Adhesive Systems Used in Indirect Restorations Cementation: Review of the Literature
Abstract
1. Introduction
1.1. Classification of Adhesive Systems
1.2. Etch–Rinse Adhesive Systems
1.3. Self-Etch Adhesives
- (1)
- A cleaning effect on the surface, chemical and mechanical, which starts with the removal of the periphery of the enamel prisms with regular wear of the surface. During the removal of the acid, the dissolved salts are also removed in the created porosities;
- (2)
- A partial demineralization effect that facilitates the crosslinking of the adhesive by means of the generated micro-porosities and the collagen network (hybridization); and
- (3)
- The chemical interaction of the weak acid with the residual hydroxyapatite, giving rise to a network of collagen coated by hydroxyapatite with exposed fibrils, describing a double adhesion both mechanical and chemical. This reaction occurs for example with the system Clearfil SE where the monomer 10 MDP (10-methacryloyloxydecyl dihydrogen phosphate) interacts with the hydroxyapatite of the barrel [32].
1.4. Causes of Failure of Indirect Restorations
1.5. Effect of Water
2. Materials and Methods
- Population: Scientific articles on adhesive systems used in indirect restorations.
- Intervention: Testing of bond strength, resistance to shear and microtraction of the adhesive systems used in indirect restorations.
- Comparison: Different types of adhesive systems, engraving and rinsing, self-etching and universal systems.
- Outcomes: bond strength in MPa of the different adhesive systems evaluated.
2.1. Inclusion Criteria
2.2. Exclusion Criteria
2.3. Search Terms
2.4. Data Collection
3. Results
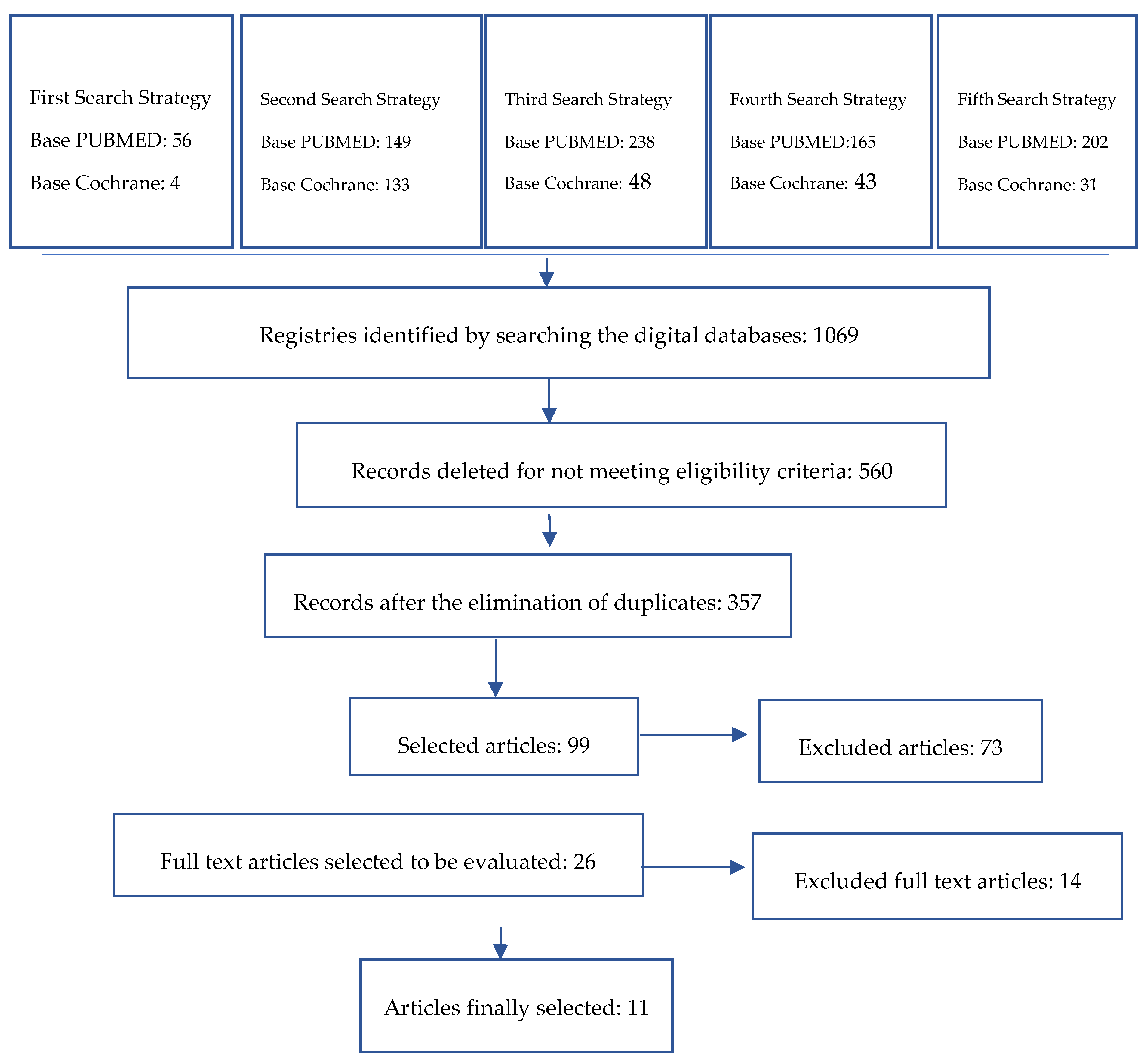
3.1. Search Strategy
3.1.1. Study Quality Assessment
3.1.2. Bond Strength
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- Deligeorgi, V.; Mjör, I.A.; Wilson, N.H.H.F. An Overview of and Replacement Reasons for the of Restorations Placement. Prim. Dent. Care 2001, 8, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Angeletaki, F.; Gkogkos, A.; Papazoglou, E.; Kloukos, D. Direct versus indirect inlay/onlay composite restorations in posterior teeth. A systematic review and meta-analysis. J. Dent. 2016, 53, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Collares, K.; Corrêa, M.B.; Laske, M.; Kramer, E.; Reiss, B.; Moraes, R.R.; Opdam, N.J. A practice-based research network on the survival of ceramic inlay/onlay restorations. Dent. Mater. 2016, 32, 687–694. [Google Scholar] [CrossRef] [PubMed]
- Guarda, G.B.; Correr, A.B.; Gonçalves, L.S.; Costa, A.R.; Borges, G.A.; Sinhoreti, M.A.C.; Correr-Sobrinho, L. Effects of Surface Treatments, Thermocycling, and Cyclic Loading on the Bond Strength of a Resin Cement Bonded to a Lithium Disilicate Glass Ceramic. Oper. Dent. 2013, 38, 208–217. [Google Scholar] [CrossRef] [PubMed]
- Song, X.-F.; Ren, H.-T.; Yin, L. Machinability of lithium disilicate glass ceramic in in vitro dental diamond bur adjusting process. J. Mech. Behav. Biomed. Mater. 2016, 53, 78–92. [Google Scholar] [CrossRef] [PubMed]
- D’Arcangelo, C.; Vanini, L.; Casinelli, M.; Frascaria, M.; De Angelis, F.; Vadini, M.; D’Amario, M. Adhesive Cementation of Indirect Composite Inlays and Onlays: A Literature Review. Compend. Contin. Educ. Dent. 2015, 36, 9. [Google Scholar]
