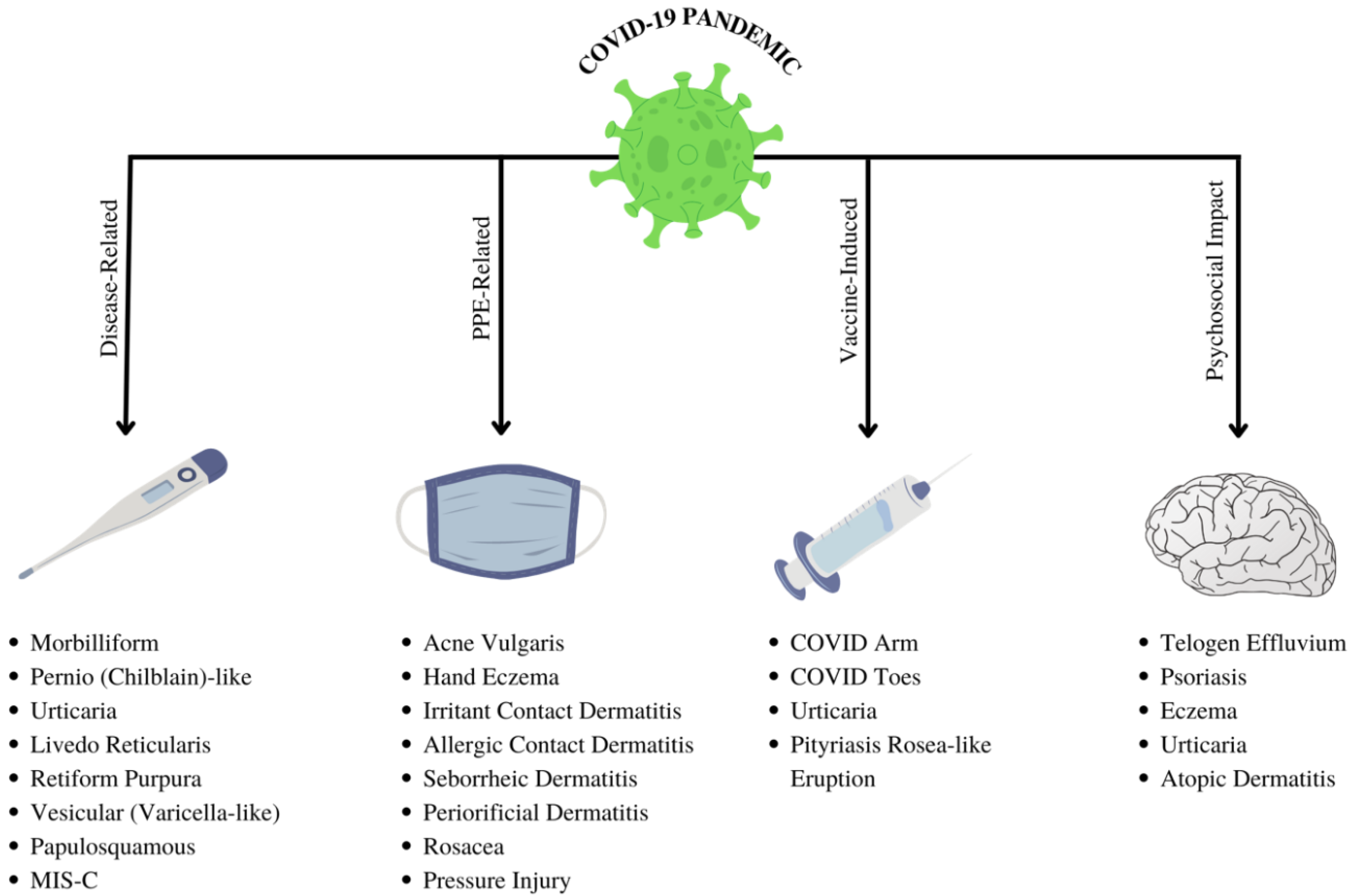
The Impact of COVID-19 Pandemic on Dermatological Conditions: A Novel, Comprehensive Review
Abstract
:1. Introduction
2. Methods
3. Results
4. COVID-19 Specific Dermatological Manifestations
4.1. Exanthematous (Morbilliform) Rash
4.2. Pernio (Chilblain)-like Acral Lesions
4.3. Urticaria
4.4. Livedo Reticularis
4.5. Livedo Racemosa/Retiform Purpura
4.6. Vesicular (Varicella-like) Eruptions
4.7. Papulosquamous Rashes and Pityriasis Rosea
4.8. Multisystem Inflammatory Syndrome in Children
- Fever
- Inflammatory markers
- Failure or involvement of two organ systems
| Rash | Relative Frequency a | COVID Severity b | Reported Treatments |
|---|---|---|---|
| Exanthematous (Morbilliform) | 11–45% [48,130] | Moderate-severe |
–Topical corticosteroids [54,57] – Oral antihistamines [57,131] – Hydroxychloroquine [131] –Low molecular heparin (if suspected coagulopathy) [131] |
| Pernio (Chilblains-like) | 18–53% [48,132] | Mild |
–Avoid cold temperatures and vasoconstrictive agents –Watchful waiting [133,134] –Corticosteroids or nifedipine for refractory cases [133,134] |
| Urticaria | 8.1–19% [23,48,80] | Moderate |
–Second-generation antihistamines [91] –Topical corticosteroids [91] –Low-dose systemic corticosteroids [92] |
| Vesicular (Varicella-like) | 9–19% [48,101] | Moderate | – Watchful waiting [102] |
| Papulosquamous | 9.9% | Moderate | –Not reported |
| Retiform Purpura | 6.4% | Severe | – Anticoagulation [135,136] |
| Livedoid Reaction | 5.3% | Mild | –Watchful waiting [95] |
| MIS-C c | 0.6% | Severe |
–Multidisciplinary approach –IVIG –Anakinra –Low dose aspirin –Enoxaparin –Tocilizumab [129] |
| MIS-C | KD | |
|---|---|---|
| Epidemiology | Non-Hispanic blacks are at higher risk [137,138] | Asians are at higher risk |
| Age of onset | 8–12 years [139] | <5 years |
| Fever | Fever >24 h | Fever > 5 days |
| Cardiovascular Abnormalities | Myocarditis/myocardial dysfunction (left ventricular dysfunction) | Coronary artery abnormalities such as aneurysms are more common |
| Platelet Count | Thrombocytopenia | Thrombocytosis |

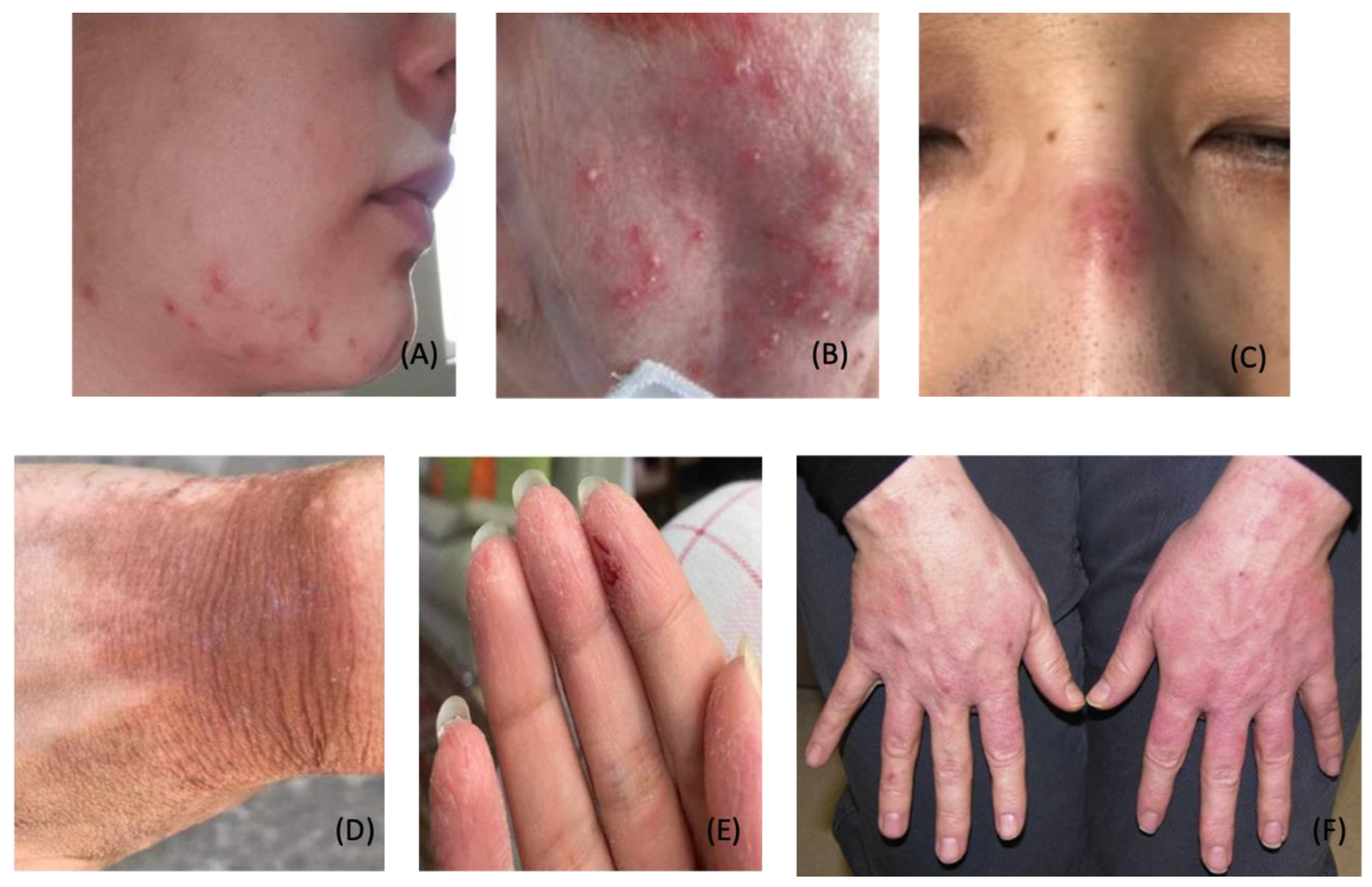
5. Dermatological Conditions Associated with Personal Protective Equipment and Hygiene Products
| Description | Prophylactic Approach | Treatment Approach | |
|---|---|---|---|
| Acne | Inflammation of pilosebaceous glands, likely worsened by heat and humidity from face mask microenvironment [29] |
–Use salicylic acid or benzoyl peroxide wash for daily facial cleansing –Use non-comedogenic products –Use a cotton mask when possible [142] –Take a 15-min mask break every 2 h [143] |
–Mild: Salicylic acid or benzoyl peroxide wash daily; topical retinoid; topical antibiotics –Moderate: Follow recommendations for mild, add oral antibiotics (i.e., doxycycline); consider oral spironolactone or combined oral contraceptives for female patients –Severe: Consider isotretinoin [144] |
| Periorificial Dermatitis | Inflammatory papulopustular condition with underlying erythema surrounding eyes, nose and/or mouth, likely worsened by face mask microenvironment [29] |
–Avoid topical steroids –Use gentle cleansers –Take a 15-min mask break every 2 h [143] |
–Mild: Topical calcineurin inhibitors, erythromycin, and/or metronidazole [145] –Moderate/Severe: Oral tetracyclines [146] |
| Papulopustular Rosacea | Facial erythema with telangiectasias, typically overlying the malar and nasal bridge regions, is likely worsened by the face mask microenvironment [29] |
–Gentle skin cleansing –Use gentle moisturizers daily –Avoid potential triggers (i.e., spicy food, alcohol, direct sunlight, acute physiologic stressors) [147] |
–Mild: Topical azelaic acid, topical ivermectin, or metronidazole; consider sodium sulfacetamide wash –Moderate: Consider oral doxycycline –Severe: Consider isotretinoin [148] –Erythema: Topical brimonidine or oxymetazoline [144] |
| Pressure Injury | Damage to skin and soft tissue due to continuous pressure and/or shear force; may present as erythema or ulcerated skin, often over the bridge of the nose, behind ears, or on cheeks [149] |
–Ensure appropriate mask fit –Topical application foam or hydrocolloid dressing at contact points [150,151] |
–Use moisturizers, skin sealants, cyanoacrylate –Use foam or hydrocolloid dressing at contact points [149] |
| Contact Dermatitis (Irritant) | Inflammation is caused by direct physical or chemical insult, often behind the ears, on cheeks, or over the nasal bridge [29] |
–Avoid allergens –Use a cotton mask when possible –Use foam or hydrocolloid dressing at contact points [143,150,151] –Take 15-min mask break every 2 h [143,151] | – Topical steroids or calcineurin inhibitors [144] |
| Contact Dermatitis (Allergic) | Localized and well-demarcated type IV hypersensitivity reaction; common triggers found in PPE include formaldehyde, dibromodicyanobutane, thurium, and metal wire [29] |
–Localized: Topical steroids or calcineurin inhibitors –Widespread: Systemic corticosteroids and other immunosuppressive therapies [144] | |
| Hand Eczema | Itchiness, dryness, and redness of the hands due to excessive hand washing, disinfectants, and glove use [144] |
–Minimize use of hot water –Frequent use of hypoallergenic moisturizer –Avoid allergens and/or irritants [152,153] |
–Nighttime petroleum-based emollient with cotton gloves –Short course topical corticosteroids [144] |
| Seborrheic Dermatitis | Superficial fungal infection, often affecting ears, nasolabial folds, eyebrows, and scalp; likely worsened by face mask microenvironment [29] |
–Gentle skin cleansing –Frequent moisturizer use [144] |
–Topical ketoconazole shampoo, body wash, or cream –For itching and erythema, mild topical corticosteroids or calcineurin inhibitors can be used [144] |
6. COVID-19 Vaccine-Induced Dermatological Manifestations

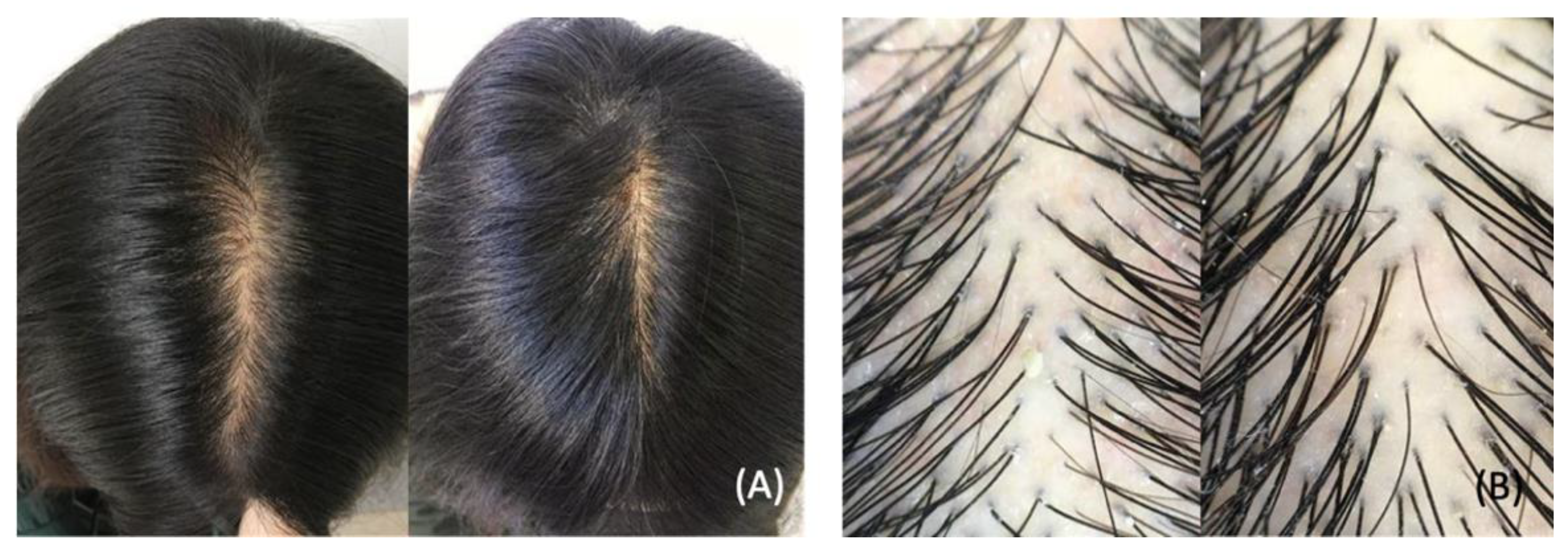
7. Stress-Induced Dermatological Conditions
7.1. Telogen Effluvium
7.2. Psoriasis
7.3. Eczema, Urticaria, and Atopic dermatitis
8. Role of Dermatologists in the COVID-19 Pandemic
8.1. Teledermatology
8.2. Clinical Practice Guidelines
9. Discussion
10. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
- We applaud the worldwide frontline physicians who have selflessly provided innovative medical care since the onset of the pandemic. Their paramount sacrifices will leave an eternal impact on the medical community and scientific literature.
- The lead author warmly acknowledges Joshua Pendlebury, CTRS for his military service in the United States Marine Corps. His sacrifices ultimately inspired an unwavering commitment to provide excellent medical care to service members. Additional gratitude is expressed to Pendlebury for his hard work at home, behind-the-scenes. His steadfast efforts and enthusiastic sacrifices made this project conceivable and achievable.
- This novel publication is dedicated to A.G. Pendlebury.
- May she blaze new trails.
- May the chain remain unbroken.
Conflicts of Interest
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A Novel Coronavirus from Patients with Pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef]
- Cucinotta, D.; Vanelli, M. WHO Declares COVID-19 a Pandemic. Acta Biomed. 2020, 91, 157–160. [Google Scholar] [CrossRef]
- Worldmeter. Coronavirus Cases. Available online: https://www.worldometers.info/coronavirus/ (accessed on 1 June 2022).
- Li, J.; Jia, H.; Tian, M.; Wu, N.; Yang, X.; Qi, J.; Ren, W.; Li, F.; Bian, H. SARS-CoV-2 and Emerging Variants: Unmasking Structure, Function, Infection, and Immune Escape Mechanisms. Front. Cell Infect. Microbiol. 2022, 12, 869832. [Google Scholar] [CrossRef]
- Liu, J.; Li, Y.; Liu, Q.; Yao, Q.; Wang, X.; Zhang, H.; Chen, R.; Ren, L.; Min, J.; Deng, F.; et al. SARS-CoV-2 cell tropism and multiorgan infection. Cell Discov. 2021, 7, 17. [Google Scholar] [CrossRef] [PubMed]
- Conceicao, C.; Thakur, N.; Human, S.; Kelly, J.T.; Logan, L.; Bialy, D.; Bhat, S.; Stevenson-Leggett, P.; Zagrajek, A.K.; Hollinghurst, P.; et al. The SARS-CoV-2 Spike protein has a broad tropism for mammalian ACE2 proteins. PLoS Biol. 2020, 18, e3001016. [Google Scholar] [CrossRef] [PubMed]
- Zou, X.; Chen, K.; Zou, J.; Han, P.; Hao, J.; Han, Z. Single-cell RNA-seq data analysis on the receptor ACE2 expression reveals the potential risk of different human organs vulnerable to 2019-nCoV infection. Front. Med. 2020, 14, 185–192. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Qi, F.; Qian, S.; Zhang, S.; Zhang, Z. Single cell RNA sequencing of 13 human tissues identify cell types and receptors of human coronaviruses. Biochem. Biophys. Res. Commun. 2020, 526, 135–140. [Google Scholar] [CrossRef]
