Optimization of Photobiomodulation Dose in Biological Tissue by Adjusting the Focal Point of Lens
Abstract
:1. Introduction
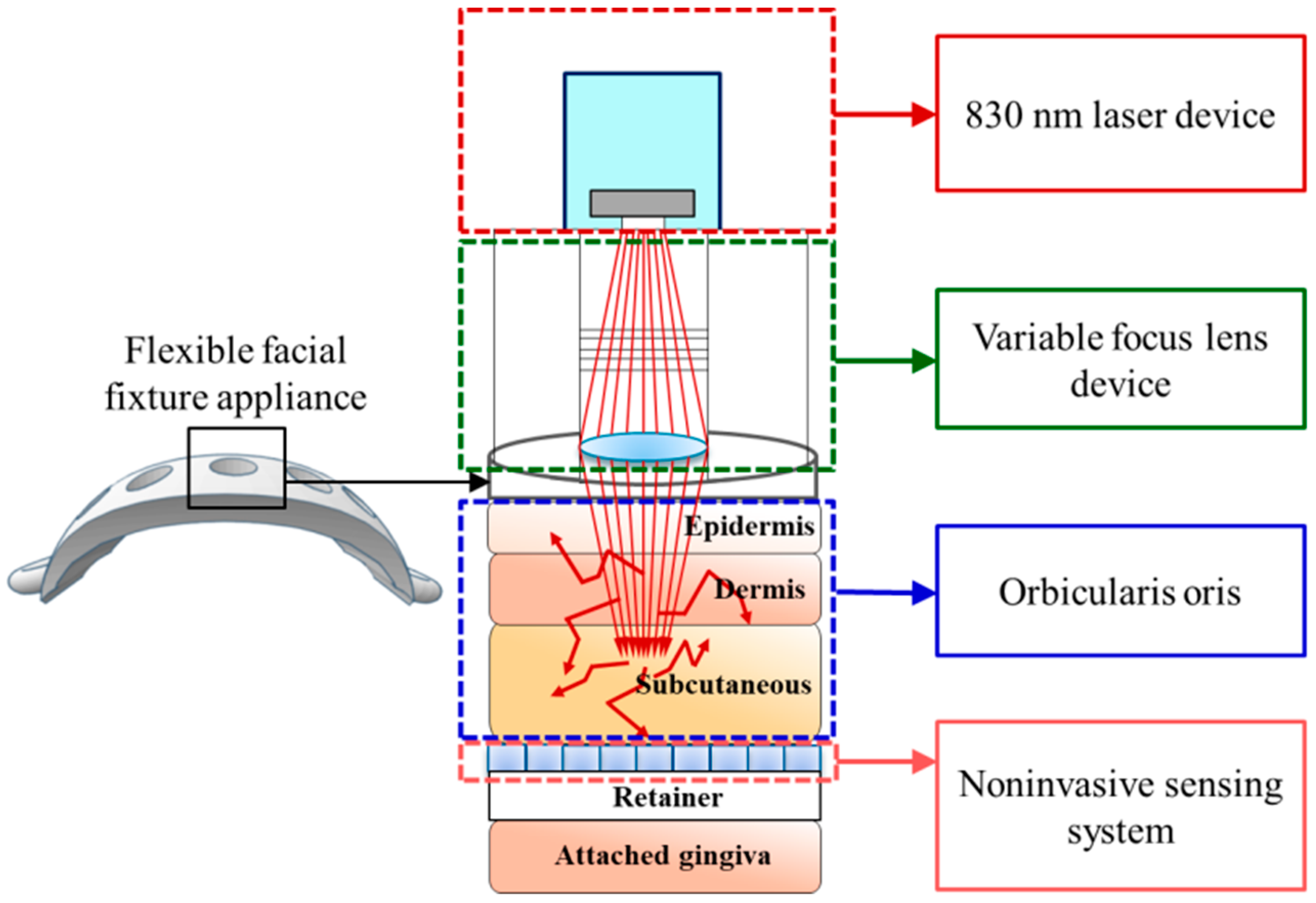
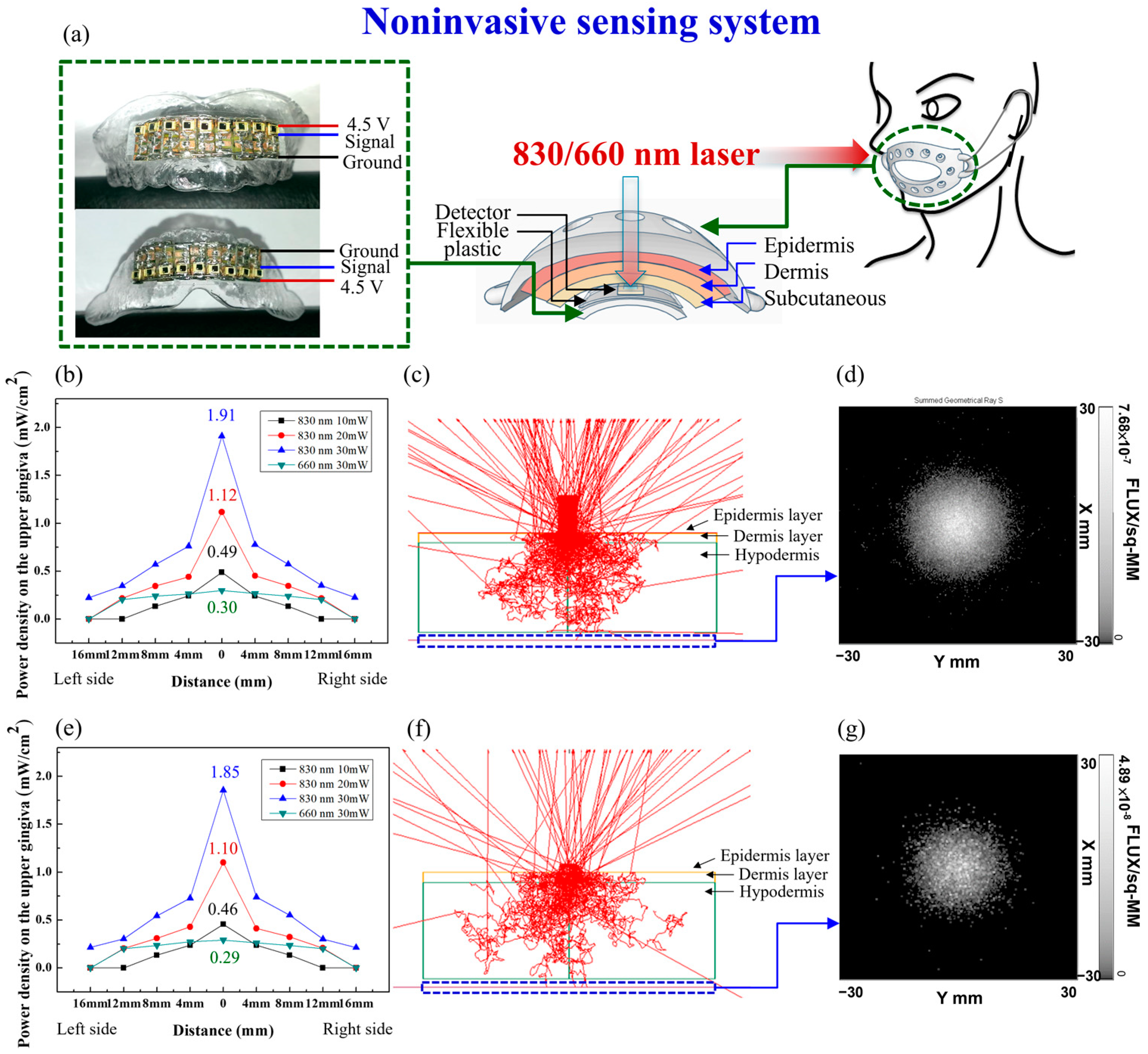
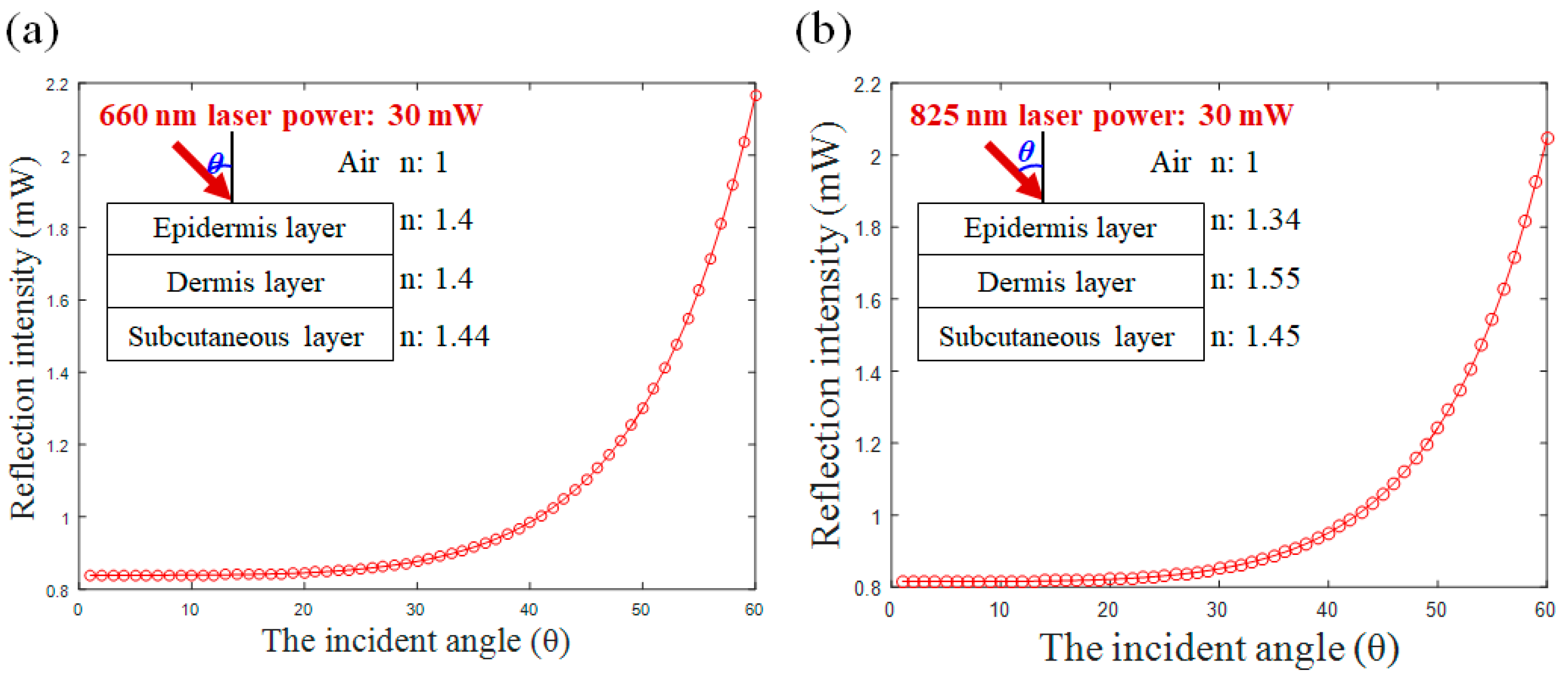
2. Materials and Methods
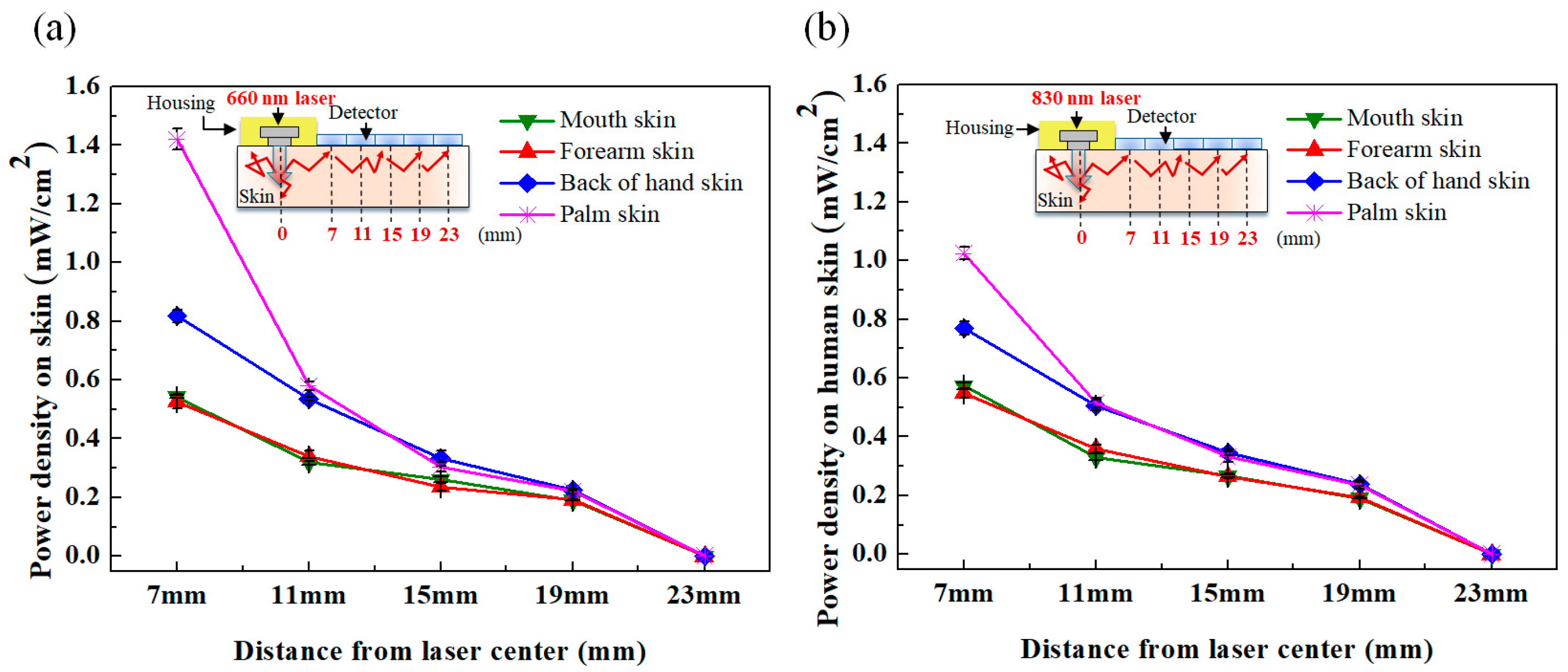
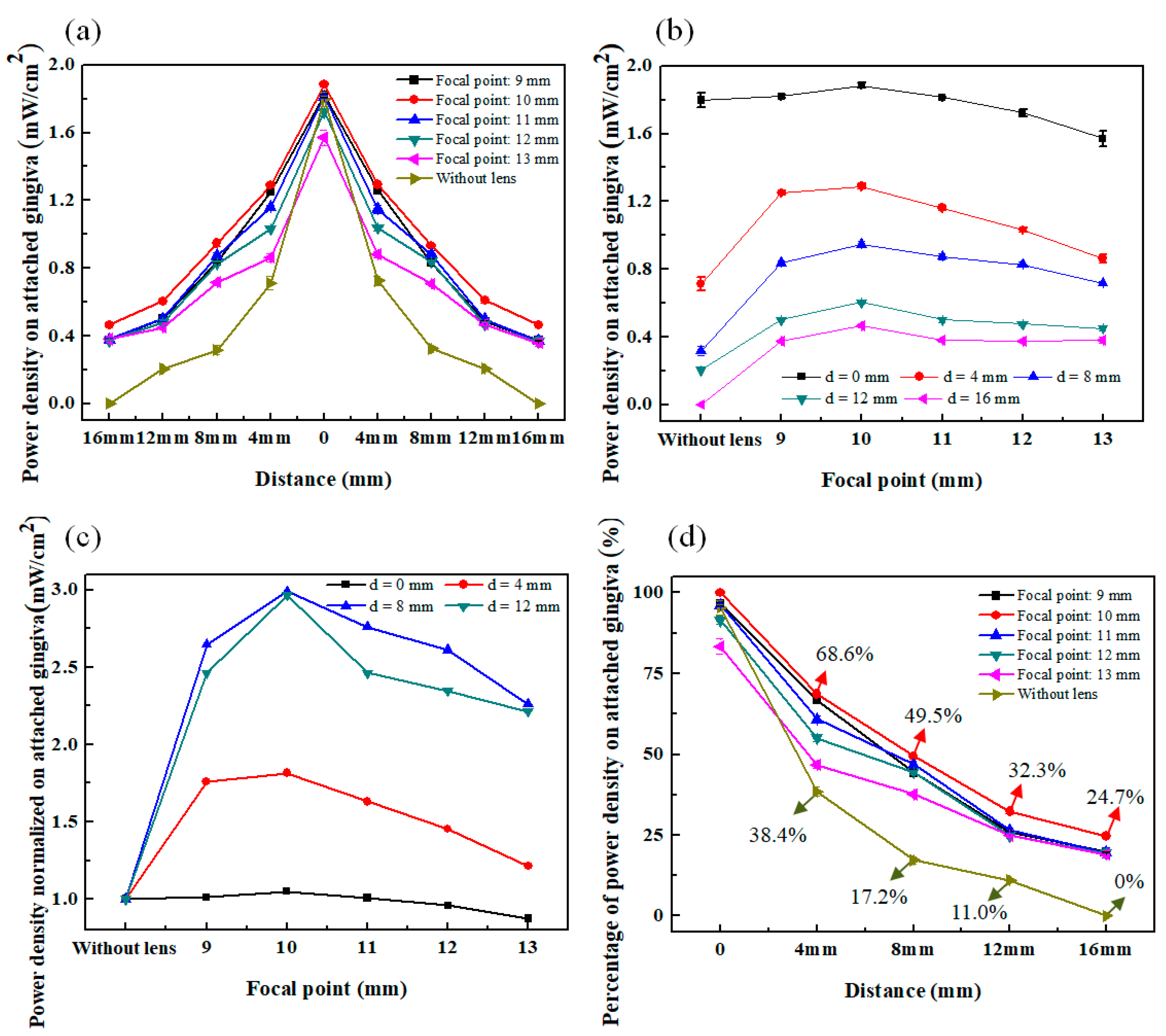
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Lin, M.L.; Wu, H.C.; Hsieh, Y.H.; Su, C.T.; Shih, Y.S.; Lin, C.W.; Wu, J.H. Evaluation of the effect of laser acupuncture and cupping with ryodoraku and visual analog scale on low back pain. Evid.-Based Complement. Altern. Med. 2012, 2012, 521612. [Google Scholar] [CrossRef] [PubMed]
- Lin, M.L.; Wu, J.H.; Lin, C.W.; Su, C.T.; Wu, H.C.; Shih, Y.S.; Chiu, I.T.; Chen, C.Y.; Chang, W.D. Clinical effects of laser acupuncture plus Chinese cupping on the pain and plasma cortisol levels in patients with chronic nonspecific lower back pain: A randomized controlled trial. Evid.-Based Complement. Altern. Med. 2017, 2017, 3140403. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zeng, Y.J.; Lin, Y.H.; Wang, Y.C.; Chang, J.H.; Wu, J.H.; Hsu, S.F.; Tsai, S.Y.; Lin, C.H.; Wen, Y.R. Laser acupuncture-induced analgesic effect and molecular alterations in an incision pain model: A comparison with electroacupuncture-induced effects. Laser Med. Sci. 2018, 33, 295–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, J.H.; Chang, W.D.; Hsieh, C.W.; Jiang, J.A.; Fang, W.; Shan, Y.C.; Chang, Y.C. Effect of low level laser stimulation on EEG. Evid.