Prevalence and Screening Tools of Intimate Partner Violence Among Pregnant and Postpartum Women: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Protocol Registration
2.2. Information Sources, Search Strategy, and Study Selection
2.3. Study Selection and Data Extraction
2.4. Quality Assessment
2.5. Data Synthesis
2.6. Statistical Analysis
2.7. Sensitivity Analyses
3. Results
3.1. Literature Search
3.2. Results Categorized by Type of Violence
3.2.1. Physical IPV
3.2.2. Psychological IPV
| Author, Year | Country | Study Period | Study Design | Sample Size | Age in Years (Range or Mean and SD) | Woman Status | People Lost (Attrition Rate) | Setting | Tool Used to Assess the Outcome | Women Victims of Physical Violence (Prevalence) |
|---|---|---|---|---|---|---|---|---|---|---|
| (Abdollahi et al., 2015) | Iran | February–September 2010 | PCS | 1461 | Mean 26.8 ± 5.8 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Physical 14.1% |
| (Abebe Abate et al., 2016) | Ethiopia | April 2014 | CSS | 282 | Mean 27 ± 6.1; range 15–44 | Pre | 17 | Community-based | WHO-WHLEQ | Physical 29.2% |
| (Abujilban et al., 2022) | Jordan | September–December 2014 | CSS | 247 | Mean 27.3 ± 5.9 | Pre and Pue | n.a. | Hospital-based | WHO-WHLEQ | Physical 31.2% |
| (Almeida et al., 2017) | Portugal | February–June 2012 | CSS | 852 | Mean 30.69 ± 5.54; range 18–44 | Pre | 352 | Hospital-based | WHO-WHLEQ | Physical 21.9% |
| (Antoniou & Iatrakis, 2019) | Greece | August–September 2009 | CSS | 546 | Mean 32.95 ± 6.78 | Pre | n.a. | Hospital-based | AAS | Physical injury (face 3.1%, abdomen 1.3%) |
| (Gómez Aristizábal et al., 2022) | Brazil | February 2010 and June 2011 | PCS | 1447 | Mean 26.1 ± 5.4 | Pre | 317 | Primary healthcare center | VAWI | Physical 12.5% |
| (Asiimwe et al., 2022) | Uganda | October 2018–February 2019 | CSS | 100 | Mean 17.8 ± 1.26 | Pre and Pue | n.a. | Hospital-based | VAWI | Physical 32.0% |
| (Atilla et al., 2023) | Turkey | September–October 2021 | CSS | 456 | Mean 26.66 ± 5.45 | Pre | 24 | Hospital-based | IPV During Pregnancy Questionnaire | Physical 6.6% |
| (Avcı et al., 2023) | Turkey | October 2017–August 2018 | CSS | 255 | Mean 28.57 ± 6.17 | Pre | n.a. | Primary healthcare center | DVWDS | Physical 14.6% |
| (Baǧcioǧlu et al., 2014) | Turkey | n.a. | CSS | 317 | Mean 27.4 ± 5.9 | Pre | 2 | Hospital-based | AAS | Physical 5.3% |
| (Bahrami-Vazir et al., 2020) | Iran | 2014 | CSS | 525 | Mean 25.8 ± 5.1 | Pre | 25 | Primary healthcare center | CTS2 | Total IPV 67.0% of which: physical 22.0% |
| (Belay et al., 2019) | Ethiopia | February–August 2017 | CSS | 589 | Mean 25; range 16–45 | Pre | n.a. | Community-based | WHO-WHLEQ | Physical 9.2% |
| (Bernstein et al., 2016) | South Africa | March 2013–April 2014 | CSS | 623 | Median age 28; range 18–44 | Pre | n.a. | Primary healthcare center | VAWI | Physical 15.0% |
| (Bikinesi et al., 2017) | Namibia | n.a. | CSS | 386 | Mean 27.5 ± 6.8 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Physical 3.4% |
| (Boonnate et al., 2015) | Thailand | n.a. | CSS | 230 | Mean 28.98 ± 5.17 | Pre | n.a. | Hospital-based | ISA | Physical 3.5% |
| (L. H. M. de Lima et al., 2016) | Brazil | May 2009–April 2010 | CSS | 359 (179 adolescents, 180 adults) | Adolescents: mean 17.5 ± 1.4; Adults: mean 26.8 ± 5.8 | Pue | 8 | Hospital-based | AAS | Physical 3.3% |
| (Dinmohammadi et al., 2021) | Iran | August 2017 | RCT | 82 (41 intervention, 41 control) | Mean 27.55 ± 5.13 (intervention), 27.26 ± 4.46 (control) | Pre | 8 | Primary healthcare center | CTS2 | Physical before 18.0% → after 7.0% |
| (Elkhateeb et al., 2021) | Egypt | n.a. | CSS | 513 | n.a. | Pre | 37 | Hospital-based | AAS | Physical 30.2% |
| (Farrokh-Eslamlou et al., 2014) | Iran | February–September 2012 | CSS | 313 | Mean 27.9 ± 5.8; range 17–46 | Pre | 37 | Hospital-based | AAS | Physical 10.2% |
| (Fekadu et al., 2018) | Ethiopia | March–May 2016 | CSS | 450 | Mean 27 ± 4.5 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Physical 32.2% |
| (Ferdos et al., 2018) | Bangladesh | July 2015 to April 2016 | CSS | 443 | <20 y 18.5%; 20–24 y 43.9%; 25–35 y 37.6% | Pue | 43 | Hospital-based | CTS | Physical 39.0% |
| (Field et al., 2018) | South Africa | November 2011–August 2012 | MMS | 376, 95 case notes analyzed qualitatively | Age categories: 18–24 years (39%), 25–29 years (30%), >29 years (31%) | Pre | 186 | Hospital-based | CTS2 | Physical 76.0% |
| (Fonseca-Machado et al., 2015) | Brazil | May 2012–May 2013 | CSS | 358 | Mean 25.0 ± 6.3; range 15–43 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Physical 36.5% |
| (Gebrekristos et al., 2023) | South Africa | July 2017–April 2018 | CSS | 90 | Mean 17.5 ± 1.4; range 14–19 | Pre and Pue | 29 | Hospital-based | CTS | Physical 16.7% |
| (Gharacheh et al., 2015) | Iran | July–December 2012 | CSS | 328 | Abused: mean 26.25 ± 4.12); Non-abused: mean 27.14 ± 4.29) | Pue | 13 | Primary healthcare center | AAS | Physical 26.0% |
| (Gul et al., 2013) | Pakistan | April 2010–March 2011 | CSS | 129 | Mean 31.42 ± 7.02; range 15–50 | Pre | n.a. | Hospital-based | AAS | Physical 35.7% |
| (Ilori et al., 2023) | Nigeria | March–September 2019 | CSS | 240 | Mean 30.7 ± 5.5 | Pre | n.a. | Hospital-based | CAS | Physical 39.3% |
| (Islam et al., 2021) | Bangladesh | October 2015–January 2016 | CSS | 426 | Mean 26.28 ± 5.87; range 15–49 | Pue | 27 | Primary healthcare center | WHO-WHLEQ | Physical 35.2% |
| (Iyengar et al., 2021) | United Kingdom | 3 months in 2016 | CSS | 120 | Mean 25.22 ± 4.93 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Physical + sexual 57.0% |
| (Kana et al., 2020) | Nigeria | January 2017–April 2019 | CSS | 293 | Mean 28.8 ± 5.9 in IPV-exposed group, 29.2 ± 5.7 in unexposed group | Pre | 35 | Hospital-based | CTS | Physical 34.1% |
| (Khaironisak et al., 2017) | Malaysia | March–August 2015 | CSS | 1200 | Mean 29.07 ± 5.39 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Physical 12.9% |
| (Khatlani et al., 2023) | Pakistan | February–May 2014 | CCS | 795 women (256 cases with stillbirths, 539 controls with live births) | Mean 29.6 ± 5.9 in stillbirth group; mean 28.7 ± 5.7 in live birth group | Pre | n.a. | Community-based | WHO-WHLEQ | Physical 9.94% |
| (Kita et al., 2017) | Japan | July 2013–July 2014 | PCS | 453 | Mean 32.1 ± 4.9; range 19–46 | Pre | 502 | Hospital-based | WAST-Short | Physical 3.3% |
| (Kita et al., 2016) | Japan | July 2013–July 2014 | PCS | 562 | Mean 32.2 ± 4.9; range 19–46 | Pre | 393 | Hospital-based | ISA | Physical 2.5% |
| (Koirala, 2022) | Nepal | June–September 2020 | CSS | 220 | Mean 30.18 ± 5.70 | Pre | n.a. | Hospital-based | VAWI | Physical 28.6% |
