Flowable Bulk-Fill Materials Compared to Nano Ceramic Composites for Class I Cavities Restorations in Primary Molars: A Two-Year Prospective Case-Control Study
Abstract
:1. Introduction
2. Materials and Methods
2.1. Sample Description
2.2. Inclusion and Exclusion Criteria
2.3. Study Population
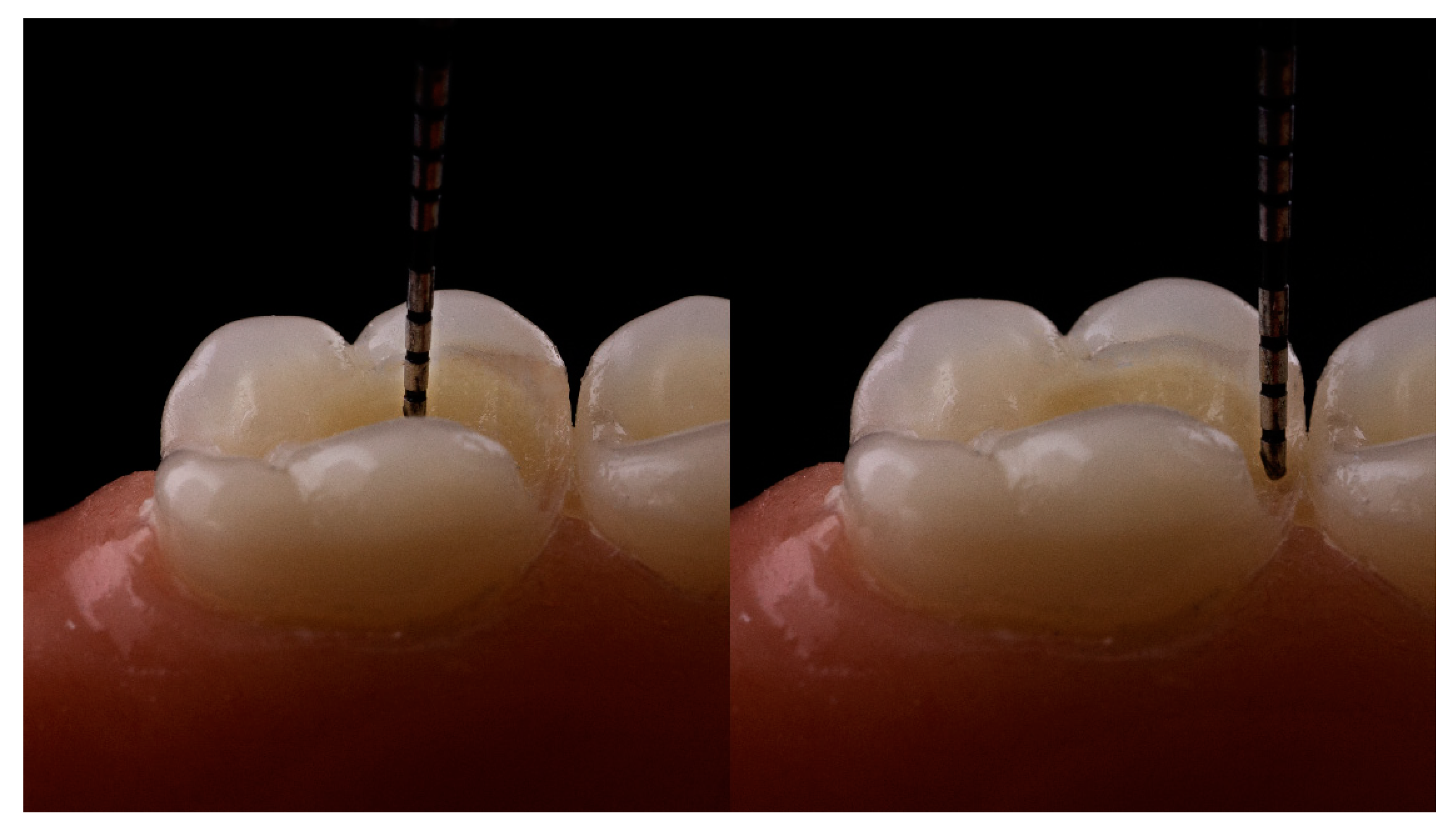
2.4. Study Interventions
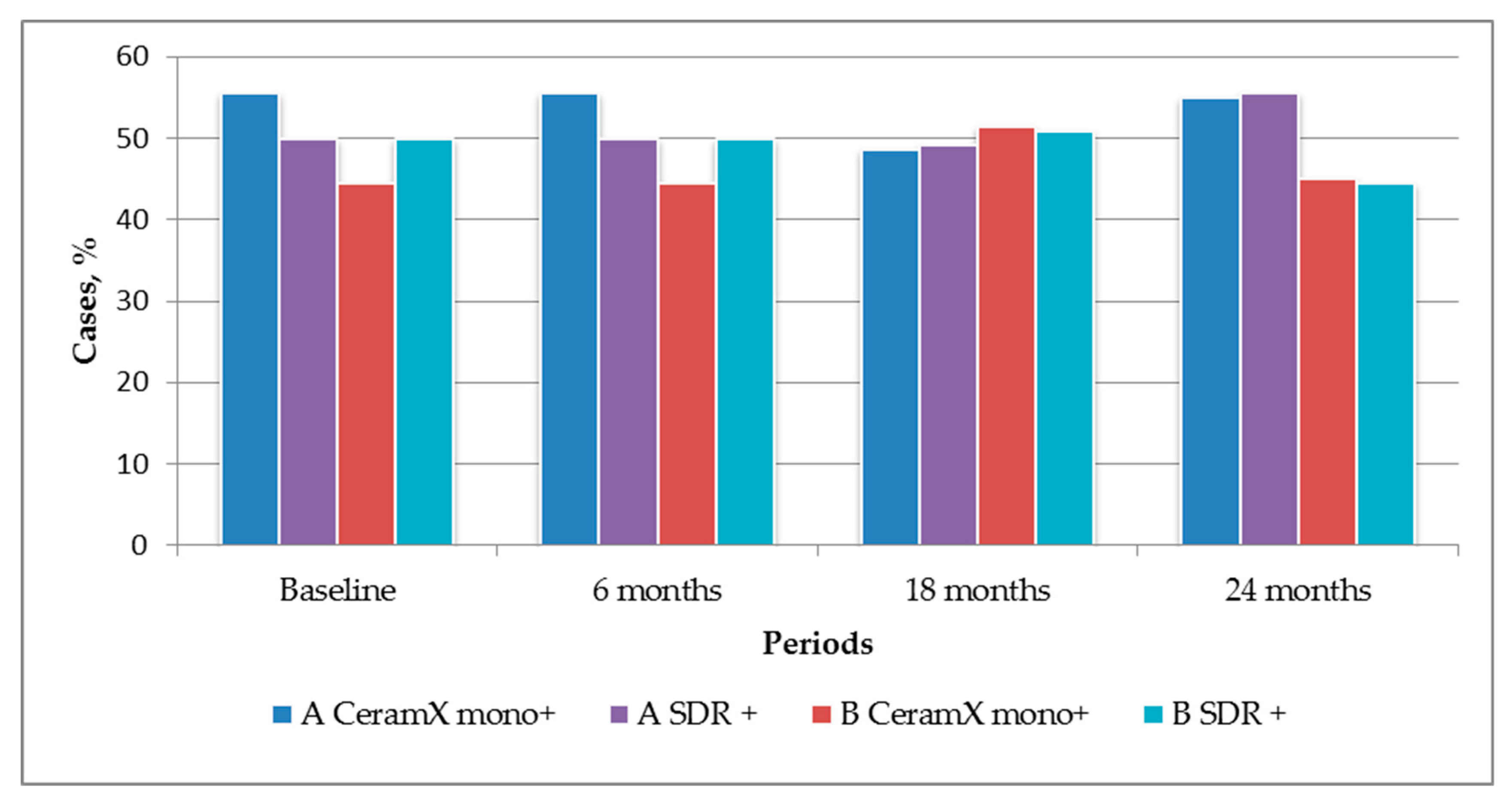
3. Results
4. Discussion
5. Conclusions
6. Limitation of the Study
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Andersson-Wenckert, I.; Sunnegårdh-Grönberg, K. Flowable resin composite as a class II restorative in primary molars: A two-year clinical evaluation. Acta Odontol. Scand. 2006, 64, 334–340. [Google Scholar] [CrossRef] [PubMed]
- ADA Council on Scientific Affairs. Direct and indirect restorative materials. J. Am. Dent. Assoc. 2003, 134, 463–472. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lohbauer, U. Dental Glass Ionomer Cements as Permanent Filling Materials?—Properties, Limitations and Future Trends. Materials 2010, 3, 76–96. [Google Scholar] [CrossRef]
- Abed, Y.A.; Sabry, H.A.; Alrobeigy, N.A. Degree of conversion and surface hardness of bulk-fill composite versus incremental-fill composite. Tanta Dent. J. 2015, 12, 71–80. [Google Scholar] [CrossRef]
