Early Life Professional and Layperson Support Reduce Poor Oral Hygiene Habits in Toddlers—A Prospective Birth Cohort Study
Abstract
1. Introduction
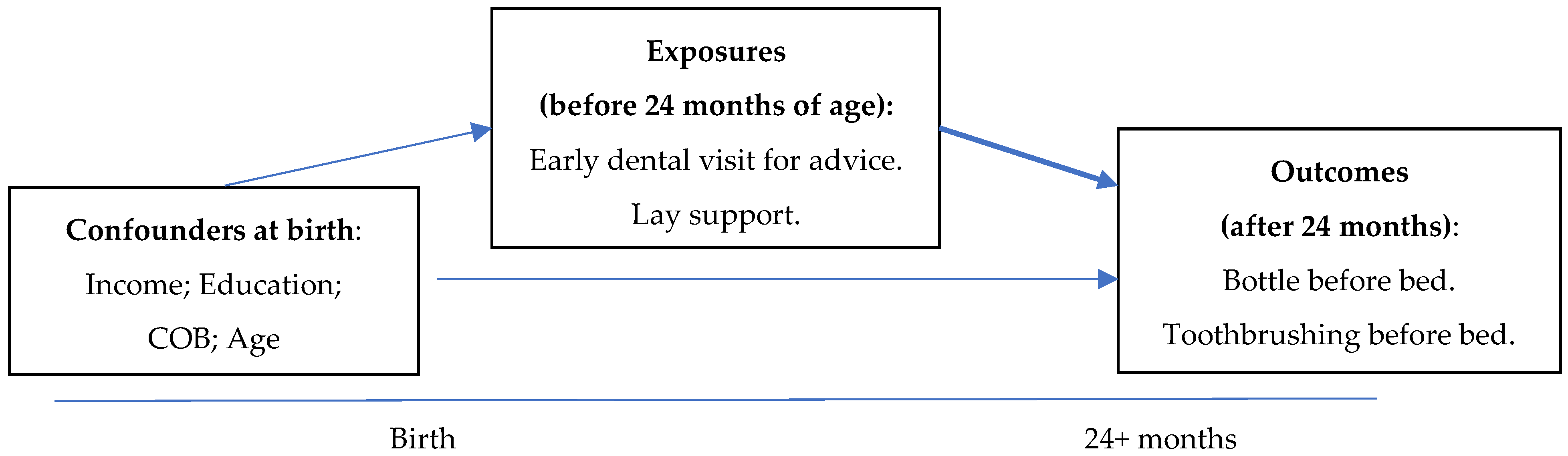
2. Methods
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Drury, T.F.; Horowitz, A.M.; Ismail, A.I.; Maertens, M.P.; Rozier, R.G.; Selwitz, R.H. Diagnosing and reporting early childhood caries for research purposes. A report of a workshop sponsored by the National Institute of Dental and Craniofacial Research, the Health Resources and Services Administration, and the Health Care Financing Administration. J. Public Health Dent. 1999, 59, 192–197. [Google Scholar] [PubMed]
- Fisher-Owens, S.A.; Gansky, S.A.; Platt, L.J.; Weintraub, J.A.; Soobader, M.J.; Bramlett, M.D.; Newacheck, P.W. Influences on children’s oral health: a conceptual model. Pediatrics 2007, 120, 510–520. [Google Scholar] [CrossRef] [PubMed]
- Armfield, J.M.; Roberts-Thomson, K.F.; Spencer, A.J. The Child Dental Health Survey, Australia 1999. Trend across the 1990s; Australian Research Centre for Population Oral Health: Adelaide, Australia, 2003. [Google Scholar]
- Ha, D.H.; Roberts-Thomson, K.F.; Armfield, J.M. The Child Dental Health Survey Australia, 2005 and 2006; Australian Institute of Health and Welfare: Bruce, Australian, 2011. [Google Scholar]
- Plutzer, K.; Spencer, A.J. Efficacy of an oral health promotion intervention in the prevention of early childhood caries. Community Dent. Oral Epidemiol. 2008, 36, 335–346. [Google Scholar] [CrossRef] [PubMed]
- Jackson, S.L.; Vann, W.F.J.; Kotch, J.B.; Pahel, B.T.; Lee, J.Y. Impact of poor oral health on children’s school attendance and performance. Am. J. Public Health 2011, 101, 1900–1906. [Google Scholar] [CrossRef] [PubMed]
- Jordan, A.R.; Becker, N.; Johren, H.P.; Zimmer, S. Early Childhood Caries and Caries Experience in Permanent Dentition: A 15-year Cohort Study. Swiss Dent. J. 2016, 126, 114–119. [Google Scholar] [PubMed]
- Leong, P.M.; Gussy, M.G.; Barrow, S.Y.; Silva-Sanigorski, A.; Waters, E. A systematic review of risk factors during first year of life for early childhood caries. Int. J. Paediatr. Dent. 2013, 23, 235–250. [Google Scholar] [CrossRef] [PubMed]
- Fleming, P. Timetable for oral prevention in childhood—A current opinion. Prog. Orthod. 2015, 16, 27. [Google Scholar] [CrossRef] [PubMed]
- Kumar, S.; Tadakamadla, J.; Johnson, N.W. Effect of Toothbrushing Frequency on Incidence and Increment of Dental Caries: A Systematic Review and Meta-Analysis. J. Dent. Res. 2016, 95, 1230–1236. [Google Scholar] [CrossRef] [PubMed]
- Rugg-Gunn, A.J. Introduction: Guidelines for Fluoride Intake—Are They Appropriate? Adv. Dent. Res. 2018, 29, 142–143. [Google Scholar] [CrossRef] [PubMed]
