Pediatricians’ Knowledge of Emergency Management of Dental Injuries and Use of Mouthguards: A Cross-Sectional Survey
Abstract
1. Introduction
2. Materials and Methods
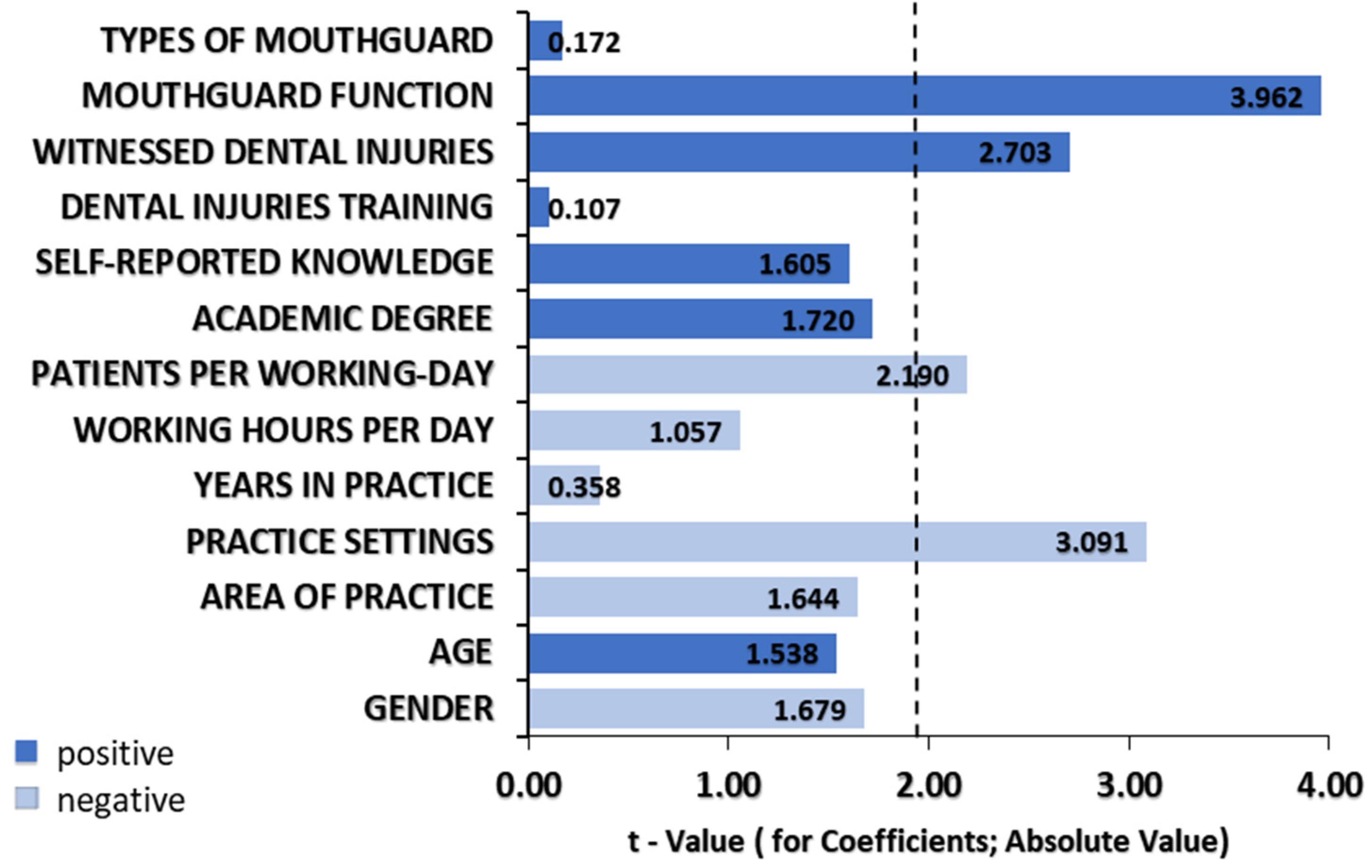
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Glendor, U. Epidemiology of traumatic dental injuries-a 12 year review of the literature. Dent. Traumatol. 2008, 24, 603–611. [Google Scholar] [CrossRef]
- Glendor, U.; Halling, A.; Andersson, L.; Eilert-Petersson, E. Incidence of traumatic tooth injuries in children and adolescents in the county of Vastmanland, Sweden. Swed. Dent. J. 1996, 20, 15–28. [Google Scholar] [PubMed]
- Cotti, E.; Mereu, M.; Lusso, D. Regenerative treatment of an immature, traumatized tooth with apical periodontitis: Report of a case. J. Endod. 2008, 34, 611–616. [Google Scholar] [CrossRef] [PubMed]
- Bakland, L.K.; Andreasen, J.O. Examination of the dentally traumatized patient. J. Calif. Dent. Assoc. 1996, 24, 35–37, 40–44. [Google Scholar]
- El-Kalla, I.H.; Shalan, H.M.; Bakr, R.A. Impact of Dental Trauma on Quality of Life among 11–14 Years Schoolchildren. Contemp. Clin. Dent. 2017, 8, 538–544. [Google Scholar] [CrossRef] [PubMed]
- Kaczmarek, U.; Gozdowski, D.; Olczak-Kowalczyk, D. Prevalence of traumatic dental injuries in Polish 15-year-olds. Dent. Med. Probl. 2019, 56, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Yigit, Y.; Helvacioglu-Yigit, D.; Kan, B.; Ilgen, C.; Yilmaz, S. Dentofacial traumatic injuries: A survey of knowledge and attitudes among emergency medicine physicians in Turkey. Dent. Traumatol. 2019, 35, 20–26. [Google Scholar] [CrossRef]
- Krol, D.M. Educating pediatricians on children’s oral health: Past, present, and future. Pediatrics 2004, 113, e487–e492. [Google Scholar] [CrossRef]
- Alrashdi, M.; Limaki, M.E.; Alrashidi, A. Oral Health Knowledge Gaps and Their Impact on the Role of Pediatricians: A Multicentric Study. Int. J. Environ. Res. Public Health 2021, 18, 10237. [Google Scholar] [CrossRef] [PubMed]
- Hadjipanayis, A.; Grossman, Z.; Del Torso, S.; Michailidou, K.; Van Esso, D.; Cauwels, R. Oral health training, knowledge, attitudes and practices of primary care paediatricians: A European survey. Eur. J. Pediatr. 2018, 177, 675–681. [Google Scholar] [CrossRef] [PubMed]
