Effect of Bleaching on the Surface Roughness of Resin Composites Evaluated by Atomic Force Microscopy (AFM)
Abstract
1. Introduction
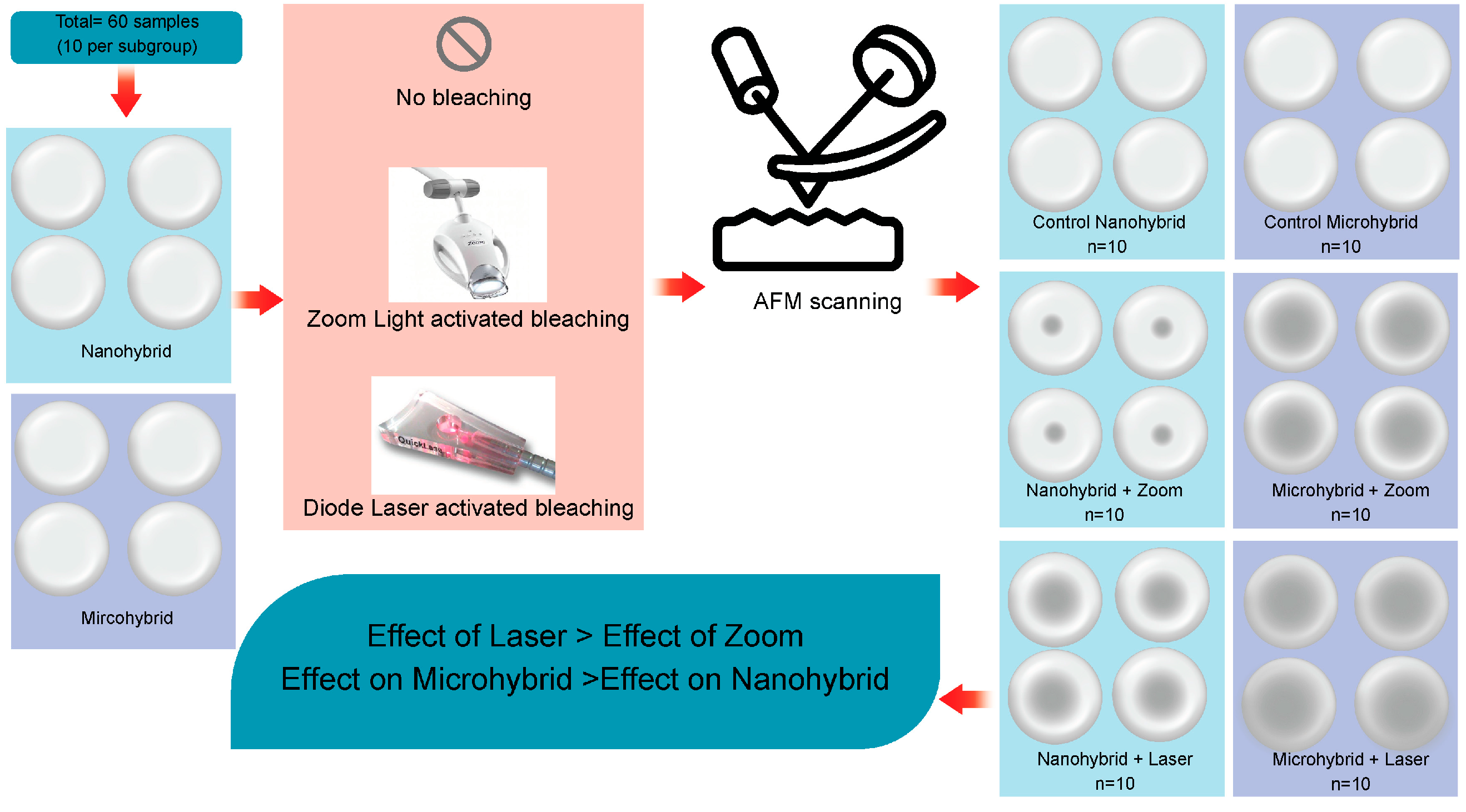
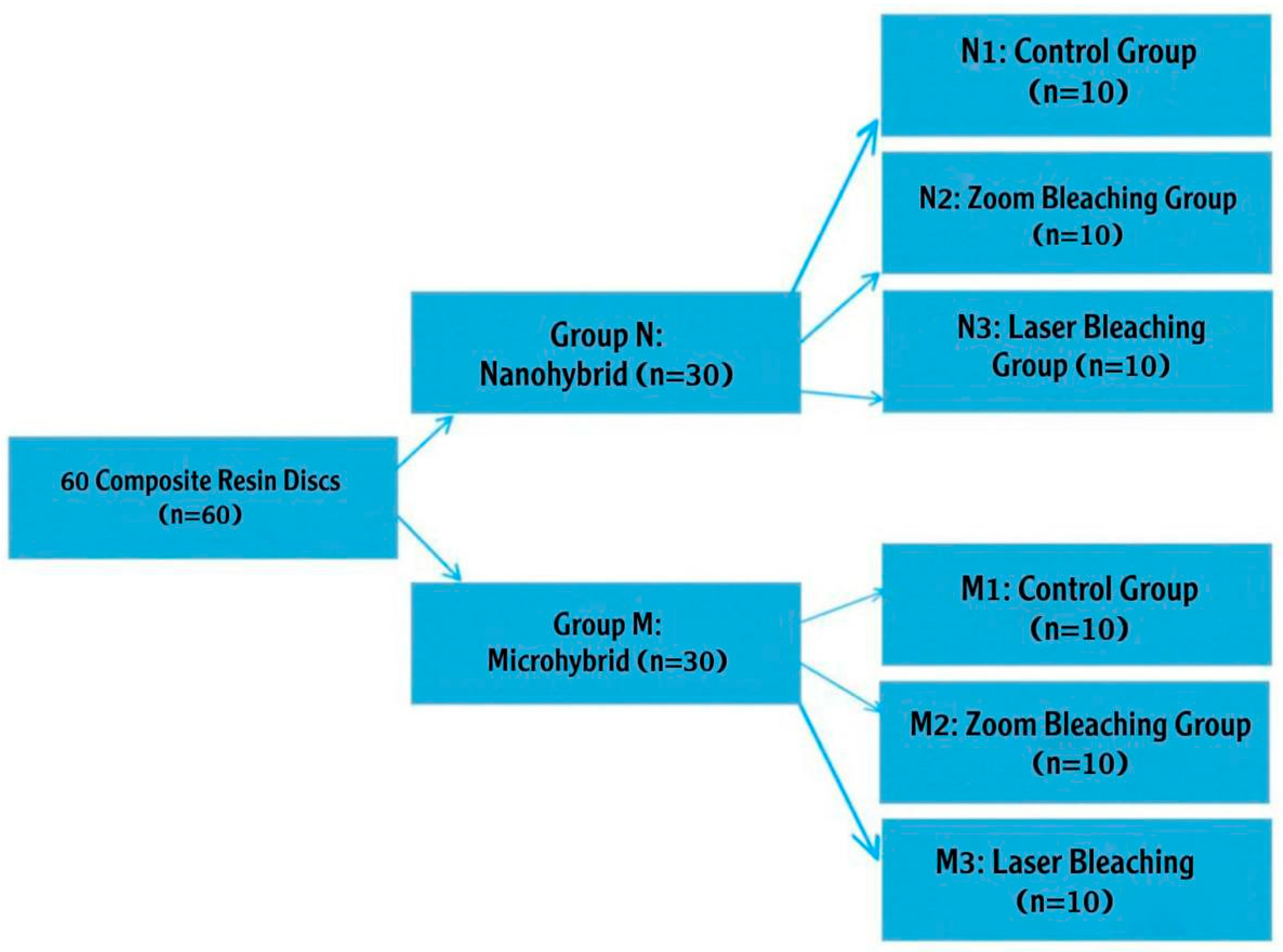
2. Materials and Methods
- Zoom Whitening + Zoom Gel (Philips Zoom, WA, USA): a light-activated bleaching system using 40% hydrogen peroxide gel.
- QuickLase Diode Laser + QuickLase Gel (QuickLase, Kent, UK): a diode laser-activated bleaching system (940 nm) with 35% hydrogen peroxide gel. For this study, the following materials, as presented in Table 1, were selected.
- N1 and M1 (control subgroups): no bleaching was applied.
- N2 and M2 (zoom subgroups): bleached using Philips Zoom light with zoom bleaching material (light activation technique).
- N3 and M3 (laser subgroups): bleached using QuickLase diode laser (940 nm) with QuickLase bleaching material (laser activation technique).
