1. Introduction
Myopia is the prevalent refractive error that affects visual acuity in children and adults. A meta-analysis predicts that by 2050, myopia will affect nearly half of the global population [
1]. Spectacles are a simple and safe method for correcting myopia, and most spectacles are currently manufactured with a 0.25 diopter (D) step. Determining the proper prescription of spectacles relies on accurate refraction, including automatic and subjective refraction. However, during subjective refraction, the 0.25D-step refraction may result in patients failing to achieve red-green balance in the Duochrome test, leading to either overcorrection or undercorrection [
2,
3]. Studies have shown that the resolution limit of the human eye to spherical lens change was about 0.05D, indicating demand for more precise prescriptions and lens manufacturing [
2]. With advancements in refraction technology, higher-precision myopia prescriptions can be obtained using a new-generation refraction device with a 0.05D step [
4,
5].
Recent research has compared the difference in visual performance of spectacles obtained with 0.05D and 0.25D step refraction techniques [
2,
3,
4,
5]. However, these studies primarily focused on static visual performance, including contrast sensitivity and best-corrected visual acuity (BCVA). In daily life, individuals frequently need to observe moving objects, and static vision may not adequately reflect visual function in real-world scenarios [
6,
7]. Dynamic visual acuity (DVA) is the ability to discriminate details of an object when relative movement exists between the object and the observer [
7]. Measuring visual acuity in dynamic situations and the detail resolution of moving objects can better reflect the visual function in real-life scenes [
8]. Therefore, DVA has gradually become an important evaluation metric for functional vision [
9,
10,
11,
12,
13,
14]. The previous study demonstrated that myopia significantly affects DVA when fully corrected with eyeglasses, and worse DVA was associated with more significant myopia [
15]. However, the impact of 0.05D versus 0.25D step spectacles on DVA remains unexplored.
The present study aims to compare the DVA with spectacles prescribed using 0.05D and 0.25D step refraction in a self-control design and to explore the associated factors for DVA. The findings may enhance the understanding of how these refraction methods influence dynamic vision and support the inclusion of DVA as an important metric to guide the selection of refraction and prescription methods based on individual needs.
2. Materials and Methods
2.1. Participants
The present study was a double-blind, randomized, self-control observational study to assess the DVA with 0.05D step spectacles compared with 0.25D step spectacles in myopic patients. The study adhered to the tenets of the Declaration of Helsinki, and the protocol was approved by the ethics committee of Peking University Third Hospital. Informed consent was obtained from all participants before being included in the study.
Participants aged between 18 and 40 years with myopia were included in the study. Exclusion criteria were as follows: (1) Monocular corrected distance visual acuity (CDVA) ≤ 0 LogMAR; (2) severe myopia (sphere < −10D) or high astigmatism (> 3D); (3) significant anisometropia with a difference in spherical equivalent > 2D between eyes; (4) the presence of ocular diseases affecting eye structure or static vision, such as glaucoma, corneal disease, or retinal disorders; (5) systemic diseases impacting static vision; (6) vestibular dysfunction or cognitive impairment; and (7) inability to track dynamic visual targets or follow instructions during testing.
