.; Arai, H.; Boirie, Y.; Chen, L.-K.; Fielding, R.A.; Martin, F.C.; Michel, J.-P.; et al. Prevalence of and interventions for sarcopenia in ageing adults: A systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing 2014, 43, 748–759. [Google Scholar] [CrossRef]
- Deutz, N.E.; Bauer, J.M.; Barazzoni, R.; Biolo, G.; Boirie, Y.; Bosy-Westphal, A.; Cederholm, T.; Cruz-Jentoft, A.J.; Krznariç, Z.; Nair, K.S.; et al. Protein intake and exercise for optimal muscle function with aging: Recommendations from the ESPEN Expert Group. Clin. Nutr. 2014, 33, 929–936. [Google Scholar] [CrossRef] [Green Version]
- Daly, R.M.; O’Connell, S.; Mundell, N.L.; Grimes, C.; Dunstan, D.; Nowson, C. Protein-enriched diet, with the use of lean red meat, combined with progressive resistance training enhances lean tissue mass and muscle strength and reduces circulating IL-6 concentrations in elderly women: A cluster randomized controlled trial. Am. J. Clin. Nutr. 2014, 99, 899–910. [Google Scholar] [CrossRef] [PubMed]
- Kukuljan, S.; Nowson, C.A.; Sanders, K.; Daly, R.M. Effects of resistance exercise and fortified milk on skeletal muscle mass, muscle size, and functional performance in middle-aged and older men: An 18-mo randomized controlled trial. J. Appl. Physiol. 2009, 107, 1864–1873. [Google Scholar] [CrossRef] [PubMed]
- Robinson, S.M.; Denison, H.J.; Cooper, C.; Sayer, A.A. Prevention and optimal management of sarcopenia: A review of combined exercise and nutrition interventions to improve muscle outcomes in older people. Clin. Interv. Aging 2015, 10, 859–869. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, L.-K.; Liu, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Bahyah, K.S.; Chou, M.-Y.; Hsu, P.-S.; Krairit, O.; Lee, J.S.; et al. Sarcopenia in Asia: Consensus Report of the Asian Working Group for Sarcopenia. J. Am. Med. Dir. Assoc. 2014, 15, 95–101. [Google Scholar] [CrossRef]
- Cappola, A.R.; Bandeen-Roche, K.; Wand, G.S.; Volpato, S.; Fried, L.P. Association of IGF-I Levels with Muscle Strength and Mobility in Older Women. J. Clin. Endocrinol. Metab. 2001, 86, 4139–4146. [Google Scholar] [CrossRef]
- Kim, J.H.; Choi, S.H.; Lim, S.; Kim, K.W.; Lim, J.-Y.; Cho, N.H.; Park, K.S.; Jang, H.C. Assessment of appendicular skeletal muscle mass by bioimpedance in older community-dwelling Korean adults. Arch. Gerontol. Geriatr. 2013, 58, 303–307. [Google Scholar] [CrossRef]
- Holick, M.F. Vitamin D Deficiency. N. Engl. J. Med. 2007, 357, 266–281. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.; McKechnie, T.; Doumouras, A.G.; Handler, C.; Eskicioglu, C.; Gmora, S.; Anvari, M.; Hong, D. Diagnostic Value of C-Reactive Protein Levels in Postoperative Infectious Complications After Bariatric Surgery: A Systematic Review and Meta-Analysis. Obes. Surg. 2019, 29, 2022–2029. [Google Scholar] [CrossRef]
- Johns, I.; Moschonas, K.E.; Medina, J.; Ossei-Gerning, N.; Kassianos, G.; Halcox, J.P. Risk classification in primary prevention of CVD according to QRISK2 and JBS3 ‘heart age’, and prevalence of elevated high-sensitivity C reactive protein in the UK cohort of the EURIKA study. Open Heart 2018, 5, e000849. [Google Scholar] [CrossRef] [Green Version]
