New Generation Wearable Antenna Based on Multimaterial Fiber for Wireless Communication and Real-Time Breath Detection
Abstract
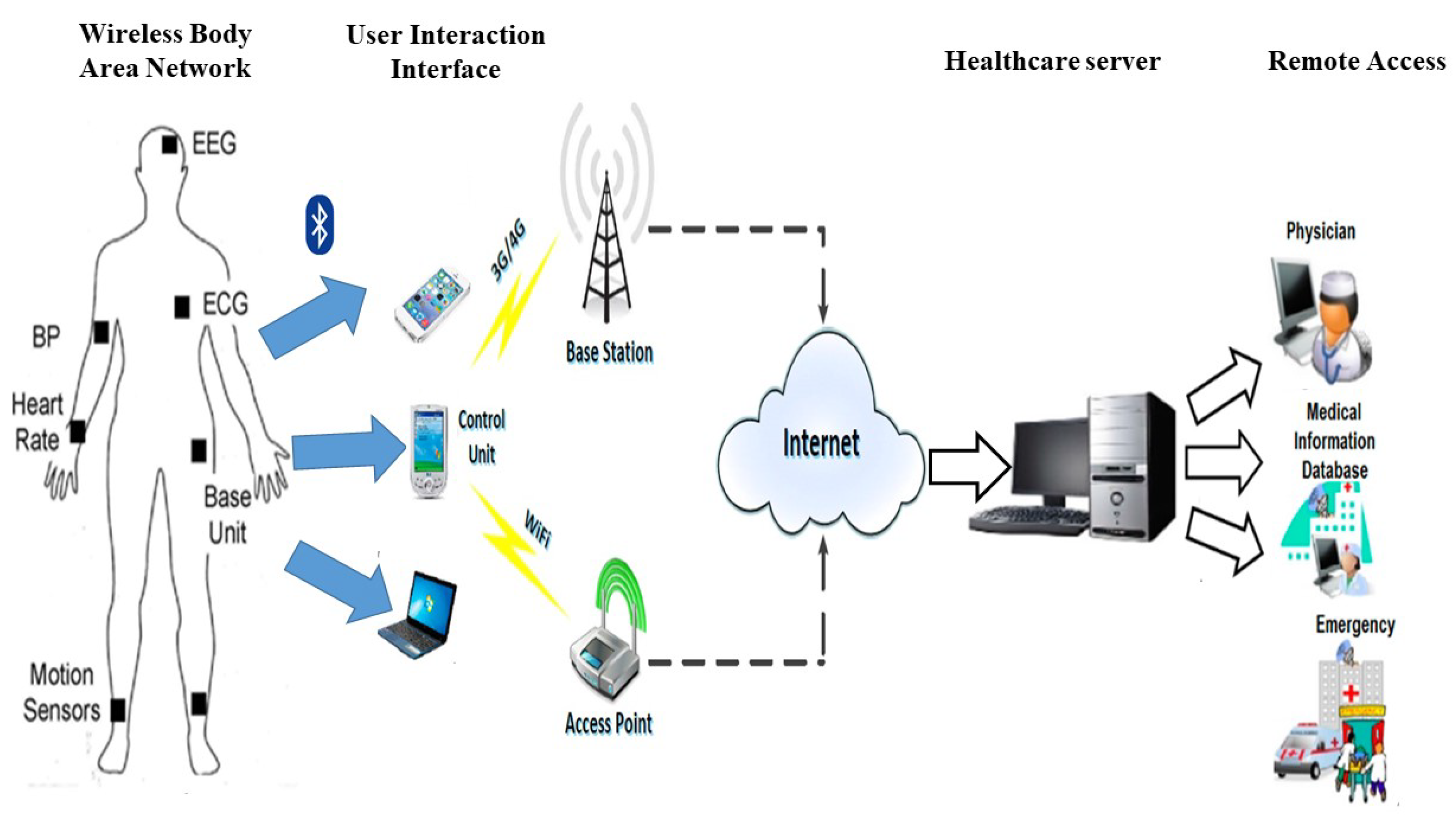
1. Introduction
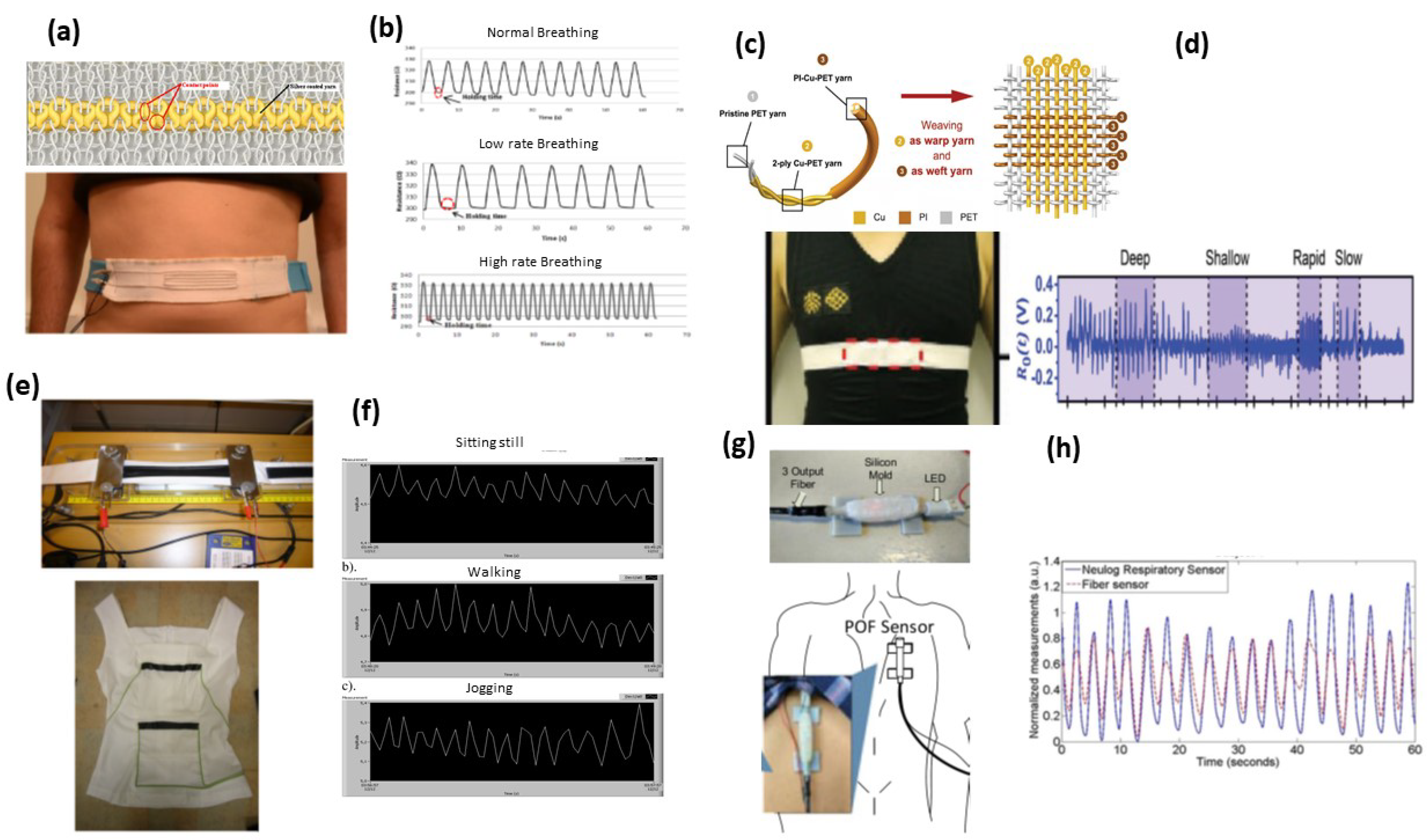
1.1. Smart Textile Biosensors and Physical Signals
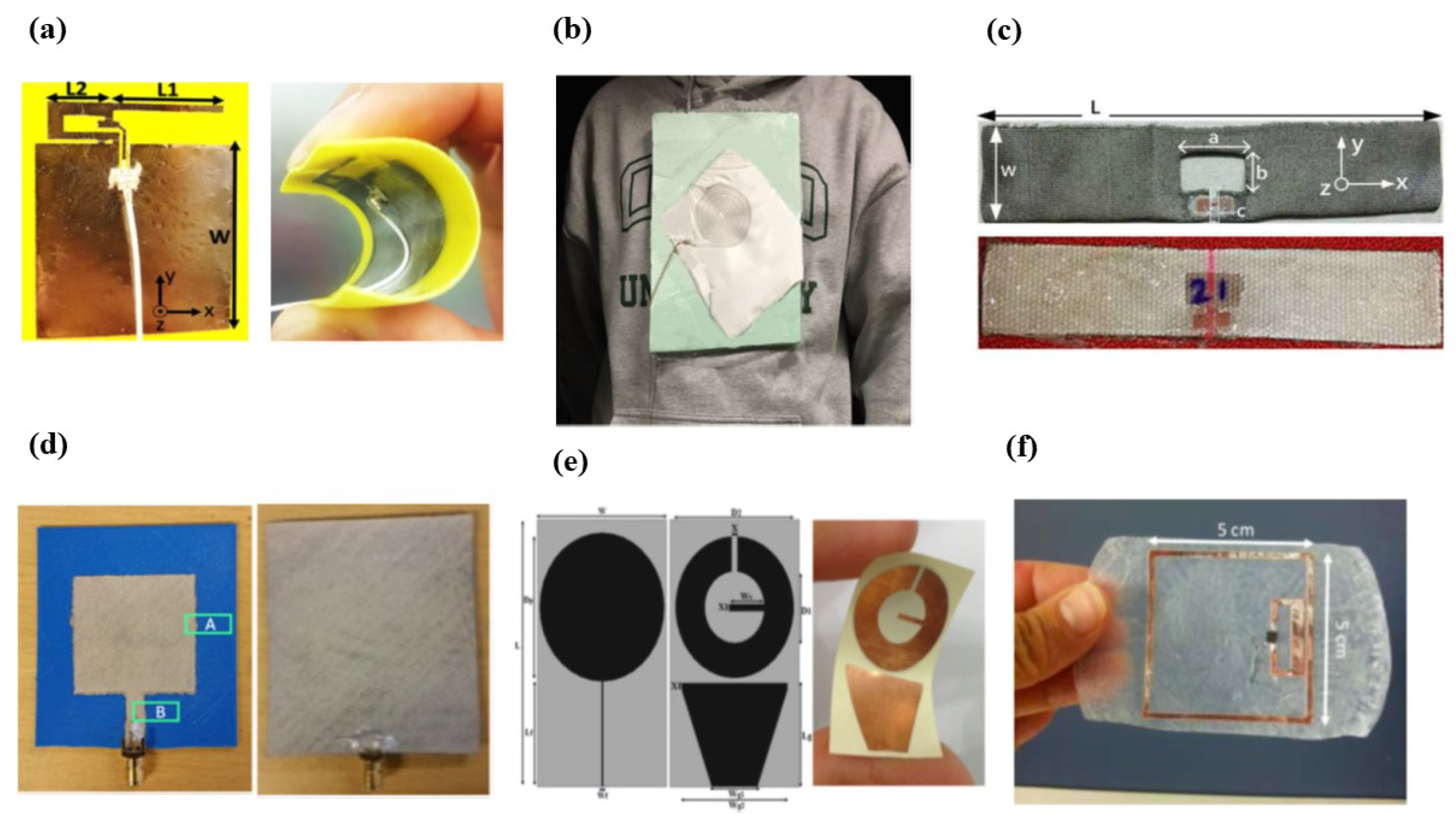
1.2. Wearable Antenna
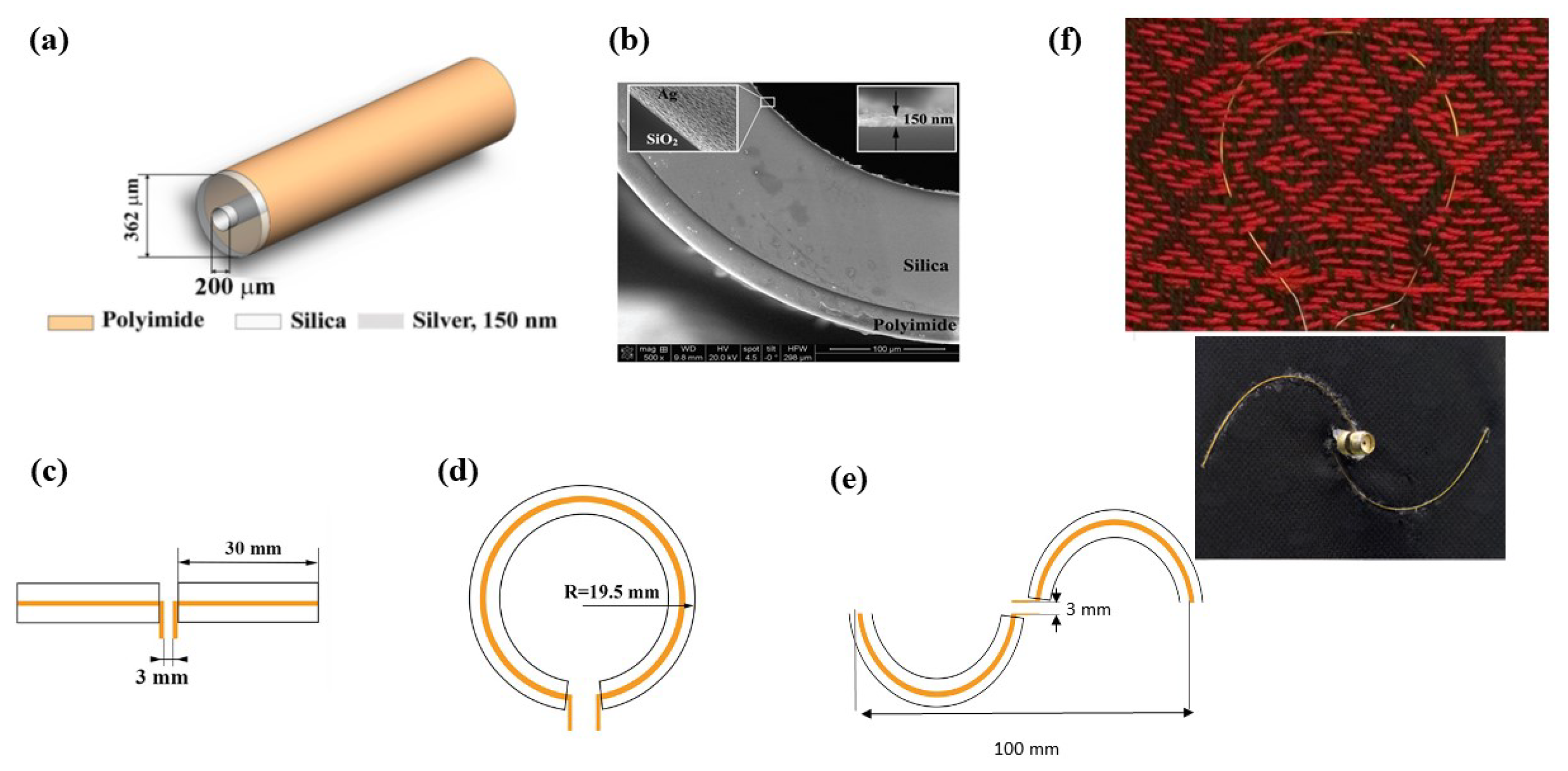
2. Smart Textile Based on Multimaterial Fiber Antenna: Design and Fabrication
2.1. Fabrication of the Fiber Antenna
2.2. Textile Integration
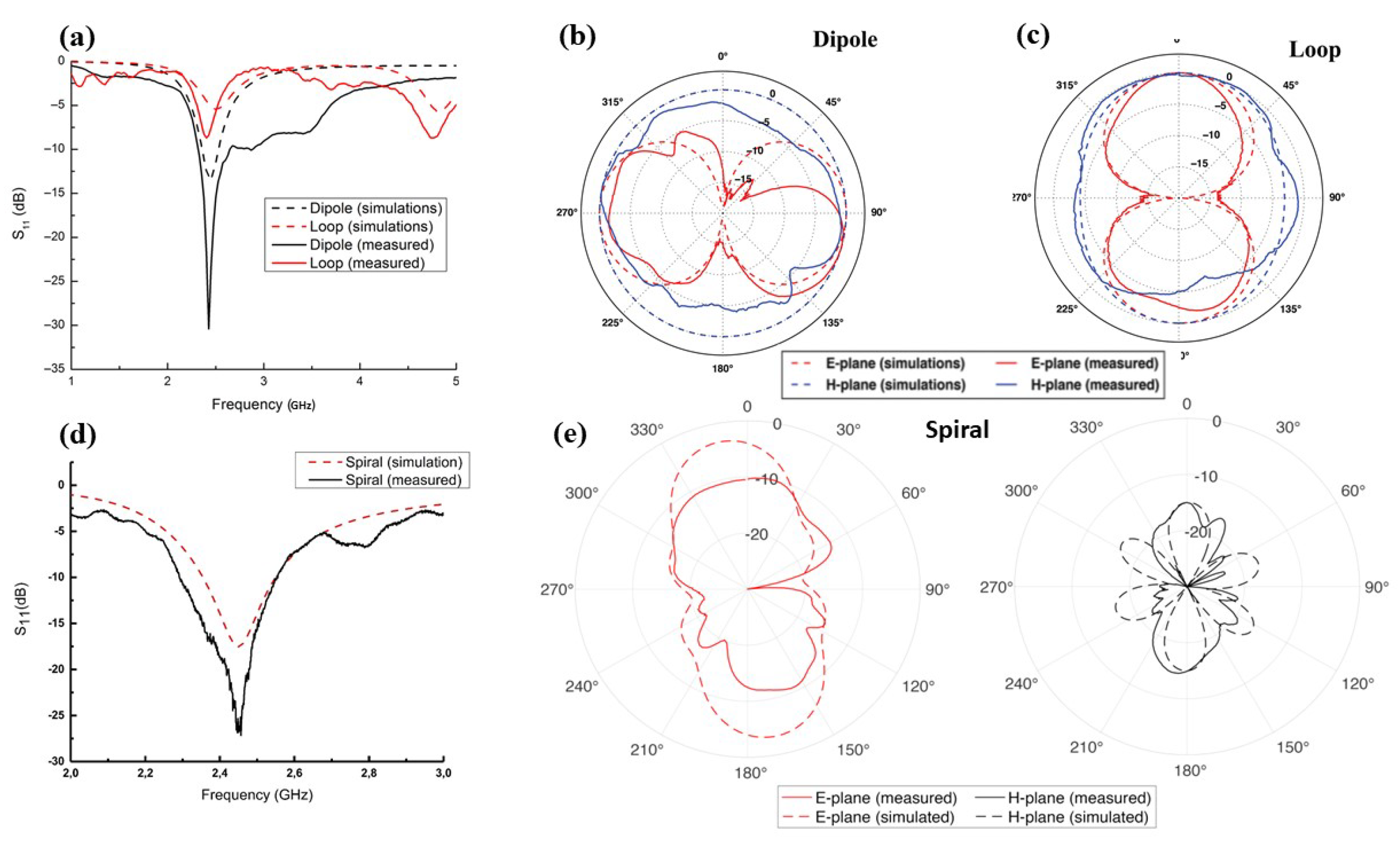
3. Emissive Properties of the Fiber Antenna in Free Space
3.1. Return Loss
3.2. Gain
3.3. Radiation Pattern
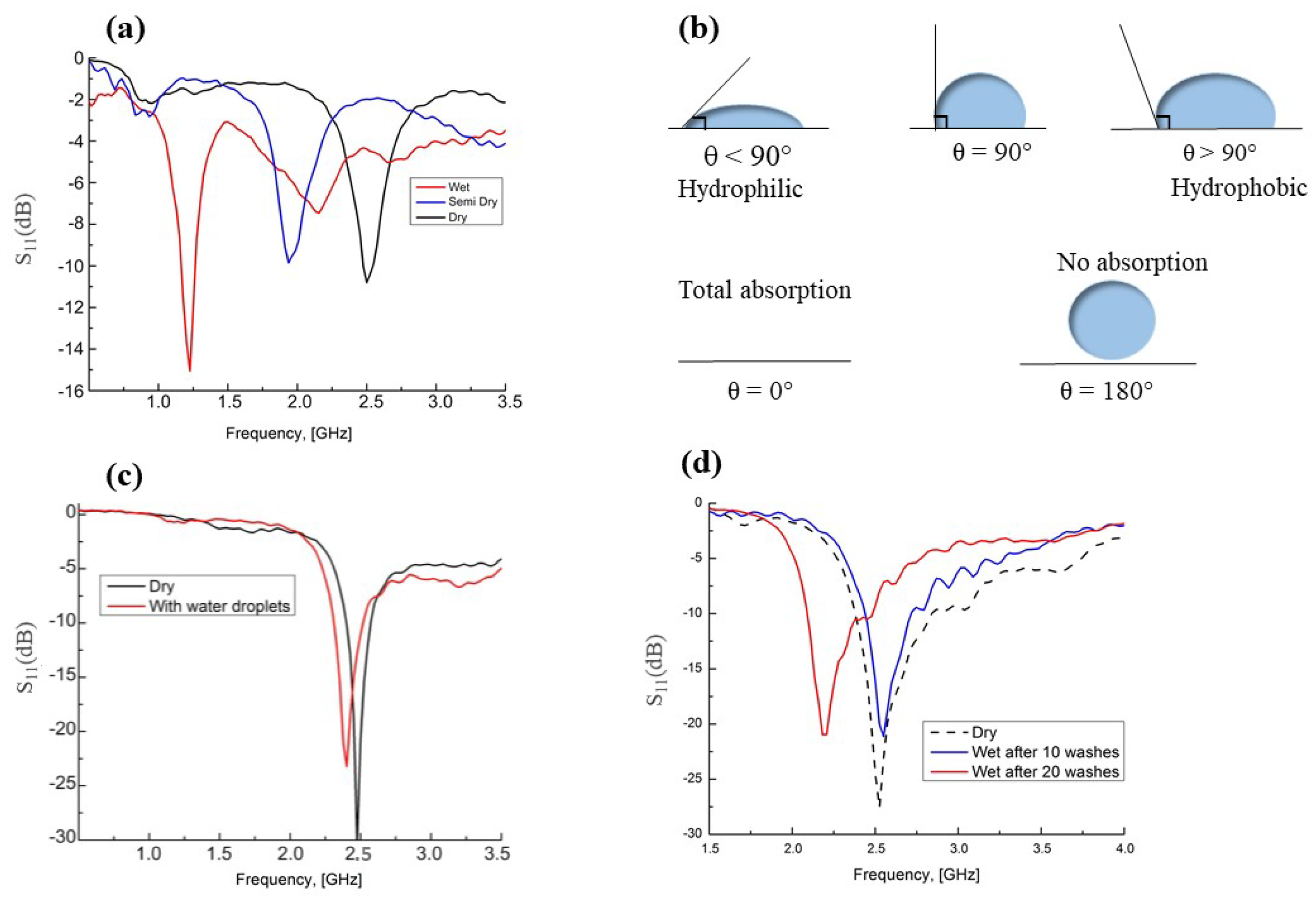
4. RF Smart Textile in Different Environmental Conditions
4.1. Influence of Moisture
4.2. Effect of Superhydrophobic Coating
4.3. Effect of Machine-Washing
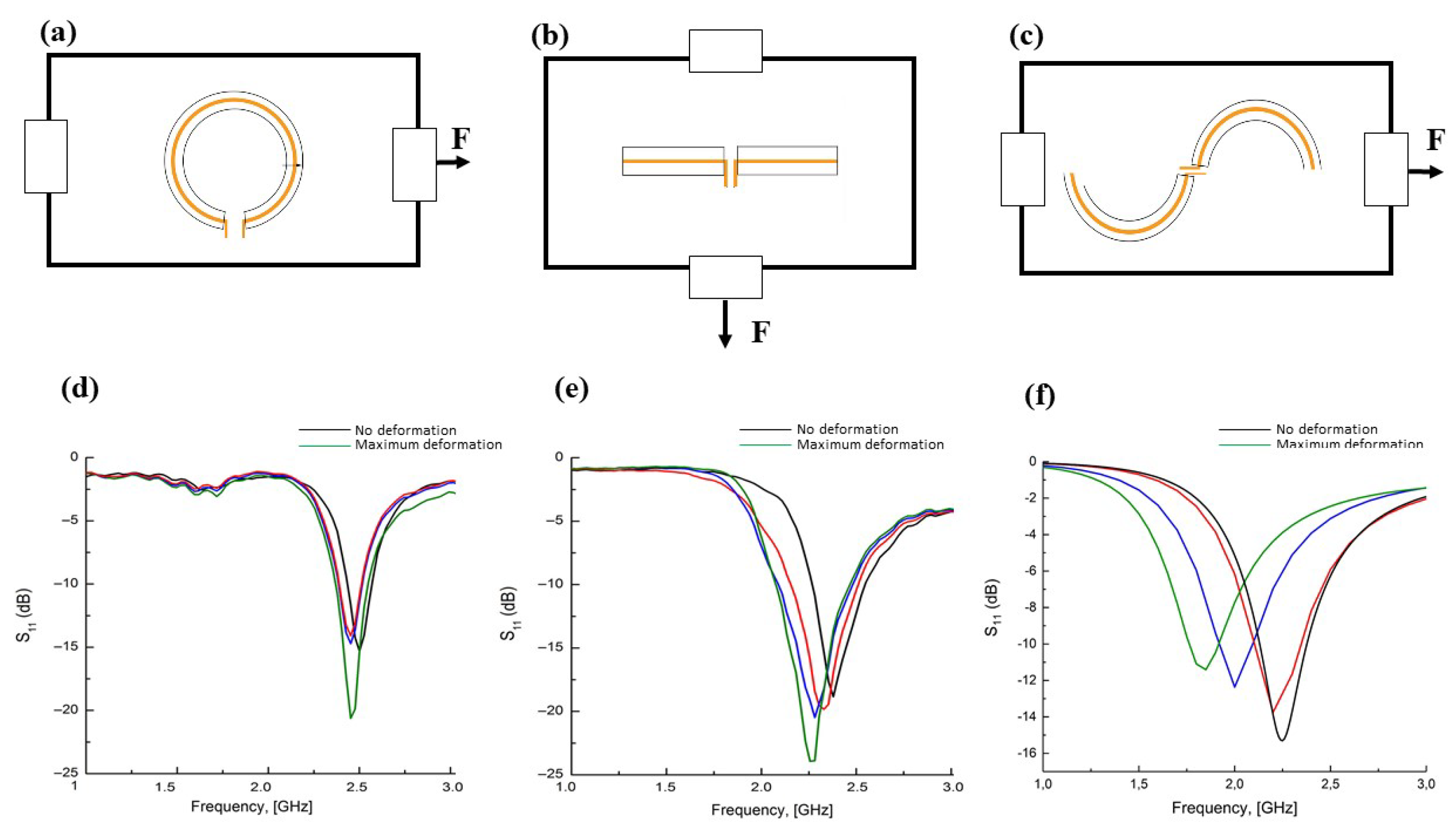
4.4. Influence of Conductive Medium: Frequency Shifts and Mechanical Stress
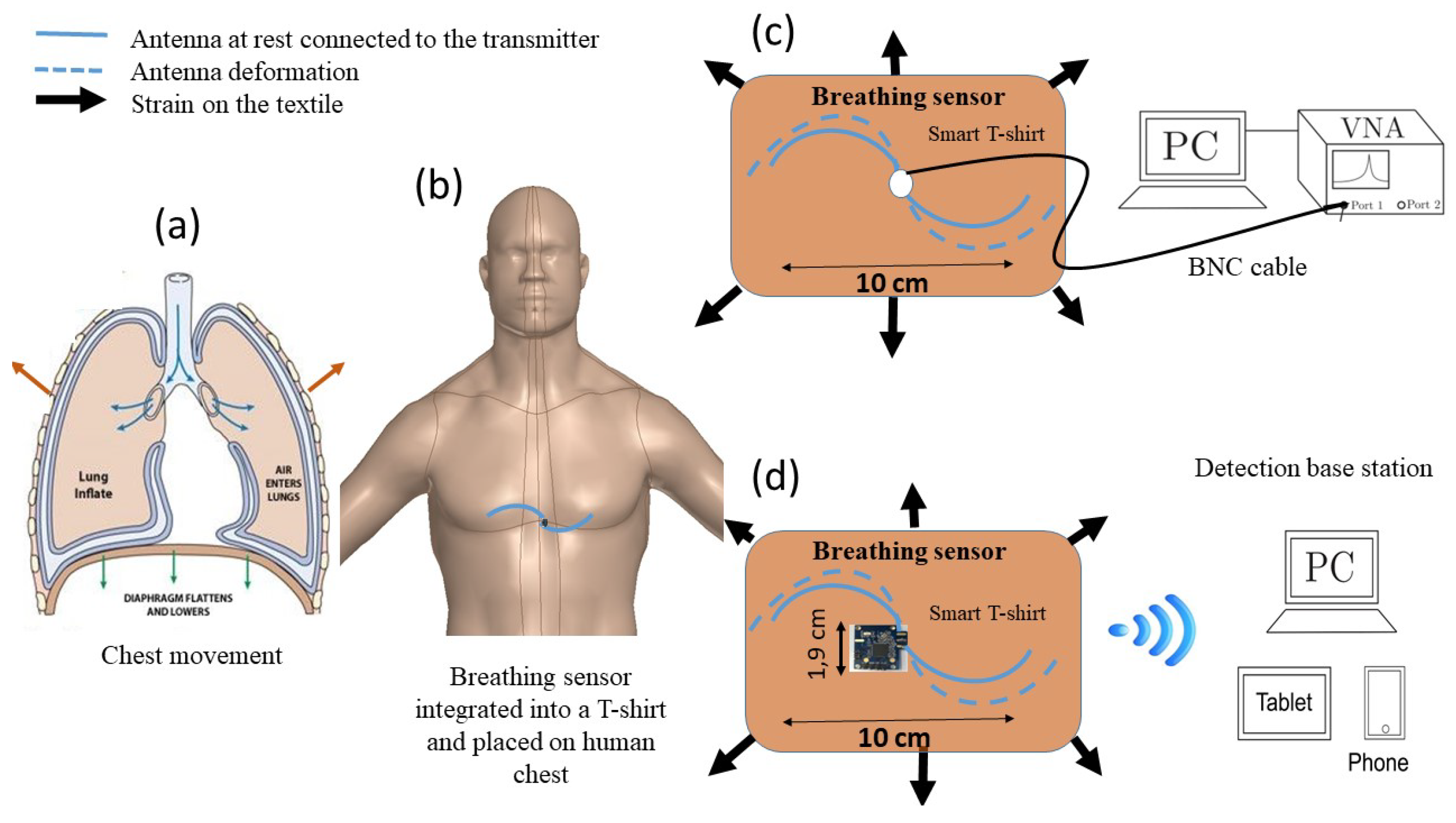
5. Multimaterial Fiber Antenna for Real Time Breath Detection
5.1. Breath Detection Mechanism
5.2. Breath Detection Based on Frequency Shift Measurements
5.3. Breath Detection Based on RSSI Measurements
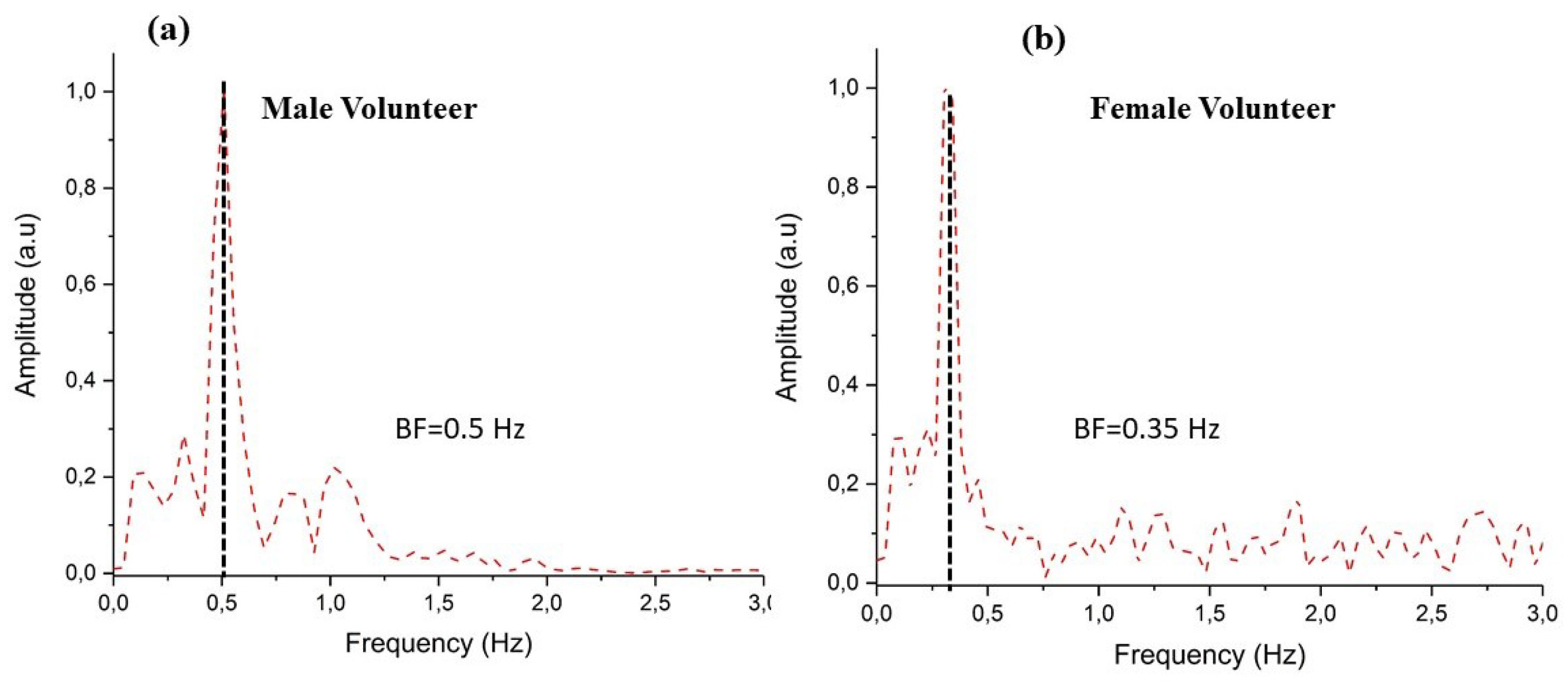
Breathing Patterns
6. Conclusions and Future Work
Author Contributions
Acknowledgments
Conflicts of Interest
References
- Majumder, S.; Mondal, T.; Jamal Deen, M. Wearable Sensors for Remote Health Monitoring. Sensors 2016, 17, 130. [Google Scholar] [CrossRef] [PubMed]
- Langereis, G.R.; Bouwstra, S.; Chen, W. Sensors, Actuators and Computing Architecture Systems for Smart Textiles. In Smart Textiles for Protection; Chapman, R., Ed.; Woodhead: Cambridge, UK, 2012; Volume 1, pp. 190–213. [Google Scholar]
- Koncar, V. Introduction to smart textiles and their applications. In Smart Textiles and their Applications; A Volume in Woodhead Publishing Series in Textiles; Woodhead Publishing: Cambridge, UK, 2016; pp. 1–8. [Google Scholar]
- Morris, D.; Schazmann, B.; Wu, Y.; Coyle, S.; Brady, S.; Hayes, J.; Slater, C.; Fay, C.; Lau, K.T.; Wallace, G.; et al. Wearable Sensors for Monitoring Sports Performance and Training. In Proceedings of the 5th International Summer School and Symposium on Medical Devices and Biosensors, Hong Kong, China, 1–3 June 2008; pp. 121–124. [Google Scholar]
- Berzowska, J. Very slowly animating textiles: Shimmering flower. In Proceedings of the 31th International Conference on Computer Graphics and Interactive Techniques, Los Angeles, CA, USA, 8–12 August 2004. [Google Scholar]
