Comparison of Two-Dimensional and Three-Dimensional Radiographs Using Clinically Relevant Parameters
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Characteristics
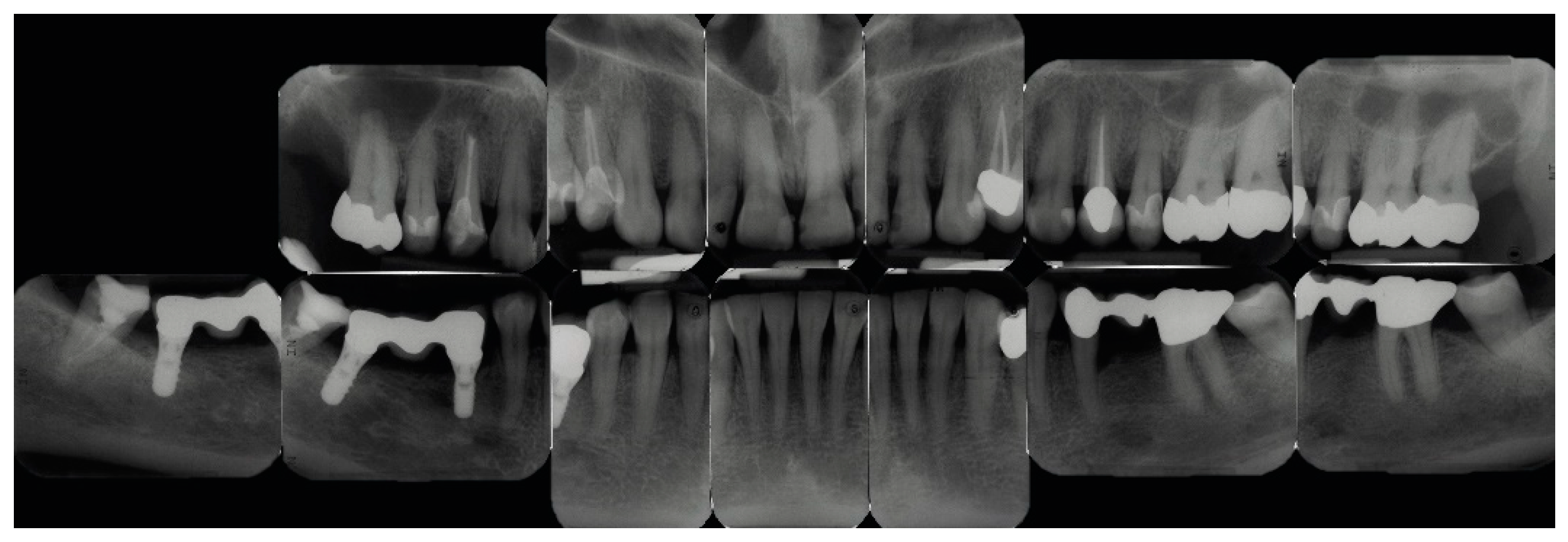
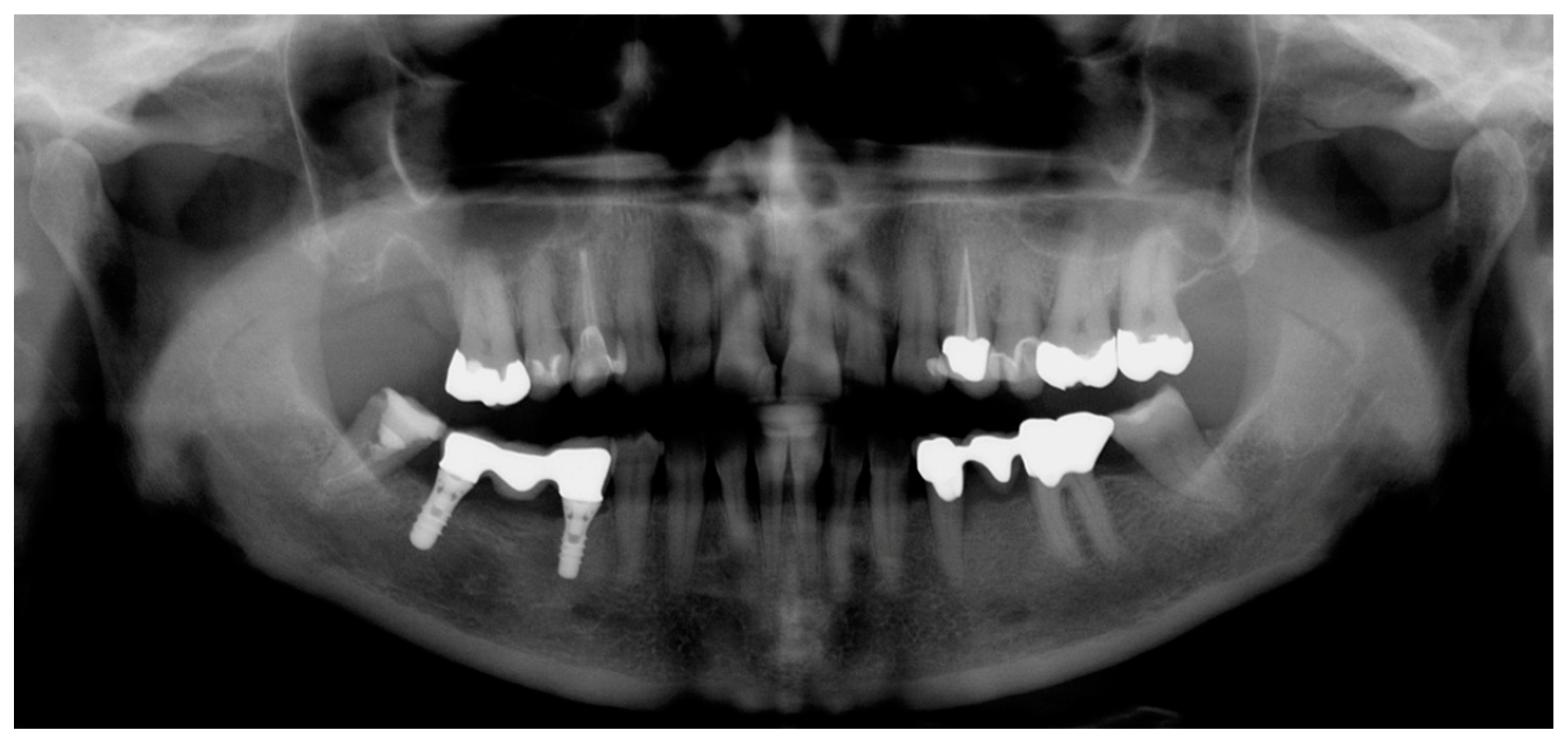
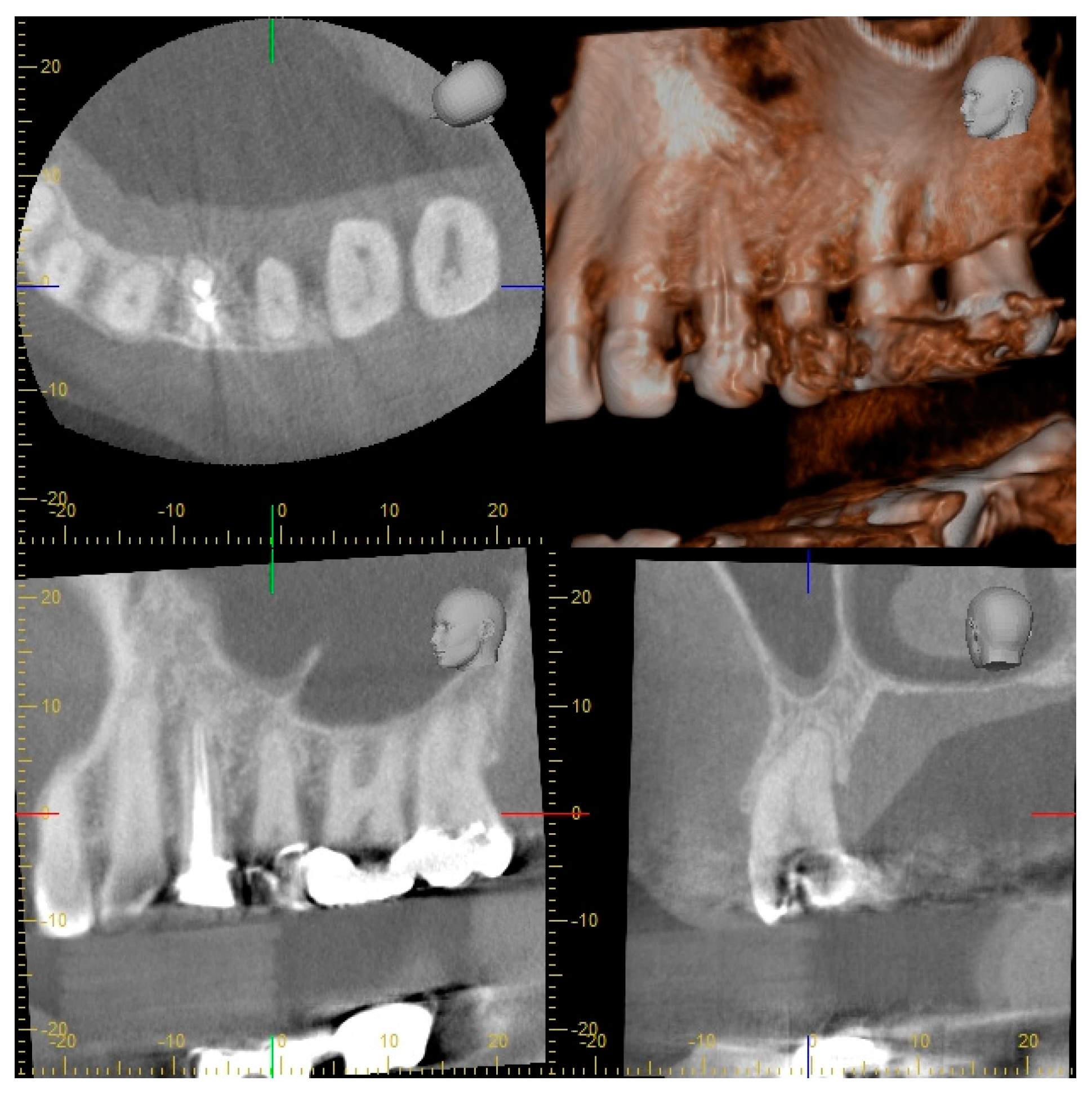
2.2. Radiographic Methods
2.3. Analysis of Radiographic Images
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Walter, C.; Buset, S.L.; Thillainathan, L.; Weiger, R.; Zitzmann, N.U. Evaluation of periodontal therapy in undergraduate courses of the University of Basle. Swiss Dent. J. 2013, 123, 861–869. [Google Scholar]
- Persson, R.E.; Tzannetou, S.; Feloutzis, A.G.; Brägger, U.; Persson, G.R.; Lang, N.P. Comparison between panoramic and intra-oral radiographs for the assessment of alveolar bone levels in a periodontal maintenance population. J. Clin. Periodontol. 2003, 30, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Dula, K.; Bornstein, M.M.; Buser, D.; Dagassan-Berndt, D.; Ettlin, D.A.; Filippi, A.; Gabioud, F.; Katsaros, C.; Krastl, G.; Lambrecht, J.T.; et al. SADMFR Guidelines for the use of cone beam computed tomography/digital volume tomography. Swiss Dent. J. 2014, 124, 1170–1183. [Google Scholar]
- Dula, K.; Benic, G.I.; Bornstein, M.; Dagassan-Berndt, D.; Filippi, A.; Hicklin, S.; Kissling-Jeger, F.; Luebbers, H.T.; Sculean, A.; Sequeira-Byron, P.; et al. SADMFR guidelines for the use of cone-beam computed tomography/digital volume tomography—Endodontics, periodontology, reconstructive dentistry, pediatric dentistry. Swiss Dent. J. 2015, 125, 945–953. [Google Scholar] [PubMed]
- Bornstein, M.M.; Lauber, R.; Sendi, P.; von Arx, T. Comparison of periapical radiography and limited cone-beam computed tomography in mandibular molars for analysis of anatomical landmarks before apical surgery. J. Endod. 2011, 37, 151–157. [Google Scholar] [CrossRef]
- Walter, C.; Schmidt, J.C.; Dula, K.; Sculean, A. Cone beam computed tomography (CBCT) for diagnosis and treatment planning in periodontology: A systematic review. Quintessence Int. 2016, 47, 25–37. [Google Scholar]
- Armitage, G.C. Development of a classification system for periodontal diseases and conditions. Ann. Periodontol. 1999, 4, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.; Saxer, U.P.; Bornstein, M.M.; Klingler, K.; Ramseier, C.A. Impact of tobacco use on the periodontium—An update (I)—Part 1: Epidemiologic and pathogenetic aspects of tobacco-related periodontal disease. Swiss Dent. J. 2007, 117, 45–60. [Google Scholar]
- Tonetti, M.S.; Greenwell, H.; Kornman, K.S. Staging and grading of periodontitis: Framework and proposal of a new classification and case definition. J. Clin. Periodontol. 2018, 45, S149–S161. [Google Scholar] [CrossRef]
- Rodriguez, F.R.; Taner, B.; Weiger, R.; Walter, C. Is smoking a predictor of apical periodontitis? Clin. Oral Investig. 2013, 17, 1947–1955. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.; Kaner, D.; Berndt, D.C.; Weiger, R.; Zitzmann, N.U. Three-dimensional imaging as a pre-operative tool in decision making for furcation surgery. J. Clin. Periodontol. 2009, 36, 250–257. [Google Scholar] [CrossRef]