2.2. Randomization and Grouping
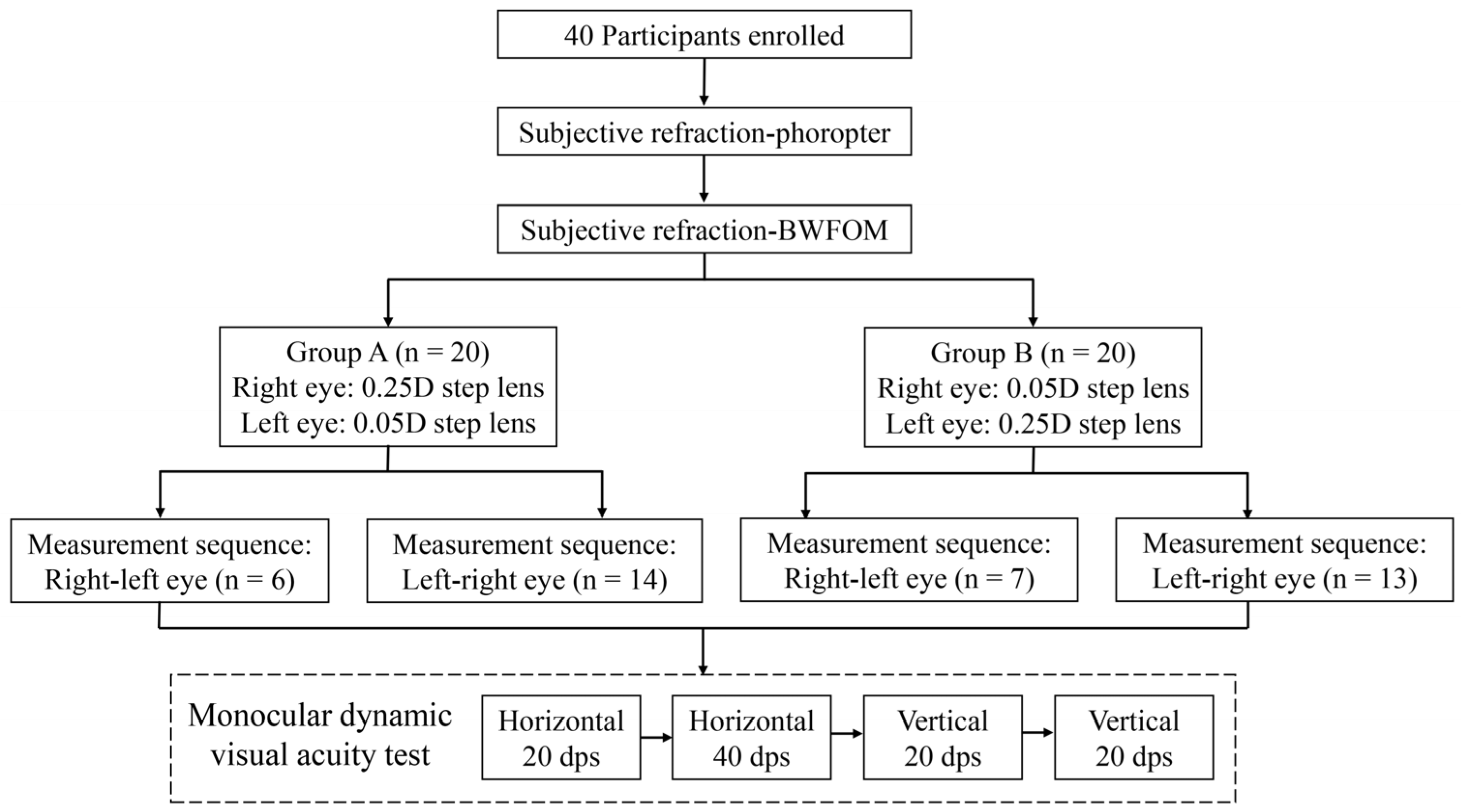
The study design and participant allocation process are shown in
Figure 1. The participants were randomly assigned 1:1 to groups A and B with block randomization. The block size was set at 2, with a total of 20 blocks. A random number table was employed to sort the participants based on their identification numbers and sequential assignment to blocks was performed according to the sorting results. In group A, participants wore spectacles with a 0.25D step lens for the right eye and a 0.05D step lens for the left eye. In contrast, participants in group B used spectacles with lenses in 0.05D step for the right eye and 0.25D for the left eye. The participants were further randomly divided into two groups with different test sequences for the right and left eye because the test sequence may affect the result due to the perceptual learning effect during the DVA test [
10]. The right eye was examined first in one group, followed by the left, while the other group reversed the test order. The lens allocation was masked to the DVA examiner and the participants.
2.3. Testing Procedure
All enrolled participants underwent slit-lamp and fundus examinations to rule out severe ocular diseases. Subsequently, subjective refraction was performed at 0.25D step using a phoropter, followed by subjective refraction at 0.05D step using a Binocular Wavefront Optometer (BWFOM, Aizhitong Medical Technology Co., Ltd., Huzhou, China). Next, based on the group assignment, the corresponding spectacles were fitted, the CDVA was measured with a LogMar visual chart, and the dominant eye was examined with the card hole method. The 0.25D step lens was prescribed with phoropter-based subjective refraction, and the 0.05D step lens was prescribed with optometer-based subjective refraction. Finally, the DVA test was performed sequentially for each eye according to the allocation wearing the prescribed spectacles.
