The Association between Tooth Loss and Alzheimer’s Disease: a Systematic Review with Meta-Analysis of Case Control Studies
Abstract
1. Introduction
Rational Meta Analysis
2. Materials and Methods
2.1. Eligibility Criteria
2.2. Research Methodology
2.3. Screening Methodology
3. Results
Study Characteristics and Data Extraction
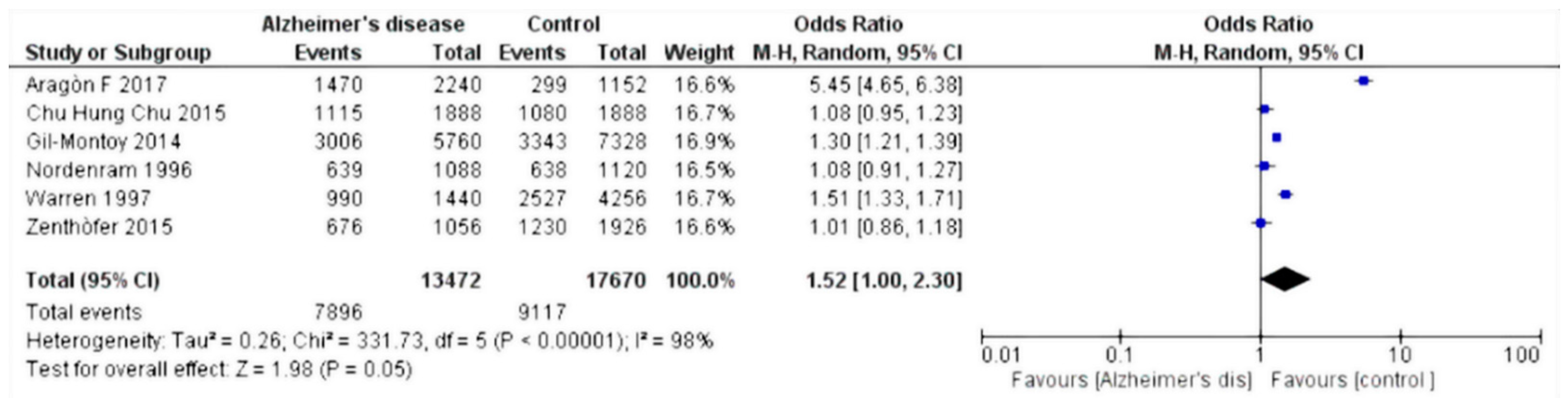
4. Data Analysis
5. Discussion
6. Conclusions
- Periodontitis, characterized by local inflammation and bacterial invasion, is one of the main causes of dental loss in adults. Local chronic inflammation could lead to the precipitation of β-amyloid (supported by a subacute inflammatory process at the CNS level). Furthermore, it is well known that different species of bacteria, endotoxins, and cytokines can reach the CNS.
- Dental elements are important in the masticatory process; good masticatory capacity contributes to increased cerebral blood flow with increased oxygenation, and therefore has a protective role.
- Dental loss also leads to decreased quality of feeding with decreased intake of vitamins and nutrients, which are important for the health of the CNS [47].
- AD and periodontitis (one of the main causes of dental loss) share common genetic factors, for example, polymorphism of interleukin 1A-B [48].
- Dental elements are also involved in proprioception, and an association between their loss and a decreased number of pyramidal cells in the hippocampus has been shown in a mouse model [49].
