3D Printed Galilean Telescope for Low-Vision Patients †
Abstract
1. Introduction
2. Galilean Telescope Fabrication
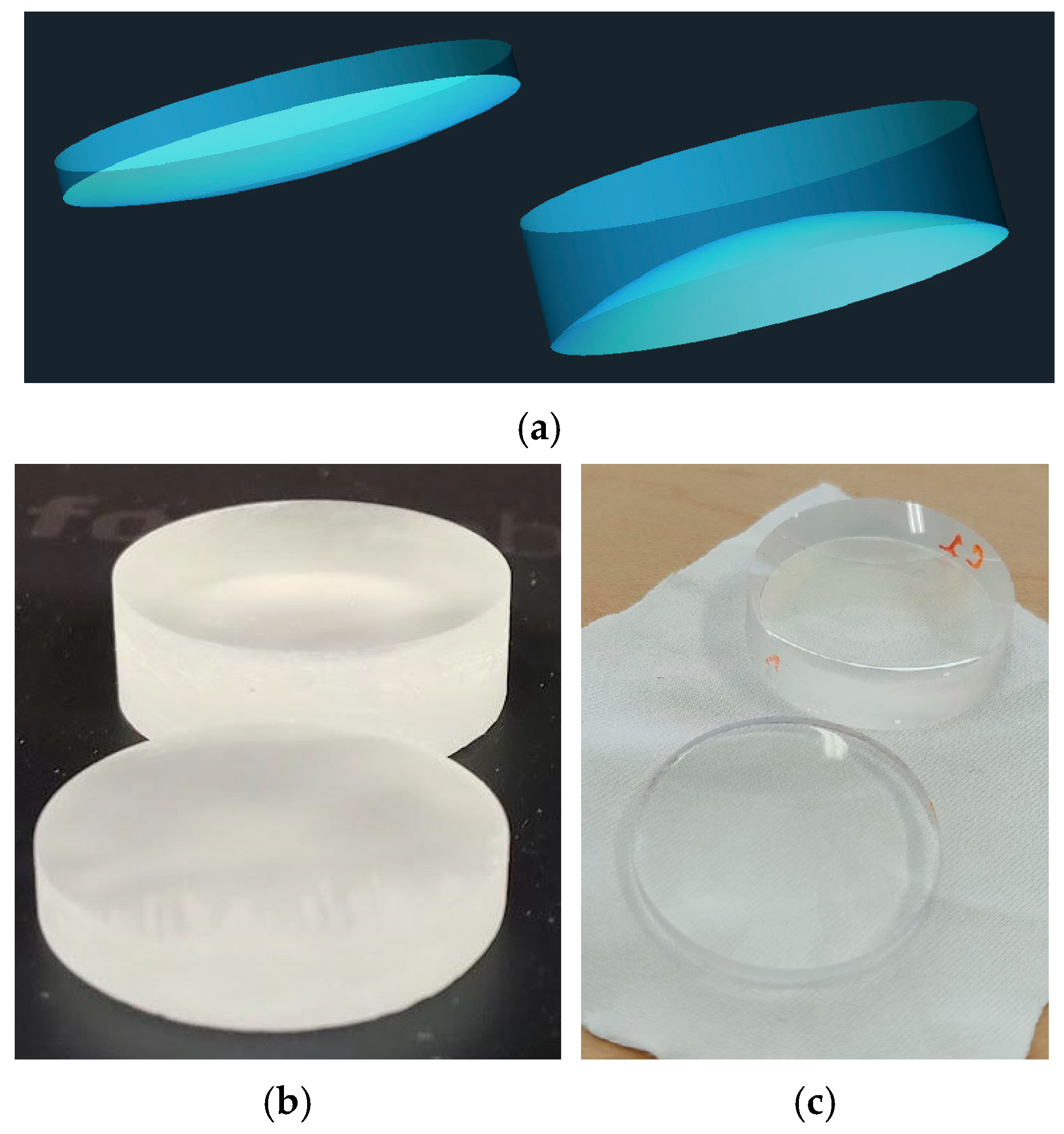
2.1. Lens Selection
2.2. Optical Fabrication
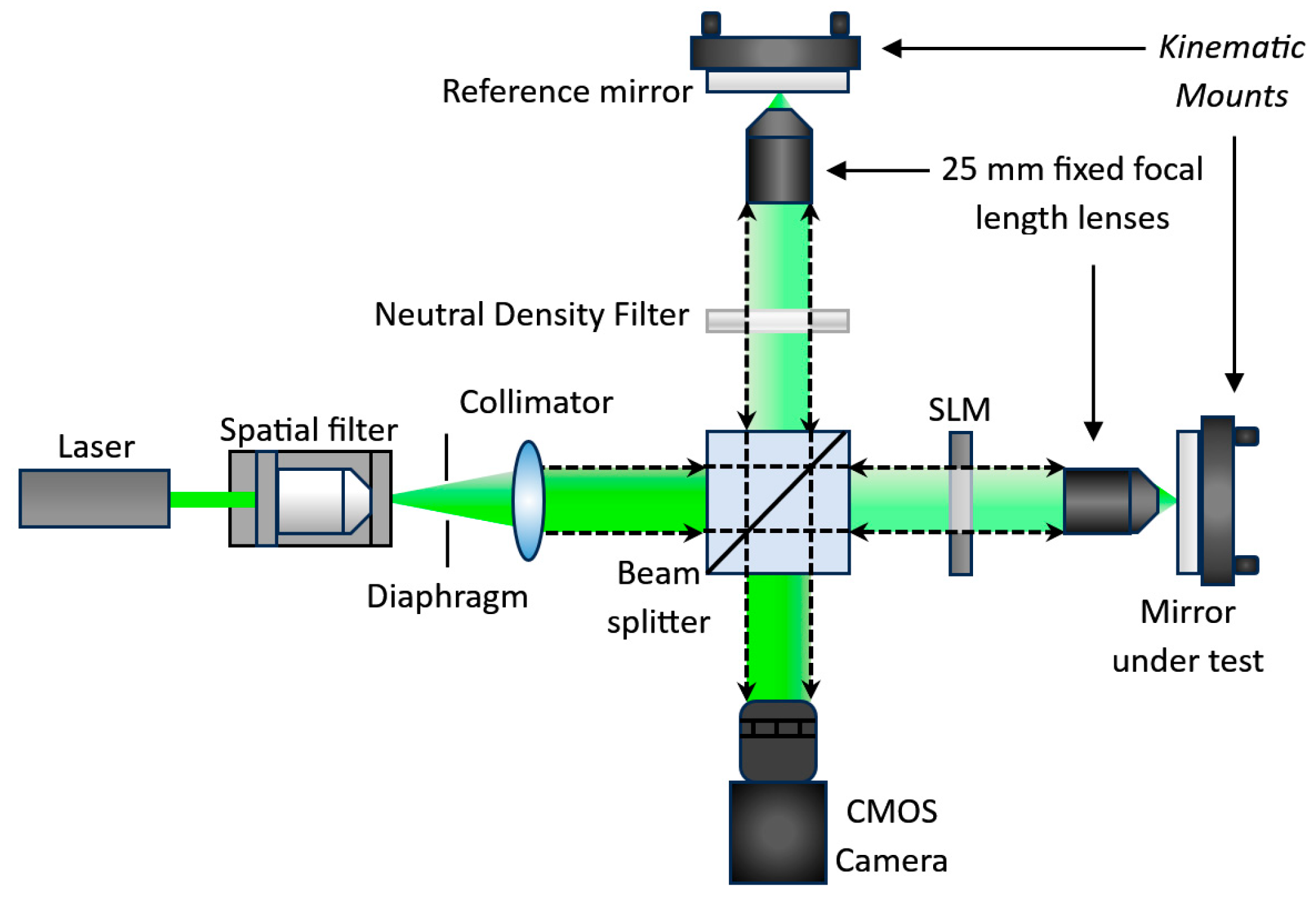
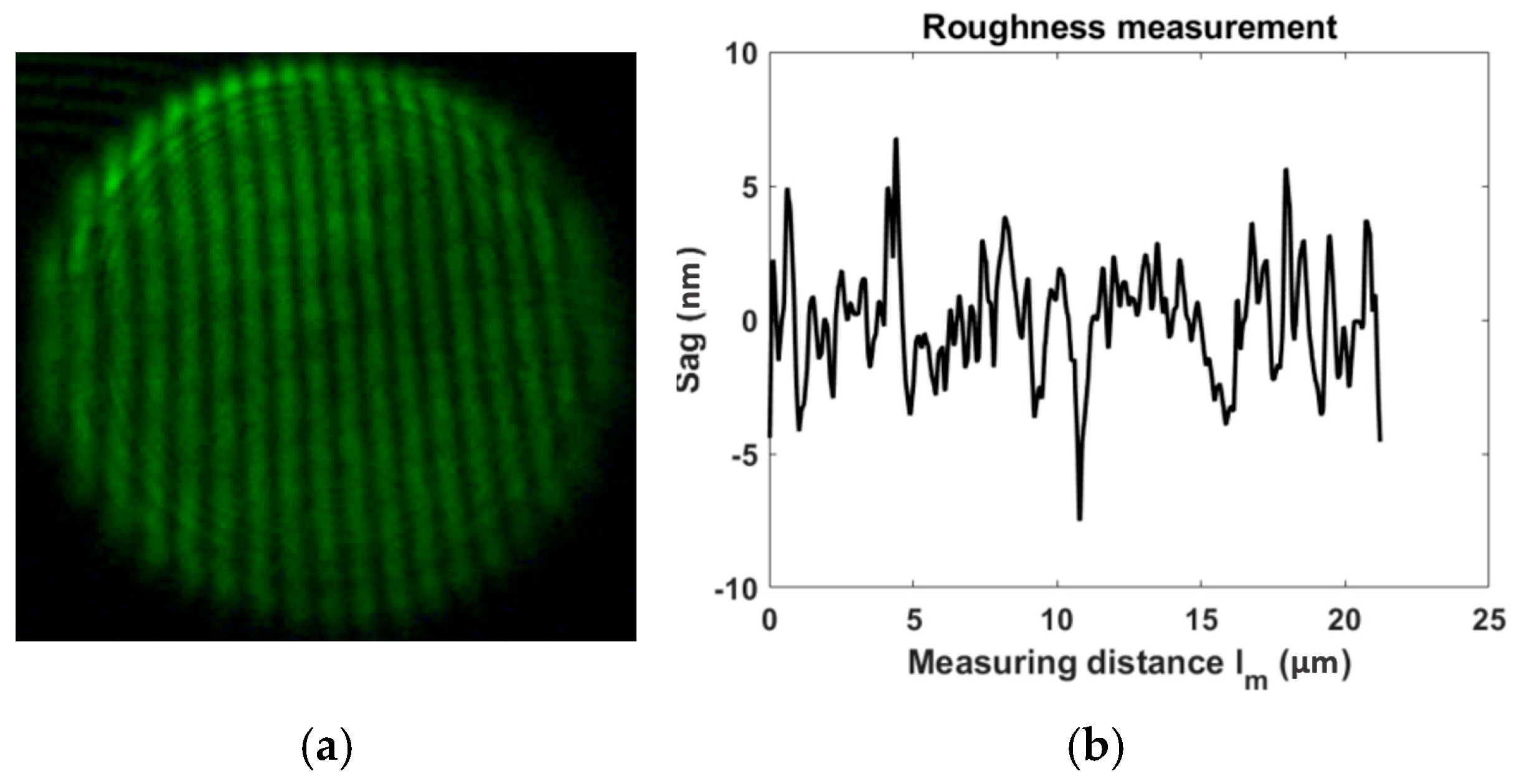
2.3. Roughness
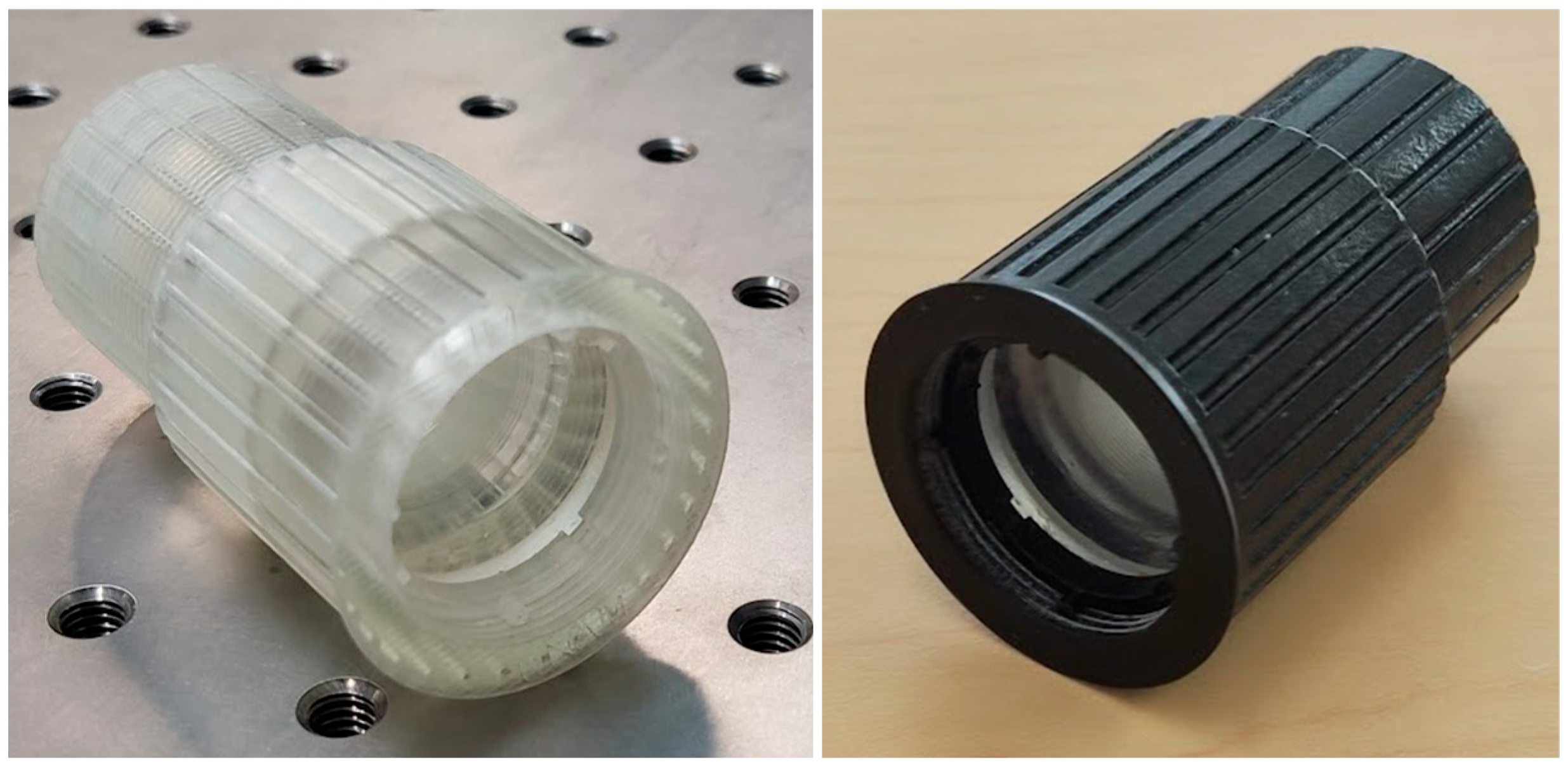
2.4. Tube Design
3. Instrument Optical Functionality
3.1. Optical Resolution
3.2. Optical Parameters
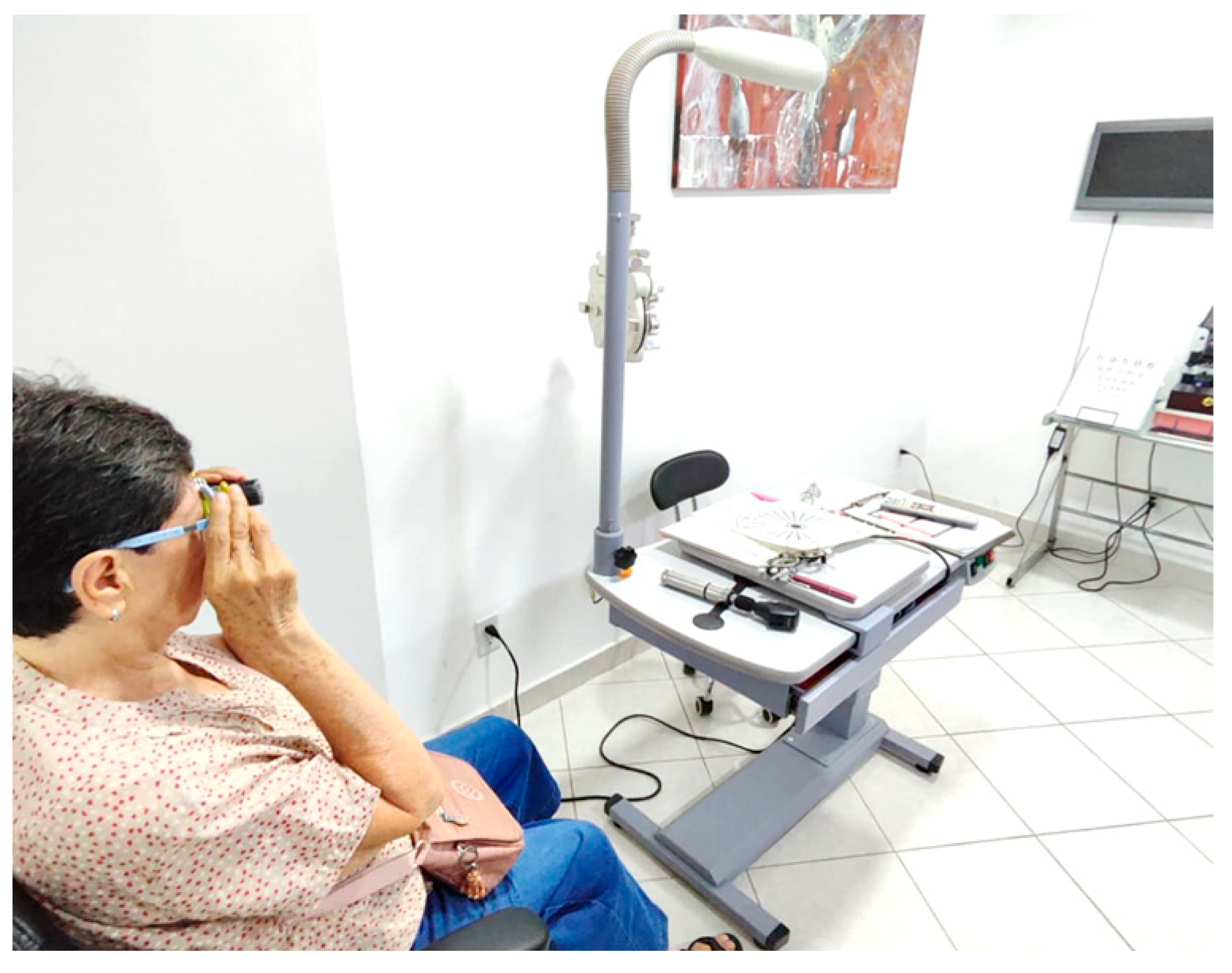
4. Instruments’ Clinical Functionality
5. Discussion
6. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- WHO. World Report on Vision. 