Bonding of Core Build-Up Composites with Glass Fiber-Reinforced Posts
Abstract
1. Introduction
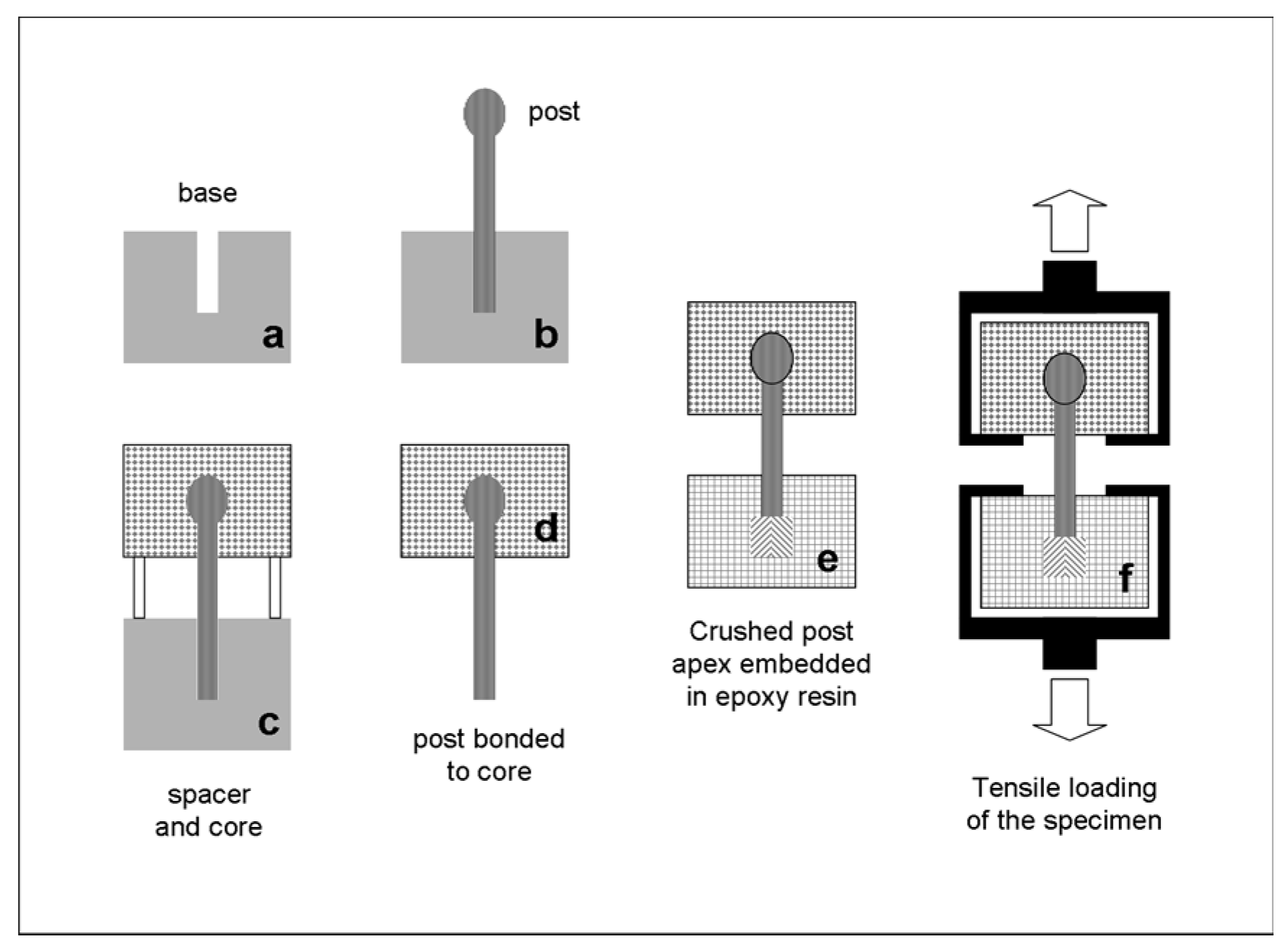
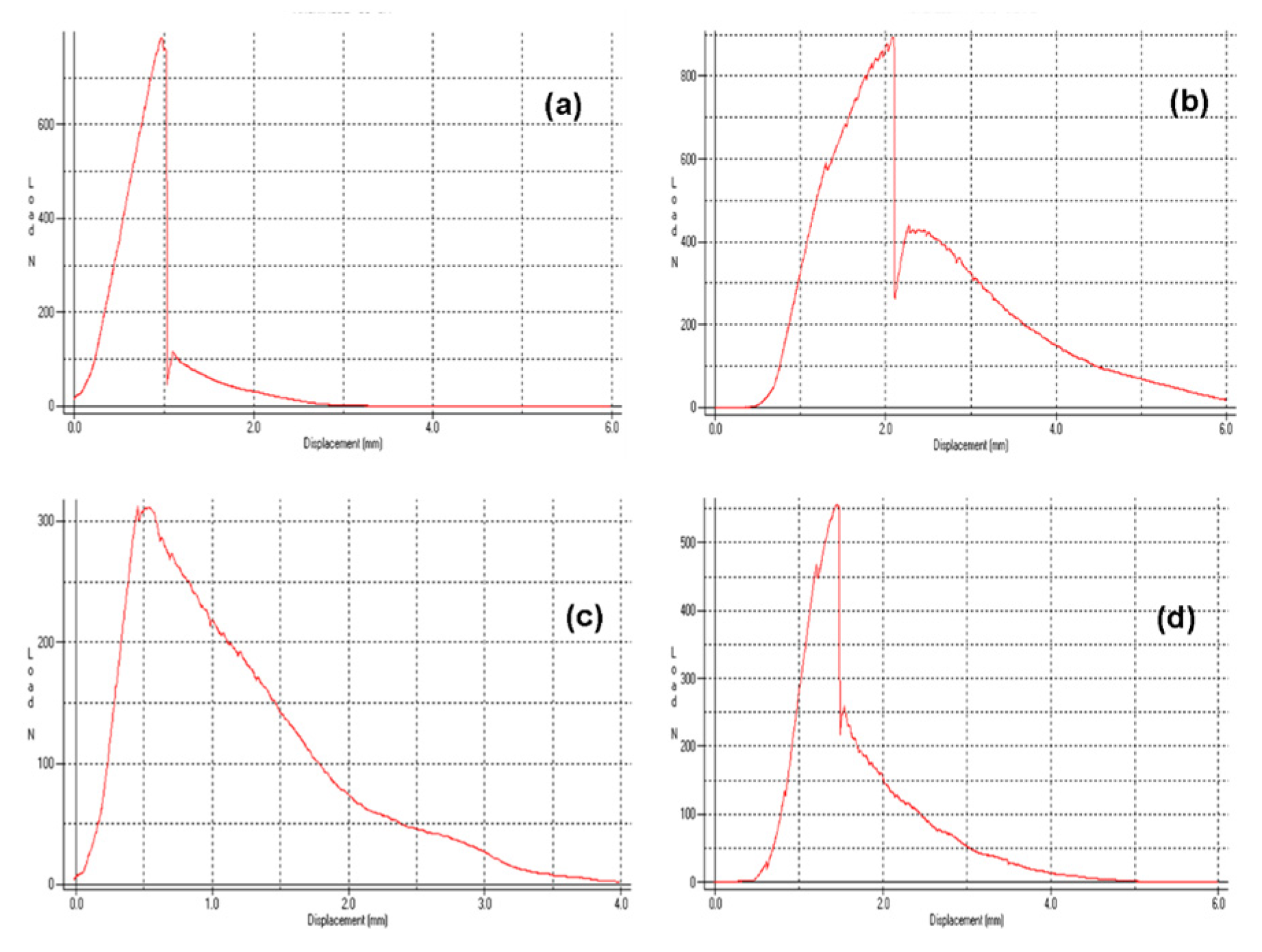
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
- The coronal parts of ARL and MPT posts were the most retentive, whereas GLX was the least retentive, irrespective of the core build-up material used.
