Abstract
Background/Objectives: Preventive oral health education plays a key role in preparing future healthcare professionals to promote and maintain good oral hygiene. Individually Trained Oral Prophylaxis (iTOP) is a structured, personalized educational program that emphasizes correct brushing techniques and interdental cleaning. This study aimed to evaluate the long-term effectiveness of a single-session iTOP intervention on clinical oral health outcomes among medical and dental students. Methods: A 2-year prospective cohort study included 82 first- and fourth-year medical and dental students at the University of Mostar, Bosnia and Herzegovina. The researchers randomly assigned participants to an iTOP intervention group or a control group. The primary analysis used multivariable linear mixed-effects models for repeated measures, adjusted for study program, academic year, smoking status, and baseline oral-hygiene habits, with effect sizes reported alongside 95% confidence intervals. Clinical periodontal parameters—plaque index, bleeding on probing, and probing depth—were assessed at baseline, three months, and two years. All participants received professional cleaning and oral hygiene kits. Only the intervention group received personalized iTOP training, consisting of a single session with brief reinforcement at the 3-month follow-up. This study was registered at ClinicalTrials.gov (NCT07085013). Results: Seventy-six students completed the follow-up. The iTOP group had significantly lower plaque index and bleeding scores at both follow-up points (p < 0.001) compared to the control group. Baseline differences were observed between subgroups (medical vs. dental; younger vs. older students), but these diminished over time. At the 2-year follow-up, only the plaque index remained significantly improved, while other clinical parameters returned to values comparable to baseline. Conclusions: The iTOP program resulted in significant short-term improvements in oral health among medical and dental students. For sustained long-term outcomes, iTOP or similar structured oral health education programs should be integrated into medical and dental curricula. Enhancing oral health awareness among healthcare providers may ultimately contribute to improved public oral health outcomes. Given the single-center design and the single-session nature of the intervention, the results should be interpreted with caution.
1. Introduction
Oral health is an essential component of general health and quality of life, affecting both physical and psychosocial well-being. In recent decades, dentistry has shifted its focus from treatment of oral diseases to prevention. Proper oral hygiene is now recognized as a key preventive measure against common conditions such as dental caries and periodontitis.
Individually Trained Oral Prophylaxis (iTOP) is a personalized approach that promotes oral hygiene through one-on-one instruction and motivation. Although general oral health education shows some efficacy, the long-term benefits of individualized interventions such as iTOP remain insufficiently explored. Some studies suggest that improvements may diminish without continuous reinforcement, while others report sustained positive outcomes after personalized training [1,2,3]. Similar findings have been reported in various populations, including hospitalized elderly patients, suggesting broader applicability [4]. This inconsistency highlights the need for further research, especially among medical and dental students, who often differ in baseline knowledge and oral health behaviors [5]. A study conducted among dental students at the University of Zagreb showed that although oral health knowledge improves with academic progression, oral hygiene behaviors may not follow the same trend, highlighting the importance of sustained motivation and self-care training throughout the curriculum [6]. In addition, a study among adolescents in Bosnia and Herzegovina found significant sex-based differences in oral health behaviors and perceptions, yet found no correlation with socioeconomic status, underscoring the complexity of behavioral factors that influence oral health [7].
Oral health has also been linked to systemic conditions such as cardiovascular and metabolic diseases, further emphasizing the importance of prevention [8].
Despite advances in dental care, the global burden of caries and periodontitis remains high and highlights the need for effective, sustainable educational strategies [9,10]. Medical and dental students are an important target group for oral health promotion, as they represent future healthcare professionals. However, studies have shown that even medical and dental students often exhibit suboptimal hygiene habits and inconsistent oral health behaviors, indicating a persistent gap between knowledge and practice [5,6,11,12,13,14]. This paradox makes them a particularly relevant population for evaluating the effectiveness of structured interventions such as iTOP.
Considerable variability in oral health knowledge, attitudes, and behaviors has been consistently observed among university students. Research from Split, Croatia, conducted among non-healthcare students, highlighted gaps in oral hygiene awareness and practice [11]. A study from Saudi Arabia involving both healthcare and non-healthcare students identified significant disparities in oral health behaviors [12]. The link between oral and mental health has received increasing attention, with cross-sectional studies from Serbia and South Korea reporting associations between stress, self-perceived oral health, and oral symptoms among university student populations [13,14]. These insights advocate for a more holistic and psychologically informed approach to oral health education.
Therefore, this study aimed to evaluate the long-term effectiveness of a single-session iTOP intervention among medical and dental students by assessing clinical periodontal parameters over a 2-year period. Understanding these effects may help guide how structured oral health education is integrated into medical and dental curricula.
Recent systematic reviews in adult populations have shown that educational and behavioral interventions can significantly improve periodontal health. One review focusing on periodontitis patients reported that tailored oral hygiene strategies—including psychological and personalized instruction—enhanced plaque control and gingival outcomes, although heterogeneity prevented a quantitative synthesis [15]. Another systematic review targeting older adults (aged 60+) and their caregivers identified that health education programs led to measurable improvements in oral hygiene and related clinical parameters [16]. These findings underscore the relevance of individualized, single-session instruction and the need to evaluate its long-term clinical impact in adult student cohorts.
2. Materials and Methods
2.1. Study Design and Participants
This was a prospective cohort study with random allocation of participants to intervention and control groups, constituting a quasi-experimental design. This study followed STROBE guidelines for observational studies and incorporated relevant CONSORT elements in reporting randomization. It was conducted at the University of Mostar School of Medicine (Bosnia and Herzegovina) over two academic years, from the 2021/2022 to the 2023/2024 academic year. This study was registered at ClinicalTrials.gov (NCT07085013). The sample included all eligible first- and fourth-year medical and dental students enrolled in 2021/2022 (n = 82), who were followed until their third and sixth years, respectively. A total of 76 participants completed all three assessments (baseline, 3 months, and 2 years). Although a formal a priori power analysis was not conducted, we included the entire accessible population. A post hoc power analysis based on the observed effect sizes indicated that the available sample size provided sufficient statistical power (>0.80) to detect moderate-to-large differences in periodontal parameters over time. Previous studies with similar designs and sample sizes also reported adequate sensitivity to detect clinically relevant changes [1,17,18]. Medical and dental students were selected because of their dual role as learners and future healthcare professionals, whose oral hygiene behaviors carry broader public health implications. This makes them a relevant population for evaluating the impact of structured educational interventions.
This study adhered to the Declaration of Helsinki and was approved by the Ethics Committee of the University of Mostar School of Medicine (the Approval Nos. 01-I-1827/21 and 01-I-911/24). All participants provided written informed consent prior to enrollment.
2.2. Inclusion and Exclusion Criteria
Inclusion criteria were active enrollment in the first and fourth years (2021/2022) or third and sixth years (2023/2024), as confirmed by Faculty Administration records. All participants also provided written informed consent.
Exclusion criteria were lack of informed consent and the presence of systemic conditions known to affect periodontal health, such as uncontrolled diabetes or immunodeficiencies. Additionally, individuals taking medications known to cause gingival overgrowth, including anticonvulsants, calcium channel blockers, or immunosuppressants, were excluded from this study.
2.3. Group Allocation and Interventions
Participants were randomly assigned using a computer-generated sequence (Random.org) to either an intervention group (iTOP training) or a control group. The researchers concealed the allocation sequence from the examiners conducting the clinical assessments to minimize potential selection bias. All clinical examinations were jointly conducted by two examiners: a board-certified specialist in periodontology with more than ten years of clinical experience, and a teaching assistant at the Department of Periodontology, University of Mostar. By working together throughout all assessments, the examiners ensured consistent data collection and diagnostic accuracy. Prior to data collection, both examiners reviewed the study protocol and underwent calibration sessions to align clinical measurement techniques.
2.4. Study Procedures
Assessments Were Conducted at Three Time Points
Baseline (2021/2022): At the first visit, participants completed a general health and oral health questionnaire and underwent a full periodontal examination. The questionnaire included items on general health, smoking status, and detailed oral hygiene habits such as brushing frequency, use of interdental brushes, and dental floss. Smoking status was also recorded again at the 2-year follow-up; however, in the primary LMM analyses, only the baseline smoking status was used as the covariate. Examiners recorded clinical parameters including plaque levels, bleeding on probing, pocket depth, and average attachment level. They were blinded to participants’ academic program (medical or dental) and intervention allocation (iTOP or control) to reduce potential assessment bias. Although the same examiners assessed participants at all three time points, they were not explicitly informed which visits represented follow-up assessments; however, given the repeated participation of the same students, complete blinding to the time point could not be guaranteed. The clinical team took periodontal measurements at six sites per tooth using the UNC-15 probe (Carl Martin AG, Solingen, Germany) and recorded them using the Bern Periodontal Chart. Clinical attachment level was measured in millimeters relative to the cementoenamel junction (CEJ). Negative values indicated that the gingival margin was located coronally to the CEJ, reflecting absence of clinical attachment loss. Bleeding on probing (BOP) was assessed at six sites per tooth (distobuccal, midbuccal, mesiobuccal, distolingual/palatal, midlingual/palatal, and mesiolingual/palatal) using a UNC-15 probe. A site was scored as positive if bleeding occurred within 30 s of gentle probing. BOP was expressed as the percentage of positive sites out of the total number of sites examined. Plaque levels were disclosed using the PCA 222 plaque indicator (Curaden AG, Kriens, Switzerland). After clinical examination, all participants underwent professional dental cleaning with the SonicFlex scaler and the KaVo ProphyFlex 4 air polisher (KaVo, Biberach, Germany). The study team provided a standardized oral hygiene kit (Curaprox toothbrush and interdental brushes; Curaden AG, Kriens, Switzerland) to all participants. After the baseline examination, participants in the iTOP group attended small-group sessions led by a licensed dental professional certified in the iTOP protocol. The iTOP training included instruction in the Modified Bass toothbrushing technique using a manual toothbrush and the “touch-to-teach” method for optimal brush positioning. Participants practiced plaque removal using a manual toothbrush, single-tuft brush, interdental brushes, and dental floss under direct supervision. Disclosing agents were applied to visualize plaque deposits and guide personalized feedback. The baseline iTOP session lasted approximately 45 min and was conducted in small groups of 10 students. Adherence to oral hygiene recommendations was not systematically monitored during follow-up.