-Based Complement. Altern. Med. 2012, 2012, 951272. [Google Scholar] [CrossRef] [PubMed]
- Shan, Y.C.; Fang, W.; Chang, Y.C.; Chang, W.D.; Wu, J.H. Effect of near-infrared pulsed light on the human brain using electroencephalography. Evid.-Based Complement. Altern. Med. 2021, 2021, 6693916. [Google Scholar] [CrossRef] [PubMed]
- Convissar, R.A. Principles and Practise of Laser Dentistry, 2nd ed.; Mosby Elsevier: Saint Louis, MO, USA, 2015. [Google Scholar]
- Huang, Y.Y.; Chen, A.C.H.; Carroll, J.D.; Hamblin, M.R. Biphasic dose response in low level light therapy. Dose-Response 2009, 7, 358–383. [Google Scholar] [CrossRef]
- Huang, Y.Y.; Sharma, S.K.; Carroll, J.; Hamblin, M.R. Biphasic dose response in low level light therapy-an update. Dose-Response 2011, 9, 602–618. [Google Scholar] [CrossRef]
- Hülsbusch, M.; Hölscher, D.; Blazek, V. Spectral monte-carlo simulations of photon penetration in biotissue in visible and near infrared. In Proceedings of the Progress in Electromagnetics Research Symposium Proceedings, Prague, Czech Republic, 27–30 August 2007; Volume 483. [Google Scholar]