- Lindhe, J.; Karring, T.; Araujo, M. The anatomy of periodontal tissues. In Clinical Periodontology and Implant Dentistry, 4th ed.; Lindhe, J., Karring, T., Lang, N.P., Eds.; Blackwell Munksgaard: Copenhagen, Denmark, 2003; pp. 3–48. [Google Scholar]
- Goldman, H.M.; Cohen, D.W. The intrabony pocket: Classification and treatment. J. Periodontol. 1957, 29, 272–279. [Google Scholar] [CrossRef]
- Papapanou, P.N.; Tonetti, M.S. Diagnosis and epidemiology of periodontal osseous lesions. Periodontol. 2000 2000, 22, 8–21. [Google Scholar] [CrossRef] [PubMed]
- Hamp, S.E.; Nyman, S.; Lindhe, J. Periodontal treatment of multirooted teeth. Results after 5 years. J. Clin. Periodontol. 1975, 2, 126–135. [Google Scholar] [CrossRef] [PubMed]
- Vermylen, K.; De Quincey, G.N.; Van’t Hof, M.A.; Wolffe, G.N.; Renggli, H.H. Classification, reproducibility and prevalence of root proximity in periodontal patients. J. Clin. Periodontol. 2005, 32, 254–259. [Google Scholar] [CrossRef]
- Vertucci, F.J. Root canal anatomy of the human permanent teeth. Oral Surg. Oral Med. Oral Pathol. 1984, 58, 589–599. [Google Scholar] [CrossRef]
- Jou, Y.; Karabucak, B.; Levin, J.; Liu, D. Endodontic working width: Current concepts and techniques. Dent. Clin. N. Am. 2004, 48, 323–335. [Google Scholar] [CrossRef]
- Ørstavik, D.; Kerekes, K.; Eriksen, H.M. The periapical index: A scoring system for radiographic assessment of apical periodontitis. Dent. Traumatol. 1986, 2, 20–34. [Google Scholar] [CrossRef]
- Weiger, R.; Hitzler, S.; Hermle, G.; Löst, C. Periapical status, quality of root canal fillings and estimated endodontic treatment needs in an urban German population. Endod. Dent. Traumatol. 1997, 13, 69–74. [Google Scholar] [CrossRef]
- Pitts, N.B. Systems for grading approximal carious lesions diagnosed from bitewing radiographs. Proposals for future standardization. Community Dent. Oral Epidemiol. 1984, 12, 114–122. [Google Scholar] [CrossRef]
- Tronstad, L.; Asbjornsen, K.; Doving, L.; Pedersen, I.; Eriksen, H.M. Influence of coronal restorations on the periapical health of endodontically treated teeth. Endod. Dent. Traumatol. 2000, 16, 218–221. [Google Scholar] [CrossRef] [PubMed]
- Zadik, Y.; Yitschaky, O.; Pikovsky, A.; Zini, A.; Fridlander Barenboim, S. Detection of mandibular condyle pseudocysts in panoramic radiographs: Digital and film-based radiology. Quintessence Int. 2015, 46, 725–730. [Google Scholar]
- ICRP: Recommendation of the International Comission on Radiological Protection ICRP Publication 26; Pergamon Press: Oxford, UK, 1977.
- Sedentexct. Guidelines on CBCT for Dental and Maxillofacial Radiology. Available online: http://www.sedentexct.eu/content/guidelines-cbct-dental-and-maxillofacial-radiology.htm (accessed on 12 April 2019).
