Effects of Amorphous Calcium Phosphate Administration on Dental Sensitivity during In-Office and At-Home Interventions
Abstract
1. Introduction
2. Materials and Methods
2.1. Patient Selection
- Age ≥ 18
- Overall good healthy condition
- With all the dentary settings
- Smokers and non-smokers
- Dental hypersensitivity
- Known periodontal problems
- Subjected to bleaching within 1 year
- Pregnancy
- Bleeding On Probing (BOP) > 5%, Plaque Index (PI) > 18%
2.2. Study Groups
2.3. Procedures
- Sonicare Philips toothbrush
- Biorepair toothpaste containing nano-hydroxyapatite
- Use of an interdental toothbrush
2.4. Statistical Analysis
3. Results
3.1. Patient Characteristics
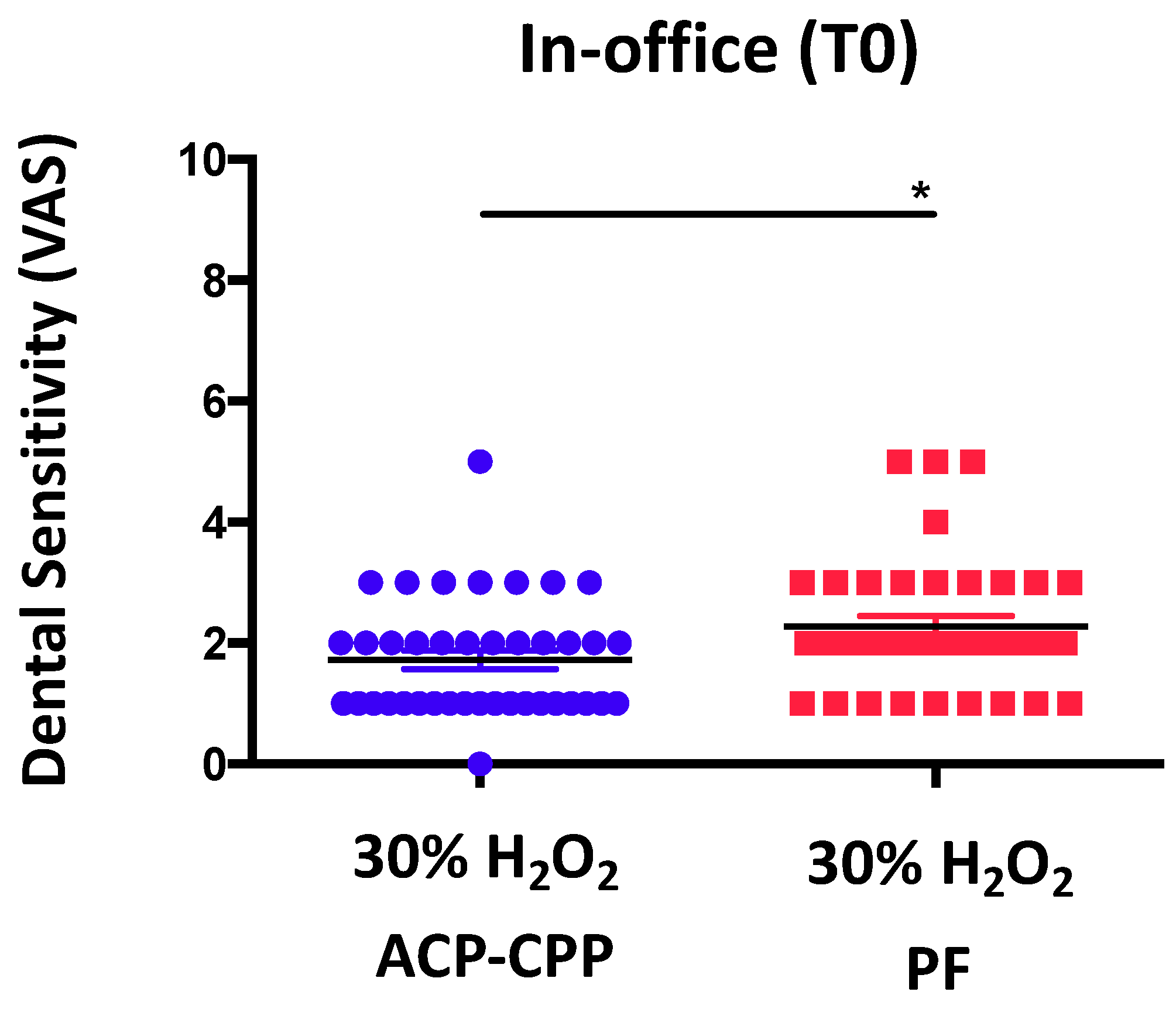
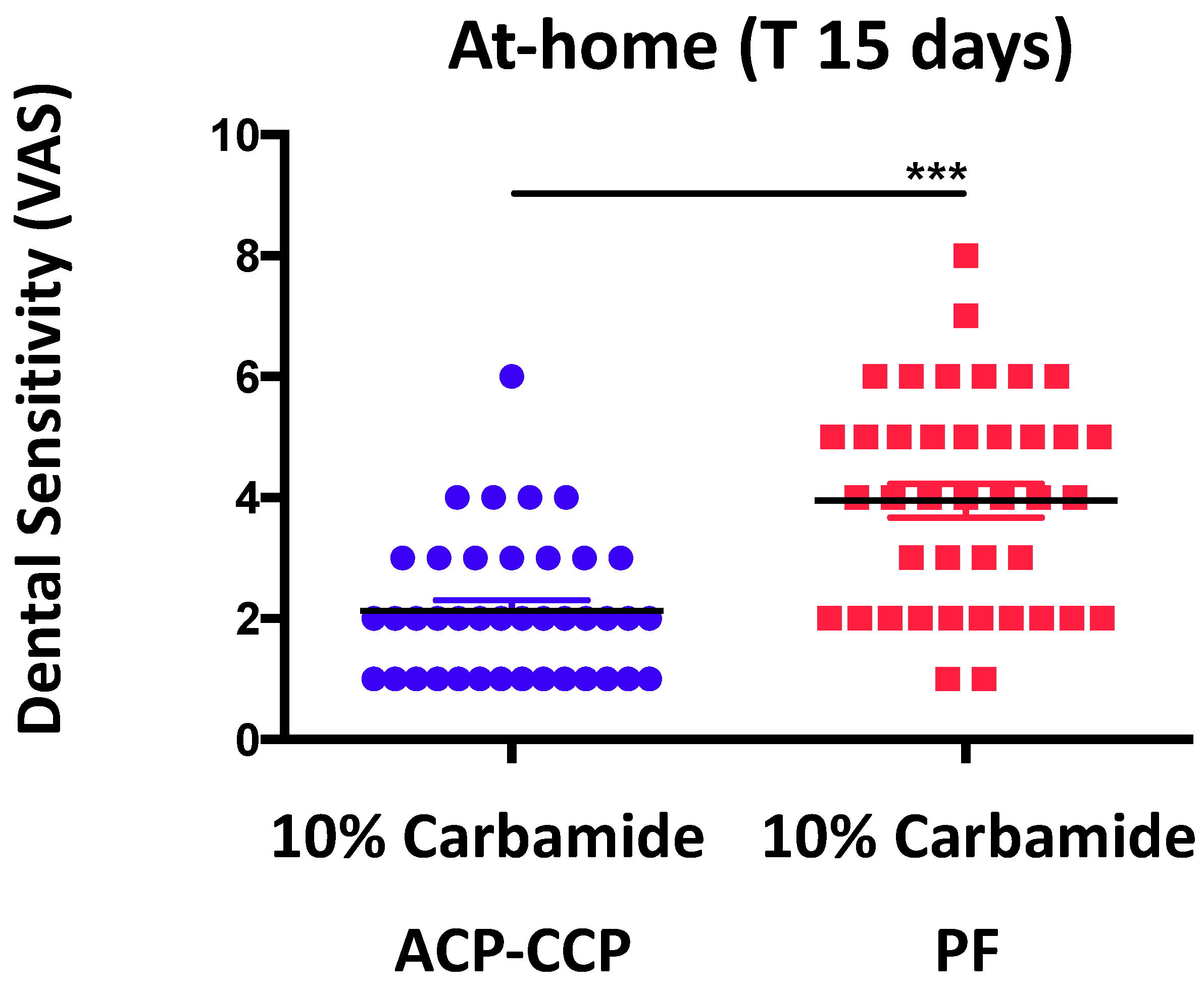
3.2. ACP-CPP Administration during Bleaching Procedures Reduces Dental Sensitivity Both in-Office and at Home
4. Discussion
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Rad, M.; Shahravan, A.; Haghdoost, A.A. Oral health knowledge, attitude, and practice in 12-year-old schoolchildren in Iran. J. Int. Soc. Prev. Community Dent. 2015, 5, 419–424. [Google Scholar] [PubMed]
- Winston, A.E.; Bhaskar, S.N. Caries prevention in the 21st century. J. Am. Dent. Assoc. 1998, 129, 1579–1587. [Google Scholar] [CrossRef] [PubMed]
- Yadav, K.; Sofat, A.; Gambhir, R.S.; Galhotra, V. Dentin hypersensitivity following tooth preparation: A clinical study in the spectrum of gender. J. Nat. Sci. Biol. Med. 2014, 5, 21–24. [Google Scholar] [PubMed]
- Henson, S.T.; Lindauer, S.J.; Gardner, W.G.; Shroff, B.; Tufekci, E.; Best, A.M. Influence of dental esthetics on social perceptions of adolescents judged by peers. Am. J. Orthod. Dent. Orthop. 2011, 140, 389–395. [Google Scholar] [CrossRef] [PubMed]
- Presoto, C.D.; Bortolatto, J.F.; de Carvalho, P.P.; Trevisan, T.C.; Floros, M.C.; Junior, O.B. New parameter for in-office dental bleaching. Case Rep. Dent. 2016, 2016, 6034757. [Google Scholar] [CrossRef] [PubMed]
- Reis, A.; Kossatz, S.; Martins, G.C.; Loguercio, A.D. Efficacy of and effect on tooth sensitivity of in-office bleaching gel concentrations: A randomized clinical trial. Oper. Dent. 2013, 38, 386–393. [Google Scholar] [CrossRef] [PubMed]