- Yoshihara, K.; Nagaoka, N.; Sonoda, A.; Maruo, Y.; Makita, Y.; Okihara, T.; Van Meerbeek, B. Effectiveness and stability of silane coupling agent incorporated in ‘universal’ adhesives. Dent. Mater. 2016, 32, 1218–1225. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.-Y.; Cho, G.-Y.; Roh, B.-D.; Shin, Y. Effect of Curing Mode on Shear Bond Strength of Self-Adhesive Cement to Composite Blocks. Materials 2016, 9, 210. [Google Scholar] [CrossRef]
- Dos Santos, V.H.; Griza, S.; de Moraes, R.R.; Faria-e-Silva, A.L. Bond strength of self-adhesive resin cements to composite submitted to different surface pretreatments. Restor. Dent. Endod. 2014, 39, 12. [Google Scholar] [CrossRef]
- Makkar, S.; Malhotra, N. Self-adhesive resin cements: A new perspective in luting technology. Dent. Update 2013, 40, 758–768. [Google Scholar] [CrossRef]
- Passia, N.; Lehmann, F.; Freitag-Wolf, S.; Kern, M. Tensile bond strength of different universal adhesive systems to lithium disilicate ceramic. J. Am. Dent. Assoc. 2015, 146, 729–734. [Google Scholar] [CrossRef] [PubMed]
- Kameyama, A.; Bonroy, K.; Elsen, C.; LŘhrs, A.K.; Suyama, Y.; Peumans, M.; De Munck, J. Luting of CAD/CAM ceramic inlays: Direct composite versus dual-cure luting cement. Biomed. Mater. Eng. 2015, 25, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Blatz, M.B.; Vonderheide, M.; Conejo, J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J. Dent. Res. 2018, 97, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Baader, K.; Hiller, K.A.; Buchalla, W.; Schmalz, G.; Federlin, M. Self-adhesive Luting of Partial Ceramic Crowns: Selective Enamel Etching Leads to Higher Survival after 6.5 Years In Vivo. J. Adhes. Dent. 2016, 18, 69–79. [Google Scholar] [PubMed]
- Tolidis, K.; Papadogiannis, D.; Papadogiannis, Y.; Gerasimou, P. Dynamic and static mechanical analysis of resin luting cements. J. Mech. Behav. Biomed. Mater. 2012, 6, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kern, M. Bonding to oxide ceramics—Laboratory testing versus clinical outcome. Dent. Mater. 2015, 31, 8–14. [Google Scholar] [CrossRef]
- Passos, S.P.; Kimpara, E.T.; Bottino, M.A.; Júnior, S.; Coelho, G.; Rizkalla, A.S. Bond Strength of Different Resin Cement and Ceramic Shades Bonded to Dentin. J. Adhes. Dent. 2013, 15, 461–466. [Google Scholar] [PubMed]
- Rohr, N.; Fischer, J. Effect of aging and curing mode on the compressive and indirect tensile strength of resin composite cements. Head Face Med. 2017, 13, 22. [Google Scholar] [CrossRef]
- Tian, T.; Tsoi, J.K.-H.; Matinlinna, J.P.; Burrow, M.F. Aspects of bonding between resin luting cements and glass ceramic materials. Dent. Mater. 2014, 30, e147–e162. [Google Scholar] [CrossRef]
- Park, J.-H.; Choi, Y.-S. Microtensile bond strength and micromorphologic analysis of surface-treated resin nanoceramics. J. Adv. Prosthodont. 2016, 8, 275. [Google Scholar] [CrossRef]
- Pekperdahci, T.; Turkoz, Y.; Ozan, O.; Seker, E. The effects of different adhesive agents on the shear bond strength of a self-adhesive resin cement. J. Appl. Biomater. Funct. Mater. 2012, 2, 149–156. [Google Scholar] [CrossRef] [PubMed]
- Spitznagel, F.A.; Horvath, S.D.; Guess, P.C.; Blatz, M.B. Resin Bond to Indirect Composite and New Ceramic/Polymer Materials: A Review of the Literature. J. Esthet. Restor. Dent. 2014, 26, 382–393. [Google Scholar] [CrossRef] [PubMed]