- Zhang, H.; Kang, Z.; Gong, H.; Xu, D.; Wang, J.; Li, Z.; Li, Z.; Cui, X.; Xiao, J.; Zhan, J.; et al. Digestive system is a potential route of COVID-19: An analysis of single-cell coexpression pattern of key proteins in viral entry process. Gut 2020, 69, 1010–1018. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhao, Z.; Wang, Y.; Zhou, Y.; Ma, Y.; Zuo, W. Single-Cell RNA Expression Profiling of ACE2, the Receptor of SARS-CoV-2. Am. J. Respir. Crit. Care Med. 2020, 202, 756–759, Erratum in Am. J. Respir. Crit. Care Med. 2021, 15, 782. [Google Scholar] [CrossRef]
- Kabbani, N.; Olds, J.L. Does COVID19 Infect the Brain? If So, Smokers Might Be at a Higher Risk. Mol. Pharmacol. 2020, 97, 351–353. [Google Scholar] [CrossRef]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; Chen, Q. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral. Sci. 2020, 12, 8. [Google Scholar] [CrossRef] [PubMed]
- Kaya, G.; Kaya, A.; Saurat, J.H. Clinical and Histopathological Features and Potential Pathological Mechanisms of Skin Lesions in COVID-19: Review of the Literature. Dermatopathology 2020, 7, 2. [Google Scholar] [CrossRef] [PubMed]
- Mjaess, G.; Karam, A.; Aoun, F.; Albisinni, S.; Roumeguère, T. COVID-19 and the male susceptibility: The role of ACE2, TMPRSS2 and the androgen receptor. Prog. Urol. 2020, 30, 484–487. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.; Wang, Y.; Li, X.; Ren, L.; Zhao, J.; Hu, Y.; Zhang, L.; Fan, G.; Xu, J.; Gu, X.; et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020, 395, 497–506, Erratum in Lancet 2020, 395, 496. [Google Scholar] [CrossRef] [Green Version]
- Richardson, S.; Hirsch, J.S.; Narasimhan, M.; Crawford, J.M.; McGinn, T.; Davidson, K.W.; The Northwell COVID-19 Research Consortium; Barnaby, D.P.; Becker, L.B.; Chelico, J.D.; et al. Presenting Characteristics, Comorbidities, and Outcomes among 5700 Patients Hospitalized with COVID-19 in the New York City Area. JAMA 2020, 323, 2052–2059, Erratum in JAMA 2020, 323, 2098. [Google Scholar] [CrossRef]
- Wang, D.; Hu, B.; Hu, C.; Zhu, F.; Liu, X.; Zhang, J.; Wang, B.; Xiang, H.; Cheng, Z.; Xiong, Y.; et al. Clinical Characteristics of 138 Hospitalized Patients with 2019 Novel Coronavirus-Infected Pneumonia in Wuhan, China. JAMA 2020, 323, 1061–1069, Erratum in JAMA 2021, 325, 1113. [Google Scholar] [CrossRef]
- Gupta, A.; Madhavan, M.V.; Sehgal, K.; Nair, N.; Mahajan, S.; Sehrawat, T.S.; Bikdeli, B.; Ahluwalia, N.; Ausiello, J.C.; Wan, E.Y.; et al. Extrapulmonary manifestations of COVID-19. Nat. Med. 2020, 26, 1017–1032. [Google Scholar] [CrossRef]
- Xue, X.; Mi, Z.; Wang, Z.; Pang, Z.; Liu, H.; Zhang, F. High Expression of ACE2 on Keratinocytes Reveals Skin as a Potential Target for SARS-CoV-2. J. Investig. Dermatol. 2021, 141, 206–209.e1. [Google Scholar] [CrossRef]
- Wei, C.; Friedman, A.J. COVID-19 Pandemic: Are There Unique Cutaneous Manifestations in Patients Infected With SARS-CoV-2? J. Drugs Dermatol. 2020, 19, 554–555. [Google Scholar]
- Freeman, E.E.; McMahon, D.E.; Fitzgerald, M.E.; Fox, L.P.; Rosenbach, M.; Takeshita, J.; French, L.E.; Thiers, B.H.; Hruza, G.J. The American Academy of Dermatology COVID-19 registry: Crowdsourcing dermatology in the age of COVID-19. J. Am. Acad. Dermatol. 2020, 83, 509–510. [Google Scholar] [CrossRef]
- Freeman, E.E.; Chamberlin, G.C.; McMahon, D.E.; Hruza, G.J.; Wall, D.; Meah, N.; Sinclair, R.; Balogh, E.A.; Feldman, S.R.; Lowes, M.A.; et al. Dermatology COVID-19 Registries: Updates and Future Directions. Dermatol. Clin. 2021, 39, 575–585. [Google Scholar] [CrossRef] [PubMed]
- Freeman, E.E.; McMahon, D.E.; Lipoff, J.B.; Rosenbach, M.; Kovarik, C.; Desai, S.R.; Harp, J.; Takeshita, J.; French, L.E.; Lim, H.W.; et al. The spectrum of COVID-19-associated dermatologic manifestations: An international registry of 716 patients from 31 countries. J. Am. Acad. Dermatol. 2020, 83, 1118–1129. [Google Scholar] [CrossRef] [PubMed]
- Marzano, A.V.; Genovese, G.; Moltrasio, C.; Gaspari, V.; Vezzoli, P.; Maione, V.; Misciali, C.; Sena, P.; Patrizi, A.; Offidani, A.; et al. The clinical spectrum of COVID-19-associated cutaneous manifestations: An Italian multicenter study of 200 adult patients. J. Am. Acad. Dermatol. 2021, 84, 1356–1363. [Google Scholar] [CrossRef] [PubMed]
- Lavery, M.J.; Bouvier, C.A.; Thompson, B. Cutaneous manifestations of COVID-19 in children (and adults): A virus that does not discriminate. Clin. Dermatol. 2021, 39, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Young, T.K.; Shaw, K.S.; Shah, J.K.; Noor, A.; Alperin, R.A.; Ratner, A.J.; Orlow, S.J.; Betensky, R.A.; Shust, G.F.; Kahn, P.J.; et al. Mucocutaneous Manifestations of Multisystem Inflammatory Syndrome in Children During the COVID-19 Pandemic. JAMA Dermatol. 2021, 157, 207–212. [Google Scholar] [CrossRef]
- Naka, F.; Melnick, L.; Gorelik, M.; Morel, K.D. A dermatologic perspective on multisystem inflammatory syndrome in children. Clin. Dermatol. 2021, 39, 337–343. [Google Scholar] [CrossRef]
- Damiani, G.; Gironi, L.C.; Grada, A.; Kridin, K.; Finelli, R.; Buja, A.; Bragazzi, N.L.; Pigatto, P.D.M.; Savoia, P. COVID-19 related masks increase severity of both acne (maskne) and rosacea (mask rosacea): Multi-center, real-life, telemedical, and observational prospective study. Dermatol. Ther. 2021, 34, e14848. [Google Scholar] [CrossRef]
- Rudd, E.; Walsh, S. Mask related acne (“maskne”) and other facial dermatoses. BMJ 2021, 373, n1304. [Google Scholar] [CrossRef]
- Yu, J.; Chen, J.K.; Mowad, C.M.; Reeder, M.; Hylwa, S.; Chisolm, S.; Dunnick, C.A.; Goldminz, A.M.; Jacob, S.E.; Wu, P.A.; et al. Occupational dermatitis to facial personal protective equipment in health care workers: A systematic review. J. Am. Acad. Dermatol. 2021, 84, 486–494. [Google Scholar] [CrossRef]
- Lin, P.; Zhu, S.; Huang, Y.; Li, L.; Tao, J.; Lei, T.; Song, J.; Liu, D.; Chen, L.; Shi, Y.; et al. Adverse skin reactions among healthcare workers during the coronavirus disease 2019 outbreak: A survey in Wuhan and its surrounding regions. Br. J. Dermatol. 2020, 183, 190–192. [Google Scholar] [CrossRef] [Green Version]
- Lan, J.; Song, Z.; Miao, X.; Li, H.; Li, Y.; Dong, L.; Yang, J.; An, X.; Zhang, Y.; Yang, L.; et al. Skin damage among health care workers managing coronavirus disease-2019. J. Am. Acad. Dermatol. 2020, 82, 1215–1216. [Google Scholar] [CrossRef] [PubMed]
- Zhou, N.Y.; Yang, L.; Dong, L.Y.; Li, Y.; An, X.J.; Yang, J.; Yang, L.; Huang, C.Z.; Tao, J. Prevention and Treatment of Skin Damage Caused by Personal Protective Equipment: Experience of the First-Line Clinicians Treating 2019-nCoV Infection. Int. J. Dermatol. Venereol. 2020; ahead of print. [Google Scholar] [CrossRef]
- Vasireddy, D.; Atluri, P.; Malayala, S.V.; Vanaparthy, R.; Mohan, G. Review of COVID-19 Vaccines Approved in the United States of America for Emergency Use. J. Clin. Med. Res. 2021, 13, 204–213, Erratum in J. Clin. Med. Res. 2021, 13, 412. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Interim Clinical Considerations for Use of COVID-19 Vaccines. Available online: https://www.cdc.gov/vaccines/covid-19/clinical-considerations/covid-19-vaccines-us.html#Appendix-C (accessed on 10 February 2022).
- Meara, A.S.; Silkowski, M.; Quin, K.; Jarjour, W. A Case of Chilblains-like Lesions Post SARS-CoV-2 Vaccine? J. Rheumatol. 2021, 48, 1754. [Google Scholar] [CrossRef]
- Català, A.; Muñoz-Santos, C.; Galván-Casas, C.; Roncero Riesco, M.; Revilla Nebreda, D.; Solá-Truyols, A.; Giavedoni, P.; Llamas-Velasco, M.; González-Cruz, C.; Cubiró, X.; et al. Cutaneous reactions after SARS-CoV-2 vaccination: A cross-sectional Spanish nationwide study of 405 cases. Br. J. Dermatol. 2022, 186, 142–152. [Google Scholar] [CrossRef] [PubMed]
- McMahon, D.E.; Amerson, E.; Rosenbach, M.; Lipoff, J.B.; Moustafa, D.; Tyagi, A.; Desai, S.R.; French, L.E.; Lim, H.W.; Thiers, B.H.; et al. Cutaneous reactions reported after Moderna and Pfizer COVID-19 vaccination: A registry-based study of 414 cases. J. Am. Acad. Dermatol. 2021, 85, 46–55. [Google Scholar] [CrossRef]
- Glowacz, F.; Schmits, E. Psychological distress during the COVID-19 lockdown: The young adults most at risk. Psychiatry Res. 2020, 293, 113486. [Google Scholar] [CrossRef]