- CPC provided the highest retention with four posts (FBK, GLX, MTP, and PRW), without statistically significant differences from CDC in two (FBK and MTP) and CNB in one (PRW). CPC and CDC were the most reliable core materials for two posts (ARL and PRW), with no statistically significant difference from CNB in three (FKB, GLX, and MTP).
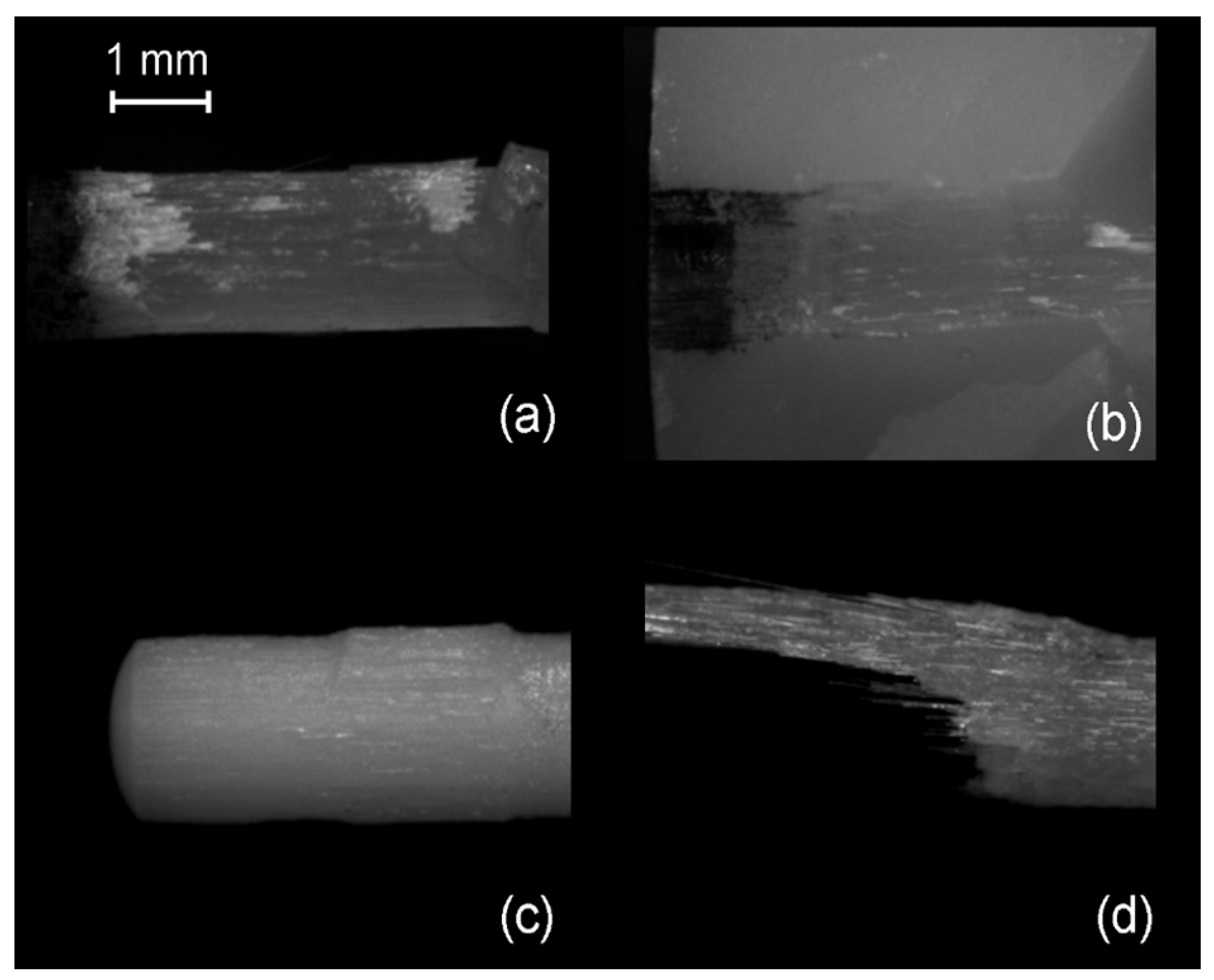
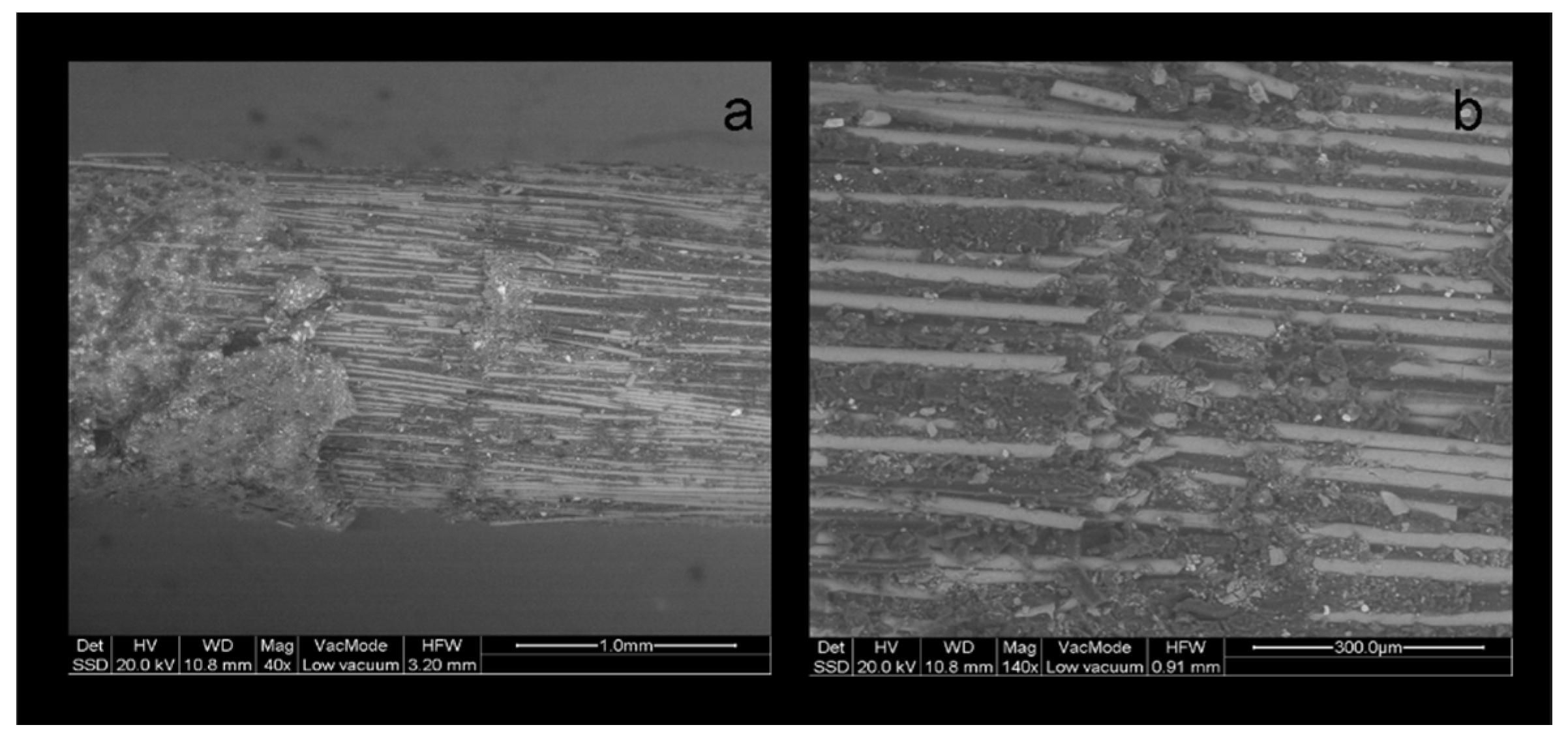
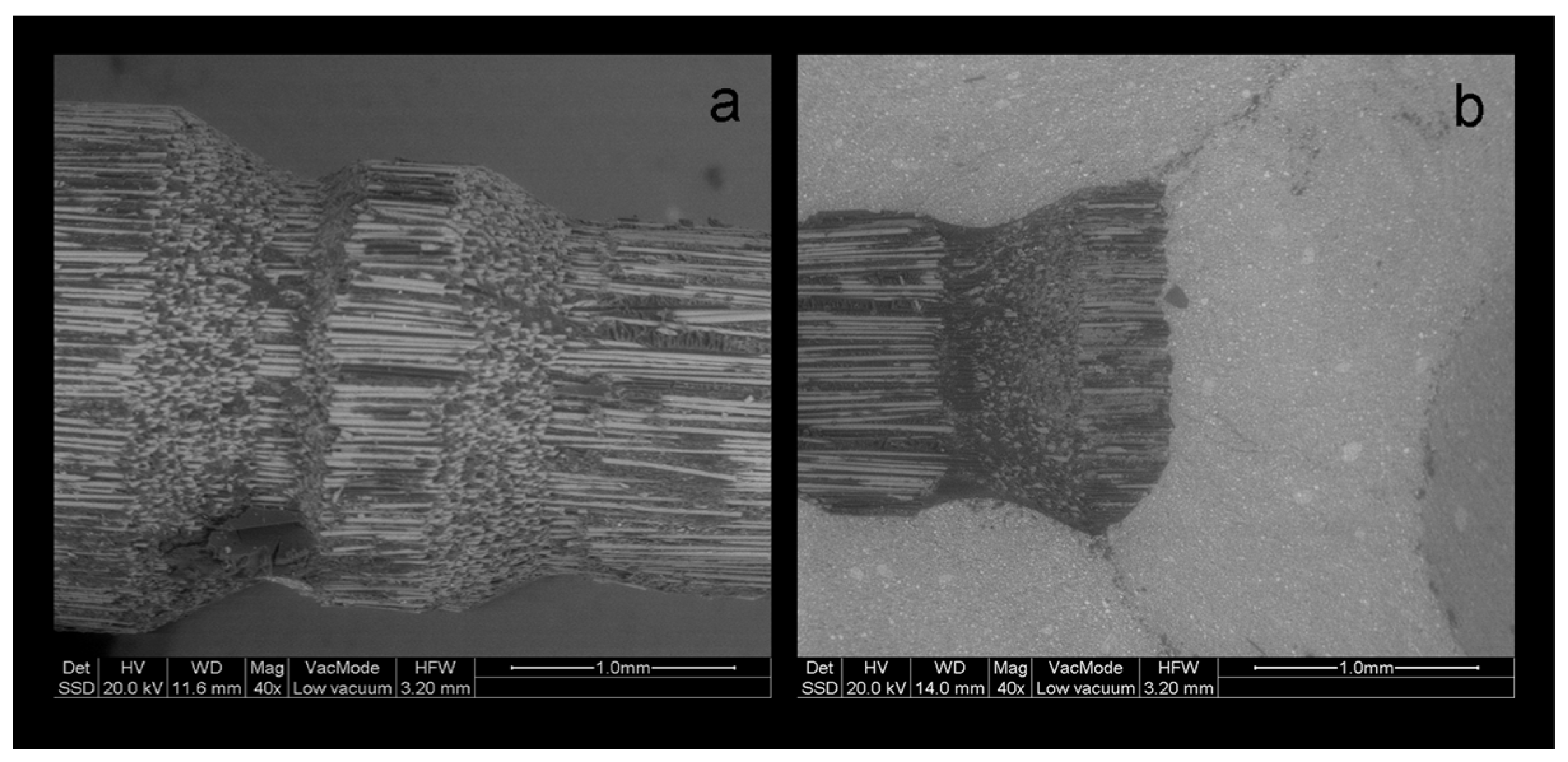
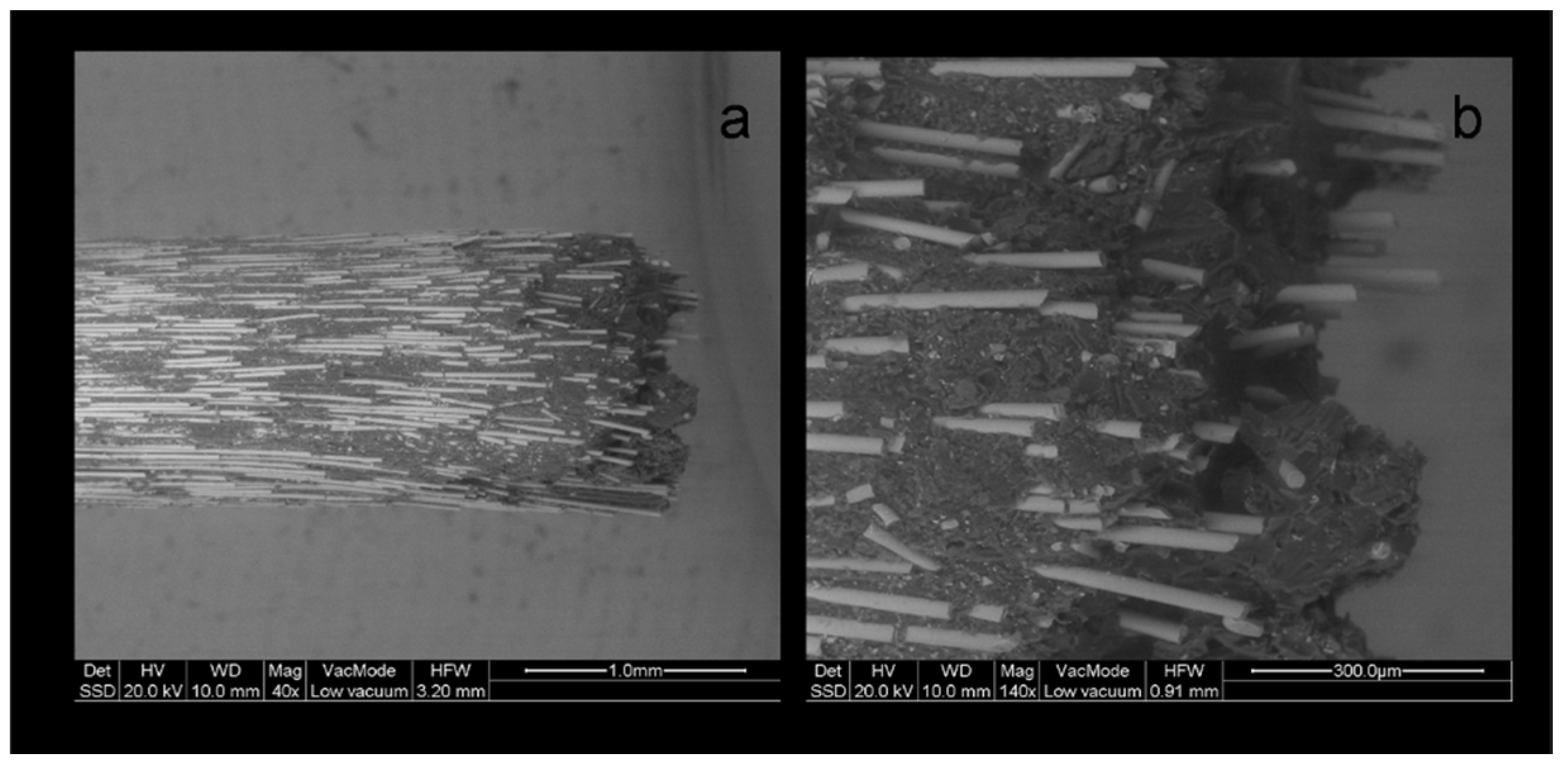
- The presence of specific coronal retention features in some posts (ARL and PRW) did not essentially ensure increased strength, due to shear fracture of the retentive features.