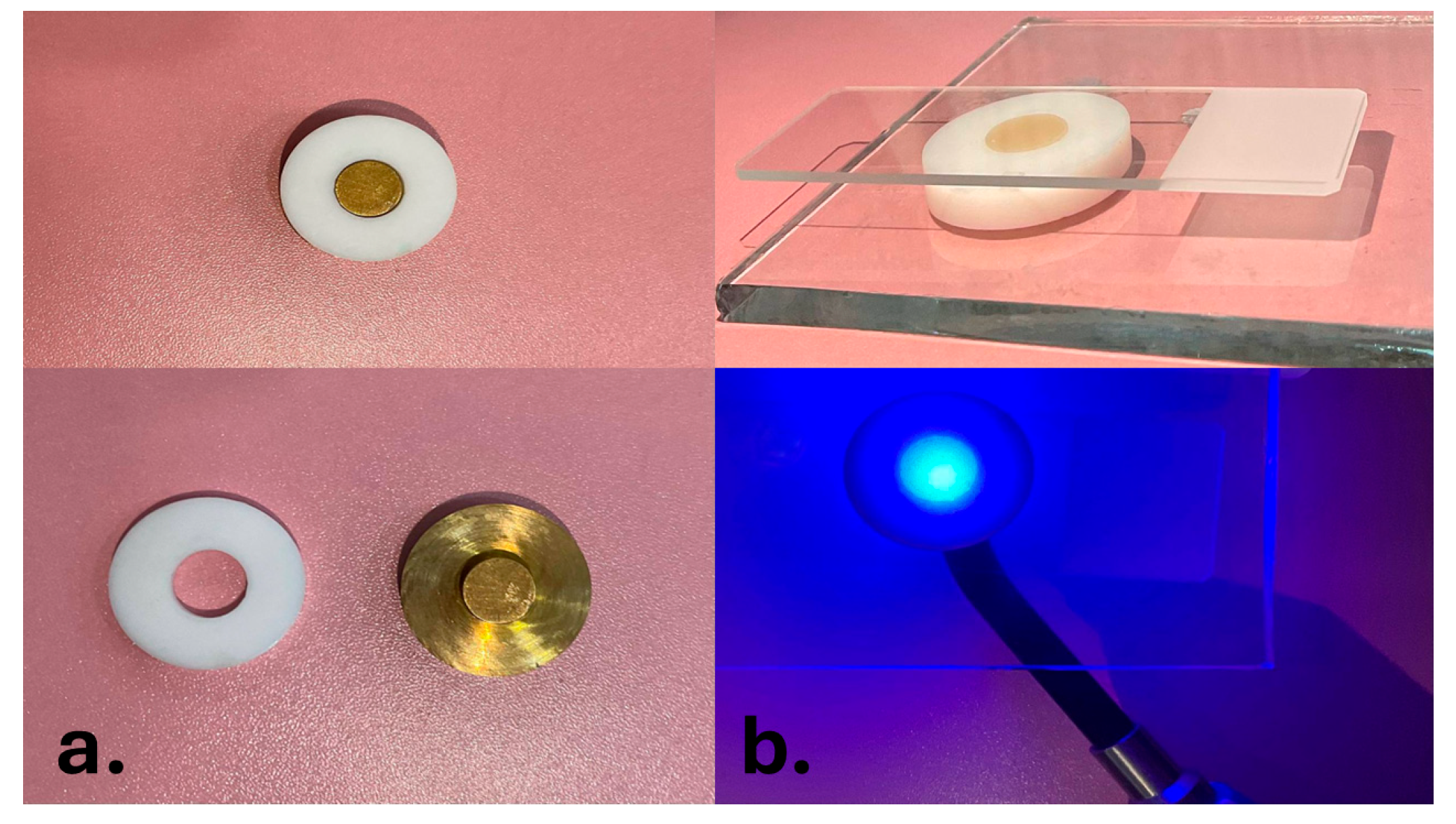
2.1. Preparation of Samples
2.2. Bleaching Technique
2.3. Measuring the Surface Roughness
2.4. Statistical Analysis
3. Results
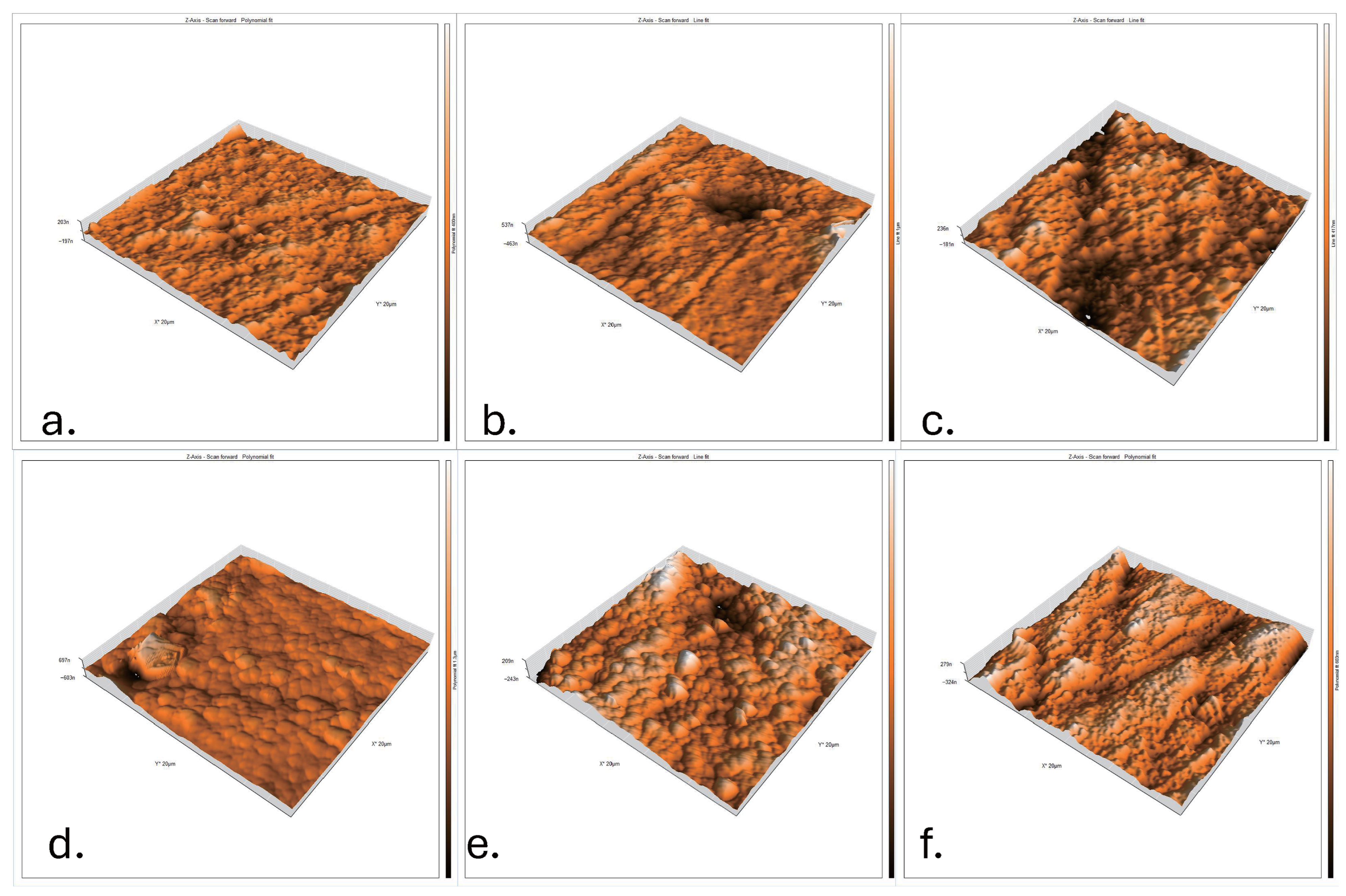
- (a)
- N1: Untreated nanohybrid composite surface showing a smooth and compact topography with minimal irregularities.
- (b)
- N2: Nanohybrid composite after zoom bleaching, with moderate roughness and irregular elevations/depressions indicating resin matrix alteration.
- (c)
- N3: Nanohybrid composite after laser bleaching, exhibiting pronounced peaks and valleys with extensive surface degradation.
- (d)
- M1: Control microhybrid composite surface, relatively smooth but with more visible micro-filler particles compared to Nano Control.
- (e)
- M2: Microhybrid composite after zoom bleaching, showing higher roughness with exposed filler–matrix boundaries due to oxidative stress.
- (f)
- M3: Microhybrid composite after laser bleaching, presenting the most disrupted surface, severe heterogeneity, and significant elevation differences.
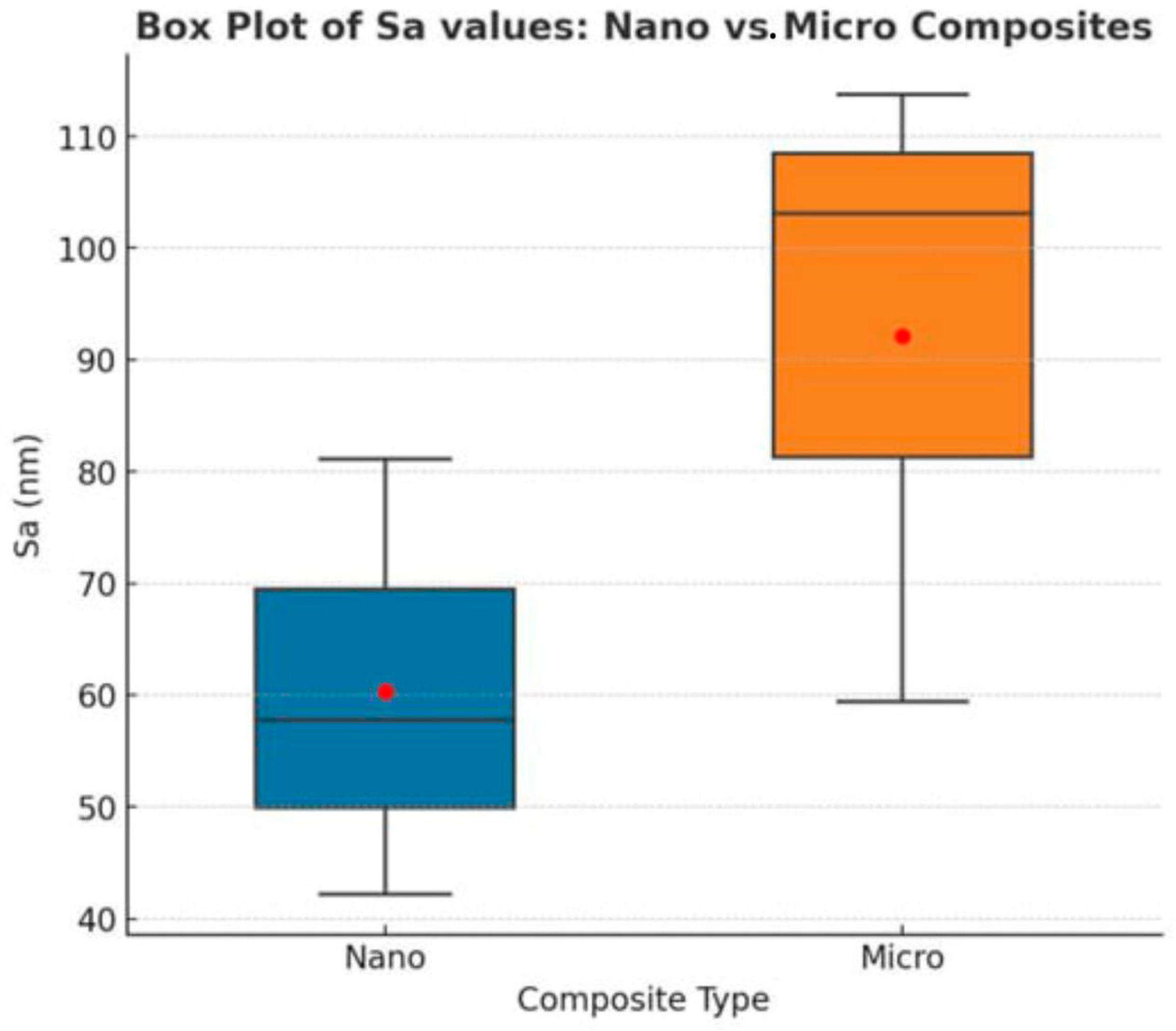
3.1. Micro- vs. Nano-Surface Roughness After Bleaching
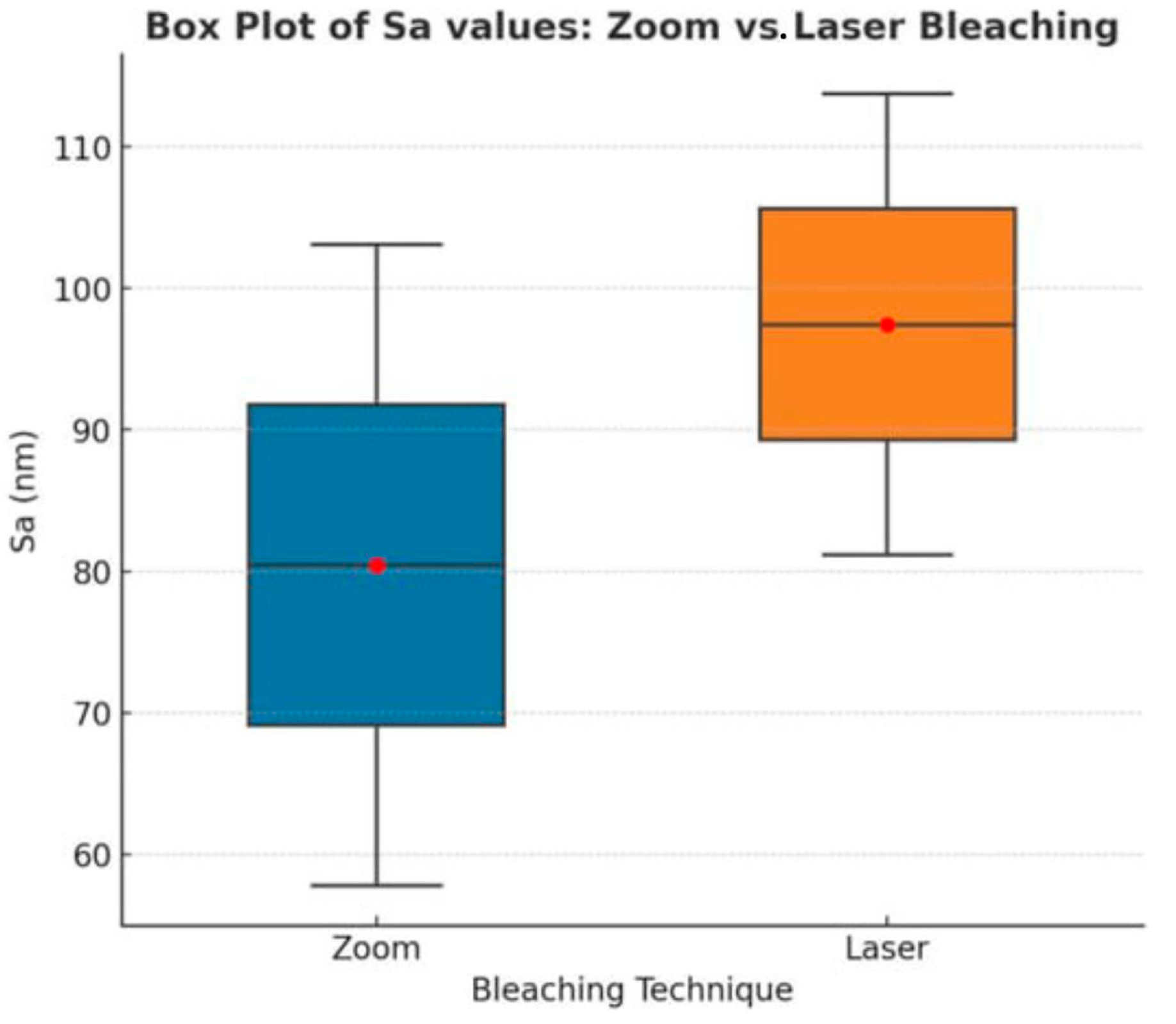
3.2. Zoom vs. Laser: Within-Group Roughness Comparison
4. Discussion
5. Conclusions
- -
- Both Zoom and laser bleaching increased composite surface roughness.
- -
- Laser bleaching produced more pronounced alterations overall.
- -
- Nanohybrid composites showed better resistance compared to microhybrid composites.
- -
- Clinical caution is advised: polishing after bleaching is recommended.
- -
- Findings are in vitro and should be validated in clinical settings.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Abbreviations
| AFM | Atomic Force Microscopy |
| CRD | Composite Resin Disk |
| Sa | Arithmetic Mean Height |
| Sq | Root Mean Square Height |
| Sz | Maximum Height |
| LED | Light-Emitting Diode |
| nm | Nanometer |