- Dickson-Swift, V.; Kenny, A.; Gussy, M.; McCarthy, C.; Bracksley-O’Grady, S. The knowledge and practice of pediatricians in children’s oral health: A scoping review. BMC Oral Health 2020, 20, 211. [Google Scholar] [CrossRef]
- Tewari, N.; Jonna, I.; Mathur, V.P.; Goel, S.; Ritwik, P.; Rahul, M.; Haldar, P.; Bansal, K.; Pandey, R.M. Global status of knowledge for the prevention and emergency management of traumatic dental injuries among non-dental healthcare professionals: A systematic review and meta-analysis. Injury 2021, 52, 2025–2037. [Google Scholar] [CrossRef] [PubMed]
- Nikolic, H.; Ivancic Jokic, N.; Bakarcic, D.; Hrvatin, S.; Jakljevic, N. Knowledge about emergency procedure in case of dental trauma among paediatricians in Croatia. Eur. J. Paediatr. Dent. 2018, 19, 277–281. [Google Scholar] [CrossRef]
- Yeng, T.; O’Sullivan, A.J.; Shulruf, B. Medical doctors’ knowledge of dental trauma management: A review. Dent. Traumatol. 2020, 36, 100–107. [Google Scholar] [CrossRef] [PubMed]
- Chanchala, H.P.; Shanbhog, R.; Ravi, M.D.; Raju, V. Pediatrician’s perspectives on dental trauma management: A cross-sectional survey. J. Indian Assoc. Public Health Dent. 2016, 14, 419–423. [Google Scholar] [CrossRef]
- Bahammam, L.A. Knowledge and attitude of emergency physician about the emergency management of tooth avulsion. BMC Oral Health 2018, 18, 57. [Google Scholar] [CrossRef]
- Ulusoy, A.T.; Onder, H.; Cetin, B.; Kaya, S. Knowledge of medical hospital emergency physicians about the first-aid management of traumatic tooth avulsion. Int. J. Paediatr. Dent. 2012, 22, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Goyal, A.; Nishant, A.; Morankar, R.; Gauba, K.; Jaiswal, M. Awareness among pediatricians regarding oral health care in children including those with special health care needs: A cross-sectional survey. J. Fam. Med. Prim. Care. 2020, 9, 4151–4155. [Google Scholar] [CrossRef]
- Croatian Health Statistics Yearbook 2019. Zagreb: Croatian Institute of Public Health, 2020. Available online: https://www.hzjz.hr/wp-content/uploads/2021/02/Ljetopis_Yerabook_2019.pdf (accessed on 27 November 2021).
