Investigating Eating Behaviors and Symptoms of Oral Frailty Using Questionnaires
Abstract
1. Introduction
2. Methods
2.1. Study Population and Survey
2.2. Questionnaire
2.3. Analysis
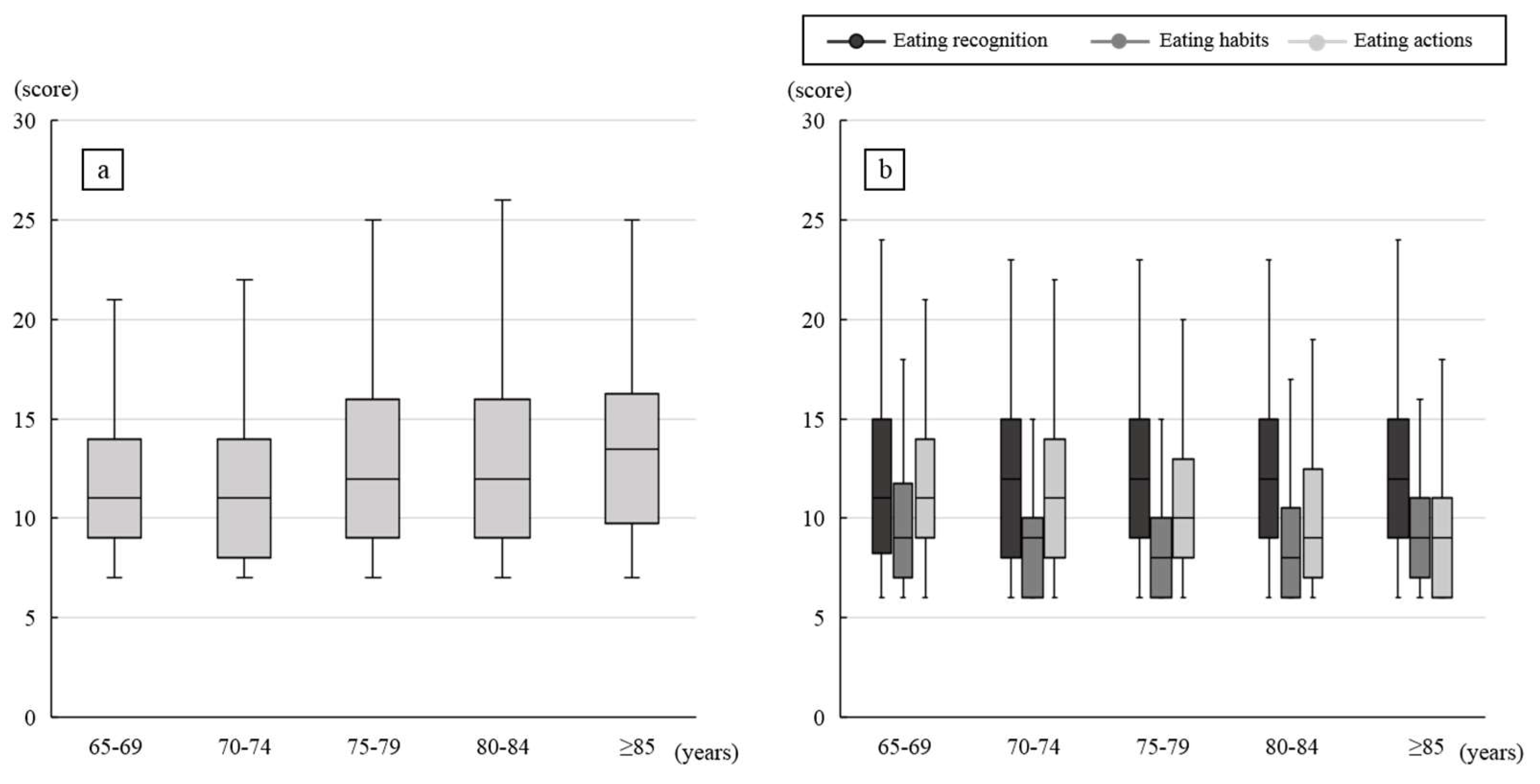
3. Results
4. Discussion
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Arai, H.; Ouchi, Y.; Toba, K.; Endo, T.; Shimokado, K.; Tsubota, K.; Matsuo, S.; Mori, H.; Yumura, W.; Yokode, M.; et al. Japan as the front-runner of super-aged societies: Perspectives from medicine and medical care in Japan. Geriatr. Gerontol. Int. 2015, 15, 673–687. [Google Scholar] [CrossRef]
- Genkai, S.; Kikutani, T.; Suzuki, R.; Tamura, F.; Yamashita, Y.; Yoshida, M. Loss of occlusal support affects the decline in activities of daily living in elderly people receiving home care. J. Prosthodont. Res. 2015, 59, 243–248. [Google Scholar] [CrossRef]
- Yanagisawa, S.; Yoshioka, M.; Shirayama, Y. Survey on nursing home caregivers’ basic knowledge of oral health management: Dental terminology. Dent. J. 2018, 6, 28. [Google Scholar] [CrossRef]
- Sasaki, E.; Ishibashi, Y.; Tsuda, E.; Ono, A.; Yamamoto, Y.; Inoue, R.; Takahashi, I.; Umeda, T.; Nakaji, S. Evaluation of locomotive disability using loco-check: A cross-sectional study in the Japanese general population. J. Orthop. Sci. 2013, 18, 121–129. [Google Scholar] [CrossRef]
- Fried, L.P.; Tangen, C.M.; Walston, J.; Newman, A.B.; Hirsch, C.; Gottdiener, J.; Seeman, T.; Tracy, R.; Kop, W.J.; Burke, G.; et al. Frailty in older adults: Evidence for a phenotype. J. Gerontol. A Biol. Sci. Med. Sci. 2001, 56, 146–156. [Google Scholar] [CrossRef]
- Niesten, D.; van Mourik, K.; van der Sanden, W. The impact of frailty on oral care behavior of older people: A qualitative study. BMC Oral Health 2013, 13, 61. [Google Scholar] [CrossRef]
- Cruz-Jentoft, A.J.; Baeyens, J.P.; Bauer, J.M.; Boirie, Y.; Cederholm, T.; Landi, F.; Martin, F.C.; Michel, J.P.; Rolland, Y.; Schneider, S.M.; et al. Sarcopenia: European consensus on definition and diagnosis: Report of the European working group on sarcopenia in older people. Age Ageing 2010, 39, 412–423. [Google Scholar] [CrossRef]
- Nakamichi, A.; Goto, T.; Ichikawa, T. Evaluation of eating behavior and mouthful volume: Validity of YN eating behavior questionnaire. J. Oral Health Biosci. 2015, 27, 71–80. [Google Scholar]
- Iijima, K. Upstream preventive strategy for age-related sarcopenia in the elderly: Why do the elderly fall into inadequate nutrition? Ann. Jpn. Prosthodont. Soc. 2015, 7, 92–101. [Google Scholar] [CrossRef][Green Version]