- Nayak, R.; Wang, L.; Padhye, R. Electronic textiles for military personnel. In Smart Fabrics and Wearable Technology in Electronic Textiles; Woodhead Publishing: Cambridge, UK, 2015; pp. 239–256. [Google Scholar]
- Cheng, J.; Amft, O.; Lukowicz, P. Active capacitive sensing: Exploring a new wearable sensing modality for activity recognition. In Proceedings of the 8th International Conference on Pervasive Computing, Helsinki, Finland, 17–20 May 2010. [Google Scholar]
- Linz, T.; Gourmelon, L.; Langereis, G. Contactless EMG sensors embroidered onto textile. In Proceedings of the 4th International Workshop Wearable Implantable Body Sensor Netw, (BSN’07), Aachen, Germany, 26–28 March 2007; Volume 13, pp. 29–34. [Google Scholar]
- Lofhede, J.; Seoane, F.; Thordstein, M. Soft textile electrodes for EEG monitoring. In Proceedings of the 10th IEEE International Conference on Information Technology and Applications in Biomedicine (ITAB), Corfu, Greece, 2–5 November 2010; pp. 1–4. [Google Scholar]
- Lofhede, J.; Seoane, F.; Thordstein, M. Textile electrodes for EEG recording—A pilot study. Sensors 2012, 12, 16907–16919. [Google Scholar] [CrossRef] [PubMed]
- Chi, Y.M.; Cauwenberghs, G. Wireless non-contact EEG/ECG electrodes for body sensor networks. In Proceedings of the International Conference on Body Sensor Netw, (BSN’10), Singapore, 7–9 June 2010; pp. 297–301. [Google Scholar]
- Omenetto, F.; Kaplan, D.; Amsden, J.; Dal Negro, L. Silk Based Biophotonic Sensors. U.S. Patent US2013/0330710 A1, 12 December 2013. [Google Scholar]
- Lee, J.; Kwon, H.; Seo, J.; Shin, S.; Koo, J.H.; Pang, C.; Son, S.; Kim, J.H.; Jang, Y.H.; Kim, D.E.; et al. Conductive fiber-based ultrasensitive textile pressure sensor for wearable electronics. Adv. Mater. 2015, 27, 2433. [Google Scholar] [CrossRef] [PubMed]
- Kinkeldei, T.; Zysset, C.; Cherenack, K.; Troster, G. A textile integrated sensor system for monitoring humidity and temperature. In Proceedings of the Solid-State Sensors, Actuators and Microsystems, Beijing, China, 5–9 June 2011. [Google Scholar]
- Halonen, T.; Romero, J.; Melero, J. GSM, GPRS and EDGE Performance: Evolution towards 3G/UMTS; John Wiley and Sons: Hoboken, NJ, USA, 2002. [Google Scholar]
- Salkintzis, K. Mobile Internet: Enabling Technologies and Services; CRC Press: Boca Raton, FL, USA, 2004. [Google Scholar]
- Dahlman, E.; Parkvall, S.; Skold, J.; Beming, P. 3G Evolution: HSPA and LTE for Mobile Broadband; Academic Press: Cambridge, MA, USA, 2010. [Google Scholar]
