The Prevalence of Benzodiazepine Use among Italian Drivers in 15,988 Cases of Driving License Regranting from 2015 to 2023: Risks and Implications for Driving Fitness
Abstract
1. Introduction
2. Materials and Methods
2.1. Samples Collection and Screening Analysis
2.2. Sample Preparation and GC/MS Analysis
2.3. Data Analysis
3. Results
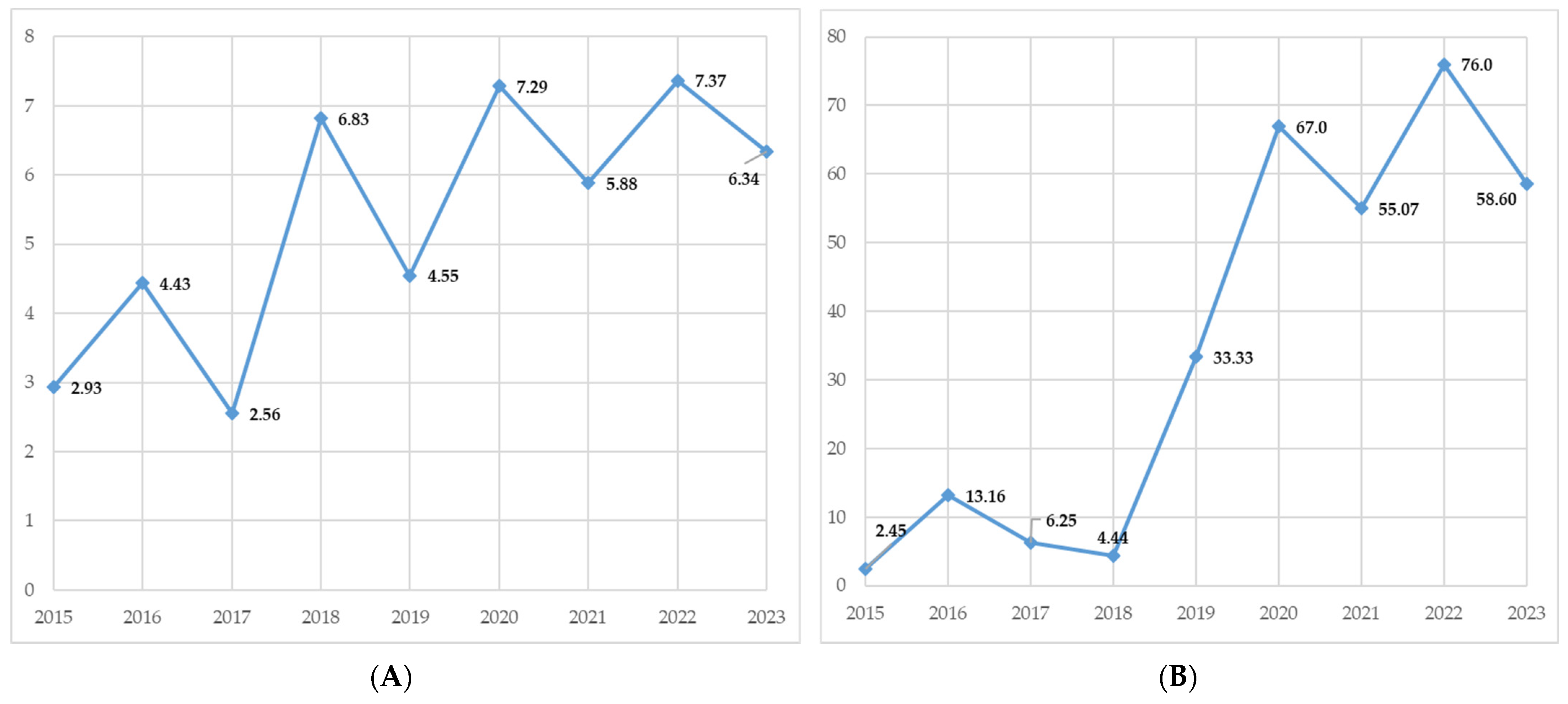
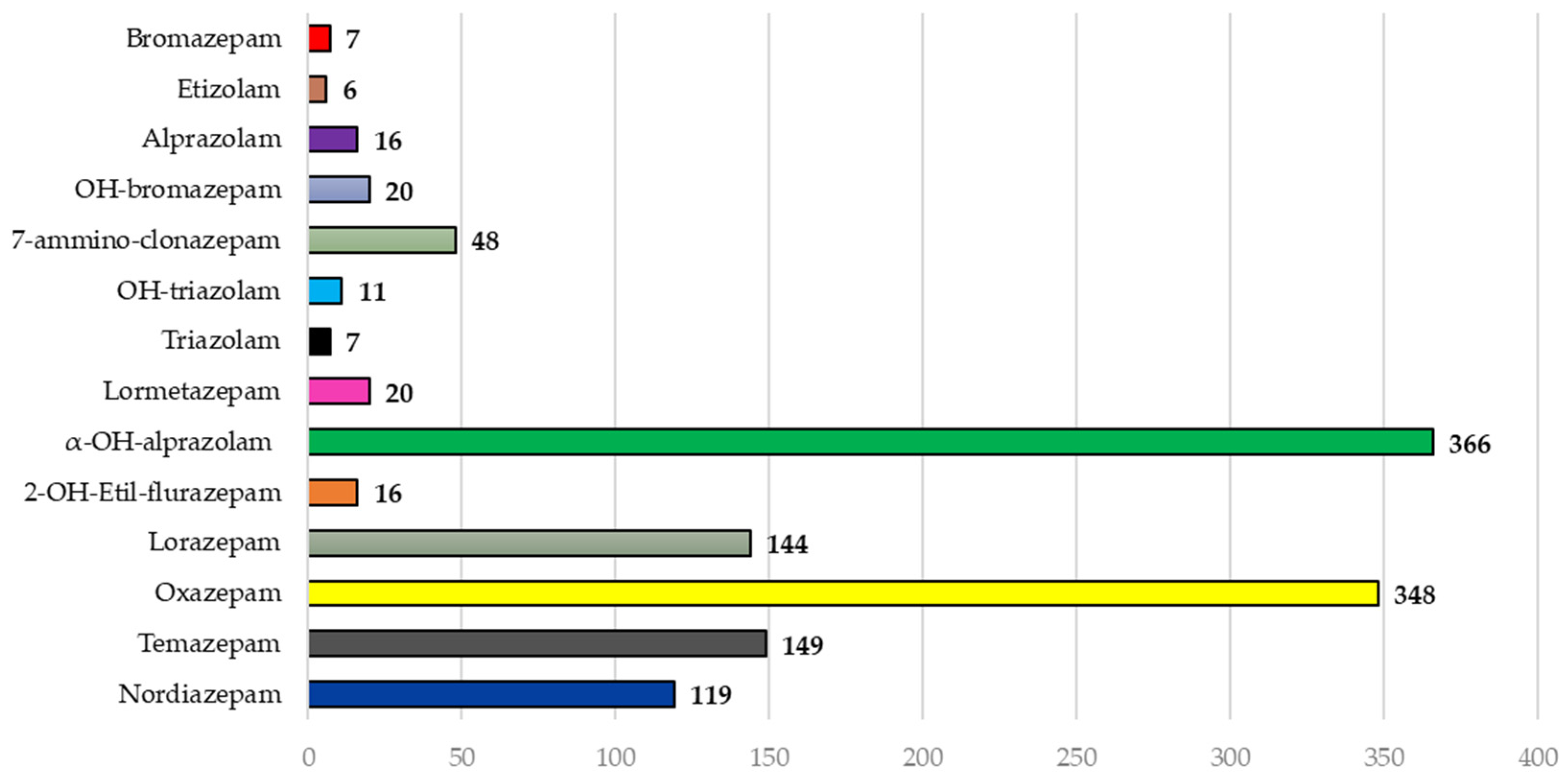
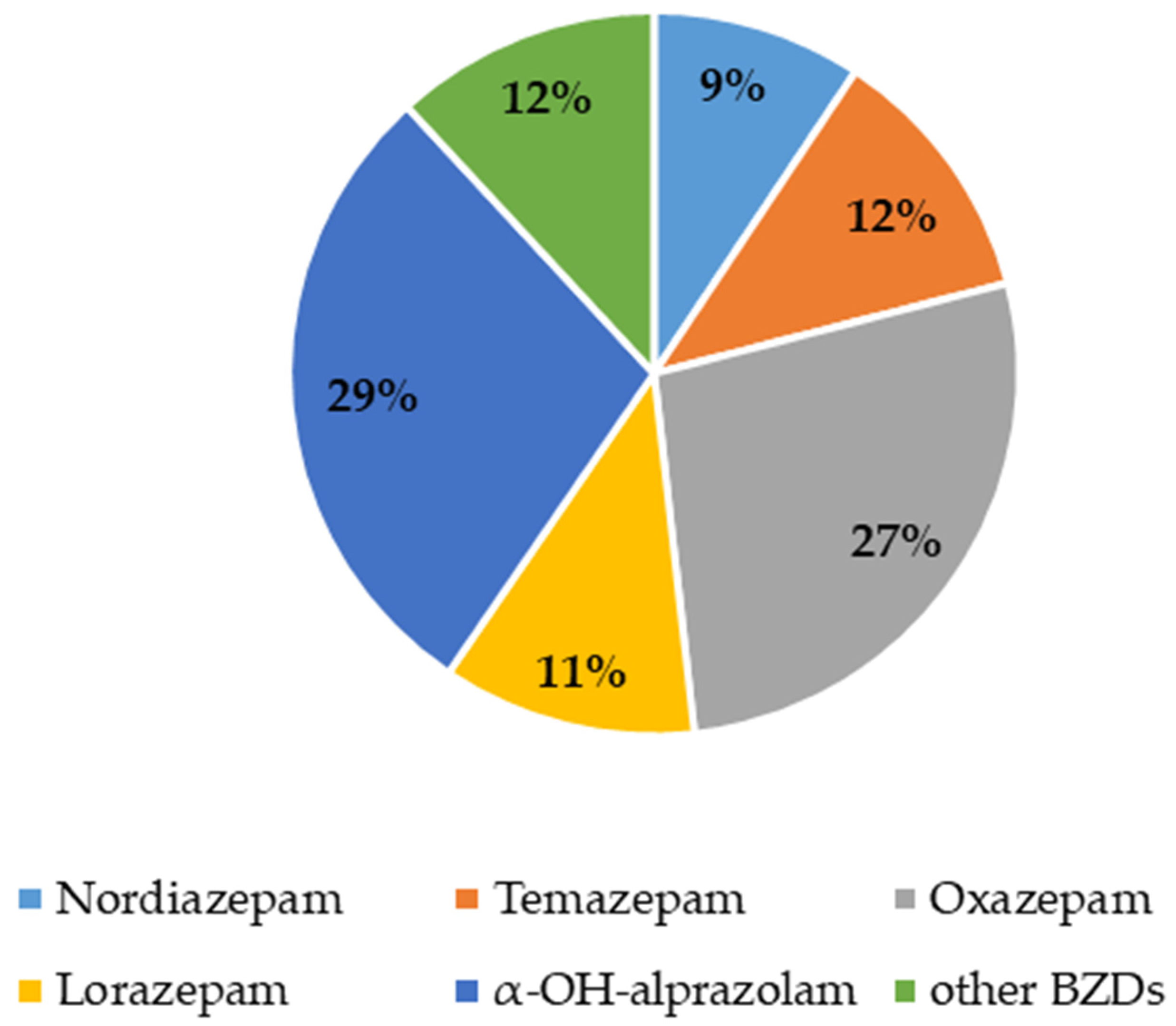
Epidemiological Data
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Edinoff, A.N.; Nix, C.A.; Hollier, J.; Sagrera, C.E.; Delacroix, B.M.; Abubakar, T.; Cornett, E.M.; Kaye, A.M.; Kaye, A.D. Benzodiazepines: Uses, Dangers, and Clinical Considerations. Neurol. Int. 2021, 13, 594–607. [Google Scholar] [CrossRef] [PubMed]
- EMCDDA New Benzodiazepines in Europe—A Review. Available online: https://www.emcdda.europa.eu/publications/rapid-communications/new-benzodiazepines-europe-review_en (accessed on 27 June 2023).
