Qualitative Enhancement of the Tooth–Filling Interface Using Cold Atmospheric Plasma
Abstract
1. Introduction
2. Material and Methods
2.1. CAP Source
2.2. Plasma Treatment Parameters
2.3. Cavities
2.4. Treatment of Cavities and Group Disposition
2.5. Preparation for Examination
2.6. Statistical Analysis
3. Results
3.1. Dye Penetration
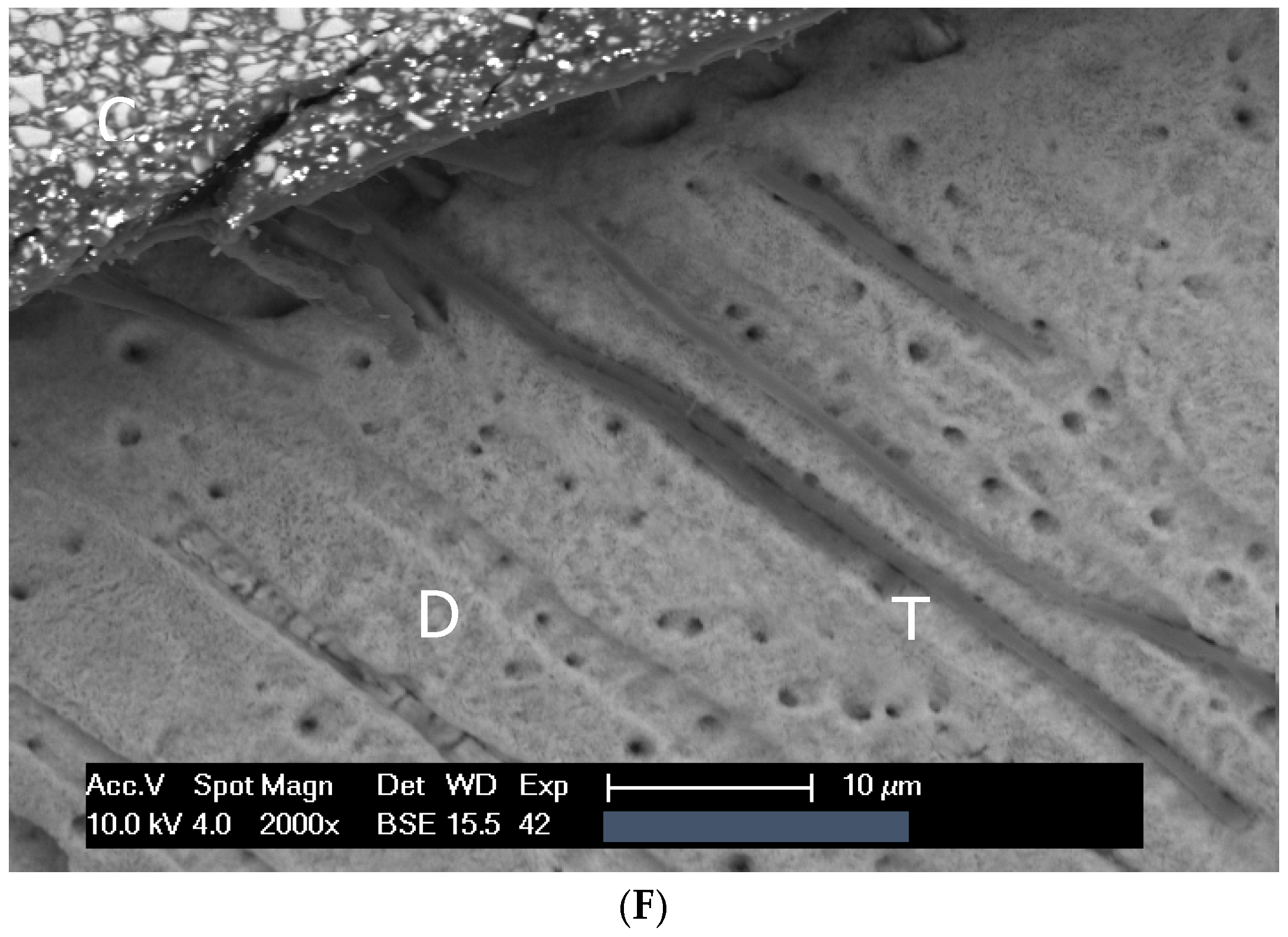
3.2. Scanning Electron Microscopic Analysis
3.2.1. Overview
3.2.2. Aging of Fillings
3.2.3. Hybrid Layer
3.2.4. Adhesive Tags
4. Discussion
5. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Stasic, J.N.; Pficer, J.K.; Milicic, B.; Puač, N.; Miletic, V. Effects of non-thermal atmospheric plasma on dentin wetting and adhesive bonding efficiency: Systematic review and meta-analysis. J. Dent. 2021, 112, 103765. [Google Scholar] [CrossRef]
- Mazzoni, A.; Scaffa, P.; Carrilho, M.; Tjäderhane, L.; Di Lenarda, R.; Polimeni, A.; Tezvergil-Mutluay, A.; Tay, F.R.; Pashley, D.H.; Breschi, M. Effects of etch-and-rinse and self-etch adhesives on dentin MMP-2 and MMP-9. J. Dent. Res. 2013, 92, 82–86. [Google Scholar] [CrossRef] [PubMed]
- Santini, A.; Miletic, V. Quantitative micro-Raman assessment of dentine demineralization, adhesive penetration, and degree of conversion of three dentine bonding systems. Eur. J. Oral Sci. 2008, 116, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Duarte, S.; Panariello, B.H.D. Comprehensive biomedical applications of low temperature plasmas. Arch. Biochem. Biophys. 2020, 693, 108560. [Google Scholar] [CrossRef] [PubMed]
- Hirata, R.; Sampaio, C.; Machado, L.S.; Coelho, P.G.; Thompson, V.P.; Duarte, S.; Almeida Ayres, A.P.; Giannini, M. Short-and Long-term Evaluation of Dentin-Resin Interfaces Formed by Etch-and-Rinse Adhesives on Plasma-treated Dentin. J. Adhes. Dent. 2016, 18, 215–222. [Google Scholar] [CrossRef]
- Ritts, A.C.; Li, H.; Yu, Q.; Xu, C.; Yao, X.; Hong, L.; Wang, Y. Dentin surface treatment using a non-thermal argon plasma brush for interfacial bonding improvement in composite restoration. Eur. J. Oral Sci. 2010, 118, 510–516. [Google Scholar] [CrossRef]
- Ayres, A.; Freitas, P.; De Munck, J.; Vananroye, A.; Clasen, C.; dos Santos Dias, C.T.; Giannini, M.; Van Meerbeek, B. Benefits of nonthermal atmospheric plasma treatment on dentin adhesion. Oper. Dent. 2018, 43, E288–E299. [Google Scholar] [CrossRef]
- Ayres, A.P.; Bonvent, J.J.; Mogilevych, B.; Soares, L.E.S.; Martin, A.A.; Ambrosano, G.M.; Nascimento, F.D.; Van Meerbeek, B.; Giannini, M. Effect of non-thermal atmospheric plasma on the dentin-surface topography and composition and on the bond strength of a universal adhesive. Eur. J. Oral Sci. 2018, 126, 53–65. [Google Scholar] [CrossRef]