- Migliau, G. Classification review of dental adhesive systems: From the IV generation to the universal type. Ann. Stomatol. 2017, 8, 1. [Google Scholar] [CrossRef] [PubMed]
- Van Landuyt, K.L.; Snauwaert, J.; De Munck, J.; Peumans, M.; Yoshida, Y.; Poitevin, A.; Van Meerbeek, B. Systematic review of the chemical composition of contemporary dental adhesives. Biomaterials 2007, 28, 3757–3785. [Google Scholar] [CrossRef] [PubMed]
- Perdigão, J.; Reis, A.; Loguercio, A.D. Dentin Adhesion and MMPs: A Comprehensive Review: Dentin Adhesion and MMPs. J. Esthet. Restor. Dent. 2013, 25, 219–241. [Google Scholar] [CrossRef] [PubMed]
- Ferreira-Filho, R.C.; Ely, C.; Amaral, R.C.; Rodrigues, J.A.; Roulet, J.F.; Cassoni, A.; Reis, A.F. Effect of Different Adhesive Systems Used for Immediate Dentin Sealing on Bond Strength of a Self-Adhesive Resin Cement to Dentin. Oper. Dent. 2018, 43, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Albaladejo, A.; Osorio, R.; Toledano, M.; Ferrari, M. Hybrid layers of etch-and-rinse versus self-etching adhesive systems. Med. Oral Patol. Oral Cir. Bucal 2010, 15, e112–e118. [Google Scholar] [CrossRef] [PubMed]
- D’Arcangelo, C.; Angelis, F.D.; Vadini, M.; D’Amario, M.; Caputi MD, S. Fracture Resistance and Deflection of Pulpless Anterior Teeth Restored with Composite or Porcelain Veneers. J. Endod. 2010, 36, 153–156. [Google Scholar] [CrossRef]
- Ekambaram, M.; Yiu, C.K.Y.; Matinlinna, J.P. An overview of solvents in resin–dentin bonding. Int. J. Adhes. Adhes. 2015, 57, 22–33. [Google Scholar] [CrossRef]
- Ozturk, N.; Aykent, F. Dentin bond strengths of two ceramic inlay systems after cementation with three different techniques and one bonding system. J. Prosthet. Dent. 2003, 89, 275–281. [Google Scholar] [CrossRef]
- Van Meerbeek, B.; De Munck, J.; Yoshida, Y.; Inoue, S.; Vargas, M.; Vijay, P.; Vanherle, G. Adhesion to Enamel and Dentin: Current Status and Future Challenges. Oper. Dent. 2003, 28, 215–235. [Google Scholar] [PubMed]
- Haller, B. Which self-etch bonding systems are suitable for which clinical indications? Quintessence Int. 2013, 44, 17. [Google Scholar]
- Tay, F.R.; Carvalho, R. Single-step, self-etch adhesives behave as permeable membranes after polymerization. Part, I. Bond strength and morphologic evidence. Am. J. Dent. 2004, 17, 271–278. [Google Scholar] [PubMed]
- Tay, F.R.; Yiu, C.K.Y. Single-step, self-etch adhesives behave as permeable membranes after polymerization. Part II. Silver tracer penetration evidence. Am. J. Dent. 2004, 17, 315–322. [Google Scholar]
- El Zohairy, A.A.; De Gee, A.J.; Mohsen, M.M.; Feilzer, A.J. Effect of conditioning time of self-etching primers on dentin bond strength of three adhesive resin cements. Dent. Mater. 2005, 21, 83–93. [Google Scholar] [CrossRef]
- Pashley, D.H.; Tay, F.R.; Breschi, L.; Tjäderhane, L.; Carvalho, R.M.; Carrilho, M.; Tezvergil-Mutluay, A. State of the art etch-and-rinse adhesives. Dent. Mater. 2011, 27, 1–16. [Google Scholar] [CrossRef]
- Opdam, N.J.M.; van de Sande, F.H.; Bronkhorst, E.; Cenci, M.S.; Bottenberg, P.; Pallesen, U.; Van Dijken, J.W. Longevity of Posterior Composite Restorations: A Systematic Review and Meta-analysis. J. Dent. Res. 2014, 93, 943–949. [Google Scholar] [CrossRef]