- Arnold, L.W.; Hoy, W.E.; Sharma, S.; Wang, Z. The Association between HbA1c and Cardiovascular Disease Markers in a Remote Indigenous Australian Community with and without Diagnosed Diabetes. J. Diabetes Res. 2016, 2016, 5342304. [Google Scholar] [CrossRef] [Green Version]
- Bidlingmaier, M.; Friedrich, N.; Emeny, R.T.; Spranger, J.; Wolthers, O.D.; Roswall, J.; Körner, A.; Obermayer-Pietsch, B.; Hübener, C.; Dahlgren, J.; et al. Reference Intervals for Insulin-like Growth Factor-1 (IGF-I) From Birth to Senescence: Results from a Multicenter Study Using a New Automated Chemiluminescence IGF-I Immunoassay Conforming to Recent International Recommendations. J. Clin. Endocrinol. Metab. 2014, 99, 1712–1721. [Google Scholar] [CrossRef] [PubMed]
- Chang, C.-J.; Wu, C.-H.; Yao, W.-J.; Yang, Y.-C.; Wu, J.-S.; Lu, F.-H. Low body mass index but high percent body fat in Taiwanese subjects: Implications of obesity cutoffs. Int. J. Obes. 2003, 27, 253–259. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.-P.; Rolland, Y.; Schneider, S.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European Working Group on Sarcopenia in Older People. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef] [Green Version]
- Chen, C.-H.; Liu, L.-K.; Chen, M.-J.; Lee, W.-J.; Lin, M.-H.; Peng, L.-N.; Chen, L.-K. Associations between vitamin D deficiency, musculoskeletal health, and cardiometabolic risk among community-living people in Taiwan: Age and sex-specific relationship. Medicine (Baltimore). Medicine 2018, 97, e13886. [Google Scholar] [CrossRef]
- Thacher, T.D.; Clarke, B.L. Vitamin D Insufficiency. Mayo Clin. Proc. 2011, 86, 50–60. [Google Scholar] [CrossRef] [Green Version]
- Lips, P. Vitamin D Deficiency and Secondary Hyperparathyroidism in the Elderly: Consequences for Bone Loss and Fractures and Therapeutic Implications. Endocr. Rev. 2001, 22, 477–501. [Google Scholar] [CrossRef]
- Visser, M.; Deeg, D.J.H.; Lips, P.; Longitudinal Aging Study Amsterdam. Low Vitamin D and High Parathyroid Hormone Levels as Determinants of Loss of Muscle Strength and Muscle Mass (Sarcopenia): The Longitudinal Aging Study Amsterdam. J. Clin. Endocrinol. Metab. 2003, 88, 5766–5772. [Google Scholar] [CrossRef]
- Halfon, M.; Phan, O.; Teta, D. Vitamin D: A Review on Its Effects on Muscle Strength, the Risk of Fall, and Frailty. BioMed Res. Int. 2015, 2015, 953241. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miller, J.W.; Harvey, D.J.; Beckett, L.A.; Green, R.; Farias, S.T.; Reed, B.R.; Olichney, J.M.; Mungas, D.M.; DeCarli, C. Vitamin D Status and Rates of Cognitive Decline in a Multiethnic Cohort of Older Adults. JAMA Neurol. 2015, 72, 1295–1303. [Google Scholar] [CrossRef]
- Pilz, S.; Gaksch, M.; Kienreich, K.; Grübler, M.R.; Verheyen, N.; Fahrleitner-Pammer, A.; Treiber, G.; Drechsler, C.; Hartaigh, B.; Obermayer-Pietsch, B.; et al. Effects of Vitamin D on Blood Pressure and Cardiovascular Risk Factors: A randomized controlled trial. Hypertension 2015, 65, 1195–1201. [Google Scholar] [CrossRef]