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Du, X.; Wang, X.; Geng, M. Alzheimer’s disease hypothesis and related therapies. Transl. Neurodegener. 2018, 7, 2. [Google Scholar] [CrossRef]
- Marchini, L.; Ettinger, R.; Caprio, T.; Jucan, A. Oral health care for patients with Alzheimer’s disease: An update. Spec. Care Dent. 2019. [Google Scholar] [CrossRef] [PubMed]
- Delwel, S.; Binnekade, T.T.; Perez, R.S.; Hertogh, C.M.; Scherder, E.J.; Lobbezoo, F. Oral health and orofacial pain in older people with dementia: A systematic review with focus on dental hard tissues. Clin. Oral Investig. 2017, 21, 17–32. [Google Scholar] [CrossRef] [PubMed]
- Natto, Z.S.; Abu Ahmad, R.H.; Alsharif, L.T.; Alrowithi, H.F.; Alsini, D.A.; Salih, H.A.; Bissada, N.F. Chronic Periodontitis Case Definitions and Confounders in Periodontal Research: A Systematic Assessment. Biomed. Res. Int. 2018, 2018, 4578782. [Google Scholar] [CrossRef]
- Eke, P.I.; Dye, B.A.; Wei, L.; Slade, G.D.; Thornton-Evans, G.O.; Borgnakke, W.S.; Taylor, G.W.; Page, R.C.; Beck, J.D.; Genco, R.J. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 to 2012. J. Periodontol. 2015, 86, 611–622. [Google Scholar] [CrossRef]
- Lertpimonchai, A.; Rattanasiri, S.; Arj-Ong Vallibhakara, S.; Attia, J.; Thakkinstian, A. The association between oral hygiene and periodontitis: A systematic review and meta-analysis. Int. Dent. J. 2017, 67, 332–343. [Google Scholar] [CrossRef] [PubMed]
- Bergstrom, J. Tobacco smoking and chronic destructive periodontal disease. Odontology 2004, 92, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Wang, J.; Lv, J.; Wang, W.; Jiang, X. Alcohol consumption and risk of periodontitis: A meta-analysis. J. Clin. Periodontol. 2016, 43, 572–583. [Google Scholar] [CrossRef] [PubMed]
- Rogers, J. The inflammatory response in Alzheimer’s disease. J. Periodontol. 2008, 79, 1535–1543. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.X.; Fuller, S.J.; Beyreuther, K.; Masters, C.L. The amyloid precursor protein of Alzheimer disease in human brain and blood. J. Leukoc. Biol. 1999, 66, 567–574. [Google Scholar] [CrossRef]
- Troiano, G.; Laino, L.; Dioguardi, M.; Giannatempo, G.; Lo Muzio, L.; Lo Russo, L. Mandibular Class II Furcation Defect Treatment: Effects of the Addition of Platelet Concentrates to Open Flap: A Systematic Review and Meta-Analysis of Randomized Clinical Trials. J. Periodontol. 2016, 87, 1030–1038. [Google Scholar] [CrossRef]
- Leira, Y.; Dominguez, C.; Seoane, J.; Seoane-Romero, J.; Pias-Peleteiro, J.M.; Takkouche, B.; Blanco, J.; Aldrey, J.M. Is Periodontal Disease Associated with Alzheimer’s Disease? A Systematic Review with Meta-Analysis. Neuroepidemiology 2017, 48, 21–31. [Google Scholar] [CrossRef]