Second Examination (Follow-up at 3 Months): Periodontal parameters were re-evaluated following the same clinical protocol as in the baseline visit. Compliance at this visit was complete (100%). As in the initial examination, all participants received a standardized oral hygiene kit (Curaprox toothbrush and interdental brushes; Curaden AG, Kriens, Switzerland). Those in the iTOP group received a brief (approximately 10 min) motivational reinforcement session.
Third Examination (Long-Term Follow-up after Two Years; 2023/2024): Seventy-six participants (92.7% of the initial sample) returned for the final assessment, during which examiners measured periodontal parameters using the same protocol as at baseline. Professional cleaning was repeated, and all participants received a new standardized oral hygiene kit.
2.5. Statistical Analysis
We assessed the distribution of all outcomes—average probing depth (APD, mm), average attachment level (AAL, mm), plaque index (%), and bleeding on probing (BOP, %)—using histograms, Q–Q plots, and the Shapiro–Wilk test, and verified homoscedasticity via residual vs. fitted plots. Because plaque and BOP are bounded percentages, they were analyzed on the logit scale after scaling to proportions with a 0.5 continuity correction, whereas APD and AAL were modeled on the raw scale.
Primary analyses were performed using linear mixed-effects models (random intercept for participant) to account for repeated measures (baseline, 3 months, 2 years). Fixed effects included Group (iTOP vs. control), Time, and their interaction (Group × Time). Models were adjusted for study program, academic year, smoking status, and baseline oral-hygiene habits. For plaque and BOP, model estimates were back-transformed to percentage points for interpretation.
We report adjusted marginal means with 95% confidence intervals (CIs), between-group differences at follow-up, and omnibus Group × Time tests. Sensitivity analyses included unadjusted models and non-parametric comparisons. Model assumptions were checked by residual diagnostics. Estimation used restricted maximum likelihood (REML) with Satterthwaite approximation for degrees of freedom. Missing data were handled under the missing-at-random assumption. All tests were two-sided with α = 0.05. Analyses were conducted in SPSS v26 (MIXED procedure) and cross-checked in R (lme4/emmeans).
Effect sizes (Cohen’s d with 95% CI) were calculated for the main between-group differences. A post hoc power analysis, based on observed effect sizes and actual sample sizes, is reported in the Section 2.6.
2.6. Post Hoc Power Analysis
No a priori sample size calculation was performed, as this study included the entire eligible student population. Post hoc power analyses were conducted for all primary outcomes (plaque index, bleeding on probing, APD, AAL) at each time point, based on observed effect sizes (Cohen’s d) and actual sample sizes. These analyses, presented in Appendix A Table A1, Table A2 and Table A3, suggest that this study had adequate statistical power (≥0.80) to detect moderate-to-large differences in plaque index and bleeding on probing. Given the limitations of post hoc power analysis, these results should be interpreted cautiously.
3. Results
3.1. Differences Between Medical and Dental Students over Time
Table 1 shows differences in clinical periodontal parameters between dental and medical students at all three time points. At baseline, medical students had significantly higher probing depth and average attachment level values than dental students (p < 0.05). No significant differences were observed between groups for the other clinical parameters. At the 2-year follow-up, these differences were no longer present for any parameter.

Table 1.
Differences in periodontal parameters between medical and dental students at all three time points.
3.2. Differences Between Junior and Senior Students over Time
Table 2 shows differences in clinical parameters between younger (first-/fourth-year) and older (third-/sixth-year) students. At baseline, younger students had significantly higher plaque index values than older students (p < 0.05). No significant differences were observed between groups for other periodontal parameters at any time point. Differences between academic levels decreased over time.

Table 2.
Differences between younger and older students in periodontal parameters at all three time points.
3.3. Intra-Group Changes over Time in the iTOP and Control Groups
Table 3 shows intra-group comparisons of periodontal parameters for the iTOP and non-iTOP groups at baseline, 3-month, and 2-year follow-ups. At the 3-month follow-up, the iTOP group showed significant reductions in probing depth, average attachment level, plaque index, and bleeding on probing compared with baseline (p < 0.001). In the control group, significant reductions were observed in probing depth, attachment level, and plaque index, whereas changes in bleeding on probing were not statistically significant. At the 2-year follow-up, the iTOP group maintained significantly lower plaque scores compared to both prior time points. However, probing depth, attachment level, and bleeding on probing increased, returning to values similar to baseline.

Table 3.
Intra-group comparisons of periodontal parameters in iTOP and non-iTOP groups at baseline, 3-month, and 2-year follow-ups.
In contrast, the non-iTOP group showed deterioration in periodontal status at the 2-year follow-up, with significantly higher probing depth, attachment level, and bleeding on probing compared with both baseline and 3-month values. Despite this, plaque scores remained significantly lower than at baseline.
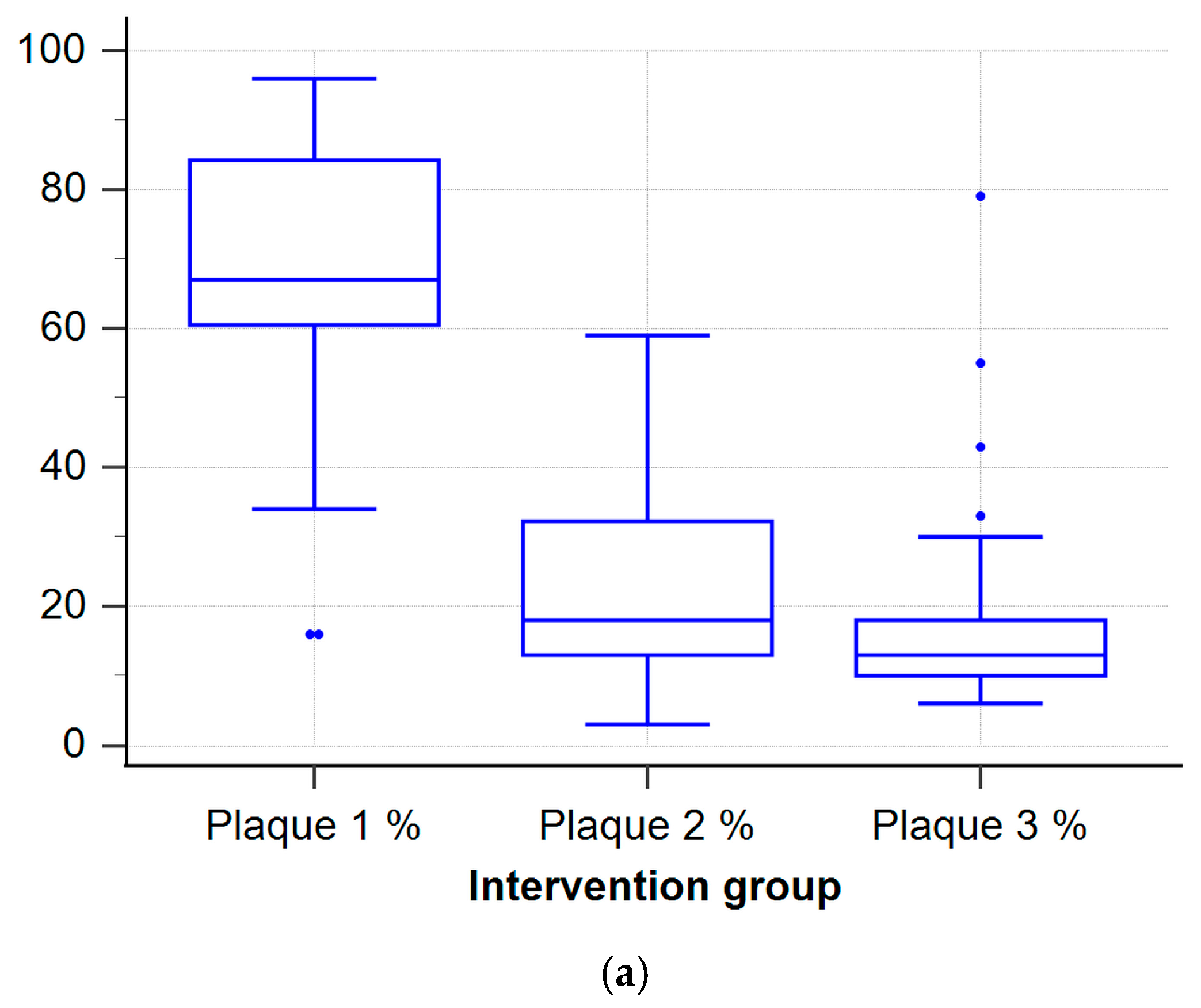
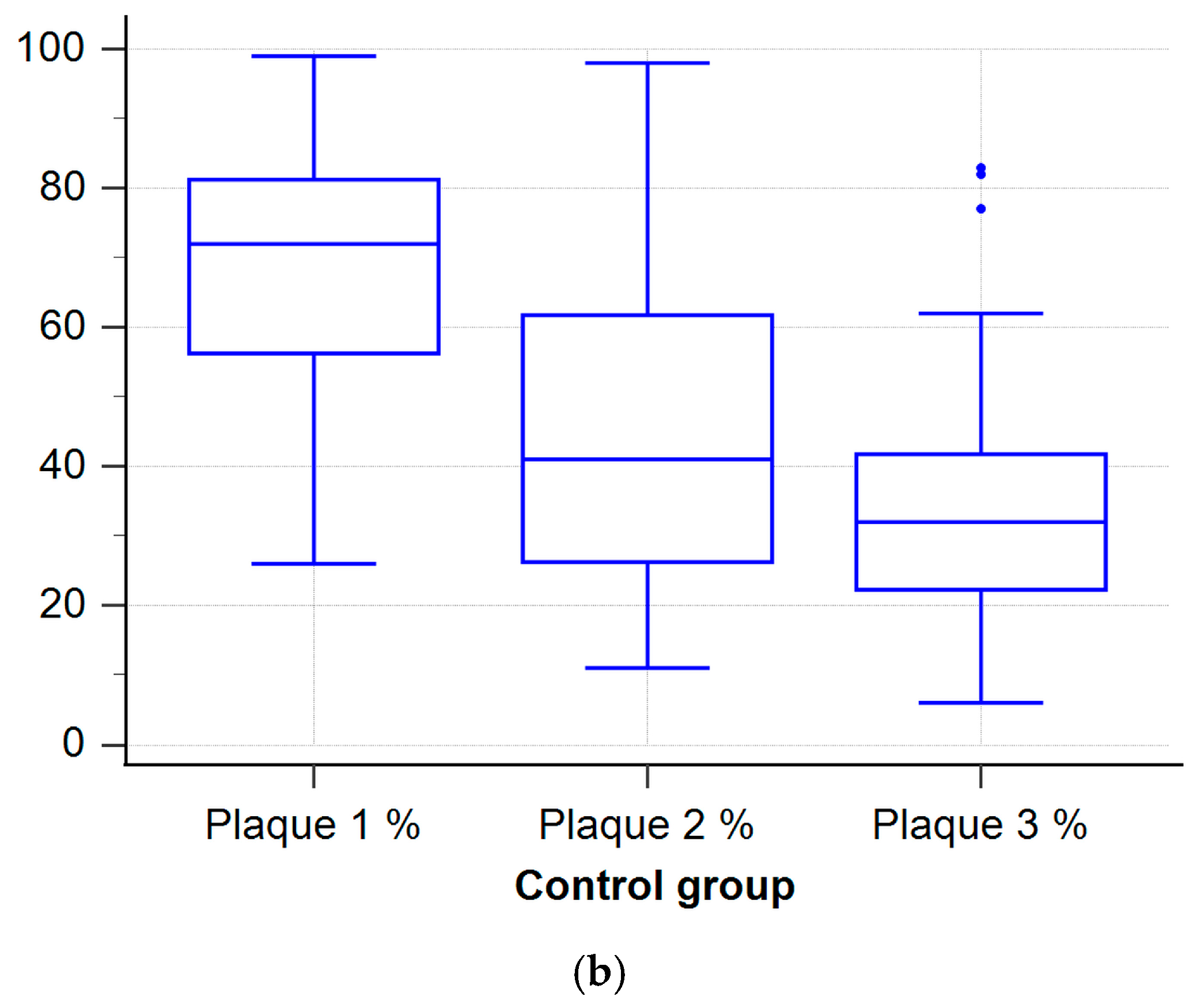
Changes in plaque index over three time points were analyzed in both the intervention group (iTOP) and the control group (non-iTOP). Results are shown in box plots (Figure 1a,b) illustrating the distribution, median, interquartile range, and outliers for each group across all time points. In the iTOP group, plaque index significantly decreased from baseline to the 2-year follow-up. In contrast, the non-iTOP group showed a smaller and more variable reduction in plaque index, with values remaining higher than in the iTOP group across all time points.