- Niwayama, M.; Yamashita, Y. Handbook of Modern Biophysics: Photon migration in tissue. In Application of Near Infrared Spectroscopy in Biomedicine; Jue, T., Masuda, K., Eds.; Springer: Berlin, Germany, 2013; pp. 21–35. [Google Scholar]
- Bashkatov, A.N.; Genina, E.A.; Kochubey, V.I.; Tuchin, V.V. Optical properties of human skin, subcutaneous and mucous tissues in the wavelength range from 400 to 2000 nm. J. Phys. D Appl. Phys. 2005, 38, 2543–2555. [Google Scholar] [CrossRef]
- Stolik, S.; Delgado, J.A.; Perez, A.; Anasagasti, L. Measurement of the penetration depths of red and near infrared light in human ‘‘ex vivo’’ tissues. J. Photochem. Photobiol. B 2000, 57, 90–93. [Google Scholar] [CrossRef]
- Barbosa, R.I.; Guirro, E.C.O.; Bachmann, L.; Brandino, H.E.; Guirro, R.R.J. Analysis of low-level laser transmission at wavelengths 660, 830 and 904 nm in biological tissue samples. J. Photochem. Photobiol. B 2020, 209, 111914. [Google Scholar] [CrossRef]
- Lilge, L.; Haw, T.; Wilson, B.C. Miniature isotropic optical fiber probes for quantitative light dosimetry in tissue. Phys. Med. Biol. 1993, 38, 215–230. [Google Scholar] [CrossRef] [PubMed]
- Hudson, E.J.; Stringer, M.R.; Staveren, H.J.V.; Smith, M.A. The development of radio-opaque, isotropic, fibre-optic probes for light dosimetry studies in photodynamic therapy. Phys. Med. Biol. 1993, 38, 1529–1536. [Google Scholar] [CrossRef]
