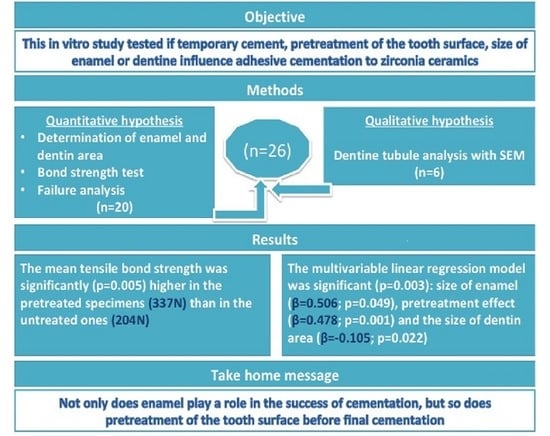
Effect of Temporary Cement, Surface Pretreatment and Tooth Area on the Bond Strength of Adhesively Cemented Ceramic Overlays—An In Vitro Study
Abstract
1. Introduction
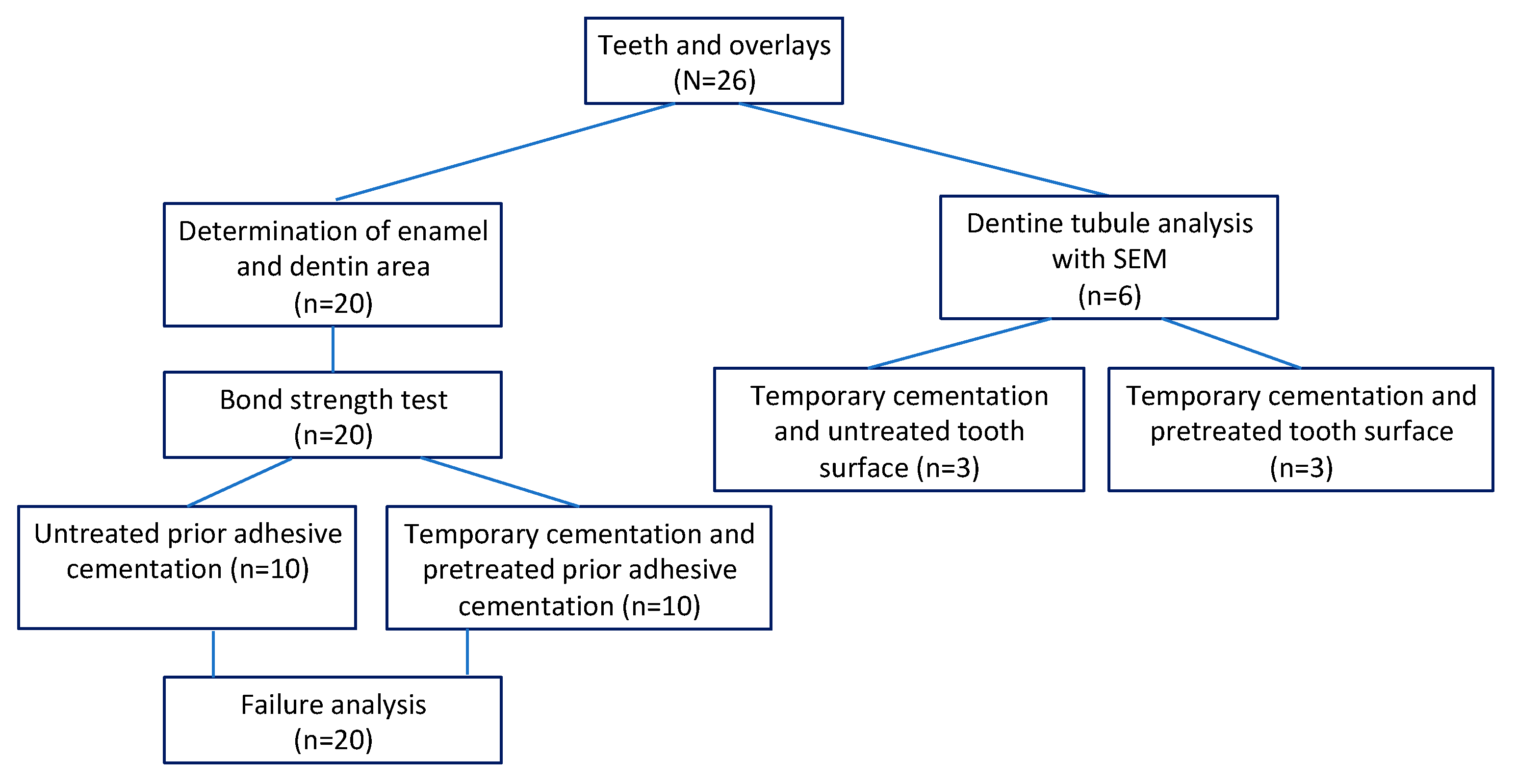
2. Materials and Methods
2.1. Inclusion of Samples
2.2. Specimen Preparation for the Surface Analysis and Bond Strength Test
2.3. Measuring Enamel and Dentin Areas
2.4. Manufacturing of Overlay
2.5. Division of Specimens in Preparation for Testing the Bond Strength
2.6. Adhesive Cementation
2.7. Tensile Bond Strength Test
2.8. Failure Mode Analysis
2.9. Specimen Preparation for Dentine Tubules Substance Analysis
2.10. Statistical Analyses
3. Results
3.1. Influence of Tooth Area on the Bond Strength
3.2. Failure Modes
3.3. Qualitative Substance Analysis of Cement Residues Present in Dentine Tubules
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Beier, U.S.; Kapferer, I.; Burtscher, D.; Giesinger, J.M.; Dumfahrt, H. Clinical performance of all-ceramic inlay and onlay restorations in posterior teeth. Int. J. Prosthodont. 2012, 25, 395–402. [Google Scholar] [PubMed]
- Gaile, M.; Papia, E.; Zalite, V.; Locs, J.; Soboleva, U. Resin Cement Residue Removal Techniques: In Vitro Analysis of Marginal Defects and Discoloration Intensity Using Micro-CT and Stereomicroscopy. Dent. J. 2022, 10, 55. [Google Scholar] [CrossRef] [PubMed]
- Ribeiro, J.C.V.; Coelho, P.G.; Janal, M.N.; Silva, N.R.F.A.; Monteiro, A.J.; Fernandes, C.A.O. The influence of temporary cements on dental adhesive systems for luting cementation. J. Dent. 2011, 39, 255–262. [Google Scholar] [CrossRef] [PubMed]
- Comino-Garayoa, R.; Peláez, J.; Tobar, C.; Rodríguez, V.; Suárez, M.J. Adhesion to Zirconia: A Systematic Review of Surface Pretreatments and Resin Cements. Materials 2021, 14, 2751. [Google Scholar] [CrossRef] [PubMed]