- Haiter-Neto, F.; Wenzel, A.; Gotfredsen, E. Diagnostic accuracy of cone beam computed tomography scans compared with intraoral image modalities for detection of caries lesions. Dentomaxillofac. Radiol. 2008, 37, 18–22. [Google Scholar] [CrossRef]
- Kamburoglu, K.; Murat, S.; Yuksel, S.P.; Cebeci, A.R.; Paksoy, C.S. Occlusal caries detection by using a cone-beam CT with different voxel resolutions and a digital intraoral sensor. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2010, 109, e63–e69. [Google Scholar] [CrossRef]
- Cheng, J.G.; Zhang, Z.L.; Wang, X.Y.; Zhang, Z.Y.; Ma, X.C. Detection accuracy of proximal caries by phosphorplate and cone-beam computerized tomography images scanned with different resolutions. Clin. Oral Investig. 2012, 16, 1015–1021. [Google Scholar] [CrossRef] [PubMed]
- Krzyzostaniak, J.; Kulczyk, T.; Czarnecka, B.; Surdacka, A. A comparative study of the diagnostic accuracy of cone beam computed tomography and intraoral radiographic modalities for the detection of nonconcavitated caries. Clin. Oral Investig. 2015, 19, 667–672. [Google Scholar] [CrossRef] [PubMed]
- Tsuchida, R.; Araki, K.; Okano, T. Evaluation of a limited cone-beam volumetric imaging system: Comparison with film radiography in detecting incipient proximal caries. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 104, 412–416. [Google Scholar] [CrossRef]
- Kayipmaz, S.; Sezgin, O.S.; Saricaoglu, S.T.; Can, G. An in vitro comparison of diagnostic abilities of conventional radiography, storage phosphor, and cone beam computed tomography to determine occlusal and approximal caries. Eur. J. Radiol. 2011, 80, 478–482. [Google Scholar] [CrossRef]
- Rathore, S.; Tyndall, D.; Wright, J.; Everett, E. Ex vivo comparison of Galileos cone beam CT and intraoral radiographs in detecting occlusal caries. Dentomaxillofac. Radiol. 2012, 41, 489–493. [Google Scholar] [CrossRef]
- Valizadeh, S.; Tavakkoli, M.A.; Karimi Vasigh, H.; Azizi, Z.; Zarrabian, T. Evaluation of cone beam computed tomography (CBCT) system: Comparison with intraoral periapical radiography in proximal caries detection. J. Dent. Res. Dent. Clin. Dent. Prosp. 2012, 6, 1–5. [Google Scholar]
- Gaalaas, L.; Tyndall, D.; Mol, A.; Everett, E.; Bangdiwala, A. Ex vivo evaluation of new 2D and 3D dental radiographic technology for detecting caries. Dentomaxillofac. Radiol. 2016, 45, 20150281. [Google Scholar] [CrossRef]
- Akkaya, N.; Kansu, O.; Kansu, H.; Cagirankaya, L.B.; Arslan, U. Comparing the accuracy of panoramic and intraoral radiography in the diagnosis of proximal caries. Dentomaxillofac. Radiol. 2006, 35, 170–174. [Google Scholar] [CrossRef]
- Akarslan, Z.Z.; Akdevelioglu, M.; Gungor, K.; Erten, H. A comparison of the diagnostic accuracy of bitewing, periapical, unfiltered and filtered digital panoramic images for approximal caries detection in posterior teeth. Dentomaxillofac. Radiol. 2008, 37, 458–463. [Google Scholar] [CrossRef]
- Kamburoglu, K.; Kolsuz, E.; Murat, S.; Yuksel, S.; Ozen, T. Proximal caries detection accuracy using intraoral bitewing radiography, extraoral bitewing radiography and panoramic radiography. Dentomaxillofac. Radiol. 2012, 41, 450–459. [Google Scholar] [CrossRef] [PubMed]
