Molar Incisor Hypomineralization: Awareness among Postdoctoral Dental Residents: A Cross-Sectional Study
Abstract
:1. Introduction
2. Materials and Methods
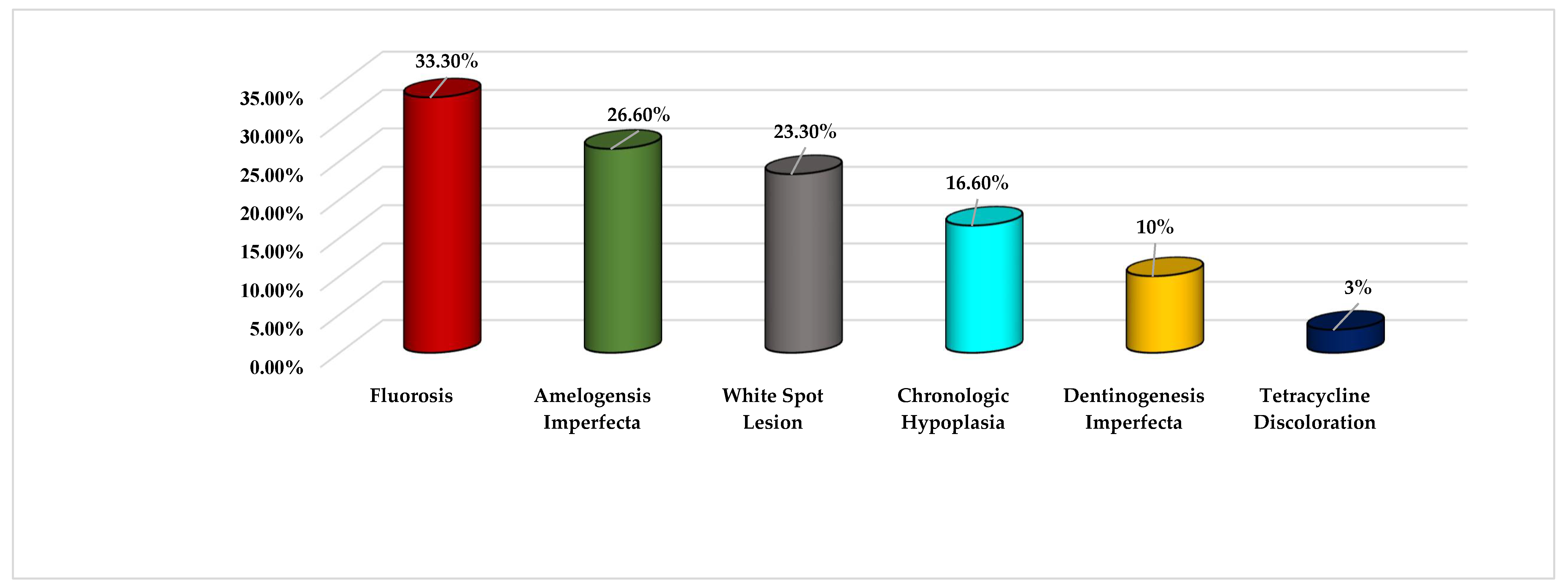
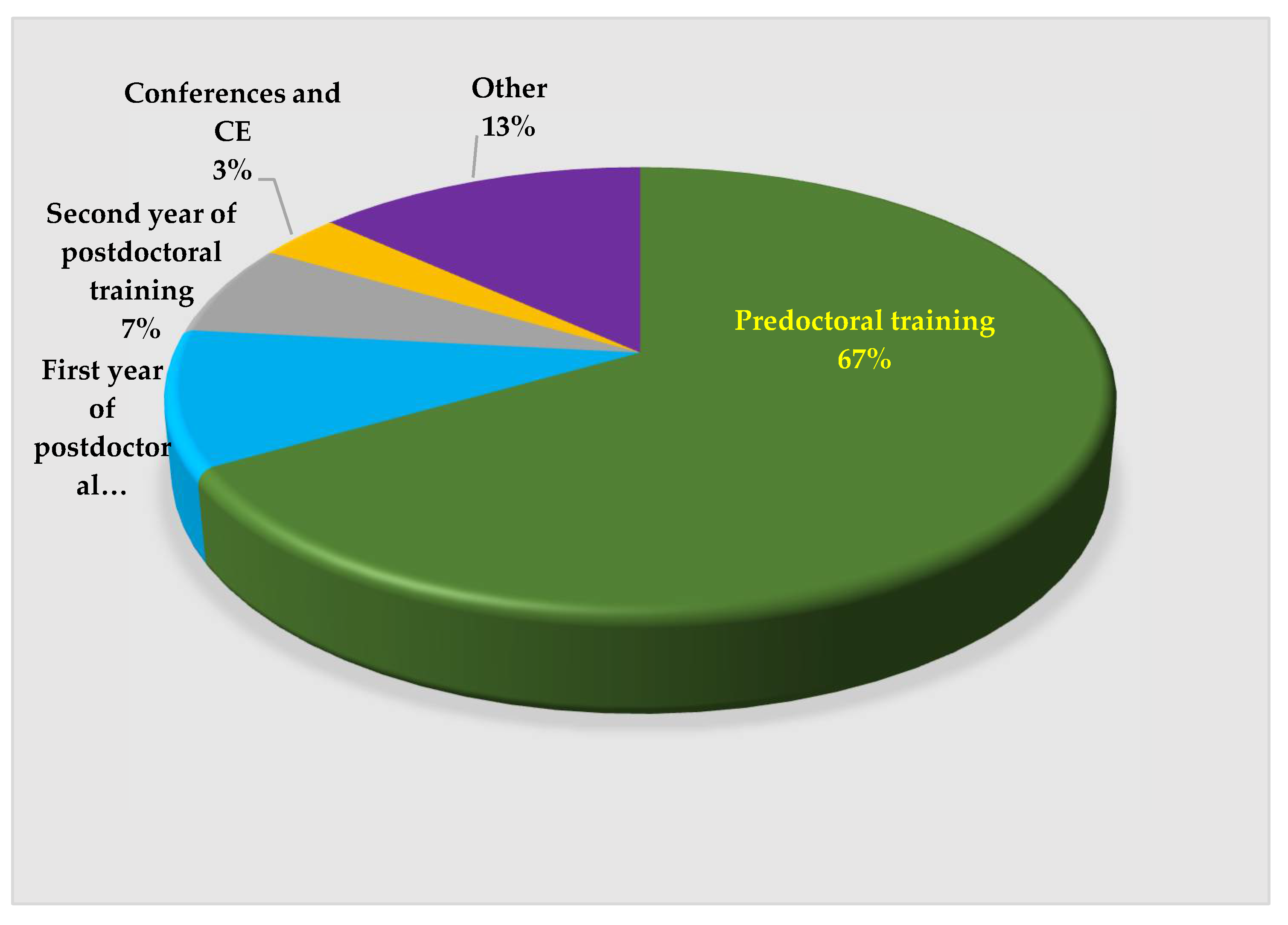
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Weerheijm, K.L.; Duggal, M.; Mejàre, I.; Papagiannoulis, L.; Koch, G.; Martens, L.C.; Hallonsten, A.L. Judgement criteria for molar incisor hypomineralisation (MIH) in epidemiologic studies: A summary of the European meeting on MIH held in Athens. Eur. J. Paediatr. Dent. 2003, 4, 110–113. [Google Scholar]
- Bussaneli, D.G.; Vieira, A.R.; Santos-Pinto, L.; Restrepo, M. Molar-incisor hypomineralisation: An updated view for aetiology 20 years later. Eur. Arch. Paediatr. Dent. 2022, 15, 193–198. [Google Scholar] [CrossRef] [PubMed]
- Schwendicke, F.; Elhennawy, K.; Reda, S.; Bekes, K.; Manton, D.J.; Krois, J. Global burden of molar incisor hypomineralization. J. Dent. 2018, 68, 10–18. [Google Scholar] [CrossRef]
- Zhao, D.; Dong, B.; Yu, D.; Ren, Q.; Sun, Y. The prevalence of molar incisor hypomineralization: Evidence from 70 studies. Int. J. Paediatr. Dent. 2018, 28, 170–179. [Google Scholar] [CrossRef]
- Portella, P.D.; Menoncin, B.L.; de Souza, J.F.; de Menezes, J.V.; Fraiz, F.C.; Assunção, L.R. Impact of molar incisor hypomineralization on quality of life in children with early mixed dentition: A hierarchical approach. Int. J. Paediatr. Dent. 2019, 29, 496–506. [Google Scholar] [CrossRef] [PubMed]
- Fatturi, A.L.; Wambier, L.M.; Chibinski, A.C.; Assunção, L.R.; Brancher, J.A.; Reis, A.; Souza, J.F. A systematic review and meta-analysis of systemic exposure associated with molar incisor hypomineralization. Community Dent. Oral Epidemiol. 2019, 47, 407–415. [Google Scholar] [CrossRef]
- Hasmun, N.; Lawson, J.; Vettore, M.V.; Elcock, C.; Zaitoun, H.; Rodd, H. Change in Oral Health-Related Quality of Life Following Minimally Invasive Aesthetic Treatment for Children with Molar Incisor Hypomineralisation: A Prospective Study. Dent. J. 2018, 6, 61. [Google Scholar] [CrossRef] [Green Version]