- Fieselmann, J.F.; Hendryx, M.S.; Helms, C.M.; Wakefield, D.S. Respiratory rate predicts cardiopulmonary arrest for internal medicine patients. J. Gen. Intern. Med. 1993, 8, 354–360. [Google Scholar] [CrossRef] [PubMed]
- Subbe, C.P.; Davies, R.G.; Williams, E.; Rutherford, P.; Gemmell, L. Effect of introducing the Modified Early Warning score on clinical outcomes, cardiopulmonary arrests and intensive care utilisation in acute medical admissions. Anaesthesia 2003, 58, 797–802. [Google Scholar] [CrossRef] [PubMed]
- Cretikos, M.; Chen, J.; Hillman, K.; Bellomo, R.; Finfer, S.; Flabouris, A. The objective medical emergency team activation criteria: A case-control study. Resuscitation 2007, 73, 62–72. [Google Scholar] [CrossRef] [PubMed]
- Murthy, R.; Pavlidis, I.; Tsiamyrtzis, P. Touchless monitoring of breathing function. In Proceedings of the 26th Annual International Conference of the IEEE Engineering in Medicine and Biology Society, San Francisco, CA, USA, 1–5 September 2004; Volume 2, pp. 1196–1199. [Google Scholar]
- Boyle, J.; Bidargaddi, N.; Sarela, A.; Karunanithi, M. Automatic Detection of Respiration Rate From Ambulatory Single-Lead ECG. IEEE Trans. Inf. Technol. Biomed. 2009, 13, 890–896. [Google Scholar] [CrossRef] [PubMed]
- Lee, Y.-D.; Chung, W.-Y. Wireless Sensor Network Based Wearable Smart Shirt for Ubiquitous Health and Activity Monitoring. Sens. Actuators B Chem. 2009, 140, 390–395. [Google Scholar] [CrossRef]
- Al Ahmadi, M. Piezoelectric extraction of ECG signal. Sci. Rep. 2016, 6, 37093. [Google Scholar] [CrossRef] [PubMed]
- Zhu, F.; Hu, J.; Zhang, H.; Shi, J.; Yang, X. Breathing Measurement on the Basis of Contact Resistance of Cross-overlapping Conductive Yarns. Fiber Polym. 2017, 18, 369–375. [Google Scholar] [CrossRef]
- Mečņika, V.; Hoerr, M.; Krieviņš, I.; Schwarz, A. Smart textiles for healthcare: Applications and technologies. In Rural Environment. Education. Personality (REEP), Proceedings of the International Scientific Conference (Latvia); Latvia University of Agriculture: Jelgava, Latvia, 2014; pp. 150–161. [Google Scholar]
- Atalay, O.; Kennon, W.R.; Demirok, E. Weft-knitted strain sensor for monitoring respiratory rate and its electro-mechanical modeling. IEEE Sens. J. 2015, 15, 110–122. [Google Scholar] [CrossRef]
- Zhao, Z.; Yan, C.; Liu, Z.; Fu, X.; Peng, L.M.; Hu, Y.; Zheng, Z. Machine-Washable Textile Triboelectric Nanogenerators for Effective Human Respiratory Monitoring through Loom Weaving of Metallic Yarns. Adv. Mater. 2016, 28, 10267–10274. [Google Scholar] [CrossRef] [PubMed]