- Kera, T.; Kawai, H.; Yoshida, H.; Hirano, H.; Kojima, M.; Fujiwara, Y.; Ihara, K.; Obuchi, S. Classification of frailty using the Kihon checklist: A cluster analysis of older adults in urban areas. Geriatr. Gerontol. Int. 2017, 17, 69–77. [Google Scholar] [CrossRef]
- Hihara, T.; Goto, T.; Yanagisawa, S.; Nakamichi, A.; Ichikawa, T. The symptoms of oral frailty and physical frailty in every age group: An investigation by questionnaire. J. Gerodont. 2017, 32, 33–47. [Google Scholar]
- Minakuchi, S.; Tsuga, K.; Ikebe, K.; Ueda, T.; Tamura, F.; Nagao, K.; Furuya, J.; Matsuo, K.; Yamamoto, K.; Kanazawa, M.; et al. Oral hypofunction in the older population: Position paper of the Japanese Society of Gerodontology in 2016. Gerodontology 2018, 35, 317–324. [Google Scholar] [CrossRef]
- Heintze, U.; Birkhed, D.; Björn, H. Secretion rate and buffer effect of resting and stimulated whole saliva as a function of age and sex. Swed. Dent. J. 1983, 7, 227–238. [Google Scholar]
- Utanohara, Y.; Hayashi, R.; Yoshikawa, M.; Yoshida, M.; Tsuga, K.; Akagawa, Y. Standard values of maximum tongue pressure taken using newly developed disposable tongue pressure measurement device. Dysphagia 2008, 23, 286–290. [Google Scholar] [CrossRef]
- Kono, R. Relationship between occlusal force and preventive factors for disability among community-dwelling elderly persons. Jpn. J. Geriatr. 2009, 46, 55–62. [Google Scholar] [CrossRef]
- Kimura, Y.; Wada, T.; Ishine, M.; Ishimoto, Y.; Kasahara, Y.; Konno, A.; Nakatsuka, M.; Sakamoto, R.; Okumiya, K.; Fujisawa, M.; et al. Food diversity is closely associated with activities of daily living, depression, and quality of life in community-dwelling elderly people. J. Am. Geriatr. Soc. 2009, 57, 922–924. [Google Scholar] [CrossRef]
- Feldman, R.S.; Kapur, K.K.; Alman, J.E.; Chauncey, H.H. Aging and mastication: Changes in performance and in the swallowing threshold with natural dentition. J. Am. Geriatr. Soc. 1980, 28, 97–103. [Google Scholar] [CrossRef]
- Guertin, T.L. Eating behavior of bulimics, self-identified binge eaters, and non-eating-disordered individuals: What differentiates these populations? Clin. Psychol. Rev. 1999, 19, 1–23. [Google Scholar] [CrossRef]
- Carnell, S.; Wardle, J. Measuring behavioural susceptibility to obesity: Validation of the child eating behaviour questionnaire. Appetite 2007, 48, 104–113. [Google Scholar] [CrossRef]
- Micali, N.; Holliday, J.; Karwautz, A.; Haidvogl, M.; Wagner, G.; Fernandez-Aranda, F.; Badia, A.; Gimenez, L.; Solano, R.; Brecelj-Anderluh, M.; et al. Childhood eating and weight in eating disorders: A multi-centre European study of affected women and their unaffected sisters. Psychother. Psychosom. 2007, 76, 234–241. [Google Scholar] [CrossRef]