- Scragg, R.; Sowers, M.; Bell, C. Serum 25-hydroxyvitamin D, Ethnicity, and Blood Pressure in the Third National Health and Nutrition Examination Survey. Am. J. Hypertens. 2007, 20, 713–719. [Google Scholar] [CrossRef]
- Rogeri, P.S.; Gasparini, S.O.; Martins, G.L.; Costa, L.K.F.; Araujo, C.C.; Lugaresi, R.; Kopfler, M.; Lancha, A.H.J. Crosstalk Between Skeletal Muscle and Immune System: Which Roles Do IL-6 and Glutamine Play? Front. Physiol. 2020, 11, 582258. [Google Scholar] [CrossRef] [PubMed]
- Fantuzzi, G. Adipose tissue, adipokines, and inflammation. J. Allergy Clin. Immunol. 2005, 115, 911–919. [Google Scholar] [CrossRef]
- Cesari, M.; Kritchevsky, S.B.; Baumgartner, R.N.; Atkinson, H.H.; Penninx, B.W.; Lenchik, L.; Palla, S.L.; Ambrosius, W.T.; Tracy, R.P.; Pahor, M. Sarcopenia, obesity, and inflammation—Results from the Trial of Angiotensin Converting Enzyme Inhibition and Novel Cardiovascular Risk Factors study. Am. J. Clin. Nutr. 2005, 82, 428–434. [Google Scholar] [CrossRef] [PubMed]
- Calçada, D.; Vianello, D.; Giampieri, E.; Sala, C.; Castellani, G.; de Graaf, A.; Kremer, B.; van Ommen, B.; Feskens, E.; Santoro, A.; et al. The role of low-grade inflammation and metabolic flexibility in aging and nutritional modulation thereof: A systems biology approach. Mech. Ageing Dev. 2014, 136–137, 138–147. [Google Scholar] [CrossRef]
- Fiatarone, M.A.; O’Neill, E.F.; Ryan, N.D.; Clements, K.M.; Solares, G.R.; Nelson, M.E.; Roberts, S.B.; Kehayias, J.J.; Lipsitz, L.A.; Evans, W.J. Exercise Training and Nutritional Supplementation for Physical Frailty in Very Elderly People. N. Engl. J. Med. 1994, 330, 1769–1775. [Google Scholar] [CrossRef] [Green Version]
- Rosendahl, E.; Lindelöf, N.; Littbrand, H.; Yifter-Lindgren, E.; Lundin-Olsson, L.; Håglin, L.; Gustafson, Y.; Nyberg, L. High-intensity functional exercise program and proteinenriched energy supplement for older persons dependent in activities of daily living: A randomised controlled trial. Aust. J. Physiother. 2006, 52, 105–113. [Google Scholar] [CrossRef] [Green Version]
- Waters, D. Advantages of dietary, exercise-related, and therapeutic interventions to prevent and treat sarcopenia in adult patients: An update. Clin. Interv. Aging 2010, 5, 259–270. [Google Scholar] [CrossRef] [Green Version]
- Kim, H.K.; Suzuki, T.; Saito, K.; Yoshida, H.; Kobayashi, H.; Kato, H.; Katayama, M. Effects of Exercise and Amino Acid Supplementation on Body Composition and Physical Function in Community-Dwelling Elderly Japanese Sarcopenic Women: A Randomized Controlled Trial. J. Am. Geriatr. Soc. 2011, 60, 16–23. [Google Scholar] [CrossRef] [PubMed]
- Chen, L.-K.; Woo, J.; Assantachai, P.; Auyeung, T.-W.; Chou, M.-Y.; Iijima, K.; Jang, H.C.; Kang, L.; Kim, M.; Kim, S.; et al. Asian Working Group for Sarcopenia: 2019 Consensus Update on Sarcopenia Diagnosis and Treatment. J. Am. Med. Dir. Assoc. 2020, 21, 300–307.e2. [Google Scholar] [CrossRef]
- Rolland, Y.; Lauwers-Cances, V.; Cournot, M.; NourhashãMi, F.; Reynish, W.; Riviãre, D.; Vellas, B.; Grandjean, H. Sarcopenia, Calf Circumference, and Physical Function of Elderly Women: A Cross-Sectional Study. J. Am. Geriatr. Soc. 2003, 51, 1120–1124. [Google Scholar] [CrossRef] [PubMed]
