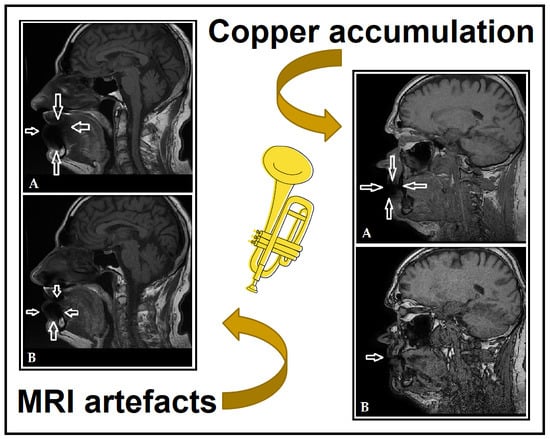
Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon
Abstract
1. Introduction
2. Materials and Methods
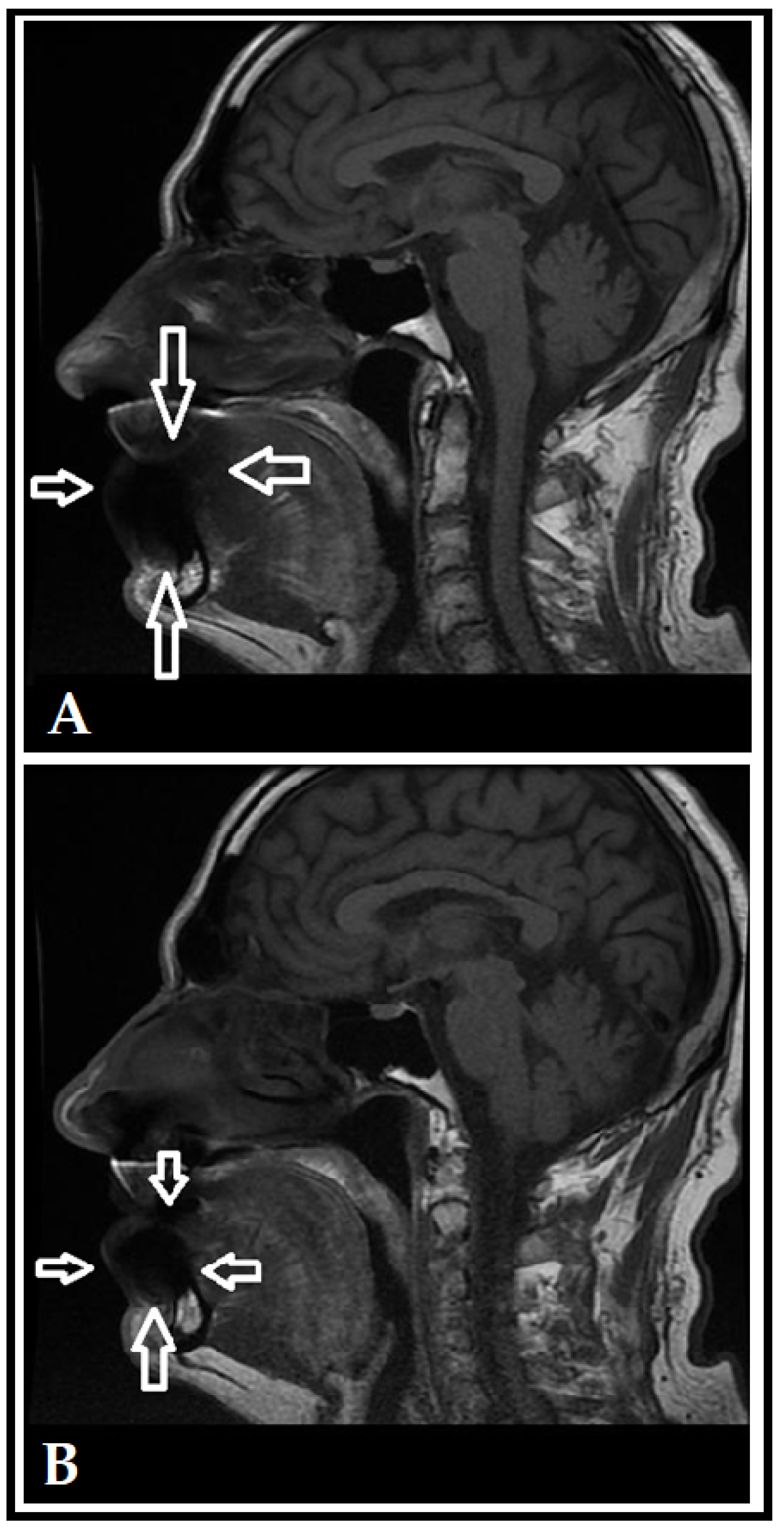
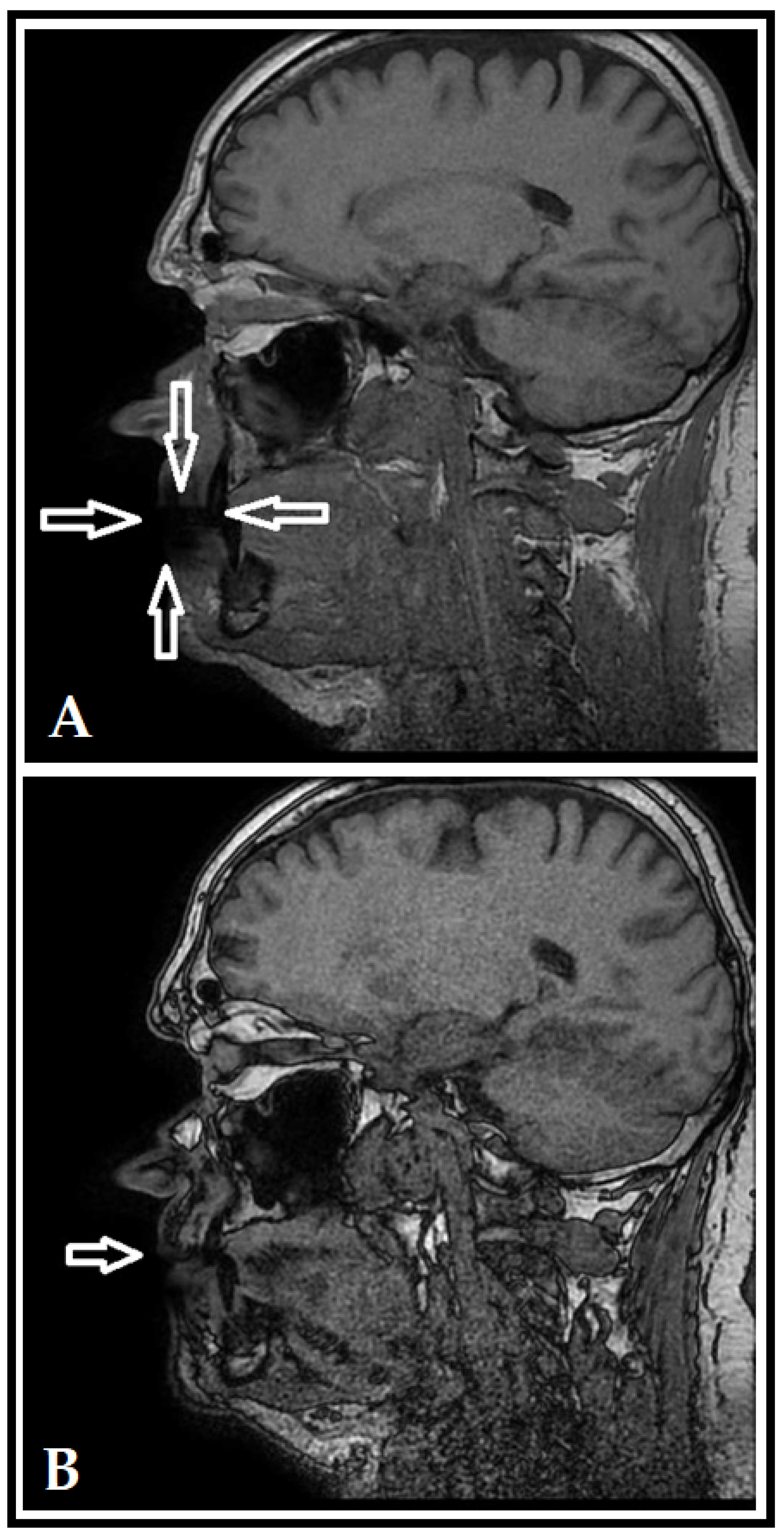
3. Results (Case Report)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Rushton, L. The Global Burden of Occupational Disease. Curr. Environ. Health. Rep. 2017, 4, 340–348. [Google Scholar] [CrossRef] [PubMed]
- WHO/ILO Joint Estimates of the Work-Related Burden of Disease and Injury, 2000–2016: Global Monitoring Report. Available online: https://www.who.int/publications/i/item/9789240034945 (accessed on 13 August 2022).
