Updates on Caries Risk Assessment—A Literature Review
Abstract
1. Introduction
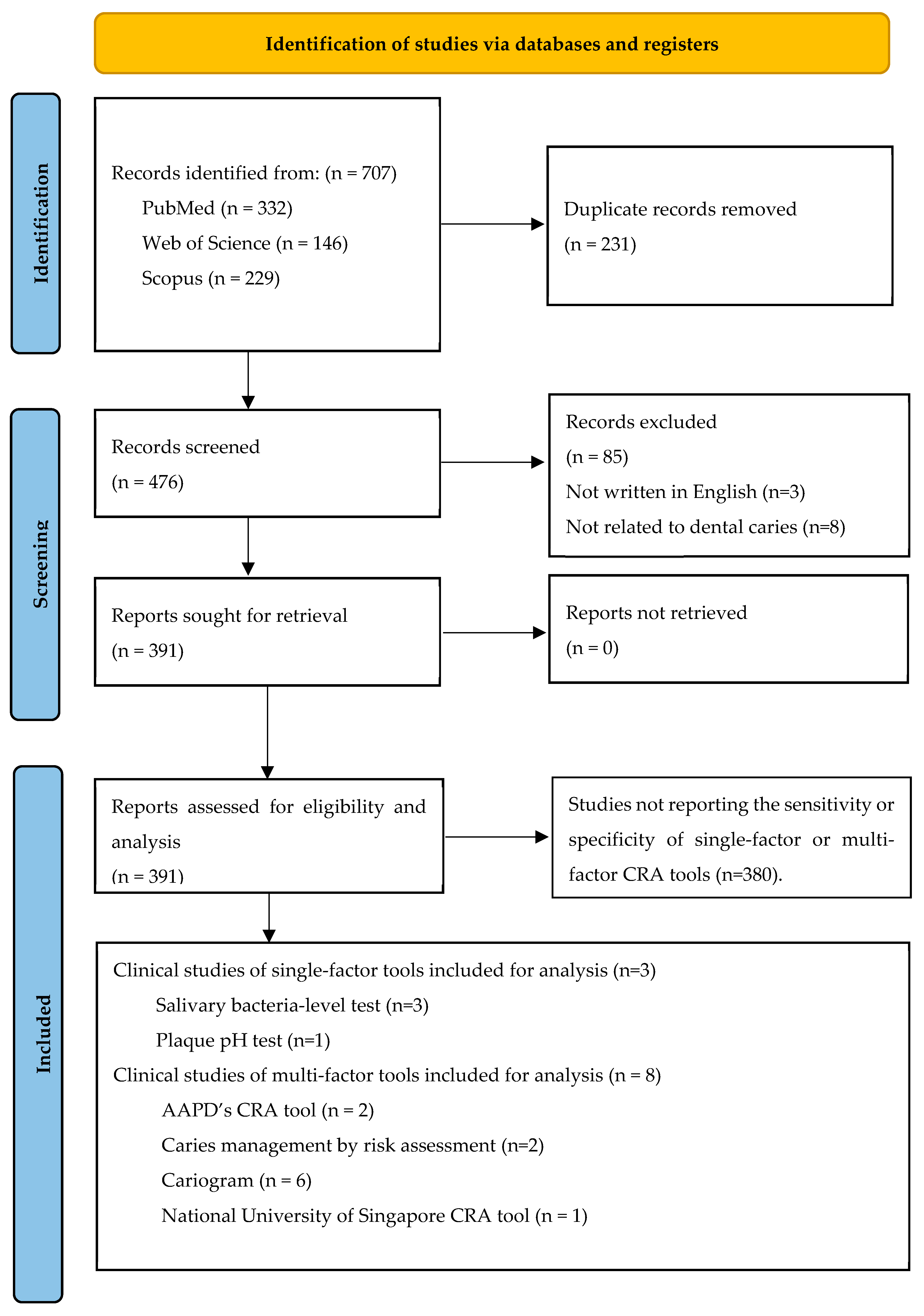
2. Literature Search
2.1. Search Strategy
2.2. Study Selection
2.3. Results
3. Factors Affecting Patients’ Caries Risk Levels
3.1. Risk Factors
3.1.1. Oral Environmental Risk Factors
Past Caries Experience
Salivary Streptococcus mutans (S. mutans) Level
Plaque pH
Malocclusion
Enamel Defects
3.1.2. Personal Behavior Factors
Diet
Maternal Conditions
3.1.3. Systemic Factors
Radiotherapy
Diabetes Mellitus
Sjögren’s Syndrome
Obesity
Stress
3.2. Protective Factors
3.2.1. Oral Environmental Protective Factors
Saliva
Fluoride
Chewing Gum
Probiotics
Dental Sealant
3.2.2. Systemic Protective Factors
Systemic Fluoride
4. Caries Risk Assessment (CRA) Tools
4.1. Single-Factor CRA Tools
4.1.1. Salivary Bacteria-Level Test
4.1.2. Salivary Property Test
4.1.3. Salivary Immunoglobulin Level
4.1.4. Plaque pH Test
4.2. Multiple-Factor CRA Tools
4.2.1. Form-Based CRA Tools
American Academy of Pediatric Dentistry’s Caries Risk Assessment Tool (AAPD-CAT)
American Dental Association’s Caries Risk Assessment Tool (ADA-CAT)
Caries Management by Risk Assessment (CAMBRA)
International Caries Classification and Management System (ICCMS™) and CariesCare International (CCI) System
4.2.2. Algorithm-Based CRA Tools
Cariogram
MySmileBuddy (MSB)
PreViser Risk Assessment Tool (PreViser)
National University of Singapore Caries Risk Assessment Tool (NUS-CRAT)
4.2.3. Accuracy of Multiple-Factor CRA Tools
5. Discussion
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Desai, H.; Stewart, C.A.; Finer, Y. Minimally Invasive Therapies for the Management of Dental Caries—A Literature Review. Dent. J. 2021, 9, 147. [Google Scholar] [CrossRef] [PubMed]
- Yon, M.J.Y.; Gao, S.S.; Chen, K.J.; Duangthip, D.; Lo, E.C.M.; Chu, C.H. Medical model in caries management. Dent. J. 2019, 7, 37. [Google Scholar] [CrossRef]
- Rechmann, P.; Chaffee, B.W.; Rechmann, B.M.T.; Featherstone, J.D.B. Changes in Caries Risk in a Practice-Based Randomized Controlled Trial. Adv. Dent. Res. 2018, 29, 15–23. [Google Scholar] [CrossRef] [PubMed]
- Aboubakr, R.M.; Alkhadragy, D.M.; Okda, M.; Rady, H.W.M.; Elnagar, R.M. Predictors of Caries Risk among Egyptian Children Attending Pediatric Dental Clinics at a University Hospital. Saudi J. Med. Med. Sci. 2023, 11, 219–228. [Google Scholar] [CrossRef] [PubMed]
- Almerich-Torres, T.; Montiel-Company, J.M.; Bellot-Arcís, C.; Iranzo-Cortés, J.E.; Ortolá-Siscar, J.C.; Almerich-Silla, J.M. Caries Prevalence Evolution and Risk Factors among Schoolchildren and Adolescents from Valencia (Spain): Trends 1998–2018. Int. J. Environ. Res Public Health 2020, 17, 6561. [Google Scholar] [CrossRef]
- Fontana, M. The Clinical, Environmental, and Behavioral Factors That Foster Early Childhood Caries: Evidence for Caries Risk Assessment. Pediatr. Dent. 2015, 37, 217–225. [Google Scholar]
- American Academy of Pediatric, D. Caries-risk Assessment and Management for Infants, Children, and Adolescents. Pediatr. Dent. 2018, 40, 205–212. [Google Scholar]
- Pitts, N.B.; Ekstrand, K.R. International Caries Detection and Assessment System (ICDAS) and its International Caries Classification and Management System (ICCMS)—Methods for staging of the caries process and enabling dentists to manage caries. Community Dent. Oral Epidemiol. 2013, 41, e41–e52. [Google Scholar] [CrossRef]
- Featherstone, J.D.B.; Crystal, Y.O.; Alston, P.; Chaffee, B.W.; Doméjean, S.; Rechmann, P.; Zhan, L.; Ramos-Gomez, F. A Comparison of Four Caries Risk Assessment Methods. Front. Oral Health 2021, 2, 656558. [Google Scholar] [CrossRef]