- Ilie, N.; Bucuta, S.; Draenert, M. Bulk-fill resin-based composites: An in vitro assessment of their mechanical performance. Oper. Dent. 2013, 38, 618–625. [Google Scholar] [CrossRef] [PubMed]
- Ilie, N.; Stark, K. Curing behaviour of high-viscosity bulk-fill composites. J. Dent. 2014, 42, 977–985. [Google Scholar] [CrossRef]
- Heck, K.; Manhart, J.; Hickel, R.; Diegritz, C. Clinical evaluation of the bulk-fill composite QuiXfil in molar class I and II cavities: 10-year results of a RCT. Dent. Mater. 2018, 34, e138–e147. [Google Scholar] [CrossRef]
- Ilie, N.; Hickel, R. Investigations on a methacrylate-based flowable composite based on the SDRTM technology. Dent. Mater. 2011, 27, 348–355. [Google Scholar] [CrossRef]
- Altan, H.; Göztas, Z.; Arslanoglu, Z. Bulk-Fill Restorative Materials in Primary Tooth: An Intrapulpal Temperature Changes Study. Contemp. Clin. Dent. 2018, 9, S52–S57. [Google Scholar] [CrossRef]
- Jin, X.; Bertrand, S.; Hammesfahr, P. New radically polymerizable resins with remarkably low curing stress. J. Dent. Res. 2009, 88, 1651. [Google Scholar]