- Otsuka, R.; Tamakoshi, K.; Yatsuya, H.; Wada, K.; Matsushita, K.; OuYang, P.; Hotta, Y.; Takefuji, S.; Mitsuhashi, H.; Sugiura, K.; et al. Eating fast leads to insulin resistance: Findings in middle-aged Japanese men and women. Prev. Med. 2008, 46, 154–159. [Google Scholar] [CrossRef]
- Lee, J.S.; Mishra, G.; Hayashi, K.; Watanabe, E.; Mori, K.; Kawakubo, K. Combined eating behaviors and overweight: Eating quickly, late evening meals, and skipping breakfast. Eat. Behav. 2016, 21, 84–88. [Google Scholar] [CrossRef]
- Lee, M.S.; Huang, Y.C.; Wahlqvist, M.L. Chewing ability in conjunction with food intake and energy status in later life affects survival in Taiwanese with the metabolic syndrome. J. Am. Geriatr. Soc. 2010, 58, 1072–1080. [Google Scholar] [CrossRef]
- Park, S.; Shin, W.S. Differences in eating behaviors and masticatory performances by gender and obesity status. Physiol. Behav. 2015, 138, 69–74. [Google Scholar] [CrossRef]
| Questions | Estimation | |||
|---|---|---|---|---|
| Questionnaires on “eating recognition” of eating behaviors | ||||
| · I feel uneasy when the there is little food left in the refrigerator. | 1 | 2 | 3 | 4 |
| · I keep a food around me. | 1 | 2 | 3 | 4 |
| · I subconsciously eat a food whenever another person eats. | 1 | 2 | 3 | 4 |
| · I eat a food when I have a free time. | 1 | 2 | 3 | 4 |
| · I eat fruits and sweets. | 1 | 2 | 3 | 4 |
| · I have a soft spot for sweet foods. | 1 | 2 | 3 | 4 |
| Questionnaires on “eating habit” of eating behaviors | ||||
| · I swing by a convenience store. | 1 | 2 | 3 | 4 |
| · I go out to eat and use delivery service. | 1 | 2 | 3 | 4 |
| · I have an irregular eating pattern. | 1 | 2 | 3 | 4 |
| · I take extra order in the restraint and delivery service. | 1 | 2 | 3 | 4 |
| · I use fast foods. | 1 | 2 | 3 | 4 |
| · I live on meat. | 1 | 2 | 3 | 4 |
| Questionnaires on “eating action” of eating behaviors | ||||
| · I am speed eating. | 1 | 2 | 3 | 4 |
| · I gain weight in taking a long holiday. | 1 | 2 | 3 | 4 |
| · I do not chew foods well. | 1 | 2 | 3 | 4 |
| · I regret eating too much. | 1 | 2 | 3 | 4 |
| · I eat with having my mouth full of foods. | 1 | 2 | 3 | 4 |
| · I continue to eat without a rest. | 1 | 2 | 3 | 4 |
| Questionnaires on oral frailty | ||||
| · I have dental problem than before. | 1 | 2 | 3 | 4 |
| · I am aware of saliva problem than before. | 1 | 2 | 3 | 4 |
| · I bite cheek and tongue than before. | 1 | 2 | 3 | 4 |
| · I drop foods while eating than before. | 1 | 2 | 3 | 4 |