- Ndagire, B.; Muwazi, L.; Nabaggala, G.S.; Kutesa, A.; Rwenyonyi, C.M. Dental Practitioners’ Knowledge, Attitude, and Practice in Caries Risk Assessment and Management: A Cross-sectional Survey in Kampala Metropolitan, Uganda. J. Contemp. Dent. Pract. 2021, 22, 1377–1385. [Google Scholar] [CrossRef]
- Fang, X.; Hua, F.; Chen, Z.; Zhang, L. Caries risk assessment-related knowledge, attitude, and behaviors among Chinese dentists: A cross-sectional survey. Clin. Oral Investig. 2023, 27, 1079–1087. [Google Scholar] [CrossRef] [PubMed]
- Strickland, M.; Duda, P.; Merdad, H.E.; Pelaez-Shelton, R.E.; Rosivack, R.G.; Markowitz, K. The clinical performance of chairside caries risk assessment kits. Quintessence Int. 2017, 48, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Voelker, M.A.; Bray, K.S.; Elledge, S.A.; Sutton, J.; Scott, J.M. Effectiveness of an Antigen-Specific Streptococcus mutans Chairside Test as Compared to a Culture-Based S. mutans Test. J. Dent. Hyg. 2018, 92, 51–56. [Google Scholar]
- Babu, V.; Hegde, K.S.; Bhat, S.; Sargod, S. Evaluation of Efficacy of Three Different Commercially Available Kit for Chairside Cariogenic Bacteria Test—Caries Risk Test, Saliva-check Mutans and CariScreen. Cureus J. Med. Sci. 2019, 11, e6504. [Google Scholar] [CrossRef]
- Gao, X.; Di Wu, I.; Lo, E.C.; Chu, C.H.; Hsu, C.Y.; Wong, M.C. Validity of caries risk assessment programmes in preschool children. J. Dent. 2013, 41, 787–795. [Google Scholar] [CrossRef] [PubMed]
- Agouropoulos, A.; Birpou, E.; Twetman, S.; Kavvadia, K. Caries risk assessment with the ‘Bangkok checklist’ in preschool children: A prospective cohort study. Int. J. Paediatr. Dent. 2022, 32, 82–89. [Google Scholar] [CrossRef]
- Sudhir, K.M.; Kanupuru, K.K.; Fareed, N.; Mahesh, P.; Vandana, K.; Chaitra, N.T. CAMBRA as a Tool for Caries Risk Prediction Among 12- to 13-year-old Institutionalised Children—A Longitudinal Follow-up Study. Oral Health Prev. Dent. 2016, 14, 355–362. [Google Scholar] [CrossRef]
- Petersson, G.H.; Twetman, S. Caries risk assessment in young adults: A 3 year validation of the Cariogram model. BMC Oral Health 2015, 15, 17. [Google Scholar] [CrossRef]
- Dou, L.; Luo, J.; Fu, X.; Tang, Y.; Gao, J.; Yang, D. The validity of caries risk assessment in young adults with past caries experience using a screening Cariogram model without saliva tests. Int. Dent. J. 2018, 68, 221–226. [Google Scholar] [CrossRef]
- Kim, J.M.; Choi, J.S.; Choi, Y.H.; Kim, H.E. Simplified Prediction Model for Accurate Assessment of Dental Caries Risk among Participants Aged 10–18 Years. Tohoku J. Exp. Med. 2018, 246, 81–86. [Google Scholar] [CrossRef]
- Birpou, E.; Agouropoulos, A.; Twetman, S.; Kavvadia, K. Validation of different Cariogram settings and factor combinations in preschool children from areas with high caries risk. Int. J. Paediatr. Dent. 2019, 29, 448–455. [Google Scholar] [CrossRef] [PubMed]
- Dolic, O.; Obradovic, M.; Kojic, Z.; Trtic, N.; Sukara, S.; Knezevic, N.; Veselinovic, V. Validation of Cariogram in Caries Prediction in Women and Their Children 4 Years after Pregnancy—Longitudinal Study. Risk Manag. Healthc. Policy 2020, 13, 549–557. [Google Scholar] [CrossRef] [PubMed]
- Twetman, S.; Fontana, M.; Featherstone, J.D. Risk assessment—Can we achieve consensus? Community Dent. Oral Epidemiol. 2013, 41, e64–e70. [Google Scholar] [CrossRef]
- Mejàre, I.; Axelsson, S.; Dahlén, G.; Espelid, I.; Norlund, A.; Tranæus, S.; Twetman, S. Caries risk assessment. A systematic review. Acta Odontol. Scand. 2014, 72, 81–91. [Google Scholar] [CrossRef]
- Lin, Y.T.; Chou, C.C.; Lin, Y.J. Caries experience between primary teeth at 3–5 years of age and future caries in the permanent first molars. J. Dent. Sci. 2021, 16, 899–904. [Google Scholar] [CrossRef] [PubMed]