Author Contributions
Funding
Conflicts of Interest
References
- Ambica, K.; Mahendran, K.; Talwar, S.; Verma, M.; Padmini, G.; Periasamy, R. Comparative Evaluation of Fracture Resistance under Static and Fatigue Loading of Endodontically Treated Teeth Restored with Carbon Fiber Posts, Glass Fiber Posts, and an Experimental Dentin Post System: An in Vitro Study. J. Endod. 2013, 39, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Cekic-Nagas, I.; Sukuroglu, E.; Canay, S. Does the surface treatment affect the bond strength of various fibre-post systems to resin-core materials? J. Dent. 2011, 39, 171–179. [Google Scholar] [CrossRef] [PubMed]
- Bitter, K.; Priehn, K.; Martus, P.; Kielbassa, A.M. In vitro evaluation of push out bond strengths of various luting agents to tooth-coloured posts. J. Prosthet. Dent. 2006, 95, 302–310. [Google Scholar] [CrossRef] [PubMed]
- Schwartz, R.S.; Robbins, J.W. Post Placement and Restoration of Endodontically Treated Teeth: A Literature Review. J. Endod. 2004, 30, 289–301. [Google Scholar] [CrossRef] [PubMed]
- Vano, M.; Goracci, C.; Monticelli, F.; Tognini, F.; Gabriele, M.; Tay, F.R.; Ferrari, M. The adhesion between fibre posts and composite resin cores: The evaluation of microtensile bond strength following various surface chemical treatments to posts. Int. Endod. J. 2006, 39, 31–39. [Google Scholar] [CrossRef] [PubMed]
- Chieruzzi, M.; Pagano, S.; Pennacchi, M.; Lombardo, G.; D’Errico, P.; Kenny, J.M. Compressive and flexural behaviour of fibre reinforced endodontic posts. J. Dent. 2012, 40, 968–978. [Google Scholar] [CrossRef]
- Torbjorner, A.; Karlsonn, S.; Syverud, M. Hensten-Pettersen, A. Carbon fibre reinforced root canal posts. Mechanical and cytotoxic properties. Eur. J. Oral Sci. 1996, 104, 605–611. [Google Scholar] [CrossRef]
- Seefeld, F.; Wenz, H.J.; Ludwig, K.; Kern, M. Resistance to fracture and structural characteristics of different fibre reinforced post systems. Dent. Mater. 2007, 23, 265–271. [Google Scholar] [CrossRef]
- Grandini, S.; Goracci, C.; Monticelli, F.; Tay, F.R.; Ferrari, M. Fatigue resistance and structural characteristics of fibre posts: Three-point bending test and SEM evaluation. Dent. Mater. 2005, 21, 75–82. [Google Scholar] [CrossRef]
- Wandscher, V.F.; Bergoli, C.D.; De Oliveira, A.F.; Kaizer, O.B.; Borges, A.L.S.; Limberguer, I.D.F.; Valandro, L.F. Fatigue surviving, fracture resistance, shear stress and finite element analysis of glass fiber posts with different diameters. J. Mech. Behav. Biomed. Mater. 2015, 43, 69–77. [Google Scholar] [CrossRef]
- Zicari, F.; Coutinho, E.; Scotti, R.; Van Meerbeek, B.; Naert, I. Mechanical properties and micro-morphology of fiber posts. Dent. Mater. 2013, 29, e45–e52. [Google Scholar] [CrossRef] [PubMed]
- Grandini, S.; Chieffi, N.; Cagidiaco, M.C.; Goracci, C.; Ferrari, M. Fatigue resistance and structural integrity of different types of fiber posts. Dent. Mater. J. 2008, 27, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Soares, C.J.; Castro, C.G.; Filho, P.C.F.S.; Soares, P.V.; Magalhães, D.; Martins, L.R.M. Two-Dimensional FEA of Dowels of Different Compositions and External Surface Configurations. J. Prosthodont. 2009, 18, 36–42. [Google Scholar] [CrossRef] [PubMed]
- Novais, V.R.; Versluis, A.; Correr-Sobrinho, L.; Soares, C.J.; Correr-Sobrinho, L. Three-point bending testing of fibre posts: Critical analysis by finite element analysis. Int. Endod. J. 2011, 44, 519–524. [Google Scholar] [CrossRef]
- Lassila, L.V.; Tanner, J.; Le Bell, A.-M.; Narva, K.; Vallittu, P.K. Flexural properties of fiber reinforced root canal posts. Dent. Mater. 2004, 20, 29–36. [Google Scholar] [CrossRef]