- Guo, L.; Berglin, L.; Li, Y.J.; Mattila, H.; Mehrjerdi, A.K.; Skrifvars, M. Disappearing Sensor’-Textile Based Sensor for Monitoring Breathing. In Proceedings of the 2011 International Conference on Control, Automation and Systems Engineering (CASE), Singapore, 30–31 July 2011; pp. 1–4. [Google Scholar]
- Yoo, W.J.; Jang, K.W.; Seo, J.K.; Heo, J.Y.; Moon, J.S.; Park, J.-Y.; Lee, B. Development of Respiration Sensors Using Plastic Optical Fiber for Respiratory Monitoring Inside MRI System. J. Opt. Soc. Korea 2010, 14, 235. [Google Scholar] [CrossRef]
- Ahmed, N.; Scully, P.; Vaughan, J.; Wilson, C.B.; Ozanyan, K. Polymer Optical Fibre Sensor for Measuring Breathing Rate of Lying Person. In Proceedings of the 8th International Conference on Sensing Technology, Liverpool, UK, 2–4 September 2014. [Google Scholar]
- Dziuda, L. Fiber-optic sensors for monitoring patient physiological parameters: A review of applicable technologies and relevance to use during magnetic resonance imaging procedures. J. Biomed. Opt. 2015, 20, 010901. [Google Scholar] [CrossRef] [PubMed]
- Davis, C.; Mazzolini, A.; Murphy, D. A new fibre sensor for respiratory monitoring. Aust. Phys. Eng. Sci. Med. 1997, 20, 214–219. [Google Scholar] [CrossRef]
- Kam, W.; Mohammed, W.S.; Leen, G.; O’Keeffe, M.; O’Sullivan, K.; O’Keeffe, S.; Lewis, E. Compact and Low-Cost Optical Fiber Respiratory Monitoring Sensor Based on Intensity Interrogation. J. Lightw. Technol. 2017, 35, 4567–4573. [Google Scholar] [CrossRef]
- Presti, D.L.; Massaroni, C.; Formica, D.; Saccomandi, P.; Giurazza, F.; Caponero, M.A.; Schena, E. Smart Textile Based on 12 Fiber Bragg Gratings Array for Vital Signs Monitoring. IEEE Sens. J. 2017, 17, 6037–6043. [Google Scholar] [CrossRef]
- Grillet, A.; Kinet, D.; Witt, J.; Schukar, M.; Krebber, K.; Pirotte, F.; Depré, A. Optical fiber sensors embedded into medical textiles for healthcare monitoring. IEEE Sens. J. 2008, 8, 1215–1222. [Google Scholar] [CrossRef]
- Zheng, W.; Tao, X.; Zhu, B.; Wang, G.; Hui, C. Fabrication and evaluation of a notched polymer optical fiber fabric strain sensor and its application in human respiration monitoring. Text. Res. J. 2014, 84, 1791–1802. [Google Scholar] [CrossRef]
- Osman, M.A.R.; Abd Rahim, M.K.; Samsuri, N.A.; Salim, H.A.M.; Ali, M.F. Embroidered Fully Textile Wearable Antenna for Medical Monitoring Applications. Prog. Electromagn. Res.-Pier. 2011, 117, 321–337. [Google Scholar] [CrossRef]
- Salvado, R.; Loss, C.; Pinho, P.; Goncalves, R. Textile materials for the design of wearable antennas: A survey. Sensors 2012, 12, 15841–15857. [Google Scholar] [CrossRef] [PubMed]