- Finlayson, T.L.; Siefert, K.; Ismail, A.I.; Sohn, W. Maternal self-efficacy and 1–5-year-old children’s brushing habits. Community Dent. Oral Epidemiol. 2007, 35, 272–281. [Google Scholar] [CrossRef] [PubMed]
- Spencer, A.J. The use of fluorides in Australia: Guidelines. Aust. Dent. J. 2006, 51, 195–199. [Google Scholar] [CrossRef]
- Do, L.; Spencer, A. Oral Health of Australian Hhildren. In The National Child Oral Health Study 2012–2014; University Press: Adelaide, Australian, 2016. [Google Scholar]
- Douglass, J.M.; Tinanoff, N.; Tang, J.M.; Altman, D.S. Dental caries patterns and oral health behaviors in Arizona infants and toddlers. Community Dent. Oral Epidemiol. 2001, 29, 14–22. [Google Scholar] [CrossRef] [PubMed]
- Van Palenstein Helderman, W.H.; Soe, W.; Van Hof, M.A. Risk factors of early childhood caries in a Southeast Asian population. J. Dent. Res. 2006, 85, 85–88. [Google Scholar] [CrossRef] [PubMed]
- Wan, A.K.; Seow, W.K.; Purdie, D.M.; Bird, P.S.; Walsh, L.J.; Tudehope, D.I. A longitudinal study of Streptococcus mutans colonization in infants after tooth eruption. J. Dent. Res. 2003, 82, 504–508. [Google Scholar] [CrossRef] [PubMed]
- Peltzer, K.; Mongkolchati, A. Severe early childhood caries and social determinants in three-year-old children from Northern Thailand: A birth cohort study. BMC Oral Health 2015, 15, 108. [Google Scholar] [CrossRef] [PubMed]
- Pieper, K.; Dressler, S.; Heinzel-Gutenbrunner, M.; Neuhauser, A.; Krecker, M.; Wunderlich, K.; Jablonski-Momeni, A. The influence of social status on pre-school children’s eating habits, caries experience and caries prevention behavior. Int. J. Public Health 2012, 57, 207–215. [Google Scholar] [CrossRef] [PubMed]
- Bhaskar, V.; McGraw, K.A.; Divaris, K. The importance of preventive dental visits from a young age: systematic review and current perspectives. Clin. Cosmet. Investig. Dent. 2014, 6, 21–27. [Google Scholar] [PubMed]
- AAPD. Perinatal and Infant Oral Health Care. Pediatr. Dent. 2017, 39, 208–212. [Google Scholar]
- Sheiham, A.; Alexander, D.; Cohen, L.; Marinho, V.; Moyses, S.; Petersen, P.E.; Weyant, R. Global oral health inequalities: Task group—Implementation and delivery of oral health strategies. Adv. Dent. Res. 2011, 23, 259–267. [Google Scholar] [CrossRef] [PubMed]
- Ismail, A.; Razak, I.A.; Ab-Murat, N. The impact of anticipatory guidance on early childhood caries: a quasi-experimental study. BMC Oral Health 2018, 18, 126. [Google Scholar] [CrossRef] [PubMed]
- Seow, W.K.; Cheng, E.; Wan, V. Effects of oral health education and tooth-brushing on mutans streptococci infection in young children. Pediatr. Dent. 2003, 25, 223–228. [Google Scholar] [PubMed]
- Popo, E.; Kenyon, S.; Dann, S.A.; MacArthur, C.; Blissett, J. Effects of lay support for pregnant women with social risk factors on infant development and maternal psychological health at 12 months postpartum. PLoS ONE 2017, 12, e0182544. [Google Scholar] [CrossRef] [PubMed]