- Yamamoto, T.; Hanabusa, M.; Kimura, S.; Momoi, Y.; Hayakawa, T. Changes in polymerization stress and elastic modulus of bulk-fill resin composites for 24 h after irradiation. Dent. Mater. J. 2018, 37, 87–94. [Google Scholar] [CrossRef] [PubMed]
- El-Damanhoury, H.; Platt, J. Polymerization shrinkage stress kinetics and related properties of bulk-fill resin composites. Oper. Dent. 2014, 39, 374–382. [Google Scholar] [CrossRef] [PubMed]
- Yokesh, C.A.; Hemalatha, P.; Muthalagu, M.; Justin, M.R. Comparative Evaluation of the Depth of Cure and Degree of Conversion of Two Bulk-fill Flowable Composites. J. Clin. Diagn. Res. 2017, 11, ZC86–ZC89. [Google Scholar] [CrossRef] [PubMed]
- Ehlers, V.; Ernst, C.P.; Willershausen, B. Bulk-Flow Restoration in the Primary Dentition—A Case Report. In Proceedings of the Annual Meeting of the IADR Continental European Division, Florence, France, 4–7 September 2013; Available online: https://www.researchgate.net/publication/266762471_Bulk-Flow_Restoration_in_the_Primary_Dentition_-_a_Case_Report (accessed on 14 December 2018).
- SDR Flow+_US Brochure_EN. Available online: https://www.dentsplysirona.com/content/dam/dentsply/pim/manufacturer/Restorative/Direct_Restoration/Composites__Flowables/Flowables/SDR_flow/Layout_ML1C0004B_SDR%20flow+%20brochures%20U.S._Canada.pdf (accessed on 14 December 2018).
