Ethyl Acetate Extract of Dracocephalum heterophyllum Benth Ameliorates Nonalcoholic Steatohepatitis and Fibrosis via Regulating Bile Acid Metabolism, Oxidative Stress and Inhibiting Inflammation
Abstract
1. Introduction
2. Materials and Methods
2.1. Apparatus and Reagents
2.2. Sample Preparation
2.3. Design and Treatment of Animal Experiments
2.3.1. Mouse MCD-Induced NASH Models
2.3.2. Mouse CCl4-Induced Liver Fibrosis Models
2.3.3. Testing Indicators and Methods
Basic Indicators
Biochemical Analysis
Quantitative Real-Time PCR
Histological Analysis
2.4. DPPH Inhibitor Recognition and Screening of Anti-Inflammatory Active Component
2.5. Medium- and High-Pressure Liquid Chromatography Separation of the Main Functional Component from the Ethyl Acetate Extraction
2.6. Purity and Activity Analysis of the Isolated Main Functional Component in the Studied Extracts
2.7. Molecular Docking Validation Analysis
2.8. Statistical Data Evaluation
3. Results and Discussion
3.1. Evaluation of the Therapeutic Effect of NASH and Liver Fibrosis
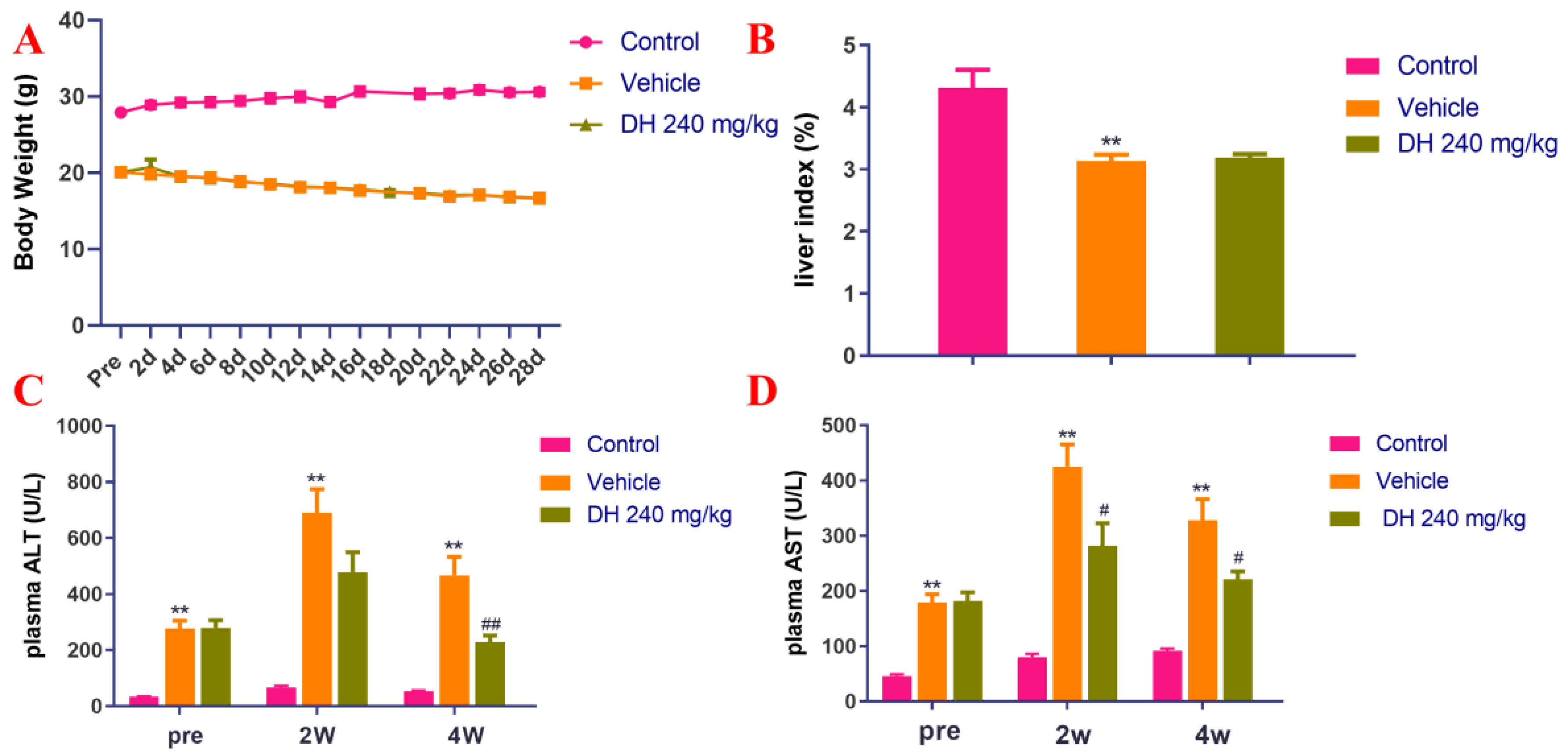
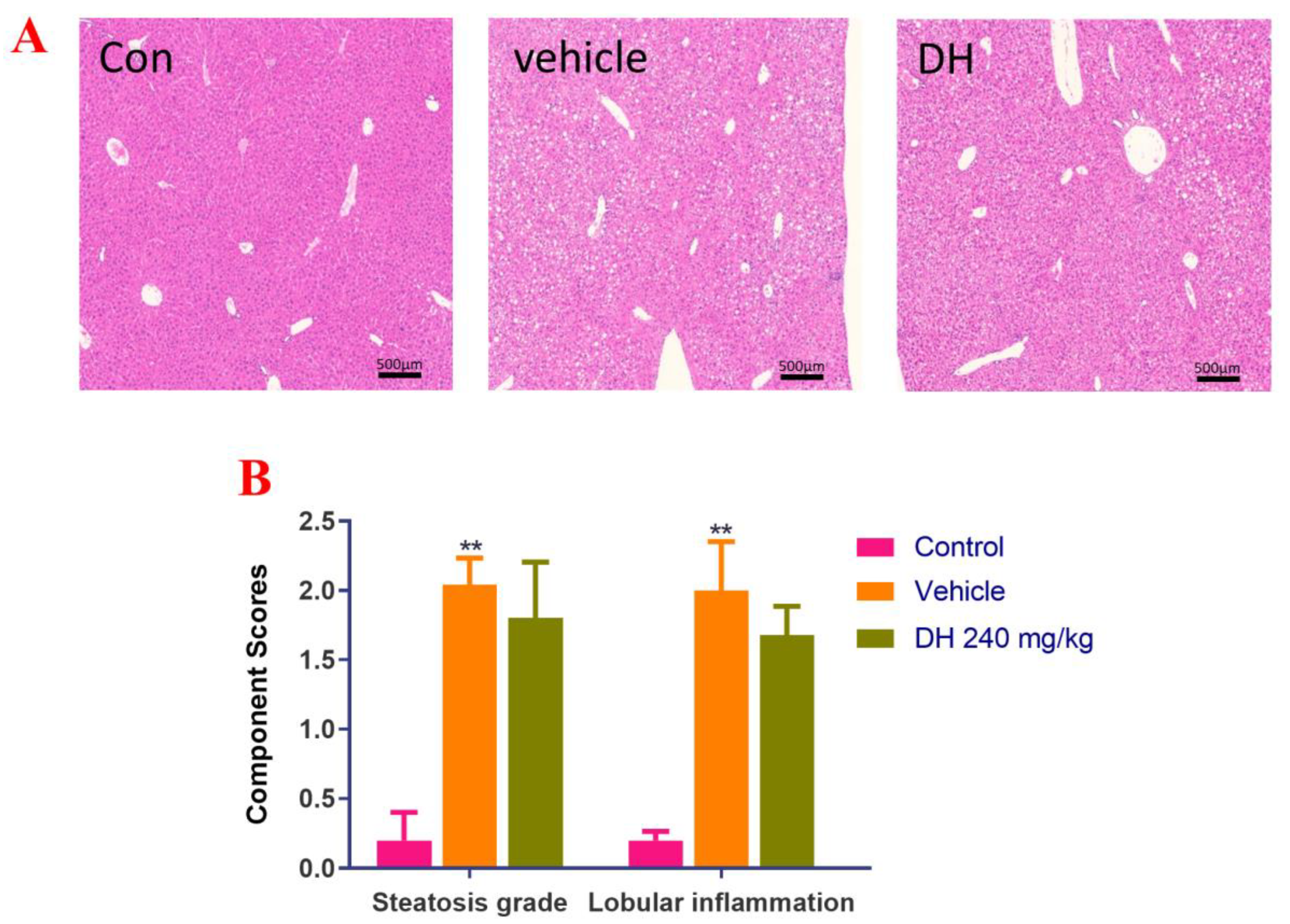
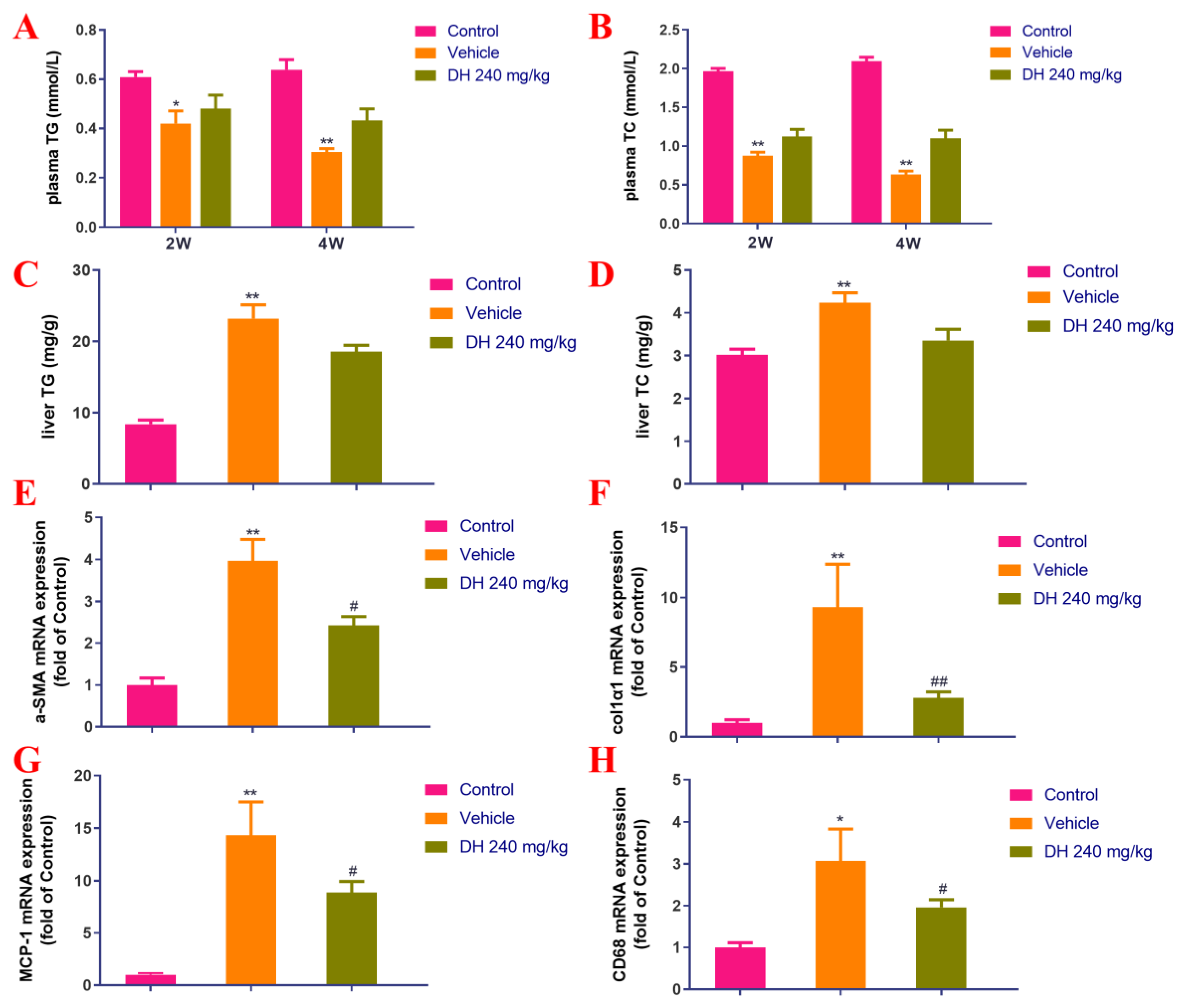
3.1.1. Effects of D. Heterophyllum Plant Extracts on Mouse MCD-Induced NASH Model
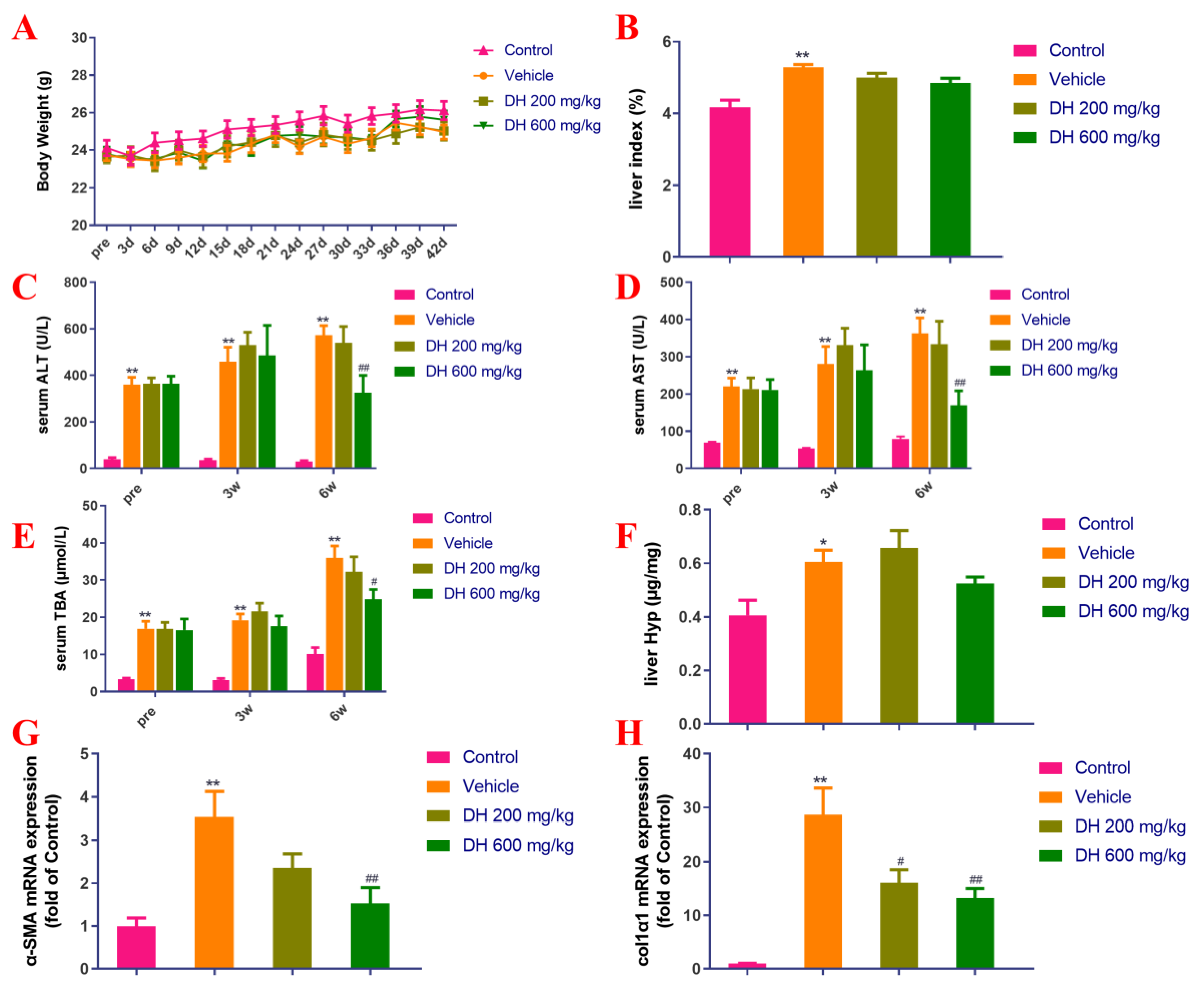
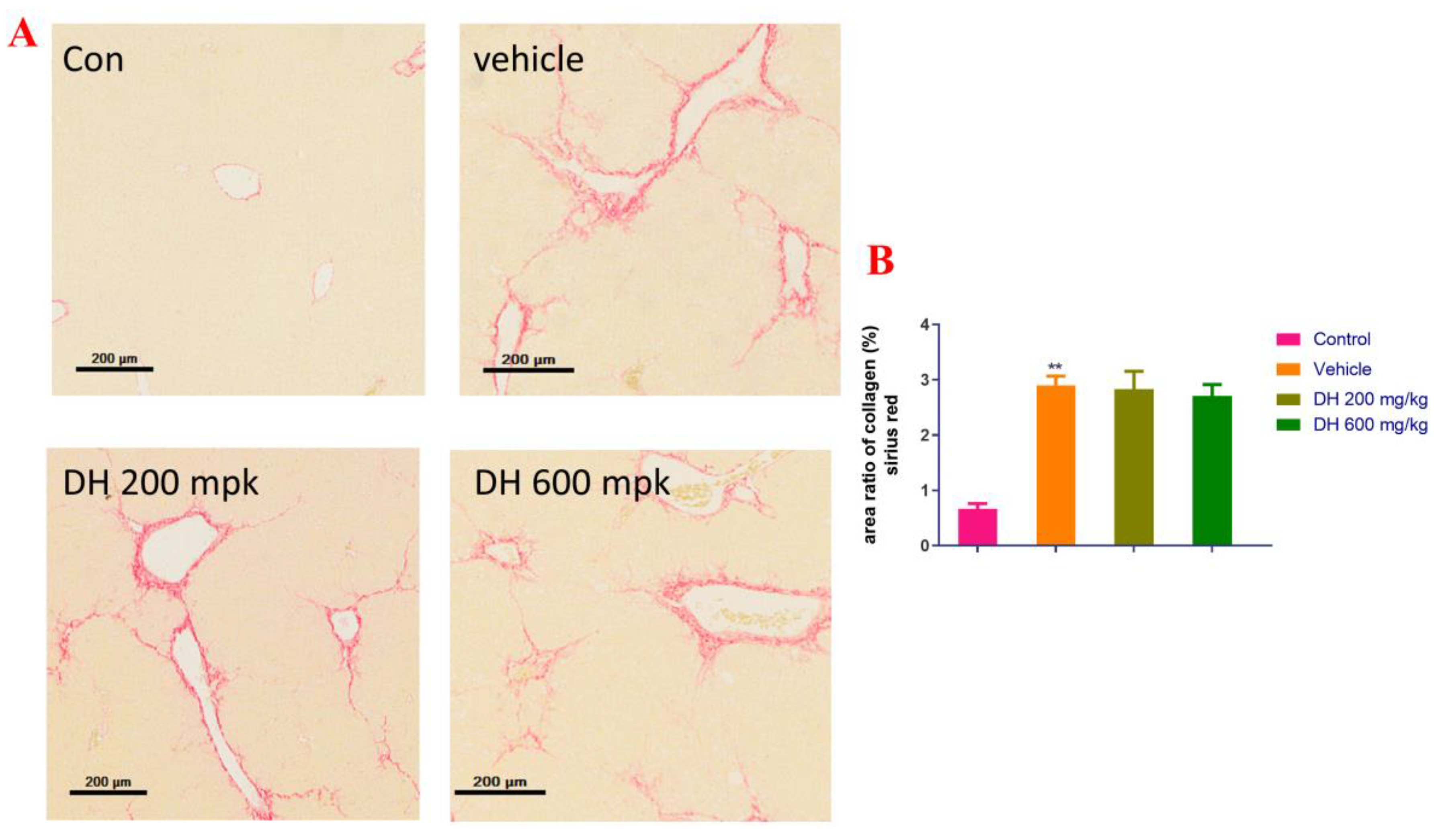
3.1.2. Effects on Mice CCl4-Induced Liver Fibrosis Model in Mice
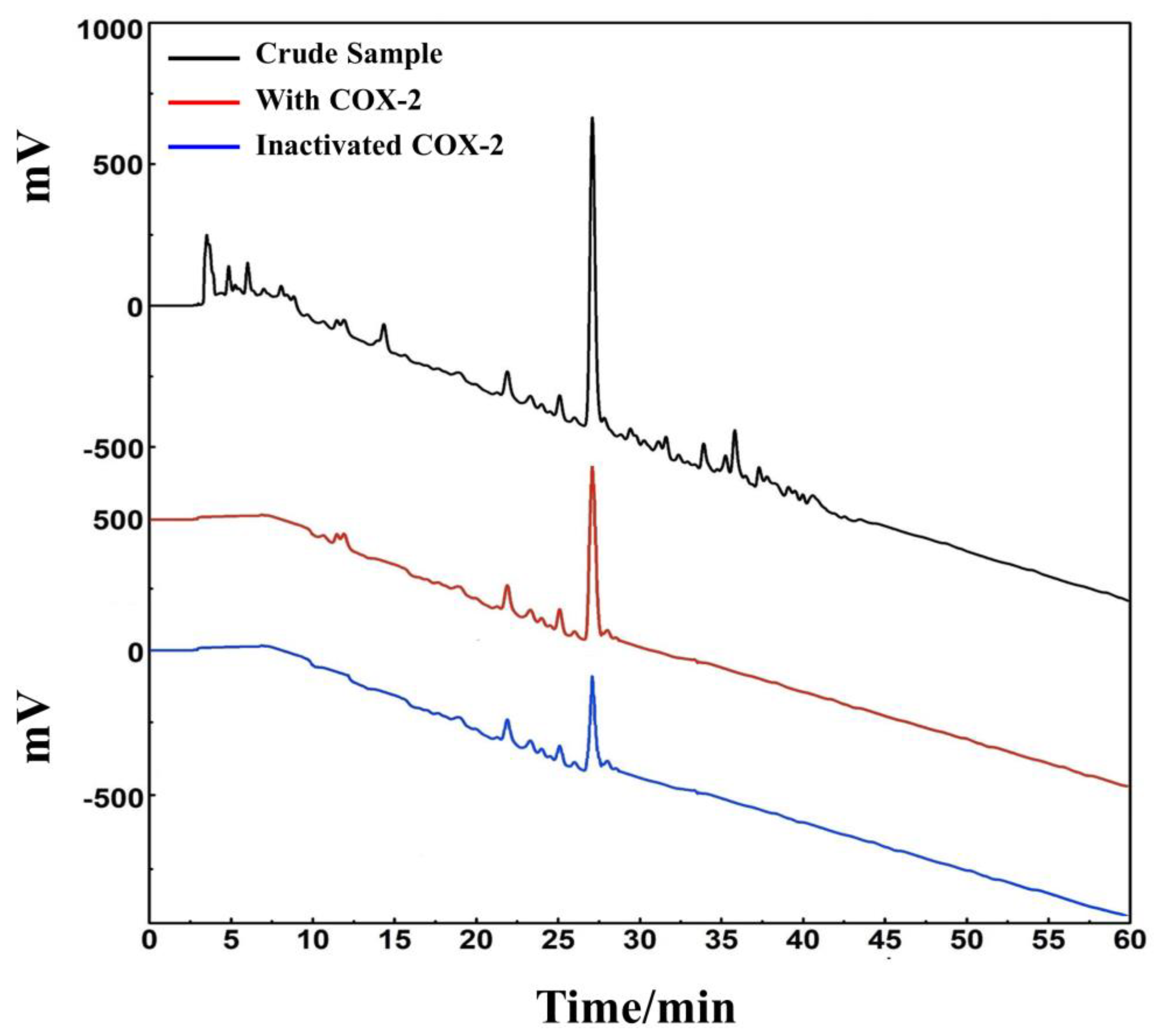
3.2. Isolation of DPPH Inhibitor and Anti-Inflammatory Active Component in Ethyl Acetate Extract Using Medium- and High-Pressure Liquid Chromatography
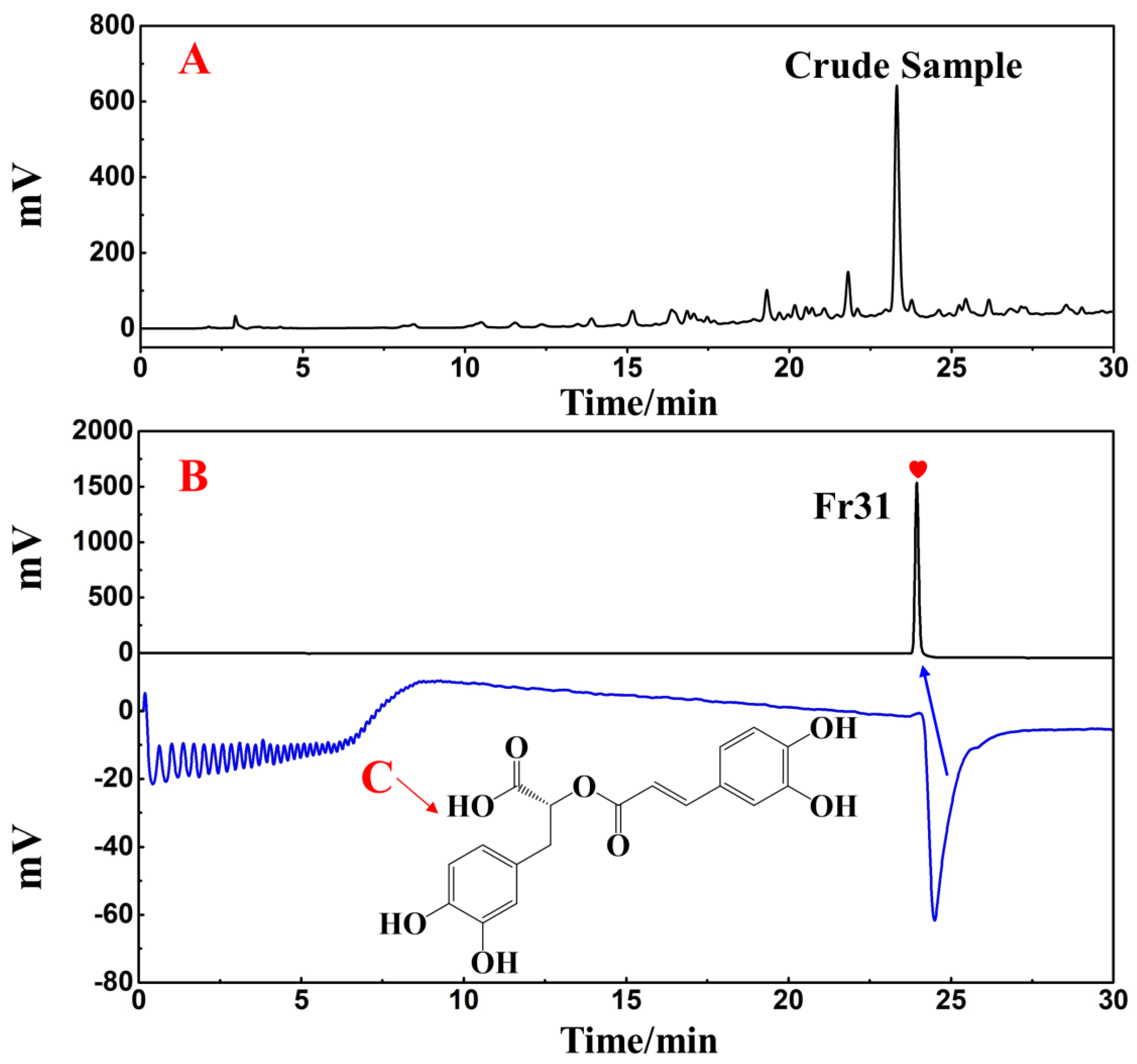
3.3. Purity Analysis and Structural Characterization of the Target Compound
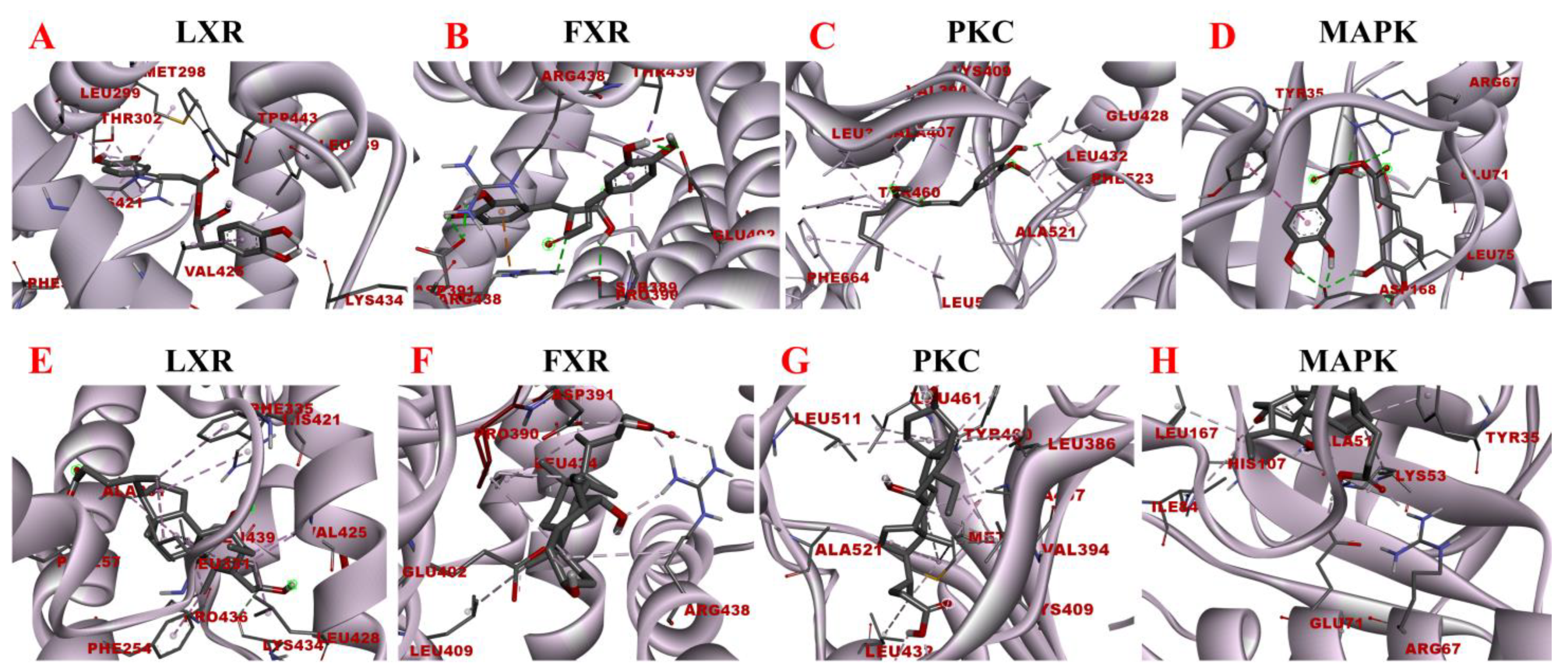
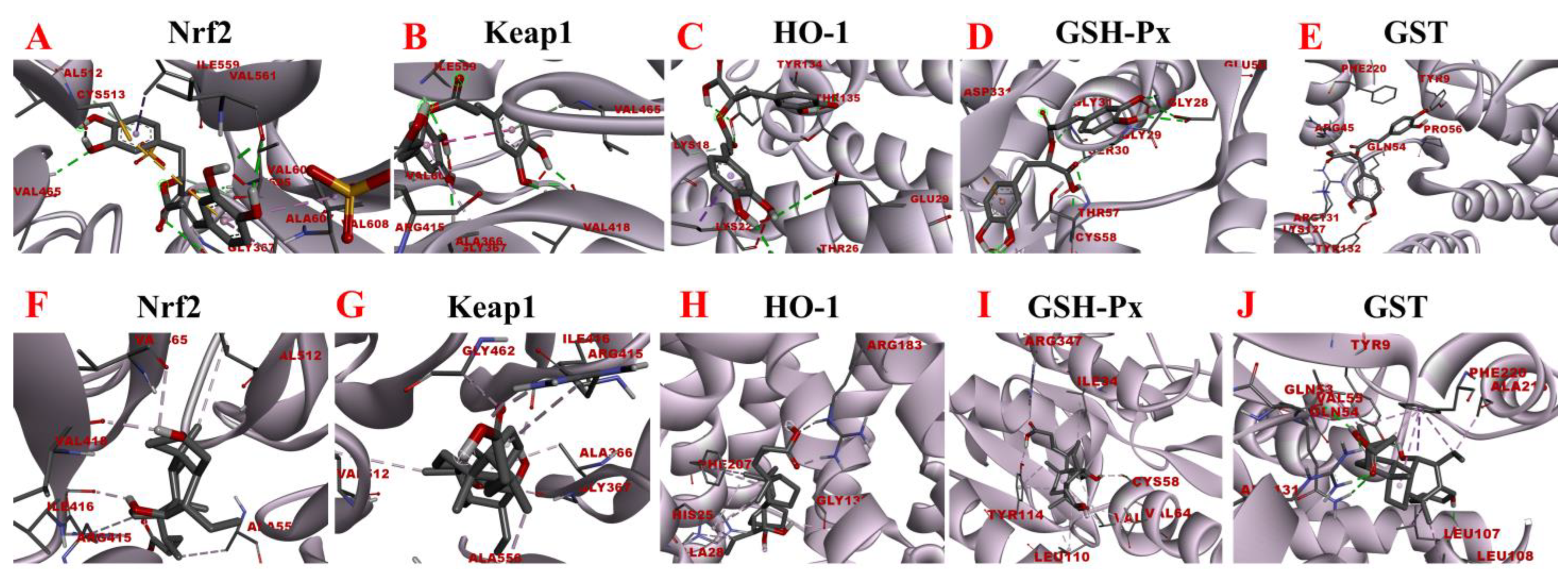
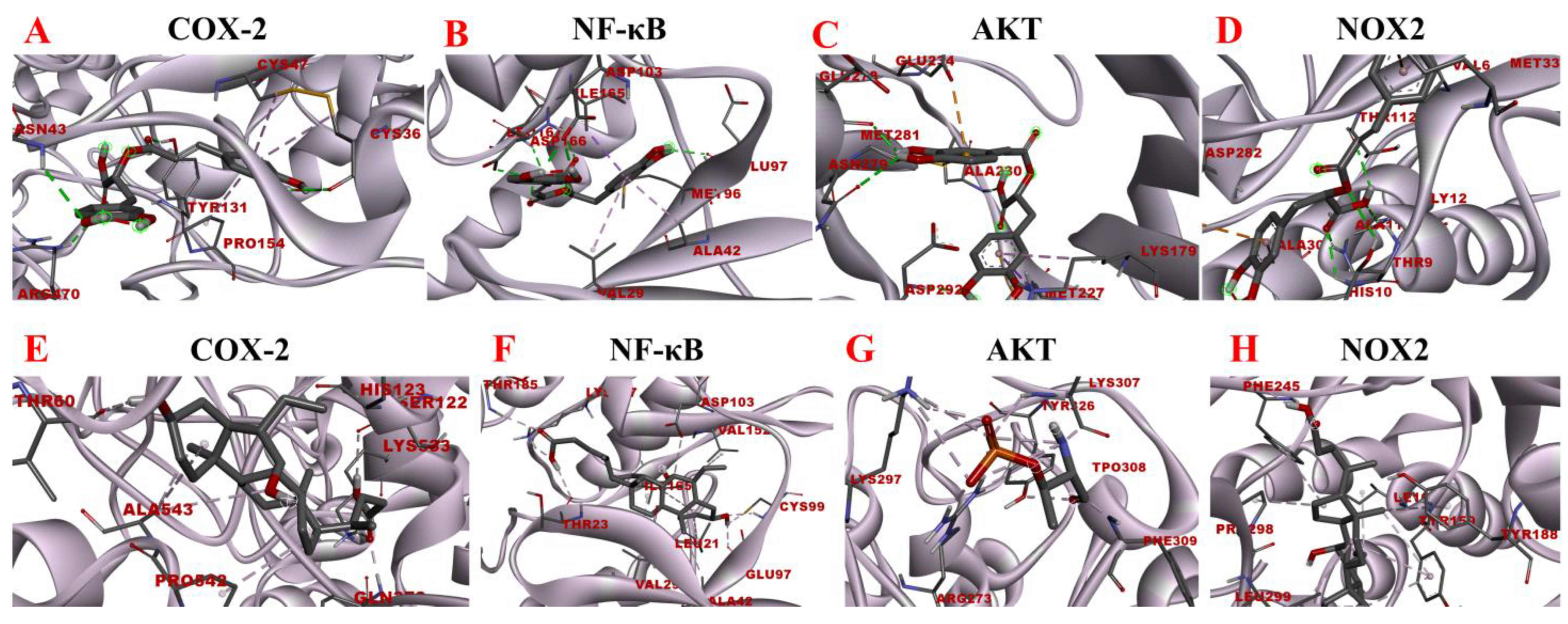
3.4. Prediction of the Therapeutic Potential of Rosmarinic Acid for Liver Diseases by Molecular Docking
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Eslam, M.; Valenti, L.; Romeo, S. Genetics and epigenetics of NAFLD and NASH: Clinical impact. J. Hepatol. 2019, 68, 268–279. [Google Scholar] [CrossRef]
- Duan, X.; Meng, Q.; Wang, C.; Liu, Z.; Liu, Q.; Sun, H.; Sun, P.; Yang, X.; Huo, X.; Peng, J.; et al. Calycosin attenuates triglyceride accumulation and hepatic fibrosis in murine model of non-alcoholic steatohepatitis via activating farnesoid X receptor. Phytomedicine 2017, 25, 83–92. [Google Scholar] [CrossRef]