- Wang, Y.; Kala, M.P.; Jafar, T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0244630. [Google Scholar] [CrossRef]
- Kim, H.H.; Jung, J.H. Social Isolation and Psychological Distress during the COVID-19 Pandemic: A Cross-National Analysis. Gerontologist 2021, 61, 103–113. [Google Scholar] [CrossRef]
- Rossi, A.; Magri, F.; Sernicola, A.; Michelini, S.; Caro, G.; Muscianese, M.; Di Fraia, M.; Chello, C.; Fortuna, M.C.; Grieco, T. Telogen Effluvium after SARS-CoV-2 Infection: A Series of Cases and Possible Pathogenetic Mechanisms. Skin Appendage Disord. 2021, 21, 1–5. [Google Scholar] [CrossRef]
- Turkmen, D.; Altunisik, N.; Sener, S.; Colak, C. Evaluation of the effects of COVID-19 pandemic on hair diseases through a web-based questionnaire. Dermatol. Ther. 2020, 33, e13923. [Google Scholar] [CrossRef]
- Rivetti, N.; Barruscotti, S. Management of telogen effluvium during the COVID-19 emergency: Psychological implications. Dermatol. Ther. 2020, 33, e13648. [Google Scholar] [CrossRef] [PubMed]
- Mahil, S.K.; Yates, M.; Yiu, Z.; Langan, S.M.; Tsakok, T.; Dand, N.; Mason, K.J.; McAteer, H.; Meynell, F.; Coker, B.; et al. Describing the burden of the COVID-19 pandemic in people with psoriasis: Findings from a global cross-sectional study. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e636–e640. [Google Scholar] [CrossRef] [PubMed]
- Yazdany, J.; Manno, R.L. Delayed Hypersensitivity. In Current Medical Diagnosis & Treatment 2022; Papadakis, M.A., McPhee, S.J., Rabow, M.W., McQuaid, K.R., Eds.; McGraw Hill: New York, NY, USA, 2022; Available online: https://accessmedicine.mhmedical.com/content.aspx?bookid=3081§ionid=258968670 (accessed on 20 May 2022).
- Giavedoni, P.; Podlipnik, S.; Pericàs, J.M.; Fuertes de Vega, I.; García-Herrera, A.; Alós, L.; Carrera, C.; Andreu-Febrer, C.; Sanz-Beltran, J.; Riquelme-Mc Loughlin, C.; et al. Skin Manifestations in COVID-19: Prevalence and Relationship with Disease Severity. J. Clin. Med. 2020, 9, 3261. [Google Scholar] [CrossRef] [PubMed]
- Galván Casas, C.; Català, A.; Carretero Hernández, G.; Rodríguez-Jiménez, P.; Fernández-Nieto, D.; Rodríguez-Villa Lario, A.; Navarro Fernández, I.; Ruiz-Villaverde, R.; Falkenhain-López, D.; Llamas Velasco, M.; et al. Classification of the cutaneous manifestations of COVID-19: A rapid prospective nationwide consensus study in Spain with 375 cases. Br. J. Dermatol. 2020, 183, 71–77. [Google Scholar] [CrossRef]
- Do, M.H.; Stewart, C.R.; Harp, J. Cutaneous Manifestations of COVID-19 in the Inpatient Setting. Dermatol. Clin. 2021, 39, 521–532. [Google Scholar] [CrossRef] [PubMed]
- Rekhtman, S.; Tannenbaum, R.; Strunk, A.; Birabaharan, M.; Wright, S.; Grbic, N.; Joseph, A.; Lin, S.K.; Zhang, A.C.; Lee, E.C.; et al. Eruptions and related clinical course among 296 hospitalized adults with confirmed COVID-19. J. Am. Acad. Dermatol. 2021, 84, 946–952. [Google Scholar] [CrossRef] [PubMed]
- Askin, O.; Altunkalem, R.N.; Altinisik, D.D.; Uzuncakmak, T.K.; Tursen, U.; Kutlubay, Z. Cutaneous manifestations in hospitalized patients diagnosed as COVID-19. Dermatol. Ther. 2020, 33, e13896. [Google Scholar] [CrossRef]
- Català, A.; Galván-Casas, C.; Carretero-Hernández, G.; Rodríguez-Jiménez, P.; Fernández-Nieto, D.; Rodríguez-Villa, A.; Navarro-Fernández, Í.; Ruiz-Villaverde, R.; Falkenhain-López, D.; Llamas-Velasco, M.; et al. Maculopapular eruptions associated to COVID-19: A subanalysis of the COVID-Piel study. Dermatol. Ther. 2020, 33, e14170. [Google Scholar] [CrossRef]
- Ghimire, K.; Adhikari, N. Morbilliform rashes in a patient with COVID-19 infection: A case report. JNMA J. Nepal Med. Assoc. 2021, 59, 399–401. [Google Scholar] [CrossRef]
- Kulkarni, R.B.; Lederman, Y.; Afiari, A.; Savage, J.A.; Jacob, J. Morbilliform Rash: An Uncommon Herald of SARS-CoV-2. Cureus 2020, 12, e9321. [Google Scholar] [CrossRef]
- Fattori, A.; Cribier, B.; Chenard, M.P.; Mitcov, M.; Mayeur, S.; Weingertner, N. Cutaneous manifestations in patients with coronavirus disease 2019: Clinical and histological findings. Hum. Pathol. 2021, 107, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Ahouach, B.; Harent, S.; Ullmer, A.; Martres, P.; Bégon, E.; Blum, L.; Tess, O.; Bachmeyer, C. Cutaneous lesions in a patient with COVID-19: Are they related? Br. J. Dermatol. 2020, 183, e31. [Google Scholar] [CrossRef] [PubMed]
- Najarian, D.J. Morbilliform exanthem associated with COVID-19. JAAD Case Rep. 2020, 6, 493–494. [Google Scholar] [CrossRef] [PubMed]
- Hedrich, C.M.; Fiebig, B.; Hauck, F.H.; Sallmann, S.; Hahn, G.; Pfeiffer, C.; Heubner, G.; Lee-Kirsch, M.A.; Gahr, M. Chilblain lupus erythematosus—A review of literature. Clin. Rheumatol. 2008, 27, 949–954. [Google Scholar] [CrossRef]
- Su, W.P.; Perniciaro, C.; Rogers, R.S., 3rd; White, J.W., Jr. Chilblain lupus erythematosus (lupus pernio): Clinical review of the Mayo Clinic experience and proposal of diagnostic criteria. Cutis 1994, 54, 395–399. [Google Scholar]
- Cappel, J.A.; Wetter, D.A. Clinical characteristics, etiologic associations, laboratory findings, treatment, and proposal of diagnostic criteria of pernio (chilblains) in a series of 104 patients at Mayo Clinic, 2000 to 2011. Mayo Clin. Proc. 2014, 89, 207–215. [Google Scholar] [CrossRef]
- de Masson, A.; Bouaziz, J.D.; Sulimovic, L.; Cassius, C.; Jachiet, M.; Ionescu, M.A.; Rybojad, M.; Bagot, M.; Duong, T.A.; SNDV (French National Union of Dermatologists-Venereologists). Chilblains is a common cutaneous finding during the COVID-19 pandemic: A retrospective nationwide study from France. J. Am. Acad. Dermatol. 2020, 83, 667–670. [Google Scholar] [CrossRef]
- Piccolo, V.; Neri, I.; Filippeschi, C.; Oranges, T.; Argenziano, G.; Battarra, V.C.; Berti, S.; Manunza, F.; Fortina, A.B.; Di Lernia, V.; et al. Chilblain-like lesions during COVID-19 epidemic: A preliminary study on 63 patients. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e291–e293. [Google Scholar] [CrossRef]
- Kolivras, A.; Dehavay, F.; Delplace, D.; Feoli, F.; Meiers, I.; Milone, L.; Olemans, C.; Sass, U.; Theunis, A.; Thompson, C.T.; et al. Coronavirus (COVID-19) infection-induced chilblains: A case report with histopathologic findings. JAAD Case Rep. 2020, 6, 489–492. [Google Scholar] [CrossRef]
- El Hachem, M.; Diociaiuti, A.; Concato, C.; Carsetti, R.; Carnevale, C.; Ciofi Degli Atti, M.; Giovannelli, L.; Latella, E.; Porzio, O.; Rossi, S.; et al. A clinical, histopathological and laboratory study of 19 consecutive Italian paediatric patients with chilblain-like lesions: Lights and shadows on the relationship with COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 34, 2620–2629. [Google Scholar] [CrossRef]
- Kanitakis, J.; Lesort, C.; Danset, M.; Jullien, D. Chilblain-like acral lesions during the COVID-19 pandemic (“COVID toes”): Histologic, immunofluorescence, and immunohistochemical study of 17 cases. J. Am. Acad. Dermatol. 2020, 83, 870–875. [Google Scholar] [CrossRef] [PubMed]
- Colmenero, I.; Santonja, C.; Alonso-Riaño, M.; Noguera-Morel, L.; Hernández-Martín, A.; Andina, D.; Wiesner, T.; Rodríguez-Peralto, J.L.; Requena, L.; Torrelo, A.; et al. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: Histopathological, immunohistochemical and ultrastructural study of seven paediatric cases. Br. J. Dermatol. 2020, 183, 729–737. [Google Scholar] [CrossRef] [PubMed]
- Santonja, C.; Heras, F.; Núñez, L.; Requena, L. COVID-19 chilblain-like lesion: Immunohistochemical demonstration of SARS-CoV-2 spike protein in blood vessel endothelium and sweat gland epithelium in a polymerase chain reaction-negative patient. Br. J. Dermatol. 2020, 183, 778–780. [Google Scholar] [CrossRef] [PubMed]
- Gambichler, T.; Reuther, J.; Stücker, M.; Stranzenbach, R.; Torres-Reyes, C.; Schlottmann, R.; Schmidt, W.E.; Hayajneh, R.; Sriram, A.; Becker, J.C.; et al. SARS-CoV-2 spike protein is present in both endothelial and eccrine cells of a chilblain-like skin lesion. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e187–e189. [Google Scholar] [CrossRef] [PubMed]
- Ko, C.J.; Harigopal, M.; Damsky, W.; Gehlhausen, J.R.; Bosenberg, M.; Patrignelli, R.; McNiff, J.M. Perniosis during the COVID-19 pandemic: Negative anti-SARS-CoV-2 immunohistochemistry in six patients and comparison to perniosis before the emergence of SARS-CoV-2. J. Cutan. Pathol. 2020, 47, 997–1002. [Google Scholar] [CrossRef]
- Baeck, M.; Hoton, D.; Marot, L.; Herman, A. Chilblains and COVID-19: Why SARS-CoV-2 endothelial infection is questioned. Br. J. Dermatol. 2020, 183, 1152–1153. [Google Scholar] [CrossRef]