- Zemaitiene, M.; Grigalauskiene, R.; Andruskeviciene, V.; Matulaitiene, Z.K.; Zubiene, J.; Narbutaite, J.; Slabsinskiene, E. Dental caries risk indicators in early childhood and their association with caries polarization in adolescence: A cross-sectional study. BMC Oral Health 2016, 17, 2. [Google Scholar] [CrossRef]
- Fernando, S.; Kumar, S.; Bakr, M.; Speicher, D.; Lea, R.; Scuffham, P.A.; Johnson, N.W. Children’s untreated decay is positively associated with past caries experience and with current salivary loads of mutans Streptococci; negatively with self-reported maternal iron supplements during pregnancy: A multifactorial analysis. J. Public Health Dent. 2019, 79, 109–115. [Google Scholar] [CrossRef]
- Edelstein, B.L.; Ureles, S.D.; Smaldone, A. Very High Salivary Streptococcus mutans Predicts Caries Progression in Young Children. Pediatr. Dent. 2016, 38, 325–330. [Google Scholar]
- Gliosca, L.A.; Stoppani, N.; Lamas, N.S.; Balsamo, C.; Salgado, P.A.; Argentieri, Á.B.; D’Eramo, L.; Squassi, A.F.; Molgatini, S.L. Validation of an adherence assay to detect group mutans streptococci in saliva samples. Acta Odontol. Latinoam. 2019, 32, 97–102. [Google Scholar]
- Lee, H.S.; Lee, E.S.; Kang, S.M.; Lee, J.H.; Choi, H.J.; Kim, B.I. Clinical Assessment of a New Caries Activity Test Using Dental Plaque Acidogenicity in Children under Three Years of Age. J. Clin. Pediatr. Dent. 2016, 40, 388–392. [Google Scholar] [CrossRef]
- Aranibar Quiroz, E.M.; Alstad, T.; Campus, G.; Birkhed, D.; Lingström, P. Relationship between plaque pH and different caries-associated variables in a group of adolescents with varying caries prevalence. Caries Res. 2014, 48, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Sá-Pinto, A.C.; Rego, T.M.; Marques, L.S.; Martins, C.C.; Ramos-Jorge, M.L.; Ramos-Jorge, J. Association between malocclusion and dental caries in adolescents: A systematic review and meta-analysis. Eur. Arch. Paediatr. Dent. 2018, 19, 73–82. [Google Scholar] [CrossRef] [PubMed]
- Macey, R.; Thiruvenkatachari, B.; O’Brien, K.; Batista, K. Do malocclusion and orthodontic treatment impact oral health? A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2020, 157, 738–744.e710. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Chen, X.; Chen, S.; Janal, M.N.; Sarnat, H. Developmental defects of enamel increase caries susceptibility in Chinese preschool children. Community Dent. Oral Epidemiol. 2018, 46, 500–510. [Google Scholar] [CrossRef]
- Kirthiga, M.; Murugan, M.; Saikia, A.; Kirubakaran, R. Risk Factors for Early Childhood Caries: A Systematic Review and Meta-Analysis of Case Control and Cohort Studies. Pediatr. Dent. 2019, 41, 95–112. [Google Scholar]
- Castaneda-Sarmiento, S.; Koecklin, K.H.U.; Hernandez, M.B.B.; Santos, G.P.; Luyo, J.C.B.; Sotomayor, J.C.S.; Ruiz-Yasuda, C.; Apaza, Z.R.; Adasme, D.P.; Ricse, D.A.T.; et al. Association between developmental defects of enamel and early childhood caries in children under 6 years old: A systematic review and meta-analysis. Heliyon 2022, 8, e10479. [Google Scholar] [CrossRef]
- Olczak-Kowalczyk, D.; Gozdowski, D.; Turska-Szybka, A. Protective Factors for Early Childhood Caries in 3-Year-Old Children in Poland. Front. Pediatr. 2021, 9, 583660. [Google Scholar] [CrossRef]
- Evans, E.W.; Hayes, C.; Palmer, C.A.; Bermudez, O.I.; Cohen, S.A.; Must, A. Dietary intake and severe early childhood caries in low-income, young children. J. Acad. Nutr. Diet. 2013, 113, 1057–1061. [Google Scholar] [CrossRef]
- Bernabé, E.; Vehkalahti, M.M.; Sheiham, A.; Aromaa, A.; Suominen, A.L. Sugar-sweetened beverages and dental caries in adults: A 4-year prospective study. J. Dent. 2014, 42, 952–958. [Google Scholar] [CrossRef]
