Comparison of Aesthetic, Mechanical Outcome, and Bone Loss in Angulated Screw Channels (ASCs) and Cement-Retained Implant-Supported Prosthesis: A Case-Control Study
Abstract
1. Introduction
2. Materials and Methods
- Patients that had received a single implant restoration cemented on stock abutments or screw-retained employing ASC.
- Implant positioned in the posterior area (premolars to molars)
- Restorations cemented on custom abutments.
- Patients that had undergone previous radiotherapy to the facial district, suffered from diseases, or were under treatment with drugs that could impair bone metabolism. (i.e., bisphosphonates)
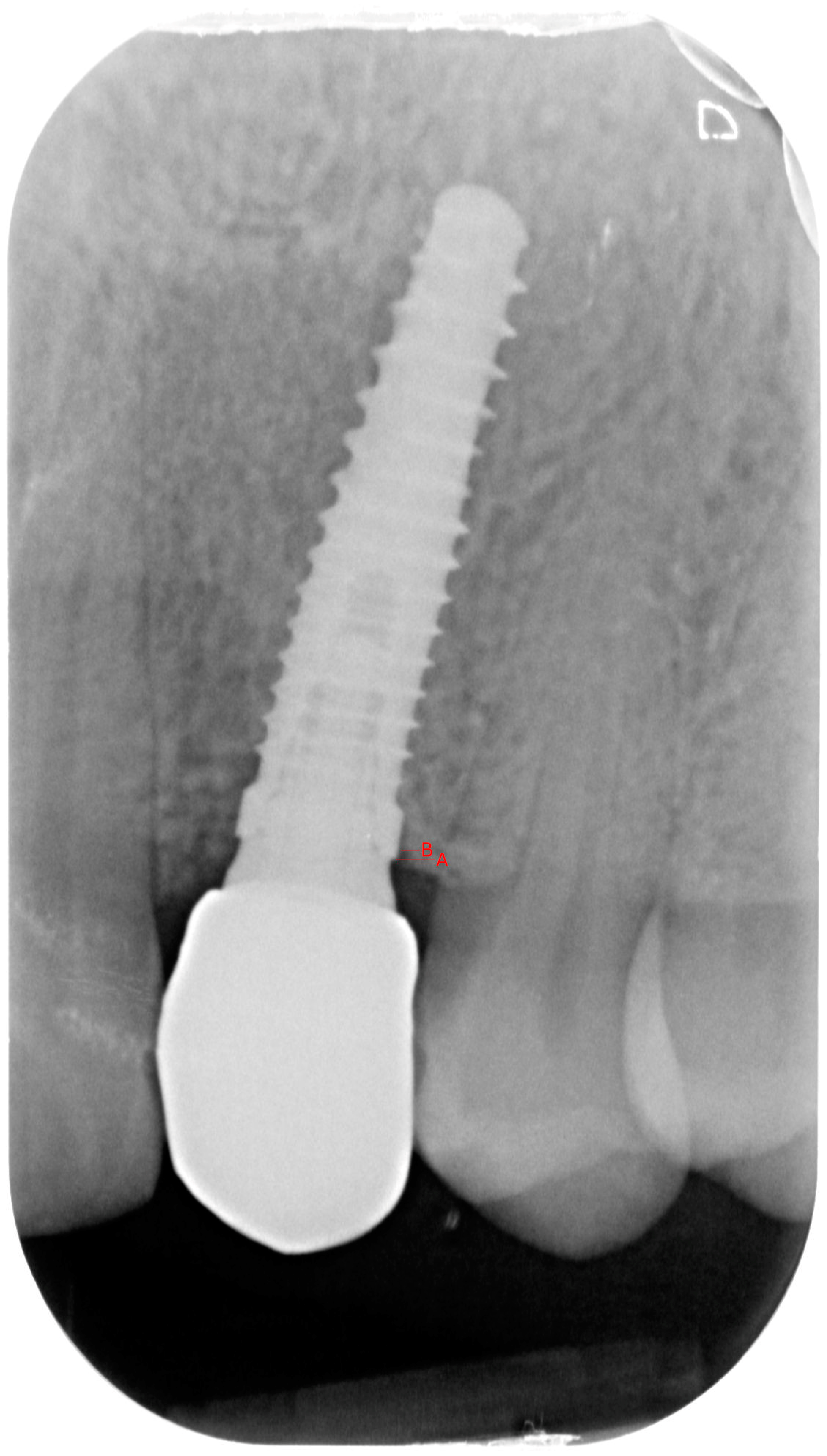
- Group 1: An implant-level impression adopting an open-tray impression technique was adopted using a polyvinylsiloxane impression material. After pouring the cast, an angled abutment was chosen, and a partially-veneered zirconia crown (limiting the veneering process to the vestibular surface) was obtained. At a second appointment, the abutment was screwed to the implant, and the crown was checked following the CMO (contact, margins, occlusion) acronym. The abutment was then manually screwed to the implant and secured at 25 Ncm. The access hole was closed with Teflon tape, and the crown was cemented with glass ionomer cement. (FujiCem 1, GC Europe, Leuven, Belgium) (Figure 1 and Figure 2).