- Kalkani, M.; Balmer, R.C.; Homer, R.M.; Day, P.F.; Duggal, M.S. Molar incisor hypomineralisation: Experience and perceived challenges among dentists specialising in paediatric dentistry and a group of general dental practitioners in the UK. Eur. Arch. Paediatr. Dent. 2016, 17, 81–88. [Google Scholar] [CrossRef] [PubMed]
- Garot, E.; Couture-Veschambre, C.; Manton, D.; Beauval, C.; Rouas, P. Analytical evidence of enamel hypomineralisation on permanent and primary molars amongst past populations. Sci. Rep. 2017, 7, 1712. [Google Scholar] [CrossRef] [PubMed]
- Elhennawy, K.; Schwendicke, F. Managing molar-incisor hypomineralization: A systematic review. J. Dent. 2016, 55, 16–24. [Google Scholar] [CrossRef]
- Villanueva-Gutiérrez, T.; Irigoyen-Camacho, M.E.; Castaño-Seiquier, A.; Zepeda-Zepeda, M.A.; Sanchez-Pérez, L.; Frechero, N.M. Prevalence and Severity of Molar-Incisor Hypomineralization, Maternal Education, and Dental Caries: A Cross-Sectional Study of Mexican Schoolchildren with Low Socioeconomic Status. J. Int. Soc. Prev. Community Dent. 2019, 9, 513–521. [Google Scholar] [PubMed]
- Mittal, R.; Chandak, S.; Chandwani, M.; Singh, P.; Pimpale, J. Assessment of association between molar incisor hypomineralization and hypomineralized second primary molar. J. Int. Soc. Prev. Community Dent. 2016, 6, 34–39. [Google Scholar] [PubMed] [Green Version]
- Fatturi, A.L.; Menoncin, B.L.; Reyes, M.T.; Meger, M.; Scariot, R.; Brancher, J.A.; Küchler, E.C.; Feltrin-Souza, J. The relationship between molar incisor hypomineralization, dental caries, socioeconomic factors, and polymorphisms in the vitamin D receptor gene: A population-based study. Clin. Oral Investig. 2020, 24, 3971–3980. [Google Scholar] [CrossRef]
- Fernandes, I.C.; Forte, F.D.; Sampaio, F.C. Molar-incisor hypomineralization (MIH), dental fluorosis, and caries in rural areas with different fluoride levels in the drinking water. Int. J. Paediatr. Dent. 2020, 32, 74–82. [Google Scholar] [CrossRef] [PubMed]
- Elhennawy, K.; Anang, M.; Splieth, C.; Bekes, K.; Manton, D.J.; Hedar, Z.; Krois, J.; Jost-Brinkmann, P.G.; Schwendicke, F. Knowledge, attitudes, and beliefs regarding molar incisor hypomineralization (MIH) amongst German dental students. Int. J. Paediatr. Dent. 2021, 31, 486–495. [Google Scholar] [CrossRef]