2020. Available online: https://iris.who.int/bitstream/handle/10665/328717/9789241516570-eng.pdf?sequence=18 (accessed on 20 February 2023).
- WHO. Eye Care in Health Systems Guide for Action. 2022. Available online: https://iris.who.int/bitstream/handle/10665/354382/9789240050068-eng.pdf?sequence=1 (accessed on 10 May 2024).
- Wong, W.L.; Su, X.; Li, X.; Cheung, C.M.; Klein, R.; Cheng, C.Y.; Wong, T.Y. Global prevalence of age-related macular degeneration and disease burden projection for 2020 and 2040: A systematic review and meta-analysis. Lancet Glob. Health 2014, 2, e106–e116. [Google Scholar] [CrossRef] [PubMed]
- WHO. International Classification of Diseases, 11th Revision. 2018. Available online: https://icd.who.int/en/ (accessed on 1 February 2025).
- Flaxman, S.R.; Bourne, R.R.A.; Resnikoff, S.; Ackland, P.; Braithwaite, T.; Cicinelli, M.V.; Das, A.; Jonas, J.B.; Keeffe, J.; Kempen, J.H.; et al. Global causes of blindness and distance vision impairment 1990–2020: A systematic review and meta-analysis. Lancet Glob. Health 2017, 5, e1221–e1234. [Google Scholar] [CrossRef] [PubMed]
- Bourne, R.R.A.; Stevens, G.A.; White, R.A.; Smith, J.L.; Flaxman, S.R.; Price, H.; Jonas, J.B.; Keeffe, J.; Leasher, J.; Naidoo, K.; et al. Causes of vision loss worldwide, 1990–2010: A systematic analysis. Lancet Glob. Health 2013, 1, E339–E349. [Google Scholar] [CrossRef]