- Yoshida, T.; Blair, A.; D’Alessandro, A.; Nemkov, T.; Dioguardi, M.; Silliman, C.C.; Dunham, A. Enhancing uniformity and overall quality of red cell concentrate with anaerobic storage. Blood Transfus. 2017, 15, 172–181. [Google Scholar] [CrossRef]
- Lo Muzio, L.; Pannone, G.; Santarelli, A.; Bambini, F.; Mascitti, M.; Rubini, C.; Testa, N.F.; Dioguardi, M.; Leuci, S.; Bascones, A.; et al. Is expression of p120ctn in oral squamous cell carcinomas a prognostic factor? Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2013, 115, 789–798. [Google Scholar] [CrossRef]
- Dioguardi, M.; Troiano, G.; Laino, L.; Lo Russo, L.; Giannatempo, G.; Lauritano, F.; Cicciu, M.; Lo Muzio, L. ProTaper and WaveOne systems three-dimensional comparison of device parameters after the shaping technique. A micro-CT study on simulated root canals. Int. J. Clin. Exp. Med. 2015, 8, 17830–17834. [Google Scholar]
- Li, J.; Xu, H.; Pan, W.; Wu, B. Association between tooth loss and cognitive decline: A 13-year longitudinal study of Chinese older adults. PLoS ONE 2017, 12, e0171404. [Google Scholar] [CrossRef] [PubMed]
- Makiura, T.; Ikeda, Y.; Hirai, T.; Terasawa, H.; Hamaue, N.; Minami, M. Influence of diet and occlusal support on learning memory in rats behavioral and biochemical studies. Res. Commun. Mol. Pathol. Pharmacol. 2000, 107, 269–277. [Google Scholar]
- Faggion, C.M., Jr. Critical appraisal of evidence supporting the placement of dental implants in patients with neurodegenerative diseases. Gerodontology 2016, 33, 2–10. [Google Scholar] [CrossRef]
- Wu, Z.; Nakanishi, H. Connection between periodontitis and Alzheimer’s disease: Possible roles of microglia and leptomeningeal cells. J. Pharmacol. Sci. 2014, 126, 8–13. [Google Scholar] [CrossRef]
- Teixeira, F.B.; Saito, M.T.; Matheus, F.C.; Prediger, R.D.; Yamada, E.S.; Maia, C.S.F.; Lima, R.R. Periodontitis and Alzheimer’s Disease: A Possible Comorbidity between Oral Chronic Inflammatory Condition and Neuroinflammation. Front. Aging Neurosci. 2017, 9, 327. [Google Scholar] [CrossRef] [PubMed]
- Fereshtehnejad, S.M.; Garcia-Ptacek, S.; Religa, D.; Holmer, J.; Buhlin, K.; Eriksdotter, M.; Sandborgh-Englund, G. Dental care utilization in patients with different types of dementia: A longitudinal nationwide study of 58,037 individuals. Alzheimers Dement. 2018, 14, 10–19. [Google Scholar] [CrossRef]
- Tiisanoja, A.; Syrjala, A.M.; Tertsonen, M.; Komulainen, K.; Pesonen, P.; Knuuttila, M.; Hartikainen, S.; Ylostalo, P. Oral diseases and inflammatory burden and Alzheimer’s disease among subjects aged 75 years or older. Spec. Care Dent. 2019, 39, 158–165. [Google Scholar] [CrossRef] [PubMed]