- Galhano, G.A.; Valandro, L.F.; De Melo, R.M.; Scotti, R.; Bottino, M.A. Evaluation of the flexural strength of carbon fiber-, quartz fiber- and glass fiber-based posts. J. Endod. 2005, 31, 209–211. [Google Scholar]
- Dietschi, D.; Duk, O.; Krejci, I.; Sadan, A. Biomechanical considerations for the restoration of endodontically treated teeth: A systematic review of the literature- part I. Composition and micro- and macrostructure alterations. Quintessence Int. 2007, 38, 733–743. [Google Scholar]
- Pegoretti, A.; Fambri, L.; Zappini, G.; Bianchetti, M. Finite element analysis of a glass fibre reinforced composite endodontic post. Biomaterials 2002, 23, 2667–2682. [Google Scholar] [CrossRef]
- Chuang, S.-F.; Yaman, P.; Herrero, A.; Dennison, J.B.; Chang, C.-H. Influence of post material and length on endodontically treated incisors: An in vitro and finite element study. J. Prosthet. Dent. 2010, 104, 379–388. [Google Scholar] [CrossRef]
- Zicari, F.; Van Meerbeek, B.; Scotti, R.; Naert, I. Effect of fibre post length and adhesive strategy on fracture resistance of endodontically treated teeth after fatigue loading. J. Dent. 2012, 40, 312–321. [Google Scholar] [CrossRef]
- Mastoras, K.; Vasiliadis, L.; Koulaouzidou, E.; Gogos, C. Evaluation of Push-out Bond Strength of Two Endodontic Post Systems. J. Endod. 2012, 38, 510–514. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, T.; Ohyama, T.; Waki, T.; Kinuta, S.; Wakabayashi, K.; Mutobe, Y.; Takano, N.; Yatani, H. Stress analysis of endodontically treated anterior teeth restored with different types of post material. Dent. Mater. J. 2006, 25, 145–150. [Google Scholar] [CrossRef] [PubMed]
- Salameh, Z.; Sorrentino, R.; Papacchini, F.; Ounsi, H.F.; Tashkandi, E.; Goracci, C.; Ferrari, M. Fracture Resistance and Failure Patterns of Endodontically Treated Mandibular Molars Restored Using Resin Composite with or Without Translucent Glass Fiber Posts. J. Endod. 2006, 32, 752–755. [Google Scholar] [CrossRef] [PubMed]
- Reid, L.C.; Kazemi, R.B.; Meiers, J.C. Effect of Fatigue Testing on Core Integrity and Post Microleakage of Teeth Restored with Different Post Systems. J. Endod. 2003, 29, 125–131. [Google Scholar] [CrossRef]
- Mannocci, F.; Sherriff, M.; Watson, T.F. Three-point bending test of fibre posts. J. Endod. 2001, 27, 758–764. [Google Scholar] [CrossRef]
- Sahafi, A.; Peutzfeldt, A.; Asmussen, E.; Gotfredsen, K. Bond strength of resin cement to dentin and to surface-treated posts of titanium alloy, glass fiber, and zirconia. J. Adhes. Dent. 2003, 5, 153–162. [Google Scholar]
- Balbosh, A.; Kern, M. Effect of surface treatment on retention of glass-fiber endodontic posts. J. Prosthet. Dent. 2006, 95, 218–223. [Google Scholar] [CrossRef]
- Radović, I.; Monticelli, F.; Goracci, C.; Cury Àlvaro, H.; Coniglio, I.; Vulicevic, Z.R.; García-Godoy, F.; Ferrari, M. The effect of sandblasting on adhesion of a dual-cured resin composite to methacrylic fiber posts: Microtensile bond strength and SEM evaluation. J. Dent. 2007, 35, 496–502. [Google Scholar] [CrossRef]
- Asmussen, E.; Peutzfeldt, A.; Sahafi, A. Bonding of resin cements to post materials: Influence of surface energy characteristics. J. Adhes. Dent. 2005, 7, 231–234. [Google Scholar]
- Kleverlaan, C.J.; Feilzer, A.J. Polymerization shrinkage and contraction stress of dental resin composites. Dent. Mater. 2005, 21, 1150–1157. [Google Scholar] [CrossRef]
- Zalkind, M.; Shkury, S.; Stern, N.; Heling, I. Effect of prefabricated metal post-head design on the retention of various core materials. J. Oral Rehabil. 2000, 27, 483–487. [Google Scholar] [CrossRef] [PubMed]