- Tham, Y.C.; Li, X.; Wong, T.Y.; Quigley, H.A.; Aung, T.; Cheng, C.Y. Global prevalence of glaucoma and projections of glaucoma burden through 2040: A systematic review and meta-analysis. Ophthalmology 2014, 121, 2081–2090. [Google Scholar] [CrossRef]
- Fricke, T.R.; Tahhan, N.; Resnikoff, S.; Papas, E.; Burnett, A.; Ho, S.M.; Naduvilath, T.; Naidoo, K.S. Global Prevalence of Presbyopia and Vision Impairment from Uncorrected Presbyopia: Systematic Review, Meta-analysis, and Modelling. Ophthalmology 2018, 125, 1492–1499. [Google Scholar] [CrossRef]
- National Research Council (US) Committee on Disability Determination for Individuals with Visual Impairments. Visual Impairments: Determining Eligibility for Social Security Benefits; Lennie, P., Van Hemel, S.B., Eds.; National Academies Press: Washington, DC, USA, 2002. [Google Scholar]
- Kv, V.; Vijayalakshmi, P. Understanding definitions of visual impairment and functional vision. Community Eye Health 2020, 33, S16–S17. [Google Scholar]
- European Council of Optometry and Optics. Low Vision. 2011. Available online: https://www.ecoo.info/wp-content/uploads/2012/09/ECOO-Position-Paper-Low-Vision-FINAL.pdf (accessed on 20 February 2025).