- Karimi, M.A.; Shamim, A. A flexible inkjet printed antenna for wearable electronics applications. In Proceedings of the 2016 IEEE International Symposium on Antennas and Propagation (APSURSI), Fajardo, Puerto Rico, 26 June–1 July 2016; pp. 1935–1936. [Google Scholar]
- Bartone, C.G.; Moore, L.; Kohli, M. An e-textile antenna for body area network. In Proceedings of the 2016 IEEE International Symposium on Antennas and Propagation (APSURSI), Fajardo, Puerto Rico, 26 June–1 July 2016; pp. 999–1000. [Google Scholar]
- Kazmi, A.; Virkki, J.; Bjrninen, T.; Ukkonen, L. Performance of silver-based textile uhf passive rfid tags after recurrent washing. In Proceedings of the 2016 IEEE International Symposium on Antennas and Propagation (APSURSI), Fajardo, Puerto Rico, 26 June–1 July 2016; pp. 939–940. [Google Scholar]
- Rizwan, M.; Khan, M.W.A.; Sydanheimo, L.; Virkki, J.; Ukkonen, L. Flexible and Stretchable Brush-Painted Wearable Antenna on a Three-Dimensional (3-D) Printed Substrate. IEEE Antennas Wirel. Propag. Lett. 2017, 16, 3108–3112. [Google Scholar] [CrossRef]
- Zahran, S.R.; Gaafar, A.; Abdalla, M.A. A flexible uwb low profile antenna for wearable applications. In Proceedings of the 2016 IEEE International Symposium on Antennas and Propagation (APSURSI), Fajardo, Puerto Rico, 26 June–1 July 2016; pp. 1931–1932. [Google Scholar]
- Milici, S.; Amendola, S.; Bianco, A.; Marrocco, G. Epidermal rfid passive sensor for body temperature measurements. In Proceedings of the 2014 IEEE RFID Technology and Applications Conference (RFID-TA), Tampere, Finland, 8–9 September 2014; pp. 140–144. [Google Scholar]
- Occhiuzzi, C.; Ajovalasit, A.; Sabatino, M.A.; Dispenza, C.; Marrocco, G. Rfid epidermal sensor including hydrogel membranes for wound monitoring and healing. In Proceedings of the 2015 IEEE International Conference on RFID (RFID), San Diego, CA, USA, 15–17 April 2015; pp. 182–188. [Google Scholar]
- Hertleer, C.; Rogier, H.; Member, S.; Vallozzi, L.; Langenhove, L.V. A Textile Antenna for Off-Body Communication Integrated into Protective Clothing for Firefighters. IEEE Trans. Adv. Pack. 2009, 57, 919–925. [Google Scholar] [CrossRef]
- Toivonen, M.; Bjorninen, T.; Sydanheimo, L.; Ukkonen, L.; RahmatSamii, Y. Impact of moisture and washing on the performance of embroidered UHF RFID tags. IEEE Antennas Wirel. Propag. Lett. 2013, 12, 1590–1593. [Google Scholar] [CrossRef]
- Rishani, N.R.; Shubair, R.M.; Aldabbagh, G. On the design of wearable and epidermal antennas for emerging medical applications. In Proceedings of the 2017 Sensors Networks Smart and Emerging Technologies (SENSET), Beirut, Lebanon, 12–14 September 2017; pp. 1–4. [Google Scholar]