- Delwel, S.; Binnekade, T.T.; Perez, R.; Hertogh, C.; Scherder, E.J.A.; Lobbezoo, F. Oral hygiene and oral health in older people with dementia: A comprehensive review with focus on oral soft tissues. Clin. Oral Investig. 2018, 22, 93–108. [Google Scholar] [CrossRef]
- Takeuchi, K.; Ohara, T.; Furuta, M.; Takeshita, T.; Shibata, Y.; Hata, J.; Yoshida, D.; Yamashita, Y.; Ninomiya, T. Tooth Loss and Risk of Dementia in the Community: The Hisayama Study. J. Am. Geriatr. Soc. 2017, 65, e95–e100. [Google Scholar] [CrossRef]
- D’Alessandro, G.; Costi, T.; Alkhamis, N.; Bagattoni, S.; Sadotti, A.; Piana, G. Oral Health Status in Alzheimer’s Disease Patients: A Descriptive Study in an Italian Population. J. Contemp. Dent. Pract. 2018, 19, 483–489. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gotzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. PLoS Med. 2009, 6, e1000100. [Google Scholar] [CrossRef]
- Chu, C.H.; Ng, A.; Chau, A.M.; Lo, E.C. Oral health status of elderly chinese with dementia in Hong Kong. Oral Health Prev. Dent. 2015, 13, 51–57. [Google Scholar] [CrossRef] [PubMed]
- Warren, J.J.; Chalmers, J.M.; Levy, S.M.; Blanco, V.L.; Ettinger, R.L. Oral health of persons with and without dementia attending a geriatric clinic. Spec. Care Dent. 1997, 17, 47–53. [Google Scholar] [CrossRef]
- Gil-Montoya, J.A.; Sanchez-Lara, I.; Carnero-Pardo, C.; Fornieles, F.; Montes, J.; Vilchez, R.; Burgos, J.S.; Gonzalez-Moles, M.A.; Barrios, R.; Bravo, M. Is periodontitis a risk factor for cognitive impairment and dementia? A case-control study. J. Periodontol. 2015, 86, 244–253. [Google Scholar] [CrossRef]
- Zenthofer, A.; Cabrera, T.; Rammelsberg, P.; Hassel, A.J. Improving oral health of institutionalized older people with diagnosed dementia. Aging Ment. Health 2016, 20, 303–308. [Google Scholar] [CrossRef]
- Aragon, F.; Zea-Sevilla, M.A.; Montero, J.; Sancho, P.; Corral, R.; Tejedor, C.; Frades-Payo, B.; Paredes-Gallardo, V.; Albaladejo, A. Oral health in Alzheimer’s disease: A multicenter case-control study. Clin. Oral Investig. 2018. [Google Scholar] [CrossRef] [PubMed]
- Nordenram, G.; Ryd-Kjellen, E.; Johansson, G.; Nordstrom, G.; Winblad, B. Alzheimer’s disease, oral function and nutritional status. Gerodontology 1996, 13, 9–16. [Google Scholar] [CrossRef] [PubMed]
- Gil-Montoya, J.A.; Sanchez-Lara, I.; Carnero-Pardo, C.; Fornieles-Rubio, F.; Montes, J.; Barrios, R.; Gonzalez-Moles, M.A.; Bravo, M. Oral Hygiene in the Elderly with Different Degrees of Cognitive Impairment and Dementia. J. Am. Geriatr. Soc. 2017, 65, 642–647. [Google Scholar] [CrossRef] [PubMed]