- Morell, S.; Kerr, C.; Driscoll, T.; Taylor, R.; Salkeld, G.; Corbett, S. Best estimate of the magnitude of mortality due to occupational exposure to hazardous substances. Occup. Environ. Med. 1998, 55, 634–641. [Google Scholar] [CrossRef] [PubMed]
- Takala, J.; Hamalainen, P.; Nenonen, N.; Takahashi, K.; Chimed-Ochir, O.; Rantanen, J. Comparative analysis of the burden of injury and illness at work in selected countries and regions. Cent. Eur. J. Occup. Environ. Med. 2017, 23, 6–31. [Google Scholar]
- Syurin, S.; Vinnikov, D. Occupational disease claims and non-occupational morbidity in a prospective cohort observation of nickel electrolysis workers. Sci. Rep. 2022, 12, e7092. [Google Scholar] [CrossRef]
- Shyagali, T.R.; Rai, N. Occupational dental health hazards: A review. Int. J. Contemp. Dent. Med. Rev. 2015, 2015, e140115. [Google Scholar]
- Petersen, P.E.; Henmar, P. Oral conditions among workers in the Danish granite industry. Scand. J. Work Environ. Health 1998, 14, 328–331. [Google Scholar] [CrossRef] [PubMed]
- Stobnicka, A.; Górny, R.L. Exposure to flour dust in the occupational environment. Int. J. Occup. Saf. Ergon. 2015, 21, 241–249. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.L.; Chen, Y.Y.; Wu, W.T.; Lai, C.H.; Sun, Y.S.; Wang, C.C. Examining relationship between occupational acid exposure and oral health in workplace. BMC Pub. Health 2020, 20, e1371. [Google Scholar] [CrossRef]
- Gupta, B.N. Occupational diseases of teeth. J. Soc. Occup. Med. 1990, 40, 149–152. [Google Scholar] [CrossRef] [PubMed]
- Gallagher, J.; Ashley, P.; Petrie, A.; Needleman, I. Oral health-related behaviours reported by elite and professional athletes. Brit. Dent. J. 2019, 227, 276–280. [Google Scholar] [CrossRef] [PubMed]
- Syed, M.; Chopra, R.; Sachdev, V. Allergic Reactions to Dental Materials-A Systematic Review. J. Clin. Diagn. Res. 2015, 9, ZE04–ZE09. [Google Scholar] [CrossRef]
- Lima, R.B.; Buarque, A. Oral health in the context of prevention of absenteeism and presenteeism in the workplace. Rev. Bras. Med. Trab. 2019, 17, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Pilotto, L.M.; Celeste, R.K. The relationship between private health plans and use of medical and dental health services in the Brazilian health system. Ciência Saúde Coletiva 2019, 24, 2727–2736. [Google Scholar] [CrossRef] [PubMed]
- Chong, J.; Lynden, M.; Harvey, D.; Peebles, M. Occupational Health Problems of Musicians. Can. Fam. Physician 1989, 35, 2341–2348. [Google Scholar] [PubMed]
- Yeo, D.K.L.; Pham, T.P.; Baker, J.; Porters, S.A.T. Specific orofacial problems experienced by musicians. Aust. Dent. J. 2002, 47, 2–11. [Google Scholar] [CrossRef] [PubMed]
- Raymond, D.M.; Romeo, J.H.; Kumke, K.V. A pilot study of occupational injury and illness experienced by classical musicians. Workplace Health Saf. 2012, 60, 19–24. [Google Scholar] [CrossRef]
- Cavalcanti, A.L.; Souto, J.M.V.; Brand, L.M.T.; Fernandes, L.H.F.; de Alencar, C.R.B.; Cavalcanti, A.F.C. Is playing string or wind musical instruments a risk factor for temporomandibular dysfunction? A Systematic Review. J. Oral Res. 2017, 6, 299–306. [Google Scholar] [CrossRef][Green Version]