Subjective refraction with a phoropter was performed monocularly based on automatic refraction (KR-8100, Topcon, Medical System, Tokyo, Japan). Fogging with a +0.75 to +1.50D lens was applied to relax accommodation. The negative lens was gradually increased in a 0.25D step, and we applied a duochrome test to achieve the first maximum plus to maximum visual acuity (MPMVA). Next, the cylinder axis was refined, followed by the power with the Jackson-cross cylinder. Then, the second MPMVA was obtained with a duochrome test to adjust the sphere. Then, the other eye was examined using the same procedure, followed by the binocular balance test.
The BWFOM is an innovative device that integrates objective and subjective refraction. Objective refraction utilizes Hartmann–Shack wavefront sensor and adaptive optics technology and separates higher- from lower-order aberrations, converting the lower-order aberration data into objective refractive values used as the starting point for subjective refraction [
4,
16]. The subjective refraction procedure with BWFOM is similar to phoropter-based refraction, including monocular spherical endpoints determination with a duochrome test, cylinder fine tune, and binocular balance test. Subjective refraction is facilitated by a series of optical modulators that simulate optical lenses. These modulators move linearly, achieving an adjustment precision of 0.05D. Leveraging this precision, the BWFOM enables examiners to prescribe lenses in the 0.05D step, delivering highly accurate refraction results for objective and subjective methods [
4,
5].
2.4. DVA Test
The DVA was evaluated with the previously reported test system [
13,
15,
17]. The DVA tests were conducted monocularly with refractive error corrected using spectacles according to the group allocation. The test was arranged at a 2.5 m distance in a quiet room, and the optotypes were presented on a 24-inch 480 Hz screen. The test software was programmed with MATLAB 2017b (MathWorks, Natick, MA, USA), which could demonstrate moving the letter E with a certain size and speed. The optotype E was configured according to the LogMAR visual chart.
Two repeated sessions were performed for the right and left eyes at 5-min intervals. Each session contained four DVA tests with different motion types and velocities, with a 1-min interval between each test. The test sequence was the same during the two sessions, in the following order: horizontal motion of 20 degrees per second (dps), vertical motion of 20 dps, horizontal motion of 40 dps, and vertical motion of 40 dps. During the horizontal motion test, the optotype appeared in the middle of the screen’s left side and horizontally moved to the right side. For the vertical motion test, the optotype appeared in the middle of the screen on the upper side and vertically moved to the lower side.
During the test, the patient was required to discern the opening direction of the letter E in a four alternative forced-choice mode. The initial optotype was four sizes bigger than the CDVA. For each size, we presented eight optotypes one by one with a random opening direction. The letter E would be switched to one size smaller if the patient could correctly identify five out of eight optotypes. The minimum size the participant could recognize was recorded, and the result was calculated using the previously reported formula [
17].