| µm | Micrometer |
| Bis-GMA | Bisphenol A-Glycidyl Methacrylate |
| TEGDMA | Triethylene Glycol Dimethacrylate |
| USA | United States of America |
References
- Bingül, A.; Nezir, M.; Atilla, A.O.; Özcan, S.; Evis, Z. A Review: Resin-Based Dental Materials and Their Characterization. Polym. Adv. Technol. 2025, 36, e70239. [Google Scholar] [CrossRef]
- Pratap, B.; Gupta, R.K.; Bhardwaj, B.; Nag, M. Resin based restorative dental materials: Characteristics and future perspectives. Jpn. Dent. Sci. Rev. 2019, 55, 126–138. [Google Scholar] [CrossRef]
- Habib, E.; Wang, R.; Wang, Y.; Zhu, M.; Zhu, X.X. Inorganic Fillers for Dental Resin Composites: Present and Future. ACS Biomater. Sci. Eng. 2016, 2, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Aktu, A.; Ulusoy, N. Effect of Polishing Systems on the Surface Roughness and Color Stability of Aged and Stained Bulk-Fill Resin Composites. Materials 2024, 17, 3576. [Google Scholar] [CrossRef]
- Hajdu, A.I.; Dumitrescu, R.; Balean, O.; Lalescu, D.V.; Buzatu, B.L.R.; Bolchis, V.; Floare, L.; Utu, D.; Jumanca, D.; Galuscan, A. Enhancing Esthetics in Direct Dental Resin Composite: Investigating Surface Roughness and Color Stability. J. Funct. Biomater. 2024, 15, 208. [Google Scholar] [CrossRef]
- Kreve, S.; Reis, A.C.D. Bacterial adhesion to biomaterials: What regulates this attachment? A review. Jpn. Dent. Sci. Rev. 2021, 57, 85–96. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Badr, C.; Spagnuolo, G.; Amenta, F.; Khairallah, C.; Mahdi, S.S.; Daher, E.; Battineni, G.; Baba, N.Z.; Zogheib, T.; Qasim, S.S.B.; et al. A Two-Year Comparative Evaluation of Clinical Performance of a Nanohybrid Composite Resin to a Flowable Composite Resin. J. Funct. Biomater. 2021, 12, 51. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Palaniappan, S.; Bharadwaj, D.; Mattar, D.L.; Peumans, M.; Van Meerbeek, B.; Lambrechts, P. Nanofilled and microhybrid composite restorations: Five-year clinical wear performances. Dent. Mater. 2011, 27, 692–700. [Google Scholar] [CrossRef] [PubMed]