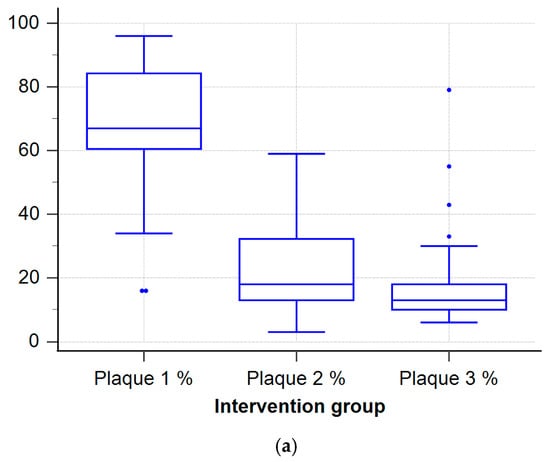
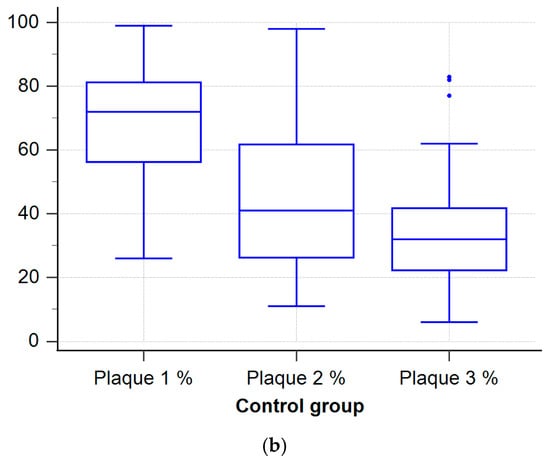
Figure 1.
Box-and-whisker plots of plaque index at baseline (Plaque 1), 3-month (Plaque 2) and 2-year (Plaque 3) follow-ups for (a) iTOP group and (b) non-iTOP group. Boxes show the interquartile range (25th–75th percentile); the horizontal line inside each box is the median; whiskers extend to the most extreme values within 1.5 × IQR. Mean values are shown as blue squares, while outliers are shown as blue dots. Blue color is used only for styling and carries no additional meaning.
3.4. Inter-Group Comparisons Between iTOP and Control Groups
Table 4 shows between-group comparisons of periodontal parameters at baseline, 3 months, and 2 years. At both the 3-month and 2-year follow-ups, the control group had significantly higher plaque index and bleeding on probing values (p < 0.001). No significant between-group differences were found for probing depth or average attachment level at any time point.

Table 4.
Comparison of clinical parameters between the iTOP and non-iTOP groups at each time point.
3.5. Primary Adjusted Analysis
Table 5 shows the results of mixed-effects models adjusted for academic program, academic year, smoking, and baseline oral hygiene habits, where the iTOP group had significantly lower plaque at both 3 months and 2 years compared with controls. At 3 months, the adjusted mean difference was −22.26 percentage points (95% CI: −32.15 to −12.90; p < 0.001), and at 2 years it was −15.40 percentage points (95% CI: −24.21 to −7.41; p < 0.001). At the 2-year follow-up, the between-group difference in plaque index corresponded to a large effect size (Cohen’s d = 1.05, 95% CI: 0.63–1.47). A post hoc power analysis indicated that this study had sufficient statistical power (1 − β = 0.995) to detect this difference.

Table 5.
Adjusted mixed-model results.
BOP was also significantly lower in the iTOP group (T2: Δ = −2.70 pp, 95% CI: −4.57 to −1.05; p = 0.001; T3: Δ = −5.65 pp, 95% CI: −9.13 to −2.50; p < 0.001).
For APD, between-group differences were not statistically significant at either follow-up (T2: Δ = −0.03 mm, 95% CI: −0.10 to 0.05; p = 0.456; T3: Δ = −0.02 mm, 95% CI: −0.10 to 0.05; p = 0.538). For AAL, no significant difference was observed at 3 months (Δ = 0.03 mm, 95% CI: −0.09 to 0.16; p = 0.594), but a small, statistically significant difference was seen at 2 years (Δ = 0.14 mm, 95% CI: 0.00 to 0.27; p = 0.043).
Table 6 shows that omnibus Group × Time interaction tests were significant for Plaque (F(2, 240) = 22.41, p < 0.001) and BOP (F(2, 240) = 7.88, p < 0.001), significant for AAL (F(2, 240) = 3.52, p = 0.031) — although the between-group differences were very small (≈0.14 mm at 2 years) and thus of limited clinical relevance—and not significant for APD (F(2, 240) = 0.78, p = 0.460).

Table 6.
Results of Omnibus Group × Time Interaction Tests for Key Clinical Outcomes.
3.6. Trends in Smoking Behavior
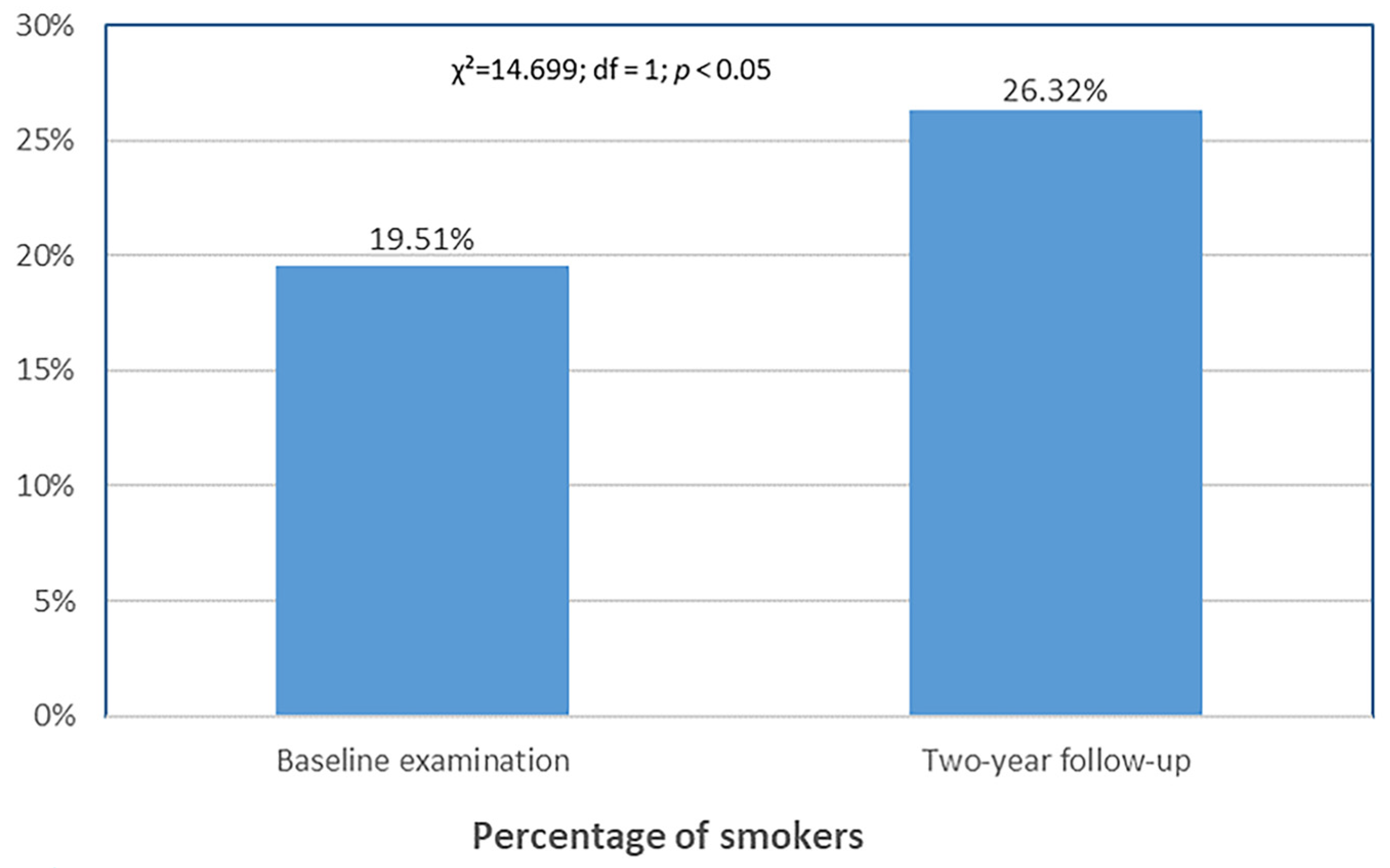
Figure 2 shows a significant increase in self-reported smoking at the 2-year follow-up compared with baseline (p < 0.05).