- Van Dijken, J.W.V.; Hasselrot, L. A prospective 15-year evaluation of extensive dentin–enamel-bonded pressed ceramic coverages. Dent. Mater. 2010, 26, 929–939. [Google Scholar] [CrossRef]
- Kuper, N.K.; Opdam, N.J.M.; Bronkhorst, E.M.; Huysmans, M.C.D.N.J.M. The influence of approximal restoration extension on the development of secondary caries. J. Dent. 2012, 40, 241–247. [Google Scholar] [CrossRef]
- Federlin, M.; Hiller, K.-A.; Schmalz, G. Effect of selective enamel etching on clinical performance of CAD/CAM partial ceramic crowns luted with a self-adhesive resin cement. Clin. Oral Investig. 2014, 18, 1975–1984. [Google Scholar] [CrossRef]
- Schenke, F.; Federlin, M.; Hiller, K.-A.; Moder, D.; Schmalz, G. Controlled, prospective, randomized, clinical evaluation of partial ceramic crowns inserted with RelyX Unicem with or without selective enamel etching. Results after 2 years. Clin. Oral Investig. 2012, 16, 451–461. [Google Scholar] [CrossRef] [PubMed]
- Nikolaus, F.; Wolkewitz, M.; Hahn, P. Bond strength of composite resin to glass ceramic after saliva contamination. Clin. Oral Investig. 2013, 17, 751–755. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Sun, M.; Zheng, Z.; Shinya, A.; Han, J.; Lin, H.; Shinya, A. Effects of rotating fatigue on the mechanical properties of microhybrid and nanofiller-containing composites. Dent. Mater. J. 2013, 32, 476–483. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Rohr, N.; Fischer, J. Tooth surface treatment strategies for adhesive cementation. J. Adv. Prosthodont. 2017, 9, 85. [Google Scholar] [CrossRef] [PubMed]
- Cristian, A.; Jeanette, L.; Francisco, M.-R.; Guillermo, P. Correlation between Microleakage and Absolute Marginal Discrepancy in Zirconia Crowns Cemented with Four Resin Luting Cements: An In Vitro Study. Int. J. Dent. 2016, 2016, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Agee, K.A.; Prakki, A.; Abu-Haimed, T.; Naguib, G.H.; Nawareg, M.A.; Tezvergil-Mutluay, A.; Brackett, M. Water distribution in dentin matrices: Bound vs. unbound water. Dent. Mater. 2015, 31, 205–216. [Google Scholar] [CrossRef] [PubMed]
- Cervino, G.; Fiorillo, L.; Spagnuolo, G.; Bramanti, E.; Laino, L.; Lauritano, F.; Cicciù, M. Interface between MTA and dental bonding agents: Scanning electron microscope evaluation. J. Int. Soc. Prev. Community Dent. 2017, 7, 64. [Google Scholar] [PubMed]
- Pucci, C.R.; Gu, L.-S.; Zeng, C.; Gou, Y.-P.; Tay, F.R.; Niu, L.-N. Susceptibility of contemporary single-bottle self-etch dentine adhesives to intrinsic water permeation. J. Dent. 2017, 66, 52–61. [Google Scholar] [CrossRef] [PubMed]
- de Araújo Matuda, L.S.; Marchi, G.M.; Aguiar, T.R.; Leme, A.A.; Ambrosano, G.M.; Bedran-Russo, A.K. Dental adhesives and strategies for displacement of water/solvents from collagen fibrils. Dent. Mater. 2016, 32, 723–731. [Google Scholar] [CrossRef] [PubMed]
- Hutton, B.; Catalá-López, F.; Moher, D. La extensión de la declaración PRISMA para revisiones sistemáticas que incorporan metaanálisis en red: PRISMA-NMA. Med. Clin. 2016, 147, 262–266. [Google Scholar] [CrossRef]
- Pamato, S.; do Valle, A.; de Andrade, G.; Vidotti, H.; So, M.; Pereira, J. Does hybridized dentin affect bond strength of self-adhesive resin cement? J. Clin. Exp. Dent. 2016, 8, e409. [Google Scholar] [CrossRef] [PubMed]