- Group 2: An implant-level impression adopting an open-tray impression technique was adopted using a polyvinylsiloxane impression material. After pouring the cast, a T-Base for ASCs was chosen, and a partially-veneered zirconia crown (limiting the veneering process to the vestibular surface) was realized. An angulated screw channel was designed, moving the access hole to the occlusal/lingual surface. At a second appointment, the crown was screwed to the implant and checked following the CMO (contact, margins, occlusion) acronym. The crown was then manually screwed to the implant and secured at 25 Ncm. The access hole was closed with Teflon tape and flowable composite resin. (Figure 3 and Figure 4).
- PES: The PES comprises the following five variables: the mesial papilla, the distal papilla, the curvature of the facial mucosa, the level of the facial mucosa, and soft tissue color and texture at the facial aspect of the implant site. A score of 2, 1, or 0 is assigned to all five PES parameters. The two papillary ratings (one for the mesial and one for the distal) are used to evaluate the extent of papillary tissue present, with a full papilla receiving a score of 2, a partial papilla receiving a score of 1, and a complete absence receiving a score of 0. The contour of the facial soft tissue line, which is also known as the point where the implant restoration emerges from the soft tissues, is assessed for its similarity to a natural control tooth. It is rated as nearly identical (score 2), slightly different (score 1), or significantly different (score 0), determining whether it creates a natural and balanced appearance or a less harmonious one.
- 2.
- WES: The WES concentrates specifically on the visible section of the restoration, referring to the implant crown emerging from the peri-implant mucosa. This evaluation is based on five key parameters: the overall shape of the tooth, the contour and size of the clinical crown, color evaluation encompassing hue and value, surface texture, and translucency with characterization. Each of the five parameters is given a score of 2, 1, or 0. Therefore, in the case of an ideal implant restoration, a maximum WES score of 10 is attained. These parameters are evaluated by directly comparing them with the natural, opposing tooth, determining the degree of similarity or any possible differences. If the esthetic aspects of the reference tooth are optimally replicated, a perfect WES score of 10 can be achieved. The accepted clinical threshold remains at a score of 6.