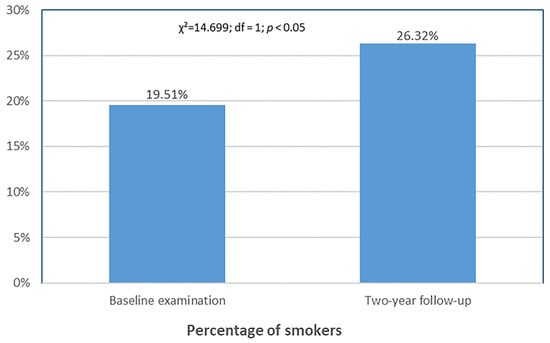
Figure 2.
Change in self-reported smoking prevalence over two years.
3.7. Self-Reported Oral Hygiene Behaviors
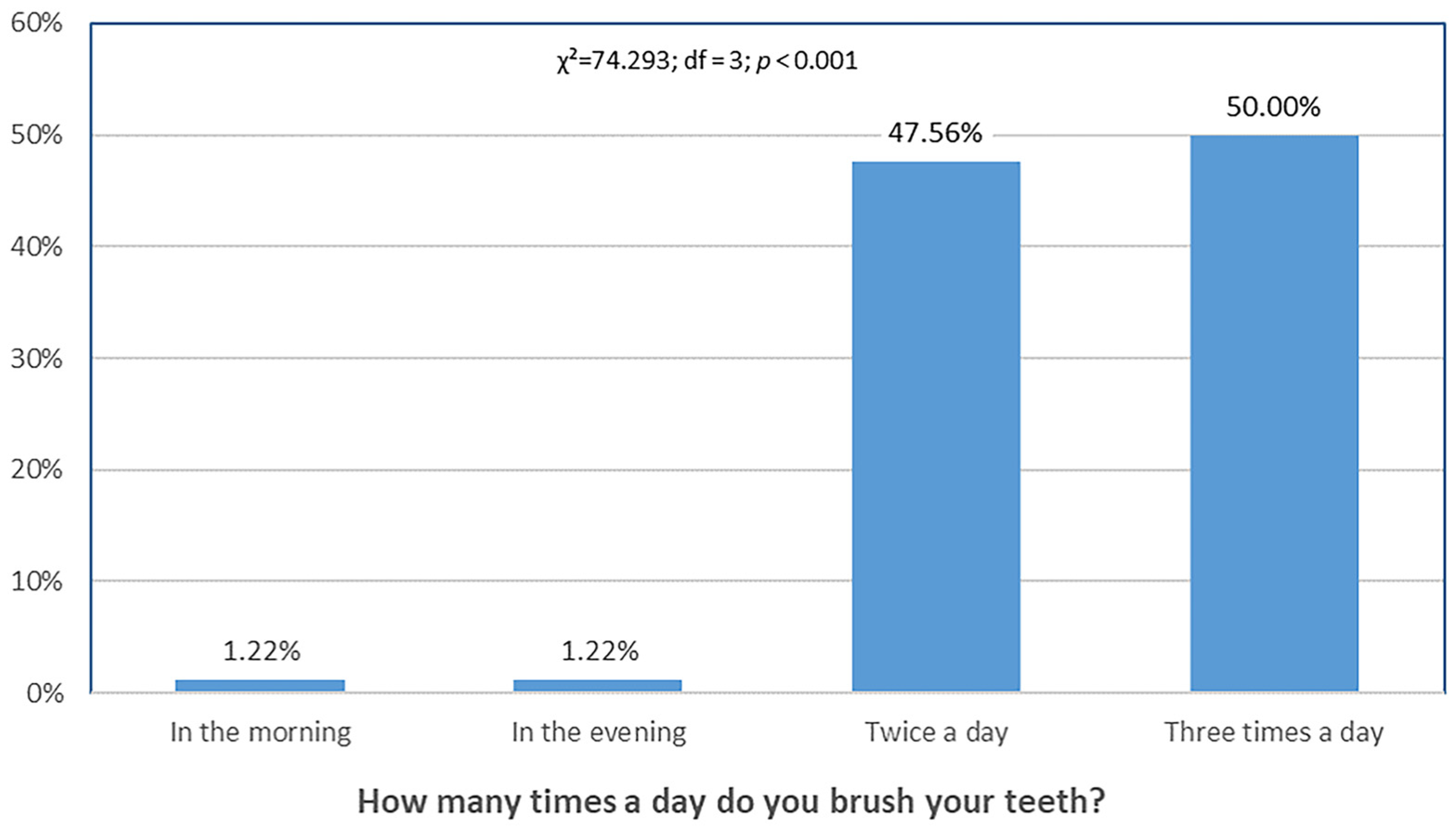
Oral hygiene behaviors were assessed using a self-reported questionnaire administered only at baseline. Participants provided information on daily toothbrushing frequency, and use of dental floss and interdental brushes. These baseline data offer a descriptive overview of the participants’ hygiene habits at the start of this study and provide context for interpreting clinical outcomes.
Figure 3 shows that the proportion of participants who brushed their teeth only once per day (morning or evening) was the lowest, with a statistically significant difference compared with other frequencies.
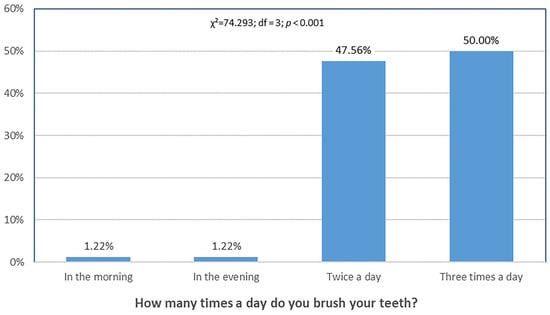
Figure 3.
Differences in toothbrushing frequency. Distribution of responses differed significantly across categories (χ2 = 74.293, df = 3, p < 0.001).
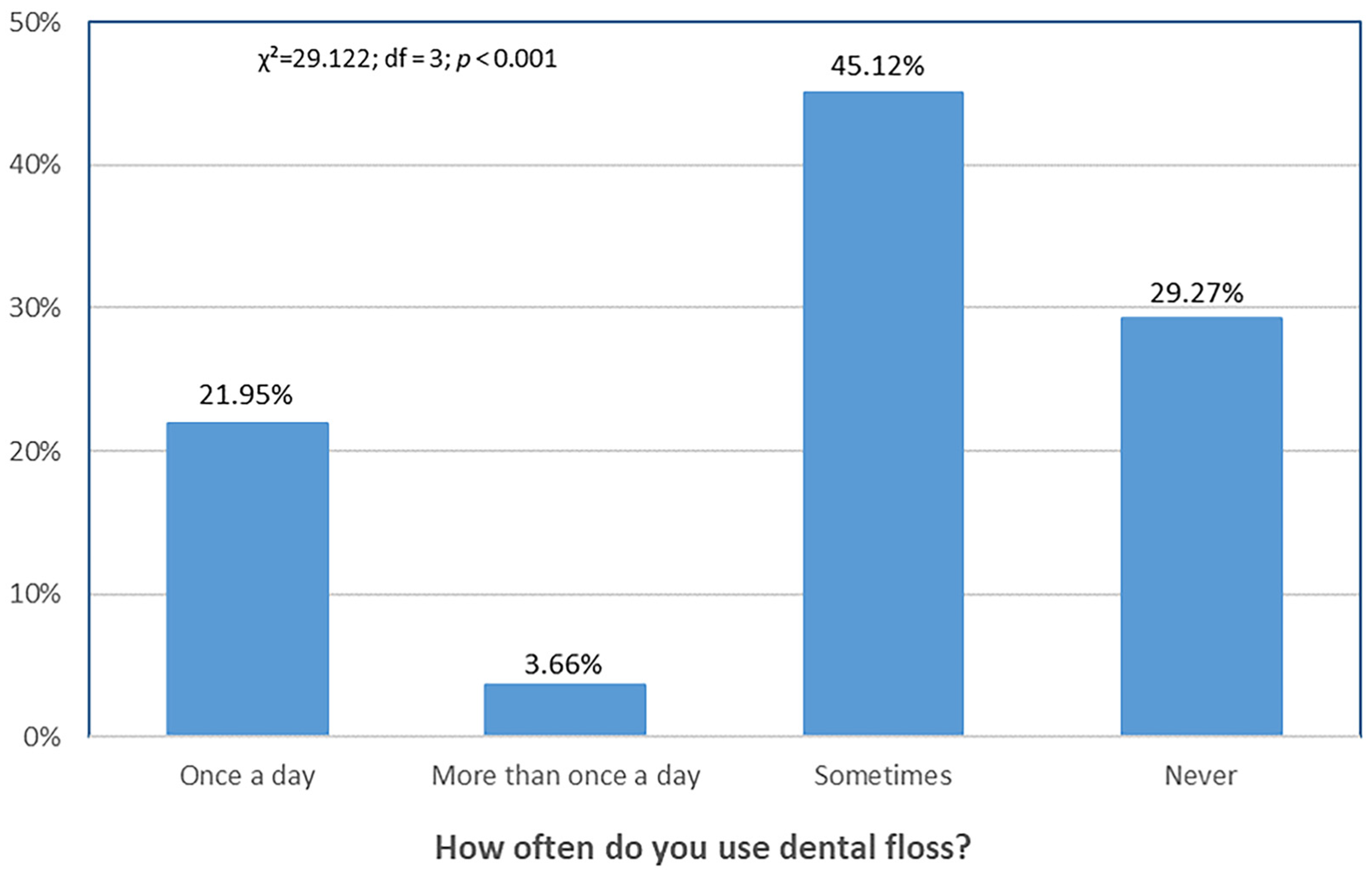
Figure 4 shows that the proportion of participants who used dental floss multiple times per day was the lowest, whereas the highest proportion used dental floss occasionally.