- Freeman, E.E.; McMahon, D.E.; Lipoff, J.B.; Rosenbach, M.; Desai, S.R.; Fassett, M.; French, L.E.; Lim, H.W.; Hruza, G.J.; Fox, L.P. Cold and COVID: Recurrent pernio during the COVID-19 pandemic. Br. J. Dermatol. 2021, 185, 214–216. [Google Scholar] [CrossRef]
- Palamaras, I.; Kyriakis, K. Calcium antagonists in dermatology: A review of the evidence and research-based studies. Dermatol. Online J. 2005, 11, 8. [Google Scholar] [CrossRef]
- Whitman, P.A.; Crane, J.S. Pernio; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Kayiran, M.A.; Akdeniz, N. Diagnosis and treatment of urticaria in primary care. North Clin. Istanb. 2019, 6, 93–99. [Google Scholar] [CrossRef] [Green Version]
- Schaefer, P. Acute and Chronic Urticaria: Evaluation and Treatment. Am. Fam. Physician 2017, 95, 717–724. [Google Scholar]
- Sabroe, R.A.; Greaves, M.W. The pathogenesis of chronic idiopathic urticaria. Arch. Dermatol. 1997, 133, 1003–1008. [Google Scholar] [CrossRef] [PubMed]
- Henry, D.; Ackerman, M.; Sancelme, E.; Finon, A.; Esteve, E. Urticarial eruption in COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e244–e245. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Recalcati, S. Cutaneous manifestations in COVID-19: A first perspective. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e212–e213. [Google Scholar] [CrossRef] [PubMed]
- Algaadi, S.A. Urticaria and COVID-19: A review. Dermatol. Ther. 2020, 33, e14290. [Google Scholar] [CrossRef] [PubMed]
- De Giorgi, V.; Recalcati, S.; Jia, Z.; Chong, W.; Ding, R.; Deng, Y.; Scarfi, F.; Venturi, F.; Trane, L.; Gori, A.; et al. Cutaneous manifestations related to coronavirus disease 2019 (COVID-19): A prospective study from China and Italy. J. Am. Acad. Dermatol. 2020, 83, 674–675. [Google Scholar] [CrossRef]
- Dastoli, S.; Bennardo, L.; Patruno, C.; Nisticò, S.P. Are erythema multiforme and urticaria related to a better outcome of COVID-19? Dermatol. Ther. 2020, 33, e13681. [Google Scholar] [CrossRef]
- Jesenak, M.; Banovcin, P.; Diamant, Z. COVID-19, chronic inflammatory respiratory diseases and eosinophils-Observations from reported clinical case series. Allergy 2020, 75, 1819–1822. [Google Scholar] [CrossRef]
- Rosenberg, H.F.; Foster, P.S. Eosinophils and COVID-19: Diagnosis, prognosis, and vaccination strategies. Semin. Immunopathol. 2021, 43, 383–392. [Google Scholar] [CrossRef]
- Ferastraoaru, D.; Hudes, G.; Jerschow, E.; Jariwala, S.; Karagic, M.; de Vos, G.; Rosenstreich, D.; Ramesh, M. Eosinophilia in Asthma Patients Is Protective against Severe COVID-19 Illness. J. Allergy Clin. Immunol. Pract. 2021, 9, 1152–1162.e3. [Google Scholar] [CrossRef]
- Rodríguez-Jiménez, P.; Chicharro, P.; De Argila, D.; Muñoz-Hernández, P.; Llamas-Velasco, M. Urticaria-like lesions in COVID-19 patients are not really urticaria—A case with clinicopathological correlation. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e459–e460. [Google Scholar] [CrossRef]
- Zipursky, J.S.; Croitoru, D. Urticaria and angioedema associated with SARS-CoV-2 infection. CMAJ 2021, 193, e1390. [Google Scholar] [CrossRef] [PubMed]
- Hassan, K. Urticaria and angioedema as a prodromal cutaneous manifestation of SARS-CoV-2 (COVID-19) infection. BMJ Case Rep. 2020, 13, e236981. [Google Scholar] [CrossRef] [PubMed]
- Najafzadeh, M.; Shahzad, F.; Ghaderi, N.; Ansari, K.; Jacob, B.; Wright, A. Urticaria (angioedema) and COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e568–e570. [Google Scholar] [CrossRef] [PubMed]
- Proietti, I.; Mambrin, A.; Bernardini, N.; Tolino, E.; Balduzzi, V.; Maddalena, P.; Marchesiello, A.; Michelini, S.; Volpe, S.; Skroza, N.; et al. Urticaria in an infant with SARS-CoV-2 positivity. Dermatol. Ther. 2020, 33, e14043. [Google Scholar] [CrossRef] [PubMed]
- Morey-Olivé, M.; Espiau, M.; Mercadal-Hally, M.; Lera-Carballo, E.; García-Patos, V. Cutaneous manifestations in the current pandemic of coronavirus infection disease (COVID 2019). An. Pediatr. 2020, 92, 374–375. [Google Scholar] [CrossRef]
- Pagali, S.; Parikh, R.S. Severe urticarial rash as the initial symptom of COVID-19 infection. BMJ Case Rep. 2021, 14, e241793. [Google Scholar] [CrossRef]
- Shanshal, M. Low- dose systemic steroids, an emerging therapeutic option for COVID-19 related urticaria. J. Dermatolog. Treat. 2022, 33, 1140–1141. [Google Scholar] [CrossRef]
- Sajjan, V.V.; Lunge, S.; Swamy, M.B.; Pandit, A.M. Livedo reticularis: A review of the literature. Indian Dermatol. Online J. 2015, 6, 315–321. [Google Scholar] [CrossRef]
- Verheyden, M.; Grosber, M.; Gutermuth, J.; Velkeniers, B. Relapsing symmetric livedo reticularis in a patient with COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e684–e686. [Google Scholar] [CrossRef]
- Khalil, S.; Hinds, B.R.; Manalo, I.F.; Vargas, I.M.; Mallela, S.; Jacobs, R. Livedo reticularis as a presenting sign of severe acute respiratory syndrome coronavirus 2 infection. JAAD Case Rep. 2020, 6, 871–874. [Google Scholar] [CrossRef]
- Agnihothri, R.; Fox, L.P. Clinical Patterns and Morphology of COVID-19 Dermatology. Dermatol. Clin. 2021, 39, 487–503. [Google Scholar] [CrossRef] [PubMed]
- Chand, S.; Rrapi, R.; Lo, J.A.; Song, S.; Gabel, C.K.; Desai, N.; Hoang, M.P.; Kroshinsky, D. Purpuric ulcers associated with COVID-19: A case series. JAAD Case Rep. 2021, 11, 13–19. [Google Scholar] [CrossRef] [PubMed]
- Pincelli, M.S.; Echavarria, A.; Criado, P.R.; Marques, G.F.; Morita, T.; Valente, N.; de Carvalho, J.F. Livedo Racemosa: Clinical, Laboratory, and Histopathological Findings in 33 Patients. Int. J. Low Extrem. Wounds 2021, 20, 22–28. [Google Scholar] [CrossRef] [PubMed]
- Jamshidi, P.; Hajikhani, B.; Mirsaeidi, M.; Vahidnezhad, H.; Dadashi, M.; Nasiri, M.J. Skin Manifestations in COVID-19 Patients: Are They Indicators for Disease Severity? A Systematic Review. Front. Med. 2021, 8, 634208. [Google Scholar] [CrossRef] [PubMed]
- Wysong, A.; Venkatesan, P. An approach to the patient with retiform purpura. Dermatol. Ther. 2011, 24, 151–172. [Google Scholar] [CrossRef] [PubMed]
- Daneshgaran, G.; Dubin, D.P.; Gould, D.J. Cutaneous Manifestations of COVID-19: An Evidence-Based Review. Am. J. Clin. Dermatol. 2020, 21, 627–639. [Google Scholar] [CrossRef]
- Marzano, A.V.; Genovese, G.; Fabbrocini, G.; Pigatto, P.; Monfrecola, G.; Piraccini, B.M.; Veraldi, S.; Rubegni, P.; Cusini, M.; Caputo, V.; et al. Varicella-like exanthem as a specific COVID-19-associated skin manifestation: Multicenter case series of 22 patients. J. Am. Acad. Dermatol. 2020, 83, 280–285. [Google Scholar] [CrossRef]
- Fernandez-Nieto, D.; Ortega-Quijano, D.; Jimenez-Cauhe, J.; Burgos-Blasco, P.; de Perosanz-Lobo, D.; Suarez-Valle, A.; Cortes-Cuevas, J.L.; Carretero, I.; Garcia-Del Real, C.; Fernandez-Guarino, M. Clinical and histological characterization of vesicular COVID-19 rashes: A prospective study in a tertiary care hospital. Clin. Exp. Dermatol. 2020, 45, 872–875. [Google Scholar] [CrossRef]
- Trellu, L.T.; Kaya, G.; Alberto, C.; Calame, A.; McKee, T.; Calmy, A. Clinicopathologic Aspects of a Papulovesicular Eruption in a Patient With COVID-19. JAMA Dermatol. 2020, 156, 922–924. [Google Scholar] [CrossRef]
- Mahé, A.; Birckel, E.; Merklen, C.; Lefèbvre, P.; Hannedouche, C.; Jost, M.; Droy-Dupré, L. Histology of skin lesions establishes that the vesicular rash associated with COVID-19 is not ‘varicella-like’. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e559–e561. [Google Scholar] [CrossRef]
- Villalon-Gomez, J.M. Pityriasis Rosea: Diagnosis and Treatment. Am. Fam. Physician 2018, 97, 38–44. [Google Scholar] [PubMed]
- Kutlu, Ö.; Metin, A. Relative changes in the pattern of diseases presenting in dermatology outpatient clinic in the era of the COVID-19 pandemic. Dermatol. Ther. 2020, 33, e14096. [Google Scholar] [CrossRef]
- Merhy, R.; Sarkis, A.S.; Stephan, F. Pityriasis rosea as a leading manifestation of COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e246–e247. [Google Scholar] [CrossRef] [PubMed]
- Dursun, R.; Temiz, S.A. The clinics of HHV-6 infection in COVID-19 pandemic: Pityriasis rosea and Kawasaki disease. Dermatol. Ther. 2020, 33, e13730. [Google Scholar] [CrossRef] [PubMed]
- Veraldi, S.; Spigariolo, C.B. Pityriasis rosea and COVID-19. J. Med. Virol. 2021, 93, 4068. [Google Scholar] [CrossRef]