| (Krishnamurti et al., 2021) | USA | January–May 2020 | QI | 959 (552 before shelter-in-place, 407 during shelter-in-place) | n.a. | Pre | n.a. | Mobile app | CDC BRFSS (for physical and sexual IPV), WEB (for psychological IPV) | Physical: before 0.4% (552), during: 0.5% (407) |
| (Lee et al., 2023) | South Korea | 2020–2021 | CSS | 5616 | Range 16–48 | Pre and Pue | 337 | Primary healthcare center | HITS | physical 0.3% |
| (L. da S. Lima et al., 2020) | Brazil | September–October 2018 | CSS | 65 | Mean 23.88; range 15–42 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Physical 18.5% |
| (Luhumyo et al., 2020) | Kenya | April–June 2017 | CSS | 369 | Median age 25 (IQR: 21–31) | Pre | n.a. | Hospital-based | VAWI | Physical 22.8% |
| (Lukasse et al., 2014) | Belgium, Iceland, Denmark, Estonia, Norway, Sweden | March 2008–August 2010 | PCS | 7174 | n.a. | Pre | n.a. | Hospital-based | NorAQ | Physical 2.2% |
| (Mahenge et al., 2013) | Tanzania | December 2011–April 2012 | CSS | 1180 | Mean 29.0; range 17–43 | Pre | 20 | Hospital-based | CTS | Physical 18.0% |
| (S. Martin-de-las-Heras et al., 2019) | Spain | February–June 2010 | PCS | 779 | Mean 29.9 ± 5.6 | Pre | 214 | Hospital-based | ISA | Physical 3.6% |
| (Stella Martin-de-las-Heras et al., 2015) | Spain | n.a. | CSS | 779 | Mean 29.9 ± 5.6 | Pre | 153 | Hospital-based | ISA | Physical 3.6% |
| (McKelvie et al., 2021) | Vanuatu | May–July 2019 | CSS | 188 | Mean 25.7 ± 5.4 | Pre | 4 | Hospital-based | VAWI | Physical 10.6% |
| (Mohamed et al., 2013) | Saudi Arabia | October 2012–February 2013 | CSS | 404 | Mean 31.19 ± 7.36 | Pre | 12 | Primary healthcare center | WAST | Physical 28.0% |
| (Musa et al., 2020) | Ethiopia | November 2018–April 2019 | CSS | 648 | n.a. | Pre | n.a. | Hospital-based | WHO-WHLEQ | Physical 25.93% |
| (Muzrif et al., 2018) | Sri Lanka | April–December 2014 | CSS | 2088 | Mean 29.63 ± 5.57); 53.9% aged 16–30 years, 46.1% aged 31–44 years | Pre | 87 | Hospital-based | AAS | Physical 6.4% |
| (Naghizadeh et al., 2021) | Iran | May–August 2020 | CSS | 250 | Mean 30.57 ± 5.87 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Physical 4.8% |
| (Nhi et al., 2019) | Vietnam | May 2014–August 2015 | PCS | 1274 | Mean 26; range 16–46 | Pre and Pue | 63 | Hospital-based | WHO-WHLEQ | Physical 3.5% |
| (Njoku et al., 2021) | Nigeria | January–March 2017 | CSS | 400 | Mean 30.1 ± 2.47; range 20–45 | Pre | n.a. | Hospital-based | AAS | Physical 44.8% |
| (Okunola et al., 2021) | Nigeria | March 2019 and September 2019 | PCS | 363 | Mean 30 ± 5.3 | Pre | 0 | Hospital-based | Ongoing abuse screen | Physical 3.6% |
| (Omoronyia et al., 2020) | Nigeria | n.a. | CSS | 250 | 29.7 ± 6.1 | Pre | n.a. | Hospital-based | CAS | Physical 26.8% |
| (Priya et al., 2019) | India | December 2013–February 2015 | CSS | 165 | 23.8 ± 3.8 | Pre | n.a. | Community-based | HITS | Physical 60.0% |
| (Pun et al., 2019) | Nepal | June 2015–September 2016 | PCS | 1381 | Age categories: 15–19 (5.6%), 20–24 (42.8%), 25–29 (37.6%), ≥30 (14.0%) | Pre | 623 | Hospital-based | VAWI | Physical 2.5% |
| (Pun et al., 2018) | Nepal | November 2014–November 2015 | CSS | 1011 | Mean 24.4 ± 4.0 | Pre | 28 | Hospital-based | AAS | Physical 4.0%; physical or psychological 6.1% |
| (Rasch et al., 2018) | Tanzania and Vietnam | n.a. | CSS | 2425 (1116 in Tanzania, 1309 in Vietnam) | n.a. | Pre | n.a. | Hospital-based | VAWI | Tanzania: physical 6.0%; Vietnam: physical 3.5% |
| (S. Rees et al., 2017) | Timor-Leste | June 2013–September 2014 | CSS | 1672 | Age groups: <20 years (8.4%), 20–24 (34.0%), 25–29 (34.4%), 30–34 (16.3%), ≥35 (6.8%) | Pre | 2 | Community-based | VAWI | Physical 6.2% |
| (S. J. Rees et al., 2016) | Timor-Leste | May 2014–January 2015 | CSS | 1672 | Age groups: 20 years: 141 (8.4%); 20–24 (34.0%); 25–29 (34.4%); 30–34 (16.3%); ≥35 (6.8%) | Pre | 2 | Hospital-based | WHO-WHLEQ | Physical 6.2% |
| (S. V. O. Ribeiro et al., 2019) | Brazil | 2010–2013 | PCS | 1139 | n.a. | Pre | n.a. | Primary healthcare center | VAWI | Physical 12.1% |
| (M. R. C. Ribeiro et al., 2017) | Brazil | February 2010–June 2011 | CSS | 1446 (São Luís), 1378 (Ribeirão Preto) | n.a. | Pre | 1 | Primary healthcare center | VAWI | Physical 12.4% |
| (Samal & Poornesh, 2022) | India | October–November 2016 | CSS | 200 | Range 19–40 | Pre | n.a. | Hospital-based | AAS | Physical 0.5% |
| (Sánchez et al., 2023) | Brazil | July 2019–September 2021 | CSS | 600 | Mean 27.0 ± 8.58; range 13–47 | Pre and Pue | n.a. | Hospital-based | AAS, WAST, HITS | Physical 2.3% |
| (Sapkota et al., 2021) | Nepal | June–August 2018 | RCT | 140 | Mean 25.3 ± 5.4 | Pre | 3 | Hospital-based | AAS | Physical 12.1% |
| (Shamu et al., 2014) | Zimbabwe | May–September 2011 | CSS | 1951 | n.a. | Pre and Pue | n.a. | Hospital-based | WHO-WHLEQ | Physical 5.8% |
| (Shamu et al., 2013) | Zimbabwe | May–September 2011 | CSS | 2042 | Mean 26 ± 5.71; range 15–48 | Pre | 59 | Primary healthcare center | WHO-WHLEQ | Physical 15.9%; physical and/or sexual 46.2% |
| (Shannon et al., 2016) | USA | August 2005–October 2007 | CSS | 77 | Mean 24.96 ± 3.83 | Pre | n.a. | Hospital-based | NVAWS, CTS2, PMWI | Physical 32.5% |
| (Shrestha et al., 2016) | Nepal | September–November 2015 | CSS | 404 | Mean 25.5 ± 4.3; 43.8% <25 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Physical 3.2% |
| (Silva et al., 2022) | Brazil | August–October 2017 | CSS | 327 | Not explicitly reported; categorized as ≤40 years and >40 years | Pre | n.a. | Hospital-based | VAWI | Physical 7.2% |
| Silva, 2019 (Silva & Leite, 2019) | Brazil | August–October 2017 | CSS | 330 | Not explicitly reported; categorized as 14–19 years and ≥20 years | Pre | n.a. | Hospital-based | VAWI | Physical 7.6% |
| (Sobhani et al., 2018) | Iran | September–December 2014 | CSS | 402 | Mean 28.24 ± 5.91; range 13–44 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Physical 10.2% |
| (Sulaiman et al., 2021) | Nigeria | November 2018–August 2019 | CSS | 403 | Mean 33 ± 4.9 | Pre | 8 | Hospital-based | HITS | Physical 22.1% |
| (Takelle et al., 2023) | Ethiopia | May–June 2022 | CSS | 473 | Mean 28.18 ± 5.28; range 18–41 | Pre | 12 | Hospital-based | WHO-WHLEQ | Physical 4.0% |
| (Utaile et al., 2023) | Ethiopia | July–October 2020 | CSS | 1535 | Mean 26.3 ± 4.7 | Pre | n.a. | Community-based | WHO-WHLEQ | Physical 34.0% |
| (Velasco et al., 2014) | Spain | 2009 | CSS | 779 | Mean 29.9 ± 5.6 | Pre | n.a. | Hospital-based | AAS, ISA | AAS: physical 1.7%; ISA: physical 3.6% |
| (Wangel et al., 2016) | Sweden | March–November 2008 | CSS | 1003 | Age groups: <25 years (11.2%), 25–29 (32%), 30–35 (43.2%), >35 (13.7%) | Pre | 22 | Hospital-based | NorAQ | Physical 14.2% |