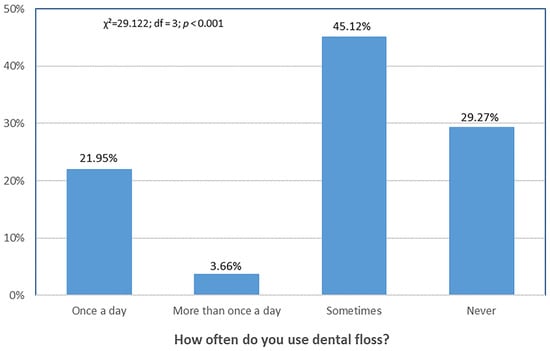
Figure 4.
Differences in frequency of dental floss use. Distribution of responses differed significantly across categories (χ2 = 29.122, df = 3, p < 0.001).
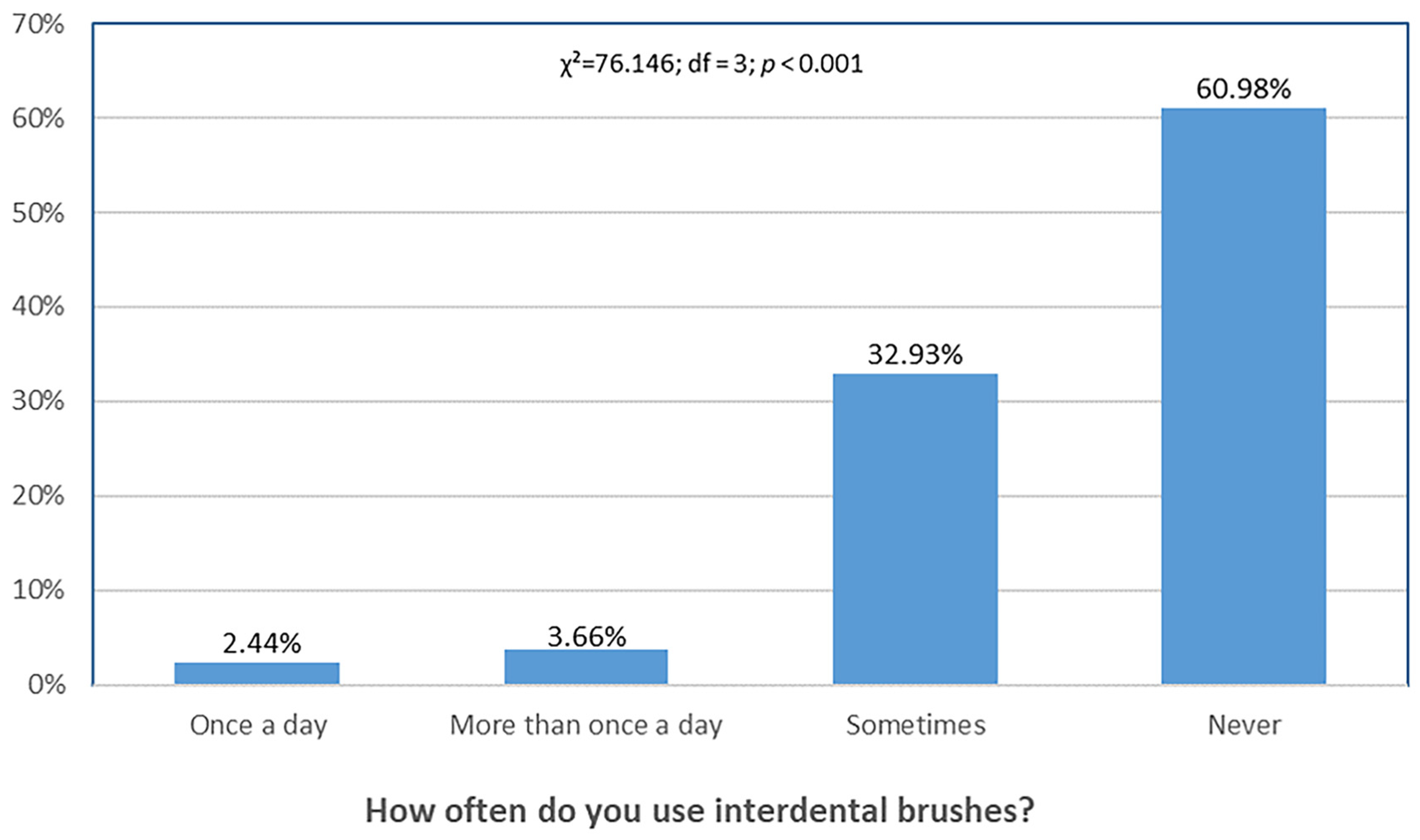
Figure 5 shows that relatively few participants used interdental brushes daily, while most reported never using them.
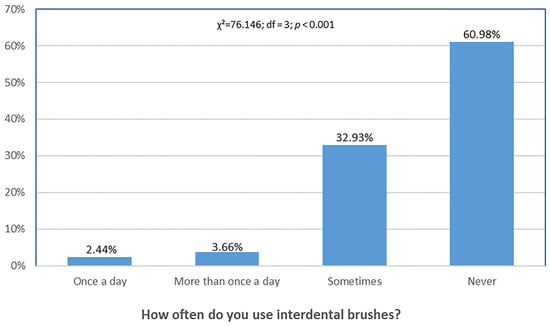
Figure 5.
Differences in frequency of interdental brush use. Distribution of responses differed significantly across categories (χ2 = 76.146, df = 3, p < 0.001).
4. Discussion
4.1. Effectiveness of Individualized Education
Participation in the iTOP program led to significant short-term improvements in key clinical oral health parameters, especially plaque index and bleeding on probing. While improvements were observed at 3 months, by the 2-year follow-up, most periodontal parameters, except plaque index, had returned to baseline. The short-term gains were supported by statistical significance, effect sizes, and post hoc power, whereas long-term benefits were limited. These findings suggest that a single iTOP session, without ongoing reinforcement, may be insufficient to sustain long-term periodontal benefits.
This study was intentionally designed as a single-session intervention to assess the isolated effect of an initial iTOP training, reflecting pragmatic curricular constraints where repeated sessions may be difficult to implement. The decline in effect may be due to the lack of structured reinforcement following the initial session and the high academic workload and stress faced by medical and dental students, which could deprioritize daily oral hygiene. Another explanation is the general tendency for behavioral gains to dissipate without ongoing motivation or environmental support. Since both groups showed some improvements over time, especially in plaque index, the sustained effect in the iTOP group at 2 years may reflect not only the intervention but also academic progression, enhanced oral health literacy, and curricular exposure. Consequently, long-term differences should be interpreted cautiously.
In the broader context of oral hygiene education, various protocols—ranging from classroom-based group lectures to school-based reinforcement and digital app–based motivational programs—have consistently produced short-term improvements in plaque control and gingival health. For instance, Jönsson et al. [1] reported clinically meaningful plaque reductions after individually tailored education for periodontal patients, while school-based repeated sessions have been shown to maintain improved oral hygiene scores over short follow-ups [19]. A recent structured group-education trial demonstrated significant short-term improvements, which diminished without reinforcement. [2]. These results are consistent with the broader literature: iTOP’s individualized, hands-on approach produces notable initial effects, though sustained benefits likely require repeated reinforcement sessions. Long-term adherence to iTOP may be affected by individual and contextual factors such as changing intrinsic motivation, limited time, and competing academic demands. Previous studies have shown that knowledge alone does not guarantee sustained oral hygiene behavior among health profession students [5,6,12], and psychosocial stressors may further reduce compliance [13,14]. Understanding these barriers is essential for designing interventions that achieve lasting behavior change. Future studies should assess the scalability, cost-effectiveness, and optimal frequency of booster sessions needed to maintain iTOP’s benefits within university curricula.
The non-iTOP group showed initial improvements, but these effects were not sustained over time. The most pronounced deterioration was observed in bleeding on probing and probing depth. These findings suggest the added value of individualized training. Although other parameters worsened, the plaque index decrease in the control group likely reflects academic progression, improved oral health literacy, and curricular exposure, rather than the intervention itself. Academic progression may partly explain this finding, since earlier studies show a link between higher education and better oral health. Higher education levels are consistently linked with increased health literacy, improved oral hygiene practices, and more favorable periodontal health [20,21,22,23].
Few cohort studies have examined how oral health changes over time after educational interventions. In a study by Kalevski et al. [17], dental students underwent an initial oral health assessment before the educational intervention. Follow-up assessments measured clinical changes in oral health parameters. Although significant improvements were reported, oral hygiene levels among dental students remained suboptimal [17]. A similar pattern was observed at the Faculty of Medicine, University of Mostar. Students in the iTOP group had significantly better clinical outcomes during the second and third assessments than their peers in the control group. Nevertheless, there remains room for improvement in overall oral hygiene and clinical indicators. While previous studies have examined oral health education among dental students in Southeast Europe, to our knowledge, this appears to be among the first studies to assess the long-term clinical effectiveness of a single-session iTOP intervention in both medical and dental students.
A systematic review by Nakre et al. [18] found that short-term gains in oral health behaviors often diminish without sustained efforts, supporting the findings of this study. In the group that participated in the iTOP program, all measured parameters—except plaque index—returned to baseline values by the end of the 2-year follow-up. Although a statistically significant improvement in oral hygiene was observed at the three-month follow-up, this effect was no longer evident after two years. The findings indicate that regular education may be important for achieving lasting behavior change and better hygiene.
The findings align with health behavior theories, such as the Health Belief Model and the Theory of Planned Behavior [24,25], which highlight perceived benefits, self-efficacy, and ongoing external reinforcement as critical for maintaining long-term behavioral adherence. Integrating these theoretical insights can inform the development of more effective oral health education interventions aimed at maintaining improved hygiene behaviors over time.
4.2. Differences by Academic Program
At baseline, dental students had better periodontal indicators than medical students. Similar findings have been reported in previous studies, with dental students consistently showing superior oral hygiene knowledge, attitudes, and behaviors compared with their medical counterparts [26,27,28]. However, in this study, group differences were minimal, with significant variation only in probing depth and attachment level. By the 2-year follow-up, these differences had diminished, indicating a convergence in periodontal status between the student groups over time.