- World Health Organization (WHO). Mental Disorders. Available online: https://www.who.int/news-room/fact-sheets/detail/mental-disorders (accessed on 27 June 2023).
- European Monitoring Centre for Drugs and Drug Addiction. European Drug Report 2023: Trends and Developments; European Monitoring Centre for Drugs and Drug Addiction: Lisbon, Portugal, 2023. [Google Scholar]
- Public Health Scotland Rapid Action Drug Alerts and Response (RADAR). Quarterly Report; Public Health Scotland: Edinburgh, Scotland, UK, 2024. [Google Scholar]
- SAMHSA. National Household Survey on Drug Abuse (NHSDA). Annual Report. 2020. Available online: https://www.samhsa.gov/data/ (accessed on 8 February 2022).
- SAMHSA. National Survey on Drug Use and Health: Detailed Tables. Substance Abuse and Mental Health Services Administration. Available online: https://www.samhsa.gov/data/report/2021-nsduh-detailed-tables (accessed on 4 January 2023).
- Diversion Control Division; National Forensic Laboratory Information System. NFLIS-Drug 2022 Annual Report; U.S. Department of Justice, U.S. Drug Enforcement Administration: Springfield, VA, USA, 2023. [Google Scholar]
- Airagnes, G.; Lemogne, C.; Renuy, A.; Goldberg, M.; Hoertel, N.; Roquelaure, Y.; Limosin, F.; Zins, M. Prevalence of Prescribed Benzodiazepine Long-Term Use in the French General Population According to Sociodemographic and Clinical Factors: Findings from the CONSTANCES Cohort. BMC Public. Health 2019, 19, 566. [Google Scholar] [CrossRef] [PubMed]
- Torres-Bondia, F.; de Batlle, J.; Galván, L.; Buti, M.; Barbé, F.; Piñol-Ripoll, G. Trends in the Consumption Rates of Benzodiazepines and Benzodiazepine-Related Drugs in the Health Region of Lleida from 2002 to 2015. BMC Public Health 2020, 20, 818. [Google Scholar] [CrossRef] [PubMed]
- Wu, C.-C.; Liao, M.-H.; Su, C.-H.; Poly, T.N.; Lin, M.-C. Benzodiazepine Use and the Risk of Dementia in the Elderly Population: An Umbrella Review of Meta-Analyses. J. Pers. Med. 2023, 13, 1485. [Google Scholar] [CrossRef]
- Olfson, M.; King, M.; Schoenbaum, M. Benzodiazepine Use in the United States. JAMA Psychiatry 2015, 72, 136–142. [Google Scholar] [CrossRef] [PubMed]
- Hockenhull, J.; Amioka, E.; Black, J.C.; Forber, A.; Haynes, C.M.; Wood, D.M.; Dart, R.C.; Dargan, P.I. Non-medical Use of Benzodiazepines and GABA Analogues in Europe. Br. J. Clin. Pharmacol. 2021, 87, 1684–1694. [Google Scholar] [CrossRef] [PubMed]
- The Department for Drug Policies (DPA)—Presidency of the Council of Ministers. Report on Drug Addiction in Italy in 2023 (Data Collected in 2022); The Department for Drug Policies (DPA)—Presidency of the Council of Ministers: Rome, Italy, 2022. [Google Scholar]
- Gagliardi, J. Consumption-Rate-of-Benzodiazepines-by-Active-Ingredient-in-Italy. Available online: https://www.statista.com/statistics/914467/consumption-rate-of-benzodiazepines-by-active-ingredient-in-italy/ (accessed on 30 August 2023).