- Rai, B.; Kaur, J.; Anand, S.C. Possible relationship between periodontitis and dementia in a North Indian old age population: A pilot study. Gerodontology 2012, 29, e200–e205. [Google Scholar] [CrossRef] [PubMed]
- De Souza Rolim, T.; Fabri, G.M.; Nitrini, R.; Anghinah, R.; Teixeira, M.J.; de Siqueira, J.T.; Cestari, J.A.; de Siqueira, S.R. Oral infections and orofacial pain in Alzheimer’s disease: A case-control study. J. Alzheimers Dis. 2014, 38, 823–829. [Google Scholar] [CrossRef]
- Ide, M.; Harris, M.; Stevens, A.; Sussams, R.; Hopkins, V.; Culliford, D.; Fuller, J.; Ibbett, P.; Raybould, R.; Thomas, R.; et al. Periodontitis and Cognitive Decline in Alzheimer’s Disease. PLoS ONE 2016, 11, e0151081. [Google Scholar] [CrossRef]
- Chen, C.K.; Wu, Y.T.; Chang, Y.C. Association between chronic periodontitis and the risk of Alzheimer’s disease: A retrospective, population-based, matched-cohort study. Alzheimers Res. Ther. 2017, 9, 56. [Google Scholar] [CrossRef]
- Ganesh, P.; Karthikeyan, R.; Muthukumaraswamy, A.; Anand, J. A Potential Role of Periodontal Inflammation in Alzheimer’s Disease: A Review. Oral Health Prev. Dent. 2017, 15, 7–12. [Google Scholar] [CrossRef]
- Zhurakivska, K.; Troiano, G.; Caponio, V.C.A.; Dioguardi, M.; Arena, C.; Lo Muzio, L. The Effects of Adjuvant Fermented Wheat Germ Extract on Cancer Cell Lines: A Systematic Review. Nutrients 2018, 10, 1546. [Google Scholar] [CrossRef] [PubMed]
- Okamoto, N.; Morikawa, M.; Tomioka, K.; Yanagi, M.; Amano, N.; Kurumatani, N. Association between tooth loss and the development of mild memory impairment in the elderly: The Fujiwara-kyo Study. J. Alzheimers Dis. 2015, 44, 777–786. [Google Scholar] [CrossRef]
- Checchi, L.; Gatto, M.R.; Pattison, A.; Felice, P. Genetic and microbiologic tests in periodontal disease. Minerva Stomatol. 2004, 53, 345–353. [Google Scholar] [PubMed]
- Lo Muzio, L.; Pannone, G.; Santarelli, A.; Lo Russo, L.; De Lillo, A.; Rubini, C.; Bambini, F.; Bufo, P.; Dioguardi, M.; Procaccini, M. Expression of poly(ADP-ribose) polymerase in bone regeneration. J. Biol. Regul. Homeost. Agents 2014, 28, 801–807. [Google Scholar] [PubMed]
- Fujimura, J.H.; Duster, T.; Rajagopalan, R. Race, genetics, and disease: Questions of evidence, matters of consequence. Soc. Stud. Sci. 2008, 38, 643–656. [Google Scholar] [CrossRef] [PubMed]
- Nakatsuka, N.; Moorjani, P.; Rai, N.; Sarkar, B.; Tandon, A.; Patterson, N.; Bhavani, G.S.; Girisha, K.M.; Mustak, M.S.; Srinivasan, S.; et al. The promise of discovering population-specific disease-associated genes in South Asia. Nat. Genet. 2017, 49, 1403–1407. [Google Scholar] [CrossRef] [PubMed]