- Chávez-Lozada, J.; Urquía-Morales, C. In-vitro evaluation of bond strength of four self-etching cements. Acta Odontol. Latinoam. 2017, 30, 8. [Google Scholar]
- Zorzin, J.; Petschelt, A.; Ebert, J.; Lohbauer, U. pH neutralization and influence on mechanical strength in self-adhesive resin luting agents. Dent. Mater. 2012, 28, 672–679. [Google Scholar] [CrossRef] [PubMed]
- Costa, L.A.; Carneiro, K.K.; Tanaka, A.; Lima, D.M.; Bauer, J. Evaluation of pH, ultimate tensile strength, and micro-shear bond strength of two self-adhesive resin cements. Braz. Oral Res. 2014, 28, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Abo-Hamar, S.E.; Hiller, K.-A.; Jung, H.; Federlin, M.; Friedl, K.-H.; Schmalz, G. Bond strength of a new universal self-adhesive resin luting cement to dentin and enamel. Clin. Oral Investig. 2005, 9, 161–167. [Google Scholar] [CrossRef] [PubMed]
- Aguiar, T.R.; Vermelho, P.M.; André, C.B.; Giannini, M. Interfacial ultramorphology evaluation of resin luting cements to dentin: A correlative scanning electron microscopy and transmission electron microscopy analysis: Ultramorphology Of Resin Cements To Dentin. Microsc. Res. Tech. 2013, 76, 1234–1239. [Google Scholar] [CrossRef] [PubMed]
- Öztürk, E.; Bolay, Ş.; Hickel, R.; Ilie, N. Shear bond strength of porcelain laminate veneers to enamel, dentine and enamel–dentine complex bonded with different adhesive luting systems. J. Dent. 2013, 41, 97–105. [Google Scholar] [CrossRef]
- Roperto, R.; Akkus, A.; Akkus, O.; Lang, L.; Sousa-Neto, M.D.; Teich, S.; Porto, T.S. Effect of different adhesive strategies on microtensile bond strength of computer aided design/computer aided manufacturing blocks bonded to dentin. Dent. Res. J. 2016, 13, 117. [Google Scholar] [CrossRef]
- Takahashi, H. Effect of calcium salt of 10-methacryloyloxydecyl dihydrogen phosphate produced on the bond durability of one-step self-etch adhesive. Dent. Mater. J. 2014, 33, 394–401. [Google Scholar] [CrossRef]
- Skupien, J.A.; Porto, J.A.S.; Münchow, E.A.; Cenci, M.S.; Pereira-Cenci, T. Impairment of resin cement application on the bond strength of indirect composite restorations. Braz. Oral Res. 2015, 29, 1–7. [Google Scholar] [CrossRef]
- Lorenzoni e Silva, F.; Pamato, S.; Kuga, M.; So, M.; Pereira, J. Bond strength of adhesive resin cement with different adhesive systems. J. Clin. Exp. Dent. 2016. [Google Scholar] [CrossRef] [PubMed]
- Peumans, M.; De Munck, J.; Mine, A.; Van Meerbeek, B. Clinical effectiveness of contemporary adhesives for the restoration of non-carious cervical lesions. A systematic review. Dent. Mater. 2014, 30, 1089–1103. [Google Scholar] [CrossRef] [PubMed]
- Bacchi, A.; Abuna, G.; Babbar, A.; Sinhoreti, M.A.; Feitosa, V.P. Influence of 3-month Simulated Pulpal Pressure on the Microtensile Bond Strength of Simplified Resin Luting Systems. J. Adhes. Dent. 2015, 3, 265–271. [Google Scholar]
- De Alexandre, R.; Santana, V.; Kasaz, A.; Arrais, C.; Rodrigues, J.; Reis, A. Effect of Long-term Simulated Pulpal Pressure on the Bond Strength and Nanoleakage of Resin-luting Agents With Different Bonding Strategies. Oper. Dent. 2014, 39, 508–520. [Google Scholar] [CrossRef]
- Han, L.; Okamoto, A.; Fukushima, M.; Okiji, T. Evaluation of Physical Properties and Surface Degradation of Self-adhesive Resin Cements. Dent. Mater. J. 2007, 26, 906–914. [Google Scholar] [CrossRef]