- Landi, F.; Onder, G.; Russo, A.; Liperoti, R.; Tosato, M.; Martone, A.M.; Capoluongo, E.; Bernabei, R. Calf circumference, frailty and physical performance among older adults living in the community. Clin. Nutr. 2013, 33, 539–544. [Google Scholar] [CrossRef]
- Bonnefoy, M.; Cornu, C.; Normand, S.; Boutitie, F.; Bugnard, F.; Rahmani, A.; Lacour, J.R.; Laville, M. The effects of exercise and protein–energy supplements on body composition and muscle function in frail elderly individuals: A long-term controlled randomised study. Br. J. Nutr. 2003, 89, 731–738. [Google Scholar] [CrossRef]
- Singh, M.A.F.; Ding, W.; Manfredi, T.J.; Solares, G.S.; O’Neill, E.F.; Clements, K.M.; Ryan, N.D.; Kehayias, J.J.; Fielding, R.A.; Evans, W.J. Insulin-like growth factor I in skeletal muscle after weight-lifting exercise in frail elders. Am. J. Physiol. Metab. 1999, 277, E135–E143. [Google Scholar] [CrossRef] [PubMed]
- De Jong, N.; A Paw, M.J.C.; De Groot, L.C.; Hiddink, G.J.; A Van Staveren, W. Dietary supplements and physical exercise affecting bone and body composition in frail elderly persons. Am. J. Public Heal. 2000, 90, 947–954. [Google Scholar] [CrossRef] [Green Version]
- Beaudart, C.; the IOF-ESCEO Sarcopenia Working Group; Dawson, A.; Shaw, S.C.; Harvey, N.; Kanis, J.A.; Binkley, N.; Reginster, J.Y.; Chapurlat, R.; Chan, D.C.; et al. Nutrition and physical activity in the prevention and treatment of sarcopenia: Systematic review. Osteoporos. Int. 2017, 28, 1817–1833. [Google Scholar] [CrossRef] [Green Version]
- Loenneke, J.P.; Loprinzi, P.D.; Murphy, C.H.; Phillips, S. Per meal dose and frequency of protein consumption is associated with lean mass and muscle performance. Clin. Nutr. 2016, 35, 1506–1511. [Google Scholar] [CrossRef] [PubMed]
- Khalil, D.A.; Lucas, E.A.; Juma, S.; Smith, B.J.; Payton, M.E.; Arjmandi, B.H. Soy Protein Supplementation Increases Serum Insulin-Like Growth Factor-I in Young and Old Men but Does Not Affect Markers of Bone Metabolism. J. Nutr. 2002, 132, 2605–2608. [Google Scholar] [CrossRef] [Green Version]
- Borst, S.E.; De Hoyos, D.V.; Garzarella, L.; Vincent, K.; Pollock, B.H.; Lowenthal, D.T.; Pollock, M.L. Effects of resistance training on insulin-like growth factor-I and IGF binding proteins. Med. Sci. Sports Exerc. 2001, 33, 648–653. [Google Scholar] [CrossRef] [Green Version]
- Nicklas, B.J.; Ryan, A.J.; Treuth, M.M.; Harman, S.M.; Blackman, M.R.; Hurley, B.F.; A Rogers, M. Testosterone, Growth Hormone and IGF-I Responses to Acute and Chronic Resistive Exercise in Men Aged 55–70 Years. Int. J. Sports Med. 1995, 16, 445–450. [Google Scholar] [CrossRef]
- Pyka, G.; Taaffe, D.; Marcus, R. Effect of a Sustained Program of Resistance Training on the Acute Growth Hormone Response to Resistance Exercise in Older Adults. Horm. Metab. Res. 1994, 26, 330–333. [Google Scholar] [CrossRef] [PubMed]
- Berg, U.; Bang, P. Exercise and Circulating Insulin-Like Growth Factor I. Horm. Res. Paediatr. 2004, 62 (Suppl. 1), 50–58. [Google Scholar] [CrossRef] [PubMed]