- Amendola, S.; Marrocco, G. Optimal performance of epidermal antennas for uhf radio frequency identification and sensing. IEEE Trans. Antennas Propag. 2017, 65, 473–481. [Google Scholar] [CrossRef]
- Bayindir, M.; Shapira, O.; Viens, J.; Abouraddy, A.; Joannopoulos, J.D.; Fink, Y. Integrated fibers for self-monitored optical transport. Nat. Mater. 2005, 4, 820–825. [Google Scholar] [CrossRef]
- Sorin, F.; Abouraddy, A.F.; Orf, N.; Shapira, O.; Viens, J.; Arnold, J.; Joannopoulos, J.D.; Fink, Y. Multimaterial photodetecting fibers: A geometric and structural study. Adv. Mater. 2007, 19, 3872–3877. [Google Scholar] [CrossRef]
- Gorgutsa, S.; Belanger-Garnier, V.; Ung, B.; Viens, J.; Gosselin, B.; LaRochelle, S.; Messaddeq, Y. Novel wireless-communicating textiles made from multi-material and minimally-invasive fibers. Sensors 2014, 14, 19260–19274. [Google Scholar] [CrossRef] [PubMed]
- Gorgutsa, S.; Blais-Roberge, M.; Belanger-Garnier, V.; Viens, J.; LaRochelle, S.; Messaddeq, Y. User-Interactive and Wireless-Communicating RF Textiles. Adv. Mater. Technol. 2016, 1, 1600032. [Google Scholar] [CrossRef]
- Benet, W.E. The mechanism of the reaction of the Tollen reagent. J. Chem. Res. 2011, 35, 675–677. [Google Scholar] [CrossRef]
- Fawwaz, T.U.; Michelssen, E.; Ravaioli, U. Fondamental of Applied Electromagnetics, 6th ed.; Pearson: Hong Kong, China, 2010; pp. 33–37. [Google Scholar]
- Gorgutsa, S.; Khalil, M.; Belanger-Garnier, V.; Viens, J.; Gosselin, B.; LaRochelle, S.; Messaddeq, Y. Emissive Properties of Wearable Wireless-Communicating Textiles Made From Multimaterial Fibers. IEEE Trans. Antennas Propag. 2016, 64, 2457–2464. [Google Scholar] [CrossRef]
- Lesnikowski, J. Przeglad Elektrotechniczny (Electrical Review); R. 88 NR 3a; SIGMA-NOT: Warszawa, Poland, 2012; ISSN 0033-2097. [Google Scholar]
- Shaw, J.A. Radiometry and the Friis Transmission Equation. Am. J. Phys. 2013, 81, 33–37. [Google Scholar] [CrossRef]
- Guay, P.; Gorgutsa, S.; LaRochelle, S.; Messaddeq, Y. Wearable Contactless Respiration Sensor Based on Multi-Material Fibers Integrated into Textile. Sensors 2017, 17, 1050. [Google Scholar] [CrossRef] [PubMed]
- Gorgutsa, S.; Bachus, K.; LaRochelle, S.; Oleschuk, R.D.; Messaddeq, Y. Flexible and reversibly deformable radio-frequency antenna based on stretchable SWCNTs/PANI/Lycra conductive fabric. Smart Mater. Struct. 2016, 25, 115027. [Google Scholar] [CrossRef]