Statistical Analysis
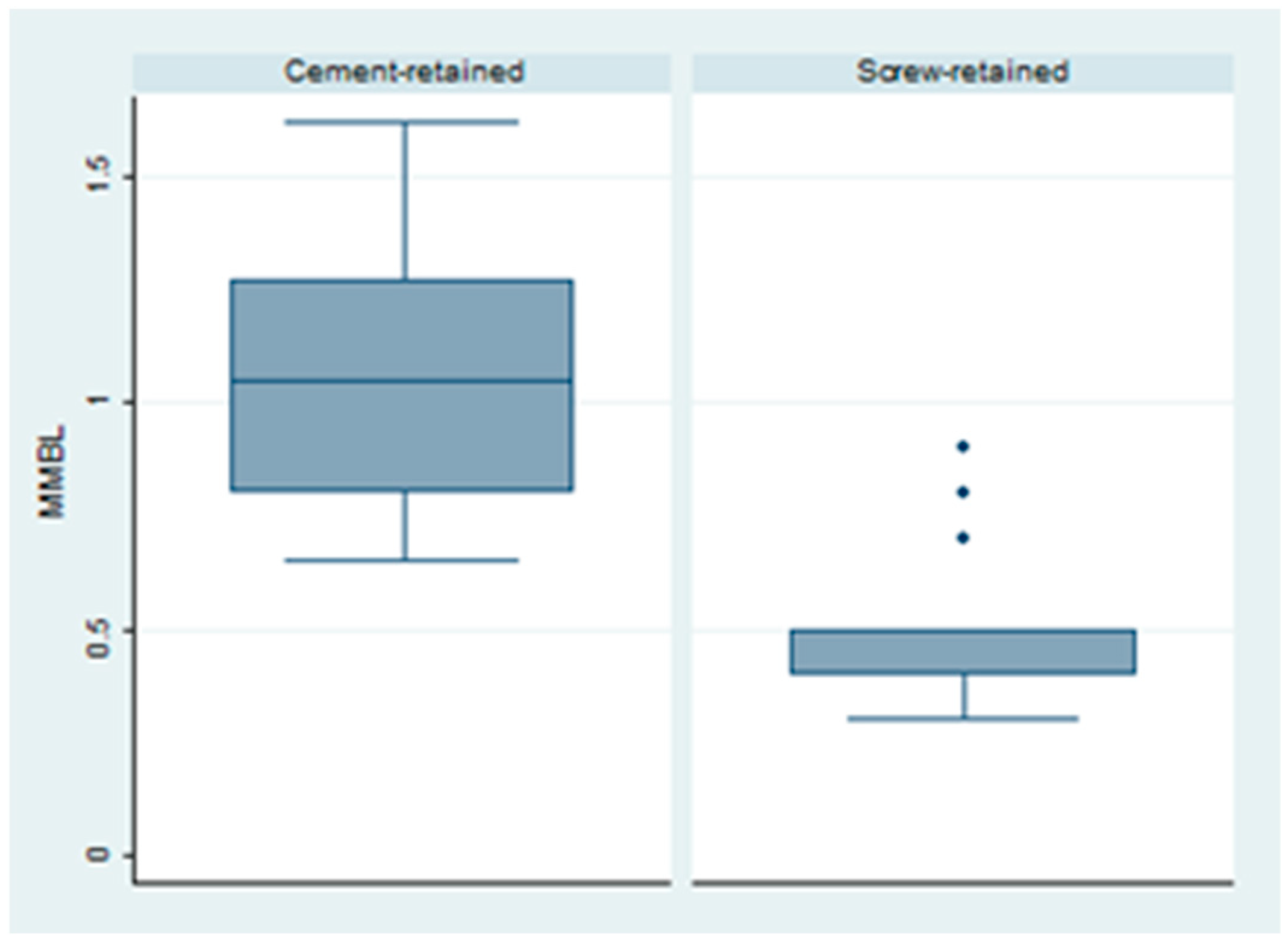
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Morton, D.; Gallucci, G.; Lin, W.-S.; Pjetursson, B.; Polido, W.; Roehling, S.; Sailer, I.; Aghaloo, T.; Albera, H.; Bohner, L.; et al. Group 2 ITI Consensus Report: Prosthodontics and Implant Dentistry. Clin. Oral Implant. Res. 2018, 29 (Suppl. 16), 215–223. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.-G.; Millen, C.; Brägger, U. Clinical Performance of Screw- versus Cement-Retained Fixed Implant-Supported Reconstructions—A Systematic Review. Int. J. Oral Maxillofac. Implant. 2014, 29, 84–98. [Google Scholar] [CrossRef] [PubMed]
- Sailer, I.; Mühlemann, S.; Zwahlen, M.; Hämmerle, C.H.F.; Schneider, D. Cemented and Screw-Retained Implant Reconstructions: A Systematic Review of the Survival and Complication Rates. Clin. Oral Implant. Res. 2012, 23, 163–201. [Google Scholar] [CrossRef]
- Kraus, R.D.; Epprecht, A.; Hämmerle, C.H.F.; Sailer, I.; Thoma, D.S. Cemented vs. Screw-Retained Zirconia-Based Single Implant Reconstructions: A 3-Year Prospective Randomized Controlled Clinical Trial. Clin. Implant. Dent. Relat. Res. 2019, 21, 578–585. [Google Scholar] [CrossRef] [PubMed]
- Manicone, P.F.; De Angelis, P.; Rella, E.; Papetti, L.; D’Addona, A. Proximal Contact Loss in Implant-Supported Restorations: A Systematic Review and Meta-Analysis of Prevalence. J. Prosthodont. 2022, 31, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Sinjari, B.; D’Addazio, G.; Traini, T.; Varvara, G.; Scarano, A.; Murmura, G.; Caputi, S. A 10-Year Retrospective Comparative Human Study on Screw-Retained versus Cemented Dental Implant Abutments. J. Biol. Regul. Homeost. Agents 2019, 33, 787–797. [Google Scholar] [PubMed]
- Edmondson, E.K.; Trejo, P.M.; Soldatos, N.; Weltman, R.L. The Ability to Screw-Retain Single Implant-Supported Restorations in the Anterior Maxilla: A CBCT Analysis. J. Prosthet. Dent. 2022, 128, 443–449. [Google Scholar] [CrossRef] [PubMed]
- Grassi, A.; Monica, D.; Minetti, E.; Ballini, A.; Gianfreda, F.; Bollero, P.; Cicciù, M.; Mastrangelo, F. Innovative Alveolar Ridge Preservation Surgical Technique with Immediate Dental Implant Placement: A Retrospective Case Report of 1-Year Follow-Up. Eur. J. Dent. 2024, 18, 408–414. [Google Scholar] [CrossRef]
- Maceiras, L.; Liñares, A.; Nóvoa, L.; Batalla, P.; Mareque, S.; Pérez, J.; Blanco, J. Marginal Changes at Bone-Level Implants Supporting Fixed Screw-Retained Partial Implant Prostheses with or without Intermediate Standardised Abutments: 1-Year Results of a Randomised Controlled Clinical Trial. Clin. Oral Implants Res. 2023, 34, 263–274. [Google Scholar] [CrossRef]