- Martín Enguix, D.; Salazar Nievas, M.D.C.; Martín Romero, D.T. Pityriasis rosea Gibert type rash in an asymptomatic patient that tested positive for COVID-19. Med. Clin. 2020, 155, 273. [Google Scholar] [CrossRef]
- Potekaev, N.N.; Zhukova, O.V.; Protsenko, D.N.; Demina, O.M.; Khlystova, E.A.; Bogin, V. Clinical characteristics of dermatologic manifestations of COVID-19 infection: Case series of 15 patients, review of literature, and proposed etiological classification. Int. J. Dermatol. 2020, 59, 1000–1009. [Google Scholar] [CrossRef]
- Sanchez, A.; Sohier, P.; Benghanem, S.; L’Honneur, A.S.; Rozenberg, F.; Dupin, N.; Garel, B. Digitate Papulosquamous Eruption Associated with Severe Acute Respiratory Syndrome Coronavirus 2 Infection. JAMA Dermatol. 2020, 156, 819–820. [Google Scholar] [CrossRef]
- Drago, F.; Ciccarese, G.; Rebora, A.; Parodi, A. Human herpesvirus-6, -7, and Epstein-Barr virus reactivation in pityriasis rosea during COVID-19. J. Med. Virol. 2021, 93, 1850–1851. [Google Scholar] [CrossRef]
- Welsh, E.; Cardenas-de la Garza, J.A.; Cuellar-Barboza, A.; Franco-Marquez, R.; Arvizu-Rivera, R.I. SARS-CoV-2 spike protein positivity in pityriasis rosea-like and urticaria-like rashes of COVID-19. Br. J. Dermatol. 2021, 184, 1194–1195. [Google Scholar] [CrossRef]
- Perna, A.; Passiatore, M.; Massaro, A.; Terrinoni, A.; Bianchi, L.; Cilli, V.; D’Orio, M.; Proietti, L.; Taccardo, G.; De Vitis, R. Skin manifestations in COVID-19 patients, state of the art. A systematic review. Int. J. Dermatol. 2021, 60, 547–553. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Multisystem Inflammatory Syndrome in Children and Adolescents with COVID-19. Available online: https://www.who.int/publications/i/item/multisystem-inflammatory-syndrome-in-children-and-adolescents-with-covid-19 (accessed on 10 February 2022).
- Lu, X.; Zhang, L.; Du, H.; Zhang, J.; Li, Y.Y.; Qu, J.; Zhang, W.; Wang, Y.; Bao, S.; Li, Y.; et al. SARS-CoV-2 Infection in Children. N. Engl. J. Med. 2020, 382, 1663–1665. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Riphagen, S.; Gomez, X.; Gonzalez-Martinez, C.; Wilkinson, N.; Theocharis, P. Hyperinflammatory shock in children during COVID-19 pandemic. Lancet 2020, 395, 1607–1608. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. Information for Healthcare Providers about Multisystem Inflammatory Syndrome in Children (mis-C). Available online: https://www.cdc.gov/mis/misc/hcp/index.html?CDC_AA_refVal=https%3A%2F%2Fwww.cdc.gov%2Fmis%2Fhcp%2Findex.html (accessed on 10 February 2022).
- Dong, Y.; Mo, X.; Hu, Y.; Qi, X.; Jiang, F.; Jiang, Z.; Tong, S. Epidemiology of COVID-19 among Children in China. Pediatrics 2020, 145, e20200702. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Licciardi, F.; Pruccoli, G.; Denina, M.; Parodi, E.; Taglietto, M.; Rosati, S.; Montin, D. SARS-CoV-2-Induced Kawasaki-Like Hyperinflammatory Syndrome: A Novel COVID Phenotype in Children. Pediatrics 2020, 146, e20201711. [Google Scholar] [CrossRef]
- Godeau, D.; Petit, A.; Richard, I.; Roquelaure, Y.; Descatha, A. An outbreak of severe Kawasaki-like disease at the Italian epicentre of the SARS-CoV-2 epidemic: An observational cohort study. Lancet 2020, 395, 1771–1778. [Google Scholar] [CrossRef]
- Hennon, T.R.; Penque, M.D.; Abdul-Aziz, R.; Alibrahim, O.S.; McGreevy, M.B.; Prout, A.J.; Schaefer, B.A.; Ambrusko, S.J.; Pastore, J.V.; Turkovich, S.J.; et al. COVID-19 associated Multisystem Inflammatory Syndrome in Children (MIS-C) guidelines; a Western New York approach. Prog. Pediatr. Cardiol. 2020, 57, 101232. [Google Scholar] [CrossRef]
- Center for Disease Control and Prevention. Multisystem Inflammatory Syndrome in Children (MIS-C) Associated with Coronavirus Disease 2019 (COVID-19). Available online: https://emergency.cdc.gov/han/2020/han00432.asp (accessed on 10 February 2022).
- Feldstein, L.R.; Rose, E.B.; Horwitz, S.M.; Collins, J.P.; Newhams, M.M.; Son, M.; Newburger, J.W.; Kleinman, L.C.; Heidemann, S.M.; Martin, A.A.; et al. Multisystem Inflammatory Syndrome in U.S. Children and Adolescents. N. Engl. J. Med. 2020, 383, 334–346. [Google Scholar] [CrossRef]
- Brumfiel, C.M.; DiLorenzo, A.M.; Petronic-Rosic, V.M. Dermatologic manifestations of COVID-19-associated multisystem inflammatory syndrome in children. Clin. Dermatol. 2021, 39, 329–333. [Google Scholar] [CrossRef]
- Shakeel, S.; Ahmad Hassali, M.A. Post-COVID-19 Outbreak of Severe Kawasaki-like Multisystem Inflammatory Syndrome in Children. Malays. J. Med. Sci. 2021, 28, 109–116. [Google Scholar] [CrossRef]
- Henderson, L.A.; Canna, S.W.; Friedman, K.G.; Gorelik, M.; Lapidus, S.K.; Bassiri, H.; Behrens, E.M.; Ferris, A.; Kernan, K.F.; Schulert, G.S.; et al. American College of Rheumatology Clinical Guidance for Multisystem Inflammatory Syndrome in Children Associated with SARS-CoV-2 and Hyperinflammation in Pediatric COVID-19: Version 1. Arthritis Rheumatol. 2020, 72, 1791–1805. [Google Scholar] [CrossRef] [PubMed]
- Wollina, U.; Karadağ, A.S.; Rowland-Payne, C.; Chiriac, A.; Lotti, T. Cutaneous signs in COVID-19 patients: A review. Dermatol. Ther. 2020, 33, e13549. [Google Scholar] [CrossRef] [PubMed]
- Sachdeva, M.; Gianotti, R.; Shah, M.; Bradanini, L.; Tosi, D.; Veraldi, S.; Ziv, M.; Leshem, E.; Dodiuk-Gad, R.P. Cutaneous manifestations of COVID-19: Report of three cases and a review of literature. J. Dermatol. Sci. 2020, 98, 75–81. [Google Scholar] [CrossRef] [PubMed]
- Zaladonis, A.; Huang, S.; Hsu, S. COVID toes or pernio? Clin. Dermatol. 2020, 38, 764–767. [Google Scholar] [CrossRef]
- Ladha, M.A.; Luca, N.; Constantinescu, C.; Naert, K.; Ramien, M.L. Approach to Chilblains During the COVID-19 Pandemic. J. Cutan. Med. Surg. 2020, 24, 504–517. [Google Scholar] [CrossRef]
- Rustin, M.H.; Newton, J.A.; Smith, N.P.; Dowd, P.M. The treatment of chilblains with nifedipine: The results of a pilot study, a double-blind placebo-controlled randomized study and a long-term open trial. Br. J. Dermatol. 1989, 120, 267–275. [Google Scholar] [CrossRef]
- Bosch-Amate, X.; Giavedoni, P.; Podlipnik, S.; Andreu-Febrer, C.; Sanz-Beltran, J.; Garcia-Herrera, A.; Alós, L.; Mascaró, J.M. Retiform purpura as a dermatological sign of coronavirus disease 2019 (COVID-19) coagulopathy. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e548–e549. [Google Scholar] [CrossRef]
- Brody, G.; Nguyen, M.O.; Foulad, D.P.; Rojek, N.W. Retiform Purpura in the Setting of COVID-19: A Harbinger of Underlying Coagulopathy and Severe Disease Course. SKIN J. Cutan. Med. 2021, 5, 434–436. [Google Scholar] [CrossRef]
- Shulman, S.T. Pediatric Coronavirus Disease-2019-Associated Multisystem Inflammatory Syndrome. J. Pediatr. Infect. Dis. Soc. 2020, 9, 285–286. [Google Scholar] [CrossRef]
- Cheung, E.W.; Zachariah, P.; Gorelik, M.; Boneparth, A.; Kernie, S.G.; Orange, J.S.; Milner, J.D. Multisystem Inflammatory Syndrome Related to COVID-19 in Previously Healthy Children and Adolescents in New York City. JAMA 2020, 324, 294–296. [Google Scholar] [CrossRef]
- Son, M.; Murray, N.; Friedman, K.; Young, C.C.; Newhams, M.M.; Feldstein, L.R.; Loftis, L.L.; Tarquinio, K.M.; Singh, A.R.; Heidemann, S.M.; et al. Multisystem Inflammatory Syndrome in Children—Initial Therapy and Outcomes. N. Engl. J. Med. 2021, 385, 23–34. [Google Scholar] [CrossRef] [PubMed]
- Bursal Duramaz, B.; Yozgat, C.Y.; Yozgat, Y.; Turel, O. Appearance of skin rash in pediatric patients with COVID-19: Three case presentations. Dermatol. Ther. 2020, 33, e13594. [Google Scholar] [CrossRef] [PubMed]
- Gianotti, R.; Recalcati, S.; Fantini, F.; Riva, C.; Milani, M.; Dainese, E.; Boggio, F. Histopathological Study of a Broad Spectrum of Skin Dermatoses in Patients Affected or Highly Suspected of Infection by COVID-19 in the Northern Part of Italy: Analysis of the Many Faces of the Viral-Induced Skin Diseases in Previous and New Reported Cases. Am. J. Dermatopathol. 2020, 42, 564–570. [Google Scholar] [CrossRef] [PubMed]
- Techasatian, L.; Lebsing, S.; Uppala, R.; Thaowandee, W.; Chaiyarit, J.; Supakunpinyo, C.; Panombualert, S.; Mairiang, D.; Saengnipanthkul, S.; Wichajarn, K.; et al. The Effects of the Face Mask on the Skin Underneath: A Prospective Survey During the COVID-19 Pandemic. J. Prim. Care Community Health 2020, 11, 2150132720966167. [Google Scholar] [CrossRef]
- Desai, S.R.; Kovarik, C.; Brod, B.; James, W.; Fitzgerald, M.E.; Preston, A.; Hruza, G.J. COVID-19 and personal protective equipment: Treatment and prevention of skin conditions related to the occupational use of personal protective equipment. J. Am. Acad. Dermatol. 2020, 83, 675–677. [Google Scholar] [CrossRef]