- Matherne, R.P.; Angelopoulos, C.; Kulild, J.C.; Tira, D. Use of cone-beam computed tomography to identify root canal systems in vitro. J. Endod. 2008, 34, 87–89. [Google Scholar] [CrossRef] [PubMed]
- Blattner, T.C.; George, N.; Lee, C.C.; Kumar, V.; Yelton, C.D. Efficacy of cone-beam computed tomography as a modality to accurately identify the presence of second mesiobuccal canals in maxillary first and second molars: A pilot study. J. Endod. 2010, 36, 867–870. [Google Scholar] [CrossRef] [PubMed]
- Michetti, J.; Maret, D.; Mallet, J.P.; Diemer, F. Validation of cone beam computed tomography as a tool to explore root canal anatomy. J. Endod. 2010, 36, 1187–1190. [Google Scholar] [CrossRef]
- Zhang, R.; Wang, H.; Tian, Y.Y.; Yu, X.; Hu, T.; Dummer, P.M.H. Use of cone-beam computed tomography to evaluate root and canal morphology of mandibular molars in Chinese individuals. Int. Endod. J. 2011, 44, 990–999. [Google Scholar] [CrossRef]
- Brady, E.; Mannocci, F.; Brown, J.; Wilson, R.; Patel, S. A comparison of cone beam computed tomography and periapical radiography for the detection of vertical root fractures in nonendodontically treated teeth. Int. Endod. J. 2013, 46. [Google Scholar] [CrossRef]
- Lofthag-Hansen, S.; Huumonen, S.; Gröndahl, K.; Gröndahl, H.G. Limited conebeam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. Endod. 2007, 103, 114–119. [Google Scholar] [CrossRef] [PubMed]
- Low, K.M.; Dula, K.; Bürgin, W.; von Arx, T. Comparison of periapical radiography and limited cone-beam tomography in posterior maxillary teeth referred for apical surgery. J. Endod. 2008, 34, 557–562. [Google Scholar] [CrossRef]
- Venskutonis, T.; Daugela, P.; Strazdas, M.; Juodzbalys, G. Accuracy of digital radiography and cone beam computed tomography on periapical radiolucency detection in endodontically treated teeth. J. Oral Maxillofac. Res. 2014, 5. [Google Scholar] [CrossRef] [PubMed]
- Kruse, C.; Spin-Neto, R.; Wenzel, A.; Kirkevang, L.L. Cone beam computed tomography and periapical lesions: A systematic review analysing studies on diagnostic efficacy by a hierarchical model. Int. Endod. J. 2015, 48, 815–828. [Google Scholar] [CrossRef] [PubMed]
- Weissman, J.; Johnson, J.D.; Anderson, M.; Hollender, L.; Huson, T.; Paranjpe, A.; Patel, S.; Cohenca, N. Association between the presence of apical periodontitis and clinical symptoms in endodontic patients using cone-beam computed tomography and periapicel radiographs. J. Endod. 2015, 41, 1824–1829. [Google Scholar] [CrossRef]
- Davies, A.; Patel, S.; Foschi, F.; Andiappan, M.; Mitchell, P.J.; Mannocci, F. The detection of periapical pathoses using digital periapical radiography and cone beam computed tomography in endodontically retreated teeth—part 2: A 1 year post-treatment follow-up. Int. Endod. J. 2016, 49, 623–635. [Google Scholar] [CrossRef] [PubMed]