- Yeng, T.; Parashos, P. Dentists’ management of dental injuries and dental trauma in Australia: A review. Dent Traumatol. 2008, 24, 268–271. [Google Scholar] [CrossRef] [PubMed]
- Domnich, A.; Panatto, D.; Arata, L.; Bevilacqua, I.; Apprato, L.; Gasparini, R.; Amicizia, D. Impact of different scoring algorithms applied to multiple-mark survey items on outcome assessment: An in-field study on health-related knowledge. J. Prev. Med. Hyg. 2015, 56, E162–E171. [Google Scholar]
- Bloom, B.S. Learning for mastery. Instruction and curriculum. Regional education laboratory for the Carolinas and Virginia. Eval. Comment 1968, 1, n2. [Google Scholar]
- Flores, M.T.; Malmgren, B.; Andersson, L.; Andreasen, J.O.; Bakland, L.K.; Barnett, F.; Bourguignon, C.; DiAngelis, A.; Hicks, L.; Sigurdsson, A.; et al. Guidelines for the management of traumatic dental injuries. III. Primary teeth. Dent. Traumatol. 2007, 23, 196–202. [Google Scholar] [CrossRef] [PubMed]
- Needleman, H.L.; Stucenski, K.; Forbes, P.W.; Chen, Q.; Stack, A.M. Massachusetts emergency departments’ resources and physicians’ knowledge of management of traumatic dental injuries. Dent. Traumatol. 2013, 29, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Trivedy, C.; Kodate, N.; Ross, A.; Al-Rawi, H.; Jaiganesh, T.; Harris, T.; Anderson, J.E. The attitudes and awareness of emergency department (ED) physicians towards the management of common dentofacial emergencies. Dent. Traumatol. 2012, 28, 121–126. [Google Scholar] [CrossRef] [PubMed]
- Diaz, J.; Bustos, L.; Herrera, S.; Sepulveda, J. Knowledge of the management of paediatric dental traumas by non-dental professionals in emergency rooms in South Araucania, Temuco, Chile. Dent. Traumatol. 2009, 25, 611–619. [Google Scholar] [CrossRef]
- Fouad, A.F.; Abbott, P.V.; Tsilingaridis, G.; Cohenca, N.; Lauridsen, E.; Bourguignon, C.; O’Connell, A.; Flores, M.T.; Day, P.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2020, 36, 331–342. [Google Scholar] [CrossRef] [PubMed]
- Aren, A.; Erdem, A.P.; Aren, G.; Şahin, Z.D.; Güney Tolgay, C.; Çayırcı, M.; Sepet, E.; Güloğlu, R.; Yanar, H.; Sarıbeyoğlu., K. Importance of knowledge of the management of traumatic dental injuries in emergency departments. Ulus Travma Acil Cerrahi Derg 2018, 24, 136–144. [Google Scholar] [CrossRef] [PubMed]
- Adnan, S.; Lone, M.M.; Khan, F.R.; Hussain, S.M.; Nagi, S.E. Which is the most recommended medium for the storage and transport of avulsed teeth? A systematic review. Dent. Traumatol. 2018, 34, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Krishna, A.; Malur, M.H.; Swapna, D.V.; Benjamin, S.; Deepak, C.A. Traumatic dental injury-an enigma for adolescents: A series of case reports. Case Rep. Dent. 2012, 2012, 756526. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bourguignon, C.; Cohenca, N.; Lauridsen, E.; Flores, M.T.; O’Connell, A.C.; Day, P.F.; Tsilingaridis, G.; Abbott, P.V.; Fouad, A.F.; Hicks, L.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 1. Fractures and luxations. Dent. Traumatol. 2020, 36, 314–330. [Google Scholar] [CrossRef]