- Khan, S.; Javed, F.; Ebadi, M.; Schroth, R. Prevalence and risk factors for ECC among preschool children from India along with the need of its own CRA tool—A systematic review. J. Int. Soc. Prev. Community Dent. 2022, 12, 295–308. [Google Scholar] [CrossRef]
- Nakayama, Y.; Mori, M. Association of environmental tobacco smoke and snacking habits with the risk of early childhood caries among 3-year-old Japanese children. J. Public Health Dent. 2015, 75, 157–162. [Google Scholar] [CrossRef] [PubMed]
- Andrysiak-Karmińska, K.; Hoffmann-Przybylska, A.; Przybylski, P.; Witkowska, Z.; Walicka, E.; Borysewicz-Lewicka, M.; Gregorczyk-Maga, I.; Rahnama, M.; Gerreth, K.; Opydo-Szymaczek, J. Factors Affecting Dental Caries Experience in 12-Year-Olds, Based on Data from Two Polish Provinces. Nutrients 2022, 14, 1948. [Google Scholar] [CrossRef] [PubMed]
- Valenzuela, M.J.; Waterhouse, B.; Aggarwal, V.R.; Bloor, K.; Doran, T. Effect of sugar-sweetened beverages on oral health: A systematic review and meta-analysis. Eur. J. Public Health 2021, 31, 122–129. [Google Scholar] [CrossRef] [PubMed]
- Pinto, G.D.S.; Azevedo, M.S.; Goettems, M.L.; Correa, M.B.; Pinheiro, R.T.; Demarco, F.F. Are Maternal Factors Predictors for Early Childhood Caries? Results from a Cohort in Southern Brazil. Braz. Dent. J. 2017, 28, 391–397. [Google Scholar] [CrossRef] [PubMed]
- Priyadarshini, H.R.; Fernandes, B.A.; Hiremath, S.S.; Rath, A.; Shivakumar, V.; Tegginamani, A.S. Assessment of maternal risk indicators for the development of caries in their children: A comparative, cross-sectional study. J. Indian. Soc. Pedod. Prev. Dent. 2017, 35, 110–114. [Google Scholar] [CrossRef]
- Majorana, A.; Cagetti, M.G.; Bardellini, E.; Amadori, F.; Conti, G.; Strohmenger, L.; Campus, G. Feeding and smoking habits as cumulative risk factors for early childhood caries in toddlers, after adjustment for several behavioral determinants: A retrospective study. BMC Pediatr. 2014, 14, 45. [Google Scholar] [CrossRef]
- Duruk, G.; Acar, B.; Temelli, Ö. Effect of different doses of radiation on morphogical, mechanical and chemical properties of primary and permanent teeth-an in vitro study. BMC Oral Health 2020, 20, 242. [Google Scholar] [CrossRef]
- Lu, H.; Zhao, Q.; Guo, J.; Zeng, B.; Yu, X.; Yu, D.; Zhao, W. Direct radiation-induced effects on dental hard tissue. Radiat. Oncol. 2019, 14, 5. [Google Scholar] [CrossRef] [PubMed]
- Deng, J.; Jackson, L.; Epstein, J.B.; Migliorati, C.A.; Murphy, B.A. Dental demineralization and caries in patients with head and neck cancer. Oral Oncol. 2015, 51, 824–831. [Google Scholar] [CrossRef]
- Noone, J.; Barclay, C. Head and Neck Cancer Patients—Information for the General Dental Practitioner. Dent. Update 2017, 44, 209–210, 213–215. [Google Scholar] [CrossRef][Green Version]
- Assiri, S.A.; El Meligy, O.A.; Alzain, I.O.; Bamashmous, N.O. Assessment of dental caries and salivary characteristics among type 1 diabetic Saudi children. J. Dent. Sci. 2022, 17, 1634–1639. [Google Scholar] [CrossRef] [PubMed]
- Coelho, A.S.; Amaro, I.F.; Caramelo, F.; Paula, A.; Marto, C.M.; Ferreira, M.M.; Botelho, M.F.; Carrilho, E.V. Dental caries, diabetes mellitus, metabolic control and diabetes duration: A systematic review and meta-analysis. J. Esthet. Restor. Dent. 2020, 32, 291–309. [Google Scholar] [CrossRef] [PubMed]
- Almusawi, M.A.; Gosadi, I.; Abidia, R.; Almasawi, M.; Khan, H.A. Potential risk factors for dental caries in Type 2 diabetic patients. Int. J. Dent. Hyg. 2018, 16, 467–475. [Google Scholar] [CrossRef] [PubMed]