- Aminoshariae, A.; Kulild, J.C.; Syed, A. Cone-beam computed tomography compared with intraoral radiographic lesions in endodontic outcome studies: A systematic review. J. Endod. 2018, 44, 1626–1631. [Google Scholar] [CrossRef]
- Bornstein, M.M.; Bingisser, A.C.; Reichart, P.A.; Sendi, P.; Bosshardt, D.D.; von Arx, T. Comparison between radiographic (2-dimensional and 3-dimensional) and histologic findings of periapical lesions treated with apical surgery. J. Endod. 2015, 41, 804–811. [Google Scholar] [CrossRef] [PubMed]
- De Faria Vasconcelos, K.; Evangelista, K.M.; Rodrigues, C.D.; Estrela, C.; de Sousa, T.O.; Silva, M.A. Detection of periodontal bone loss using cone beam CT and intraoral radiography. Dentomaxillofac. Radiol. 2012, 41, 64–69. [Google Scholar] [CrossRef]
- Grimard, B.A.; Hoidal, M.J.; Mills, M.P.; Mellonig, J.T.; Nummikoski, P.V.; Mealey, B.L. Comparison of clinical, periapical radiograph, and conebeam volume tomography measurement techniques for assessing bone level changes following regenerative periodontal therapy. J. Periodontol. 2009, 80, 48–55. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.; Schmidt, J.C.; Dula, K.; Sculean, A. Einsatz der digitalen volumentomographie zur diagnostik und behandlungsplanung in der parodontologie—Eine systematische übersicht. Quintessenz 2017, 68, 1151–1165. [Google Scholar]
- Hirschfeld, L.; Wasserman, B. A long-term survey of tooth loss in 600 treated periodontal patients. J. Periodontol. 1978, 49, 225–237. [Google Scholar] [CrossRef]
- Loos, B.; Nylund, K.; Claffey, N.; Egelberg, J. Clinical effects of root debridement in molar and non-molar teeth. A 2-year follow-up. J. Clin. Periodontol. 1989, 16, 498–504. [Google Scholar] [CrossRef]
- Nordland, P.; Garrett, S.; Kiger, R.; Vanooteghem, R.; Hutchens, L.H.; Egelberg, J. The effect of plaque control and root debridement in molar teeth. J. Clin. Periodontol. 1987, 14, 231–236. [Google Scholar] [CrossRef] [PubMed]
- Walter, C.; Weiger, R.; Zitzmann, N.U. Periodontal surgery in furcation-involved maxillary molars revisited: An introduction of guidelines for comprehensive treatment. Clin. Oral Investig. 2011, 15, 9–20. [Google Scholar] [CrossRef]
- Walter, C.; Weiger, R.; Zitzmann, N.U. Accuracy of three-dimensional imaging in assessing maxillary molar furcation involvement. J. Clin. Periodontol. 2010, 37, 436–441. [Google Scholar] [CrossRef]
- Walter, C.; Weiger, R.; Dietrich, T.; Lang, N.P.; Zitzmann, N.U. Does three-dimensional imaging offer a financial benefit for treating maxillary molars with furcation involvement? A pilot clinical case series. Clin. Oral Implants. Res. 2012, 23, 351–358. [Google Scholar] [CrossRef] [PubMed]
| Parameter | Scoring System/Classification | Criteria for Scoring/Classification of Parameters | ||
|---|---|---|---|---|
| Number of roots | 1 | 1 root | • complete root fusion = 1 root • incomplete root fusion = multirooted teeth (≥2 roots) | |
| 2 | 2 roots | |||
| 3 | 3 roots | |||
| Dehiscence | 0 | not present | • distance between alveolar crest and CEJ > 2 mm, resulting in exposed cervical root surface [12], buccally assessed | |