- Scott, I.U.; Smiddy, W.E.; Schiffman, J.; Feuer, W.J.; Pappas, C.J. Quality of life of low-vision patients and the impact of low-vision services. Am. J. Ophthalmol. 1999, 128, 54–62. [Google Scholar] [CrossRef]
- Corn, A.L.; Erin, J.N. Foundations of Low Vision: Clinical and Functional Perspectives, 2nd ed.; AFB Press: New York, NY, USA, 2010. [Google Scholar]
- Jose, R.T. (Ed.) Understanding Low Vision; AFB Press: New York, NY, USA, 2004. [Google Scholar]
- Wu, Y.; Liu, J.; Kang, L.; Tian, J.; Zhang, X.; Hu, J.; Huang, Y.; Liu, F.; Wang, H.; Wu, Z. An overview of 3D printed metal implants in orthopedic applications: Present and future perspectives. Heliyon 2023, 9, e17718. [Google Scholar] [CrossRef] [PubMed]
- Rankin, T.M.; Giovinco, N.A.; Cucher, D.J.; Watts, G.; Hurwitz, B.; Armstrong, D.G. Three-dimensional printing surgical instruments: Are we there yet? J. Surg. Res. 2014, 189, 193–197. [Google Scholar] [CrossRef]
- He, Y.; Xue, G.; Fu, J. Fabrication of low cost soft tissue prostheses with the desktop 3D printer. Sci. Rep. 2014, 4, 6973. [Google Scholar] [CrossRef]
- Bhatti, S.S.; Singh, J. 3D printing of biomaterials for biomedical applications: A review. Int. J. Interact. Des. Manuf. 2023. [Google Scholar] [CrossRef]
- Atala, A. Introduction: 3D Printing for Biomaterials. Chem. Rev. 2020, 120, 10545–10546. [Google Scholar] [CrossRef] [PubMed]
- Grygier, D.; Kujawa, M.; Kowalewski, P. Deposition of Biocompatible Polymers by 3D Printing (FDM) on Titanium Alloy. Polymers 2022, 14, 235. [Google Scholar] [CrossRef] [PubMed]
- Aguirre-Aguirre, D.; Gonzalez-Utrera, D.; Villalobos-Mendoza, B.; Díaz-Uribe, R. Fabrication of biconvex spherical and aspherical lenses using 3D printing. Appl. Opt. 2023, 62, C14–C20. [Google Scholar] [CrossRef] [PubMed]
- Alam, F.; Ali, M.; Elsherif, M.; Salih, A.E.; El-Atab, N.; Butt, H. 3D printed intraocular lens for managing the color blindness. Addit. Manuf. Lett. 2023, 5, 100129. [Google Scholar] [CrossRef]
- Zhu, Y.; Tang, T.; Zhao, S.; Joralmon, D.; Poit, Z.; Ahire, B.; Keshav, S.; Rajendra Raje, A.; Blair, J.; Zhang, Z.; et al. Recent advancements and applications in 3D printing of functional optics. Addit. Manuf. 2022, 52, 102682. [Google Scholar] [CrossRef]
- Bautista-Hernández, A.; Villalobos-Mendoza, B.; Pérez-Tijerina, E.; Aguirre-Aguirre, D. Study and characterization of components fabricated in a 3D printer. J. Phys. Conf. Ser. 2022, 2307, 012026. [Google Scholar] [CrossRef]
- Gonzalez-Utrera, D.; Villalobos-Mendoza, B.; Aguirre-Aguirre, D. Fabrication of Alvarez Lenses Prototypes Using a 3D Printer. In Frontiers in Optics + Laser Science 2022 (FIO, LS), Technical Digest Series; Optica Publishing Group: Washington, DC, USA, 2022; p. JW5B.9. [Google Scholar] [CrossRef]
- Aguirre-Aguirre, D.; Gonzalez-Utrera, D.; Villalobos-Mendoza, B.; Campos-Garcia, M. Biconvex Lens Fabrication Using a 3D Printer. In Frontiers in Optics + Laser Science 2022 (FIO, LS), Technical Digest Series; Optica Publishing Group: Washington, DC, USA, 2022; p. JW4B.2. [Google Scholar] [CrossRef]
- Gonzalez-Utrera, D.; Villalobos-Mendoza, B.; Diaz-Uribe, R.; Aguirre-Aguirre, D. Modeling, fabrication, and metrology of 3D printed Alvarez lenses prototypes. Opt. Express 2024, 32, 3512–3527. [Google Scholar] [CrossRef]
- Bautista-Hernández, A.M.; Villalobos-Mendoza, B.; Izazaga-Pérez, R.; Solís-Pomar, F.; Gutiérrez-Lazos, C.D.; Aviles-Alvarado, A.; Garcia-Castillo, F.A.; Pérez-Tijerina, E.G.; Aguirre-Aguirre, D. Design and fabrication of a lightweight 3D first surface mirror aluminized by DC magnetron sputtering. Appl. Opt. 2023, 62, 9089–9095. [Google Scholar] [CrossRef]
- Formlabs. Form3+ Rapid, Flawless Prints Every Time. Available online: https://formlabs.com/3d-printers/form-3/ (accessed on 10 May 2024).