- Hochman, N.; Feinzaig, I.; Zalkind, M. Effect of design of pre-fabricated posts and post heads on the retention of various cements and core materials. J. Oral Rehabil. 2003, 30, 702–707. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Grandini, S.; Simonetti, M.; Monticelli, F.; Goracci, C. Influence of a microbrush on bonding fiber post into root canals under clinical conditions. Oral Surg. Oral Med. Oral Path. Oral Radiol. Endod. 2001, 94, 627–631. [Google Scholar] [CrossRef] [PubMed]
- Ferrari, M.; Vichi, A.; Grandini, S.; Goracci, C. Efficacy of a self-curing adhesive-resin cement system on luting glass-fiber posts into root canals: An SEM investigation. Int. J. Prosthodont. 2001, 14, 543–549. [Google Scholar]
- Morris, M.D.; Lee, K.-W.; Agee, K.A.; Bouillaguet, S.; Pashley, D.H. Effects of Sodium Hypochlorite and RC-Prep on Bond Strengths of Resin Cement to Endodontic Surfaces. J. Endod. 2001, 27, 753–757. [Google Scholar] [CrossRef]
- Ngoh, E.C.; Pashley, D.H.; Loushine, R.J.; Weller, R.N.; Kimbrough, W.F. Effects of Eugenol on Resin Bond Strengths to Root Canal Dentin. J. Endod. 2001, 27, 411–414. [Google Scholar] [CrossRef]
- Bouillaguet, S.; Troesch, S.; Wataha, J.C.; Krejci, I.; Meyer, J.M.; Pashley, D.H. Microtensile bond strength between adhesive cements and root canal dentin. Dent. Mater. 2003, 19, 199–205. [Google Scholar] [CrossRef]
- Perdigao, J.; Gomes, G.; Lee, I. The effect of silane on the bond strengths of fiber posts. Dent. Mater. 2006, 22, 752–758. [Google Scholar] [CrossRef]
- Giovannetti, A.; Goracci, C.; Vichi, A.; Chieffi, N.; Polimeni, A.; Ferrari, M. Post retentive ability of a new resin composite with low stress behaviour. J. Dent. 2012, 40, 322–328. [Google Scholar] [CrossRef]
- McCabe, J.; Walls, A. The treatment of results for tensile bond strength testing. J. Dent. 1986, 14, 165–168. [Google Scholar] [CrossRef]
- Spinell, T.; Schedle, A.; Watts, D.C. Polymerization shrinkage kinetics of dimethacrylate resin-cements. Dent. Mater. 2009, 25, 1058–1066. [Google Scholar] [CrossRef] [PubMed]
- Goracci, C.; Raffaelli, O.; Monticelli, F.; Balleri, B.; Bertelli, E.; Ferrari, M. The adhesion between prefabricated FRC posts and composite resin cores: Microtensile bond strength with and without post-silanization. Dent. Mater. 2005, 21, 437–444. [Google Scholar] [CrossRef] [PubMed]
- Novais, V.R.; Rodrigues, R.B.; Júnior, P.C.S.; Lourenço, C.-S.; Soares, C.J. Correlation between the Mechanical Properties and Structural Characteristics of Different Fiber Posts Systems. Braz. Dent. J. 2016, 27, 46–51. [Google Scholar] [CrossRef] [PubMed]
- Chang, L.; Hong, L.; Qian, Y.-T.; Zhu, S.; Zhao, S.-Q. The influence of four dual-cure resin cements and surface treatment selection to bond strength of fiber post. Int. J. Oral Sci. 2014, 6, 56–60. [Google Scholar]
- Matinlinna, J.P.; Lassila, L.V.J.; Ozcan, M.; Yli-Urpo, A.; Vallittu, P.K. An introduction to silanes and their clinical applications in dentistry. Int. J. Prosthodont. 2004, 17, 155–164. [Google Scholar]
- Monticelli, F.; Toledano, M.; Tay, F.R.; Cury, A.H.; Goracci, C.; Ferrari, M. Post-surface conditioning improves interfacial adhesion in post/core restorations. Dent. Mater. 2006, 22, 602–609. [Google Scholar] [CrossRef]
- Ferrari, M.; Goracci, C.; Sadek, F.T.; Monticelli, F.; Tay, F.R. An investigation of the interfacial strengths of methacrylate resin-based glass fiber post-core buildups. J. Adhes. Dent. 2006, 8, 239–245. [Google Scholar]