| 1 | present | |||
| Fenestration | 0 | not present | • lack of alveolar bone, not affecting the marginal alveolar bone and resulting in exposed root surface [12], buccally assessed | |
| 1 | present | |||
| Vertical bone defect | 0 | not present | • apical location of the base of the pocket with regard to the residual alveolar crest [13,14] • intrabony = infrabony component of the defect affecting one tooth/implant • crater = defect affecting two adjacent root/implant surfaces | |
| 1 | intrabony defect | |||
| 2 | crater | |||
| Number of bone walls | 1 | one-wall defect | • number of residual alveolar bone walls in intrabony defects [14] | |
| 2 | two-wall defect | |||
| 3 | three-wall defect | |||
| 4 | combination defect | |||
| Furcation involvement | 0 | not present | • horizontal loss of periodontal tissue support, that is, radiolucency in the furcation area [15] • classification according to Hamp et al. [15] | |
| 1 | present (I, II, III) | I | horizontal loss of periodontal tissue support ≤ 3 mm | |
| II | horizontal loss > 3 mm but not “through and through” destruction | |||
| III | horizontal “through and through” tissue destruction in the furcation | |||
| Root fusion | 0 | not present | • lack of a separating periodontal ligament between two adjacent roots [11] | |
| 1 | present | |||
| Root proximity | 0 | not present | • separating periodontal ligaments between two adjacent roots ≤ 0.8 mm [16] | |
| 1 | present | |||
| Root canal anatomy | I | 1 canal, 1 foramen | • classification according to Vertucci [17] • evaluation of each root separately | |
| II | 2 canals, fusion, 1 foramen | |||
| III | 1 canal, division, fusion, 1 foramen | |||
| IV | 2 canals, no fusion, 2 foramina | |||
| V | 1 canal, division, 2 foramina | |||
| VI | 2 canals, fusion, division, 2 foramina | |||
| VII | 1 canal, division, fusion, division, 2 foramina | |||
| VIII | 3 canals, no fusion, 3 foramina | |||
| Root canal cross-section | 1 | round | • classification according to Jou et al. [18] • evaluation of each root canal separately | |
| 2 | oval | |||
| 3 | long oval | |||
| 4 | flattened | |||
| 5 | irregular | |||
| Periapical status | 1 | healthy (PAI 1, 2) | • scoring system according to Ørstavik et al. [19] | |
| PAI 1 | normal periapical structure | |||
| PAI 2 | small changes in bone structure | |||
| PAI 3 | changes in bone structure with mineral loss | |||
| 2 | diseased (PAI 3, 4, 5) | PAI 4 | apical periodontitis with well-defined radiolucent areas | |
| PAI 5 | severe apical periodontitis with exacerbating features | |||
| • multirooted teeth were given the highest score detected at any root [10] | ||||
| Root canal filling | 0 | insufficient (score >1) | • scoring system according to Weiger et al. [20] • length: (1) 0-2 mm short of the radiographic apex, (2) >2 mm short of the radiographic apex, (3) extruded beyond the radiographic apex • density: (1) no voids and close adaptation to root canal walls, (2) voids or insufficient adaptation | |