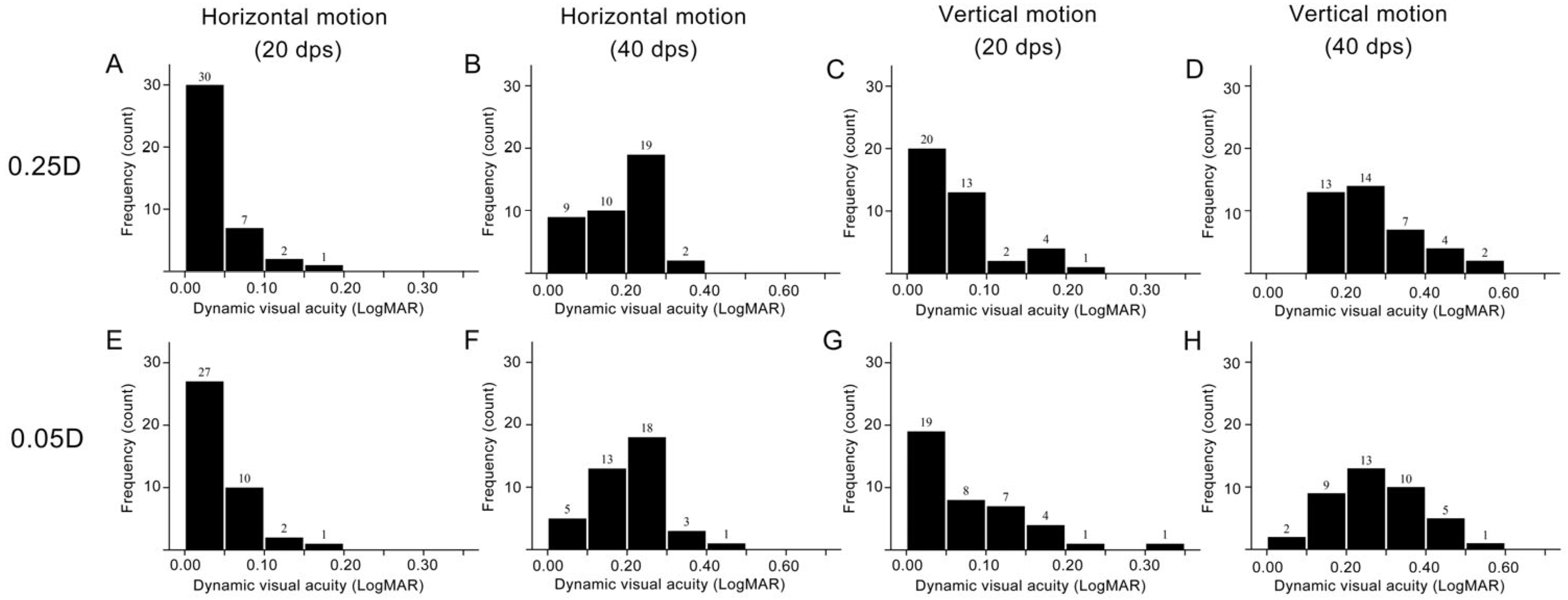
2.5. Statistical Analysis
The statistical analysis was conducted using SPSS 26.0 (IBM, Armonk, NY, USA). The spherical equivalent (SE) was calculated as the sphere plus half of the cylinder diopter. The Kolmogorov-Smirnov test was performed to determine the normality of the distribution. Descriptive statistics were reported as mean and standard deviation (SD) for continuous variables, whereas number and percentage were for categorical variables. Considering the correlation between two eyes, a linear mixed model was used to compare the DVA between 0.25D and 0.05D step spectacles, and the random intercept for the subject was included in the model. Subgroup analysis was performed by the dominant eye and test sequence. A p-value less than 0.05 was considered statistically significant.
4. Discussion
Accurate refraction is crucial for spectacle prescription and refractive surgery design. Benefiting from wavefront aberration and adaptive optics technology, 0.05D step refraction has become feasible in routine clinical practice. However, the clinical effectiveness of higher-precision spectacles correction for refractive errors remains insufficiently validated by research. This study aimed to investigate the differences in DVA between two eyes with spectacles prescribed with 0.05D and 0.25D step lenses in a self-control design. We found no significant difference in DVA performance in myopic eyes corrected with 0.05D and 0.25D step lenses in most DVA test patterns.
As for the subjective refraction results, statistically significant differences in sphere and cylinder exist between the outcomes obtained using phoropter and BWFOM, but the difference is not clinically significant since the difference was minimal. The phoropter measured more myopia and astigmatism than BWFOM in the present research. The result was consistent with previous research in myopic children that also showed a myopic tendency in cycloplegic subjective refraction measured with retinoscopy compared with BWFOM [
4]. In contrast, Cheng et al. study demonstrated that BWFOM measured more myopic than conventional subjective refraction in noncycloplegic conditions but less myopic in cycloplegic conditions [
5]. The contradicting results might be attributed to the difference in subjective refraction device and procedure since the fogging and cylinder fine-tuning procedures were omitted during the subjective refraction in previous research [
5].