| (Watson & Taft, 2013) | Australia | April 2002–March 2004 | CCS | 1726 | n.a. | Pre | 54 | Hospital-based | CAS | Physical 9.9% |
| (Wokoma et al., 2014) | United Kingdom | January 2011–November 2012 | CSS | 507 | TOP group (women requesting termination of pregnancy) mean 24.4, ANC group (antenatal care) mean 28.8 | Pre | 55 | Hospital-based | AAS | Physical: TOP 4.7%, ANC 0.9% |
| (Zapata-Calvente et al., 2022) | Spain | January 2017–March 2019 | CSS | 592 | Mean 31.82 ± 5.61 | Pre | 138 | Primary healthcare center | WAST-Short, AAS | Physical 5.4% |
| (Zheng et al., 2020) | China | July–October 2019 | CSS | 813 | Mean 28.98 ± 4.52 | Pre | n.a. | Community-based | AAS | Physical 0.98% |
| (Zou et al., 2015) | China | October 2006–February 2007 | CSS | 223 (86 in DV group, 137 in non-DV group) | DV group: 27.8 ± 2.7; non-DV group: 27.2 ± 3.0 | Pre | 23 | Primary healthcare center | AAS | Physical + psychological + sexual 2.3% |
| Author, Year | Country | Study Period | Study Design | Sample Size | Age in Years (Range or Mean and SD) | Woman Status | People Lost (Attrition Rate) | Setting | Tool Used to Assess the Outcome | Women Victims of Psychological Violence (Prevalence) |
|---|---|---|---|---|---|---|---|---|---|---|
| (Abebe Abate et al., 2016) | Ethiopia | April 2014 | CSS | 282 | Mean 27 ± 6.1; range 15–44 | Pre | 17 | Community-based | WHO-WHLEQ | Psychological 16.3% |
| (Abujilban et al., 2022) | Jordan | September–December 2014 | CSS | 247 | Mean 27.3 ± 5.9 | Pre and Pue | n.a. | Hospital-based | WHO-WHLEQ | Psychological 66.0% |
| (Almeida et al., 2017) | Portugal | February–June 2012 | CSS | 852 | Mean 30.69 ± 5.54; range 18–44 | Pre | 352 | Hospital-based | WHO-WHLEQ | Psychological 43.2% |
| (Antoniou & Iatrakis, 2019) | Greece | August–September 2009 | CSS | 546 | Mean 32.95 ± 6.78 | Pre | n.a. | Hospital-based | AAS | Psychological 2.8% |
| (Gómez Aristizábal et al., 2022) | Brazil | February 2010 and June 2011 | PCS | 1447 | Mean 26.1 ± 5.4 | Pre | 317 | Primary healthcare center | VAWI | Psychological 48.5% |
| (Atilla et al., 2023) | Turkey | September–October 2021 | CSS | 456 | Mean 26.66 ± 5.45 | Pre | 24 | Hospital-based | IPV During Pregnancy Questionnaire | Psychological 33.3% |
| (Avcı et al., 2023) | Turkey | October 2017–August 2018 | CSS | 255 | Mean 28.57 ± 6.17 | Pre | n.a. | Primary healthcare center | DVWDS | Psychological 38.8% |
| (Bahrami-Vazir et al., 2020) | Iran | 2014 | CSS | 525 | Mean 25.8 ± 5.1 | Pre | 25 | Primary healthcare center | CTS2 | Total IPV 67.0% of which: psychological 58.0% |
| (Belay et al., 2019) | Ethiopia | February–August 2017 | CSS | 589 | Mean 25; range 16–45 | Pre | n.a. | Community-based | WHO-WHLEQ | Psychological 14.6% |
| (Bernstein et al., 2016) | South Africa | March 2013–April 2014 | CSS | 623 | Median age 28; range 18–44 | Pre | n.a. | Primary healthcare center | VAWI | Psychological 15.0% |
| (Bikinesi et al., 2017) | Namibia | n.a. | CSS | 386 | Mean 27.5 ± 6.8 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Psychological 7.0% |
| (Debono et al., 2017) | Malta | October 2014–January 2015 | CSS | 300 | Mean 30.7; range: 18–43 | Pre | 80 | Hospital-based | VAWI | Psychological 15.0% |
| (Dinmohammadi et al., 2021) | Iran | August 2017 | RCT | 82 (41 intervention, 41 control) | Mean 27.55 ± 5.13 (intervention), 27.26 ± 4.46 (control) | Pre | 8 | Primary healthcare center | CTS2 | Psychological before 56.0% → after 36.0% |
| (Elkhateeb et al., 2021) | Egypt | n.a. | CSS | 513 | n.a. | Pre | 37 | Hospital-based | AAS | Psychological 45.4% |
| (Farrokh-Eslamlou et al., 2014) | Iran | February–September 2012 | CSS | 313 | Mean 27.9 ± 5.8; range 17–46 | Pre | 37 | Hospital-based | AAS | Psychological 43.5% |
| (Fekadu et al., 2018) | Ethiopia | March–May 2016 | CSS | 450 | Mean 27 ± 4.5 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Psychological 57.8% |
| (Field et al., 2018) | South Africa | November 2011–August 2012 | MMS | 376, 95 case notes analyzed qualitatively | Age categories: 18–24 years (39%), 25–29 years (30%), >29 years (31%) | Pre | 186 | Hospital-based | CTS2 | Psychological 81.0% |
| (Fonseca-Machado et al., 2015) | Brazil | May 2012–May 2013 | CSS | 358 | Mean 25.0 ± 6.3; range 15–43 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Psychological 95.2% |
| (Gebrekristos et al., 2023) | South Africa | July 2017–April 2018 | CSS | 90 | Mean 17.5 ± 1.4; range 14–19 | Pre and Pue | 29 | Hospital-based | CTS | Psychological 36.7% |
| (Gharacheh et al., 2015) | Iran | July–December 2012 | CSS | 328 | Abused: mean 26.25 ± 4.12); Non-abused: mean 27.14 ± 4.29) | Pue | 13 | Primary healthcare center | AAS | Psychological 88.4% |
| (Gul et al., 2013) | Pakistan | April 2010–March 2011 | CSS | 129 | Mean 31.42 ± 7.02; range 15–50 | Pre | n.a. | Hospital-based | AAS | Psychological 46.5% |
| (Ilori et al., 2023) | Nigeria | March–September 2019 | CSS | 240 | Mean 30.7 ± 5.5 | Pre | n.a. | Hospital-based | CAS | Psychological 40.2% |
| (Islam et al., 2021) | Bangladesh | October 2015–January 2016 | CSS | 426 | Mean 26.28 ± 5.87; range 15–49 | Pue | 27 | Primary healthcare center | WHO-WHLEQ | Psychological 65.0% |
| (Iyengar et al., 2021) | United Kingdom | 3 months in 2016 | CSS | 120 | Mean 25.22 ± 4.93 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Psychological 43.0% |
| (Kana et al., 2020) | Nigeria | January 2017–April 2019 | CSS | 293 | Mean 28.8 ± 5.9 in IPV-exposed group, 29.2 ± 5.7 in unexposed group | Pre | 35 | Hospital-based | CTS | Psychological 51.2% |
| (Khaironisak et al., 2017) | Malaysia | March–August 2015 | CSS | 1200 | Mean 29.07 ± 5.39 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Psychological 29.8% |
| (Khatlani et al., 2023) | Pakistan | February–May 2014 | CCS | 795 women (256 cases with stillbirths, 539 controls with live births) | Mean 29.6 ± 5.9 in stillbirth group; mean 28.7 ± 5.7 in live birth group | Pre | n.a. | Community-based | WHO-WHLEQ | Psychological 38.87% |
| (Koirala, 2022) | Nepal | June–September 2020 | CSS | 220 | Mean 30.18 ± 5.70 | Pre | n.a. | Hospital-based | VAWI | Psychological 30.9% |
| (Krishnamurti et al., 2021) | USA | January–May 2020 | QI | 959 (552 before shelter-in-place, 407 during shelter-in-place) | n.a. | Pre | n.a. | Mobile app | CDC BRFSS (for physical and sexual IPV), WEB (for psychological IPV) | Psychological before 1.0% (552), during 0.7% (407) |
| (Lee et al., 2023) | South Korea | 2020–2021 | CSS | 5616 | Range 16–48 | Pre and Pue | 337 | Primary healthcare center | HITS | Psychological 3.4% |
| (L. da S. Lima et al., 2020) | Brazil | September–October 2018 | CSS | 65 | Mean 23.88; range 15–42 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Psychological 40.0% |