| 1 | sufficient (score =1) | |||
| Caries | R0 | sound (no radiolucency) | • scoring system according to Pitts [21] • evaluation of each tooth surface separately • each tooth was given the highest score detected at any tooth surface | |
| R1 | outer half enamel lesion | |||
| R2 | inner half enamel lesion | |||
| R3 | outer half dentin lesion | |||
| R4 | inner half dentin lesion | |||
| Restoration quality | 0 | intact | • scoring system according to Tronstad et al. [22] • not intact = sign of overhangs, recurrent decay or open margins • intact = any restoration that appeared intact radiographically | |
| 1 | not intact | |||
| In addition to all scores: | N not assessable | • for example, due to artefacts, overlapping effects, resolution capacity and/or contrast limitations | ||
| Parameter | Number of Assessed Structures | Distribution of the Scores of Parameters (Number of Structures) * | ||
|---|---|---|---|---|
| CBCT | I-O | OPT | ||
| Number of roots | 23 teeth | 1 (19), 2 (1), 3 (3) | 1 (19), 2 (1), 3 (3) | 1 (19), 2 (1), 3 (1), N (2) |
| Dehiscence | 27 roots | 0 (16), 1 (11) | N (27) | N (27) |
| Fenestration | 27 roots | 0 (18), 1 (9) | N (27) | N (27) |
| Vertical bone defect | 23 teeth, 2 implants | 0 (22), 1 (3) | 0 (20), 1 (3), 2 (2) | 0 (23), 2 (2) |
| Number of bone walls | 2-5 vertical defects | 3 (1), 4 (2) | N (5) | N (2) |
| Furcation involvement | 11 furcation entrances | 0 (11) | 0 (4), N (7) | 0 (1), N (10) |
| Root fusion | 10 pairs of roots | 0 (10) | 0 (4), N (6) | 0 (2), N (8) |
| Root proximity | 10 pairs of roots | 0 (8), 1 (2) | 0 (2), 1 (2), N (6) | 0 (1), 1 (1), N (8) |
| Root canal anatomy | 30 roots | I (24), II (4), N (2) | I (18), II (2), N (10) | I (16), II (2), N (12) |
| Root canal cross-section | 34 root canals | 1 (30), N (4) | N (34) | N (34) |
| Periapical status | 30 roots, 2 implants | 1 (30), 2 (2) | 1 (31), 2 (1) | 1 (21), N (11) |
| Root canal filling | 2 root canal fillings | 1 (2) | 1 (2) | 0 (1), 1 (1) |
| Caries | 23 teeth | R0 (6), R3 (1), N (16) | R0 (23) | R0 (16), N (7) |
| Restoration quality | 16 restorations | 0 (2), N (14) | 0 (14), 1 (1), N (1) | 0 (4), 1 (1), N (11) |
| CBCT versus I-O | CBCT versus OPT | I-O versus OPT | CBCT vs. I-O vs. OPT | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| CBCT = I-O | CBCT > I-O | CBCT < I-O | Overall | CBCT = OPT | CBCT > OPT | CBCT < OPT | Overall | I-O = OPT | I-O > OPT | I-O < OPT | Overall | Overall | |
| Number of roots 1 | 23 (13, 10) | 0 | 0 | CBCT = I-O (100) | 21 (11, 10) | 2 (2, 0) | 0 | CBCT > OPT (9) | 21 (11, 10) | 2 (2, 0) | 0 | I-O > OPT (9) | CBCT = I-O > OPT |
| Dehiscence | 0 | 27 (16, 11) | 0 | CBCT > I-O (100) | 0 | 27 (16, 11) | 0 | CBCT > OPT (100) | 27 (16, 11) | 0 | 0 | I-O = OPT (100) | CBCT > I-O = OPT |
| Fenestration | 0 | 27 (16, 11) | 0 | CBCT > I-O (100) | 0 | 27 (16, 11) | 0 | CBCT > OPT (100) | 27 (16, 11) | 0 | 0 | I-O = OPT (100) | CBCT > I-O = OPT |