- Green, J.I. The Role of Mouthguards in Preventing and Reducing Sports-related Trauma. Prim. Dent. J. 2017, 16, 27–34. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, L.M.; Neto, J.C.L.; Lima, T.F.R.; Magno, M.B.; Santiago, B.M.; Cavalcanti, Y.W.; de Almeida, L.F.D. The use of mouthguards and prevalence of dento-alveolar trauma among athletes: A systematic review and meta-analysis. Dent. Traumatol. 2019, 35, 54–72. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Social Welfare of the Republic of Croatia. Rulebook on Specialist Training of Doctor of Medicine Addendum II. Pediatrician. Zagreb: Narodne Novine; 2011. Available online: https://narodne-novine.nn.hr/clanci/sluzbeni/full/2011_09_100_2057.html (accessed on 30 April 2021).
- Douglass, A.B.; Douglass, J.M.; Krol, D.M. Educating paediatricians and family physicians in children’s oral health. Acad. Pediatr. 2009, 9, 452–456. [Google Scholar] [CrossRef] [PubMed]
- Herndon, J.B.; Tomar, S.L.; Catalanotto, F.A. Effect of training paediatricians and family physicians in Early Childhood Caries prevention. J. Pediatr. 2015, 166, 1055–1061. [Google Scholar] [CrossRef] [PubMed]
- Alshunaiber, R.; Alzaid, H.; Meaigel, S.; Aldeeri, A.; Adlan, A. Early childhood caries and infant’s oral health; pediatricians’ and family physicians’ practice, knowledge and attitude in Riyadh city, Saudi Arabia. Saudi Dent. J. 2019, 31, S96–S105. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Total n (%) | Knowledge Score Mean ± SD | p Value | |
|---|---|---|---|---|
| Gender | Male | 78 (41.9) | 3.9 ± 1.4 | 0.016 * |
| Female | 108 (58.1) | 3.4 ± 1.6 | ||
| Age group (years) | 25–35 | 34 (18.3) | 3.1 ± 1.6 | 0.224 |
| 36–45 | 46 (24.7) | 3.6 ± 1.5 | ||
| 46–55 | 56 (30.1) | 3.6 ± 1.5 | ||
| ≥55 | 50 (26.9) | 3.8 ± 1.5 | ||
| Academic degree | Doctor of Medicine | 123 (66.1) | 3.5 ± 1.5 | 0.738 |
| Master of Science | 38 (20.4) | 3.6 ± 1.5 | ||
| Doctor of Philosophy | 25 (13.4) | 3.8 ± 1.7 | ||
| Area of practice | Northern—Croatia | 60 (32.3) | 3.5 ± 1.6 | 0.105 |
| Eastern—Croatia | 13 (7.0) | 3.9 ± 1.1 | ||
| Southern—Croatia | 73 (39.2) | 3.8 ± 1.5 | ||
| Western—Croatia | 40 (21.5) | 3.2 ± 1.5 | ||
| Practice setting | Primary care | 92 (49.5) | 3.6 ± 1.5 | 0.086 |
| Secondary care | 43(23.1) | 3.9 ± 1.6 | ||
| Tertiary care | 51 (27.4) | 3.2 ± 1.4 | ||
| Number of years in practice | 1–10 | 78 (41.9) | 3.3 ± 1.5 a | 0.027 * |
| 11–20 | 57 (30.6) | 3.9 ± 1.6 a | ||
| ≥21 | 51 (27.4) | 3.6 ± 1.4 | ||