- Moore, R.K. Effects of a Surrounding Conducting Medium on Antenna Analysis. IEEE Trans. Antennas Propag. 1963, 11, 216–225. [Google Scholar] [CrossRef]
- Malmberg, C.G.; Maryott, A.A. Dielectric constant of water from 0 to 100 C. J. Res. Natl. Bur. Stand. 1956, 56, 2641. [Google Scholar] [CrossRef]
- Ivšić, B.G.; Golemac, G.; Bonefačić, D. Performance of wearable antenna exposed to adverse environmental conditions. In Proceedings of the ICECom 2013, Dubrovnik, Croatia, 14–16 October 2013; pp. 1–4. [Google Scholar]
- Jaehoon, K.; Rahmat-Samii, Y. Implanted antennas inside a human body: Simulations, designs, and characterizations. IEEE Trans. Microw. Theory Technol. 2004, 52, 1934–1943. [Google Scholar]
- Karacolak, T.; Hood, A.Z.; Topsakal, E. Design of a dual-band implantable antenna and development of skin mimicking gels for continuous glucose monitoring. IEEE Trans. Microw. Theory Technol. 2008, 56, 1001–1008. [Google Scholar] [CrossRef]
- Ito, K. Human body phantoms for evaluation of wearable and implantable antennas. In Proceedings of the 2nd European Conference on Antennas and Propagation, EuCAP 2007, Edinburgh, UK, 11–16 November 2007; pp. 1–6. [Google Scholar]
- Roudjane, M.; Bellemare-Rousseau, S.; Khalil, M.; Gorgutsa, S.; Miled, A.; Messaddeq, Y. A Portable Wireless Communication Platform Based on a Multi-Material Fiber Sensor for Real-Time Breath Detection. Sensors 2018, 18, 973. [Google Scholar] [CrossRef] [PubMed]
- 3D Content Central. Human Heart. Available online: http://www.3dcontentcentral.com (accessed on 6 February 2018).
- FCC. Body Tissue Dielectric Parameters. Available online: https://www.fcc.gov/general/body-tissue-dielectric-parameters (accessed on 6 February 2018).
- Italian National Research Council. Body Tissue Dielectric Parameters. Available online: http://niremf.ifac.cnr.it/tissprop/htmlclie/htmlclie.php (accessed on 6 February 2018).
- Harrington, R.F. Time-Harmonic Electromagnetic Fields; McGraw-Hill: NewYork, NY, USA, 1961. [Google Scholar]
- Tuovinen, T.; Berg, M.; Iinatti, J. Analysis of the impedance behaviour for broadband dipoles in proximity of a body tissue: Approach by using antenna equivalent circuits. Prog. Electromagn. Res.-Pier 2014, 59, 135–150. [Google Scholar] [CrossRef]
- Moll, J.M.; Wright, V. An objective clinical study of chest expansion. Ann. Rheum. Dis. 1972, 31, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Gabriel, C.; Gabriel, S. Compilation of the Dielectric Properties of Body Tissues at RF and Microwave Frequencies; Armstrong Laboratory (AFMC), Occupational and Environmental Health Directorate, Radiofrequency Radiation Division Brooks Air Force Base: San Antonio, TX, USA, 1998. [Google Scholar]