- Xu, J.; Dai, L.; Zhang, Y.; Wang, A.; Li, H.; Wang, Y.; Meng, X.; Wu, S.; Wang, Y. Severity of Nonalcoholic Fatty Liver Disease and Risk of Future Ischemic Stroke Events. Stroke 2021, 52, 103–110. [Google Scholar] [CrossRef]
- Younossi, Z.; Anstee, Q.M.; Marietti, M.; Hardy, T.; Henry, L.; Eslam, M.; George, J.; Bugianesi, E. Global burden of NAFLD and NASH: Trends, predictions, risk factors and prevention. Nat. Rev. Gastroenterol. Hepatol. 2018, 15, 11–20. [Google Scholar] [CrossRef] [PubMed]
- Schuppan, D.; Surabattula, R.; Wang, X.Y. Determinants of fibrosis progression and regression in NASH. J. Hepatol. 2018, 68, 238–250. [Google Scholar] [CrossRef]
- Sheka, A.C.; Adeyi, O.; Thompson, J.; Hameed, B.; Crawford, P.A.; Ikramuddin, S. Nonalcoholic Steatohepatitis: A Review. JAMA 2020, 323, 1175–1183. [Google Scholar] [CrossRef]
- Hua, Y.Q.; Zeng, Y.; Xu, J.; Xu, X.L. Naringenin alleviates nonalcoholic steatohepatitis in middle-aged Apoe-/-mice: Role of SIRT1. Phytomedicine 2021, 81, 153412. [Google Scholar] [CrossRef]
- Li, S.; Li, X.; Chen, F.; Liu, M.; Ning, L.; Yan, Y.; Zhang, S.; Huang, S.; Tu, C. Nobiletin mitigates hepatocytes death, liver inflammation, and fibrosis in a murine model of NASH through modulating hepatic oxidative stress and mitochondrial dysfunction. J. Nutr. Biochem. 2022, 100, 108888. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, T.; Reker, D.; Schneider, P.; Schneider, G. Counting on natural products for drug design. Nat. Chem. 2016, 8, 531–541. [Google Scholar] [CrossRef]
- Harvey, A.L.; Edrada-Ebel, R.; Quinn, R.J. The re-emergence of natural products for drug discovery in the genomics era. Nat. Rev. Drug Discov. 2015, 14, 111–129. [Google Scholar] [CrossRef]
- Gouveia, D.N.; Guimarães, A.G.; Santos, W.B.D.R.; Quintans-Júnior, L.J. Natural products as a perspective for cancer pain management: A systematic review. Phytomedicine 2019, 58, 152766. [Google Scholar] [CrossRef]
- Chopra, B.; Dhingra, A.K. Natural products: A lead for drug discovery and development. Phytother. Res. 2021, 35, 4660–4702. [Google Scholar] [CrossRef] [PubMed]