- Eisen, D.; Zee, R.Y.L.; Farmelant, J.; Eisen, S.E. Contaminated Musical Wind Instruments as a Vector for Disease Transmission. Adv. Dent. Oral Health 2022, 15, 555912. [Google Scholar]
- Lund, A.E. Used musical instruments may pose oral health risk. J. Am. Dent. Assoc. 2011, 142, 490–491. [Google Scholar] [CrossRef]
- Barbieri, C.B.; Diomede, A.; Domingues, N.R.A.P.; Pasquinelli, F.; Pimentel, A.C.; Roman-Torres, C.V.G. Musicians of wind instruments and oral condition. J. Dent. Oral Care Med. 2020, 6, 1–4. [Google Scholar]
- Tischenko, K.I.; Beloglazkina, E.K.; Mazhuga, A.G.; Zyk, N.V. Copper-containing enzymes: Site types and low-molecular-weight model compounds. Rev. J. Chem. 2016, 6, 49–82. [Google Scholar] [CrossRef]
- Taylor, A.A.; Tsuji, J.S.; Garry, M.R.; McArdle, M.E.; Goodfellow, W.L., Jr.; Adams, W.J.; Menzie, C.A. Critical Review of Exposure and Effects: Implications for Setting Regulatory Health Criteria for Ingested Copper. Environ. Manag. 2020, 65, 131–159. [Google Scholar] [CrossRef] [PubMed]
- Haase, L.M.; Birk, T.; Bachand, A.; Mundt, K. A Health Surveillance Study of Workers Employed at a Copper Smelter—Effects of Long-Term Exposure to Copper on Lung Function Using Spirometric Data. J. Occup. Environ. Med. 2021, 63, e480–e489. [Google Scholar] [CrossRef]
- Ozturk, M.; Karacelebi, E.; Gungor, K.; Coskun, S.; Boysan, E. Evaluation of oxidative events and copper accumulatıon in oral tissues of patients wıth Wilson’s disease: Three case report. Int. J. Clin. Exp. Pathol. 2015, 8, 3943–3945. [Google Scholar]
- Donoghue, A.M.; Ferguson, M.M. Superficial copper staining of the teeth in a brass foundry worker. Occup. Med. 1996, 46, 233–234. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Herrström, P.; Högstedt, B. Clinical study of oral galvanism: No evidence of toxic mercury exposure but anxiety disorder an important background factor. Scand. J. Dent. Res. 1993, 101, 232–237. [Google Scholar] [CrossRef] [PubMed]
- Quezada-Castillo, E.; Aguilar-Castro, W.; Quezada-Alván, B. Corrosion of galvanic pairs of dental alloys copper base with silver amalgams in artificial saliva. Matéria 2019, 24, e12299. [Google Scholar] [CrossRef]
- Sutow, E.J.; Maillet, W.A.; Taylor, J.C.; Hall, G.C. In vivo galvanic currents of intermittently contacting dental amalgam and other metallic restorations. Dent. Mater. 2004, 20, 823–831. [Google Scholar] [CrossRef] [PubMed]
- Nagao, T.; Warnakulasuriya, S.; Hasegawa, S.; Sakuma, H.; Miyabe, S.; Komaki, K.; Ishii, K.; Machida, J.; Kimura, H.; Kuroyanagi, N.; et al. Elucidating risk factors for oral leukoplakia affecting gingivae in Japanese subjects. Transl. Res. Oral Oncol. 2016, 1, 1–11. [Google Scholar] [CrossRef]
- Sachdev, P.K.; Freeland-Graves, J.; Beretvas, N.S.; Sanjeevi, N. Zinc, Copper, and Iron in Oral Submucous Fibrosis: A Meta-Analysis. Int. J. Dent. 2018, 2018, e3472087. [Google Scholar] [CrossRef]