- Abdali, S.; Yu, J. Occupational Dermatoses Related to Personal Protective Equipment Used During the COVID-19 Pandemic. Dermatol. Clin. 2021, 39, 555–568. [Google Scholar] [CrossRef]
- Schwarz, T.; Kreiselmaier, I.; Bieber, T.; Thaci, D.; Simon, J.C.; Meurer, M.; Werfel, T.; Zuberbier, T.; Luger, T.A.; Wollenberg, A. A randomized, double-blind, vehicle-controlled study of 1% pimecrolimus cream in adult patients with perioral dermatitis. J. Am. Acad. Dermatol. 2008, 59, 34–40. [Google Scholar] [CrossRef]
- Wilkinson, D.S.; Kirton, V.; Wilkinson, J.D. Perioral dermatitis: A 12-year review. Br. J. Dermatol. 1979, 101, 245–257. [Google Scholar] [CrossRef]
- Two, A.M.; Wu, W.; Gallo, R.L.; Hata, T.R. Rosacea: Part I. Introduction, categorization, histology, pathogenesis, and risk factors. J. Am. Acad. Dermatol. 2015, 72, 749–760. [Google Scholar] [CrossRef]
- Park, H.; Del Rosso, J.Q. Use of oral isotretinoin in the management of rosacea. J. Clin. Aesthet. Dermatol. 2011, 4, 54–61. [Google Scholar]
- Smart, H.; Opinion, F.B.; Darwich, I.; Elnawasany, M.A.; Kodange, C. Preventing Facial Pressure Injury for Health Care Providers Adhering to COVID-19 Personal Protective Equipment Requirements. Adv. Skin Wound Care 2020, 33, 418–427. [Google Scholar] [CrossRef] [PubMed]
- Gefen, A.; Ousey, K. Update to device-related pressure ulcers: SECURE prevention. COVID-19, face masks and skin damage. J. Wound Care 2020, 29, 245–259. [Google Scholar] [CrossRef] [PubMed]
- Dowdle, T.S.; Thompson, M.; Alkul, M.; Nguyen, J.M.; Sturgeon, A. COVID-19 and dermatological personal protective equipment considerations. Bayl. Univ. Med Cent. Proc. 2021, 34, 469–472. [Google Scholar] [CrossRef] [PubMed]
- Beiu, C.; Mihai, M.; Popa, L.; Cima, L.; Popescu, M.N. Frequent Hand Washing for COVID-19 Prevention Can Cause Hand Dermatitis: Management Tips. Cureus 2020, 12, e7506. [Google Scholar] [CrossRef] [Green Version]
- Cavanagh, G.; Wambier, C.G. Rational hand hygiene during the coronavirus 2019 (COVID-19) pandemic. J. Am. Acad. Dermatol. 2020, 82, e211. [Google Scholar] [CrossRef]
- Shanshal, M.; Ahmed, H.S.; Asfoor, H.; Salih, R.I.; Ali, S.A.; Aldabouni, Y.K. Impact of COVID-19 on medical practice: A nationwide survey of dermatologists and health care providers in Iraq. Clin. Dermatol. 2021, 39, 500–509. [Google Scholar] [CrossRef]
- Chiriac, A.E.; Wollina, U.; Azoicai, D. Flare-up of Rosacea due to Face Mask in Healthcare Workers during COVID-19. Maedica 2020, 15, 416–417. [Google Scholar] [CrossRef]
- Yin, Z.Q. Covid-19: Countermeasure for N95 mask-induced pressure sore. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e294–e295. [Google Scholar] [CrossRef]
- Rundle, C.W.; Presley, C.L.; Militello, M.; Barber, C.; Powell, D.L.; Jacob, S.E.; Atwater, A.R.; Watsky, K.L.; Yu, J.; Dunnick, C.A. Hand hygiene during COVID-19: Recommendations from the American Contact Dermatitis Society. J. Am. Acad. Dermatol. 2020, 83, 1730–1737. [Google Scholar] [CrossRef]
- U.S. Food and Drug Administration. COVID-19 Vaccines. Available online: https://www.fda.gov/emergency-preparedness-and-response/coronavirus-disease-2019-covid-19/covid-19-vaccines (accessed on 10 February 2022).
- GOV.UK. Decision Conditions of Authorisation for COVID-19 Vaccine AstraZeneca (Regulation 174). Available online: https://www.gov.uk/government/publications/regulatory-approval-of-covid-19-vaccine-astrazeneca (accessed on 10 February 2022).
- Baraniuk, C. COVID-19: What do we know about Sputnik V and other Russian vaccines? BMJ 2021, 372, n743. [Google Scholar] [CrossRef]
- Montano, D. Frequency and Associations of Adverse Reactions of COVID-19 Vaccines Reported to Pharmacovigilance Systems in the European Union and the United States. Front. Public Health 2022, 9, 756633. [Google Scholar] [CrossRef] [PubMed]
- Centers for Disease Control and Prevention. Allergic Reactions Including Anaphylaxis after Receipt of the First Dose of Moderna COVID-19 Vaccine—United States, December 21, 2020–January 10, 2021. Available online: https://www.cdc.gov/mmwr/volumes/70/wr/mm7004e1.htm (accessed on 10 February 2022).
- McLendon, K.; Sternard, B.T. Anaphylaxis. In StatPearls; StatPearls Publishing: Treasure Island, FL, USA, 15 May 2022. [Google Scholar]
- Sobczak, M.; Pawliczak, R. The risk of anaphylaxis behind authorized COVID-19 vaccines: A meta-analysis. Clin. Mol. Allergy 2022, 20, 1. [Google Scholar] [CrossRef] [PubMed]
- Iguchi, T.; Umeda, H.; Kojima, M.; Kanno, Y.; Tanaka, Y.; Kinoshita, N.; Sato, D. Cumulative Adverse Event Reporting of Anaphylaxis After mRNA COVID-19 Vaccine (Pfizer-BioNTech) Injections in Japan: The First-Month Report. Drug Saf. 2021, 44, 1209–1214. [Google Scholar] [CrossRef] [PubMed]
- Cabanillas, B.; Akdis, C.A.; Novak, N. Allergic reactions to the first COVID-19 vaccine: A potential role of polyethylene glycol? Allergy 2021, 76, 1617–1618. [Google Scholar] [CrossRef]
- Garvey, L.H.; Nasser, S. Anaphylaxis to the first COVID-19 vaccine: Is polyethylene glycol (PEG) the culprit? Br. J. Anaesth. 2021, 126, e106–e108. [Google Scholar] [CrossRef]
- Banerji, A.; Wickner, P.G.; Saff, R.; Stone, C.A., Jr.; Robinson, L.B.; Long, A.A.; Wolfson, A.R.; Williams, P.; Khan, D.A.; Phillips, E.; et al. mRNA Vaccines to Prevent COVID-19 Disease and Reported Allergic Reactions: Current Evidence and Suggested Approach. J. Allergy Clin. Immunol. Pract. 2021, 9, 1423–1437. [Google Scholar] [CrossRef]
- Wenande, E.C.; Skov, P.S.; Mosbech, H.; Poulsen, L.K.; Garvey, L.H. Inhibition of polyethylene glycol-induced histamine release by monomeric ethylene and diethylene glycol: A case of probable polyethylene glycol allergy. J. Allergy Clin. Immunol. 2013, 131, 1425–1427. [Google Scholar] [CrossRef]
- Bruusgaard-Mouritsen, M.A.; Johansen, J.D.; Garvey, L.H. Clinical manifestations and impact on daily life of allergy to polyethylene glycol (PEG) in ten patients. Clin. Exp. Allergy 2021, 51, 463–470. [Google Scholar] [CrossRef]
- Sellaturay, P.; Nasser, S.; Ewan, P. Polyethylene Glycol-Induced Systemic Allergic Reactions (Anaphylaxis). J. Allergy Clin. Immunol. Pract. 2021, 9, 670–675. [Google Scholar] [CrossRef]
- Brandt, N.; Garvey, L.H.; Bindslev-Jensen, U.; Kjaer, H.F.; Bindslev-Jensen, C.; Mortz, C.G. Three cases of anaphylaxis following injection of a depot corticosteroid with evidence of IgE sensitization to macrogols rather than the active steroid. Clin. Transl. Allergy 2017, 7, 2. [Google Scholar] [CrossRef] [Green Version]
- Zhou, Z.H.; Stone, C.A., Jr.; Jakubovic, B.; Phillips, E.J.; Sussman, G.; Park, J.; Hoang, U.; Kirshner, S.L.; Levin, R.; Kozlowski, S. Anti-PEG IgE in anaphylaxis associated with polyethylene glycol. J. Allergy Clin. Immunol. Pract. 2021, 9, 1731–1733. [Google Scholar] [CrossRef] [PubMed]
- Kozma, G.T.; Mészáros, T.; Vashegyi, I.; Fülöp, T.; Örfi, E.; Dézsi, L.; Rosivall, L.; Bavli, Y.; Urbanics, R.; Mollnes, T.E. Pseudo-anaphylaxis to Polyethylene Glycol (PEG)-Coated Liposomes: Roles of Anti-PEG IgM and Complement Activation in a Porcine Model of Human Infusion Reactions. ACS Nano 2019, 13, 9315–9324. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tihy, M.; Menzinger, S.; André, R.; Laffitte, E.; Toutous-Trellu, L.; Kaya, G. Clinicopathological features of cutaneous reactions after mRNA-based COVID-19 vaccines. J. Eur. Acad. Dermatol. Venereol. 2021, 35, 2456–2461. [Google Scholar] [CrossRef] [PubMed]
- Kempf, W.; Kettelhack, N.; Kind, F.; Courvoisier, S.; Galambos, J.; Pfaltz, K. ‘COVID arm’—Histological features of a delayed-type hypersensitivity reaction to Moderna mRNA-1273 SARS-CoV2 vaccine. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e730–e732. [Google Scholar] [CrossRef]
- Ramos, C.L.; Kelso, J.M. “COVID Arm”: Very delayed large injection site reactions to mRNA COVID-19 vaccines. J. Allergy Clin. Immunol. Pract. 2021, 9, 2480–2481. [Google Scholar] [CrossRef]
- Lindgren, A.L.; Austin, A.H.; Welsh, K.M. COVID Arm: Delayed Hypersensitivity Reactions to SARS-CoV-2 Vaccines Misdiagnosed as Cellulitis. J Prim Care Community Health. 2021, 12, 21501327211024431. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention. COVID-19 Vaccine Distribution Allocations by Jurisdiction—Pfizer. Available online: https://data.cdc.gov/Vaccinations/COVID-19-Vaccine-Distribution-Allocations-by-Juris/saz5–9hgg (accessed on 10 February 2022).