- van Dijken, J.W.V.; Pallesen, U. A randomized controlled three year evaluation of “bulk-filled” posterior resin restorations based on stress decreasing resin technology. Dent. Mater. 2014, 30, e245–e251. [Google Scholar] [CrossRef] [PubMed]
- van Dijken, J.W.V.; Pallesen, U. Posterior bulk-filled resin composite restorations: A 5-year randomized controlled clinical study. J. Dent. 2016, 51, 29–35. [Google Scholar] [CrossRef] [PubMed]
- van Dijken, J.W.; Pallesen, U. Randomized 3-year clinical evaluation of Class I and II posterior resin restorations placed with a bulk-fill resin composite and a one-step self-etching adhesive. J. Adhes. Dent. 2015, 17, 81–88. [Google Scholar] [PubMed]
- Antczak-Bouckoms, A.A.; Tulloch, J.F.C.; Berkey, C.S. Split-mouth and cross-over designs in dental research. J. Clin. Periodontol. 1990, 17, 446–453. [Google Scholar] [CrossRef]
- Kühnisch, J.; Ekstrand, K.R.; Pretty, I.; Twetman, S.; van Loveren, C.; Gizani, S.; Spyridonos Loizidou, M. Best clinical practice guidance for management of early caries lesions in children and young adults: An EAPD policy document. Eur. Arch. Paediatr. Dent. 2016, 17, 3–12. [Google Scholar] [CrossRef]
- American Academy of Pediatric Dentistry. Guideline on Restorative Dentistry. Pediatr. Dent. 2016, 38, 250–262. [Google Scholar]
- Dabawala, S.; Chacko, V.; Suprabha, B.S.; Rao, A.; Natarajan, S.; Ongole, R. Evaluation of Pulp Chamber Dimensions of Primary Molars from Bitewing Radiographs. Pediatr. Dent. 2015, 37, 361–365. [Google Scholar]
- Selvakumar, H.; Kavitha, S.; Vijayakumar, R.; Eapen, T.; Bharathan, R. Study of pulp chamber morphology of primary mandibular molars using spiral computed tomography. J. Contemp. Dent. Pract. 2014, 15, 726–729. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Pongprueksa, P.; Van Meerbeek, B.; De Munck, J. Curing profile of bulk-fill resin-based composites. J. Dent. 2015, 43, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Flury, S.; Hayoz, S.; Peutzfeldt, A.; Hüsler, J.; Lussi, A. Depth of cure of resin composites: Is the ISO 4049 method suitable for bulk-fill materials? Dent. Mater. 2012, 28, 521–528. [Google Scholar] [CrossRef] [PubMed]
- Yengopal, V.; Harnekar, S.Y.; Patel, N.; Siegfried, N. Dental fillings for the treatment of caries in the primary dentition. Cochrane Database Syst. Rev. 2016, 15, CD004483. [Google Scholar] [CrossRef] [PubMed]
- Cvar, J.F.; Ryge, G. Reprint of criteria for the clinical evaluation of dental restorative materials 1971. Clin. Oral Investig. 2005, 9, 215–232. [Google Scholar]
- Chesterman, J.; Jowett, A.; Gallacher, A.; Nixon, P. Bulk-fill resin-based composite restorative materials: A review. Br. Dent. J. 2017, 222, 337–344. [Google Scholar] [CrossRef]
- Leprince, J.G.; Palin, W.M.; Vanacker, J.; Sabbagh, J.; Devaux, J.; Leloup, G. Physico-mechanical characteristics of commercially available bulk-fill composites. J. Dent. 2014, 42, 993–1000. [Google Scholar] [CrossRef]
- Ehlers, V.; Gran, K.; Callaway, A.; Azrak, B.; Ernst, C.-P. One-year Clinical Performance of Flowable Bulk-fill Composite vs. Conventional Compomer Restorations in Primary Molars. J. Adhes. Dent. 2019, 21, 247–254. [Google Scholar]
- Goumans, C.; Veerkamp, J.S.J.; Aartman, I.H.A. Dental anxiety and behavioural problems: What is their influence on the treatment plan? Eur. J. Paediatr. Dent. 2004, 5, 15–18. [Google Scholar]
- van Bochove, J.A.; van Amerongen, W.E. The influence of restorative treatment approaches and the use of local analgesia, on the children’s discomfort. Eur. Arch. Paediatr. Dent. 2006, 1, 11–16. [Google Scholar] [CrossRef]
- Chisini, L.A.; Collares, K.; Cademartori, M.G.; de Oliveira, L.J.C.; Conde, M.C.M.; Demarco, F.F.; Corrêa, M.B. Restorations in primary teeth: A systematic review on survival and reasons for failures. Int. J. Paediatr. Dent. 2018, 28, 123–139. [Google Scholar] [CrossRef] [PubMed]
| Characteristic | Rating | Criteria |
|---|---|---|