- Hudson, D.E.; Hudson, D.O.; Wininger, J.M.; Richardson, B.D. Penetration of Laser Light at 808 and 980 nm in Bovine Tissue Samples. Photomed. Laser Surg. 2013, 31, 163–168. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lan, K.C.; Wang, C.Y.; Kuo, C.C.; Chang, S.C.; Lin, H.A.; Wu, X.Y.; Ding, J.Y.; Litscher, G. Effects of the new lift-thrust operation in laser acupuncture investigated by thermal imaging. Evid.-Based Complement. Alternat. Med. 2019, 2019, 4212079. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Enwemeka, C.S. Attenuation and penetration of visible 632.8 nm and invisible infrared 904 nm light in soft tissues. Laser Ther. 2000, 13, 95–101. [Google Scholar] [CrossRef] [Green Version]
- Sasaki, K.; Calderheadt, R.G.; Chin, I.; Inomata, K. To examine the adverse photothermal effects of extended dosage laser therapy in vivo on the skin and subcutaneous tissue in the rat model. Laser Ther. 1992, 4, 69–73. [Google Scholar] [CrossRef] [Green Version]
- Karu, T.I.; Kolyakov, S.F. Exact action spectra for cellular responses relevant to phototherapy. Photomed. Laser Surg. 2005, 23, 355–361. [Google Scholar] [CrossRef] [Green Version]
- Desmet, K.D.; Paz, D.A.; Corry, J.J.; Eells, J.T.; Wong-Riley, M.T.T.; Henry, M.M.; Buchmann, E.V.; Connelly, M.P.; Dovi, J.V.; Liang, H.L.; et al. Clinical and experimental applications of NIR-LED photobiomodulation. Photomed. Laser Surg. 2006, 24, 121–128. [Google Scholar] [CrossRef]