- Wei, N.; Fishman, M.; Wattenberg, D.; Gordon, M.; Lebwohl, M. “COVID arm”: A reaction to the Moderna vaccine. JAAD Case Rep. 2021, 10, 92–95. [Google Scholar] [CrossRef]
- Kelso, J.M.; Coda, A.B.; Keating, R.M.; Vaccari, D.M. “COVID Toes” After mRNA COVID-19 Vaccines. J. Allergy Clin. Immunol. Pract. 2021, 9, 3196–3197. [Google Scholar] [CrossRef]
- Lesort, C.; Kanitakis, J.; Donzier, L.; Jullien, D. Chilblain-like lesions after BNT162b2 mRNA COVID-19 vaccine: A case report suggesting that ‘COVID toes’ are due to the immune reaction to SARS-CoV-2. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e630–e632. [Google Scholar] [CrossRef]
- Tan, S.W.; Tam, Y.C.; Oh, C.C. Skin manifestations of COVID-19: A worldwide review. JAAD Int. 2021, 2, 119–133. [Google Scholar] [CrossRef]
- Akdaş, E.; İlter, N.; Öğüt, B.; Erdem, Ö. Pityriasis rosea following CoronaVac COVID-19 vaccination: A case report. J. Eur. Acad. Dermatol. Venereol. 2021, 35, e491–e493. [Google Scholar] [CrossRef] [PubMed]
- Burlando, M.; Herzum, A.; Cozzani, E.; Parodi, A. Acute urticarial rash after COVID-19 vaccination containing Polysorbate 80. Clin. Exp. Vaccine Res. 2021, 10, 298–300. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.M.; Tasnim, S.; Sultana, A.; Faizah, F.; Mazumder, H.; Zou, L.; McKyer, E.; Ahmed, H.U.; Ma, P. Epidemiology of mental health problems in COVID-19: A review. F1000Research 2020, 9, 636. [Google Scholar] [CrossRef] [PubMed]
- Chaves, C.; Castellanos, T.; Abrams, M.; Vazquez, C. The impact of economic recessions on depression and individual and social well-being: The case of Spain (2006–2013). Soc. Psychiatry Psychiatr. Epidemiol. 2018, 53, 977–986. [Google Scholar] [CrossRef]
- Tapia Granados, J.A.; Christine, P.J.; Ionides, E.L.; Carnethon, M.R.; Diez Roux, A.V.; Kiefe, C.I.; Schreiner, P.J. Cardiovascular Risk Factors, Depression, and Alcohol Consumption During Joblessness and During Recessions Among Young Adults in CARDIA. Am. J. Epidemiol. 2018, 187, 2339–2345. [Google Scholar] [CrossRef]
- Beaglehole, B.; Mulder, R.T.; Frampton, C.M.; Boden, J.M.; Newton-Howes, G.; Bell, C.J. Psychological distress and psychiatric disorder after natural disasters: Systematic review and meta-analysis. Br. J. Psychiatry. 2018, 213, 716–722. [Google Scholar] [CrossRef] [Green Version]
- Reich, A.; Wójcik-Maciejewicz, A.; Slominski, A.T. Stress and the skin. G. Ital. Dermatol. Venereol. 2010, 145, 213–219. [Google Scholar]
- Ferreira, B.R.; Jafferany, M. Classification of psychodermatological disorders. J. Cosmet. Dermatol. 2021, 20, 1622–1624. [Google Scholar] [CrossRef]
- Lv, S.; Wang, L.; Zou, X.; Wang, Z.; Qu, B.; Lin, W.; Yang, D.A. Case of Acute Telogen Effluvium after SARS-CoV-2 Infection. Clin. Cosmet. Investig. Dermatol. 2021, 14, 385–387. [Google Scholar] [CrossRef]
- Malkud, S. Telogen Effluvium: A Review. J. Clin. Diagn. Res. 2015, 9, WE01–WE3. [Google Scholar] [CrossRef]
- Sharquie, K.E.; Jabbar, R.I. COVID-19 infection is a major cause of acute telogen effluvium. Ir. J. Med. Sci. 2021, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Mieczkowska, K.; Deutsch, A.; Borok, J.; Guzman, A.K.; Fruchter, R.; Patel, P.; Wind, O.; McLellan, B.N.; Mann, R.E.; Halverstam, C.P. Telogen effluvium: A sequela of COVID-19. Int. J. Dermatol. 2021, 60, 122–124. [Google Scholar] [CrossRef] [PubMed]
- Nair, P.A.; Badri, T. Psoriasis; StatPearls Publishing: Treasure Island, FL, USA, 2022. [Google Scholar]
- Cullen, G.; Kroshinsky, D.; Cheifetz, A.S.; Korzenik, J.R. Psoriasis associated with anti-tumour necrosis factor therapy in inflammatory bowel disease: A new series and a review of 120 cases from the literature. Aliment. Pharmacol. Ther. 2011, 34, 1318–1327. [Google Scholar] [CrossRef] [PubMed]
- Pugliese, D.; Guidi, L.; Ferraro, P.M.; Marzo, M.; Felice, C.; Celleno, L.; Landi, R.; Andrisani, G.; Pizzolante, F.; De Vitis, I.; et al. Paradoxical psoriasis in a large cohort of patients with inflammatory bowel disease receiving treatment with anti-TNF alpha: 5-year follow-up study. Aliment. Pharmacol. Ther. 2015, 42, 880–888. [Google Scholar] [CrossRef] [PubMed]
- Eickstaedt, J.B.; Killpack, L.; Tung, J.; Davis, D.; Hand, J.L.; Tollefson, M.M. Psoriasis and Psoriasiform Eruptions in Pediatric Patients with Inflammatory Bowel Disease Treated with Anti-Tumor Necrosis Factor Alpha Agents. Pediatr. Dermatol. 2017, 34, 253–260. [Google Scholar] [CrossRef] [PubMed]
- Ali, E.; Mohamed, A.; Abuodeh, J.; Albuni, M.K.; Al-Mannai, N.; Salameh, S.; Petkar, M.; Habas, E. SARS-CoV-2 and guttate psoriasis: A case report and review of literature. Clin. Case Rep. 2021, 9, e04568. [Google Scholar] [CrossRef]
- Kuang, Y.; Shen, M.; Wang, Q.; Xiao, Y.; Lv, C.; Luo, Y.; Zhu, W.; Chen, X. Association of outdoor activity restriction and income loss with patient-reported outcomes of psoriasis during the COVID-19 pandemic: A web-based survey. J. Am. Acad. Dermatol. 2020, 83, 670–672. [Google Scholar] [CrossRef]
- Breuer, K.; Göldner, F.M.; Jäger, B.; Werfel, T.; Schmid-Ott, G. Chronic stress experience and burnout syndrome have appreciable influence on health-related quality of life in patients with psoriasis. J. Eur. Acad. Dermatol. Venereol. 2015, 29, 1898–1904. [Google Scholar] [CrossRef]
- Guertler, A.; Moellhoff, N.; Schenck, T.L.; Hagen, C.S.; Kendziora, B.; Giunta, R.E.; French, L.E.; Reinholz, M. Onset of occupational hand eczema among healthcare workers during the SARS-CoV-2 pandemic: Comparing a single surgical site with a COVID-19 intensive care unit. Contact Dermat. 2020, 83, 108–114. [Google Scholar] [CrossRef]
- Singh, M.; Pawar, M.; Bothra, A.; Choudhary, N. Overzealous hand hygiene during the COVID 19 pandemic causing an increased incidence of hand eczema among general population. J. Am. Acad. Dermatol. 2020, 83, e37–e41. [Google Scholar] [CrossRef]
- Edison, K.E.; Ward, D.S.; Dyer, J.A.; Lane, W.; Chance, L.; Hicks, L.L. Diagnosis, diagnostic confidence, and management concordance in live-interactive and store-and-forward teledermatology compared to in-person examination. Telemed. E-Health 2008, 14, 889–895. [Google Scholar] [CrossRef] [PubMed]
- Yeboah, C.B.; Harvey, N.; Krishnan, R.; Lipoff, J.B. The Impact of COVID-19 on Teledermatology: A Review. Dermatol. Clin. 2021, 39, 599–608. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.J.; English, J.C., 3rd. Teledermatology: A Review and Update. Am. J. Clin. Dermatol. 2018, 19, 253–260. [Google Scholar] [CrossRef]
- Wang, R.H.; Barbieri, J.S.; Nguyen, H.P.; Stavert, R.; Forman, H.P.; Bolognia, J.L.; Kovarik, C.L.; Group for Research of Policy Dynamics in Dermatology. Clinical effectiveness and cost-effectiveness of teledermatology: Where are we now, and what are the barriers to adoption? J. Am. Acad. Dermatol. 2020, 83, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Oakley, A.M.; Reeves, F.; Bennett, J.; Holmes, S.H.; Wickham, H. Diagnostic value of written referral and/or images for skin lesions. J. Telemed. Telecare 2006, 12, 151–158. [Google Scholar] [CrossRef]
- Ríos-Yuil, J.M. Correlación del Teleateneo con el Ateneo presencial de Dermatología en el diagnóstico de las patologías cutáneas. Actas Dermosifiliogr. 2012, 103, 138–143. [Google Scholar] [CrossRef] [PubMed]
- Vidal-Alaball, J.; Garcia Domingo, J.L.; Garcia Cuyàs, F.; Mendioroz Peña, J.; Flores Mateo, G.; Deniel Rosanas, J.; Sauch Valmaña, G. A cost savings analysis of asynchronous teledermatology compared to face-to-face dermatology in Catalonia. BMC Health Serv. Res. 2018, 18, 650. [Google Scholar] [CrossRef]
- Snoswell, C.L.; Caffery, L.J.; Whitty, J.A.; Soyer, H.P.; Gordon, L.G. Cost-effectiveness of Skin Cancer Referral and Consultation Using Teledermoscopy in Australia. JAMA Dermatol. 2018, 154, 694–700. [Google Scholar] [CrossRef] [Green Version]
- Viola, K.V.; Tolpinrud, W.L.; Gross, C.P.; Kirsner, R.S.; Imaeda, S.; Federman, D.G. Outcomes of referral to dermatology for suspicious lesions: Implications for teledermatology. Arch. Dermatol. 2011, 147, 556–560. [Google Scholar] [CrossRef]
- Ferrándiz, L.; Ojeda-Vila, T.; Corrales, A.; Martín-Gutiérrez, F.J.; Ruíz-de-Casas, A.; Galdeano, R.; Álvarez-Torralba, I.; Sánchez-Ibáñez, F.; Domínguez-Toro, J.M.; Encina, F.; et al. Internet-based skin cancer screening using clinical images alone or in conjunction with dermoscopic images: A randomized teledermoscopy trial. J. Am. Acad. Dermatol. 2017, 76, 676–682. [Google Scholar] [CrossRef]
- Datta, S.K.; Warshaw, E.M.; Edison, K.E.; Kapur, K.; Thottapurathu, L.; Moritz, T.E.; Reda, D.J.; Whited, J.D. Cost and Utility Analysis of a Store-and-Forward Teledermatology Referral System: A Randomized Clinical Trial. JAMA Dermatol. 2015, 151, 1323–1329. [Google Scholar] [CrossRef] [PubMed]
- Mahendran, R.; Goodfield, M.J.; Sheehan-Dare, R.A. An evaluation of the role of a store-and-forward teledermatology system in skin cancer diagnosis and management. Clin. Exp. Dermatol. 2005, 30, 209–214. [Google Scholar] [CrossRef] [PubMed]
- Ferrandiz, L.; Moreno-Ramirez, D.; Nieto-Garcia, A.; Carrasco, R.; Moreno-Alvarez, P.; Galdeano, R.; Bidegain, E.; Rios-Martin, J.J.; Camacho, F.M. Teledermatology-based presurgical management for nonmelanoma skin cancer: A pilot study. Dermatol. Surg. 2007, 33, 1092–1098. [Google Scholar] [CrossRef]