- Angerame, D.; De Biasi, M. Do Nanofilled/Nanohybrid Composites Allow for Better Clinical Performance of Direct Restorations Than Traditional Microhybrid Composites? A Systematic Review. Oper. Dent. 2018, 43, E191–E209. [Google Scholar] [CrossRef] [PubMed]
- Popescu, A.D.; Tuculina, M.J.; Diaconu, O.A.; Gheorghiță, L.M.; Nicolicescu, C.; Cumpătă, C.N.; Petcu, C.; Abdul-Razzak, J.; Rîcă, A.M.; Voinea-Georgescu, R. Effects of Dental Bleaching Agents on the Surface Roughness of Dental Restoration Materials. Medicina 2023, 59, 1067. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Shafiei, F.; Doustfatemeh, S. Effect of a Combined Bleaching Regimen on the Microhardness of a Sealed Methacrylate-based and a Silorane-based Composite. J. Dent. 2013, 14, 111–117. [Google Scholar] [PubMed] [PubMed Central]
- Alkhuzaie, A.I.; Elawsya, M.E.; Elkholany, N.R. Impact of Different Bleaching Methods on Surface Roughness, Microhardness, and Tooth-Restoration Interface of Ormocer- and Methacrylate-based Restorative Systems. J. Clin. Exp. Dent. 2025, 17, e422–e431. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Boruga, M.; Tapalaga, G.; Luca, M.M.; Bumbu, B.A. Hydrogen Peroxide-Free Color Correctors for Tooth Whitening in Adolescents and Young Adults: A Systematic Review of In Vitro and Clinical Evidence. Dent. J. 2025, 13, 346. [Google Scholar] [CrossRef]
- Podulka, P. The Effect of Surface Topography Feature Size Density and Distribution on the Results of a Data Processing and Parameters Calculation with a Comparison of Regular Methods. Materials 2021, 14, 4077. [Google Scholar] [CrossRef]
- Saad, D.A.; Shatila, R.; Khazaal, G.; Abboud, M.; Kharouf, N.; Zogheib, C.M. The Effect of Dental Bleaching on Nanohybrid Composite Surface Roughness: A Comparative In Vitro Study of SEM and Profilometry. J. Compos. Sci. 2025, 9, 313. [Google Scholar] [CrossRef]
