Survival of a Maxillary Incisor in an Adolescent Male 16 Years after Its Delayed Replantation
Abstract
1. Introduction
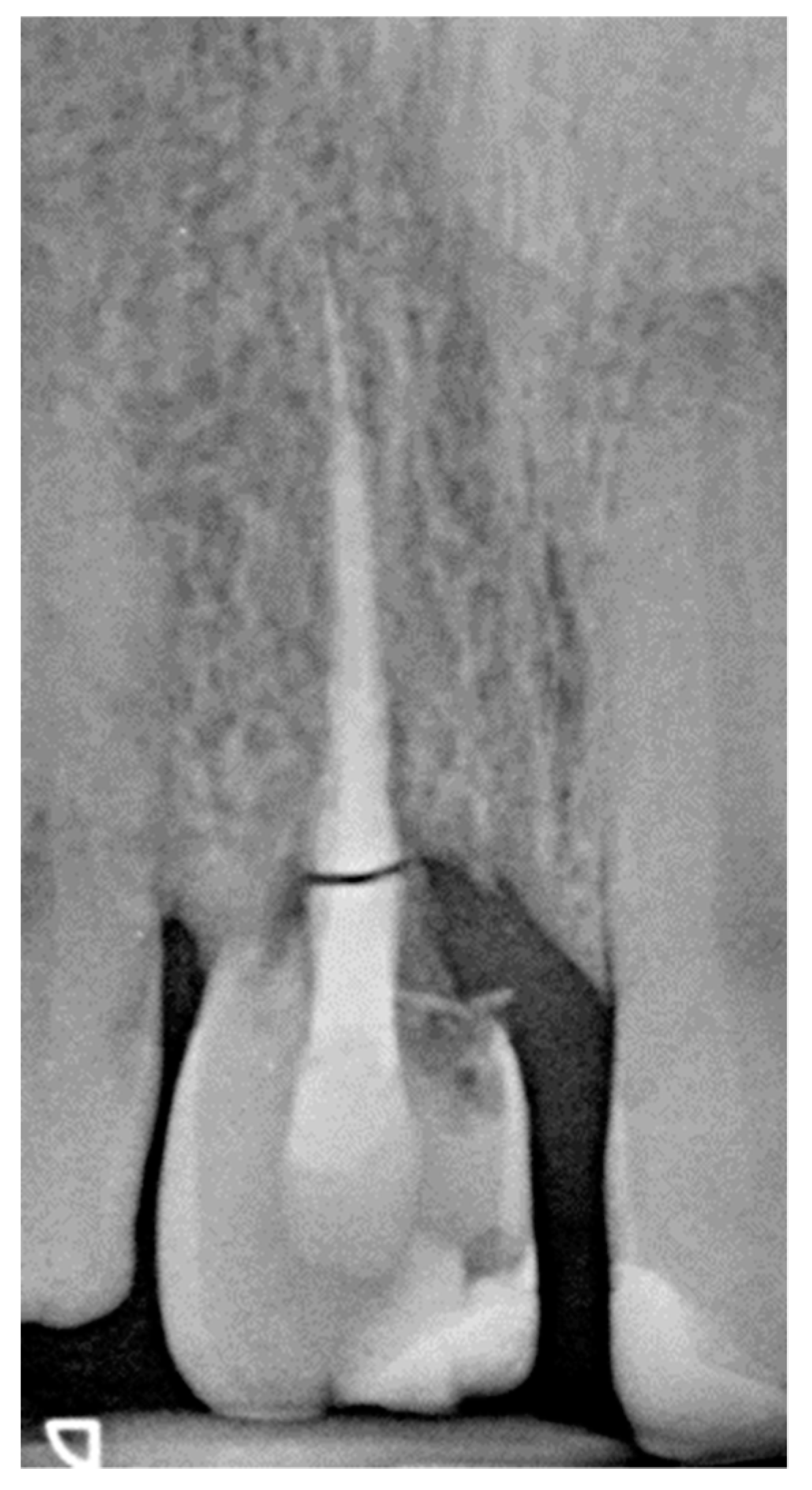
2. Case Presentation
3. Discussion
4. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Andreasen, J.O.; Andreasen, F.M.; Avulsions, J. Textbook and Color Atlas of Traumatic Injuries to the Teeth, 4th ed.; Andreasen, J.O., Andreasen, F.M., Andersson, I., Eds.; Blackwell Publishing Ltd.: Oxford, UK, 2007; pp. 444–488. [Google Scholar]
- Glendor, U. Aetiology and risk factors related to traumatic dental injuries—A review of the literature. Dent. Traumatol. 2009, 25, 19–31. [Google Scholar] [CrossRef] [PubMed]
- Trope, M. Clinical management of the avulsed tooth present strategies and future directions. Dent. Traumatol. 2002, 18, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Huang, G.T.; Sonoyama, W.; Liu, Y.; Liu, J.; Wang, S.; Shi, S. The hidden treasure in apical papilla: The potential role in pulp/dentin regeneration and bioroot engineering. J. Endod. 2008, 34, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Khinda, V.I.; Kaur, G.; Brar, G.S.; Kallar, S.; Khurana, H. Clinical and practical implications of storage media used for tooth avulsion. Int. J. Clin. Pediatr. Dent. 2017, 10, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Adnan, S.; Lone, M.M.; Khan, F.R.; Hussain, S.M.; Nagi, S.E. Which is the most recommended medium for the storage and transport of avulsed teeth? A systematic review. Dent. Traumatol. 2018, 34, 59–70. [Google Scholar] [CrossRef] [PubMed]
- Biagi, R. Pulp and periodontal healing after replantation of a maxillary immature incisor: A 13-year follow-up. Eur. J. Paediatr. Dent. 2014, 15, 195–198. [Google Scholar] [PubMed]
- Holan, G.; Shmueli, Y. Knowledge of physicians in hospital emergency rooms in Israel on their role in cases of avulsion of permanent incisors. Int. J. Paediatr. Dent. 2003, 13, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Ulusoy, A.T.; Onder, H.; Cetin, B.; Kaya, S. Knowledge of medical hospital emergency physicians about the first-aid management of traumatic tooth avulsion. Int. J. Paediatr. Dent. 2012, 22, 211–216. [Google Scholar] [CrossRef] [PubMed]