- Du, K.Z.; Sun, A.L.; Yan, C.; Liang, C.; Qi, L.; Wang, C.; Yang, R.; Cui, Y.; Shang, Y.; Li, J.; et al. Recent advances of green pretreatment techniques for quality control of natural products. Electrophoresis 2020, 41, 1469–1481. [Google Scholar] [CrossRef]
- Bian, J.; Wang, K.; Wang, Q.L.; Wang, P.; Wang, T.; Shi, W.Y.; Ruan, Q.G. Dracocephalum heterophyllum (DH) Exhibits Potent Anti-Proliferative Effects on Autoreactive CD4+ T Cells and Ameliorates the Development of Experimental Autoimmune Uveitis. Front. Immunol. 2020, 11, 575669. [Google Scholar] [CrossRef]
- Shi, Q.Q.; Dang, J.; Wen, H.X.; Yuan, X.; Tao, Y.D.; Wang, Q.L. Anti-hepatitis, antioxidant activities and bioactive compounds of Dracocephalum heterophyllum extracts. Bot. Stud. 2016, 57, 16. [Google Scholar] [CrossRef]
- Stappen, I.; Wanner, J.; Tabanca, N.; Wedge, D.E.; Ali, A.; Kaul, V.K.; Lal, B.; Jaitak, V.; Gochev, V.K.; Schmidt, E.; et al. Chemical Composition and Biological Activity of Essential Oils of Dracocephalum heterophyllum and Hyssopus officinalis from Western Himalaya. Nat. Prod. Commun. 2015, 10, 133–138. [Google Scholar] [CrossRef] [PubMed]
- Khoo, H.T.; Leow, C.H. Advancements in the preparation and application of monolithic silica columns for efficient separation in liquid chromatography. Talanta 2021, 224, 121777. [Google Scholar] [CrossRef]
- Gulcin, İ. Antioxidants and antioxidant methods: An updated overview. Arch. Toxicol. 2020, 94, 651–715. [Google Scholar] [CrossRef]
- Zhang, X.W.; Bian, G.L.; Kang, P.Y.; Cheng, X.J.; Yan, K.; Liu, Y.L.; Gao, Y.X.; Li, D.Q. Recent advance in the discovery of tyrosinase inhibitors from natural sources via separation methods. J. Enzyme Inhib. Med. Chem. 2021, 36, 2104–2117. [Google Scholar] [CrossRef] [PubMed]
- Crampon, K.; Giorkallos, A.; Deldossi, M.; Baud, S.; Steffenel, L.A. Machine-learning methods for ligand-protein molecular docking. Drug Discov. Today 2022, 27, 151–164. [Google Scholar] [CrossRef]
- Ballante, F.; Kooistra, A.J.; Kampen, S.; de Graaf, C.; Carlsson, J. Structure-Based Virtual Screening for Ligands of G Protein-Coupled Receptors: What Can Molecular Docking Do for You? Pharmacol. Rev. 2021, 73, 527–565. [Google Scholar] [CrossRef]
- Batool, M.; Ahmad, B.; Choi, S. A Structure-Based Drug Discovery Paradigm. Int. J. Mol. Sci. 2019, 20, 2783. [Google Scholar] [CrossRef]
- Tacke, F.; Zimmermann, H.W. Macrophage heterogeneity in liver injury and fibrosis. J. Hepatol. 2014, 60, 1090–1096. [Google Scholar] [CrossRef]