| (Luhumyo et al., 2020) | Kenya | April–June 2017 | CSS | 369 | Median age 25 (IQR: 21–31) | Pre | n.a. | Hospital-based | VAWI | Psychological 27.4% |
| (Lukasse et al., 2014) | Belgium, Iceland, Denmark, Estonia, Norway, Sweden | March 2008–August 2010 | PCS | 7174 | n.a. | Pre | n.a. | Hospital-based | NorAQ | Psychological 2.7% |
| (S. Martin-de-las-Heras et al., 2019) | Spain | February–June 2010 | PCS | 779 | Mean 29.9 ± 5.6 | Pre | 214 | Hospital-based | ISA | Psychological 21.0% |
| (Stella Martin-de-las-Heras et al., 2015) | Spain | n.a. | CSS | 779 | Mean 29.9 ± 5.6 | Pre | 153 | Hospital-based | ISA | Psychological 21.0% |
| (McKelvie et al., 2021) | Vanuatu | May–July 2019 | CSS | 188 | Mean 25.7 ± 5.4 | Pre | 4 | Hospital-based | VAWI | Psychological 39.1% |
| (Mohamed et al., 2013) | Saudi Arabia | October 2012–February 2013 | CSS | 404 | Mean 31.19 ± 7.36 | Pre | 12 | Primary healthcare center | WAST | Psychological 39% |
| (Musa et al., 2020) | Ethiopia | November 2018–April 2019 | CSS | 648 | n.a. | Pre | n.a. | Hospital-based | WHO-WHLEQ | Psychological 25.62% |
| (Naghizadeh et al., 2021) | Iran | May–August 2020 | CSS | 250 | Mean 30.57 ± 5.87 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Psychological 32.8% |
| (Nhi et al., 2019) | Vietnam | May 2014–August 2015 | PCS | 1274 | Mean 26; range 16–46 | Pre and Pue | 63 | Hospital-based | WHO-WHLEQ | Psychological 32.3% |
| (Njoku et al., 2021) | Nigeria | January–March 2017 | CSS | 400 | Mean 30.1 ± 2.47; range 20–45 | Pre | n.a. | Hospital-based | AAS | Psychological 34.3% |
| (Okunola et al., 2021) | Nigeria | March 2019 and September 2019 | PCS | 363 | Mean 30 ± 5.3 | Pre | 0 | Hospital-based | Ongoing abuse screen | Psychological 3.9% |
| (Omoronyia et al., 2020) | Nigeria | n.a. | CSS | 250 | 29.7 ± 6.1 | Pre | n.a. | Hospital-based | CAS | Psychological 51.2%; psychological + sexual 10.8% |
| (Pun et al., 2019) | Nepal | June 2015–September 2016 | PCS | 1381 | Age categories: 15–19 (5.6%), 20–24 (42.8%), 25–29 (37.6%), ≥30 (14.0%) | Pre | 623 | Hospital-based | VAWI | Psychological 5.2% |
| (Pun et al., 2018) | Nepal | November 2014–November 2015 | CSS | 1011 | Mean 24.4 ± 4.0 | Pre | 28 | Hospital-based | AAS | Psychological or physical 6.1% |
| (Rasch et al., 2018) | Tanzania and Vietnam | n.a. | CSS | 2425 (1116 in Tanzania, 1309 in Vietnam) | n.a. | Pre | n.a. | Hospital-based | VAWI | Tanzania: psychological 22.8%; Vietnam: psychological 32.2% |
| (S. Rees et al., 2017) | Timor-Leste | June 2013–September 2014 | CSS | 1672 | Age groups: <20 years (8.4%), 20–24 (34.0%), 25–29 (34.4%), 30–34 (16.3%), ≥35 (6.8%) | Pre | 2 | Community-based | VAWI | Psychological 30.6% |
| (S. J. Rees et al., 2016) | Timor-Leste | May 2014–January 2015 | CSS | 1672 | Age groups: 20 years 141 (8.4%); 20–24 (34.0%); 25–29 (34.4%); 30–34 (16.3%); ≥35 (6.8%) | Pre | 2 | Hospital-based | WHO-WHLEQ | Psychological 30.6% |
| (S. V. O. Ribeiro et al., 2019) | Brazil | 2010–2013 | PCS | 1139 | n.a. | Pre | n.a. | Primary healthcare center | VAWI | Psychological 47.3% |
| (M. R. C. Ribeiro et al., 2017) | Brazil | February 2010–June 2011 | CSS | 1446 (São Luís), 1378 (Ribeirão Preto) | n.a. | Pre | 1 | Primary healthcare center | VAWI | Psychological 48.4% |
| (Samal & Poornesh, 2022) | India | October–November 2016 | CSS | 200 | Range 19–40 | Pre | n.a. | Hospital-based | AAS | Psychological 1.0% |
| (Shamu et al., 2014) | Zimbabwe | May–September 2011 | CSS | 1951 | n.a. | Pre and Pue | n.a. | Hospital-based | WHO-WHLEQ | Psychological 18.0% |
| (Shamu et al., 2013) | Zimbabwe | May–September 2011 | CSS | 2042 | Mean 26 ± 5.71; range 15–48 | Pre | 59 | Primary healthcare center | WHO-WHLEQ | Psychological 44.0% |
| (Shannon et al., 2016) | USA | August 2005–October 2007 | CSS | 77 | Mean 24.96 ± 3.83 | Pre | n.a. | Hospital-based | NVAWS, CTS2, PMWI | Psychological 71.4% |
| (Shrestha et al., 2016) | Nepal | September–November 2015 | CSS | 404 | Mean 25.5 ± 4.3; 43.8% <25 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Psychological 16.6% |
| (Silva et al., 2022) | Brazil | August–October 2017 | CSS | 327 | Not explicitly reported; categorized as ≤40 years and >40 years | Pre | n.a. | Hospital-based | VAWI | Psychological 16.8% |
| (Silva & Leite, 2019) | Brazil | August–October 2017 | CSS | 330 | Not explicitly reported; categorized as 14–19 years and ≥20 years | Pre | n.a. | Hospital-based | VAWI | Psychological 16.1% |
| (Sobhani et al., 2018) | Iran | September–December 2014 | CSS | 402 | Mean 28.24 ± 5.91; range 13–44 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Psychological 45.5% |
| (Takelle et al., 2023) | Ethiopia | May–June 2022 | CSS | 473 | Mean 28.18 ± 5.28; range 18–41 | Pre | 12 | Hospital-based | WHO-WHLEQ | Psychological 6.3% |
| (Utaile et al., 2023) | Ethiopia | July–October 2020 | CSS | 1535 | Mean 26.3 ± 4.7 | Pre | n.a. | Community-based | WHO-WHLEQ | Psychological 34.6% |
| (Velasco et al., 2014) | Spain | 2009 | CSS | 779 | Mean 29.9 ± 5.6 | Pre | n.a. | Hospital-based | AAS, ISA | AAS: psychological 4.8%; ISA: psychological 21.0% |
| (Watson & Taft, 2013) | Australia | April 2002–March 2004 | CCS | 1726 | n.a. | Pre | 54 | Hospital-based | CAS | Psychological 12.8% |
| (Wokoma et al., 2014) | United Kingdom | January 2011–November 2012 | CSS | 507 | TOP group (women requesting termination of pregnancy) mean 24.4, ANC group (antenatal care) mean 28.8 | Pre | 55 | Hospital-based | AAS | Psychological: TOP 9.9%, ANC 1.8% |
| (Zapata-Calvente et al., 2022) | Spain | January 2017–March 2019 | CSS | 592 | Mean 31.82 ± 5.61 | Pre | 138 | Primary healthcare center | WAST-Short, AAS | Psychological 19.3% |
| (Zheng et al., 2020) | China | July–October 2019 | CSS | 813 | Mean 28.98 ± 4.52 | Pre | n.a. | Community-based | AAS | Psychological 11.07% |
| (Zou et al., 2015) | China | October 2006–February 2007 | CSS | 223 (86 in DV group, 137 in non-DV group) | DV group: 27.8 ± 2.7; non-DV group: 27.2 ± 3.0 | Pre | 23 | Primary healthcare center | AAS | Psychological 63.9%; psychological + sexual 33.7%; psychological + sexual + physical 2.3% |
3.2.3. Sexual IPV
| Author, Year | Country | Study Period | Study Design | Sample Size | Age in Years (Range or Mean and SD) | Woman Status | People Lost (Attrition Rate) | Setting | Tool Used to Assess the Outcome | Women Victims of Sexual Violence (Prevalence) |
|---|---|---|---|---|---|---|---|---|---|---|
| (Abebe Abate et al., 2016) | Ethiopia | April 2014 | CSS | 282 | Mean 27 ± 6.1; range 15–44 | Pre | 17 | Community-based | WHO-WHLEQ | Sexual 30.2% |
| (Abujilban et al., 2022) | Jordan | September–December 2014 | CSS | 247 | Mean 27.3 ± 5.9 | Pre and Pue | n.a. | Hospital-based | WHO-WHLEQ | Sexual 8.9% |