- Frystyk, J. Exercise and the Growth Hormone-Insulin-Like Growth Factor Axis. Med. Sci. Sports Exerc. 2010, 42, 58–66. [Google Scholar] [CrossRef] [PubMed]
| Variable | Control (n = 12) | Milk (n = 12) | Soy Milk (n = 11) | p2 |
|---|---|---|---|---|
| Mean ± SD or n (%) | ||||
| Demographic data | ||||
| Gender | 0.5528 | |||
| Male, n (%) | 9 (75) | 11 (92) | 9 (82) | |
| Female, n (%) | 3 (25) | 1 (8) | 2 (18) | |
| Age (years) | 84.67 ± 7.5 | 85.25 ± 5.38 | 85 ± 5.62 | 0.9741 |
| Medical history | ||||
| CVD (n) | 9 | 9 | 8 | 0.9899 |
| COPD (n) | 5 | 6 | 6 | 0.8204 |
| DM (n) | 9 | 8 | 8 | 0.8970 |
| CKD (n) | 10 | 8 | 10 | 0.3271 |
| Dementia (n) | 11 | 11 | 8 | 0.3313 |
| Variable | Control (n = 12) | Milk (n = 12) | Soy Milk (n = 11) | p2 | |||||
|---|---|---|---|---|---|---|---|---|---|
| Mean ± SD or n (%) | Time | Treatment | Time × Treatment | ||||||
| Liver function | Baseline | Week 12 | Baseline | Week 12 | Baseline | Week 12 | |||
| ALT (U/L) | 12.2 ± 2.9 | 11.67 ± 3.5 | 15.3 ± 7.0 | 13.08 ± 4.8 | 10.8 ± 4.1 | 41.18 ± 99.0 | 0.3317 | 0.4293 | 0.2888 |
| Kidney function | |||||||||
| Creatinine (mg/dL) | 1.06 ± 0.35 | 1.0 ± 0.3 | 1.1 ± 0.4 | 1.07 ± 0.36 | 1.1 ± 0.3 | 1.05 ± 0.2 | 0.5524 | 0.8294 | 0.9873 |
| Nutritional status | |||||||||
| Prealbumin (mg/dL) | 19.3 ± 4.8 | 17.73 ± 6.3 | 20.4 ± 5.6 | 19.15 ± 3.8 | 22.3 ± 6.8 | 22.76 ± 6.2 | 0.5622 | 0.0527 | 0.8049 |
| 25-hydroxyvitamin D (ng/mL) | 14.0 ± 7.0 | 11.85 ± 6.8 | 20.8 ± 8.6 | 17.96 ± 7.7 | 21.1 ± 7.8 | 17.13 ± 6.8 | 0.1003 | 0.606 | 0.9161 |
| Inflammation index | |||||||||
| hsCRP (mg/dL) | 0.7 ± 1.0 | 1.16 ± 1.64 | 0.7 ± 1.1 | 1.43 ± 2.2 | 1.3 ± 3.1 | 1.28 ± 1.79 | 0.3984 | 0.8115 | 0.7963 |
| Insulin resistance index | |||||||||
| FBS (mg/dL) | 83.7 ± 13.3 | 93 ± 20.6 | 93.3 ± 27.4 | 98 ± 40.6 | 108.6 ± 49.7 | 101.45 ± 22.96 | 0.7619 | 0.1993 | 0.6548 |
| Insulin (mIU/L) | 6.1 ± 4.9 | 6.9 ± 7.7 | 6.1 ± 4.2 | 6.1 ± 3.47 | 5.3 ± 2.2 | 8.0 ± 6.4 | 0.3628 | 0.9351 | 0.6632 |
| HbA1c (%) | 5.76 ± 0.43 | 5.68 ± 0.44 | 6.01 ± 1.24 | 5.93 ± 1.01 | 6.43 ± 1.28 | 6.08 ± 0.59 | 0.4341 | 0.1374 | 0.8410 |
| HOMA-IR | 1.31 ± 1.1 | 1.91 ± 3.05 | 1.37 ± 0.87 | 1.40 ± 0.73 | 1.39 ± 0.72 | 2.20 ± 2.09 | 0.2343 | 0.7048 | 0.7321 |
| Hormonal factor | |||||||||
| IGF-1 (mg/dL) | 73.3 ± 22.0 | 68.6 ± 28.1 | 92.7 ± 26.8 | 89.4 ± 34.4 | 103.0 ± 44.0 | 112.3 ± 49.7 # | 0.9587 | 0.003 | 0.7589 |
| Control (n = 12) | Milk (n = 12) | Soy Milk (n = 11) | p2 | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Baseline | Week 6 | Week 12 | Baseline | Week 6 | Week 12 | Baseline | Week 6 | Week 12 | Time | Treatment | Time × Treatment | |
| Anthropometric data | ||||||||||||
| BW (kg) | 56.2 ± 8.6 | 54.7 ± 11.9 | 56.7 ± 8.4 | 58.3 ± 9.1 | 59.2 ± 9.1 | 59.7 ± 9 | 55.4 ± 8.7 | 55.2 ± 9.2 | 56.4 ± 9.1 | 0.9436 | 0.2345 | 0.9953 |
| BMI (kg/m2) | 22.1 ± 2.4 | 21.5 ± 4.1 | 22.3 ± 2.3 | 22.1 ± 3.2 | 22.4 ± 3.0 | 22.6 ± 3.1 | 22.6 ± 2.2 | 22.6 ± 2.7 | 23.1 ± 2.5 | 0.7484 | 0.5169 | 0.9893 |