- Abo-Hamar, S.E.; Federlin, M.; Hiller, K.-A.; Friedl, K.-H.; Schmalz, G. Effect of temporary cements on the bond strength of ceramic luted to dentin. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2005, 21, 794–803. [Google Scholar] [CrossRef]
- Song, M.-Y.; An, H.; Park, E.-J. The Effect of Temporary Cement Cleaning Methods on the Retention of Crowns. J. Prosthodont. Off. J. Am. Coll. Prosthodont. 2019, 28, e210–e215. [Google Scholar] [CrossRef]
- Carvalho, C.N.; de Oliveira Bauer, J.R.; Loguercio, A.D.; Reis, A. Effect of ZOE temporary restoration on resin-dentin bond strength using different adhesive strategies. J. Esthet. Restor. Dent. Off. Publ. Am. Acad. Esthet. Dentistry 2007, 19, 144–152. [Google Scholar] [CrossRef]
- Leung, G.K.-H.; Wong, A.W.-Y.; Chu, C.-H.; Yu, O.Y. Update on Dental Luting Materials. Dent. J. 2022, 10, 208. [Google Scholar] [CrossRef]
- Grasso, C.A.; Caluori, D.M.; Goldstein, G.R.; Hittelman, E. In vivo evaluation of three cleansing techniques for prepared abutment teeth. J. Prosthet. Dent. 2002, 88, 437–441. [Google Scholar] [CrossRef]
- Erkut, S.; Küçükesmen, H.C.; Eminkahyagil, N.; Imirzalioglu, P.; Karabulut, E. Influence of previous provisional cementation on the bond strength between two definitive resin-based luting and dentin bonding agents and human dentin. Oper. Dent. 2007, 32, 84–93. [Google Scholar] [CrossRef]
- Politano, G.; Van Meerbeek, B.; Peumans, M. Nonretentive Bonded Ceramic Partial Crowns: Concept and Simplified Protocol for Long-lasting Dental Restorations. J. Adhes. Dent. 2018, 20, 495–510. [Google Scholar] [CrossRef] [PubMed]
- Buj-Corral, I.; Vidal, D.; Tejo-Otero, A.; Padilla, J.A.; Xuriguera, E.; Fenollosa-Artés, F. Characterization of 3D Printed Yttria-Stabilized Zirconia Parts for Use in Prostheses. Nanomaterials 2021, 11, 2942. [Google Scholar] [CrossRef] [PubMed]
- Katana Zirconia STML Technical Guide. Available online: https://www.kuraraynoritake.eu/pub/media/pdfs/21599_1_Katana_discs_Technical_Guide_LR_21.pdf (accessed on 5 October 2022).