- Karu, T.I. Cellular and molecular mechanisms of photobiomodulation (low-power laser therapy). IEEE J. Sel. Top. Quantum Electron. 2014, 20, 143–148. [Google Scholar] [CrossRef]
- Hamblin, M.R.; Sousa, M.V.P.; Arany, P.R.; Carroll, J.D.; Patthoff, D. Low level laser (light) therapy and photobiomodulation: The path forward. In Proceedings of the SPIE Mechanisms for Low-Light Therapy X, San Francisco, CA, USA, 7–12 February 2015; Volume 9309, p. 930902. [Google Scholar]
- Liebert, A.D.; Bicknell, B.T.; Adams, R.D. Protein conformational modulation by photons: A mechanism for laser treatment effects. Med. Hypotheses 2014, 82, 275–281. [Google Scholar] [CrossRef]
- Henderson, T.A.; Morries, L.D. Near-infrared photonic energy penetration: Can infrared phototherapy effectively reach the human brain? Neuropsychiatr. Dis. Treat. 2015, 11, 2191–2208. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, A.C.H.; Arany, P.R.; Huang, Y.Y.; Tomkinson, E.M.; Saleem, T.; Yull, F.E.; Blackwell, T.S.; Hamblin, M.R. Low level laser therapy activates NF-κB via generation of reactive oxygen species in mouse embryonic fibroblasts. Proc. SPIE 2009, 7165, 71650. [Google Scholar] [CrossRef] [Green Version]