| Number of hours worked per workday | 1–4 | 2 (1.1) | 2.5 ± 0.7 | 0.561 |
| 4–8 | 113 (60.8) | 3.6 ± 1.4 | ||
| ≥8 | 71 (38.2) | 3.5 ± 1.7 | ||
| Number of patients seen in a workday | <10 | 14 (7.5) | 3.7 ± 1.7 | 0.368 |
| 10–20 | 112 (60.2) | 3.6 ± 1.5 | ||
| 21–50 | 35 (18.8) | 3.7 ± 1.5 | ||
| >50 | 25 (13.4) | 3.1 ± 1.7 | ||
| Question | Answer | Total n (%) |
|---|---|---|
| Can avulsed primary tooth be replanted? | No | 75 (40.3) |
| I do not know | 90 (48.4) | |
| Yes | 21 (11.3) | |
| Can avulsed permanent tooth be replanted? | Yes | 110 (59.1) |
| I do not know | 13 (7.0) | |
| No | 63 (33.9) | |
| During reimplantation, how would you hold an avulsed permanent tooth? | By the crown | 59 (31.7) |
| By the root | 31 (16.7) | |
| By the whole tooth | 20 (10.8) | |
| I do not know | 74 (39.8) | |
| If the avulsed permanent tooth was unable to be replanted, how would you store it until till reach the dentist? | Special tissue culture solutions | 16 (8.6) |
| Saliva—mouth of child | 8 (4.3) | |
| Milk | 32 (17.2) | |
| Saline solution | 120 (64.5) | |
| Disinfection solutions | 0 (0) | |
| Tap water | 0 (0) | |
| Handkerchief | 5 (2.7) | |
| Alcohol | 3 (1.6) | |
| Ice | 2 (1.1) | |
| What is the ideal time to seek professional assistance in the case of permanent tooth avulsion? | Immediately, within the first 30 min from the injuries | 28 (15.1) |
| Within a few hours | 83 (44.6) | |
| Within 24 h | 45 (24.2) | |
| Next day | 3 (1.6) | |
| Within few next days | 1 (0.5) | |
| There are no limited restrictions | 2 (1.1) | |
| I do not know | 24 (12.9) | |
| What is the best immediate treatment for an avulsed permanent tooth at site of accident? | Wash the tooth with water and put it back into the socket | 54 (29.0) |
| Wash the tooth with disinfection solution and put it back into the socket | 16 (8.6) | |
| Scrub the tooth and put it back into the socket | 85 (45.7) | |
| Put the tooth back into the socket without cleaning | 8 (4.3) | |
| I do not know | 23 (12.4) | |
| Is it possible to provide reattachment of broken tooth fragment | Yes | 81 (43.6) |
| No | 55 (29.5) | |
| I do not know | 50 (26.9) |
| Question | Total n (%) | Knowledge Score Mean ± SD | p Value | |
|---|---|---|---|---|
| Self-reported knowledge about dental injuries | Insufficient | 51 (27.4) | 3.7 ± 1.7 | 0.060 |
| Sufficient but incomplete | 109 (58.6) | 3.6 ± 1.5 | ||
| Comprehensive | 26 (14.0) | 3.7 ± 1.5 | ||
| Dental injuries and first aid training during academic or professional education | No | 175 (94.1) | 3.5 ± 1.5 | 0.351 |
| Yes | 11 (5.9) | 4.0 ± 1.3 | ||
| Willing to attend training on dental injuries in future | No | 44 (23.7) | 3.0 ± 1.7 | 0.008 * |
| Yes | 142 (76.3) | 3.7 ± 1.4 | ||
| Witnessed dental injures | No | 103 (55.4) | 3.3 ± 1.5 | 0.003 * |
| Yes | 83 (44.6) | 3.9 ± 1.4 | ||