- Berman, N.; Vivino, F.; Baker, J.; Dunham, J.; Pinto, A. Risk factors for caries development in primary Sjogren syndrome. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2019, 128, 117–122. [Google Scholar] [CrossRef]
- Hayden, C.; Bowler, J.O.; Chambers, S.; Freeman, R.; Humphris, G.; Richards, D.; Cecil, J.E. Obesity and dental caries in children: A systematic review and meta-analysis. Community Dent. Oral Epidemiol. 2013, 41, 289–308. [Google Scholar] [CrossRef]
- Hegde, S. Is there an association between body weight and early childhood caries experience? Evid. Based Dent. 2020, 21, 114–115. [Google Scholar] [CrossRef]
- Pereira, A.L.P.; Frias, A.C.; Hasegawa, C.C.T.; Ramos, D.V.R.; Rocha, A.L.; Bonfim, D. Assessment Between Dental Caries Index and Body Mass Index among Adults. Oral Health Prev. Dent. 2018, 16, 563–569. [Google Scholar] [CrossRef]
- Costacurta, M.; Di Renzo, L.; Sicuro, L.; Gratteri, S.; De Lorenzo, A.; Docimo, R. Dental caries and childhood obesity: Analysis of food intakes, lifestyle. Eur. J. Paediatr. Dent. 2014, 15, 343–348. [Google Scholar]
- Raj, A.; Kashyap, S.; Kundra, K.; Kandari, S.; Rela, R.; Naz, F. Correlation Between BMI, Caries Prevalence, and Sugar-containing Beverage Intake in 6–10 Year Old Children. J. Pharm. Bioallied Sci. 2022, 14, S991–S994. [Google Scholar] [CrossRef]
- Abdolsamadi, H.; Poormoradi, B.; Yaghoubi, G.; Farhadian, M.; Jazaeri, M. Relationship between body mass index and oral health indicators: A cross-sectional study. Eur. J. Transl. Myol. 2023, 33, 11259. [Google Scholar] [CrossRef]
- Hall-Scullin, E.P.; Whitehead, H.; Rushton, H.; Milsom, K.; Tickle, M. A longitudinal study of the relationship between dental caries and obesity in late childhood and adolescence. J. Public Health Dent. 2018, 78, 100–108. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.; Tellez, M.; Ismail, A.I. Emotional distress and risk of dental caries: Evaluating effect modification by chronic conditions among low-income African American caregivers in Detroit, Michigan. Front. Public Health 2023, 11, 1050511. [Google Scholar] [CrossRef] [PubMed]
- Dos Santos Letieri, A.; Siqueira, W.L.; Solon-de-Mello, M.; Masterson, D.; Freitas-Fernandes, L.B.; Valente, A.P.; Ribeiro de Souza, I.P.; da Silva Fidalgo, T.K.; Maia, L.C. A critical review on the association of hyposalivation and dental caries in children and adolescents. Arch. Oral Biol. 2022, 144, 105545. [Google Scholar] [CrossRef]
- Vila, T.; Rizk, A.M.; Sultan, A.S.; Jabra-Rizk, M.A. The power of saliva: Antimicrobial and beyond. PLoS Pathog. 2019, 15, e1008058. [Google Scholar] [CrossRef] [PubMed]
- Shahid, M. Regular supervised fluoride mouthrinse use by children and adolescents associated with caries reduction. Evid. Based Dent. 2017, 18, 11–12. [Google Scholar] [CrossRef]
- Levine, R.S. What concentration of fluoride toothpaste should dental teams be recommending? Evid. Based Dent. 2019, 20, 74–75. [Google Scholar] [CrossRef]
- Latifi-Xhemajli, B.; Begzati, A.; Veronneau, J.; Kutllovci, T.; Rexhepi, A. Effectiveness of fluoride varnish four times a year in preventing caries in the primary dentition: A 2 year randomized controlled trial. Community Dent. Health 2019, 36, 190–194. [Google Scholar] [CrossRef]
- Manchanda, S.; Sardana, D.; Liu, P.; Lee, G.H.; Li, K.Y.; Lo, E.C.; Yiu, C.K. Topical fluoride to prevent early childhood caries: Systematic review with network meta-analysis. J. Dent. 2022, 116, 103885. [Google Scholar] [CrossRef]
- Wu, L.; Chang, R.; Mu, Y.; Deng, X.; Wu, F.; Zhang, S.; Zhou, D. Association between obesity and dental caries in Chinese children. Caries Res. 2013, 47, 171–176. [Google Scholar] [CrossRef]