- Su, C.T.; Chen, C.M.; Chen, C.C.; Wu, J.H. Dose Analysis of Photobiomodulation Therapy in Stomatology. Evid.-Based Complement. Altern. Med. 2020, 2020, 8145616. [Google Scholar] [CrossRef] [PubMed]
- Meglinsky, I.V.; Matcher, S.J. Modelling the sampling volume for skin blood oxygenation measurements. Med. Biol. Eng. Comput. 2001, 39, 44–50. [Google Scholar] [CrossRef] [PubMed]
- Born, M.; Wolf, E. Principles of Optics: Electromagnetic Theory of Propagation, Interference and Diffraction of Light, 6th ed.; Pergamon Press: Oxford, UK, 1986. [Google Scholar]
- Kopola, H.K.; Lahti, A.; Myllylae, R.A.; Hannuksela, M. Two-channel fiber optic skin erythema meter. Opt. Eng. 1993, 32, 222–226. [Google Scholar] [CrossRef]
- Kirillin, M.Y.; Priezzhev, A.V.; Myllylä, R. Comparative analysis of sensitivity of different light-scattering techniques to blood oxygenation on the basis of multilayer tissue model. In Proceedings of the SPIE Saratov Fall Meeting 2005: Optical Technologies in Biophysics and Medicine VII, Saratov, Russian, 27–30 September 2005; Volume 6163, pp. 1–7. [Google Scholar]
- Reuss, J.L. Multilayer modeling of reflectance pulse oximetry. IEEE Trans. Biomed. Eng. 2005, 52, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Song, Y.; Hao, Q.; Kong, X.; Hu, L.; Cao, J.; Gao, T. Simulation of the recharging method of implantable biosensors based on a wearable incoherent light source. Sensors 2014, 14, 20687–20701. [Google Scholar] [CrossRef] [Green Version]