- Gagliardi, J. Consumption Rate of Benzodiazepines in Italy 2022, by Region. Available online: https://www.statista.com/statistics/915561/consumption-rate-of-benzodiazepines-by-region-in-italy/ (accessed on 30 August 2023).
- The Medicines Utilization Monitoring Centre. National Report on Medicines Use in Italy—Year 2022. Available online: https://www.aifa.gov.it/documents/20142/2143103/Rapporto-OsMed-2022_EN.pdf (accessed on 1 December 2023).
- Colizzi, M.; Meneghin, N.; Bertoldi, A.; Lugoboni, F. Further Evidence on the Interplay between Benzodiazepine and Z-Drug Abuse and Emotion Dysregulation. J. Affect. Disord. Rep. 2021, 6, 100234. [Google Scholar] [CrossRef]
- Ministry of Health. Allegato 1—Riassunto Delle Caratteristiche Del Prodotto; Supplemento ordinario alla GAZZETTA UFFICIALE; Ministry of Justice: Rome, Italy, 1999; pp. 7–24. [Google Scholar]
- Thomas, R.E. Benzodiazepine Use and Motor Vehicle Accidents. Systematic Review of Reported Association. Can. Fam. Physician 1998, 44, 799–808. [Google Scholar] [PubMed]
- Smink, B.E.; Egberts, A.C.G.; Lusthof, K.J.; Uges, D.R.A.; de Gier, J.J. The Relationship between Benzodiazepine Use and Traffic Accidents: A Systematic Literature Review. CNS Drugs 2010, 24, 639–653. [Google Scholar] [CrossRef]
- Orriols, L.; Gbaguidi, G.N.; Contrand, B.; Gadegbeku, B.; Lagarde, E. Trends in Benzodiazepine Anxiolytics and Z-Hypnotics Use among French Drivers Involved in Road Traffic Crashes from 2005 to 2015: A Responsibility Case-Control Study. Inj. Epidemiol. 2019, 6, 32. [Google Scholar] [CrossRef]
- Van der Sluiszen, N.N.J.J.M.; Vermeeren, A.; Verster, J.C.; van de Loo, A.J.A.E.; van Dijken, J.H.; Veldstra, J.L.; Brookhuis, K.A.; de Waard, D.; Ramaekers, J.G. Driving Performance and Neurocognitive Skills of Long-Term Users of Benzodiazepine Anxiolytics and Hypnotics. Hum. Psychopharmacol. 2019, 34, e2715. [Google Scholar] [CrossRef] [PubMed]
- Dubois, S.; Bédard, M.; Weaver, B. The Impact of Benzodiazepines on Safe Driving. Traffic Inj. Prev. 2008, 9, 404–413. [Google Scholar] [CrossRef] [PubMed]
- Longo, M.C.; Hunter, C.E.; Lokan, R.J.; White, J.M.; White, M.A. The Prevalence of Alcohol, Cannabinoids, Benzodiazepines and Stimulants amongst Injured Drivers and Their Role in Driver Culpability. Accid. Anal. Prev. 2000, 32, 623–632. [Google Scholar] [CrossRef] [PubMed]
- Longo, M.; Lokan, R.; White, J. The Relationship between Blood Benzodiazepine Concentration and Vehicle Crash Culpability. J. Traffic Med. 2001, 29, 36–43. [Google Scholar]
- Jones, A.W. Driving Under the Influence of Drugs in Sweden with Zero Concentration Limits in Blood for Controlled Substances. Traffic Inj. Prev. 2005, 6, 317–322. [Google Scholar] [CrossRef] [PubMed]