- Nasseripour, M.; Newton, J.T.; Warburton, F.; Awojobi, O.; Di Giorgio, S.; Gallagher, J.E.; Banerjee, A. A systematic review and meta-analysis of the role of sugar-free chewing gum on Streptococcus mutans. BMC Oral Health 2021, 21, 217. [Google Scholar] [CrossRef]
- Yeung, C.Y.-Y.; Chu, C.-H.; Yu, O.Y. A concise review of chewing gum as an anti-cariogenic agent. Front. Oral Health 2023, 4, 1213523. [Google Scholar] [CrossRef] [PubMed]
- Haghgoo, R.; Afshari, E.; Ghanaat, T.; Aghazadeh, S. Comparing the efficacy of xylitol-containing and conventional chewing gums in reducing salivary counts of Streptococcus mutans: An in vivo study. J. Int. Soc. Prev. Community Dent. 2015, 5, S112–S117. [Google Scholar] [CrossRef] [PubMed]
- Cannon, M.L.; Vorachek, A.; Le, C.; White, K. Retrospective Review of Oral Probiotic Therapy. J. Clin. Pediatr. Dent. 2019, 43, 367–371. [Google Scholar] [CrossRef]
- Meng, N.; Liu, Q.; Dong, Q.; Gu, J.; Yang, Y. Effects of probiotics on preventing caries in preschool children: A systematic review and meta-analysis. J. Clin. Pediatr. Dent. 2023, 47, 85–100. [Google Scholar] [CrossRef]
- Tahmourespour, A.; Kasra-Kermanshahi, R.; Salehi, R. Lactobacillus rhamnosus biosurfactant inhibits biofilm formation and gene expression of caries-inducing Streptococcus mutans. Dent. Res. J. 2019, 16, 87–94. [Google Scholar] [CrossRef]
- Ng, T.C.-H.; Chu, C.-H.; Yu, O.Y. A concise review of dental sealants in caries management. Front. Oral Health 2023, 4, 1180405. [Google Scholar] [CrossRef]
- Wright, J.T.; Tampi, M.P.; Graham, L.; Estrich, C.; Crall, J.J.; Fontana, M.; Gillette, E.J.; Nový, B.B.; Dhar, V.; Donly, K.; et al. Sealants for preventing and arresting pit-and-fissure occlusal caries in primary and permanent molars: A systematic review of randomized controlled trials—A report of the American Dental Association and the American Academy of Pediatric Dentistry. J. Am. Dent. Assoc. 2016, 147, 631–645.e618. [Google Scholar] [CrossRef]
- Soto-Barreras, U.; Escalante-Villalobos, K.Y.; Holguín-Loya, B.; Perez-Aguirre, B.; Nevárez-Rascón, A.; Martínez-Martínez, R.E.; Loyola-Rodríguez, J.P. Effect of fluoride in drinking water on dental caries and IQ in children. Fluoride 2019, 52, 474–482. [Google Scholar]
- Fontana, M.; Eckert, G.J.; Keels, M.A.; Jackson, R.; Katz, B.; Levy, B.T.; Levy, S.M. Fluoride Use in Health Care Settings: Association with Children’s Caries Risk. Adv. Dent. Res. 2018, 29, 24–34. [Google Scholar] [CrossRef]
- Toumba, K.J.; Twetman, S.; Splieth, C.; Parnell, C.; van Loveren, C.; Lygidakis, N. Guidelines on the use of fluoride for caries prevention in children: An updated EAPD policy document. Eur. Arch. Paediatr. Dent. 2019, 20, 507–516. [Google Scholar] [CrossRef]
- Pappa, E.; Vastardis, H.; Rahiotis, C. Chair-side saliva diagnostic tests: An evaluation tool for xerostomia and caries risk assessment in children with type 1 diabetes. J. Dent. 2020, 93, 103224. [Google Scholar] [CrossRef] [PubMed]
- Choudhary, A.; Bhat, M.; Choudhary, H.; Joshi, V.; Singh Walia, S.; Soni, R.K. Prevalence of Dental Caries with Salivary Assessment in Six to Twelve Years Old School-Going Children in Shahpura Tehsil, Jaipur. Cureus 2022, 14, e27802. [Google Scholar] [CrossRef] [PubMed]
- Ichim, D.L.; Sachelarie, L.; Calin, G.; Burlui, A. Are Saliva Tests Important in the Prediction of Carious Disease? Appl. Sci. 2021, 11, 5932. [Google Scholar] [CrossRef]
- Jayaraj, D.; Ganesan, S. Salivary pH and Buffering Capacity as Risk Markers for Early Childhood Caries: A Clinical Study. Int. J. Clin. Pediatr. Dent. 2015, 8, 167–171. [Google Scholar] [CrossRef] [PubMed]
- Cunha-Cruz, J.; Scott, J.; Rothen, M.; Mancl, L.; Lawhorn, T.; Brossel, K.; Berg, J. Salivary characteristics and dental caries: Evidence from general dental practices. J. Am. Dent. Assoc. 2013, 144, e31–e40. [Google Scholar] [CrossRef]