| (Almeida et al., 2017) | Portugal | February–June 2012 | CSS | 852 | Mean 30.69 ± 5.54; range 18–44 | Pre | 352 | Hospital-based | WHO-WHLEQ | Sexual 19.6% |
| (Antoniou & Iatrakis, 2019) | Greece | August–September 2009 | CSS | 546 | Mean 32.95 ± 6.78 | Pre | n.a. | Hospital-based | AAS | Sexual 1.9% |
| (Asiimwe et al., 2022) | Uganda | October 2018–February 2019 | CSS | 100 | Mean 17.8 ± 1.26) | Pre and Pue | n.a. | Hospital-based | VAWI | Sexual 45.0% |
| (Atilla et al., 2023) | Turkey | September–October 2021 | CSS | 456 | Mean 26.66 ± 5.45 | Pre | 24 | Hospital-based | IPV During Pregnancy Questionnaire | Sexual 5.7% |
| (Avcı et al., 2023) | Turkey | October 2017–August 2018 | CSS | 255 | Mean 28.57 ± 6.17 | Pre | n.a. | Primary healthcare center | DVWDS | Sexual 7.4% |
| (Baǧcioǧlu et al., 2014) | Turkey | n.a. | CSS | 317 | Mean 27.4 ± 5.9 | Pre | 2 | Hospital-based | AAS | Sexual 5.0% |
| (Bahrami-Vazir et al., 2020) | Iran | 2014 | CSS | 525 | Mean 25.8 ± 5.1 | Pre | 25 | Primary healthcare center | CTS2 | Total IPV 67.0%, of which sexual 30.0% |
| (Belay et al., 2019) | Ethiopia | February–August 2017 | CSS | 589 | Mean 25; range 16–45 | Pre | n.a. | Community-based | WHO-WHLEQ | Sexual 9.5% |
| (Bernstein et al., 2016) | South Africa | March 2013–April 2014 | CSS | 623 | Median age 28; range 18–44 | Pre | n.a. | Primary healthcare center | VAWI | Sexual 2.0% |
| (Bikinesi et al., 2017) | Namibia | n.a. | CSS | 386 | Mean 27.5 ± 6.8 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Sexual 1.6% |
| (L. H. M. de Lima et al., 2016) | Brazil | May 2009–April 2010 | CSS | 359 (179 adolescents, 180 adults) | Adolescents: mean 17.5 ± 1.4; Adults: mean 26.8 ± 5.8 | Pue | 8 | Hospital-based | AAS | Sexual 1.1% |
| (Dinmohammadi et al., 2021) | Iran | August 2017 | RCT | 82 (41 intervention, 41 control) | Mean 27.55 ± 5.13 (intervention), 27.26 ± 4.46 (control) | Pre | 8 | Primary healthcare center | CTS2 | Sexual before 27.0% → after 15.0% |
| (Elkhateeb et al., 2021) | Egypt | n.a. | CSS | 513 | n.a. | Pre | 37 | Hospital-based | AAS | Sexual 20.0% |
| (Farrokh-Eslamlou et al., 2014) | Iran | February–September 2012 | CSS | 313 | Mean 27.9 ± 5.8; range 17–46 | Pre | 37 | Hospital-based | AAS | Sexual 17.2% |
| (Fekadu et al., 2018) | Ethiopia | March–May 2016 | CSS | 450 | Mean 27 ± 4.5 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Sexual 7.6% |
| (Ferdos et al., 2018) | Bangladesh | July 2015 to April 2016 | CSS | 443 | <20 y 18.5%; 20–24 y 43.9%; 25–35 y 37.6% | Pue | 43 | Hospital-based | CTS | Sexual 26.3% |
| (Field et al., 2018) | South Africa | November 2011–August 2012 | MMS | 376, 95 case notes analyzed qualitatively | Age categories: 18–24 years (39%), 25–29 years (30%), >29 years (31%) | Pre | 186 | Hospital-based | CTS2 | Sexual 26.0% |
| (Fonseca-Machado et al., 2015) | Brazil | May 2012–May 2013 | CSS | 358 | Mean 25.0 ± 6.3; range 15–43 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Sexual 1.6% |
| (Gharacheh et al., 2015) | Iran | July–December 2012 | CSS | 328 | Abused: mean 26.25 ± 4.12); Non-abused: mean 27.14 ± 4.29) | Pue | 13 | Primary healthcare center | AAS | Sexual 34.9% |
| (Gul et al., 2013) | Pakistan | April 2010–March 2011 | CSS | 129 | Mean 31.42 ± 7.02; range 15–50 | Pre | n.a. | Hospital-based | AAS | Sexual 20.4% |
| (Ilori et al., 2023) | Nigeria | March–September 2019 | CSS | 240 | Mean 30.7 ± 5.5 | Pre | n.a. | Hospital-based | CAS | Sexual 38.1% |
| (Islam et al., 2021) | Bangladesh | October 2015–January 2016 | CSS | 426 | Mean 26.28 ± 5.87; range 15–49 | Pue | 27 | Primary healthcare center | WHO-WHLEQ | Sexual 18.5% |
| (Iyengar et al., 2021) | United Kingdom | 3 months in 2016 | CSS | 120 | Mean 25.22 ± 4.93 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Sexual + physical 57.0% |
| (Kana et al., 2020) | Nigeria | January 2017–April 2019 | CSS | 293 | Mean 28.8 ± 5.9 in IPV-exposed group, 29.2 ± 5.7 in unexposed group | Pre | 35 | Hospital-based | CTS | Sexual 30.7% |
| (Khaironisak et al., 2017) | Malaysia | March–August 2015 | CSS | 1200 | Mean 29.07 ± 5.39 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Sexual 9.8% |
| (Khatlani et al., 2023) | Pakistan | February–May 2014 | CCS | 795 women (256 cases with stillbirths, 539 controls with live births) | Mean 29.6 ± 5.9 in stillbirth group; mean 28.7 ± 5.7 in live birth group | Pre | n.a. | Community-based | WHO-WHLEQ | Sexual 9.81% |
| (Koirala, 2022) | Nepal | June–September 2020 | CSS | 220 | Mean 30.18 ± 5.70 | Pre | n.a. | Hospital-based | VAWI | Sexual 22.7% |
| (Krishnamurti et al., 2021) | USA | January–May 2020 | QI | 959 (552 before shelter-in-place, 407 during shelter-in-place) | n.a. | Pre | n.a. | Mobile app | CDC BRFSS (for physical and sexual IPV), WEB (for psychological IPV) | Sexual before 0.4% (552), during: 0.2% (407) |
| (L. da S. Lima et al., 2020) | Brazil | September–October 2018 | CSS | 65 | Mean 23.88; range 15–42 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Sexual 3.1% |
| (Luhumyo et al., 2020) | Kenya | April–June 2017 | CSS | 369 | Median age 25 (IQR: 21–31) | Pre | n.a. | Hospital-based | VAWI | Sexual 13.0% |
| (Lukasse et al., 2014) | Belgium, Iceland, Denmark, Estonia, Norway, Sweden | March 2008–August 2010 | PCS | 7174 | n.a. | Pre | n.a. | Hospital-based | NorAQ | Sexual 0.4% |
| (Mahenge et al., 2013) | Tanzania | December 2011–April 2012 | CSS | 1180 | Mean 29.0; range 17–43 | Pre | 20 | Hospital-based | CTS | Sexual 20.0% |
| (McKelvie et al., 2021) | Vanuatu | May–July 2019 | CSS | 188 | Mean 25.7 ± 5.4 | Pre | 4 | Hospital-based | VAWI | Sexual 7.4% |
| (Mohamed et al., 2013) | Saudi Arabia | October 2012–February 2013 | CSS | 404 | Mean 31.19 ± 7.36 | Pre | 12 | Primary healthcare center | WAST | Sexual 14.0% |
| (Musa et al., 2020) | Ethiopia | November 2018–April 2019 | CSS | 648 | n.a. | Pre | n.a. | Hospital-based | WHO-WHLEQ | Sexual 3.7% |
| (Naghizadeh et al., 2021) | Iran | May–August 2020 | CSS | 250 | Mean 30.57 ± 5.87 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Sexual 12.4% |
| (Nhi et al., 2019) | Vietnam | May 2014–August 2015 | PCS | 1274 | Mean 26; range 16–46 | Pre and Pue | 63 | Hospital-based | WHO-WHLEQ | Sexual 9.8% |
| (Njoku et al., 2021) | Nigeria | January–March 2017 | CSS | 400 | Mean 30.1 ± 2.47; range 20–45 | Pre | n.a. | Hospital-based | AAS | Sexual 7.3%% |
| (Okunola et al., 2021) | Nigeria | March 2019 and September 2019 | PCS | 363 | Mean 30 ± 5.3 | Pre | 0 | Hospital-based | Ongoing abuse screen | Sexual 3.6% |
| (Omoronyia et al., 2020) | Nigeria | n.a. | CSS | 250 | 29.7 ± 6.1 | Pre | n.a. | Hospital-based | CAS | Sexual 29.2%; psychological + sexual 10.8% |