- Papia, E.; Larsson, C.; du Toit, M.; Vult von Steyern, P. Bonding between oxide ceramics and adhesive cement systems: A systematic review. J. Biomed. Mater. Res. Part B Appl. Biomater. 2014, 102, 395–413. [Google Scholar] [CrossRef] [PubMed]
- Al-Akhali, M.; Al-Dobaei, E.; Wille, S.; Mourshed, B.; Kern, M. Influence of elapsed time between airborne-particle abrasion and bonding to zirconia bond strength. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2021, 37, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Panavia V5 Instructions for Use. Available online: https://kuraraydental.com/wp-content/uploads/2018/05/panavia-v5-ifu.pdf (accessed on 5 October 2022).
- Emamieh, S.; Sadr, A.; Ghasemi, A.; Torabzadeh, H.; Akhavanzanjani, V.; Tagami, J. Effects of solvent drying time and water storage on ultimate tensile strength of adhesives. J. Investig. Clin. Dent. 2014, 5, 51–57. [Google Scholar] [CrossRef]
- ISO/TS 11405:2003; International Standards Organization. Dental Materials-Testing of Adhesion to Tooth Structure. European Committee for Standardization: Geneva, Switzerland, 2003.
- Scherrer, S.S.; Cesar, P.F.; Swain, M.V. Direct comparison of the bond strength results of the different test methods: A critical literature review. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2010, 26, e78–e93. [Google Scholar] [CrossRef]
- Hill, E.E.; Lott, J. A clinically focused discussion of luting materials. Aust. Dent. J. 2011, 56 (Suppl. 1), 67–76. [Google Scholar] [CrossRef]
- Kanakuri, K.; Kawamoto, Y.; Matsumura, H. Influence of temporary cement remnant and surface cleaning method on bond strength to dentin of a composite luting system. J. Oral Sci. 2005, 47, 9–13. [Google Scholar] [CrossRef]
- Saraç, D.; Bulucu, B.; Saraç, Y.S.; Kulunk, S. The effect of dentin-cleaning agents on resin cement bond strength to dentin. J. Am. Dent. Assoc. 2008, 139, 751–758. [Google Scholar] [CrossRef]
- Attia, A.; Kern, M. Effect of cleaning methods after reduced-pressure air abrasion on bonding to zirconia ceramic. J. Adhes. Dent. 2011, 13, 561–567. [Google Scholar] [CrossRef]
- Mine, A.; Nikaido, T.; Matsumoto, M.; Takagaki, T.; Ishida, M.; Ban, S.; Yamanaka, A.; Takaishi, M.; Yumitate, M.; Hagino, R.; et al. Status of decontamination methods after using dentin adhesion inhibitors on indirect restorations: An integrative review of 19 publications. Jpn. Dent. Sci. Rev. 2021, 57, 147–153. [Google Scholar] [CrossRef] [PubMed]
- Watanabe, E.K.; Yatani, H.; Ishikawa, K.; Suzuki, K.; Yamashita, A. Pilot study of conditioner/primer effects on resin-dentin bonding after provisional cement contamination using SEM, energy dispersive x-ray spectroscopy, and bond strength evaluation measures. J. Prosthet. Dent. 2000, 83, 349–355. [Google Scholar] [CrossRef]
- Peutzfeldt, A.; Asmussen, E. Influence of eugenol-containing temporary cement on bonding of self-etching adhesives to dentin. J. Adhes. Dent. 2006, 8, 31–34. [Google Scholar] [PubMed]
- Lee, J.J.; Nettey-Marbell, A.; Cook, A., Jr.; Pimenta, L.A.F.; Leonard, R.; Ritter, A.V. Using extracted teeth for research: The effect of storage medium and sterilization on dentin bond strengths. J. Am. Dent. Assoc. 2007, 138, 1599–1603. [Google Scholar] [CrossRef] [PubMed]
- Armstrong, S.; Breschi, L.; Özcan, M.; Pfefferkorn, F.; Ferrari, M.; Van Meerbeek, B. Academy of Dental Materials guidance on in vitro testing of dental composite bonding effectiveness to dentin/enamel using micro-tensile bond strength (μTBS) approach. Dent. Mater. Off. Publ. Acad. Dent. Mater. 2017, 33, 133–143. [Google Scholar] [CrossRef]
- Qahtani, W.L. Assessment of Marginal Opening for Different Cementation Techniques for Heat-Pressed Ceramic Veneers. Niger. J. Clin. Pract. 2020, 23, 1643–1647. [Google Scholar] [CrossRef]