- Parola, M.; Pinzani, M. Liver fibrosis: Pathophysiology, pathogenetic targets and clinical issues. Mol. Asp. Med. 2019, 65, 37–55. [Google Scholar] [CrossRef] [PubMed]
- Schwabe, R.F.; Tabas, I.; Pajvani, U.B. Mechanisms of Fibrosis Development in Nonalcoholic Steatohepatitis. Gastroenterology 2020, 158, 1913–1928. [Google Scholar] [CrossRef] [PubMed]
- Higashi, T.; Friedman, S.L.; Hoshida, Y. Hepatic stellate cells as key target in liver fibrosis. Adv. Drug Deliv. Rev. 2017, 121, 27–42. [Google Scholar] [CrossRef]
- Wen, Y.; Lambrecht, J.; Ju, C.; Tacke, F. Hepatic macrophages in liver homeostasis and diseases-diversity, plasticity and therapeutic opportunities. Cell. Mol. Immunol. 2021, 18, 45–56. [Google Scholar] [CrossRef] [PubMed]
- Wang, C.; Ma, C.; Gong, L.; Guo, Y.; Fu, K.; Zhang, Y.; Zhou, H.; Li, Y. Macrophage Polarization and Its Role in Liver Disease. Front. Immunol. 2021, 12, 803037. [Google Scholar] [CrossRef]
- Mohammadi, A.; Blesso, C.N.; Barreto, G.E.; Banach, M.; Majeed, M.; Sahebkar, A. Macrophage plasticity, polarization and function in response to curcumin, a diet-derived polyphenol, as an immunomodulatory agent. J. Nutr. Biochem. 2019, 66, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Yamate, J.; Izawa, T.; Kuwamura, M. Histopathological Analysis of Rat Hepatotoxicity Based on Macrophage Functions: In Particular, an Analysis for Thioacetamide-induced Hepatic Lesions. Food Saf. 2016, 4, 61–73. [Google Scholar] [CrossRef]
- Lin, C.C.; Yang, H.M. Fibrolamellar Carcinoma: A Concise Review. Arch. Pathol. Lab. Med. 2018, 142, 1141–1145. [Google Scholar] [CrossRef]
- Xie, L.; Lee, D.Y.; Shang, Y.; Cao, X.; Wang, S.; Liao, J.; Zhang, T.; Dai, R. Characterization of spirostanol glycosides and furostanol glycosides from anemarrhenae rhizoma as dual targeted inhibitors of 5-lipoxygenase and Cyclooxygenase-2 by employing a combination of affinity ultrafiltration and HPLC/MS. Phytomedicine 2020, 77, 153284. [Google Scholar] [CrossRef]
- Yang, H.; Xuefeng, Y.; Shandong, W.; Jianhua, X. COX-2 in liver fibrosis. Clin. Chim. Acta 2020, 506, 196–203. [Google Scholar] [CrossRef]
- Dang, J.; Ma, J.; Du, Y.; Dawa, Y.; Wang, Q.; Chen, C.; Wang, Q.; Tao, Y.; Ji, T. Large-scale preparative isolation of bergenin standard substance from Saxifraga atrata using polyamide coupled with MCI GEL® CHP20P as stationary phases in medium pressure chromatography. J. Chromatogr. B 2021, 1170, 122617. [Google Scholar] [CrossRef]