- Conforti, C.; Giuffrida, R.; Dianzani, C.; Di Meo, N.; Zalaudek, I. COVID-19 and psoriasis: Is it time to limit treatment with immunosuppressants? A call for action. Dermatol. Ther. 2020, 33, e13298. [Google Scholar] [CrossRef]
- Conforti, C.; Giuffrida, R.; Dianzani, C.; Di Meo, N.; Zalaudek, I. Biologic therapy for psoriasis during the COVID-19 outbreak: The choice is to weigh risks and benefits. Dermatol. Ther. 2020, 33, e13490. [Google Scholar] [CrossRef] [PubMed]
- Galimberti, F.; McBride, J.; Cronin, M.; Li, Y.; Fox, J.; Abrouk, M.; Herbst, A.; Kirsner, R.S. Evidence-based best practice advice for patients treated with systemic immunosuppressants in relation to COVID-19. Clin. Dermatol. 2020, 38, 775–780. [Google Scholar] [CrossRef]
- Cheng, S.; Zhao, Y.; Wang, F.; Chen, Y.; Kaminga, A.C.; Xu, H. Comorbidities’ potential impacts on severe and non-severe patients with COVID-19: A systematic review and meta-analysis. Medicine 2021, 100, e24971. [Google Scholar] [CrossRef]
- Suchonwanit, P.; Leerunyakul, K.; Kositkuljorn, C. Cutaneous manifestations in COVID-19: Lessons learned from current evidence. J. Am. Acad. Dermatol. 2020, 83, e57–e60. [Google Scholar] [CrossRef]
- Jimenez-Cauhe, J.; Ortega-Quijano, D.; de Perosanz-Lobo, D.; Burgos-Blasco, P.; Vañó-Galván, S.; Fernandez-Guarino, M.; Fernandez-Nieto, D. Enanthem in Patients With COVID-19 and Skin Rash. JAMA Dermatol. 2020, 156, 1134–1136. [Google Scholar] [CrossRef]
- Mercola, J.; Grant, W.B.; Wagner, C.L. Evidence Regarding Vitamin D and Risk of COVID-19 and Its Severity. Nutrients 2020, 12, 3361. [Google Scholar] [CrossRef]
- Entrenas Castillo, M.; Entrenas Costa, L.M.; Vaquero Barrios, J.M.; Alcalá Díaz, J.F.; López Miranda, J.; Bouillon, R.; Quesada Gomez, J.M. Effect of calcifediol treatment and best available therapy versus best available therapy on intensive care unit admission and mortality among patients hospitalized for COVID-19: A pilot randomized clinical study. J. Steroid Biochem. Mol. Biol. 2020, 203, 105751. [Google Scholar] [CrossRef] [PubMed]
- Quesada-Gomez, J.M.; Entrenas-Castillo, M.; Bouillon, R. Vitamin D receptor stimulation to reduce acute respiratory distress syndrome (ARDS) in patients with coronavirus SARS-CoV-2 infections: Revised Ms SBMB 2020_166. J. Steroid Biochem. Mol. Biol. 2020, 202, 105719. [Google Scholar] [CrossRef] [PubMed]
- Nogues, X.; Ovejero, D.; Pineda-Moncusí, M.; Bouillon, R.; Arenas, D.; Pascual, J.; Ribes, A.; Guerri-Fernandez, R.; Villar-Garcia, J.; Rial, A.; et al. Calcifediol Treatment and COVID-19-Related Outcomes. J. Clin. Endocrinol. Metab. 2021, 106, e4017–e4027. [Google Scholar] [CrossRef] [PubMed]
- Uwitonze, A.M.; Razzaque, M.S. Role of Magnesium in Vitamin D Activation and Function. J. Am. Osteopath. Assoc. 2018, 118, 181–189. [Google Scholar] [CrossRef] [Green Version]
- Gallizzi, R.; Sutera, D.; Spagnolo, A.; Bagnato, A.M.; Cannavò, S.P.; Grasso, L.; Guarneri, C.; Nunnari, G.; Mazza, F.; Pajno, G.B. Management of pernio-like cutaneous manifestations in children during the outbreak of COVID-19. Dermatol. Ther. 2020, 33, e14312. [Google Scholar] [CrossRef]
- Mahé, A.; Birckel, E.; Krieger, S.; Merklen, C.; Bottlaender, L. A distinctive skin rash associated with coronavirus disease 2019? J. Eur. Acad. Dermatol. Venereol. 2020, 34, e246–e247. [Google Scholar] [CrossRef] [Green Version]
- Iancu, G.M.; Solomon, A.; Birlutiu, V. Viral exanthema as manifestation of SARS-CoV-2 infection: A case report. Medicine 2020, 99, e21810. [Google Scholar] [CrossRef]
- Abuelgasim, E.; Dona, A.C.M.; Sondh, R.S.; Harky, A. Management of urticaria in COVID-19 patients: A systematic review. Dermatol. Ther. 2021, 34, e14328. [Google Scholar] [CrossRef]
- van Damme, C.; Berlingin, E.; Saussez, S.; Accaputo, O. Acute urticaria with pyrexia as the first manifestations of a COVID-19 infection. J. Eur. Acad. Dermatol. Venereol. 2020, 34, e300–e301. [Google Scholar] [CrossRef]
- McCullough, P.A.; Kelly, R.J.; Ruocco, G.; Lerma, E.; Tumlin, J.; Wheelan, K.R.; Katz, N.; Lepor, N.E.; Vijay, K.; Carter, H.; et al. Pathophysiological Basis and Rationale for Early Outpatient Treatment of SARS-CoV-2 (COVID-19) Infection. Am. J. Med. 2021, 134, 16–22. [Google Scholar] [CrossRef]
- McCullough, P.A.; Alexander, P.E.; Armstrong, R.; Arvinte, C.; Bain, A.F.; Bartlett, R.P.; Berkowitz, R.L.; Berry, A.C.; Borody, T.J.; Brewer, J.H.; et al. Multifaceted highly targeted sequential multidrug treatment of early ambulatory high-risk SARS-CoV-2 infection (COVID-19). Rev. Cardiovasc. Med. 2020, 21, 517–530. [Google Scholar] [CrossRef] [PubMed]
- Abou-Ismail, M.Y.; Diamond, A.; Kapoor, S.; Arafah, Y.; Nayak, L. The hypercoagulable state in COVID-19: Incidence, pathophysiology, and management. Thromb Res. 2020, 194, 101–115. [Google Scholar] [CrossRef]
- Magro, C.; Mulvey, J.J.; Berlin, D.; Nuovo, G.; Salvatore, S.; Harp, J.; Baxter-Stoltzfus, A.; Laurence, J. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl. Res. 2020, 220, 1–13. [Google Scholar] [CrossRef]
- Zhou, B.; She, J.; Wang, Y.; Ma, X. Venous thrombosis and arteriosclerosis obliterans of lower extremities in a very severe patient with 2019 novel coronavirus disease: A case report. J. Thromb. Thrombolysis 2020, 50, 229–232. [Google Scholar] [CrossRef] [PubMed]
- Manalo, I.F.; Smith, M.K.; Cheeley, J.; Jacobs, R. A dermatologic manifestation of COVID-19: Transient livedo reticularis. J. Am. Acad. Dermatol. 2020, 83, 700. [Google Scholar] [CrossRef] [PubMed]
- Risma, K.A.; Edwards, K.M.; Hummell, D.S.; Little, F.F.; Norton, A.E.; Stallings, A.; Wood, R.A.; Milner, J.D. Potential mechanisms of anaphylaxis to COVID-19 mRNA vaccines. J. Allergy Clin. Immunol. 2021, 147, 2075–2082.e2. [Google Scholar] [CrossRef]
- Preissner, K.T.; Fischer, S.; Deindl, E. Extracellular RNA as a Versatile DAMP and Alarm Signal That Influences Leukocyte Recruitment in Inflammation and Infection. Front. Cell Dev. Biol. 2020, 8, 619221. [Google Scholar] [CrossRef]
- Harris, J.M.; Chess, R.B. Effect of pegylation on pharmaceuticals. Nat. Rev. Drug Discov. 2003, 2, 214–221. [Google Scholar] [CrossRef]
| Definition | Examples | |
|---|---|---|
| Psychophysiological dermatoses | Group of skin diseases that are exacerbated by psychological stress |
–Chronic urticaria –Telogen effluvium –Alopecia areata –Psoriasis –Eczema |
| Primary cutaneous psychopathology | Group of skin symptoms of skin-inflicted skin lesion as a result of an underlying psychiatric illness without primary dermatosis |
–Delusional infestations –Factitious disorders –Skin picking |
| Cutaneous sensory disorders | Group of heterogeneous clinical situations that present with disagreeable skin sensations, pain, or negative sensory symptoms |
–Hypoesthesia –Numbness –Allodynia –Stinging –Burning –Itching |
| Dermatoses leading to psychosocial comorbidities | Disfiguring skin conditions that contribute to psychosocial distress |
–Telogen effluvium –Alopecia areata –Psoriasis |
| Obstacles | Examples |
|---|---|
| Difficulty in Diagnosis | Inadequate clinical history, lack of context Inability to palpate lesions Inability to perform complete skin exams Poor image quality Technical difficulties Incorrect clinical photographs Lack of imaging or technique standards Lack of access to prior medication records |
| Compromised Continuity of Care | No continuity and/or longitudinal care Inability to consult patient in person Obstacles in obtaining diagnostic or lab tests Lack of communication with primary care providers Less integration into hospital health systems |
| Policy/Legal Risk | Medico-legal/malpractice risk Security breaches HIPAA * violations ** |
| Services/Costs Reimbursements | Lack of universal payments ** Limited reimbursements: Medicare/Medicaid ** Lack of universal private payer parity Maintenance costs for individual systems |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Pendlebury, G.A.; Oro, P.; Haynes, W.; Merideth, D.; Bartling, S.; Bongiorno, M.A. The Impact of COVID-19 Pandemic on Dermatological Conditions: A Novel, Comprehensive Review. Dermatopathology 2022, 9, 212-243. https://doi.org/10.3390/dermatopathology9030027
Pendlebury GA, Oro P, Haynes W, Merideth D, Bartling S, Bongiorno MA. The Impact of COVID-19 Pandemic on Dermatological Conditions: A Novel, Comprehensive Review. Dermatopathology. 2022; 9(3):212-243. https://doi.org/10.3390/dermatopathology9030027
Chicago/Turabian StylePendlebury, Gehan A., Peter Oro, William Haynes, Drew Merideth, Samantha Bartling, and Michelle A. Bongiorno. 2022. "The Impact of COVID-19 Pandemic on Dermatological Conditions: A Novel, Comprehensive Review" Dermatopathology 9, no. 3: 212-243. https://doi.org/10.3390/dermatopathology9030027
APA StylePendlebury, G. A., Oro, P., Haynes, W., Merideth, D., Bartling, S., & Bongiorno, M. A. (2022). The Impact of COVID-19 Pandemic on Dermatological Conditions: A Novel, Comprehensive Review. Dermatopathology, 9(3), 212-243. https://doi.org/10.3390/dermatopathology9030027