- Naorungroj, S.; Slade, G.D.; Divaris, K.; Heiss, G.; Offenbacher, S.; Beck, J.D. Racial differences in periodontal disease and 10-year self-reported tooth loss among late middle-aged and older adults: The dental ARIC study. J. Public Health Dent. 2017, 77, 372–382. [Google Scholar] [CrossRef] [PubMed]
- Deguchi, M.; Mau, M.; Davis, J.; Niederman, R. Preventable Tooth Loss in Hawai’i: The Role of Socioeconomic Status, Diabetes, and Dental Visits. Prev. Chronic Dis. 2017, 14, E115. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Perrone, D.; Ardito, F.; Giannatempo, G.; Dioguardi, M.; Troiano, G.; Lo Russo, L.; DE Lillo, A.; Laino, L.; Lo Muzio, L. Biological and therapeutic activities, and anticancer properties of curcumin. Exp. Ther. Med. 2015, 10, 1615–1623. [Google Scholar] [CrossRef]
- Gayathri, R.; Saadi, A.V.; Bhat, K.M.; Bhat, S.G.; Satyamoorthy, K. Allele, genotype, and composite genotype effects of IL-1A +4845 and IL-1B +3954 polymorphisms for chronic periodontitis in an Indian population. Indian J. Dent. Res. 2011, 22, 612. [Google Scholar] [CrossRef]
- Oue, H.; Miyamoto, Y.; Koretake, K.; Okada, S.; Doi, K.; Jung, C.G.; Michikawa, M.; Akagawa, Y. Tooth loss might not alter molecular pathogenesis in an aged transgenic Alzheimer’s disease model mouse. Gerodontology 2016, 33, 308–314. [Google Scholar] [CrossRef]
- Chapman, P.J.; Shaw, R.M. Normative dental treatment needs of Alzheimer patients. Aust. Dent. J. 1991, 36, 141–144. [Google Scholar] [CrossRef] [PubMed]
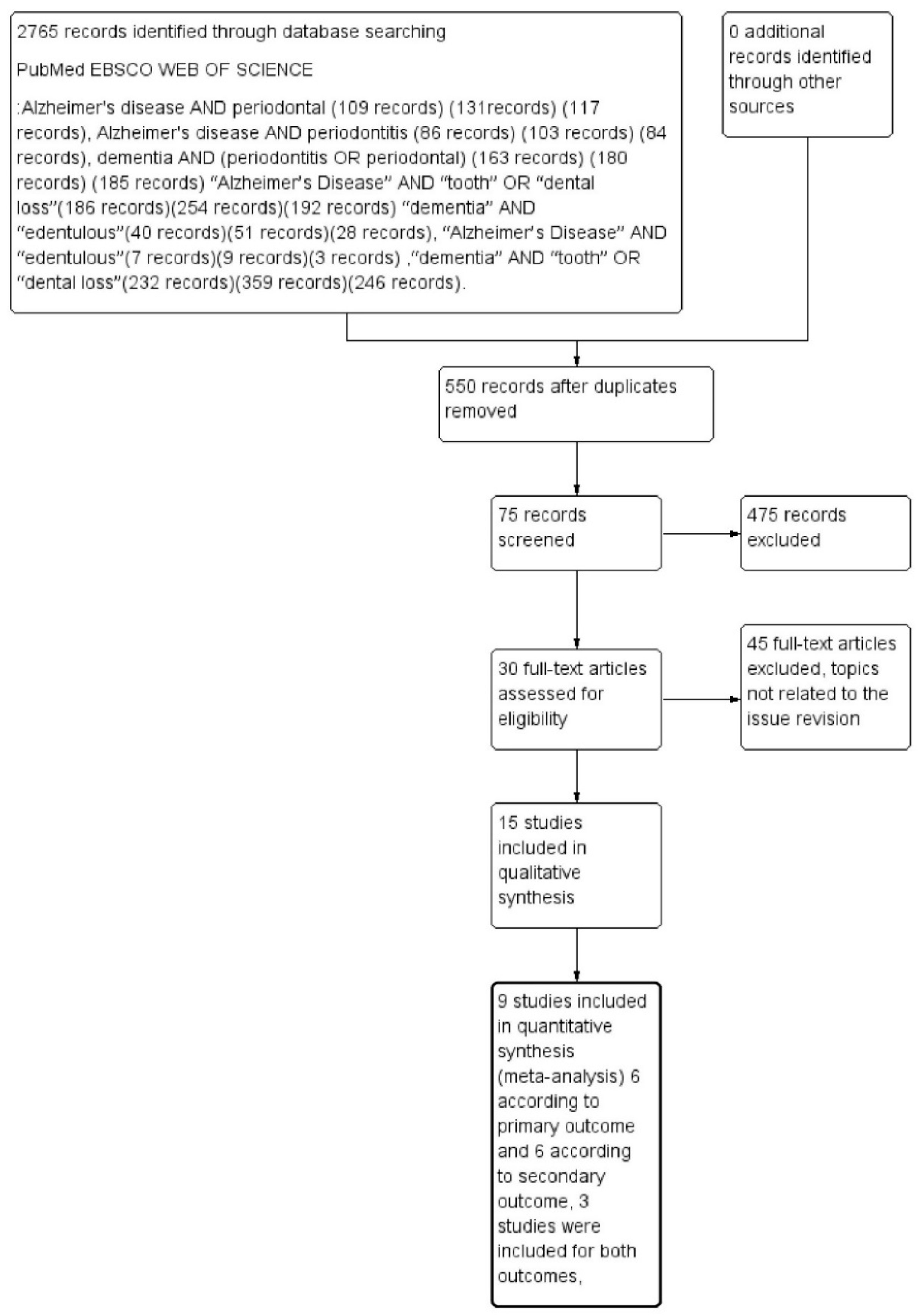

| Keywords | PubMed | EBSCO | Web of Science | Total |
|---|---|---|---|---|
| Alzheimer’s disease AND periodontal | 109 records | 131 records | 117 records | 357 records |
| Alzheimer’s disease AND periodontitis | 86 records | 103 records | 84 records | 273 records |
| dementia AND (periodontitis OR periodontal) | 163 records | 180 records | 185 records | 528 records |
| “Alzheimer’s Disease” AND “tooth” OR “dental loss” | 186 records | 254 records | 192 records | 632 records |
| “dementia” AND “edentulous” | 40 records | 51 records | 28 records | 119 records |
| “Alzheimer’s Disease” AND “edentulous” | 7 records | 9 records | 3 records | 19 records |
| “dementia” AND “tooth” OR “dental loss” | 232 records | 359 records | 246 records | 837 records |
| Total | 823 records | 1087 records | 855 records | 2765 records |
| Case Control, Author, Date | Dementia Group (AD) | Control Group | Missing Teeth AD | Missing Teeth Control |
|---|---|---|---|---|
| Chun et al. 2015 | 59 | 59 | 1115 | 1080 |
| Warren et al. 1997 | 45 | 133 | 990 | 2527 |
| Gil-Montoya et al. 2014 | 180 | 229 | 3006 | 3343 |
| Zenthòfer et al. 2015 | 33 | 60 | 676 | 1230 |
| Aragòn et al. 2018 | 70 | 36 | 1470 | 299 |