- Yuan, C.; Dang, J.; Han, Y.; Liu, C.; Yu, S.; Lv, Y.; Cui, Y.; Wang, Z.; Li, G. Preparative isolation of maltol glycoside from Dianthus superbus and its anti-inflammatory activity in vitro. RSC Adv. 2022, 12, 5031–5041. [Google Scholar] [CrossRef]
- Dapkevicius, A.; van Beek, T.A.; Lelyveld, G.P.; van Veldhuizen, A.; de Groot, A.; Linssen, J.P.; Venskutonis, R. Isolation and structure elucidation of radical scavengers from Thymus vulgaris leaves. J. Nat. Prod. 2002, 65, 892–896. [Google Scholar] [CrossRef] [PubMed]
- Panzitt, K.; Wagner, M. FXR in liver physiology: Multiple faces to regulate liver metabolism. Biochim. Biophys. Acta Mol. Basis Dis. 2021, 1867, 166133. [Google Scholar] [CrossRef] [PubMed]
- Filali-Mouncef, Y.; Hunter, C.; Roccio, F.; Zagkou, S.; Dupont, N.; Primard, C.; Proikas-Cezanne, T.; Reggiori, F. The ménage à trois of autophagy, lipid droplets and liver disease. Autophagy 2022, 18, 50–72. [Google Scholar] [CrossRef] [PubMed]
- Wang, B.; Tontonoz, P. Liver X receptors in lipid signalling and membrane homeostasis. Nat. Rev. Endocrinol. 2018, 14, 452–463. [Google Scholar] [CrossRef]
- Lu, M.C.; Ji, J.A.; Jiang, Z.Y.; You, Q.D. The Keap1-Nrf2-ARE Pathway As a Potential Preventive and Therapeutic Target: An Update. Med. Res. Rev. Sep. 2016, 36, 924–963. [Google Scholar] [CrossRef]
- Bhattacharjee, S.; Dashwood, R.H. Epigenetic Regulation of NRF2/KEAP1 by Phytochemicals. Antioxidants 2020, 9, 865. [Google Scholar] [CrossRef]
- Alhouayek, M.; Muccioli, G.G. COX-2-derived endocannabinoid metabolites as novel inflammatory mediators. Trends Pharmacol. Sci. 2014, 35, 284–292. [Google Scholar] [CrossRef]
- Lin, S.; Li, X.; Zhang, J.; Zhang, Y. Omentin-1: Protective impact on ischemic stroke via ameliorating atherosclerosis. Clin. Chim. Acta 2021, 517, 31–40. [Google Scholar] [CrossRef]
- Yahfoufi, N.; Alsadi, N.; Jambi, M.; Matar, C. The Immunomodulatory and Anti-Inflammatory Role of Polyphenols. Nutrients 2018, 10, 1618. [Google Scholar] [CrossRef]


| Gene | Forward Primer (5′-3′) | Reverse Primer (5′-3′) |
|---|---|---|
| α-SMA | CTGACAGAGGCACCACTGAA | CATCTCCAGAGTCCAGCACA |
| Col1α1 | GAGCGGAGAGTACTGGATCG | TACTCGAACGGGAATCCATC |