- Hikita, K.; Van Meerbeek, B.; De Munck, J.; Ikeda, T.; Van Landuyt, K.; Maida, T.; Peumans, M. Bonding effectiveness of adhesive luting agents to enamel and dentin. Dent. Mater. 2007, 23, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Schenke, F.; Hiller, K.-A.; Schmalz, G.; Federlin, M. Marginal Integrity of Partial Ceramic Crowns Within Dentin with Different Luting Techniques and Materials. Oper. Dent. 2008, 33, 516–525. [Google Scholar] [CrossRef] [PubMed]
- Lin, J.; Shinya, A.; Gomi, H.; Shinya, A. Bonding of self-adhesive resin cements to enamel using different surface treatments: Bond strength and etching pattern evaluations. Dent. Mater. J. 2010, 29, 425–432. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Behr, M.; Hansmann, M.; Rosentritt, M.; Handel, G. Marginal adaptation of three self-adhesive resin cements vs. a well-tried adhesive luting agent. Clin. Oral Investig. 2009, 13, 459–464. [Google Scholar] [CrossRef]
- Suyama, Y.; de Munck, J.; Cardoso, M.V.; Yamada, T.; Van Meerbeek, B. Bond durability of self-adhesive composite cements to dentine. J. Dent. 2013, 41, 908–917. [Google Scholar] [CrossRef]
- Peumans, M.; Voet, M.; De Munck, J.; Van Landuyt, K.; Van Ende, A.; Van Meerbeek, B. Four-year clinical evaluation of a self-adhesive luting agent for ceramic inlays. Clin. Oral Investig. 2013, 17, 739–750. [Google Scholar] [CrossRef] [PubMed]
- Aguiar, T.R.; André, C.B.; Correr-Sobrinho, L.; Arrais, C.A.G.; Ambrosano, G.M.B.; Giannini, M. Effect of storage times and mechanical load cycling on dentin bond strength of conventional and self-adhesive resin luting cements. J. Prosthet. Dent. 2014, 111, 404–410. [Google Scholar] [CrossRef] [PubMed]
- Figueiredo, R.J.A.; Andrade, A.K.M.; Duarte, R.M. In vitro evaluation of incompatibility between simplified adhesive systems and dual-cure resin cement. Rev. Gaúch. Odontol. 2012, 60, 3. [Google Scholar]
- Stawarczyk, B.; Krawczuk, A.; Ilie, N. Tensile bond strength of resin composite repair in vitro using different surface preparation conditionings to an aged CAD/CAM resin nanoceramic. Clin. Oral Investig. 2015, 19, 299–308. [Google Scholar] [CrossRef] [PubMed]
- Azad, E.; Atai, M.; Zandi, M.; Shokrollahi, P.; Solhi, L. Structure-properties relationships in dental adhesives: Effect of initiator, matrix monomer structure, and nano-filler incorporation. Dent. Mater. 2018, 34, 1263–1270. [Google Scholar] [CrossRef] [PubMed]
- Belli, R.; Kreppel, S.; Petschelt, A.; Hornberger, H.; Boccaccini, A.R.; Lohbauer, U. Strengthening of dental adhesives via particle reinforcement. J. Mech. Behav. Biomed. Mater. 2014, 37, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Garcia, I.; Leitune, V.; Samuel, S.; Collares, F. Influence of Different Calcium Phosphates on an Experimental Adhesive Resin. J. Adhes. Dent. 2017, 19, 379–384. [Google Scholar]
- Fadaie, P.; Atai, M.; Imani, M.; Karkhaneh, A.; Ghasaban, S. Cyanoacrylate–POSS nanocomposites: Novel adhesives with improved properties for dental applications. Dent. Mater. 2013, 29, e61–e69. [Google Scholar] [CrossRef]
- Hammad, S.M.; El-Wassefy, N.; Maher, A.; Fawakerji, S.M. Effect of nanotechnology in self-etch bonding systems on the shear bond strength of stainless steel orthodontic brackets. Dent. Press J. Orthod. 2017, 22, 47–56. [Google Scholar] [CrossRef]