- Do, L.G.; Scott, J.A.; Thomson, W.M.; Stamm, J.W.; Rugg-Gunn, A.J.; Levy, S.M.; Spencer, A.J. Common risk factor approach to address socioeconomic inequality in the oral health of preschool children—A prospective cohort study. BMC Public Health 2014, 14, 429. [Google Scholar] [CrossRef] [PubMed]
- Marshman, Z.; Ahern, S.M.; McEachan, R.R.C.; Rogers, H.J.; Gray-Burrows, K.A.; Day, P.F. Parents’ Experiences of Toothbrushing with Children: A Qualitative Study. JDR Clin. Trans. Res. 2016, 1, 122–130. [Google Scholar] [CrossRef] [PubMed]
- Kobayashi, M.; Chi, D.; Coldwell, S.E.; Domoto, P.; Milgrom, P. The effectiveness and estimated costs of the access to baby and child dentistry program in Washington State. J. Am. Dent. Assoc. 2005, 136, 1257–1263. [Google Scholar] [CrossRef] [PubMed]
- Medeiros, P.B.; Otero, S.A.; Frencken, J.E.; Bronkhorst, E.M.; Leal, S.C. Effectiveness of an oral health program for mothers and their infants. Int. J. Paediatr. Dent. 2015, 25, 29–34. [Google Scholar] [CrossRef] [PubMed]
| Variables | Total (n = 1183) * | % | 95% CI | Sample at Birth n = 2112 (%) | Population + |
|---|---|---|---|---|---|
| OUTCOMES | |||||
| Put child to bed with bottle | |||||
| No | 741 | 63.4 | 60.7–66.2 | -- | -- |
| Yes | 427 | 36.6 | 33.8–39.3 | -- | -- |
| Brushing child’s teeth before bed | |||||
| No | 299 | 25.6 | 23.1–28.1 | -- | -- |
| Yes | 868 | 74.4 | 71.9–76.9 | -- | -- |
| EXPLANATORY VARIABLES | |||||
| Early dental visit for advice | |||||
| No | 749 | 70.7 | 67.9–73.4 | -- | -- |
| Yes | 311 | 29.3 | 26.6-32.1 | -- | -- |
| Lay support | |||||
| Yes | 840 | 81.6 | 79.2–83.9 | -- | -- |
| No | 190 | 18.5 | 16.1–20.8 | -- | -- |
| COVARIATES | |||||
| Family income at birth | |||||
| Q1 (<AU$80,000) | 539 | 46.1 | 43.1–49.0 | 53.9 | 43.8 |
| Q2 (AU$80,000–120,000) | 353 | 30.2 | 27.5–32.9 | 27.6 | 31.8 |
| Q3 (>AU120,000) | 278 | 23.7 | 21.3–26.3 | 18.5 | 24.4 |
| Mother’s COB | |||||
| Other | 73 | 6.2 | 4.9–7.6 | 6.7 | 8.2 |
| Asia except India | 132 | 11.3 | 9.5–13.1 | 11.4 | 8.8 |
| India | 90 | 7.7 | 6.2–9.2 | 8.9 | 4.0 |
| Aust., NZ, UK | 875 | 74.8 | 72.3–77.3 | 73.0 | 79.0 |
| Mother’s age groups | |||||
| <25 year old | 124 | 10.7 | 8.9–12.5 | 16.3 | 17.8 |
| 25–34 | 787 | 68.1 | 65.5–70.9 | 64.2 | 62.4 |
| >=35 year old | 244 | 21.1 | 18.7–23.4 | 19.5 | 19.8 |
| Mother’s education | |||||
| School/Vocational | 626 | 54.1 | 51.2–56.9 | 54.0 | 59.2 |
| Tertiary | 532 | 45.9 | 43.1–48.8 | 46.0 | 40.8 |
| Variables | Put Child to Bed with a Bottle | Did Not Brush Child’s Teeth before Bed |
|---|---|---|
| % (95% CI) | % (95% CI) | |
| Early dental visit for advice | ||
| Yes | 29.4 (24.3–34.4) | 20.9 (16.4–25.4) |
| No | 37.5 (34.0–41.0) | 27.3 (24.1–30.5) |
| Lay support | ||