4.3. Impact of Academic Year
Baseline data showed that older students had significantly lower plaque index than younger students. This may reflect better oral hygiene habits among more advanced students. No significant differences were observed in other periodontal parameters between the two academic levels. After two years, when the cohorts reached their third and sixth years, the groups showed no significant differences in oral health.
Most previous studies have focused on comparing oral health knowledge between medical and dental students, analyzing differences in their understanding and attitudes. Within these groups, particular attention has been given to comparing the knowledge and attitudes of junior versus senior students. Studies in the general population suggest that younger individuals often have better oral health than older adults [29]. However, studies of medical and dental students have produced inconsistent findings regarding their knowledge and attitudes toward oral health. Yao et al. [30] found no significant differences in oral health knowledge and attitudes between first-year medical and dental students, although the latter had marginally higher scores. In addition, third-year dental students outperformed their medical peers in the same parameters, with statistically significant differences [30]. Other studies assessing medical students’ knowledge and attitudes have revealed a generally low level of awareness on this topic. Nevertheless, senior students showed significantly better awareness than junior ones. [31].
Additionally, studies analyzing dental students’ attitudes toward oral health and their personal oral hygiene practices have included both preclinical and clinical students. However, findings across these studies are inconsistent. Some report no significant differences between preclinical and clinical students [32], while others indicate that preclinical students have lower oral health knowledge, attitudes, and behaviors [33]. This highlights the need for structured educational interventions.
Such variations may be due to differences in target populations (e.g., medical vs. dental students), as well as disparities in conceptual frameworks, methodology, questionnaire types, and sample sizes.
4.4. Smoking Behavior Trends
Smoking prevalence increased during this study. Specifically, during the first assessment, 19.51% of participants reported being smokers, while by the third assessment—conducted two years later—this number had risen to 26.32%. This increase may reflect the high stress levels experienced by medical and dental students during academic training [34,35]. However, other studies show no statistical link between smoking and student age, suggesting that academic year may not reliably predict smoking behavior [36,37]. The lack of adequate smoking prevention and cessation programs at universities further worsens the situation. It is essential to develop prevention and education strategies aimed at reducing smoking rates among students [38]. Smoking has numerous negative effects not only on oral health but also on overall health [39]. This increase in smoking prevalence may have adversely influenced clinical outcomes, especially bleeding on probing and probing depth. Given that smoking is a well-known risk factor for periodontal disease, the increase in smoking prevalence may have partially attenuated the long-term effects of the iTOP intervention. Future studies should carefully account for smoking status as a potential confounder. While larger sample sizes may facilitate more comprehensive multivariate modeling, the influence of smoking on intervention effects should be interpreted with caution given the limitations of observational designs.
4.5. Study Limitations and Future Directions
The findings of this study are generally consistent with previous research, although no directly comparable study was identified. Adjusted mixed-model analyses yielded the same main conclusions as the non-parametric analyses, supporting the consistency of our findings. As with all research, several limitations should be acknowledged. Aligned with descriptive and model-based analyses, changes in probing depth and attachment level were small and not statistically significant, suggesting that the primary benefit of the intervention was in plaque control. First, this study was conducted at a single institution, which may limit the generalizability of the findings to other educational settings or cultural contexts. In addition, the study population consisted exclusively of medical and dental students, who may be more motivated and knowledgeable about oral hygiene than the general public. This may have led to greater adherence to oral hygiene recommendations and, consequently, to somewhat more favorable clinical outcomes than would be expected in broader, more heterogeneous populations. Furthermore, while medical and dental students represent a relevant and high-impact group, future studies should aim to replicate these findings in other academic or community populations to enhance the external validity and generalizability of the intervention. Second, the sample size was relatively small and constrained by the number of students available per academic year. Moreover, the sample included only first/fourth- and third/sixth-year students from both medicine and dentistry programs. Furthermore, academic progression and increased curricular exposure over the 2-year follow-up may have contributed to improvements in oral health parameters in both groups, potentially confounding the observed long-term difference in plaque index. Another limitation is the Hawthorne effect, whereby participants may have improved their behavior simply because they were being observed. Repeated professional cleanings in both groups may have further amplified this effect, potentially contributing to improvements independent of the intervention. Additionally, the single-site academic setting and culturally homogeneous sample limit the generalizability of our findings. Additionally, all participants received standardized oral hygiene kits at each assessment point, which may have inadvertently influenced the control group’s behavior and diminished observable differences between the intervention and control groups. This potential bias should be considered when interpreting the results. This study assessed the effects of a single-session iTOP with only a brief 3-month reinforcement; no ongoing reinforcement beyond that was provided. Long-term adherence to the techniques was not systematically monitored, and no objective compliance measures were obtained beyond baseline self-reports, limiting attribution of 2-year outcomes solely to the intervention. Therefore, the observed decline should be viewed in light of this limitation, and outcomes could potentially differ with repeated interventions.
Although we made efforts to standardize conditions across participants, we were unable to control for all potential confounding factors. These include individual motivation, differences in curricular exposure, use of additional hygiene tools, academic stress, personal health beliefs, and other lifestyle-related behaviors. Such unmeasured variables may have influenced the outcomes and should be carefully considered in future research designs. Furthermore, the local context in which this study was conducted may have influenced the results. Factors such as the local education system, the availability of preventive dental services, and cultural attitudes toward oral hygiene may significantly influence oral health behaviors and outcomes. These contextual factors limit the generalizability of our findings to other academic or geographical settings.
Although the final response rate was high (92.7%), a small number of non-responders may still introduce attrition bias.
Future studies of this type should aim to increase the sample size and ideally include all students at the Faculty of Medicine, University of Mostar. Multiple studies have confirmed that knowledge about oral health tends to improve with age and level of education [20,21,22,23]. To ensure this trend is reflected at the University of Mostar, ongoing education and awareness campaigns on oral health should be maintained.
Given the high prevalence of oral diseases such as caries, gingivitis, and periodontitis, targeted research in specific populations, e.g., schoolchildren and university students, is essential [40,41]. Such studies help assess oral health awareness and support the development of preventive and educational interventions. Although results may not be immediate, investing in education is a long-term strategy for improving oral health among future generations [42]. Educating young individuals on proper hygiene and the importance of oral health has the potential to positively influence not only their own long-term health, but also the health of those around them, particularly within their future families and professional roles.
5. Conclusions
This study suggests that Individually Trained Oral Prophylaxis (iTOP) is effective in achieving short-term improvements in oral health among medical and dental students. Plaque index was the only parameter showing a sustained effect at 2 years, which should be interpreted cautiously, as improvements in both groups may reflect academic progression and enhanced oral health literacy rather than the intervention alone. Other parameters, such as probing depth and bleeding on probing, reverted to baseline levels. These findings underscore the need for continuous reinforcement of oral health education. A single session appears insufficient for lasting behavioral change; therefore, future programs should include repeated or supplemental interventions. Differences between subgroups decreased over time, which may reflect both the intervention and academic progression. Overall, iTOP led to short-term improvements and a sustained effect on plaque index, supported by effect sizes and post hoc power, whereas other periodontal parameters reverted to baseline. iTOP appears promising as an educational intervention, though its incorporation into university curricula warrants cautious consideration. Due to the single-center design and limited sample size, these findings are preliminary, and further multicenter studies are warranted before wider implementation.
Author Contributions
Conceptualization, Z.L. and J.K.; methodology, Z.L. and A.P.B.; validation, M.M., I.M.L. and A.P.B.; formal analysis, B.M.; investigation, Z.L. and B.M.; resources, J.K. and I.M.L.; data curation, Z.L. and B.M.; writing—original draft preparation, Z.L. and B.M.; writing—review and editing, Z.L., B.M., M.M. and A.P.B.; visualization, B.M.; supervision, A.P.B. All authors have read and agreed to the published version of this manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study was conducted according to the guidelines of the Declaration of Helsinki, and approved by the Ethics Committee of School of Medicine, University of Mostar, Mostar, Bosnia and Herzegovina (No.: 01-I-1827/21) and (No.: 01-I-911/24).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
The data that support the findings of this study are available upon request from the authors.
Acknowledgments
The authors sincerely appreciate Biasco d.o.o. for supplying the oral hygiene kits used in this study. The supplier had no role in study design, data collection, analysis, or manuscript preparation.
Conflicts of Interest
The authors declare no conflicts of interest.
Abbreviations
The following abbreviations are used in this manuscript:
| iTOP | Individually trained oral prophylaxis |
| APD | Average probing depth |
| AAL | Average attachment level |
| BOP | Bleeding on probing |
| PLQ | Plaque index |
| CI | Confidence interval |
| IQR | Interquartile range |
| CEJ | Cementoenamel junction |
| UNC-15 | University of North Carolina 15 probe |
| pp | percentage points |
Appendix A
Post hoc power analyses were conducted for the main between-group comparisons (iTOP vs. control, dental vs. medical students, and younger vs. older students) for each primary outcome across time points. The analyses report the observed effect size (Cohen’s d) and the corresponding post hoc statistical power (1 − β), calculated for the actual sample sizes using a two-tailed independent-samples t-test with α = 0.05. In this context, 1 − β represents the probability of detecting the observed effect given the sample size; values ≥ 0.80 are generally considered to indicate adequate statistical power.

Table A1.
Post hoc power (1 − β) and Cohen’s d for between-group comparisons: iTOP vs. control group.
Table A1.