- Alanzi, A.; Faridoun, A.; Kavvadia, K.; Ghanim, A. Dentists’ perception, knowledge, and clinical management of molar-incisor-hypomineralisation in Kuwait: A cross-sectional study. BMC Oral Health 2018, 1, 34. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tagelsir, A.; Dean, J.A.; Eckert, G.J.; Martinez-Mier, E.A. US Pediatric Dentists’ Perception of Molar Incisor Hypomineralization. Pediatr. Dent. 2018, 40, 272–278. [Google Scholar]
- Wall, A.; Leith, R. A questionnaire study on perception and clinical management of molar incisor hypomineralisation (MIH) by Irish dentists. Eur. Arch. Paediatr. Dent. 2020, 21, 703–710. [Google Scholar] [CrossRef]
- Gambetta-Tessini, K.; Marino, R.; Ghanim, A.; Calache, H.; Manton, D.J. Knowledge, experience and perceptions regarding Molar-Incisor Hypomineralisation (MIH) amongst Australian and Chilean public oral health care practitioners. BMC Oral Health 2016, 16, 75. [Google Scholar] [CrossRef] [Green Version]
- Serna-Munoz, C.; Martinez-Beneyto, Y.; Perez-Silva, A.; Poza-Pascual, A.; Ibanez-Lopez, F.J.; Ortiz-Ruiz, A.J. Perception, knowledge, and attitudes towards molar incisor hypomineralization among Spanish dentists: A cross-sectional study. BMC Oral Health 2020, 20, 260. [Google Scholar] [CrossRef] [PubMed]
- Gamboa, G.C.S.; Lee, G.H.M.; Ekambaram, M.; Yiu, C.K.Y. Knowledge, perceptions, and clinical experiences on molar incisor hypomineralization among dental care providers in Hong Kong. BMC Oral Health 2018, 18, 217. [Google Scholar] [CrossRef] [PubMed]
- Craveia, J.; Rouas, P.; Carat, T.; Manton, D.J.; Boileau, M.J.; Garot, E. Knowledge and Management of First Permanent Molars with Enamel Hypomineralization among Dentists and Orthodontists. J. Clin. Pediatr. Dent. 2020, 44, 20–27. [Google Scholar] [CrossRef] [PubMed]
- Hussein, A.; Ghanim, A.; Abu-Hassan, M.; Manton, D. Knowledge, management and perceived barriers to treatment of molar-incisor hypomineralisation in general dental practitioners and dental nurses in Malaysia. Eur. Arch. Paediatr. Dent. 2014, 15, 301–307. [Google Scholar] [CrossRef]