- Minoux, M.; Serfaty, R. Vital tooth bleaching: Biologic adverse effects—A review. Quintessence Int. 2008, 39, 645–659. [Google Scholar] [PubMed]
- Buchalla, W.; Attin, T. External bleaching therapy with activation by heat, light or laser—A systematic review. Dent. Mater. 2007, 23, 586–596. [Google Scholar] [CrossRef] [PubMed]
- Joiner, A. The bleaching of teeth: A review of the literature. J. Dent. 2006, 34, 412–419. [Google Scholar] [CrossRef] [PubMed]
- Poggio, C.; Grasso, N.; Ceci, M.; Beltrami, R.; Colombo, M.; Chiesa, M. Ultrastructural evaluation of enamel surface morphology after tooth bleaching followed by the application of protective pastes. Scanning 2016, 38, 221–226. [Google Scholar] [CrossRef] [PubMed]
- Basting, R.T.; Rodrigues, A.L., Jr.; Serra, M.C. The effect of 10% carbamide peroxide, carbopol and/or glycerin on enamel and dentin microhardness. Oper. Dent. 2005, 30, 608–616. [Google Scholar] [PubMed]
- Goldberg, M.; Grootveld, M.; Lynch, E. Undesirable and adverse effects of tooth-whitening products: A review. Clin. Oral Investig. 2010, 14, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Bortolatto, J.F.; Pretel, H.; Floros, M.C.; Luizzi, A.C.; Dantas, A.A.; Fernandez, E.; Moncada, G.; de Oliveira, O.B., Jr. Low concentration H2O2/TiO_N in office bleaching: A randomized clinical trial. J. Dent. Res. 2014, 93, 66S–71S. [Google Scholar] [CrossRef] [PubMed]
- Jorgensen, M.G.; Carroll, W.B. Incidence of tooth sensitivity after home whitening treatment. J. Am. Dent. Assoc. 2002, 133, 1076–1082. [Google Scholar] [CrossRef] [PubMed]
- Cunha-Cruz, J.; Wataha, J.C.; Zhou, L.; Manning, W.; Trantow, M.; Bettendorf, M.M.; Heaton, L.J.; Berg, J. Treating dentin hypersensitivity: Therapeutic choices made by dentists of the northwest precedent network. J. Am. Dent. Assoc. 2010, 141, 1097–1105. [Google Scholar] [CrossRef] [PubMed]
- Miglani, S.; Aggarwal, V.; Ahuja, B. Dentin hypersensitivity: Recent trends in management. J. Conserv. Dent. 2010, 13, 218–224. [Google Scholar] [CrossRef] [PubMed]