- Oilo, G. Bond strength testing--what does it mean? Int. Dent. J. 1993, 43, 492–498. [Google Scholar]
- Aung, S.S.M.P.; Takagaki, T.; Ko, A.K.; Halabi, S.; Sato, T.; Ikeda, M.; Nikaido, T.; Burrow, M.F.; Tagami, J. Adhesion durability of dual-cure resin cements and acid–base resistant zone formation on human dentin. Dent. Mater. 2019, 35, 945–952. [Google Scholar] [CrossRef]
- Rohr, N.; Fischer, J. Tooth surface treatment strategies for adhesive cementation. J. Adv. Prosthodont. 2017, 9, 85–92. [Google Scholar] [CrossRef]
- Müller, J.A.; Rohr, N.; Fischer, J. Evaluation of ISO 4049: Water sorption and water solubility of resin cements. Eur. J. Oral Sci. 2017, 125, 141–150. [Google Scholar] [CrossRef]
- Baldi, A.; Comba, A.; Ferrero, G.; Italia, E.; Michelotto Tempesta, R.; Paolone, G.; Mazzoni, A.; Breschi, L.; Scotti, N. External gap progression after cyclic fatigue of adhesive overlays and crowns made with high translucency zirconia or lithium silicate. J. Esthet. Restor. Dent. Off. Publ. Am. Acad. Esthet. Dentistry 2022, 34, 557–564. [Google Scholar] [CrossRef] [PubMed]
- Beltrami, R.; Chiesa, M.; Scribante, A.; Allegretti, J.; Poggio, C. Comparison of shear bond strength of universal adhesives on etched and nonetched enamel. J. Appl. Biomater. Funct. Mater. 2016, 14, e78–e83. [Google Scholar] [CrossRef] [PubMed]
- Abdelaziz, K.M.; Al-Qahtani, N.M.; Al-Shehri, A.S.; Abdelmoneam, A.M. Bonding quality of contemporary dental cements to sandblasted esthetic crown copings. J. Investig. Clin. Dent. 2012, 3, 142–147. [Google Scholar] [CrossRef] [PubMed]
- Koch, T.; Peutzfeldt, A.; Malinovskii, V.; Flury, S.; Häner, R.; Lussi, A. Temporary zinc oxide-eugenol cement: Eugenol quantity in dentin and bond strength of resin composite. Eur. J. Oral Sci. 2013, 121, 363–369. [Google Scholar] [CrossRef] [PubMed]






| Untreated Group | Pretreated Group | p Values # | |
|---|---|---|---|
| Mean (SD) | Mean (SD) | ||
| Total tooth area (mm2) | 59.4 (15.0) | 60.1 (10.6) | 0.913 |
| Dentin area (mm2) | 33.4 (7.9) | 30.5 (4.6) | 0.319 |
| Enamel area (mm2) | 26.0 (9.2) | 29.6 (7.4) | 0.347 |
| Bond strength (N) | 203.6 (59.2) | 337.4 (116.7) | 0.005 |
| Outcome: Bond Strength (N) at Time of Specimen Fracture Model Summary: p = 0.003, Adj. R2 = 0.577. | ||||
|---|---|---|---|---|
| PREDICTORS | Unstand. Coef (95% CI) | Stand. Coeff. β | p Values | Tolerance |
| Untreated vs. treated | 106.8 (21.1; 192.6) | 0.478 | 0.001 | 0.807 |
| Dentin area (mm2) | −1.9 (−9.4; 5.6) | −0.105 | 0.022 | 0.669 |
| Enamel area (mm2) | 7.0 (1.2; 12.8) | 0.506 | 0.049 | 0.673 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Grinberga, S.; Papia, E.; Aleksejuniene, J.; Zalite, V.; Locs, J.; Soboleva, U. Effect of Temporary Cement, Surface Pretreatment and Tooth Area on the Bond Strength of Adhesively Cemented Ceramic Overlays—An In Vitro Study. Dent. J. 2023, 11, 19. https://doi.org/10.3390/dj11010019
Grinberga S, Papia E, Aleksejuniene J, Zalite V, Locs J, Soboleva U. Effect of Temporary Cement, Surface Pretreatment and Tooth Area on the Bond Strength of Adhesively Cemented Ceramic Overlays—An In Vitro Study. Dentistry Journal. 2023; 11(1):19. https://doi.org/10.3390/dj11010019
Chicago/Turabian StyleGrinberga, Sanita, Evaggelia Papia, Jolanta Aleksejuniene, Vita Zalite, Janis Locs, and Una Soboleva. 2023. "Effect of Temporary Cement, Surface Pretreatment and Tooth Area on the Bond Strength of Adhesively Cemented Ceramic Overlays—An In Vitro Study" Dentistry Journal 11, no. 1: 19. https://doi.org/10.3390/dj11010019
APA StyleGrinberga, S., Papia, E., Aleksejuniene, J., Zalite, V., Locs, J., & Soboleva, U. (2023). Effect of Temporary Cement, Surface Pretreatment and Tooth Area on the Bond Strength of Adhesively Cemented Ceramic Overlays—An In Vitro Study. Dentistry Journal, 11(1), 19. https://doi.org/10.3390/dj11010019