| · I feel the difficulty to chew than before. | 1 | 2 | 3 | 4 |
| · I feel non smoothness of tongue actions than before. | 1 | 2 | 3 | 4 |
| · I am aware of swallowing action than before. | 1 | 2 | 3 | 4 |
| Age (Years) | Male | Female | Total |
|---|---|---|---|
| 65–69 | 98 | 152 | 250 |
| 70–74 | 53 | 103 | 156 |
| 75–79 | 43 | 114 | 157 |
| 80-84 | 32 | 75 | 107 |
| ≥85 | 31 | 43 | 56 |
| Total | 257 | 487 | 744 |
| Category | Questions on Eating Behaviors | β | t-Value | VIF |
|---|---|---|---|---|
| Eating recognition | I feel uneasy when the there is little food left in the refrigerator. | 0.065 | 1.899 | 1.160 |
| I keep food around me. | 0.006 | 0.173 | 1.368 | |
| I subconsciously eat a food whenever another person eats. | 0.025 | 0.635 | 1.612 | |
| I eat a food when I have s free time. | 0.073 | 1.881 | 1.520 | |
| I eat fruits and sweets. | 0.058 | 1.457 | 1.610 | |
| I have a soft spot for sweet foods. | 0.101 * | 2.801 | 1.298 | |
| Eating habit | I swing by a convenience store. | 0.023 | 0.671 | 1.151 |
| I go out to eat and use delivery service. | 0.039 | 1.131 | 1.210 | |
| I have an irregular eating pattern | 0.070 * | 2.067 | 1.167 | |
| I take extra order in the restraint and delivery service. | 0.091 * | 2.487 | 1.335 | |
| I use fast foods. | 0.058 | 1.603 | 1.335 | |
| I live on meat. | 0.018 | 0.509 | 1.204 | |
| Eating action | I am speed eating | −0.081 * | −2.156 | 1.436 |
| I gain weight when taking a long holiday. | 0.054 | 1.522 | 1.279 | |
| I do not chew foods well. | 0.209 * | 5.418 | 1.494 | |
| I regret eating too much. | 0.01 | 0.245 | 1.627 | |
| I eat with having my mouth full of foods. | 0.026 | 0.700 | 1.360 | |
| I continue to eat without a rest. | 0.101 * | 2.692 | 1.403 |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hihara, T.; Goto, T.; Ichikawa, T. Investigating Eating Behaviors and Symptoms of Oral Frailty Using Questionnaires. Dent. J. 2019, 7, 66. https://doi.org/10.3390/dj7030066
Hihara T, Goto T, Ichikawa T. Investigating Eating Behaviors and Symptoms of Oral Frailty Using Questionnaires. Dentistry Journal. 2019; 7(3):66. https://doi.org/10.3390/dj7030066
Chicago/Turabian StyleHihara, Tsukasa, Takaharu Goto, and Tetsuo Ichikawa. 2019. "Investigating Eating Behaviors and Symptoms of Oral Frailty Using Questionnaires" Dentistry Journal 7, no. 3: 66. https://doi.org/10.3390/dj7030066
APA StyleHihara, T., Goto, T., & Ichikawa, T. (2019). Investigating Eating Behaviors and Symptoms of Oral Frailty Using Questionnaires. Dentistry Journal, 7(3), 66. https://doi.org/10.3390/dj7030066