- Attin, T.; Vollmer, D.; Wiegand, A.; Attin, R.; Betke, H. Subsurface microhardness of enamel and dentin after different external bleaching procedures. Am. J. Dent. 2005, 18, 8–12. [Google Scholar] [PubMed]
- Zalkind, M.; Arwaz, J.R.; Goldman, A.; Rotstein, I. Surface morphology changes in human enamel, dentin and cementum following bleaching: A scanning electron microscopy study. Dent. Traumatol. 1996, 12, 82–88. [Google Scholar] [CrossRef]
- Pimenta-Dutra, A.C.; Albuquerque, R.C.; Morgan, L.S.; Pereira, G.M.; Nunes, E.; Horta, M.C.; Silveira, F.F. Effect of bleaching agents on enamel surface of bovine teeth: A sem study. J. Clin. Exp. Dent. 2017, 9, e46–e50. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, G.M.; Ritter, A.V.; Heymann, H.O.; Swift, E., Jr.; Donovan, T.; Brock, G.; Wright, T. Remineralization effect of cpp-acp and fluoride for white spot lesions in vitro. J. Dent. 2014, 42, 1592–1602. [Google Scholar] [CrossRef] [PubMed]
- Pliska, B.T.; Warner, G.A.; Tantbirojn, D.; Larson, B.E. Treatment of white spot lesions with acp paste and microabrasion. Angle Orthod. 2012, 82, 765–769. [Google Scholar] [CrossRef] [PubMed]
- Tao, S.; Zhu, Y.; Yuan, H.; Tao, S.; Cheng, Y.; Li, J.; He, L. Efficacy of fluorides and cpp-acp vs fluorides monotherapy on early caries lesions: A systematic review and meta-analysis. PLoS ONE 2018, 13, e0196660. [Google Scholar] [CrossRef] [PubMed]
- Martin, J.; Fernandez, E.; Bahamondes, V.; Werner, A.; Elphick, K.; Oliveira, O.B., Jr.; Moncada, G. Dentin hypersensitivity after teeth bleaching with in-office systems. Randomized clinical trial. Am. J. Dent. 2013, 26, 10–14. [Google Scholar] [PubMed]
- Alqahtani, M.Q. Tooth-bleaching procedures and their controversial effects: A literature review. Saudi Dent. J. 2014, 26, 33–46. [Google Scholar] [CrossRef] [PubMed]
- Gabardo, M.C.; Moyses, S.J.; Moyses, S.T.; Olandoski, M.; Olinto, M.T.; Pattussi, M.P. Social, economic, and behavioral variables associated with oral health-related quality of life among brazilian adults. Cienc. Saude Colet. 2015, 20, 1531–1540. [Google Scholar] [CrossRef] [PubMed]