Post hoc power (1 − β) and Cohen’s d for between-group comparisons: iTOP vs. control group.
| Comparison | Timepoint | Outcome | Group 1 | Group 2 | Group 1 Mean CI | Group 2 Mean CI | Cohen’s d | Post Hoc Power Test |
|---|---|---|---|---|---|---|---|---|
| iTOP group versus control group | T1 | APD | 40 | 42 | 1.85 (95% CI: 1.78, 1.92) | 1.88 (95% CI: 1.82, 1.93) | −0.14 | 0.10 |
| T1 | AAL | 40 | 42 | −1.85 (95% CI: −1.92, −1.79) | −1.88 (95% CI: −1.93, −1.83) | 0.13 | 0.09 | |
| T1 | PLQ | 40 | 42 | 67.60 (95% CI: 61.46, 73.74) | 67.38 (95% CI: 61.12, 73.65) | 0.01 | 0.05 | |
| T1 | BOP | 40 | 42 | 8.72 (95% CI: 6.65, 10.80) | 8.14 (95% CI: 5.99, 10.29) | 0.09 | 0.07 | |
| T2 | APD | 40 | 42 | 1.74 (95% CI: 1.69, 1.80) | 1.78 (95% CI: 1.74, 1.82) | −0.23 | 0.18 | |
| T2 | AAL | 40 | 42 | −1.74 (95% CI: −1.79, −1.69) | −1.78 (95% CI: −1.82, −1.74) | 0.25 | 0.20 | |
| T2 | PLQ | 40 | 42 | 23.35 (95% CI: 19.14, 27.56) | 44.55 (95% CI: 37.28, 51.81) | −1.11 | 1.00 | |
| T2 | BOP | 40 | 42 | 4.53 (95% CI: 3.27, 5.78) | 7.90 (95% CI: 6.04, 9.77) | −0.66 | 0.84 | |
| T3 | APD | 37 | 39 | 1.92 (95% CI: 1.87, 1.97) | 1.95 (95% CI: 1.90, 2.00) | −0.23 | 0.16 | |
| T3 | AAL | 37 | 39 | −1.81 (95% CI: −2.02, −1.60) | −1.96 (95% CI: −2.01, −1.91) | 0.32 | 0.28 | |
| T3 | PLQ | 37 | 39 | 17.46 (95% CI: 12.62, 22.30) | 35.08 (95% CI: 29.03, 41.12) | −1.05 | 0.99 | |
| T3 | BOP | 37 | 39 | 7.41 (95% CI: 6.32, 8.49) | 13.59 (95% CI: 11.68, 15.50) | −1.29 | 1.00 |
Time points are labeled as: (T1) baseline, (T2) 3-month follow-up, and (T3) 2-year follow-up. Outcomes are labeled as: (APD) average probing depth, (AAL) average attachment level, (PLQ) plaque, and (BOP) bleeding on probing.

Table A2.
Post hoc power (1 − β) and Cohen’s d for between-group comparisons: dental students vs. medical students.
Table A2.
Post hoc power (1 − β) and Cohen’s d for between-group comparisons: dental students vs. medical students.
| Comparison | Timepoint | Outcome | Group 1 | Group 2 | Group 1 Mean CI | Group 2 Mean CI | Cohen’s d | Post Hoc Power Test |
|---|---|---|---|---|---|---|---|---|
| Dental students versus Medical students | T1 | APD | 40 | 42 | 1.82 (95% CI: 1.75, 1.88) | 1.91 (95% CI: 1.86, 1.96) | −0.49 | 0.59 |
| T1 | AAL | 40 | 42 | −1.82 (95% CI: −1.89, −1.76) | −1.90 (95% CI: −1.95, −1.86) | 0.47 | 0.55 | |
| T1 | PLQ | 40 | 42 | 67.42 (95% CI: 60.91, 73.94) | 67.55 (95% CI: 61.63, 73.47) | −0.01 | 0.05 | |
| T1 | BOP | 40 | 42 | 7.22 (95% CI: 5.50, 8.95) | 9.57 (95% CI: 7.21, 11.93) | −0.36 | 0.36 | |
| T2 | APD | 40 | 42 | 1.74 (95% CI: 1.69, 1.78) | 1.78 (95% CI: 1.73, 1.83) | −0.30 | 0.27 | |
| T2 | AAL | 40 | 42 | −1.74 (95% CI: −1.79, −1.69) | −1.78 (95% CI: −1.83, −1.73) | 0.29 | 0.25 | |
| T2 | PLQ | 40 | 42 | 32.62 (95% CI: 26.02, 39.23) | 35.71 (95% CI: 28.59, 42.84) | −0.14 | 0.10 | |
| T2 | BOP | 40 | 42 | 5.47 (95% CI: 4.07, 6.88) | 7.00 (95% CI: 5.11, 8.89) | −0.29 | 0.25 | |
| T3 | APD | 38 | 38 | 1.92 (95% CI: 1.87, 1.97) | 1.95 (95% CI: 1.90, 2.00) | −0.20 | 0.14 | |
| T3 | AAL | 38 | 38 | −1.92 (95% CI: −1.96, −1.87) | −1.86 (95% CI: −2.06, −1.65) | −0.14 | 0.09 | |
| T3 | PLQ | 38 | 38 | 27.13 (95% CI: 20.06, 34.20) | 25.87 (95% CI: 20.58, 31.15) | 0.07 | 0.06 | |
| T3 | BOP | 38 | 38 | 10.18 (95% CI: 8.51, 11.86) | 10.97 (95% CI: 8.91, 13.04) | −0.14 | 0.09 |
Time points are labeled as: (T1) baseline, (T2) 3-month follow-up, and (T3) 2-year follow-up. Outcomes are labeled as: (APD) average probing depth, (AAL) average attachment level, (PLQ) plaque, and (BOP) bleeding on probing.

Table A3.
Post hoc power (1 − β) and Cohen’s d for between-group comparisons: younger students vs. older students.
Table A3.
Post hoc power (1 − β) and Cohen’s d for between-group comparisons: younger students vs. older students.
| Comparison | Timepoint | Outcome | Group 1 | Group 2 | Group 1 Mean CI | Group 2 Mean CI | Cohen’s d | Post Hoc Power Test |
|---|---|---|---|---|---|---|---|---|
| Younger students versus older students | T1 | APD | 40 | 42 | 1.86 (95% CI: 1.80, 1.91) | 1.87 (95% CI: 1.81, 1.93) | −0.06 | 0.06 |
| T1 | AAL | 40 | 42 | −1.85 (95% CI: −1.90, −1.80) | −1.88 (95% CI: −1.94, −1.82) | 0.16 | 0.11 | |
| T1 | PLQ | 40 | 42 | 72.05 (95% CI: 65.73, 78.37) | 63.14 (95% CI: 57.36, 68.93) | 0.47 | 0.55 | |
| T1 | BOP | 40 | 42 | 9.88 (95% CI: 7.29, 12.46) | 7.05 (95% CI: 5.60, 8.50) | 0.43 | 0.49 | |
| T2 | APD | 40 | 42 | 1.77 (95% CI: 1.72, 1.83) | 1.75 (95% CI: 1.71, 1.79) | 0.15 | 0.10 | |
| T2 | AAL | 40 | 42 | −1.76 (95% CI: −1.82, −1.71) | −1.75 (95% CI: −1.80, −1.71) | −0.07 | 0.06 | |
| T2 | PLQ | 40 | 42 | 36.58 (95% CI: 29.27, 43.88) | 31.95 (95% CI: 25.52, 38.39) | 0.21 | 0.16 | |
| T2 | BOP | 40 | 42 | 6.97 (95% CI: 5.01, 8.94) | 5.57 (95% CI: 4.20, 6.94) | 0.26 | 0.22 | |
| T3 | APD | 36 | 40 | 1.95 (95% CI: 1.89, 2.00) | 1.92 (95% CI: 1.87, 1.97) | 0.16 | 0.10 | |
| T3 | AAL | 36 | 40 | −1.84 (95% CI: −2.06, −1.63) | −1.93 (95% CI: −1.97, −1.88) | 0.18 | 0.12 | |
| T3 | PLQ | 36 | 40 | 30.00 (95% CI: 22.24, 37.76) | 23.35 (95% CI: 18.92, 27.78) | 0.36 | 0.33 | |
| T3 | BOP | 36 | 40 | 11.36 (95% CI: 9.02, 13.70) | 9.88 (95% CI: 8.50, 11.25) | 0.26 | 0.20 |
Time points are labeled as: (T1) baseline, (T2) 3-month follow-up, and (T3) 2-year follow-up. Outcomes are labeled as: (APD) average probing depth, (AAL) average attachment level, (PLQ) plaque, and (BOP) bleeding on probing.