| Yes | 33.6 (30.4–36.8) | 23.4 (20.5–26.3) |
| No | 40.2 (33.2–47.2) | 30.7 (24.1–37.3) |
| Family income at birth | ||
| Q1 (<AU$80,000) | 38.7 (34.6–42.9) | 29.2 (25.3–33.1) |
| Q2 (AU$80,000–120,000) | 39.8 (34.7–45.0) | 24.4 (19.9–28.9) |
| Q3 (>AU120,000) | 27.7 (22.4–32.9) | 20.0 (15.3–24.7) |
| Mother’s COB | ||
| Other | 35.6 (24.6–46.6) | 30.1 (19.6–40.7) |
| Asia except India | 42.4 (34.0–50.9) | 25.2 (17.8–32.6) |
| India | 44.4 (34.2–54.7) | 58.4 (48.2–68.7) |
| Aust., NZ, UK | 35.1 (31.9–38.3) | 21.9 (19.2–24.7) |
| Mother’s age group | ||
| <25 years old | 47.1 (38.2–56.0) | 24.6 (17.0–32.2) |
| 25–34 years old | 35.4 (32.1–38.8) | 24.4 (21.4–27.4) |
| ≥35 years old | 35.4 (29.4–41.4) | 31.0 (25.2–36.8) |
| Mother’s education | ||
| School/vocational | 40.7 (36.4−44.9) | 26.0 (22.2−29.8) |
| Tertiary | 33.5 (29.9−37.1) | 25.2 (21.9−28.6) |
| Variables | Putting Child to Bed with a Bottle | Did Not Brush Child’s Teeth before Bed | ||
|---|---|---|---|---|
| Adj. PR | 95% CI | Adj. PR | 95% CI | |
| Early dental visit for advice | ||||
| Yes | Ref | Ref | ||
| No | 1.30 | 1.04–1.64 | 1.37 | 1.02–1.84 |
| Lay support | ||||
| Yes | Ref | Ref | ||
| No | 1.21 | 0.97–1.49 | 1.20 | 0.93–1.55 |
| Family income | ||||
| Q1 (<AU$80,000) | 1.15 | 0.87–1.51 | 0.99 | 0.73–1.34 |
| Q2 (AU$80,000–120,000) | 1.30 | 0.99–1.70 | 1.02 | 0.74–1.41 |
| Q3 (>AU120,000) | Ref | Ref | ||
| Mother’s COB | ||||
| Others | 1.08 | 0.72–1.62 | 1.17 | 0.73–1.85 |
| Asia except India | 1.44 | 1.07–1.93 | 1.26 | 0.86–1.83 |
| India | 1.63 | 1.20–2.21 | 2.69 | 1.99–3.62 |
| Aust., NZ, UK | Ref | Ref | ||
| Mother’s age group | ||||
| <25 year old | 1.26 | 0.91–1.76 | 0.61 | 0.38–1.00 |
| 25–34 | 0.99 | 0.78–1.24 | 0.63 | 0.49–0.81 |
| >=35 year old | Ref | Ref | ||
| Mother’s education | ||||
| School/vocational | 1.26 | 1.02–1.56 | 1.25 | 0.97–1.60 |
| Tertiary | Ref | Ref | ||
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ha, D.H.; Do, L.G. Early Life Professional and Layperson Support Reduce Poor Oral Hygiene Habits in Toddlers—A Prospective Birth Cohort Study. Dent. J. 2018, 6, 56. https://doi.org/10.3390/dj6040056
Ha DH, Do LG. Early Life Professional and Layperson Support Reduce Poor Oral Hygiene Habits in Toddlers—A Prospective Birth Cohort Study. Dentistry Journal. 2018; 6(4):56. https://doi.org/10.3390/dj6040056
Chicago/Turabian StyleHa, Diep Hong, and Loc Giang Do. 2018. "Early Life Professional and Layperson Support Reduce Poor Oral Hygiene Habits in Toddlers—A Prospective Birth Cohort Study" Dentistry Journal 6, no. 4: 56. https://doi.org/10.3390/dj6040056
APA StyleHa, D. H., & Do, L. G. (2018). Early Life Professional and Layperson Support Reduce Poor Oral Hygiene Habits in Toddlers—A Prospective Birth Cohort Study. Dentistry Journal, 6(4), 56. https://doi.org/10.3390/dj6040056