- Bruzell, E.M.; Pallesen, U.; Thoresen, N.R.; Wallman, C.; Dahl, J.E. Side effects of external tooth bleaching: A multi-centre practice-based prospective study. Br. Dent. J. 2013, 215, E17. [Google Scholar] [CrossRef] [PubMed]
- Carey, C.M. Tooth whitening: What we now know. J. Evid. Based Dent. Pract. 2014, 14, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Walsh, L.J. Safety issues relating to the use of hydrogen peroxide in dentistry. Aust. Dent. J. 2000, 45, 257–269. [Google Scholar] [CrossRef] [PubMed]
- de Geus, J.L.; Wambier, L.M.; Kossatz, S.; Loguercio, A.D.; Reis, A. At-home vs in-office bleaching: A systematic review and meta-analysis. Oper. Dent. 2016, 41, 341–356. [Google Scholar] [CrossRef] [PubMed]
- Bruno, M.; Taddeo, F.; Medeiros, I.S.; Boaro, L.C.; Moreira, M.S.; Marques, M.M.; Calheiros, F.C. Relationship between toothpastes properties and patient-reported discomfort: Crossover study. Clin. Oral Investig. 2016, 20, 485–494. [Google Scholar] [CrossRef] [PubMed]

© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Oldoini, G.; Bruno, A.; Genovesi, A.M.; Parisi, L. Effects of Amorphous Calcium Phosphate Administration on Dental Sensitivity during In-Office and At-Home Interventions. Dent. J. 2018, 6, 52. https://doi.org/10.3390/dj6040052
Oldoini G, Bruno A, Genovesi AM, Parisi L. Effects of Amorphous Calcium Phosphate Administration on Dental Sensitivity during In-Office and At-Home Interventions. Dentistry Journal. 2018; 6(4):52. https://doi.org/10.3390/dj6040052
Chicago/Turabian StyleOldoini, Giacomo, Antonino Bruno, Anna Maria Genovesi, and Luca Parisi. 2018. "Effects of Amorphous Calcium Phosphate Administration on Dental Sensitivity during In-Office and At-Home Interventions" Dentistry Journal 6, no. 4: 52. https://doi.org/10.3390/dj6040052
APA StyleOldoini, G., Bruno, A., Genovesi, A. M., & Parisi, L. (2018). Effects of Amorphous Calcium Phosphate Administration on Dental Sensitivity during In-Office and At-Home Interventions. Dentistry Journal, 6(4), 52. https://doi.org/10.3390/dj6040052