- Grover, N.; Sharma, J.; Sengupta, S.; Singh, S.; Singh, N.; Kaur, H. Long-term effect of tobacco on unstimulated salivary pH. J. Oral Maxilofac. Pathol. 2016, 20, 16–19. [Google Scholar] [CrossRef]
- Kanwar, A.; Sah, K.; Grover, N.; Chandra, S.; Singh, R.R. Long-term effect of tobacco on resting whole mouth salivary flow rate and pH: An institutional based comparative study. Exp. J. Gen. Dent. 2013, 2, 296–300. [Google Scholar] [CrossRef]
- Flügge, T.; Ludwig, U.; Amrein, P.; Kernen, F.; Vach, K.; Maier, J.; Nelson, K. MRI for the display of autologous onlay bone grafts during early healing—An experimental study. Dentomax. Radiol. 2020, 50, e2020068. [Google Scholar] [CrossRef]
- Wanner, L.; Ludwig, U.; Hövener, J.B.; Nelson, K.; Flügge, T. Magnetic resonance imaging—A diagnostic tool for postoperative evaluation of dental implants: A case report. Oral Surg. Oral Med. Oral Pathol. Oral Radiol. 2018, 125, e103–e107. [Google Scholar] [CrossRef] [PubMed]
- Nagy, Á.L.; Tóth, Z.; Tarjányi, T.; Práger, N.T.; Baráth, Z.L. Biomechanical properties of the bone during implant placement. BMC Oral Health 2021, 21, e86. [Google Scholar] [CrossRef]
- Mohr, I.; Weiss, K.H. Current anti-copper therapies in management of Wilson disease. Ann. Transl. Med. 2019, 7, S69. [Google Scholar] [CrossRef] [PubMed]
| Patient 1 | Patient 2 | |
|---|---|---|
| Sex | male | male |
| Age | 63 years | 61 years |
| Underlying conditions | none | glaucoma |
| Medication use | none | latanoprost |
| Known allergies | none | none |
| Tobacco and alcohol consumption | alcohol: very rarely tobacco: between 5–10 cigarettes/day | alcohol: very rarely tobacco: >25 cigarettes/day |
| Oral health status | fixed implants, metal-ceramic crowns | composite and amalgam fillings, metal-fused porcelain bridge in the upper right quadrant, chronic periodontitis, partially missing teeth |
| Type of mouthpiece | Stowasser | Schlagmüller U3 |
| Instrument cleaning practices | infrequently, using Sidol | none reported |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Baráth, Z.; Heltai, N.; Kereszty, É.; Kiss, I.; Gajdács, M.; Práger, N.T.; Kárpáti, K.; Matusovits, D. Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon. Dent. J. 2022, 10, 203. https://doi.org/10.3390/dj10110203
Baráth Z, Heltai N, Kereszty É, Kiss I, Gajdács M, Práger NT, Kárpáti K, Matusovits D. Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon. Dentistry Journal. 2022; 10(11):203. https://doi.org/10.3390/dj10110203
Chicago/Turabian StyleBaráth, Zoltán, Nóra Heltai, Éva Kereszty, Ildikó Kiss, Márió Gajdács, Nándor Tamás Práger, Krisztina Kárpáti, and Danica Matusovits. 2022. "Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon" Dentistry Journal 10, no. 11: 203. https://doi.org/10.3390/dj10110203
APA StyleBaráth, Z., Heltai, N., Kereszty, É., Kiss, I., Gajdács, M., Práger, N. T., Kárpáti, K., & Matusovits, D. (2022). Copper Accumulation in the Lips of Brass Players: Case Report of a Rare Phenomenon. Dentistry Journal, 10(11), 203. https://doi.org/10.3390/dj10110203