- Van der Sluiszen, N.; Vermeeren, A.; Jongen, S.; Vinckenbosch, F.; Ramaekers, J. Influence of Long-Term Benzodiazepine Use on Neurocognitive Skills Related to Driving Performance in Patient Populations: A Review. Pharmacopsychiatry 2017, 50, 189–196. [Google Scholar] [CrossRef] [PubMed]
- Smink, B.E.; Lusthof, K.J.; de Gier, J.J.; Uges, D.R.A.; Egberts, A.C.G. The Relation between the Blood Benzodiazepine Concentration and Performance in Suspected Impaired Drivers. J. Forensic Leg. Med. 2008, 15, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Verster, J. Effects of Alprazolam on Driving Ability, Memory Functioning and Psychomotor Performance A Randomized, Placebo-Controlled Study. Neuropsychopharmacology 2002, 27, 260–269. [Google Scholar] [CrossRef] [PubMed]
- Pascali, J.P.; Vaiano, F.; Palumbo, D.; Umani Ronchi, F.; Mari, F.; Bertol, E. Psychotropic Substance Abuse and Fitness to Hold a Driving License in Italy. Traffic Inj. Prev. 2019, 20, 244–248. [Google Scholar] [CrossRef]
- Office of Drug and Alcohol Policy and Compliance. DOT Urine Specimen Collection Guidelines; United States Department of Transportation: Washington, DC, USA, 2018. [Google Scholar]
- Strano Rossi, S.; Frison, G.; Chericoni, S.; Bertol, E.; Favretto, D.; Pichini, S.; Salomone, A.; Tagliaro, F.; Vignali, C. Linee Guida per La Determinazione Di Sostanze Stupefacenti e Psicotrope Su Campioni Biologici Con Finalità Tossicologico-Forensi e Medico-Legali. La Riv. Ital. Della Med. Lab. 2023, 19, 192–205. [Google Scholar] [CrossRef]
- Uddin, M.N.; Samanidou, V.F.; Papadoyannis, I.N. Bio-Sample Preparation and Gas Chromatographic Determination of Benzodiazepines—A Review. J. Chromatogr. Sci. 2013, 51, 587–598. [Google Scholar] [CrossRef] [PubMed]
- Balon, R.; Starcevic, V.; Silberman, E.; Cosci, F.; Dubovsky, S.; Fava, G.A.; Nardi, A.E.; Rickels, K.; Salzman, C.; Shader, R.I.; et al. The Rise and Fall and Rise of Benzodiazepines: A Return of the Stigmatized and Repressed. Braz. J. Psychiatry 2020, 42, 243–244. [Google Scholar] [CrossRef] [PubMed]
- Organisation for Economic Cooperation and Development (OECD). Health at a Glance: Europe 2022; OECD: Paris, France, 2022; ISBN 9789264462113. [Google Scholar]
- Alabaku, O.; Yang, A.; Tharmarajah, S.; Suda, K.; Vigod, S.; Tadrous, M. Global Trends in Antidepressant, Atypical Antipsychotic, and Benzodiazepine Use: A Cross-Sectional Analysis of 64 Countries. PLoS ONE 2023, 18, e0284389. [Google Scholar] [CrossRef] [PubMed]
- EMCDDA Spotlight On… Non-Medical Use of Benzodiazepines. Available online: https://www.emcdda.europa.eu/spotlights/non-medical-use-benzodiazepines_en (accessed on 27 June 2023).