- Ravichandran, R.; Saba, E.; Chen, K.-Y.; Goel, M.; Gupta, S.; Patel, S.N. WiBreathe: Estimating Respiration Rate Using Wireless Signals in Natural Settings in the Home. In Proceedings of the 2015 IEEE International Conference on Pervasive Computing and Communications (PerCom), St. Louis, MO, USA, 23–27 March 2015; pp. 131–139. [Google Scholar]
- Patwari, N.; Wilson, J.; Ananthanarayanan, S.; Kasera, S.K.; Westenskow, D.R. Monitoring Breathing via Signal Strength in Wireless Networks. IEEE Trans. Mob. Comput. 2014, 13, 1774–1786. [Google Scholar] [CrossRef]
- Kaltiokallio, O.; Yigitler, H.; Jantti, R.; Patwari, N. Non-invasive respiration rate monitoring using a single COTS TX-RX pair. In Proceedings of the 13th International Symposium on Information Processing in Sensor Networks, Berlin, Germany, 15–17 April 2014; pp. 59–69. [Google Scholar]
- Kaltiokallio, O.; Yigitler, H.; Jantti, R.; Patwari, N. Catch a Breath: Non-invasive Respiration Rate Monitoring via Wireless Communication. arXiv, 2013; arXiv:1307.0084. [Google Scholar]

| Smart T-Shirt | Sensor | Measured Parameter | Detection | Cons | Pros |
|---|---|---|---|---|---|
| Platform 1 | Spiral fiber antenna connected to an SMA | Frequency shift via return Loss | Vector Network Analyzer (VNA) |
|
|
| Platform 2 | Spiral fiber antenna connected to a Bluetooth transmitter | RSSI | Wireless communication with a portable base station |
|
|
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Roudjane, M.; Khalil, M.; Miled, A.; Messaddeq, Y. New Generation Wearable Antenna Based on Multimaterial Fiber for Wireless Communication and Real-Time Breath Detection. Photonics 2018, 5, 33. https://doi.org/10.3390/photonics5040033
Roudjane M, Khalil M, Miled A, Messaddeq Y. New Generation Wearable Antenna Based on Multimaterial Fiber for Wireless Communication and Real-Time Breath Detection. Photonics. 2018; 5(4):33. https://doi.org/10.3390/photonics5040033
Chicago/Turabian StyleRoudjane, Mourad, Mazen Khalil, Amine Miled, and Younés Messaddeq. 2018. "New Generation Wearable Antenna Based on Multimaterial Fiber for Wireless Communication and Real-Time Breath Detection" Photonics 5, no. 4: 33. https://doi.org/10.3390/photonics5040033
APA StyleRoudjane, M., Khalil, M., Miled, A., & Messaddeq, Y. (2018). New Generation Wearable Antenna Based on Multimaterial Fiber for Wireless Communication and Real-Time Breath Detection. Photonics, 5(4), 33. https://doi.org/10.3390/photonics5040033