| Nordenram et al. 1996 | 34 | 35 | 639 | 638 |
| Case Control, Author Date | Dementia Group (AD) | Control Group | Edentulous AD | Edentulous Control |
|---|---|---|---|---|
| Chun et al. 2015 | 59 | 59 | 10 | 8 |
| Warren et al. 1997 | 45 | 133 | 18 | 42 |
| De Souza Rolim et al. 2013 | 29 | 30 | 10 | 13 |
| Nordenram et al. 1996 | 34 | 35 | 7 | 6 |
| Gil-Montoya et al. 2016 | 240 | 324 | 95 | 60 |
| Rai et al. 2010 | 20 | 32 | 4 | 11 |
| Selection | Comparability | Exposure | Score | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Case Control Study | Definition of Cases | Representativeness of Cases | Selection of Controls | Definition of Controls | Age | Gender | Assessment of Oral Health | Same Method Cases and Controls | Nonresponse Rate | Total |
| Chun et al. 2015 | − | + | − | + | + | + | + | − | − | 5 |
| Warren et al. 1997 | + | + | − | − | + | + | + | + | + | 7 |
| Gil-Montoya et al. 2014 | + | − | + | − | + | + | + | + | + | 7 |
| Zenthòfer et al. 2015 | − | − | + | − | + | − | + | + | − | 4 |
| Aragòn et al. 2018 | + | + | − | + | − | + | + | + | − | 6 |
| Nordenram et al. 1996 | + | + | + | + | + | + | + | + | − | 8 |
| Rai et al. 2010 | + | − | − | − | + | + | + | + | − | 5 |
| Gil-Montoya et al. 2016 | + | − | + | − | + | + | + | + | − | 6 |
| De Souza Rolim et al. 2013 | + | + | + | + | + | + | + | + | − | 8 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Dioguardi, M.; Di Gioia, G.; Caloro, G.A.; Capocasale, G.; Zhurakivska, K.; Troiano, G.; Lo Russo, L.; Lo Muzio, L. The Association between Tooth Loss and Alzheimer’s Disease: a Systematic Review with Meta-Analysis of Case Control Studies. Dent. J. 2019, 7, 49. https://doi.org/10.3390/dj7020049
Dioguardi M, Di Gioia G, Caloro GA, Capocasale G, Zhurakivska K, Troiano G, Lo Russo L, Lo Muzio L. The Association between Tooth Loss and Alzheimer’s Disease: a Systematic Review with Meta-Analysis of Case Control Studies. Dentistry Journal. 2019; 7(2):49. https://doi.org/10.3390/dj7020049
Chicago/Turabian StyleDioguardi, Mario, Giovanni Di Gioia, Giorgia Apollonia Caloro, Giorgia Capocasale, Khrystyna Zhurakivska, Giuseppe Troiano, Lucio Lo Russo, and Lorenzo Lo Muzio. 2019. "The Association between Tooth Loss and Alzheimer’s Disease: a Systematic Review with Meta-Analysis of Case Control Studies" Dentistry Journal 7, no. 2: 49. https://doi.org/10.3390/dj7020049
APA StyleDioguardi, M., Di Gioia, G., Caloro, G. A., Capocasale, G., Zhurakivska, K., Troiano, G., Lo Russo, L., & Lo Muzio, L. (2019). The Association between Tooth Loss and Alzheimer’s Disease: a Systematic Review with Meta-Analysis of Case Control Studies. Dentistry Journal, 7(2), 49. https://doi.org/10.3390/dj7020049