| Study | Teeth Randomization | Caries-Free Teeth | Control Group | Samples with Similar Dimensions | Evaluation of Failure Mode | Description of Coefficient of Variation | Sample Size Calculation | Blinding of the Examiner | Risk of Bias |
|---|---|---|---|---|---|---|---|---|---|
| Pamato | Yes | Yes | Yes | Yes | Yes | No | No | No | Medium |
| Aguiar | Yes | yes | No | Yes | Yes | No | No | No | Medium |
| Ozturk | Yes | Yes | No | Yes | Yes | No | No | No | Medium |
| Skupien | Yes | Yes | No | Yes | Yes | Yes | No | Yes | Low |
| Lorenzoni | Yes | Yes | No | Yes | Yes | No | No | No | Medium |
| Pekperdahci | Yes | Yes | Yes | Yes | Yes | No | No | No | Medium |
| Chávez | Yes | Yes | Yes | Yes | Yes | Yes | No | No | Low |
| Vaz | Yes | No | Yes | Yes | Yes | No | No | No | High |
| Bacchi | Yes | Yes | Yes | Yes | Yes | No | No | No | Low |
| Alexandre | Yes | Yes | No | Yes | Yes | No | No | No | Medium |
| Roperto | Yes | Yes | Yes | Yes | No | No | No | No | Medium |
| Author | 3-Step Adhesive System | Cement | Enamel Bond Strength (MPa) | Dentin Bond Strength (MPa) |
|---|---|---|---|---|
| Pamato | Optibond | U200 | Data Not Available | 13.3 |
| Pamato | Adper Scotchbond | U200 | Data Not Available | 16 |
| Aguiar | Adper Scotchbond | Rely X ARC | Data Not Available | 17.1 |
| Ozturk | Adper Scotchbond | RelyX Veneer | 22.46 | 5.42 |
| Ozturk | Heliobond Syntac | Variolink II | 23.64 | 13.78 |
| Ozturk | Heliobond Syntac | Variolink Veneer | 24.76 | 13.84 |
| Skupien | Adper Scotchbond | RelyX ARC | Data Not Available | 20.29 |
| Lorenzoni | Adper Scotchbond | Duo Link | Data Not Available | 11.6 |
| Lorenzoni | Optibond | Duo Link | Data Not Available | 12.29 |
| Lorenzoni | All Bond 3 | Duo Link | Data Not Available | 6.16 |
| Author | 2-Step Adhesive System | Cement | Enamel Bond Strength (MPa) | Dentin Bond Strength (MPa) |
|---|---|---|---|---|
| Pamato | Adper Single Bond 2 | U200 | Data Not Available | 15.79 |
| Pekperdahci | Adper Single Bond 2 | RelyX ARC | Data Not Available | 370.07 ∗ |
| Pekperdahci | Adper Single Bond 2 | RelyX Unicem | Data Not Available | 96.56 ∗ |
| Chavez | Adper Single Bond 2 | RelyX ARC | Data Not Available | 15.52 |
| Vaz | All Bond 2 | C&B Cement | Data Not Available | 19.5 |
| Vaz | Adper Single Bond 2 | RelyX ARC | Data Not Available | 40.8 |
| Bacchi | Adper Single Bond 2 | RelyX ARC | Data Not Available | 25 |
| Alexandre | Adper Single Bond 2 | RelyX ARC | Data Not Available | 34.8 |
| Skupien | Adper single Bond 2 | RelyX ARC | Data Not Available | 17.68 |
| Roperto | Primer and Bond NT | Calibra | Data Not Available | 17.68 |
| Lorenzoni | Adper Single Bond 2 | Duo Link | Data Not Available | 14.5 |
| Author | 1-Step Adhesive System | Cement | Enamel Bond Strength (MPa) | Dentine Bond Strength (MPa) |
|---|---|---|---|---|
| Pamato | Bond Force | U200 | Data Not Available | 15.0 |
| Pekperdahci | Adper Prompt | Rely X Unicem | Data Not Available | 77.06 ∗ |
| Aguiar | Clearfil DC Bond | Clearfil Esthetic Cement | Data Not Available | 13.3 |
| Bacchi | ED Primer | Panavia F2.0 | Data Not Available | 15 |
| Lorenzoni | Bond Force | Duo Link | Data Not Available | 9.4 |