- Wang, D.Y.; Wang, P.; Xie, N.; Yan, X.Z.; Xu, W.; Wang, L.M.; Liu, N.; Wang, Y.; Ding, P. In vitro study on non-thermal argon plasma in improving the bonding efficacy between dentin and self-etch adhesive systems. Dent. Mater. J. 2022, 41, 595–600. [Google Scholar] [CrossRef]
- Chen, M.; Zhang, Y.; Dusevich, V.; Liu, Y.; Yu, Q.; Wang, Y. Non-thermal atmospheric plasma brush induces HEMA grafting onto dentin collagen. Dent. Mater. 2014, 30, 1369–1377. [Google Scholar] [CrossRef]
- Kim, D.S.; Ahn, J.J.; Kim, G.C.; Jeong, C.M.; Huh, J.B.; Lee, S.H. Influence of non-thermal atmospheric pressure plasma treatment on retentive strength between zirconia crown and titanium implant abutment. Materials 2021, 14, 2352. [Google Scholar] [CrossRef]
- Kim, D.S.; Ahn, J.J.; Bae, E.B.; Kim, G.C.; Jeong, C.M.; Huh, J.B.; Lee, S.H. Influence of non-thermal atmospheric pressure plasma treatment on shear bond strength between Y-TZP and self-adhesive resin cement. Materials 2019, 12, 3321. [Google Scholar] [CrossRef]
- Da Veiga, A.M.A.; Cunha, A.C.; Ferreira, D.M.T.P.; Da Silva Fidalgo, T.K.; Chianca, T.K.; Reis, K.R.; Maia, L.C. Longevity of direct and indirect resin composite restorations in permanent posterior teeth: A systematic review and meta-analysis. J. Dent. 2016, 54, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Lehmann, A.; Pietag, F.; Arnold, T. Human health risk evaluation of a microwave-driven atmospheric plasma jet as medical device. Clin. Plasma Med. 2017, 7–8, 16–23. [Google Scholar] [CrossRef]
- Jablonowski, L.; Kocher, T.; Schindler, A.; Müller, K.; Dombrowski, F.; Von Woedtke, T.; Arnold, T.; Lehmann, A.; Rupf, S.; Evert, M.; et al. Side effects by oral application of atmospheric pressure plasma on the mucosa in mice. PLoS ONE 2019, 14, e0215099. [Google Scholar] [CrossRef]
- Han, G.; Kim, J.; Cho, B.; Hwang, Y.; Kim, H. Improved resin-to-dentin bond strength and durability via non-thermal atmospheric pressure plasma drying of etched dentin. Eur. J. Oral Sci. 2019, 127, 170–178. [Google Scholar] [CrossRef]
- Zhu, X.M.; Zhou, J.F.; Guo, H.; Zhang, X.F.; Liu, X.Q.; Li, H.P.; Tan, J.G. Effects of a modified cold atmospheric plasma jet treatment on resin-dentin bonding. Dent. Mater. J. 2018, 37, 798–804. [Google Scholar] [CrossRef]
- Abreu, J.L.B.D.; Prado, M.; Simão, R.A.; Silva, E.M.D.; Dias, K.R.H.C. Effect of non-thermal argon plasma on bond strength of a self-etch adhesive system to NaOCl-treated dentin. Braz. Dent. J. 2016, 27, 446–451. [Google Scholar] [CrossRef]