- Fidalgo, T.K.; Freitas-Fernandes, L.B.; Ammari, M.; Mattos, C.T.; de Souza, I.P.; Maia, L.C. The relationship between unspecific s-IgA and dental caries: A systematic review and meta-analysis. J. Dent. 2014, 42, 1372–1381. [Google Scholar] [CrossRef]
- Hamid, H.; Adanir, N.; Asiri, F.Y.I.; Abid, K.; Zafar, M.S.; Khurshid, Z. Salivary IgA as a Useful Biomarker for Dental Caries in Down’s Syndrome Patients: A Systematic Review and Meta-analysis. Eur. J. Dent. 2020, 14, 665–671. [Google Scholar] [CrossRef]
- Featherstone, J.D.B.; Crystal, Y.O.; Alston, P.; Chaffee, B.W.; Doméjean, S.; Rechmann, P.; Zhan, L.; Ramos-Gomez, F. Evidence-Based Caries Management for All Ages-Practical Guidelines. Front. Oral Health 2021, 2, 657518. [Google Scholar] [CrossRef]
- Martignon, S.; Cortes, A.; Douglas, G.V.A.; Newton, J.T.; Pitts, N.B.; Avila, V.; Usuga-Vacca, M.; Gamboa, L.F.; Deery, C.; Abreu-Placeres, N.; et al. CariesCare International adapted for the pandemic in children: Caries OUT multicentre single-group interventional study protocol. BMC Oral Health 2021, 21, 329. [Google Scholar] [CrossRef]
- Anup, N.; Vishnani, P. Cariogram—A Multi-factorial Risk Assessment Software for Risk Prediction of Dental Caries. Int. J. Sci. Study 2014, 1, 58–62. [Google Scholar]
- MySmileBuddy. How Is the Mysmilebuddy Program Implemented? Available online: https://www.mysmilebuddy.tech/q15 (accessed on 7 April 2024).
- Busby, M.; Chapple, E.; Matthews, R.; Chapple, I.L. Practitioner evaluation of a novel online integrated oral health and risk assessment tool: A practice pilot. Br. Dent. J. 2013, 215, 115–120. [Google Scholar] [CrossRef] [PubMed]
- Busby, M.; Fayle, S.; Chapple, L.; Clover, H.; Chapple, I. Practitioner evaluation of an online oral health and risk assessment tool for young patients. Br. Dent. J. 2017, 223, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Christian, B.; Armstrong, R.; Calache, H.; Carpenter, L.; Gibbs, L.; Gussy, M. A systematic review to assess the methodological quality of studies on measurement properties for caries risk assessment tools for young children. Int. J. Paediatr. Dent. 2019, 29, 106–116. [Google Scholar] [CrossRef]
- Chaffee, B.W.; Cheng, J.; Featherstone, J.D. Baseline caries risk assessment as a predictor of caries incidence. J. Dent. 2015, 43, 518–524. [Google Scholar] [CrossRef]
- Kriegler, K.; Blue, C.M. Caries Management by Risk Assessment vs. Traditional Preventive Strategies: Effect on Oral Health Behaviors and Caries Diagnoses: A Retrospective Case-Control Observational Design. Clin. Case Rep. 2021, 9, e04751. [Google Scholar] [CrossRef]
- Coelho, A.; Amaro, I.; Iunes, T.; Paula, A.; Marto, C.M.; Saraiva, J.; Ferreira, M.M.; Carrilho, E. CAMBRA Protocol Efficacy: A Systematic Review and Critical Appraisal. Dent. J. 2022, 10, 97. [Google Scholar] [CrossRef] [PubMed]
- Khallaf, Y.S.; Hafez, S.; Shaalan, O.O. Evaluation of ICCMS versus CAMBRA Caries Risk Assessment Models Acquisition on Treatment Plan in Young Adult Population: A Randomized Clinical Trial. Clin. Cosmet. Investig. Dent. 2021, 13, 293–304. [Google Scholar] [CrossRef]
- Cagetti, M.G.; Bontà, G.; Cocco, F.; Lingstrom, P.; Strohmenger, L.; Campus, G. Are standardized caries risk assessment models effective in assessing actual caries status and future caries increment? A systematic review. BMC Oral Health 2018, 18, 123. [Google Scholar] [CrossRef]
- Agouropoulos, A.; Birpou, E.; Twetman, S.; Kavvadia, K. Validation of Three Caries Risk Assessment Tools for Preschool Children from Areas with High Caries Prevalence. Pediatr. Dent. 2019, 41, 391–399. [Google Scholar]