- Silva, M.J.; Alhowaish, L.; Ghanim, A.; Manton, D.J. Knowledge and attitudes regarding molar incisor hypomineralisation amongst Saudi Arabian dental practitioners and dental students. Eur. Arch. Paediatr. Dent. 2016, 17, 215–222. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, R.; Ghanim, A.; Azar, M.; Manton, D. Molar incisor hypomineralisation: Discernment a group of Iranian dental academics. J. Oral Health Oral Epidemiol. 2014, 3, 21. [Google Scholar]
- Bekes, K.; Melichar, K.; Stamm, T.; Elhennawy, K. Dental Students’ Knowledge, Attitudes and Beliefs Regarding Molar Incisor Hypomineralization (MIH): A Survey in Vienna, Austria. J. Multidiscip. Health 2021, 14, 2881–2889. [Google Scholar] [CrossRef]
- Somani, C.; Taylor, G.D.; Garot, E.; Rouas, P.; Lygidakis, N.A.; Wong, F.S. An update of treatment modalities in children and adolescents with teeth affected by molar incisor hypomineralisation (MIH): A systematic review. Eur. Arch. Paediatr. Dent. 2021, 10, 39–64. [Google Scholar] [CrossRef]
- Rajic, V.; Modric, V.; Malcic, A.; Gorseta, K.; Zoran Karlovic, Z.; Verzak, Z. Molar Incisor Hypomineralization in Children with Intellectual Disabilities. Dent. J. 2021, 9, 21. [Google Scholar] [CrossRef]
- Taylor, G.D.; Pearce, K.F.; Vernazza, C.R. Management of compromised first permanent molars in children: Cross-Sectional analysis of attitudes of UK general dental practitioners and specialists in paediatric dentistry. Int. J. Paediatr. Dent. 2019, 29, 267–280. [Google Scholar] [CrossRef] [PubMed]
- Crombie, F.A.; Manton, D.J.; Weerheijm, K.L.; Kilpatrick, N.M. Molar incisor hypomineralization: A survey of members of the Australian and new Zealand Society of Paediatric Dentistry. Aust. Dent. J. 2008, 53, 160–166. [Google Scholar] [CrossRef]
- Kopperud, S.E.; Pedersen, C.G.; Espelid, I. Treatment decisions on molar-incisor hypomineralization (MIH) by Norwegian dentists—A questionnaire study. BMC Oral Health 2016, 17, 3. [Google Scholar] [CrossRef] [Green Version]
- Upadhyay, S.; Kumar, G.; Dhillon, J.K.; Gill, N.C. Perception of Indian dental surgeons regarding molar incisor hypomineralization. Int. J. Clin. Pediatr. Dent. 2018, 11, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Anderson, A.J.; Vingrys, A.J. Small samples: Does size matter? Investig. Ophthalmol. Vis. Sci. 2001, 42, 1411–1413. [Google Scholar]