- Sakamoto, S.; Ro, M.; Al-Ardah, A.; Goodacre, C. Esthetic Abutment Design for Angulated Screw Channels: A Technical Report. J. Prosthet. Dent. 2018, 119, 912–915. [Google Scholar] [CrossRef]
- Gianfreda, F.; Bollero, P. Dental Materials Design and Innovative Treatment Approach. Dent. J. 2023, 11, 85. [Google Scholar] [CrossRef] [PubMed]
- Farré-Berga, O.; Cercadillo-Ibarguren, I.; Sánchez-Torres, A.; Domènech-Mestres, C.; Gil, F.J.; Escuin, T.; Berástegui, E. Novel Ball Head Screw and Screwdriver Design for Implant-Supported Prostheses with Angled Channels: A Finite Element Analysis. J. Oral Implantol. 2018, 44, 416–422. [Google Scholar] [CrossRef] [PubMed]
- Hu, E.; Petrich, A.; Imamura, G.; Hamlin, C. Effect of Screw Channel Angulation on Reverse Torque Values of Dental Implant Abutment Screws. J. Prosthodont. 2019, 28, 969–972. [Google Scholar] [CrossRef] [PubMed]
- Farré-Berga, O.; Cercadillo-Ibarguren, I.; Sánchez-Torres, A.; Gil, F.J.; Escuin, T.; Berástegui, E. Torsion Resistance of the Ball Head System Screw and Screwdriver for Angled Screw Channels on Implant Prosthetics. J. Oral Implantol. 2020, 46, 365–371. [Google Scholar] [CrossRef] [PubMed]
- Opler, R.; Wadhwani, C.; Chung, K.-H. The Effect of Screwdriver Angle Variation on the Off-Axis Implant Abutment System and Hexalobular Screw. J. Prosthet. Dent. 2020, 123, 524–528. [Google Scholar] [CrossRef] [PubMed]
- Friberg, B.; Ahmadzai, M. A Prospective Study on Single Tooth Reconstructions Using Parallel Walled Implants with Internal Connection (NobelParallel CC) and Abutments with Angulated Screw Channels (ASC). Clin. Implant. Dent. Relat. Res. 2019, 21, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Pol, C.W.P.; Raghoebar, G.M.; Maragkou, Z.; Cune, M.S.; Meijer, H.J.A. Full-Zirconia Single-Tooth Molar Implant-Supported Restorations with Angulated Screw Channel Abutments: A 1-Year Prospective Case Series Study. Clin. Implant. Dent. Relat. Res. 2020, 22, 138–144. [Google Scholar] [CrossRef] [PubMed]
- Gianfreda, F.; Pesce, P.; Marcano, E.; Pistilli, V.; Bollero, P.; Canullo, L. Clinical Outcome of Fully Digital Workflow for Single-Implant-Supported Crowns: A calibrs Clinical Study. Dent. J. 2022, 10, 139. [Google Scholar] [CrossRef] [PubMed]
- Drew, A.; Randi, A.; DiPede, L.; Luke, A. Fracture Strength of Implant Screw-Retained All-Ceramic Crowns with the Use of the Angulated Screw Channel: A Pilot Study. Int. J. Periodontics Restor. Dent. 2020, 40, 245–252. [Google Scholar] [CrossRef]
- Rella, E.; De Angelis, P.; Damis, G.; D’Addona, A.; Manicone, P.F. The Application of Angulated Screw-Channels in Metal-Free, Implant-Supported Restorations: A Retrospective Survival Analysis. Materials 2021, 14, 7006. [Google Scholar] [CrossRef]