| (Pun et al., 2019) | Nepal | June 2015–September 2016 | PCS | 1381 | Age categories: 15–19 (5.6%), 20–24 (42.8%), 25–29 (37.6%), ≥30 (14.0%) | Pre | 623 | Hospital-based | VAWI | Sexual 0.9% |
| (Pun et al., 2018) | Nepal | November 2014–November 2015 | CSS | 1011 | Mean 24.4 ± 4.0 | Pre | 28 | Hospital-based | AAS | Sexual 1.6% |
| (Rasch et al., 2018) | Tanzania and Vietnam | n.a. | CSS | 2425 (1116 in Tanzania, 1309 in Vietnam) | n.a. | Pre | n.a. | Hospital-based | VAWI | Tanzania: sexual 15.4%; Vietnam: sexual 9.9% |
| (M. R. C. Ribeiro et al., 2017) | Brazil | February 2010–June 2011 | CSS | 1446 (São Luís), 1378 (Ribeirão Preto) | n.a. | Pre | 1 | Primary healthcare center | VAWI | Sexual 2.8% |
| (Samal & Poornesh, 2022) | India | October–November 2016 | CSS | 200 | Range 19–40 | Pre | n.a. | Hospital-based | AAS | Sexual 0% |
| (Sapkota et al., 2021) | Nepal | June–August 2018 | RCT | 140 | Mean 25.3 ± 5.4 | Pre | 3 | Hospital-based | AAS | Sexual 15.0% |
| (Shamu et al., 2014) | Zimbabwe | May–September 2011 | CSS | 1951 | n.a. | Pre and Pue | n.a. | Hospital-based | WHO-WHLEQ | Sexual 22.6% |
| (Shamu et al., 2013) | Zimbabwe | May–September 2011 | CSS | 2042 | Mean 26 ± 5.71; range 15–48 | Pre | 59 | Primary healthcare center | WHO-WHLEQ | Sexual 38.9%; sexual and/or physical 46.2% |
| (Shannon et al., 2016) | USA | August 2005–October 2007 | CSS | 77 | Mean 24.96 ± 3.83 | Pre | n.a. | Hospital-based | NVAWS, CTS2, PMWI | Sexual 14.3% |
| (Shrestha et al., 2016) | Nepal | September–November 2015 | CSS | 404 | Mean 25.5 ± 4.3; 43.8% <25 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Sexual 17.3% |
| (Silva et al., 2022) | Brazil | August–October 2017 | CSS | 327 | Not explicitly reported; categorized as ≤40 years and >40 years | Pre | n.a. | Hospital-based | VAWI | Sexual 3.08% |
| (Silva & Leite, 2019) | Brazil | August–October 2017 | CSS | 330 | Not explicitly reported; categorized as 14–19 years and ≥20 years | Pre | n.a. | Hospital-based | VAWI | Sexual 2.7% |
| (Sobhani et al., 2018) | Iran | September–December 2014 | CSS | 402 | Mean 28.24 ± 5.91; range 13–44 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Sexual 16.7% |
| (Takelle et al., 2023) | Ethiopia | May–June 2022 | CSS | 473 | Mean 28.18 ± 5.28; range 18–41 | Pre | 12 | Hospital-based | WHO-WHLEQ | Sexual 3.2% |
| (Utaile et al., 2023) | Ethiopia | July–October 2020 | CSS | 1535 | Mean 26.3 ± 4.7 | Pre | n.a. | Community-based | WHO-WHLEQ | Sexual 19.3% |
| (Velasco et al., 2014) | Spain | 2009 | CSS | 779 | Mean 29.9 ± 5.6 | Pre | n.a. | Hospital-based | AAS, ISA | AAS sexual 0.5% |
| (Wangel et al., 2016) | Sweden | March–November 2008 | CSS | 1003 | Age groups: <25 years (11.2%), 25–29 (32%), 30–35 (43.2%), >35 (13.7%) | Pre | 22 | Hospital-based | NorAQ | Sexual 15.5% |
| (Watson & Taft, 2013) | Australia | April 2002–March 2004 | CCS | 1726 | n.a. | Pre | 54 | Hospital-based | CAS | Sexual 5.1% |
| (Zapata-Calvente et al., 2022) | Spain | January 2017–March 2019 | CSS | 592 | Mean 31.82 ± 5.61 | Pre | 138 | Primary healthcare center | WAST-Short, AAS | Sexual 2.4% |
| (Zheng et al., 2020) | China | July–October 2019 | CSS | 813 | Mean 28.98 ± 4.52 | Pre | n.a. | Community-based | AAS | Sexual 0.86% |
| (Zou et al., 2015) | China | October 2006–February 2007 | CSS | 223 (86 in DV group, 137 in non-DV group) | DV group: 27.8 ± 2.7; non-DV group: 27.2 ± 3.0 | Pre | 23 | Primary healthcare center | AAS | Sexual + psychological 33.7%; Sexual + physical + psychological 2.3% |
3.2.4. Any IPV
| Author, Year | Country | Study Period | Study Design | Sample Size | Age in Years (Range or Mean and SD) | Woman Status | People Lost (Attrition Rate) | Setting | Tool Used to Assess the Outcome | Women Victims of any IPV (Prevalence) |
|---|---|---|---|---|---|---|---|---|---|---|
| (Abebe Abate et al., 2016) | Ethiopia | April 2014 | CSS | 282 | Mean 27 ± 6.1; range 15–44 | Pre | 17 | Community-based | WHO-WHLEQ | Any IPV 44.5% |
| (Abujilban et al., 2022) | Jordan | September–December 2014 | CSS | 247 | Mean 27.3 ± 5.9 | Pre and Pue | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 93.1% |
| (Alhalal et al., 2022) | Saudi Arabia | December 2019–March 2020 | CSS | 684 | Mean 31.19 ± 7.36 | Pre and Pue | 66 | Hospital-based | CAS | Any IPV 28.9% |
| (Alhusen et al., 2015) | USA | February 2009–March 2010 | CSS | 166 | Mean 23.3 ± 5.4 | Pre | n.a. | Hospital-based | AAS | Any IPV 19.3% |
| (Almeida et al., 2017) | Portugal | February–June 2012 | CSS | 852 | Mean 30.69 ± 5.54; range 18–44 | Pre | 352 | Hospital-based | WHO-WHLEQ | Any IPV 43.4% |
| (Andreasen et al., 2023) | Denmark, Spain | 2021–2022 | PCS | Total 16,068 (Denmark 14,013, Spain 2055) | Mean Denmark: 28.7 ± 5.1; Spain: 31.6 ± 5.9 | Pre | 77 | Hospital-based | AAS | Any IPV 9.62%: Denmark 8.53%; Spain 17.03% |
| (Antoniou & Iatrakis, 2019) | Greece | August–September 2009 | CSS | 546 | Mean 32.95 ± 6.78 | Pre | n.a. | Hospital-based | AAS | Any IPV 6.0% |
| (Gómez Aristizábal et al., 2022) | Brazil | February 2010 and June 2011 | PCS | 1447 | Mean 26.1 ± 5.4 | Pre | 317 | Primary healthcare center | VAWI | Any IPV 49.7% |
| (Atilla et al., 2023) | Turkey | September–October 2021 | CSS | 456 | Mean 26.66 ± 5.45 | Pre | 24 | Hospital-based | IPV During Pregnancy Questionnaire | Any IPV 44.1% |
| (Avcı et al., 2023) | Turkey | October 2017–August 2018 | CSS | 255 | Mean 28.57 ± 6.17 | Pre | n.a. | Primary healthcare center | DVWDS | Any IPV 9.8% |
| (Baǧcioǧlu et al., 2014) | Turkey | n.a. | CSS | 317 | Mean 27.4 ± 5.9 | Pre | 2 | Hospital-based | AAS | Any IPV 10.3% |
| (Belay et al., 2019) | Ethiopia | February–August 2017 | CSS | 589 | Mean 25; range 16–45 | Pre | n.a. | Community-based | WHO-WHLEQ | Any IPV 21.2% |
| (Bernstein et al., 2016) | South Africa | March 2013–April 2014 | CSS | 623 | Median age 28; range 18–44 | Pre | n.a. | Primary healthcare center | VAWI | Any IPV 21% |
| (Bikinesi et al., 2017) | Namibia | n.a. | CSS | 386 | Mean 27.5 ± 6.8 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Any IPV 8.0% |
| (Boonnate et al., 2015) | Thailand | n.a. | CSS | 230 | Mean 28.98 ± 5.17 | Pre | n.a. | Hospital-based | ISA | Any IPV 11.7% |
| (Caprara et al., 2020) | Brazil | 2011–2016 | PCS | 232 | Mean 27.4 ± 6.7 | Pue | n.a. | Hospital-based | AAS | Any IPV 15.1% |
| (Chen et al., 2017) | USA | January 2003–December 2009 | RCS | 1438 | Mean 26.0 (victims: 27.1; non-victims: 25.9) | Pre | n.a. | Hospital-based | HITS | Any IPV 7.5% |
| (Dinmohammadi et al., 2021) | Iran | August 2017 | RCT | 82 (41 intervention, 41 control) | Mean 27.55 ± 5.13 (intervention), 27.26 ± 4.46 (control) | Pre | 8 | Primary healthcare center | CTS2 | Any IPV before 59.0% → after 38.0% |