Accurate refraction is crucial for spectacle prescription to provide satisfactory visual performance. In the present research, despite the significant difference observed between phoropter and BWFOM measured sphere and cylinder, the spectacle-corrected static visual acuity and DVA were comparable between eyes with 025D and 0.05D lenses. The result was inconsistent with previous research, which demonstrated that eyes achieved better high contrast and low contrast visual acuity and contrast sensitivity with 0.05D step lens than with 0.25D step lens, but the difference between lenses was minimal [
3]. In the previous research, the subjective refraction was performed with a trial lens rather than a phoropter, and the cylinder remained unchanged during lens fitting, which may cause inadequate precision in refraction prescription and less optimal static vision [
3]. Theoretically, visual performance may benefit from precision refraction of 0.05D step because studies have shown that the resolution limit of the human eye to spherical lens change was about 0.05D [
2]. The insignificant difference in DVA between eyes corrected with 0.05D and 0.25D step lenses might be attributed to the reason that DVA was influenced by multiple factors, including age, refractive error severity, continuous vision, and eye movement pattern [
14,
15,
18]. Additionally, unlike static visual signals, mainly transmitted with the parvocellular pathway, the magnocellular pathway was applied to transmit high temporal frequency signals [
7,
19]. Thus, the advantage of a 0.05D step lens on visual performance may be inadequate to offset the impact of other influential factors on DVA. Considering the limitation of prescribing 0.05D step lenses, including availability of lenses and cost-effectiveness, the spectacles prescribed to 0.05D step do not show an advantage over 0.25D step to correct DVA in myopic patients.
For the horizontal motion test at 40 dps, the dominant eye showed significantly better DVA than the nondominant eye. The DVA test result is associated with eye movement tracking and visual information processing in the brain. Previous studies have found that, compared to the nondominant eye, the target seen by the dominant eye appears more prominent and is more easily detected, which may lead to faster processing of visual information from the dominant eye [
20]. Another possibility is that more cortical neurons in the brain process information from the dominant eye [
21]. However, the specific mechanisms behind the superior performance of the dominant eye and the difference in motion direction and speed remain to be further studied. When the dominant eye was corrected with 0.25D lens, the DVA was better in eyes with 0.25D than 0.05D lens in the 40 dps horizontal motion test, but the difference was not shown when the 0.05D lens was fitted to the dominant eye. The result may indicate that the dominant eye was more adapted to refractive correction with a phoropter than an optometer. The optometer applies a set of optical modulators that simulate optical lenses, while the phoropter uses tangible lenses. The participant wore spectacles prescribed directly from the optometer during the DVA test, without the procedure adaption process with trial lens tunning. The lack of trial lens adaption may cause the difference, and further research is required to illustrate the mechanism.
Furthermore, during the 40 dps horizontal motion test, the second-tested eye exhibited better DVA than the first, suggesting a learning effect. The result is consistent with previous studies, which found significant short-term learning effects in DVA tests, especially in horizontal motion and high-speed tests [
10,
22]. Although the DVA test included a brief pre-training stage before the formal test, perceptual learning may also affect the test result in the examination, and the test sequence was randomized to avoid the learning effect as much as possible in the present research. When the first-measured eye was corrected with a 0.05D step lens, the 40 dps horizontal motion DVA was significantly better in eyes with 0.25D than with a 0.05D step lens. However, the difference was not shown when the first-measured eye was corrected with a 0.25D step lens. The categorical analysis demonstrated that when the first-measured eye wore 0.25D lens-fitted spectacles, 61.9% was the dominant eye. The advantage of eye dominance on dynamic object identification may offset the inferiority during the first measurement.
This study has several limitations. Firstly, the sample size was relatively small, which may limit the generalizability of the findings. Secondly, this study only included young adults aged 18–40 with corrected normal vision. Previous research has shown that DVA is affected by age [
15]. Therefore, future studies should investigate the visual performance of 0.05D refraction in other age groups. Thirdly, the subjective refraction was only performed by one experienced optometrist. The experience and procedure of subjective refraction may influence the result. Fourth, eye dominance was not considered during allocation, which caused the dominant eye proportion to be different among different groups. Further research may apply stratified randomization in the allocation that considers the impact of eye dominance and measurement sequence to solve the problem.