| Color match | Alpha | Restoration matches adjacent tooth structure in color and translucency |
| Bravo | Mismatch in within an acceptable range of tooth color and translucency | |
| Charlie | Mismatch is outside the acceptable range | |
| Cavosurface marginal discoloration | Alpha | Absence of marginal discoloration |
| Bravo | Presence of marginal discoloration limited and not extended | |
| Charlie | Evident marginal discoloration penetrated toward the pulp chamber | |
| Marginal integrity | Alpha | Closely adapted, no visible crevice |
| Bravo | Visible crevice, explorer will penetrate | |
| Charlie | Crevice in which dentin is exposed | |
| Surface texture | Alpha | Smooth surface |
| Bravo | Slightly rough or pitted, can be refinished | |
| Charlie | Rough, cannot be refinished | |
| Postoperative sensitivity | Alpha | Absence of dentinal hypersensitivity |
| Bravo | Presence of dentinal hypersensitivity | |
| Secondary caries | Alpha | No evidence of caries |
| Bravo | Caries is evident | |
| Fracture | Alpha | No evidence of fracture |
| Bravo | Evidence of fracture |
| Time | Color Match | Cavosurface Marginal Discoloration | Marginal Integrity | Surface Texture | Postoperative Sensitivity | Secondary Caries | Fracture | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Prevalence of Scores/Complications, % | A | B | C | A | B | C | A | B | C | A | B | C | A | B | A | B | A | B |
| CeramX mono + Prime and Bond NT (prevalence of scores/complications, %) | ||||||||||||||||||
| Baseline | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 100 | 0 | 100 | 0 | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| 6 months | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 100 | 0 | 100 | 0 | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| 18 months | 100 | 0 | 0 | 92.6 | 7.4 | 0 | 100 | 100 | 0 | 96.3 | 3.7 | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| 24 months | 100 | 0 | 0 | 92.6 | 7.4 | 0 | 96.3 | 3.7 | 0 | 96.3 | 3.7 | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| SDR + Prime and Bond NT (prevalence of scores/complications, %) | ||||||||||||||||||
| Baseline | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 100 | 0 | 100 | 0 | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| 6 months | 100 | 0 | 0 | 100 | 0 | 0 | 100 | 100 | 0 | 100 | 0 | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| 18 months | 100 | 0 | 0 | 92.6 | 7.4 | 0 | 100 | 100 | 0 | 100 | 0 | 0 | 100 | 0 | 100 | 0 | 100 | 0 |
| 24 months | 100 | 0 | 0 | 92.6 | 7.4 | 0 | 92.6 | 7.4 | 0 | 100 | 0 | 0 | 100 | 0 | 96.3 | 3.7 | 100 | 0 |
| Criterion | U | P |
|---|---|---|
| Color match | 72.00 | 1.00 |
| Cavosurface marginal discoloration | 72.00 | 1.00 |
| Marginal integrity | 72.00 | 1.00 |
| Surface texture | 68.00 | 0.82 |
| Postoperative sensitivity | 6.00 | 0.69 |
| Secondary caries | 4.00 | 0.34 |
| Fracture | 4.00 | 0.34 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sarapultseva, M.; Sarapultsev, A. Flowable Bulk-Fill Materials Compared to Nano Ceramic Composites for Class I Cavities Restorations in Primary Molars: A Two-Year Prospective Case-Control Study. Dent. J. 2019, 7, 94. https://doi.org/10.3390/dj7040094
Sarapultseva M, Sarapultsev A. Flowable Bulk-Fill Materials Compared to Nano Ceramic Composites for Class I Cavities Restorations in Primary Molars: A Two-Year Prospective Case-Control Study. Dentistry Journal. 2019; 7(4):94. https://doi.org/10.3390/dj7040094
Chicago/Turabian StyleSarapultseva, Maria, and Alexey Sarapultsev. 2019. "Flowable Bulk-Fill Materials Compared to Nano Ceramic Composites for Class I Cavities Restorations in Primary Molars: A Two-Year Prospective Case-Control Study" Dentistry Journal 7, no. 4: 94. https://doi.org/10.3390/dj7040094
APA StyleSarapultseva, M., & Sarapultsev, A. (2019). Flowable Bulk-Fill Materials Compared to Nano Ceramic Composites for Class I Cavities Restorations in Primary Molars: A Two-Year Prospective Case-Control Study. Dentistry Journal, 7(4), 94. https://doi.org/10.3390/dj7040094