| CD68 | TACATGGCGGTGGAGTACAA | AGGTGGACAGCTGGTGAAAG |
| MCP-1 | ACTGCATCTGCCCTAAGGTCT | AGGCATCACAGTCCGAGTCA |
| Col1α1 | TGCCGTGACCTCAAGATGTG | CACAAGCGTGCTGTAGGTGA |
| GAPDH | TCTCCTGCGACTTCAACA | TGGTCCAGGGTTTCTTACT |
| Proteins | Binding Energy (kcal/mol) | Binding Residues | Type |
|---|---|---|---|
| LXR | −7.77 | LEU-439 LYS-434 TRP-433 HIS-421 HIS-421 HIS-421 VAL-425 LEU-299 PHE-335 THR-302 MET-298 | Pi-Sigma Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Sigma Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl |
| PKC | −5.89 | PHE-664 LEU-511 TYR-460 ALA-407 LEU-386 ALA-521 GLU-428 PHE-523 VAL-394 LEU-432 LYS-409 | Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl |
| FXR | −7.17 | SER-389 ARG-438 ARG-438 ASP-391 PRO-390 THR-439 ARG-438 GLU-402 | Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Cation Conventional Hydrogen Bond Pi-Alkyl Pi-Sigma Pi-Alkyl Conventional Hydrogen Bond |
| MAPK | −5.87 | TYR-35 ASP-168 GLU-71 ARG-67 LEU-75 | Pi-Pi Stacked Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Alkyl |
| Proteins | Binding Energy (kcal/mol) | Binding Residues | Type |
|---|---|---|---|
| LXR | −9.44 | PRO-436 LEU-439 LYS-434 VAL-425 PHE-254 LEU-428 LEU-331 PHE-335 PHE-257 HIS-421 | Pi-Alkyl Pi-Alkyl Carbon Hydrogen Bond Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl |
| PKC | −8.39 | PHE-664 LEU-461 LEU-386 LEU-511 TYR-460 VAL-394 ALA-407 ALA-521 LEU-432 MET-458 GLU-428 LYS-409 | Pi-Lone Pair Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond |
| FXR | −8.76 | LEU-434 ARG-438 ARG-438 ASP-391 LEU-409 PRO-390 GLU-402 | Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond |
| MAPK | −7.34 | TYR-35 GLU-71 ARG-67 ALA-51 LYS-53 ILE-84 LEU-167 HIS-107 | Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond |
| Proteins | Binding Energy (kcal/mol) | Binding Residues | Type |
|---|---|---|---|
| Nrf2 | −7.61 | GLY-367 VAL-606 VAL-465 GLY-605 ILE-559 VAL-608 ALA-607 VAL-561 VAL-512 CYS-513 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Carbon Hydrogen Bond Pi-Sigma Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Sulfur |
| Keap1 | −7.96 | ARG-415 VAL-465 VAL-418 GLY-367 VAL-606 ALA-366 ILE-559 | Carbon Hydrogen Bond Carbon Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Alkyl Conventional Hydrogen Bond |