- Sayli, Ö.; Aksel, E.B.; Akin, A. Crosstalk and error analysis of fat layer on continuous wave near-infrared spectroscopy measurements. J. Biomed. Opt. 2008, 13, 1–11. [Google Scholar] [CrossRef] [Green Version]
- Henyey, L.G.; Greenstein, J.L. Diffuse radiation in the galaxy. Astrophys. J. 1941, 93, 70–83. [Google Scholar] [CrossRef]
- Toublanc, D. Henyey–Greenstein and Mie phase functions in Monte Carlo radiative transfer computations. Appl. Opt. 1996, 35, 3270–3274. [Google Scholar] [CrossRef]
- Hardy, A.C. Handbook of Colorimetry. Prepared by the Staff of the Color Measurement Laboratory of Massachusetts Institute of Technology; The Technology Press: Cambridge, UK, 1936. [Google Scholar]
- Buckley, W.R.; Grum, F. Reflection spectrophotometry III: Absorption characteristics and color of human skin. Arch. Dermatol. 1964, 89, 110–116. [Google Scholar] [CrossRef] [PubMed]
- Amaroli, A.; Arany, P.; Pasquale, C.; Benedicenti, S.; Bosco, A.; Ravera, S. Improving consistency of photobiomodulation therapy: A novel flat-top beam hand-piece versus standard gaussian probes on mitochondrial activity. Int. J. Mol. Sci. 2021, 22, 7788. [Google Scholar] [CrossRef] [PubMed]