- Mendes-Felipe, C.; Patrocinio, D.; Laza, J.M.; Ruiz-Rubio, L.; Vilas-Vilela, J.L. Evaluation of postcuring process on the thermal and mechanical properties of the Clear02™ resin used in stereolithography. Polym. Test. 2018, 72, 115–121. [Google Scholar] [CrossRef]
- Berglund, D.G.; Tkaczyk, S.T. Fabrication of optical components using a consumer-grade lithographic printer. Opt. Express 2019, 27, 30405–30420. [Google Scholar] [CrossRef] [PubMed]
- Peli, E.; Vargas-Martin, F. In-the-spectacle-lens telescopic device. J. Biomed. Opt. 2008, 13, 034027. [Google Scholar] [CrossRef][Green Version]
- Choyce, P. A Galilean telescope using an anterior-chamber implant as eyepiece. Lancet 1963, 281, 794–796. [Google Scholar] [CrossRef]
- Vincent, S.J. The use of contact lens telescopic systems in low vision rehabilitation. Contact Lens Anterior Eye 2017, 40, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Safrani, A.; Abdulhalim, I. Real-time phase shift interference microscopy. Opt. Lett. 2014, 39, 5220–5223. [Google Scholar] [CrossRef]
- Tien, C.L.; Lin, H.Y.; Chang, C.K.; Tang, C.J. Effect of Oxygen Flow Rate on the Optical, Electrical, and Mechanical Properties of DC Sputtering ITO Thin Films. Adv. Condens. Matter Phys. 2018, 2647282. [Google Scholar] [CrossRef]
- Assefa, B.G.; Saastamoinen, T.; Pekkarinen, M.; Biskop, J.; Nissinen, V.; Kuittinen, M.; Turunen, J.; Saarinen, J. Realizing freeform optics using 3d-printer for industrial based tailored irradiance distribution. OSA Contin. 2019, 2, 690–702. [Google Scholar] [CrossRef]
- Muñoz-Juárez, I.; Rodríguez-Rodríguez, M.I.; Zarco-López, D.T.; Hernández-Carbajal, R.E.; Izazaga-Pérez, R.; Aguirre-Aguirre, D. Desempeño de telescopios galileanos híbridos en pacientes con diagnóstico de baja visión. ACONTACS 2024, 6, 136–144. [Google Scholar]
- Muñoz-Juárez, I.; Rodríguez-Rodríguez, M.I.; Aguirre-Aguirre, D.; Hernández-Carbajal, R.E. Desempeño de telescopios galileanos en pacientes informados con diagnóstico de baja visión. ACONTACS 2023, 5, 62–72. [Google Scholar]
- İdil, A.; Şahli, E. Pediatric Vitreoretinal Surgery. Low Vision Aids; Springer: Cham, Switzerland, 2023; pp. 1059–1078. [Google Scholar]
- Fok, D.; Polgar, J.M.; Shaw, L.; Jutai, J.W. Low vision assistive technology device usage and importance in daily occupations. Work 2011, 39, 37–48. [Google Scholar] [CrossRef]
- Naidoo, K.S.; Maharaj, Y.I.; Pillay, V.; Fellhauer, S. Optical products for refractive error and low vision. Community Eye Health 2011, 24, 42–43. [Google Scholar] [PubMed]
- Karnani, A.G.; Garrette, B.; Kassalow, J.S.; Lee, M. Better Vision for the Poor. Stanf. Soc. Innov. Rev. 2011, 9, 66–71. [Google Scholar] [CrossRef]
- Sumalini, R.; Satgunam, P. Ophthalmic Diagnostics. Visual Acuity: High Contrast and Low Contrast; Springer: Singapore, 2024; pp. 1–14. [Google Scholar]