- Nothdurft, F.P.; Doppler, K.E.; Erdelt, K.J.; Knauber, A.W.; Pospiech, P.R. Fracture Behavior of Straight or Angulated Zirconia Implant Abutments Supporting Anterior Single Crowns. Clin. Oral Investig. 2011, 15, 157–163. [Google Scholar] [CrossRef]
- Thulasidas, S.; Givan, D.A.; Lemons, J.E.; O’Neal, S.J.; Ramp, L.C.; Liu, P.-R. Influence of Implant Angulation on the Fracture Resistance of Zirconia Abutments. J. Prosthodont. 2015, 24, 127–135. [Google Scholar] [CrossRef] [PubMed]
- Garcia-Hammaker, S.; Saglik, B.; Sierraalta, M.; Razzoog, M. Influence of Screw Channel Angulation on the Fracture Resistance of Zirconia Abutments: An In Vitro Study. J. Prosthodont. 2021, 30, 329–334. [Google Scholar] [CrossRef]
- Naveau, A.; Rignon-Bret, C.; Wulfman, C. Zirconia Abutments in the Anterior Region: A Systematic Review of Mechanical and Esthetic Outcomes. J. Prosthet. Dent. 2019, 121, 775–781.e1. [Google Scholar] [CrossRef] [PubMed]
- Wittneben, J.-G.; Joda, T.; Weber, H.-P.; Brägger, U. Screw Retained vs. Cement Retained Implant-Supported Fixed Dental Prosthesis. Periodontology 2017, 73, 141–151. [Google Scholar] [CrossRef] [PubMed]
- Guarnieri, R.; Testarelli, L.; DeVilliers, P. Features of Peri-Implantitis Associated with Luting Cement Extrusion: A Histopathologic Report in Humans. Quintessence Int. 2020, 51, 398–404. [Google Scholar] [CrossRef]
- Anitua, E.; Fernández-de-Retana, S.; Alkhraisat, M.H. Survival and Marginal Bone Loss of Dental Implants Supporting Cad-Cam Angled Channel Restorations: A Split-Mouth Retrospective Study. Eur. J. Dent. 2020, 14, 194–199. [Google Scholar] [CrossRef]
- Jones, A.R.; Martin, W. Comparing Pink and White Esthetic Scores to Layperson Perception in the Single-Tooth Implant Patient. Int. J. Oral Maxillofac. Implants 2014, 29, 1348–1353. [Google Scholar] [CrossRef]
- Angelis, P.D.; Manicone, P.F.; Rosa, G.D.; Giorgi, A.D.; Liguori, M.G.; Cavalcanti, C.; D’Addona, A.; Rella, E. Clinical Outcomes of Conometric Retention for Implant-Supported Fixed Prostheses: A Systematic Review and Meta-Analysis. J. Prosthet. Dent. 2023; in press. [Google Scholar] [CrossRef]
- Millen, C.; Brägger, U.; Wittneben, J.-G. Influence of Prosthesis Type and Retention Mechanism on Complications with Fixed Implant-Supported Prostheses: A Systematic Review Applying Multivariate Analyses. Int. J. Oral Maxillofac. Implant. 2015, 30, 110–124. [Google Scholar] [CrossRef]
- Swamidass, R.S.; Kan, J.Y.K.; Kattadiyil, M.T.; Goodacre, C.J.; Lozada, J. Abutment Screw Torque Changes with Straight and Angled Screw-Access Channels. J. Prosthet. Dent. 2021, 125, 675–681. [Google Scholar] [CrossRef]
- Mulla, S.H.; Seghi, R.R.; Johnston, W.M.; Yilmaz, B. Effect of Cyclic Loading on Reverse Torque Values of Angled Screw Channel Systems. J. Prosthet. Dent. 2022, 128, 458–466. [Google Scholar] [CrossRef] [PubMed]