- Bahari, M.; Ebrahimi Chaharom, M.E.; Daneshpooy, M.; Gholizadeh, S.; Pashayi, H. Effect of bleaching protocols on surface roughness and biofilm formation on silorane-based composite resin. Dent. Res. J. 2019, 16, 264–270. [Google Scholar] [CrossRef]
- Pallarés-Serrano, A.; Pallarés-Serrano, A.; Pallarés-Serrano, S.; Pallarés-Sabater, A. Study of the Intra-Coronal Pressure Generated by Internal Bleaching Agents and Its Influence on Temporary Restoration. Appl. Sci. 2022, 12, 2799. [Google Scholar] [CrossRef]
- Elfakhri, F.; Alkahtani, R.; Li, C.; Khaliq, J. Influence of filler characteristics on the performance of dental composites: A comprehensive review. Ceram. Int. 2022, 48, 27280–27294. [Google Scholar] [CrossRef]
- Păstrav, M.; Păstrav, O.; Chisnoiu, A.M.; Chisnoiu, R.M.; Cuc, S.; Petean, I.; Saroși, C.; Feștilă, D. Properties of Nanohybrid Dental Composites—A Comparative In Vitro Study. Biomedicines 2024, 12, 243. [Google Scholar] [CrossRef] [PubMed]
- Aminoroaya, A.; Esmaeely Neisiany, R.; Nouri Khorasani, S.; Panahi, P.; Das, O.; Madry, H.; Cucchiarini, M.; Ramakrishna, S. A review of dental composites: Challenges, chemistry aspects, filler influences, and future insights. Compos. Part B-Eng. 2021, 216, 108852. [Google Scholar] [CrossRef]
- Markovic, L.; Jordan, R.A.; Glasser, M.C.; Arnold, W.H.; Nebel, J.; Tillmann, W.; Ostermann, T.; Zimmer, S. Effects of bleaching agents on surface roughness of filling materials. Dent. Mater. J. 2014, 33, 59–63. [Google Scholar] [CrossRef] [PubMed]
- Mierzejewska, Ż.A.; Łukaszuk, K.; Rusztyn, B.; Maliszewski, K. The Influence of Bleaching Intensity and Laser Activation on the Durability of Selected Aesthetic Composites—An In Vitro Study. J. Funct. Biomater. 2025, 16, 193. [Google Scholar] [CrossRef]