- Cheuk, R.; Adeniyi, A.; Farmer, J.; Singhal, S.; Jessani, A. Teledentistry use during the COVID-19 pandemic: Perceptions and practices of Ontario dentists. BMC Oral Health 2023, 23, 72. [Google Scholar] [CrossRef]
- Islam, M.R.R.; Islam, R.; Ferdous, S.; Watanabe, C.; Yamauti, M.; Alam, M.K.; Sano, H. Teledentistry as an Effective Tool for the Communication Improvement between Dentists and Patients: An Overview. Healthcare 2022, 10, 1586. [Google Scholar] [CrossRef] [PubMed]
| Author (Year) | Brand | Age (Year) | Sample Size | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|
| Salivary bacteria-level test | |||||
| Strickland et al. (2017) * [12] | Saliva-Check Mutans (GC, Tokyo, Japan) | Adult: 25–35 Children: 3–10 | Adult: 20 Children: 25 | 88 | 90 |
| Voelker et al. (2018) [13] | Saliva-Check Mutans (GC, Tokyo, Japan) | NA | 53 | 88 | 25 |
| Babu et al. (2019) [14] | Saliva-Check Mutans (GC, Tokyo, Japan) | 9–14 | 25 | 88 | 75 |
| Caries Risk Test (Ivoclar Vivadent, Schaan, Liechtenstein) | 93 | 92 | |||
| Cariscreen Caries Susceptibility Test (Oral BioTech, New York, United States) | 92 | 92 | |||
| Plaque pH test | |||||
| Strickland et al. (2017) * [12] | Plaque-check pH kit (GC, Tokyo, Japan) | Adult: 25–35 Children: 3–10 | Adult: 20 Children: 25 | 72 | 55 |
| Author (Year) | Follow-Up Duration (Year) | Age at Baseline (Year) | Final Sample Size | Sensitivity (%) | Specificity (%) |
|---|---|---|---|---|---|
| American Academy of Pediatric Dentistry’s Caries Risk Assessment Tool | |||||
| Gao et al. (2013) * [15] | 1 | 3 | 485 | 100 | 3.6 |
| Agouropoulos et al. (2019) [16] | 2 | 2–5 | 146 | 94 | 7 |
| Caries Management by Risk Assessment Tool | |||||
| Gao et al. (2013) * [15] | 1 | 3 | 485 | 84 | 63 |
| Sudhir et al. (2016) [17] | 2 | 12–13 | 72 | 48 | 80 |
| Cariogram | |||||
| Gao et al. (2013) * [15] | 1 | 3 | 485 | 65 | 79 |
| Peterson (2015) [18] | 3 | 19 | 982 | Low risk: 89 Moderate risk: 61 High risk: 26 Very high risk: 12 | Low risk: 34 Moderate: 71 High risk: 91 Very high risk: 95 |
| Dou (2018) [19] | 2 | 18–29 | 192 | Very low risk: 12 Low risk: 26 Moderate risk: 56 High risk: 84 Very high risk: 99 | Very-low-risk: 100 Low risk: 91 Moderate risk: 80 High risk: 56 Very high risk: 24 |
| Kim et al. (2018) [20] | NA | 10–18 | 171 | 61 | 85 |
| Birpou et al. (2019) [21] | 2 | 2–5 | 154 | 68 | 59 |
| Dolic et al. (2020) [22] | 4 | 0 | 80 | Very low to moderate risk: 61 Moderate to very high risk: 82 | Very low to moderate risk: 91 Moderate to very high risk: 65 |
| 4 | 20–42 | 80 | Very low to moderate risk: 54 Moderate to very high risk: 81 | Very low to moderate risk: 69 Moderate to very high risk: 58 | |
| National University of Singapore Caries Risk Assessment Tool | |||||
| Gao et al. (2013) * [15] | 1 | 3 | 485 | 78 | 85 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ng, T.C.-H.; Luo, B.W.; Lam, W.Y.-H.; Baysan, A.; Chu, C.-H.; Yu, O.Y. Updates on Caries Risk Assessment—A Literature Review. Dent. J. 2024, 12, 312. https://doi.org/10.3390/dj12100312
Ng TC-H, Luo BW, Lam WY-H, Baysan A, Chu C-H, Yu OY. Updates on Caries Risk Assessment—A Literature Review. Dentistry Journal. 2024; 12(10):312. https://doi.org/10.3390/dj12100312
Chicago/Turabian StyleNg, Toby Cheuk-Hang, Bella Weijia Luo, Walter Yu-Hang Lam, Aylin Baysan, Chun-Hung Chu, and Ollie Yiru Yu. 2024. "Updates on Caries Risk Assessment—A Literature Review" Dentistry Journal 12, no. 10: 312. https://doi.org/10.3390/dj12100312
APA StyleNg, T. C.-H., Luo, B. W., Lam, W. Y.-H., Baysan, A., Chu, C.-H., & Yu, O. Y. (2024). Updates on Caries Risk Assessment—A Literature Review. Dentistry Journal, 12(10), 312. https://doi.org/10.3390/dj12100312