- Leung, S.Y. Benzodiazepines, Opioids and Driving: An Overview of the Experimental Research. Drug Alcohol. Rev. 2011, 30, 281–286. [Google Scholar] [CrossRef] [PubMed]
- Morrow, A.L.; Paul, S.M. Benzodiazepine Enhancement of Gamma-Aminobutyric Acid-Mediated Chloride Ion Flux in Rat Brain Synaptoneurosomes. J. Neurochem. 1988, 50, 302–306. [Google Scholar] [CrossRef] [PubMed]
- Volkow, N.D.; Fowler, J.S.; Gatley, S.J.; Logan, J.; Wang, G.J.; Ding, Y.S.; Dewey, S. PET Evaluation of the Dopamine System of the Human Brain. J. Nucl. Med. 1996, 37, 1242–1256. [Google Scholar]
- Volkow, N.D.; Wang, G.J.; Fowler, J.S.; Hitzemann, R.; Gatley, S.J.; Dewey, S.S.; Pappas, N. Enhanced Sensitivity to Benzodiazepines in Active Cocaine-Abusing Subjects: A PET Study. Am. J. Psychiatry 1998, 155, 200–206. [Google Scholar] [CrossRef]
- Maxwell, H.G.; Dubois, S.; Weaver, B.; Bédard, M. The Additive Effects of Alcohol and Benzodiazepines on Driving. Can. J. Public Health 2010, 101, 353–357. [Google Scholar] [CrossRef]
- Appenzeller, B.M.R.; Schneider, S.; Yegles, M.; Maul, A.; Wennig, R. Drugs and Chronic Alcohol Abuse in Drivers. Forensic Sci. Int. 2005, 155, 83–90. [Google Scholar] [CrossRef]
- Fiorelli, D.; Romani, L.; Treglia, M.; Pallocci, M.; Passalacqua, P.; Coppeta, L.; Marsella, L.T.; Tittarelli, R. Carbohydrate-Deficient Transferrin (CDT) as a Biomarker of Alcohol Abuse: A Retrospective Study of the Italian Drinking Trend among Drivers from 2016 to 2022. Toxics 2023, 11, 914. [Google Scholar] [CrossRef]
- World Health Organization (WHO). COVID-19 Pandemic Triggers 25% Increase in Prevalence of Anxiety and Depression Worldwide. Available online: https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide (accessed on 27 June 2023).
- OECD. A New Benchmark for Mental Health Systems; OECD: Paris, France, 2021; ISBN 9789264710139. [Google Scholar]
- European Commission; Directorate-General for Communication. Flash Eurobarometer FL530: Mental Health, Version v1.00; Directorate-General for Communication: Brussels, Belgium, 2023; Available online: http://data.europa.eu/88u/dataset/s3032_fl530_eng (accessed on 21 May 2024).