- Tanaka, R.; Fujishima, A.; Shibata, Y.; Manabe, A.; Miyazaki, T. Cooperation of phosphate monomer and silica modification on zirconia. J. Dent. Res. 2008, 87, 666–670. [Google Scholar] [CrossRef]
- Dimitriadi, M.; Zafiropoulou, M.; Zinelis, S.; Silikas, N.; Eliades, G. Silane reactivity and resin bond strength to lithium disilicate ceramic surfaces. Dent. Mater. 2019, 35, 1082–1094. [Google Scholar] [CrossRef]
- Sadek, F.T.; Monticelli, F.; Goracci, C.; Tay, F.R.; Cardoso, P.E.; Ferrari, M.; Cardoso, P.E.C. Bond strength performance of different resin composites used as core materials around fiber posts. Dent. Mater. 2007, 23, 95–99. [Google Scholar] [CrossRef]
- Schittly, E.; Bouter, D.; Le Goff, S.; Degrange, M.; Attal, J.-P. Compatibility of five self-etching adhesive systems with two resin luting cements. J. Adhes. Dent. 2010, 12, 137–142. [Google Scholar] [PubMed]
- Gómez, F.M.; De Góes, M.F. Effect of different silane-containing solutions on glass- ceramic/cement bonding interacting with dual-cure resin cements. ODOVTOS-Int. J. Dent. Sci. 2014, 16, 77–95. [Google Scholar]
- Hanabusa, M.; Yoshihara, K.; Yoshida, Y.; Okihara, T.; Yamamoto, T.; Momoi, Y.; Van Meerbeek, B. Interference of functional monomers with polymerization efficiency of adhesives. Eur. J. Oral Sci. 2016, 124, 204–209. [Google Scholar] [CrossRef] [PubMed]
- Suh, B.I.; Feng, L.; Pashley, D.H.; Tay, F.R. Factors contributing to the incompatibility between simplified-step adhesives and chemically-cured or dual-cured composites. Part III. Effect of acidic resin monomers. J. Adhes. Dent. 2003, 5, 267–282. [Google Scholar] [PubMed]
| Product (Code) | Composition * | Manufacturer |
|---|---|---|
| A. Posts | ||
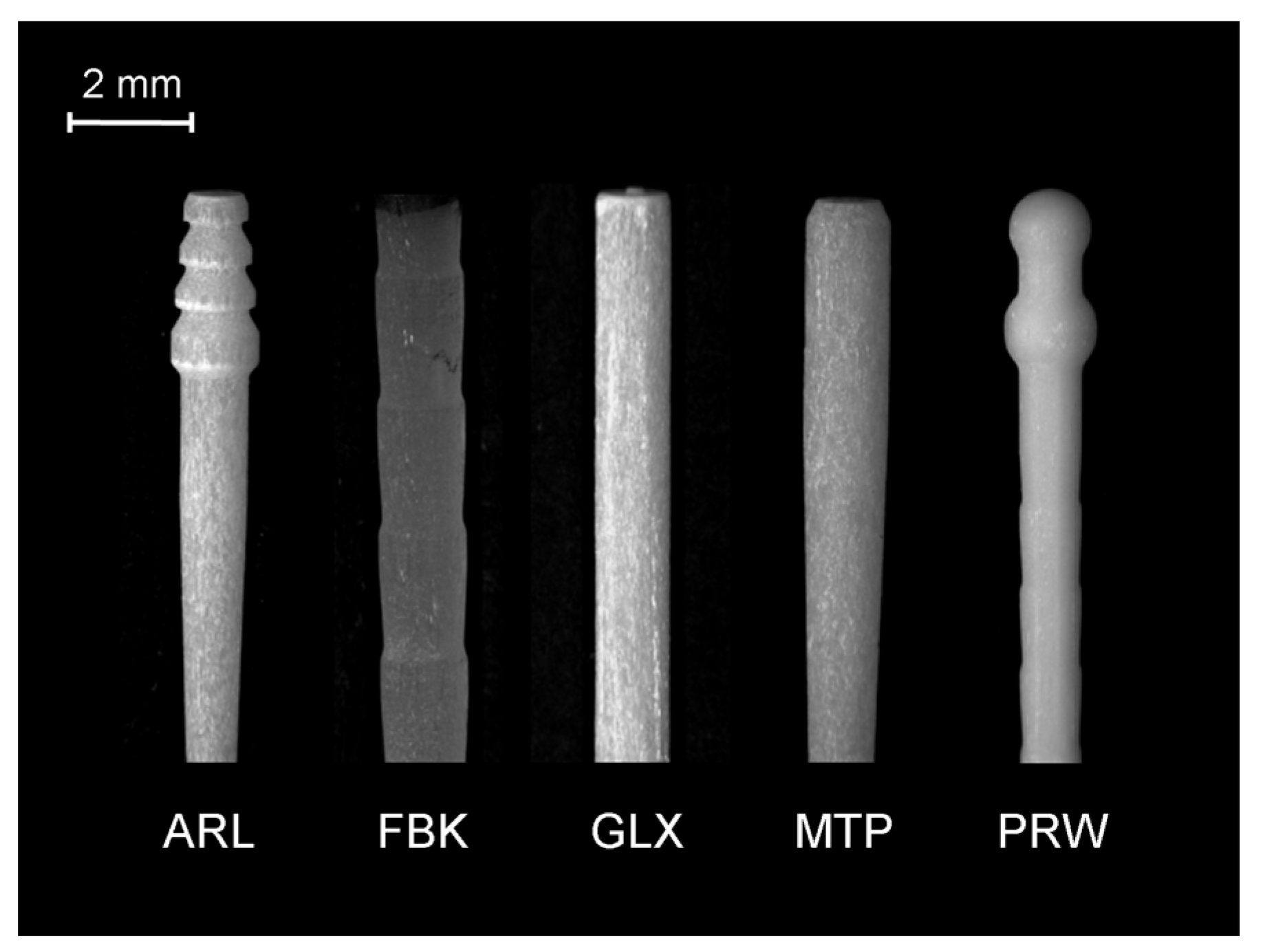
| Archimede Line (ARL) | Glass fiber, composite (diameter: 1.2 mm) | Innotech, Robbio, Italy |
| Fibrekleer (FBK) | Bis-EMA, HDDMA, glass oxide 30–60%, YbF3 10–30 wt % (diameter: 1.5 mm) | Pentron, Wallingford, CT, USA |
| Glassix (GLX) | Epoxy resin, braded glass fiber (65 wt %, diameter: 1.5 mm) | R. Nordin, Montreux, Switzerland |
| Matrix Plus (MTP) | Glass fiber, composite (diameter: 2.0 mm coronal, 1.2 mm apical) | Innotech, Robbio, Italy |
| ParaPost Fiber White (PRW) | Resin 29%, glass fiber 42%, fillers 29 wt % (diameter: 1.5 mm) | Coltene/Whalede nt, Mawhaw, NJ, USA |
| B. Core Build-up Composites | ||
| Clearfil Photocore (CPC) | Bis-GMA, TEGDMA, silanated silica, silanated barium glass (total filler: 83 wt %, 68 vol %), camphoroquinone, accelerators | Kuraray Medical Inc, Okayama, Japan |
| Clearfil DC Core (CDC) | Bis-GMA, TEGDMA, hydrophilic aliphatic dimethacrylate, hydrophobic aromatic dimethacrylate, silanated barium glass, silanated colloidal silica, colloidal silica, alumina (total filler: 74 wt %, 52 vol %), camphoroquinone, accelerators. | Kuraray Medical Inc, Okayama, Japan |
| Clearfil Core New Bond (CNB) | Bis-GMA, TEGDMA, silanated silica, colloidal silica, silanated lanthanum glass (total filler content: 78 wt %, 63 vol %), benzoyl peroxide-amine | Kuraray Medical Inc, Okayama, Japan |
| Descriptive Statistics (n = 20/post) | Core | Post | ||||
|---|---|---|---|---|---|---|
| ARL | FBK | GLX | MTP | PRW | ||
| Mean standard deviation 95% CI of mean median 5–75% percentiles | CPC | 684.9 | 559 | 486.3 | 707.1 | 637.7 |
| 97.7 | 37.1 | 88 | 83.7 | 41 | ||
| 45.7 | 17.4 | 41.2 | 39.2 | 19.2 | ||
| 694 | 553.5 | 482.7 | 701 | 645.7 | ||
| 652.6–738.7 | 528.8–583.5 | 405.1–561.9 | 669–761.7 | 602.4–667 | ||
| Mean standard deviation 95% CI of mean median 25–75% percentiles | CDC | 706.5 | 535.8 | 431.7 | 665.9 | 536.1 |
| 69.7 | 41.3 | 66.3 | 115.3 | 68.9 | ||