- Ovsianikov, A.; Farsari, M.; Chichkov, B.N. Photonic and Biomedical Applications of the Two-Photon Polymerization Technique. Stereolithography; Springer: Boston, MA, USA, 2011; pp. 257–297. [Google Scholar]
- Singhal, A.; Dalmiya, A.; Lynch, P.T.; Paprotny, I. 2-Photon Polymerized IP-Dip 3D Photonic Crystals for Mid IR Spectroscopic Applications. IEEE Photonics Technol. Lett. 2023, 35, 410–413. [Google Scholar] [CrossRef]
- Thompson, J.R.; Worthington, K.S.; Green, B.J.; Mullin, N.K.; Jiao, C.; Kaalberg, E.E.; Wiley, L.A.; Han, I.C.; Russell, S.R.; Sohn, E.H.; et al. Two-photon polymerized poly(caprolactone) retinal cell delivery scaffolds and their systemic and retinal biocompatibility. Acta Biomater. 2019, 94, 204–218. [Google Scholar] [CrossRef]




| Eyepiece Lens (mm) | Objective Lens (mm) | |
|---|---|---|
| Thorlabs code | LC1715 | LA1509 |
| Diameter | 25.4 | 25.4 |
| Focal length | −50 | 100 |
| Radius of curvature Surface #1 | −25.7 | 51.5 |
| Radius of curvature Surface #2 | Inf. | Inf. |
| Central thickness | 2 | 3 |
| Parameter | Value |
|---|---|
| Density (g/cm3) | 1.15 |
| Thermal expansion (μm/m-°C) | 122.4 |
| Tensile modulus (GPa) | 2.8 |
| Friction coefficient | 0.48 |
| Solvent resistance (IPA weight gain) % | <1.0 |
| Index of refraction (D line) | 1.505 |
| Glass Telescope | Resin Telescope | |
|---|---|---|
| Amplification | 1.94× | 1.96× |
| Field of view (FOV) | 11.31° | 10.31° |
| Parameter | Patient |
|---|---|
| Sex |
|
| Age |
|
| Diagnosis |
|
| VA with Rx |
|
| CS with Rx |
|
| Test | Non Telescope | Glass Telescope | Resin Telescope |
|---|---|---|---|
| Visual acuity (VA) | 10/100 | 10/40 | 10/32 |
| Contrast sensitivity (CS) | 6 cpd level 8 | 18 cpd level 4 | 18 cpd level 4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aguirre-Aguirre, D.; Muñoz-Juárez, I.; Rodríguez-Rodríguez, M.I.; Villalobos-Mendoza, B.; Hernández-Carbajal, R.E.; Díaz-Uribe, R.; Izazaga-Pérez, R. 3D Printed Galilean Telescope for Low-Vision Patients. Photonics 2025, 12, 815. https://doi.org/10.3390/photonics12080815
Aguirre-Aguirre D, Muñoz-Juárez I, Rodríguez-Rodríguez MI, Villalobos-Mendoza B, Hernández-Carbajal RE, Díaz-Uribe R, Izazaga-Pérez R. 3D Printed Galilean Telescope for Low-Vision Patients. Photonics. 2025; 12(8):815. https://doi.org/10.3390/photonics12080815
Chicago/Turabian StyleAguirre-Aguirre, Daniel, Itzel Muñoz-Juárez, Martin Isaías Rodríguez-Rodríguez, Brenda Villalobos-Mendoza, Ruth Eva Hernández-Carbajal, Rufino Díaz-Uribe, and Rafael Izazaga-Pérez. 2025. "3D Printed Galilean Telescope for Low-Vision Patients" Photonics 12, no. 8: 815. https://doi.org/10.3390/photonics12080815
APA StyleAguirre-Aguirre, D., Muñoz-Juárez, I., Rodríguez-Rodríguez, M. I., Villalobos-Mendoza, B., Hernández-Carbajal, R. E., Díaz-Uribe, R., & Izazaga-Pérez, R. (2025). 3D Printed Galilean Telescope for Low-Vision Patients. Photonics, 12(8), 815. https://doi.org/10.3390/photonics12080815