- Pitman, J.; Van Craenenbroeck, M.; Glibert, M.; Christiaens, V. Screw Loosening in Angulation-Correcting Single Implant Restorations: A Systematic Review of in Vitro Studies. J. Prosthet. Dent. 2022; online ahead of print. [Google Scholar] [CrossRef]
- Rasaie, V.; Abduo, J.; Falahchai, M. Clinical and Laboratory Outcomes of Angled Screw Channel Implant Prostheses: A Systematic Review. Eur. J. Dent. 2022, 16, 488–499. [Google Scholar] [CrossRef] [PubMed]
- Staubli, N.; Walter, C.; Schmidt, J.C.; Weiger, R.; Zitzmann, N.U. Excess Cement and the Risk of Peri-Implant Disease—A Systematic Review. Clin. Oral Implant. Res. 2017, 28, 1278–1290. [Google Scholar] [CrossRef] [PubMed]
- Yang, H.; Xu, L.; Jiang, J.; Xu, Y.; Li, X.; He, F. Clinical Effect of Nobel Biocare Angulated Screw Channel Crown Compared with Cement Crown in the Aesthetic Area: A Retrospective Cohort Study with a Mean 32 Months Follow-up (Range 12 to 70 Months). Clin. Implant. Dent. Relat. Res. 2023, 25, 1178–1186. [Google Scholar] [CrossRef]
- Lv, X.-L.; Qian, S.-J.; Qiao, S.-C.; Gu, Y.-X.; Lai, H.-C.; Shi, J.-Y. Clinical, Radiographic, and Immunological Evaluation of Angulated Screw-Retained and Cemented Single-Implant Crowns in the Esthetic Region: A 1-Year Randomized Controlled Clinical Trial. Clin. Implant. Dent. Relat. Res. 2021, 23, 692–702. [Google Scholar] [CrossRef]





Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rella, E.; De Angelis, P.; Papetti, L.; Damis, G.; Gasparini, G.; D’Addona, A.; Manicone, P.F. Comparison of Aesthetic, Mechanical Outcome, and Bone Loss in Angulated Screw Channels (ASCs) and Cement-Retained Implant-Supported Prosthesis: A Case-Control Study. Dent. J. 2024, 12, 233. https://doi.org/10.3390/dj12080233
Rella E, De Angelis P, Papetti L, Damis G, Gasparini G, D’Addona A, Manicone PF. Comparison of Aesthetic, Mechanical Outcome, and Bone Loss in Angulated Screw Channels (ASCs) and Cement-Retained Implant-Supported Prosthesis: A Case-Control Study. Dentistry Journal. 2024; 12(8):233. https://doi.org/10.3390/dj12080233
Chicago/Turabian StyleRella, Edoardo, Paolo De Angelis, Laura Papetti, Giovanni Damis, Giulio Gasparini, Antonio D’Addona, and Paolo Francesco Manicone. 2024. "Comparison of Aesthetic, Mechanical Outcome, and Bone Loss in Angulated Screw Channels (ASCs) and Cement-Retained Implant-Supported Prosthesis: A Case-Control Study" Dentistry Journal 12, no. 8: 233. https://doi.org/10.3390/dj12080233
APA StyleRella, E., De Angelis, P., Papetti, L., Damis, G., Gasparini, G., D’Addona, A., & Manicone, P. F. (2024). Comparison of Aesthetic, Mechanical Outcome, and Bone Loss in Angulated Screw Channels (ASCs) and Cement-Retained Implant-Supported Prosthesis: A Case-Control Study. Dentistry Journal, 12(8), 233. https://doi.org/10.3390/dj12080233