| Vertical bone defect 2 | 22 (11, 11) | 3 (2, 1) | 0 | CBCT > I-O (12) | 21 (10, 11) | 4 (3, 1) | 0 | CBCT > OPT (16) | 22 (12, 10) | 3 (1, 2) | 0 | I-O > OPT (12) | CBCT > I-O > OPT |
| Number of bone walls | 0 | 3 (2, 1) | 0 | CBCT > I-O (100) | 0 | 1 (1, 0) | 0 | CBCT > OPT (100) | 2 (2, 0) | 0 | 0 | I-O = OPT (100) | CBCT > I-O = OPT |
| Furcation involvement 3 | 4 (3, 1) | 7 (6, 1) | 0 | CBCT > I-O (64) | 1 (0, 1) | 10 (9, 1) | 0 | CBCT > OPT (91) | 8 (6, 2) | 3 (3, 0) | 0 | I-O > OPT (27) | CBCT > I-O > OPT |
| Root fusion | 4 (3, 1) | 6 (6, 0) | 0 | CBCT > I-O (60) | 2 (1, 1) | 8 (8, 0) | 0 | CBCT > OPT (80) | 8 (7, 1) | 2 (2, 0) | 0 | I-O > OPT (20) | CBCT > I-O > OPT |
| Root proximity | 4 (3, 1) | 6 (6, 0) | 0 | CBCT > I-O (60) | 2 (1, 1) | 8 (8, 0) | 0 | CBCT > OPT (80) | 8 (7, 1) | 2 (2, 0) | 0 | I-O > OPT (20) | CBCT > I-O > OPT |
| Root canal anatomy | 21 (12, 9) | 9 (7, 2) | 0 | CBCT > I-O (30) | 19 (10, 9) | 11 (9, 2) | 0 | CBCT > OPT (37) | 28 (17, 11) | 2 (2, 0) | 0 | I-O > OPT (7) | CBCT > I-O > OPT |
| Root canal cross-section | 5 (4, 1) | 29 (18, 11) | 0 | CBCT > I-O (85) | 5 (4, 1) | 29 (18, 11) | 0 | CBCT > OPT (85) | 34 (22, 12) | 0 | 0 | I-O = OPT (100) | CBCT > I-O = OPT |
| Periapical status | 31 (18, 13) | 1 (1, 0) | 0 | CBCT > I-O (3) | 19 (6, 13) | 13 (13, 0) | 0 | CBCT > OPT (41) | 20 (7, 13) | 12 (12, 0) | 0 | I-O > OPT (38) | CBCT > I-O > OPT |
| Root canal filling | 2 (2, 0) | 0 | 0 | CBCT = I-O (100) | 1 (1, 0) | 1 (1, 0) | 0 | CBCT > OPT (50) | 1 (1, 0) | 1 (1, 0) | 0 | I-O > OPT (50) | CBCT = I-O > OPT |
| Caries | 6 (1, 5) | 1 (0, 1) | 16 (12, 4) | CBCT < I-O (70) | 11 (6, 5) | 2 (1, 1) | 10 (6, 4) | CBCT < OPT (43) | 16 (6, 10) | 7 (7, 0) | 0 | I-O > OPT (30) | I-O > OPT > CBCT |
| Restoration quality | 2 (1, 1) | 1 (1, 0) | 13 (9, 4) | CBCT < I-O (81) | 12 (9, 3) | 1 (1, 0) | 3 (1, 2) | CBCT < OPT (19) | 6 (3, 3) | 10 (8, 2) | 0 | I-O > OPT (63) | I-O > OPT > CBCT |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schmidt, J.C.; Gutekunst, C.-J.; Dagassan-Berndt, D.; Schmidlin, P.R.; Walter, C. Comparison of Two-Dimensional and Three-Dimensional Radiographs Using Clinically Relevant Parameters. Dent. J. 2019, 7, 50. https://doi.org/10.3390/dj7020050
Schmidt JC, Gutekunst C-J, Dagassan-Berndt D, Schmidlin PR, Walter C. Comparison of Two-Dimensional and Three-Dimensional Radiographs Using Clinically Relevant Parameters. Dentistry Journal. 2019; 7(2):50. https://doi.org/10.3390/dj7020050
Chicago/Turabian StyleSchmidt, Julia C., Claudia-Julie Gutekunst, Dorothea Dagassan-Berndt, Patrick R. Schmidlin, and Clemens Walter. 2019. "Comparison of Two-Dimensional and Three-Dimensional Radiographs Using Clinically Relevant Parameters" Dentistry Journal 7, no. 2: 50. https://doi.org/10.3390/dj7020050
APA StyleSchmidt, J. C., Gutekunst, C.-J., Dagassan-Berndt, D., Schmidlin, P. R., & Walter, C. (2019). Comparison of Two-Dimensional and Three-Dimensional Radiographs Using Clinically Relevant Parameters. Dentistry Journal, 7(2), 50. https://doi.org/10.3390/dj7020050