| HO-1 | −6.57 | THR-135 TYR-134 ARG-183 LYS-18 LYS-22 GLU-29 THR-26 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Carbon Hydrogen Bond Pi-Sigma Conventional Hydrogen Bond Conventional Hydrogen Bond |
| GSH-Px | −8.11 | GLY-31 THR-57 THR-57 SER-30 CYS-58 GLY-29 ASP-331 ASP-331 CYS-63 CYS-63 GLY-28 GLU-50 | Conventional Hydrogen Bond Conventional Hydrogen Bond Carbon Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Carbon Hydrogen Bond Pi-Anion Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond |
| GST | −8.41 | TYR-132 LYS-127 ARG-131 GLN-54 ARG-45 TYR-9 PRO-56 PHE-220 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Carbon Hydrogen Bond Pi-Pi Stacked |
| Proteins | Binding Energy (kcal/mol) | Binding Residues | Type |
|---|---|---|---|
| Nrf2 | −9.42 | VAL-418 VAL-465 VAL-512 ILE-416 ARG-415 ALA-556 | Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl |
| Keap1 | −9.25 | GLY-367 VAL-512 ALA-366 ALA-556 ILE-416 GLY-462 ARG-415 ARG-415 ARG-415 | Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Pi-Alkyl Carbon Hydrogen Bond Pi-Alkyl Carbon Hydrogen Bond Conventional Hydrogen Bond |
| HO-1 | −8.65 | ARG-183 PHE-207 HIS-25 GLY-139 ALA-28 PHE-207 | Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl |
| GSH-Px | −8.67 | ILE-343 ARG-347 TYR-114 TYR-114 VAL-64 LEU-110 CYS-58 CYS-58 | Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Sigma Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl |
| GST | −8.47 | ALA-216 LEU-107 LEU-107 LEU-108 TYR-9 PHE-220 PHE-220 VAL-55 GLN-53 ARG-131 GLN-54 | Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Pi-Sigma Conventional Hydrogen Bond Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond |
| Proteins | Binding Energy (kcal/mol) | Binding Residues | Type |
|---|---|---|---|
| COX-2 | −6.21 | ARG-470 TYR-131 ASN-43 CYS-47 PRO-154 CYS-36 CYS-36 ASN-43 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond |
| NF-κB | −6.94 | GLU-97 LEU-167 ASP-166 ASP-103 MET-96 ALA-42 VAL-29 ILE-165 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Sulfur Pi-Alkyl Pi-Alkyl Pi-Sigma |
| AKT | −6.73 | GLU-198 ASP-292 ALA-230 MET-227 LYS-179 MET-281 GLU-234 ASN-279 GLU-278 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Sigma Pi-Alkyl Pi-Sulfur Pi-Anion Conventional Hydrogen Bond Conventional Hydrogen Bond |