- Gottenbos, B.; de Witz, C.; Heintzmann, S.; Born, M.; Hötzl, S. Insights into blue light accelerated tooth whitening. Heliyon 2021, 7, e05913. [Google Scholar] [CrossRef] [PubMed]
- Arias-Herrera, S.; Sánchez-Martos, R.; Alfaro-Ochoa, L. Introduction to Diode Laser Therapies in Dentistry; IntechOpen: London, UK, 2024. [Google Scholar] [CrossRef]
- Sachelarie, L.; Cristea, R.; Burlui, E.; Hurjui, L.L. Laser Technology in Dentistry: From Clinical Applications to Future Innovations. Dent. J. 2024, 12, 420. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Dey, P.; Suprabha, B.S.; Suman, E.; Natarajan, S.; Shenoy, R.; Rao, A. Comparative evaluation of surface roughness and bacterial adhesion on two bioactive cements: An in-vitro study. BMC Oral Health 2024, 24, 1278. [Google Scholar] [CrossRef]

| Material Type | Name | Manufacturer | Composition/Specifications | Lot No. | Application Procedure |
|---|---|---|---|---|---|
| Composite Resin (Microhybrid) | HerculiteXRV (Microhybrid Composite) | Kerr Italia S.r.l., Salerno, Italy | Bis-GMA, TEGDMA, barium glass and silicon dioxide fillers, additives, stabilizers, catalysts | 11,023,474 | Fabricated into 10 × 4 mm disks; light-cured 20 s per side with LED unit; finished/polished before testing |
| Composite Resin (Nanohybrid) | HerculiteUltra (Nanohybrid Composite) | Kerr Corporation, Orange, CA, USA (or Kerr Italia S.r.l., Salerno, Italy) | Bis-GMA, TEGDMA, prepolymerized filler, silica nanofiller (20–50 nm), barium submicron fillers (0.6 µm), TiO2, pigments | 11,023,471 | Same as above |
| Bleaching Agent (Light-activated) | Zoom Gel 40% HP | Philips Oral Healthcare, Bothell, WA, USA | Hydrogen peroxide 40% concentration | 3,402,981 | Apply ~2–3 mm layer; activate with Zoom LED for 15 min; remove gel; repeat ×3 with 1 min intervals; rinse and dry (per IFU) |