| Group | Very Confident | Confident | Not Confident | p-Value |
|---|---|---|---|---|
| Pediatric (%) | 44.4% | 55.6% | 0.0% | |
| Ortho (%) | 0.0% | 41.2% | 58.8% | 0.005 |
| GPR (%) | 0.0% | 33.3% | 66.7% | |
| Total (%) | 13.8% | 44.8% | 41.4% |
| Cases | Restoration of Choice | Percent | p-Value |
|---|---|---|---|
| Case 1: Healthy 9-year-old with MIH on a symptomless first permanent molar | Glass ionomer | 10% | |
| Resin-modified GI | 48% | 0.012 | |
| Composite resin | 35% | ||
| Stainless steel crowns | 7% | ||
| Case 2: Healthy 10-year-old MIH on first permanent molar with hypersensitivity | Glass ionomer | 4% | |
| Resin-modified GI | 7% | 0.025 | |
| Composite resin | 20% | ||
| Stainless steel crowns | 65% | ||
| Case 3: Healthy 4-year-old with MIH on a symptomless second primary molar | Glass ionomer | 12% | |
| Resin-modified GI | 50% | 0.183 | |
| Composite resin | 26% | ||
| Stainless steel crowns | 12% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Negrescu, J.; Kodra, L.; Ziada, H.; Al-Talib, T.; Abubakr, N.H. Molar Incisor Hypomineralization: Awareness among Postdoctoral Dental Residents: A Cross-Sectional Study. Dent. J. 2022, 10, 64. https://doi.org/10.3390/dj10040064
Negrescu J, Kodra L, Ziada H, Al-Talib T, Abubakr NH. Molar Incisor Hypomineralization: Awareness among Postdoctoral Dental Residents: A Cross-Sectional Study. Dentistry Journal. 2022; 10(4):64. https://doi.org/10.3390/dj10040064
Chicago/Turabian StyleNegrescu, Jana, Laurenc Kodra, Hassan Ziada, Tanya Al-Talib, and Neamat Hassan Abubakr. 2022. "Molar Incisor Hypomineralization: Awareness among Postdoctoral Dental Residents: A Cross-Sectional Study" Dentistry Journal 10, no. 4: 64. https://doi.org/10.3390/dj10040064
APA StyleNegrescu, J., Kodra, L., Ziada, H., Al-Talib, T., & Abubakr, N. H. (2022). Molar Incisor Hypomineralization: Awareness among Postdoctoral Dental Residents: A Cross-Sectional Study. Dentistry Journal, 10(4), 64. https://doi.org/10.3390/dj10040064