| (Elkhateeb et al., 2021) | Egypt | n.a. | CSS | 513 | n.a. | Pre | 37 | Hospital-based | AAS | Any IPV 50.8% |
| (Farrokh-Eslamlou et al., 2014) | Iran | February–September 2012 | CSS | 313 | Mean 27.9 ± 5.8; range 17–46 | Pre | 37 | Hospital-based | AAS | Any IPV 55.9% |
| (Fekadu et al., 2018) | Ethiopia | March–May 2016 | CSS | 450 | Mean 27 ± 4.5 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 58.7% |
| (Field et al., 2018) | South Africa | November 2011–August 2012 | MMS | 376, 95 case notes analyzed qualitatively | Age categories: 18–24 years (39%), 25–29 years (30%), >29 years (31%) | Pre | 186 | Hospital-based | CTS2 | Any IPV 15.0% |
| (Fisher et al., 2013) | Vietnam | December 2009–June 2011 | PCS | 417 (pregnancy), 453 (postpartum) | Mean 26.1 ± 4.8 | Pre and Pue | 80 | Community-based | WHO-WHLEQ | Any IPV 3.8% (pregnancy); any IPV 5.9% (postpartum) |
| (Fonseca-Machado et al., 2015) | Brazil | May 2012–May 2013 | CSS | 358 | Mean 25.0 ± 6.3; range 15–43 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 17.6% |
| (Gashaw et al., 2019) | Ethiopia | November 2015–March 2016 | CSS | 720 | Mean 25 ± 5.0 | Pre | n.a. | Hospital-based | AAS | Any IPV 44.0% |
| (Gebrekristos et al., 2023) | South Africa | July 2017–April 2018 | CSS | 90 | Mean 17.5 ± 1.4; range 14–19 | Pre and Pue | 29 | Hospital-based | CTS | Any IPV 40.0% |
| (Gelaye et al., 2016) | Peru | February 2012–March 2014 | CSS | 2970 | Mean 28.1 ± 6.3; range 18–35 | Pre | 89 | Hospital-based | WHO-WHLEQ | Any IPV 36.7% |
| (Gharacheh et al., 2015) | Iran | July–December 2012 | CSS | 328 | Abused: mean 26.25 ± 4.12); non-abused: mean 27.14 ± 4.29) | Pue | 13 | Primary healthcare center | AAS | Any IPV 44.5% |
| (Hooker & Taft, 2021) | Australia | 2011 | CSS | 2621 | Mean 34.0 | Pue | n.a. | Primary healthcare center | CAS | Any IPV 6.8% |
| (Ilori et al., 2023) | Nigeria | March–September 2019 | CSS | 240 | Mean 30.7 ± 5.5 | Pre | n.a. | Hospital-based | CAS | Any IPV 45.8% |
| (Iyengar et al., 2021) | United Kingdom | 3 months in 2016 | CSS | 120 | Mean 25.22 ± 4.93 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 35.0% |
| (Kana et al., 2020) | Nigeria | January 2017–April 2019 | CSS | 293 | Mean 28.8 ± 5.9 in IPV-exposed group, 29.2 ± 5.7 in unexposed group | Pre | 35 | Hospital-based | CTS | Any IPV 66.6% |
| (Kataoka & Imazeki, 2018) | Japan | September–December 2011 | QUAL | 43 | Age categories: <20 years (2.3%), 20–29 (32.6%), ≥30 (65.1%) | Pue | 5 | Hospital-based | VAWS | Any IPV 18.6% |
| (Khaironisak et al., 2017) | Malaysia | March–August 2015 | CSS | 1200 | Mean 29.07 ± 5.39 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 35.9% |
| (Kian et al., 2019) | Iran | 2015–2016 | CSS | 400 (200 rural, 200 urban) | Mean 29.15 ± 5.37 (urban), 28.25 ± 6.3 (rural) | Pre and Pue | n.a. | Primary healthcare center | Standardized violence questionnaire | Any IPV: rural 40.56%; urban 37.25% |
| (Kita et al., 2017) | Japan | July 2013–July 2014 | PCS | 453 | Mean 32.1 ± 4.9; range 19–46 | Pre | 502 | Hospital-based | WAST-Short | Any IPV 12.1% |
| (Koirala, 2022) | Nepal | June–September 2020 | CSS | 220 | Mean 30.18 ± 5.70 | Pre | n.a. | Hospital-based | VAWI | Any IPV 32.7% |
| (Lee et al., 2023) | South Korea | 2020–2021 | CSS | 5616 | Range 16–48 | Pre and Pue | 337 | Primary healthcare center | HITS | Any IPV 7.6% |
| (Luhumyo et al., 2020) | Kenya | April–June 2017 | CSS | 369 | Median age 25 (IQR: 21–31) | Pre | n.a. | Hospital-based | VAWI | Any IPV 34.1% |
| (Mahenge et al., 2013) | Tanzania | December 2011–April 2012 | CSS | 1180 | Mean 29.0; range 17–43 | Pre | 20 | Hospital-based | CTS | Any IPV 27.0% |
| (Stella Martin-de-las-Heras et al., 2015) | Spain | n.a. | CSS | 779 | Mean 29.9 ± 5.6 | Pre | 153 | Hospital-based | ISA | Any IPV 21.3% |
| (McKelvie et al., 2021) | Vanuatu | May–July 2019 | CSS | 188 | Mean 25.7 ± 5.4 | Pre | 4 | Hospital-based | VAWI | Any IPV 44.68% |
| (Mohamed et al., 2013) | Saudi Arabia | October 2012–February 2013 | CSS | 404 | Mean 31.19 ± 7.36 | Pre | 12 | Primary healthcare center | WAST | Any IPV 52.0% |
| (Musa et al., 2020) | Ethiopia | November 2018–April 2019 | CSS | 648 | n.a. | Pre | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 39.81% |
| (Naghizadeh et al., 2021) | Iran | May–August 2020 | CSS | 250 | Mean 30.57 ± 5.87 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 35.2% |
| (Nhi et al., 2019) | Vietnam | May 2014–August 2015 | PCS | 1274 | Mean 26; range 16–46 | Pre and Pue | 63 | Hospital-based | WHO-WHLEQ | Any IPV 35.3% |
| (Njoku et al., 2021) | Nigeria | January–March 2017 | CSS | 400 | Mean 30.1 ± 2.47; range 20–45 | Pre | n.a. | Hospital-based | AAS | Any IPV 43.0% |
| (Nongrum et al., 2014) | India | Not reported | PCS | 150 | Mean 26.32 ± 4.22 | Pre | 18 | Hospital-based | AAS | Any IPV 7.3% |
| (Okunola et al., 2021) | Nigeria | March 2019 and September 2019 | PCS | 363 | Mean 30 ± 5.3 | Pre | 0 | Hospital-based | Ongoing abuse screen | Any IPV 15.4% |
| (Omoronyia et al., 2020) | Nigeria | n.a. | CSS | 250 | 29.7 ± 6.1 | Pre | n.a. | Hospital-based | CAS | Any IPV 54.8% |
| (Priya et al., 2019) | India | December 2013–February 2015 | CSS | 165 | 23.8 ± 3.8 | Pre | n.a. | Community-based | HITS | Any IPV 23.0% |
| (Pun et al., 2019) | Nepal | June 2015–September 2016 | PCS | 1381 | Age categories: 15–19 (5.6%), 20–24 (42.8%), 25–29 (37.6%), ≥30 (14.0%) | Pre | 623 | Hospital-based | VAWI | Any IPV 20.5% |
| (Pun et al., 2018) | Nepal | November 2014–November 2015 | CSS | 1011 | Mean 24.4 ± 4.0 | Pre | 28 | Hospital-based | AAS | Any IPV 23.7% |
| (Rasch et al., 2018) | Tanzania and Vietnam | n.a. | CSS | 2425 (1116 in Tanzania, 1309 in Vietnam) | n.a. | Pre | n.a. | Hospital-based | VAWI | Tanzania: any IPV 30.2%; Vietnam: any IPV 35.2% |
| (M. R. C. Ribeiro et al., 2017) | Brazil | February 2010–June 2011 | CSS | 1446 (São Luís), 1378 (Ribeirão Preto) | n.a. | Pre | 1 | Primary healthcare center | VAWI | Any IPV 49.6% |
| (Rishal et al., 2020) | Nepal | August 2014–November 2016 | PCS | 1010 screened, 181 reported IPV | n.a. | Pre | 119 | Hospital-based | AAS | Any IPV 17.9%; at follow-up: no longer IPV 48.3%; still IPV 51.7% |
| (Samal & Poornesh, 2022) | India | October–November 2016 | CSS | 200 | Range 19–40 | Pre | n.a. | Hospital-based | AAS | Any IPV 6.5% |
| (Sánchez et al., 2023) | Brazil | July 2019–September 2021 | CSS | 600 | Mean 27.0 ± 8.58; range 13–47 | Pre and Pue | n.a. | Hospital-based | AAS, WAST, HITS | WAST: Any IPV 6.7%; HITS: Any IPV 3.5% |
| (Shamu et al., 2014) | Zimbabwe | May–September 2011 | CSS | 1951 | n.a. | Pre and Pue | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 32.8% |