| Bleaching Agent (Laser-activated) | QuickLase Gel 35% HP | QuickLase Ltd., Canterbury, Kent, UK | Hydrogen peroxide 35% concentration; vehicle (water/glycerin), thickener, stabilizers/buffer | 101,101 | Apply ~2–3 mm layer; activate with 940 nm diode laser for two cycles × 30 s; leave gel ~8 min after second cycle; suction, rinse and dry (per IFU) |
| Group | Sa Mean | Sa SD | Sa SE |
|---|---|---|---|
| N1 | 42.18 | 6.62 | 2.09 |
| N2 | 57.77 | 13.88 | 4.39 |
| N3 | 81.15 | 22.06 | 6.98 |
| M1 | 59.43 | 9.33 | 2.95 |
| M2 | 103.12 | 19.25 | 6.09 |
| M3 | 113.74 | 36.16 | 11.43 |
| Groups | N | Mean | Std. Deviation | Test Value | p-Value | |
|---|---|---|---|---|---|---|
| Zoom | Nano | 10 | 57.7720 | 13.87759 | 6.042 | 0.0001 ** |
| Micro | 10 | 103.1150 | 19.25045 | |||
| Laser | Nano | 10 | 78.1270 | 23.29051 | 2.583 | 0.019 * |
| Micro | 10 | 106.1600 | 25.21317 | |||
| Groups | N | Mean | Std. Deviation | Test Value | p-Value | |
|---|---|---|---|---|---|---|
| Nano | Zoom | 10 | 57.7720 | 13.87759 | 2.374 | 0.032 * |
| Laser | 10 | 78.1270 | 23.29051 | |||
| Micro | Zoom | 10 | 103.1150 | 19.25045 | 0.304 | 0.765 |
| Laser | 10 | 106.1600 | 25.21317 | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fadhil, K.; Amin, B.K. Effect of Bleaching on the Surface Roughness of Resin Composites Evaluated by Atomic Force Microscopy (AFM). Dent. J. 2025, 13, 470. https://doi.org/10.3390/dj13100470
Fadhil K, Amin BK. Effect of Bleaching on the Surface Roughness of Resin Composites Evaluated by Atomic Force Microscopy (AFM). Dentistry Journal. 2025; 13(10):470. https://doi.org/10.3390/dj13100470
Chicago/Turabian StyleFadhil, Kabas, and Bassam Karem Amin. 2025. "Effect of Bleaching on the Surface Roughness of Resin Composites Evaluated by Atomic Force Microscopy (AFM)" Dentistry Journal 13, no. 10: 470. https://doi.org/10.3390/dj13100470
APA StyleFadhil, K., & Amin, B. K. (2025). Effect of Bleaching on the Surface Roughness of Resin Composites Evaluated by Atomic Force Microscopy (AFM). Dentistry Journal, 13(10), 470. https://doi.org/10.3390/dj13100470