- Su, C.T.; Chen, C.J.; Chen, C.M.; Chen, C.C.; Ma, S.H.; Wu, J.H. Optical profile: A key determinant of antibacterial efficacy of photodynamic therapy in dentistry. Photodiagn. Photodyn. Ther. 2021, 35, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Amaroli, A.; Pasquale, C.; Zekiy, A.; Utyuzh, A.; Benedicenti, S.; Signore, A.; Ravera, S. Photobiomodulation and oxidative stress: 980 nm diode laser light regulates mitochondrial activity and reactive oxygen species production. Oxid. Med. Cell. Longev. 2021, 2021, 6626286. [Google Scholar] [CrossRef]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Su, C.-T.; Chiu, F.-C.; Ma, S.-H.; Wu, J.-H. Optimization of Photobiomodulation Dose in Biological Tissue by Adjusting the Focal Point of Lens. Photonics 2022, 9, 350. https://doi.org/10.3390/photonics9050350
Su C-T, Chiu F-C, Ma S-H, Wu J-H. Optimization of Photobiomodulation Dose in Biological Tissue by Adjusting the Focal Point of Lens. Photonics. 2022; 9(5):350. https://doi.org/10.3390/photonics9050350
Chicago/Turabian StyleSu, Chuan-Tsung, Fu-Chien Chiu, Shih-Hsin Ma, and Jih-Huah Wu. 2022. "Optimization of Photobiomodulation Dose in Biological Tissue by Adjusting the Focal Point of Lens" Photonics 9, no. 5: 350. https://doi.org/10.3390/photonics9050350
APA StyleSu, C.-T., Chiu, F.-C., Ma, S.-H., & Wu, J.-H. (2022). Optimization of Photobiomodulation Dose in Biological Tissue by Adjusting the Focal Point of Lens. Photonics, 9(5), 350. https://doi.org/10.3390/photonics9050350