References
- Jönsson, B.; Ohrn, K.; Oscarson, N.; Lindberg, P. The effectiveness of an individually tailored oral health educational programme on oral hygiene behaviour in patients with periodontal disease: A blinded randomized-controlled clinical trial (one-year follow-up). J. Clin. Periodontol. 2009, 36, 1025–1034. [Google Scholar] [CrossRef] [PubMed]
- Taheri, A.M.; Zarei, F.; Hidarnia, A.; Tavousi, M. Effectiveness of a school-based educational intervention on oral health knowledge, attitudes, practices, and self-efficacy among female secondary school students: A randomized controlled trial. BMC Oral Health 2025, 25, 625. [Google Scholar] [CrossRef] [PubMed]
- Swe, K.K.; Soe, A.K.; Aung, S.H.; Soe, H.Z. Effectiveness of oral health education on 8- to 10-year-old school children in rural areas of the Magway Region, Myanmar. BMC Oral Health 2021, 21, 2. [Google Scholar] [CrossRef]
- Viebranz, S.; Dederichs, M.; Kwetkat, A.; Schüler, I.M. Effectiveness of Individual Oral Health Care Training in Hospitalized Inpatients in Geriatric Wards. Int. J. Environ. Res. Public Health 2023, 20, 4275. [Google Scholar] [CrossRef]
- Kumar, H.; Behura, S.; Ramachandra, S.; Nishat, R.; Dash, K.; Mohiddin, G. Oral Health Knowledge, Attitude, and Practices Among Dental and Medical Students in Eastern India—A Comparative Study. J. Int. Soc. Prev. Community Dent. 2017, 7, 58. [Google Scholar] [CrossRef]
- Lujo, M.; Meštrović, M.; Malčić, A.I.; Karlović, Z.; Matijević, J.; Jukić, S. Knowledge, Attitudes and Habits Regarding Oral Health in First- and Final-Year Dental Students. Acta Clin. Croat. 2016, 55, 636–643. [Google Scholar] [CrossRef][Green Version]
- Habibovic, J.; Demirovic, K.; Habibovic, E.; Durek, J. Assessment of the Oral Health Perceptions and Behaviours of Adolescents in Bosnia and Herzegovina: A Cross Sectional Study. Healthcare 2025, 13, 1347. [Google Scholar] [CrossRef]
- Herrera, D.; Sanz, M.; Shapira, L.; Brotons, C.; Chapple, I.; Frese, T.; Graziani, F.; Hobbs, F.D.R.; Huck, O.; Hummers, E.; et al. Periodontal diseases and cardiovascular diseases, diabetes, and respiratory diseases: Summary of the consensus report by the European Federation of Periodontology and WONCA Europe. Eur. J. Gen. Pract. 2024, 30, 2320120. [Google Scholar] [CrossRef]
- Peres, M.A.; Macpherson, L.M.D.; Weyant, R.J.; Daly, B.; Venturelli, R.; Mathur, M.R.; Listl, S.; Celeste, R.K.; Guarnizo-Herreño, C.C.; Kearns, C.; et al. Oral diseases: A global public health challenge. Lancet 2019, 394, 249–260. [Google Scholar] [CrossRef]
- Ghaffari, M.; Rakhshanderou, S.; Ramezankhani, A.; Buunk-Werkhoven, Y.; Noroozi, M.; Armoon, B. Are educating and promoting interventions effective in oral health?: A systematic review. Int. J. Dent. Hyg. 2018, 16, 48–58. [Google Scholar] [CrossRef] [PubMed]
- Tadin, A.; Poljak Guberina, R.; Domazet, J.; Gavic, L. Oral Hygiene Practices and Oral Health Knowledge among Students in Split, Croatia. Healthcare 2022, 10, 406. [Google Scholar] [CrossRef]
- Kandasamy, G.; Almeleebia, T. Assessment of Oral Health Knowledge, Attitudes, and Behaviours among University Students in the Asir Region-Saudi Arabia: A Cross-Sectional Study. Healthcare 2023, 11, 3100. [Google Scholar] [CrossRef] [PubMed]
- Janicijevic, N.; Dimovic, T.; Stajic, D.; Djonovic, N.; Vasiljevic, D.; Tepavcevic, M.; Stepovic, M.; Delic, S.; Petrovic, M.; Jovanovic, K.; et al. Correlation between the Oral and Mental Health of University Students in Serbia—A Cross-Sectional Study. Healthcare 2024, 12, 1431. [Google Scholar] [CrossRef]
- Jeong, J.; Jeong, W.; Jung, Y. Association Between Self-Perceived Oral Health, Stress, and Oral Symptoms in South Korean University Students: A Cross-Sectional Study. Healthcare 2025, 13, 984. [Google Scholar] [CrossRef]
- Vilar Doceda, M.; Petit, C.; Huck, O. Behavioral Interventions on Periodontitis Patients to Improve Oral Hygiene: A Systematic Review. J. Clin. Med. 2023, 12, 2276. [Google Scholar] [CrossRef]
- Bashirian, S.; Khoshravesh, S.; Ayubi, E.; Karimi-Shahanjarini, A.; Shirahmadi, S.; Solaymani, P.F. The impact of health education interventions on oral health promotion among older people: A systematic review. BMC Geriatr. 2023, 23, 548. [Google Scholar] [CrossRef]
- Kalevski, K.; Vojinovic, J.; Gajic, M.; Aleksic, E.; Tambur, Z.; Milutinovic, J.; Borotic, N.; Mladenovic, R. The Outcomes of an Interventional Oral Health Program on Dental Students’ Oral Hygiene. Int. J. Environ. Res. Public Health 2021, 18, 3242. [Google Scholar] [CrossRef]
- Nakre, P.D.; Harikiran, A.G. Effectiveness of oral health education programs: A systematic review. J. Int. Soc. Prev. Community Dent. 2013, 3, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Potisomporn, P.; Sukarawan, W.; Sriarj, W. Oral Health Education Improved Oral Health Knowledge, Attitudes, and Plaque Scores in Thai Third-grade Students: A Randomised Clinical Trial. Oral Health Prev. Dent. 2019, 17, 523–531. [Google Scholar] [CrossRef] [PubMed]
- Paulander, J.; Axelsson, P.; Lindhe, J. Association between level of education and oral health status in 35-, 50-, 65- and 75-year-olds. J. Clin. Periodontol. 2003, 30, 697–704. [Google Scholar] [CrossRef]
- Ehsan, H.; Ahmadzai, N.; Orfani, Z.; Rezayee, B.M.; Wally, M.; Daftani, S. Oral Health Knowledge, Attitude, and Behavior Among Health Professions’ Students at Kabul University of Medical Sciences. Clin. Cosmet. Investig. Dent. 2023, 15, 349–358. [Google Scholar] [CrossRef]
- Vano, M.; Gennai, S.; Karapetsa, D.; Miceli, M.; Giuca, M.R.; Gabriele, M.; Graziani, F. The influence of educational level and oral hygiene behaviours on DMFT index and CPITN index in an adult Italian population: An epidemiological study. Int. J. Dent. Hyg. 2015, 13, 151–157. [Google Scholar] [CrossRef]
- Walther, C.; Spinler, K.; Borof, K.; Kofahl, C.; Heydecke, G.; Seedorf, U.; Beikler, T.; Terschüren, C.; Hajek, A.; Aarabi, G. Evidence from the Hamburg City Health Study—Association between education and periodontitis. BMC Public Health 2022, 22, 1662. [Google Scholar] [CrossRef]
- Rosenstock, I.M. The Health Belief Model and Preventive Health Behavior. Health Educ. Monogr. 1974, 2, 354–386. [Google Scholar] [CrossRef]
- Ajzen, I. The Theory of Planned Behavior. Organ. Behav. Human. Decis. Process. 1991, 50, 179–211. [Google Scholar] [CrossRef]
- Hasan, S.; Ahmed, S.; Panigrahi, R.; Chaudhary, P.; Vyas, V.; Saeed, S. Oral cavity and eating disorders: An insight to holistic health. J. Fam. Med. Prim. Care 2020, 9, 3890–3897. [Google Scholar] [CrossRef] [PubMed]
- Fiorillo, L. Oral Health: The First Step to Well-Being. Medicna 2019, 55, 676. [Google Scholar] [CrossRef] [PubMed]
- Orlandi, M.; Muñoz Aguilera, E.; Marletta, D.; Petrie, A.; Suvan, J.; D’Aiuto, F. Impact of the treatment of periodontitis on systemic health and quality of life: A systematic review. J. Clin. Periodontol. 2022, 49 (Suppl. S24), 314–327. [Google Scholar] [CrossRef]
- Silva-Junior, M.F.; Sousa, A.C.C.; Batista, M.J.; Sousa, M. Oral health condition and reasons for tooth extraction among an adult population (20–64 years old). Cien Saude Colet. 2017, 22, 2693–2702. [Google Scholar] [CrossRef]
- Yao, K.; Yao, Y.; Shen, X.; Lu, C.; Guo, Q. Assessment of the oral health behavior, knowledge and status among dental and medical undergraduate students: A cross-sectional study. BMC Oral Health 2019, 19, 26. [Google Scholar] [CrossRef]
- Bk, S.; Yavagal, P.; Gomez, M. Assessment of oral health awareness among undergraduate Medical Students in Davangere city: A cross-sectional survey. J. Indian Assoc. Public Health Dent. 2014, 12, 43. [Google Scholar] [CrossRef]
- Mekhemar, M.; Conrad, J.; Attia, S.; Dörfer, C. Oral Health Attitudes among Preclinical and Clinical Dental Students in Germany. Int. J. Environ. Res. Public Health 2020, 17, 4253. [Google Scholar] [CrossRef]
- Al-Wesabi, A.A.; Abdelgawad, F.; Sasahara, H.; El Motayam, K. Oral health knowledge, attitude and behaviour of dental students in a private university. BDJ Open 2019, 5, 16. [Google Scholar] [CrossRef]
- Zhu, T.; Feng, B.; Wong, S.; Choi, W.; Zhu, S.-H. A comparison of smoking behaviors among medical and other college students in China. Health Promot. Int. 2004, 19, 189–196. [Google Scholar] [CrossRef][Green Version]
- Steiner-Hofbauer, V.; Holzinger, A. How to Cope with the Challenges of Medical Education? Stress, Depression, and Coping in Undergraduate Medical Students. Acad. Psychiatry 2020, 44, 380–387. [Google Scholar] [CrossRef] [PubMed]
- Ilić, M.; Grujičić, M.; Novaković, B.; Vrkatić, A.; Lozanov-Crvenković, Z. Cigarette Smoking among Medical Students from the Western Balkan. Int. J. Environ. Res. Public Health 2022, 19, 3055. [Google Scholar] [CrossRef] [PubMed]
- Lotrean, L.M.; Man, M.; Gavrilescu, C.; Florea, M. Electronic Cigarette Use and Its Relationship with Smoking and Alcohol and Illicit Drug Consumption among Romanian University Students. Medcina 2021, 57, 137. [Google Scholar] [CrossRef] [PubMed]
- Majra, J. Do our medical colleges inculcate health-promoting lifestyle among medical students: A pilot study from two medical colleges from southern India. Int. J. Prev. Med. 2013, 4, 425–429. [Google Scholar]
- Maki, K.A.; Ganesan, S.M.; Meeks, B.; Farmer, N.; Kazmi, N.; Barb, J.J.; Joseph, P.V.; Wallen, G.R. The role of the oral microbiome in smoking-related cardiovascular risk: A review of the literature exploring mechanisms and pathways. J. Transl. Med. 2022, 20, 584. [Google Scholar] [CrossRef]
- Eke, P.I.; Dye, B.A.; Wei, L.; Slade, G.D.; Thornton-Evans, G.O.; Borgnakke, W.S.; Taylor, G.W.; Page, R.C.; Beck, J.D.; Genco, R.J. Update on Prevalence of Periodontitis in Adults in the United States: NHANES 2009 to 2012. J. Periodontol. 2015, 86, 611–622. [Google Scholar] [CrossRef]
- Kassebaum, N.J.; Bernabé, E.; Dahiya, M.; Bhandari, B.; Murray, C.J.; Marcenes, W. Global burden of severe periodontitis in 1990–2010: A systematic review and meta-regression. J. Dent. Res. 2014, 93, 1045–1053. [Google Scholar] [CrossRef] [PubMed]
- Sanadhya, Y.K.; Thakkar, J.P.; Divakar, D.D.; Pareek, S.; Rathore, K.; Yousuf, A.; Ganta, S.; Sobti, G.; Maniar, R.; Asawa, K.; et al. Effectiveness of oral health education on knowledge, attitude, practices and oral hygiene status among 12–15-year-old schoolchildren of fishermen of Kutch district, Gujarat, India. Int. Marit. Health 2014, 65, 99–105. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).