- Chen, M.; Zhang, Y.; Sky Driver, M.; Caruso, A.N.; Yu, Q.; Wang, Y. Surface modification of several dental substrates by non-thermal, atmospheric plasma brush. Dent. Mater. 2013, 29, 871–880. [Google Scholar] [CrossRef]
- Dong, X.; Ritts, A.C.; Staller, C.; Yu, Q.; Chen, M.; Wang, Y. Evaluation of plasma treatment effects on improving adhesive-dentin bonding by using the same tooth controls and varying cross-sectional surface areas. Eur. J. Oral Sci. 2013, 121, 355–362. [Google Scholar] [CrossRef]
- Imiolczyk, S.M.; Hertel, M.; Hase, I.; Paris, S.; Blunck, U.; Hartwig, S.; Preissner, S. The Influence of Cold Atmospheric Plasma Irradiation on the Adhesive Bond Strength in Non-Demineralized and Demineralized Human Dentin: An In Vitro Study. Open Dent. J. 2018, 12, 960–968. [Google Scholar] [CrossRef]
- Han, G.J.; Kim, J.H.; Chung, S.N.; Chun, B.H.; Kim, C.K.; Seo, D.G.; Son, H.H.; Cho, B.H. Effects of non-thermal atmospheric pressure pulsed plasma on the adhesion and durability of resin composite to dentin. Eur. J. Oral Sci. 2014, 122, 417–423. [Google Scholar] [CrossRef] [PubMed]
- Ayres, A.P.A.; Pongprueksa, P.; De Munck, J.; Gré, C.P.; Nascimento, F.D.; Giannini, M.; Van Meerbeek, B. Mini-interfacial fracture toughness of a multimode adhesive bonded to plasma-treated dentin. J. Adhes. Dent. 2017, 19, 409–416. [Google Scholar] [CrossRef]
- Stasic, J.N.; Selaković, N.; Puač, N.; Miletić, M.; Malović, G.; Petrović, Z.L.; Veljovic, D.N.; Miletic, V. Effects of non-thermal atmospheric plasma treatment on dentin wetting and surface free energy for application of universal adhesives. Clin. Oral Investig. 2019, 23, 1383–1396. [Google Scholar] [CrossRef] [PubMed]
- Dong, X.; Chen, M.; Wang, Y.; Yu, Q. A mechanistic study of plasma treatment effects on demineralized dentin surfaces for improved adhesive/dentin interface bonding. Clin. Plasma Med. 2014, 2, 11–16. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Dong, X.; Li, H.; Chen, M.; Wang, Y.; Yu, Q. Plasma treatment of dentin surfaces for improving self-etching adhesive/dentin interface bonding. Clin. Plasma Med. 2015, 3, 10–16. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Han, G.J.; Kim, C.K.; Oh, K.H.; Chung, S.N.; Chun, B.H. Promotion of adhesive penetration and resin bond strength to dentin using non-thermal atmospheric pressure plasma. Eur. J. Oral Sci. 2016, 124, 89–95. [Google Scholar] [CrossRef]
- Temel, U.B.; Kam Hepdeniz, O.; Gulec, A. Evaluation of the bonding effectiveness of a universal adhesive to the plasma-activated dentin surface. Eur. J. Oral Sci. 2023, 131, e12914. [Google Scholar] [CrossRef]




| Groups | Conditioning (Phosphoric Acid) | Plasma Treatment | Filling | Thermo-Mechanical Loading |