| Witnessed dental injures—avulsion | No | 110 (59.1) | 3.3 ± 1.5 | 0.001 * |
| Yes | 76 (40.9) | 4.0 ± 1.4 | ||
| Witnessed dental injures—tooth luxation (lateral luxation, intrusion, extrusion) | No | 170 (91.4) | 3.7 ± 1.5 | 0.904 |
| Yes | 16 (8.6) | 3.6 ± 1.7 | ||
| Witnessed dental injures—tooth fracture | No | 141 (75.8) | 3.5 ± 1.5 | 0.186 |
| Yes | 45 (24.2) | 3.8 ± 1.5 | ||
| Self-reported knowledge about dental injuries first aid—avulsion | No | 83 (44.6) | 3.2 ± 1.5 | 0.001 * |
| Yes | 103 (55.4) | 3.9 ± 1.4 | ||
| Self-reported knowledge about dental injuries first aid—tooth luxation | No | 179 (96.2) | 3.5 ± 1.5 | 0.216 |
| Yes | 7 (3.8) | 4.3 ± 1.5 | ||
| Self-reported knowledge about dental injuries first aid—tooth fracture | No | 122 (65.6) | 3.5 ± 1.5 | 0.375 |
| Yes | 64 (34.4) | 3.7 ± 1.5 | ||
| Questions | Total n (%) | Knowledge Score Mean ± SD | p Value | |
|---|---|---|---|---|
| Do you know mouthguard function? | No | 83 (44.6) | 3.1 ± 1.5 | 0.001 * |
| Yes | 103 (55.4) | 3.9 ± 1.5 | ||
| Do you recommend to your patients the usage of mouthguard? | No | 88 (47.3) | 3.3 ± 1.5 | 0.016 * |
| Yes | 98 (52.7) | 3.8 ± 1.5 | ||
| Do you know the types of mouthguards? | No | 176 (94.6) | 3.6 ± 1.5 | 0.500 |
| Yes | 10 (5.4) | 3.9 ± 1.4 | ||
| Do you know the difference between custom and off-the-shelf mouthguards? | No | 4 (2.2) | 2.2 ± 1.5 | 0.192 |
| Yes | 47 (25.3) | 3.7 ± 1.6 | ||
| I do not know | 135 (72.6) | 3.6 ± 1.5 | ||
| How much usage of mouthguard can prevent or reduce sports-related dental injuries? | 10% | 4 (2.2) | 3.2 ± 1.5 | 0.880 |
| 20% | 25 (13.4) | 3.4 ± 1.5 | ||
| 40% | 91 (48.9) | 3.6 ± 1.3 | ||
| 60% | 66 (35.5) | 3.6 ± 1.8 | ||
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tadin, A.; Delic, D.; Delic Jukic, I.K.; Gorseta, K.; Gavic, L. Pediatricians’ Knowledge of Emergency Management of Dental Injuries and Use of Mouthguards: A Cross-Sectional Survey. Dent. J. 2021, 9, 152. https://doi.org/10.3390/dj9120152
Tadin A, Delic D, Delic Jukic IK, Gorseta K, Gavic L. Pediatricians’ Knowledge of Emergency Management of Dental Injuries and Use of Mouthguards: A Cross-Sectional Survey. Dentistry Journal. 2021; 9(12):152. https://doi.org/10.3390/dj9120152
Chicago/Turabian StyleTadin, Antonija, Danijela Delic, Ivana Kristina Delic Jukic, Kristina Gorseta, and Lidia Gavic. 2021. "Pediatricians’ Knowledge of Emergency Management of Dental Injuries and Use of Mouthguards: A Cross-Sectional Survey" Dentistry Journal 9, no. 12: 152. https://doi.org/10.3390/dj9120152
APA StyleTadin, A., Delic, D., Delic Jukic, I. K., Gorseta, K., & Gavic, L. (2021). Pediatricians’ Knowledge of Emergency Management of Dental Injuries and Use of Mouthguards: A Cross-Sectional Survey. Dentistry Journal, 9(12), 152. https://doi.org/10.3390/dj9120152