- Andersson, L.; Andreasen, J.O.; Day, P.; Heithersay, G.; Trope, M.; Diangelis, A.J.; Kenny, D.J.; Sigurdsson, A.; Bourguignon, C.; Flores, M.T.; et al. International Association of Dental Traumatology guidelines for the management of traumatic dental injuries: 2. Avulsion of permanent teeth. Dent. Traumatol. 2012, 28, 88–96. [Google Scholar] [CrossRef] [PubMed]
- Stewart, C.J.; Elledge, R.O.; Kinirons, M.J.; Welbury, R.R. Factors affecting the time of pulp extirpation in a sample of 66 replanted avulsed teeth in children and adolescents. Dent. Traumatol. 2008, 24, 625–627. [Google Scholar] [CrossRef] [PubMed]
- Hinckfuss, S.E.; Messer, L.B. An evidence-based assessment of the clinical guidelines for replanted avulsed teeth. Part I: Timing of pulp extirpation. Dent. Traumatol. 2009, 25, 32–42. [Google Scholar] [PubMed]
- Andersson, L.; Bodin, I.; Sörensen, S. Progression of root resorption following replantation of human teeth after extended extraoral storage. Endod. Dent. Traumatol. 1989, 5, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Malmgren, B.; Malmgren, O. Rate of infraposition of reimplanted ankylosed incisors related to age and growth in children and adolescents. Dent. Traumatol. 2002, 18, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Steiner, D.R. Avulsed maxillary central incisors: The case of replantation. Am. J. Orthod. Dentofacial Orthop. 2012, 142, 8–17. [Google Scholar] [CrossRef] [PubMed]
- Hinckfuss, S.E.; Messer, L.B. Splint duration and periodontal outcome for replanted avulsed teeth: A systematic review. Dent. Traumatol. 2009, 25, 150–157. [Google Scholar] [CrossRef] [PubMed]










© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Biagi, R.; Maccagnola, V. Survival of a Maxillary Incisor in an Adolescent Male 16 Years after Its Delayed Replantation. Dent. J. 2019, 7, 101. https://doi.org/10.3390/dj7040101
Biagi R, Maccagnola V. Survival of a Maxillary Incisor in an Adolescent Male 16 Years after Its Delayed Replantation. Dentistry Journal. 2019; 7(4):101. https://doi.org/10.3390/dj7040101
Chicago/Turabian StyleBiagi, Roberto, and Valerio Maccagnola. 2019. "Survival of a Maxillary Incisor in an Adolescent Male 16 Years after Its Delayed Replantation" Dentistry Journal 7, no. 4: 101. https://doi.org/10.3390/dj7040101
APA StyleBiagi, R., & Maccagnola, V. (2019). Survival of a Maxillary Incisor in an Adolescent Male 16 Years after Its Delayed Replantation. Dentistry Journal, 7(4), 101. https://doi.org/10.3390/dj7040101