| 32.6 | 19.4 | 31 | 54 | 32.2 | ||
| 712.3 | 528.7 | 440.6 | 684 | 528.9 | ||
| 650.9–767.1 | 520.6–561.2 | 369–487.8 | 633.2–739.7 | 490.2–590.3 | ||
| Mean standard deviation 95% CI of mean median 75% percentiles | CNB | 619.7 | 478 | 323.1 | 611.3 | 588.4 |
| 126.8 | 63.4 | 53.1 | 91.2 | 86.2 | ||
| 59.4 | 29.7 | 24.8 | 42.7 | 40.3 | ||
| 622.9 | 474.1 | 323.2 | 600.9 | 590.7 | ||
| 521.6–720.3 | 428.3–538.4 | 369.2 | 554.9–679.9 | 517.4–651.3 | ||
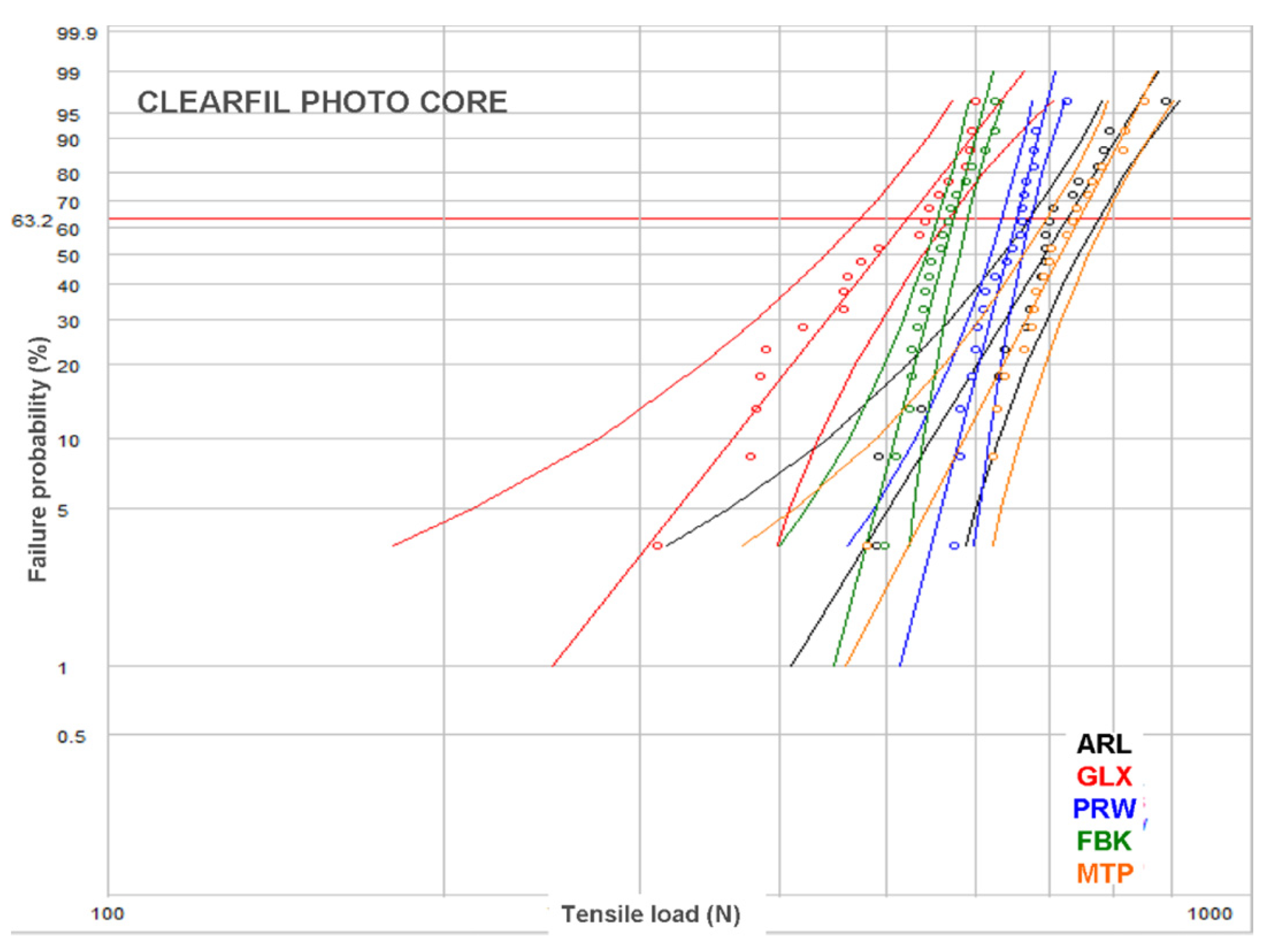
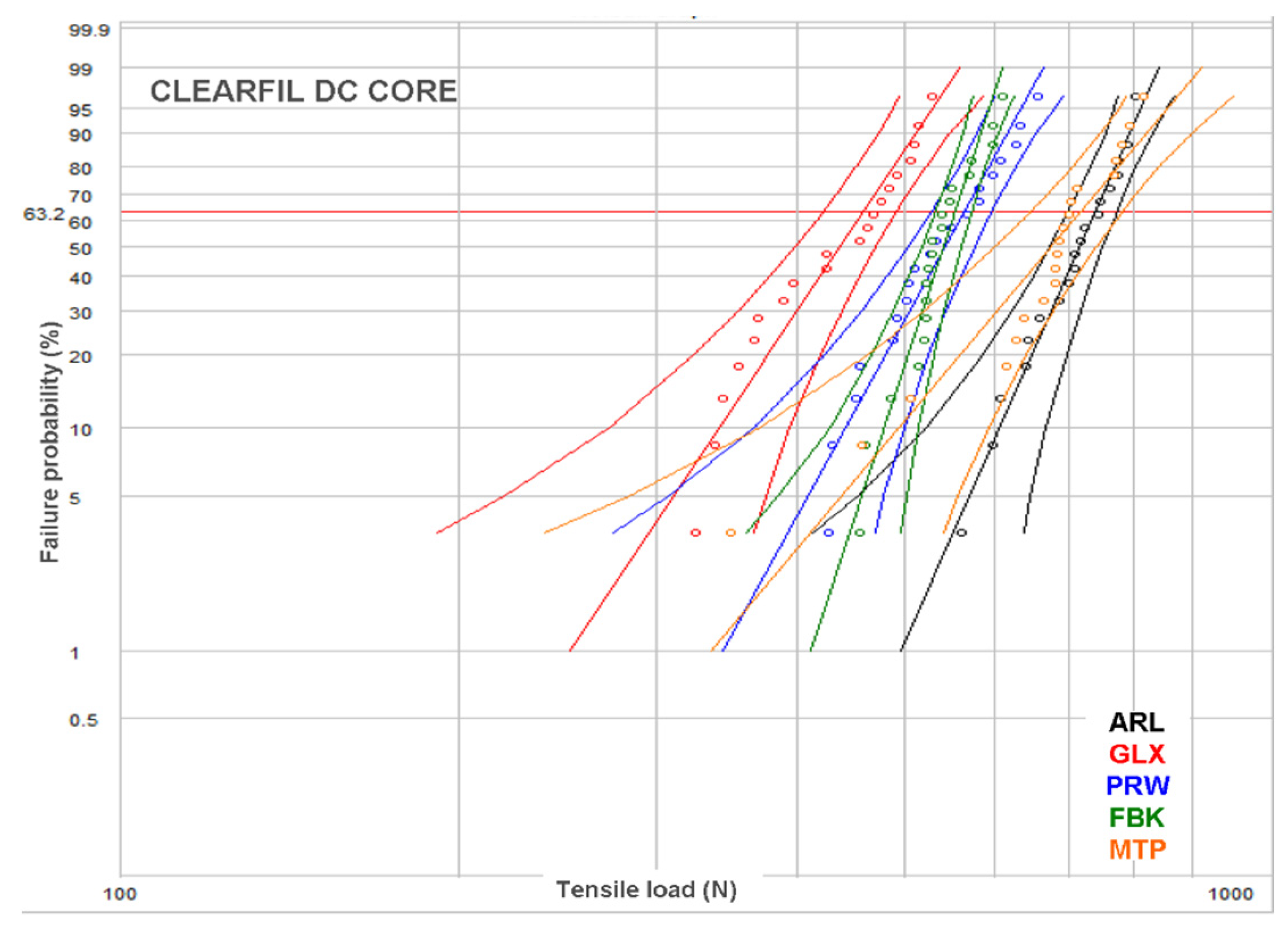
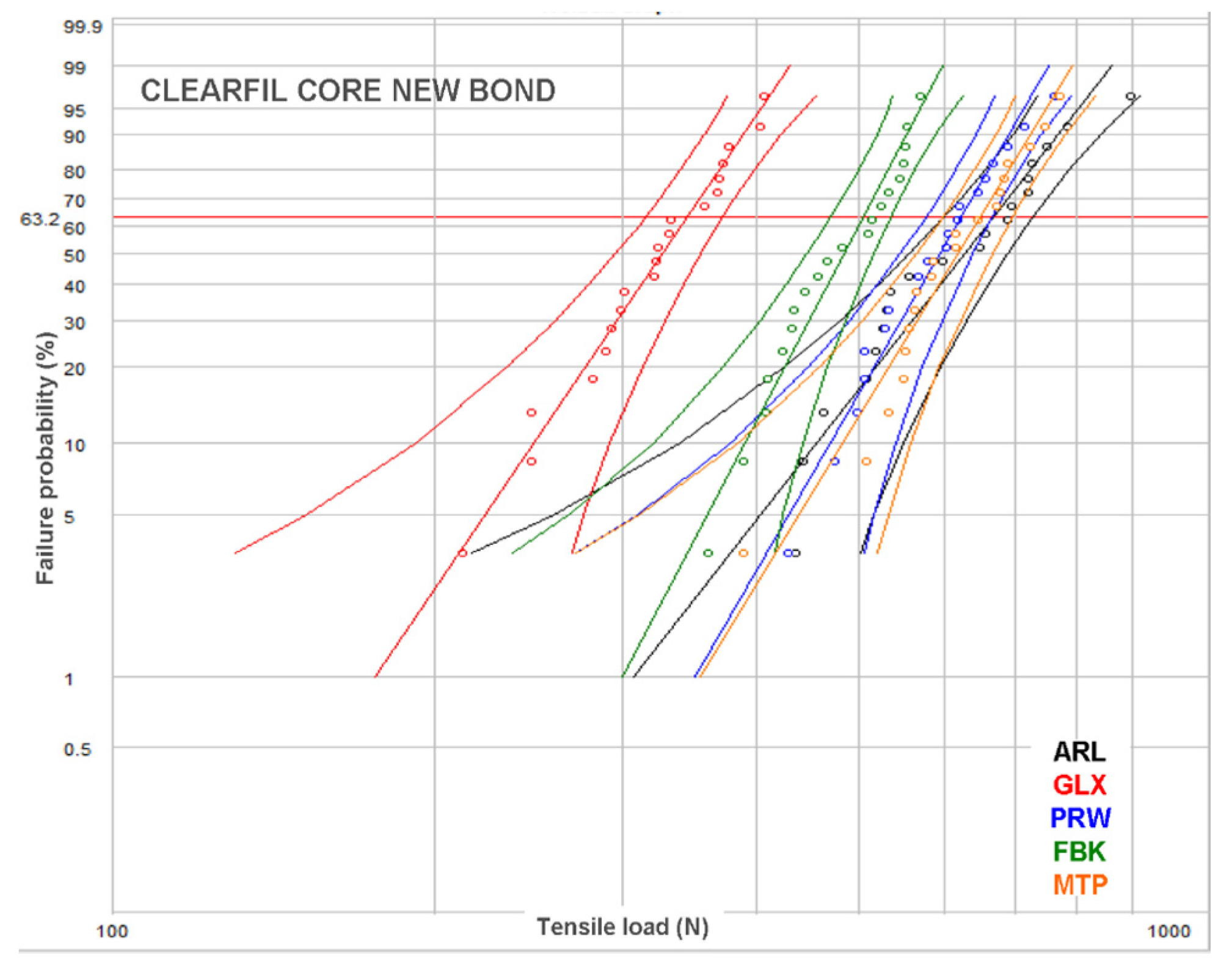
| Core | Weibull Parameter | Post | ||||
|---|---|---|---|---|---|---|
| ARL | FBK | GLX | MTP | PRW | ||
| CPC | β (95% CI) | 8.1 a,A,B (5.9–11.3) | 15.9 b,A (11.4–21.9) | 6.8 a,A (4.7–9.8) | 10.2 a,b,A (7.3–14.3) | 16.7 b,A (12.1–23) |
| σο (N) (95% CI) | 725.2 a,A (685.1–767.6) | 576.4 b,A (559.8–593.6) | 521.9 c,A (487.8–558.4) | 741.9 a,A (709.1–776.4) | 656.7 d,A (638.7–675.3) | |
| r2 | 0.93 | 0.92 | 0.96 | 0.94 | 0.91 | |
| CDC | Β (95% CI) | 12.9 a,A (9–18.4) | 14.4 a,A (10.3–19.9) | 7.9 a,A (5.6–11.3) | 8.1 a,A (5.6–11.7) | 8.9 a,B (6.3–12.0) |
| σο (N) (95% CI) | 736.3 a,A (710.4–763.1) | 554.5 b,A (536.8–572.7) | 459.4 c,B (433.5–486.9) | 708.8 a,A,B (670.1–749.8) | 566 b,B (537.3–596.2) | |
| r2 | 0.99 | 0.93 | 0.94 | 0.9 | 0.95 | |
| CNB | β (95% CI) | 5.4 a,B (3.9–7.5) | 9.1 a,A (6.4–12.9) | 7.3 a,A (5.1–10.4) | 7.9 a,A (5.6–11) | 7.6 a,B (5.5–10.6) |
| σο (N) (95% CI) | 670.9 a,A (615.7–731.1) | 505.1 b,B (480.1–531.4) | 344.9 c,C (323.8–367.4) | 649.2 a,B (612.1–688.5) | 625.1 a,A,B (588.1–664.4) | |
| r2 | 0.93 | 0.96 | 0.98 | 0.99 | 0.97 | |
| Type of Failure | Core | Post | Total per Core (n = 100) | ||||
|---|---|---|---|---|---|---|---|
| ARL | FBK | GLX | MTP | PRW | |||
| I | CPC | 6 (30%) | 0 (-) | 17 (85) | 0 (-) | 18 (90%) | 41 |
| II | 0 (-) | 3 (15%) | 0 (-) | 1 (5%) | 2 (10%) | 6 | |
| III | 2 (10%) | 0 (-) | 3 (15%) | 1 (5%) | 0 (-) | 6 | |
| IV | 12 (60%) | 17 (85%) | 0 (-) | 18 (90%) | 0 (-) | 47 | |
| I | CDC | 9 (45%) | 6 (30%) | 20 (100%) | 3 (15%) | 19 (95%) | 57 |
| II | 4 (20%) | 14 (70%) | 0 (-) | 7 (35%) | 1 (5%) | 26 | |
| III | 1 (5%) | 0 (-) | 0 (-) | 0 (-) | 0 (-) | 1 | |
| IV | 6 (30%) | 0 (-) | 0 (-) | 10 (50%) | 0 (-) | 16 | |
| I | CNB | 3 (15%) | 0 (-) | 19 (95%) | 0 (-) | 19 (95%) | 41 |
| II | 0 (-) | 5 (25%) | 0 (-) | 5 (25%) | 1 (5%) | 11 | |
| III | 0 (-) | 0 (-) | 1 (5%) | 9 (45%) | 0 (-) | 10 | |
| IV | 17 (85%) | 15 (75%) | 0 (-) | 6 (30%) | 0 (-) | 38 | |
| I | Total per post (n = 60) | 18 (30%) | 6 (10%) | 56 (93%) | 3 (5%) | 56 (93%) | |
| II | 4 (7%) | 22 (37%) | 0 (-) | 13 (22%) | 4 (7%) | ||
| III | 3 (5%) | 0 (-) | 4 (7%) | 10 (17%) | 0 (-) | ||
| IV | 35 (58%) | 32 (53%) | 0 (-) | 34 (56%) | 0 (-) | ||
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fragkouli, M.; Tzoutzas, I.; Eliades, G. Bonding of Core Build-Up Composites with Glass Fiber-Reinforced Posts. Dent. J. 2019, 7, 105. https://doi.org/10.3390/dj7040105
Fragkouli M, Tzoutzas I, Eliades G. Bonding of Core Build-Up Composites with Glass Fiber-Reinforced Posts. Dentistry Journal. 2019; 7(4):105. https://doi.org/10.3390/dj7040105
Chicago/Turabian StyleFragkouli, Margarita, Ioannis Tzoutzas, and George Eliades. 2019. "Bonding of Core Build-Up Composites with Glass Fiber-Reinforced Posts" Dentistry Journal 7, no. 4: 105. https://doi.org/10.3390/dj7040105
APA StyleFragkouli, M., Tzoutzas, I., & Eliades, G. (2019). Bonding of Core Build-Up Composites with Glass Fiber-Reinforced Posts. Dentistry Journal, 7(4), 105. https://doi.org/10.3390/dj7040105