- The Italian National Institute of Statistics. Mental Health at Various Stages of Life; The Italian National Institute of Statistics: Rome, Italy, 2018. [Google Scholar]
- Zaami, S.; Graziano, S.; Tittarelli, R.; Beck, R.; Marinelli, E. BDZs, Designer BDZs and Z-Drugs: Pharmacology and Misuse Insights. Curr. Pharm. Des. 2022, 28, 1221–1229. [Google Scholar] [CrossRef] [PubMed]
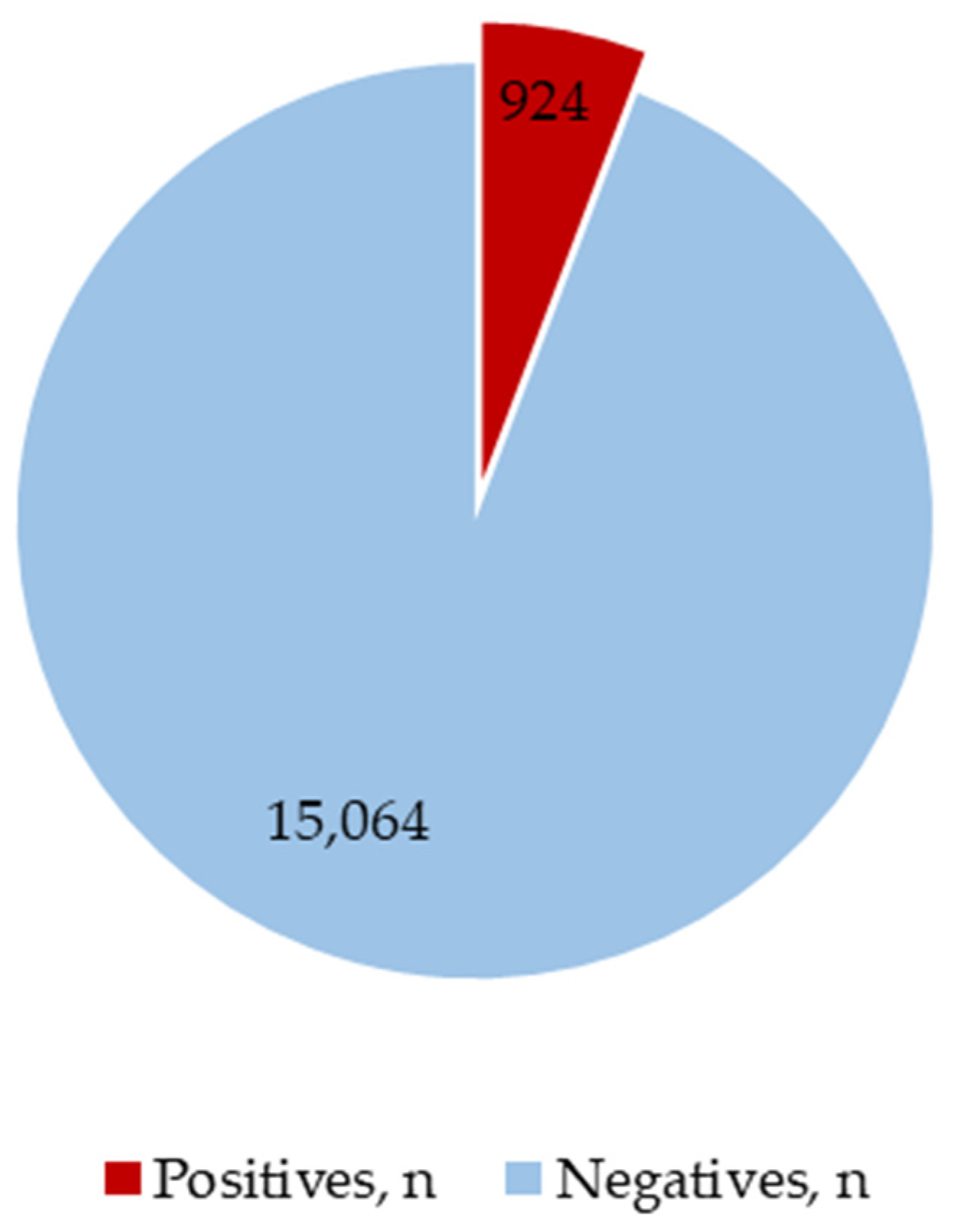


| Study Group | Positives |
|---|---|
| n = 15,988 | n = 924 |
| Female, n (%) | 223 (24.13) |
| Male, n (%) | 701 (75.87) |
| Median Age | 46.74 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Stefani, L.; Mineo, F.; Romani, L.; Vernich, F.; Russo, C.; Marsella, L.T.; Tittarelli, R. The Prevalence of Benzodiazepine Use among Italian Drivers in 15,988 Cases of Driving License Regranting from 2015 to 2023: Risks and Implications for Driving Fitness. Separations 2024, 11, 169. https://doi.org/10.3390/separations11060169
Stefani L, Mineo F, Romani L, Vernich F, Russo C, Marsella LT, Tittarelli R. The Prevalence of Benzodiazepine Use among Italian Drivers in 15,988 Cases of Driving License Regranting from 2015 to 2023: Risks and Implications for Driving Fitness. Separations. 2024; 11(6):169. https://doi.org/10.3390/separations11060169
Chicago/Turabian StyleStefani, Lucrezia, Federico Mineo, Leonardo Romani, Francesca Vernich, Carmelo Russo, Luigi Tonino Marsella, and Roberta Tittarelli. 2024. "The Prevalence of Benzodiazepine Use among Italian Drivers in 15,988 Cases of Driving License Regranting from 2015 to 2023: Risks and Implications for Driving Fitness" Separations 11, no. 6: 169. https://doi.org/10.3390/separations11060169
APA StyleStefani, L., Mineo, F., Romani, L., Vernich, F., Russo, C., Marsella, L. T., & Tittarelli, R. (2024). The Prevalence of Benzodiazepine Use among Italian Drivers in 15,988 Cases of Driving License Regranting from 2015 to 2023: Risks and Implications for Driving Fitness. Separations, 11(6), 169. https://doi.org/10.3390/separations11060169