| Body fat (%) | 30.6 ± 8.6 | 29.9 ± 9.1 | 31.7 ± 8.8 | 32.7 ± 5.6 | 29.3 ± 7.7 | 30.9 ± 6. | 32.3 ± 6.5 | 32.4 ± 8.1 | 32.8 ± 7.7 | 0.7157 | 0.5801 | 0.9337 |
| Sarcopenic index | ||||||||||||
| ASMI (kg/m2) 3 | 6.1 ± 0.6 | 6.0 ± 0.6 | 6.0 ± 0.7 | 6.2 ± 0.5 | 6.2 ± 0.61 | 6.0 ± 0.6 | 6.0 ± 0.7 | 6.1 ± 0.7 | 6.1 ± 0.7 | 0.8800 | 0.7997 | 0.9244 |
| CC (cm) | 30.8 ± 2.5 | 31.2 ± 2.2 | 31.5 ± 2.0 * | 30.7 ± 2.6 | 30.6 ± 2.32 | 30.9 ± 2.5 | 31.3 ± 2.1 | 31.6 ± 2.0 | 32.3 ± 1.7 * | 0.4843 | 0.1788 | 0.9784 |
| HG (kg) | 17.4 ± 5.3 | 17.6 ± 5.4 | 19.1 ± 5.6 | 18.7 ± 6.2 | 19.2 ± 5.62 | 21.2 ± 6.4 * | 18.6 ± 6.8 | 19.5 ± 5.6 | 21.0 ± 6.1 * | 0.2716 | 0.3985 | 0.9990 |
| GS (m/s) | 0.6 ± 0.3 | 0.6 ± 0.3 | 0.7 ± 0.3 * | 0.4 ± 0.2 | 0.4 ± 0.22 | 0.4 ± 0.2 | 0.4 ± 0.2 | 0.4 ± 0.2 | 0.5 ± 0.3 | 0.5059 | 0.3504 | 0.9399 |
| Stage of Sarcopenia | Control (n = 12) | Milk (n = 12) | Soy Milk (n = 11) | |||
|---|---|---|---|---|---|---|
| Baseline | Week 12 | Baseline | Week 12 | Baseline | Week 12 | |
| Pre-sarcopenia (n, %) | 0 (0%) | 1 (8%) | 0 (0%) | 0 | 0 | 1 (9%) |
| Sarcopenia (n, %) | 3 (25%) | 9 (75%) | 3 (25%) | 4 (33%) | 2 (18%) | 4 (36%) |
| Severe sarcopenia (n, %) | 9 (75%) | 2 (17%) | 9 (75%) | 8 (67%) | 9 (82%) | 6 (55%) |
| p2 | 0.0146 | NA | 0.322 | |||
| Control (n = 12) | Milk (n = 11) | Soy Milk (n = 12) | p2 | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Nutrients | Baseline | Week 12 | Baseline | Week 12 | Baseline | Week 12 | Time | Treatment | Time × Treatment |
| Energy (kcal/day) | 1677 ± 319 | 1714 ± 252 | 1857 ± 195 | 1881 ± 204 | 1845 ± 219 | 1898 ± 247 | 0.5176 | 0.0235 | 0.9796 |
| CHO (g/day) | 225 ± 52 | 225 ± 43 | 256 ± 35 | 241 ± 41 | 251 ± 44 | 247 ± 30 | 0.4631 | 0.1158 | 0.8612 |
| Protein (g/day) | 70.3 ± 11.9 | 74.7 ± 15.4 | 76.4 ± 9.5 | 77.3 ± 3.2 | 76.1 ± 7.9 | 77.7 ± 7.9 | 0.3453 | 0.2413 | 0.8230 |
| Fat (g/day) | 54.8 ± 10.7 | 55.8 ± 11.2 | 59.5 ± 8.8 | 61.5 ± 11.6 | 60.6 ± 7.9 | 61.4 ± 7.6 | 0.5889 | 0.0950 | 0.9750 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chiang, F.-Y.; Chen, J.-R.; Lee, W.-J.; Yang, S.-C. Effects of Milk or Soy Milk Combined with Mild Resistance Exercise on the Muscle Mass and Muscle Strength in Very Old Nursing Home Residents with Sarcopenia. Foods 2021, 10, 2581. https://doi.org/10.3390/foods10112581
Chiang F-Y, Chen J-R, Lee W-J, Yang S-C. Effects of Milk or Soy Milk Combined with Mild Resistance Exercise on the Muscle Mass and Muscle Strength in Very Old Nursing Home Residents with Sarcopenia. Foods. 2021; 10(11):2581. https://doi.org/10.3390/foods10112581
Chicago/Turabian StyleChiang, Feng-YI, Jiun-Rong Chen, Wei-Ju Lee, and Suh-Ching Yang. 2021. "Effects of Milk or Soy Milk Combined with Mild Resistance Exercise on the Muscle Mass and Muscle Strength in Very Old Nursing Home Residents with Sarcopenia" Foods 10, no. 11: 2581. https://doi.org/10.3390/foods10112581
APA StyleChiang, F.-Y., Chen, J.-R., Lee, W.-J., & Yang, S.-C. (2021). Effects of Milk or Soy Milk Combined with Mild Resistance Exercise on the Muscle Mass and Muscle Strength in Very Old Nursing Home Residents with Sarcopenia. Foods, 10(11), 2581. https://doi.org/10.3390/foods10112581