|---|---|---|---|---|
| G1: E-F | Enamel 30 s Dentin 10 s, Water spray 15 s | Non | Optibond FL/Herculite XRV | non |
| G2: E-F-TB | Enamel 30 s Dentin 10 s, Water spray 15 s | Non | 3 × (1000 cycles of thermal load and 100,000 cycles mechanical stressing) | |
| G3: E-P3W-F-TB | Enamel 30 s Dentin 10 s, Water spray 15 s | 3 W, 1.8 s/mm2, 40 °C | ||
| G4: E-P1.5W-F-TB | Enamel 30 s Dentin 10 s, Water spray 15 s | 1.5 W, 1.8 s/mm2, 40 °C | ||
| G5: P3W-E-F-TB | Enamel 30 s Dentin 10 s, Water spray 15 s | 3 W, 1.8 s/mm2, 40 °C | ||
| G6: P3W-F-TB | Non | 3 W, 1.8 s/mm2, 40 °C |
| Score 0 | No dye penetration |
| Score 1 | Dye penetration limited to enamel |
| Score 2 | Dye penetration beyond the dentino-enamel junction but limited to 2/3rds of the cervical wall length |
| Score 3 | Dye penetration beyond 2/3rds of the cervical wall length but not to the pulpal wall |
| Score 4 | Dye penetration to the pulpal wall |
| Group | Hybrid Layer | Dye Penetration, % Score 0 | Average Dye Penetration Score | Average Thickness Hybrid Layer | Average Intratubular Adhesive Penetration | Lateral Branches (%) |
|---|---|---|---|---|---|---|
| G1: E-F | 100% | 75% | 0.875 | 2.66 µm | 36.16 µm | 37.5% |
| G2: E-F-TB | 100% | 44% | 1.125 | 2.41 µm | 31.73 µm | 37.5% |
| G3: E-P3W-F-TB | 100% | 13% | 3.125 | 3.1 µm * | 60.27 µm * | 87.5% |
| G4: E-P1.5W-F-TB | 100% | 81% | 0.5 | 3.94 µm * | 74.44 µm * | 87.5% |
| G5: P3W-E-F-TB | 100% | 44% | 1.125 | 3.11 µm * | 55.83 µm * | 75% |
| G6: P3W-F-TB | 100% | 6% | 2.875 | 1.83 µm | 25.21 µm | 25% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gund, M.P.; Naim, J.; al Muhammad, M.; Lehmann, A.; Schindler, A.; Hannig, M.; Rupf, S. Qualitative Enhancement of the Tooth–Filling Interface Using Cold Atmospheric Plasma. Dent. J. 2025, 13, 406. https://doi.org/10.3390/dj13090406
Gund MP, Naim J, al Muhammad M, Lehmann A, Schindler A, Hannig M, Rupf S. Qualitative Enhancement of the Tooth–Filling Interface Using Cold Atmospheric Plasma. Dentistry Journal. 2025; 13(9):406. https://doi.org/10.3390/dj13090406
Chicago/Turabian StyleGund, Madline Priska, Jusef Naim, Muhammad al Muhammad, Antje Lehmann, Axel Schindler, Matthias Hannig, and Stefan Rupf. 2025. "Qualitative Enhancement of the Tooth–Filling Interface Using Cold Atmospheric Plasma" Dentistry Journal 13, no. 9: 406. https://doi.org/10.3390/dj13090406
APA StyleGund, M. P., Naim, J., al Muhammad, M., Lehmann, A., Schindler, A., Hannig, M., & Rupf, S. (2025). Qualitative Enhancement of the Tooth–Filling Interface Using Cold Atmospheric Plasma. Dentistry Journal, 13(9), 406. https://doi.org/10.3390/dj13090406