| Author | 2-Step System | Cement | Enamel Bond Strength (MPa) | Dentine Bond Strength (MPa) |
|---|---|---|---|---|
| Alexandre | Panavia 21 | Panavia F2.0 | Data Not Available | 7.8 |
| Alexandre | Clearfil SE Bond | Panavia F2.0 | Data Not Available | 38.0 |
| Roperto | Clearfil SE Bond | Panavia F2.0 | Data Not Available | 12.22 |
| Author | Universal Adhesive System | Cement | Enamel Bond Strength (MPa) | Dentine Bond Strength (MPa) |
|---|---|---|---|---|
| Pamato | Single Bond Universal | U200 | Data Not Available | 12.6 |
| Lorenzoni | Single Bond Universal | Duo Link | Data Not Available | 8.3 |
| Author | Test | Aging | Storage | Highest Value/Lowest Value (MPa) |
|---|---|---|---|---|
| Saulo Pamato | Microshear bond strength | ______________ | _____________ | Adper Single Bond 2: 16<break/>U 200: 11.190 |
| Pekperdahci | Microshear bond strength | Water 5 °C/55 °C for 10,000 cycles | Distilled water at 37 °C for two days | ARC Single Bond 2: 370.07 Relyx Unicem/Adper Prompt 77.06 |
| Chávez | Microshear bond strength | _____________ | Distilled water and kept at a constant temperature of 37 °C | Relyx ARC Single Bond 2: 15.52 Set PP 3.17 |
| Ozturk | Microshear bond strength | Thermocycled between 5 °C and 55 °C in Deionized water for 5000 cycles. | Distilled water for 24 h at 37 °C | Variolink Venner/Heliobond: 24.76 (enamel) RelyX Veneer/Adper Scottchbond: 5.42 (dentin) |
| Lorenzoni | Microshear bond strength | ______________ | ________________ | Adper Single Bond 2/Duo Link: 14.5 All Bondl/Duo Link: 6.16 |
| Aguiar | Microtensile bond strength | Mechanical load cycling, submitted to 50,000 cycles | Artificial saliva for 1 day | Relyx Unicem: 21.3 Clearfil Esthetic Cement/Clearfil DC Bond: 13.3 |
| Vaz | Microtensile bond strength | ______________ | 37 °C and 100% relative humidity | Relyx ARC/Adper Single Bond 2: 40.8 C&B Cement/All-Bond 2: 19.5 |
| Bacchi | Microtensile bond strength | Pulpal pressure for 3 months | 20 cm distilled water | Relyx ARC/Adper single bond 2: 25 U200: 8 |
| Alexandre | Microtensile bond strength | Pulpal pressure for 24 h | Distilled water | Clearfil SE Bond/Panavia F: 38.0 Panavia 21/Panavia F2.0: 7.8 |
| Roperto | Microtensile bond strength | _______________ | Water for 24 h at 37 °C | Primer and Bond NT/Calibra: 17.68 Smart Cem: 6.48 |
| Skupien | Microtensile bond strength | Distilled water at 37 °C for 24 h | Adper Scotchbond/Relyx ARC: 20.29 U100: 9.69 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Abad-Coronel, C.; Naranjo, B.; Valdiviezo, P. Adhesive Systems Used in Indirect Restorations Cementation: Review of the Literature. Dent. J. 2019, 7, 71. https://doi.org/10.3390/dj7030071
Abad-Coronel C, Naranjo B, Valdiviezo P. Adhesive Systems Used in Indirect Restorations Cementation: Review of the Literature. Dentistry Journal. 2019; 7(3):71. https://doi.org/10.3390/dj7030071
Chicago/Turabian StyleAbad-Coronel, Cristian, Belén Naranjo, and Pamela Valdiviezo. 2019. "Adhesive Systems Used in Indirect Restorations Cementation: Review of the Literature" Dentistry Journal 7, no. 3: 71. https://doi.org/10.3390/dj7030071
APA StyleAbad-Coronel, C., Naranjo, B., & Valdiviezo, P. (2019). Adhesive Systems Used in Indirect Restorations Cementation: Review of the Literature. Dentistry Journal, 7(3), 71. https://doi.org/10.3390/dj7030071