| NOX2 | −6.67 | HIS-10 ALA-11 GLY-12 THR-112 THR-9 ASP-282 ALA-303 MET-33 VAL-81 VAL-6 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Anion Pi-Alkyl Pi-Sulfur Conventional Hydrogen Bond Pi-Alkyl |
| Proteins | Binding Energy (kcal/mol) | Binding Residues | Type |
|---|---|---|---|
| COX-2 | −8.15 | GLN-373 LYS-533 SER-122 PRO-542 ALA-543 HIS-123 THR-60 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond |
| NF-κB | −8.81 | LYA-147 THR-185 THR-23 ASP-103 VAL-152 VAL-29 LEU-21 ILE-165 ALA-42 GLU-97 CYS-99 | Conventional Hydrogen Bond Conventional Hydrogen Bond Conventional Hydrogen Bond Carbon Hydrogen Bond Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Conventional Hydrogen Bond |
| AKT | −7.56 | ARG-273 LYS-297 LYS-297 LYS-307 | Attractive Charge Attractive Charge Conventional Hydrogen Bond Conventional Hydrogen Bond |
| NOX2 | −8.71 | TYR-188 PHE-245 PHE-245 LEU-299 TYR-159 PRO-298 ILE-160 | Pi-Alkyl Pi-Alkyl Conventional Hydrogen Bond Pi-Alkyl Pi-Alkyl Pi-Alkyl Pi-Alkyl |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Fang, Y.; Sun, D.; Li, G.; Lv, Y.; Li, J.; Wang, Q.; Dang, J. Ethyl Acetate Extract of Dracocephalum heterophyllum Benth Ameliorates Nonalcoholic Steatohepatitis and Fibrosis via Regulating Bile Acid Metabolism, Oxidative Stress and Inhibiting Inflammation. Separations 2022, 9, 273. https://doi.org/10.3390/separations9100273
Fang Y, Sun D, Li G, Lv Y, Li J, Wang Q, Dang J. Ethyl Acetate Extract of Dracocephalum heterophyllum Benth Ameliorates Nonalcoholic Steatohepatitis and Fibrosis via Regulating Bile Acid Metabolism, Oxidative Stress and Inhibiting Inflammation. Separations. 2022; 9(10):273. https://doi.org/10.3390/separations9100273
Chicago/Turabian StyleFang, Yan, Dandan Sun, Gang Li, Yue Lv, Jia Li, Qilan Wang, and Jun Dang. 2022. "Ethyl Acetate Extract of Dracocephalum heterophyllum Benth Ameliorates Nonalcoholic Steatohepatitis and Fibrosis via Regulating Bile Acid Metabolism, Oxidative Stress and Inhibiting Inflammation" Separations 9, no. 10: 273. https://doi.org/10.3390/separations9100273
APA StyleFang, Y., Sun, D., Li, G., Lv, Y., Li, J., Wang, Q., & Dang, J. (2022). Ethyl Acetate Extract of Dracocephalum heterophyllum Benth Ameliorates Nonalcoholic Steatohepatitis and Fibrosis via Regulating Bile Acid Metabolism, Oxidative Stress and Inhibiting Inflammation. Separations, 9(10), 273. https://doi.org/10.3390/separations9100273