| (Shamu et al., 2013) | Zimbabwe | May–September 2011 | CSS | 2042 | Mean 26 ± 5.71; range 15–48 | Pre | 59 | Primary healthcare center | WHO-WHLEQ | Any IPV 63.1% |
| (Shannon et al., 2016) | USA | August 2005–October 2007 | CSS | 77 | Mean 24.96 ± 3.83 | Pre | n.a. | Hospital-based | NVAWS, CTS2, PMWI | Any IPV 75.3% |
| (Shrestha et al., 2016) | Nepal | September–November 2015 | CSS | 404 | Mean 25.5 ± 4.3; 43.8% <25 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 27.2% |
| (Sobhani et al., 2018) | Iran | September–December 2014 | CSS | 402 | Mean 28.24 ± 5.91; range 13–44 | Pre | n.a. | Hospital-based | WHO-WHLEQ | Any IPV 48.5% |
| (Sulaiman et al., 2021) | Nigeria | November 2018–August 2019 | CSS | 403 | Mean 33 ± 4.9 | Pre | 8 | Hospital-based | HITS | Any IPV 56.3% |
| (Sussmann et al., 2020) | Brazil | January 2006–March 2007 | CSS | 700 | Age categories: 16–20 years, 21–30 years, >31 years | Pue | 128 | Community-based | VAWI | Any IPV 24.7% |
| (Suzuki et al., 2018) | Japan | April–October 2016 | CSS | 470 | n.a. | Pre | 2 | Hospital-based | VAWS | Any IPV 4.1% |
| (Utaile et al., 2023) | Ethiopia | July–October 2020 | CSS | 1535 | Mean 26.3 ± 4.7 | Pre | n.a. | Community-based | WHO-WHLEQ | Any IPV 48.0% |
| (Velasco et al., 2014) | Spain | 2009 | CSS | 779 | Mean 29.9 ± 5.6 | Pre | n.a. | Hospital-based | AAS, ISA | AAS: Any IPV 7.7%; ISA: Any IPV 21.0% |
| (Watson & Taft, 2013) | Australia | April 2002–March 2004 | CCS | 1726 | n.a. | Pre | 54 | Hospital-based | CAS | Any IPV 14.9% |
| (Zapata-Calvente et al., 2022) | Spain | January 2017–March 2019 | CSS | 592 | Mean 31.82 ± 5.61 | Pre | 138 | Primary healthcare center | WAST-Short, AAS | Any IPV 9.5% |
| (Zheng et al., 2020) | China | July–October 2019 | CSS | 813 | Mean 28.98 ± 4.52 | Pre | n.a. | Community-based | AAS | Any IPV 15.62% |
3.2.5. Verbal IPV
3.2.6. Economic IPV
| Author, Year | Country | Study Period | Study Design | Sample Size | Age in Years (Range or Mean and SD) | Woman Status | People Lost (Attrition Rate) | Setting | Tool Used to Assess the Outcome | Women Victims of Verbal Violence (Prevalence) |
|---|---|---|---|---|---|---|---|---|---|---|
| (Baǧcioǧlu et al., 2014) | Turkey | n.a. | CSS | 317 | Mean 27.4 ± 5.9 | Pre | 2 | Hospital-based | AAS | Verbal 4.4% |
| (Debono et al., 2017) | Malta | October 2014–January 2015 | CSS | 300 | Mean 30.7; range: 18–43 | Pre | 80 | Hospital-based | VAWI | Verbal 12.0% |
| (Elkhateeb et al., 2021) | Egypt | n.a. | CSS | 513 | n.a. | Pre | 37 | Hospital-based | AAS | Verbal 41.7% |
| (Gul et al., 2013) | Pakistan | April 2010–March 2011 | CSS | 129 | Mean 31.42 ± 7.02; range 15–50 | Pre | n.a. | Hospital-based | AAS | Verbal 51.9% |
| (Lee et al., 2023) | South Korea | 2020–2021 | CSS | 5616 | Range 16–48 | Pre and Pue | 337 | Primary healthcare center | HITS | Verbal 0.3% |
| (Njoku et al., 2021) | Nigeria | January–March 2017 | CSS | 400 | Mean 30.1 ± 2.47; range 20–45 | Pre | n.a. | Hospital-based | AAS | Verbal 85.5% |
| (Samal & Poornesh, 2022) | India | October–November 2016 | CSS | 200 | Range 19–40 | Pre | n.a. | Hospital-based | AAS | Verbal 3.0% |
| (Sulaiman et al., 2021) | Nigeria | November 2018–August 2019 | CSS | 403 | Mean 33 ± 4.9 | Pre | 8 | Hospital-based | HITS | Verbal 38.4% |
| Author, Year | Country | Study Period | Study Design | Sample Size | Age in Years (Range or Mean and SD) | Woman Status | People Lost (Attrition Rate) | Setting | Tool Used to Assess the Outcome | Women Victims of Economic Violence (Prevalence) |
|---|---|---|---|---|---|---|---|---|---|---|
| (Atilla et al., 2023) | Turkey | September–October 2021 | CSS | 456 | Mean 26.66 ± 5.45 | Pre | 24 | Hospital-based | IPV During Pregnancy Questionnaire | Economic 28.9% |
| (Avcı et al., 2023) | Turkey | October 2017–August 2018 | CSS | 255 | Mean 28.57 ± 6.17 | Pre | n.a. | Primary healthcare center | DVWDS | Economic 8.2% |
| (Baǧcioǧlu et al., 2014) | Turkey | n.a. | CSS | 317 | Mean 27.4 ± 5.9 | Pre | 2 | Hospital-based | AAS | Economic 6.6% |
| (Bikinesi et al., 2017) | Namibia | n.a. | CSS | 386 | Mean 27.5 ± 6.8 | Pre | n.a. | Primary healthcare center | WHO-WHLEQ | Economic 5.2% |
| (Gul et al., 2013) | Pakistan | April 2010–March 2011 | CSS | 129 | Mean 31.42 ± 7.02; range 15–50 | Pre | n.a. | Hospital-based | AAS | Economic 33.3% |
| (Njoku et al., 2021) | Nigeria | January–March 2017 | CSS | 400 | Mean 30.1 ± 2.47; range 20–45 | Pre | n.a. | Hospital-based | AAS | Economic 48.3% |
| (Samal & Poornesh, 2022) | India | October–November 2016 | CSS | 200 | Range 19–40 | Pre | n.a. | Hospital-based | AAS | Economic 2.0% |
3.2.7. Non-Physical Violence
| Author, Year | Country | Study Period | Study Design | Sample Size | Age in Years (Range or Mean and SD) | Woman Status | People Lost (Attrition Rate) | Setting | Tool Used to Assess the Outcome | Women Victims of Violence (Prevalence) |
|---|---|---|---|---|---|---|---|---|---|---|
| (Boonnate et al., 2015) | Thailand | n.a. | CSS | 230 | Mean 28.98 ± 5.17 | Pre | n.a. | Hospital-based | ISA | Non-physical 4.3% |
| (Kita et al., 2017) | Japan | July 2013–July 2014 | PCS | 453 | Mean 32.1 ± 4.9; range 19–46 | Pre | 502 | Hospital-based | WAST-Short | Non-physical 3.1% |
| (Kita et al., 2016) | Japan | July 2013–July 2014 | PCS | 562 | Mean 32.2 ± 4.9; range 19–46 | Pre | 393 | Hospital-based | ISA | Non-physical 3.6% |
3.3. Sensitivity Analyses by WHO Region and Income Level
3.4. Quality Assessment
4. Discussion
4.1. Interpretation of the Main Results
4.2. Implications for Policies and Practices
4.3. Future Directions
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Abdollahi, F., Abhari, F. R., Delavar, M. A., & Charati, J. Y. (2015). Physical violence against pregnant women by an intimate partner, and adverse pregnancy outcomes in Mazandaran Province, Iran. Journal of Family & Community Medicine, 22(1), 13–18. [Google Scholar] [CrossRef]
- Abebe Abate, B., Admassu Wossen, B., & Tilahun Degfie, T. (2016). Determinants of intimate partner violence during pregnancy among married women in Abay Chomen district, Western Ethiopia: A community based cross sectional study. BMC Women’s Health, 16, 16. [Google Scholar] [CrossRef]
- Abujilban, S., Mrayan, L., & Damra, J. K. (2022). Intimate partner violence among Jordanian pregnant women and its predictors. Nursing Open, 9(1), 267–276. [Google Scholar] [CrossRef]
- Alhalal, H., Alhalal, E., Alhaizan, M., Alghuson, L., Alahmari, M., Alkhayyal, N., & Akkour, K. (2022). Intimate partner violence and its associations with adverse pregnancy outcomes in Saudi Arabia: A cross-sectional study. Journal of Interpersonal Violence, 37(15–16), NP14457–NP14484. [Google Scholar] [CrossRef]
- Alhusen, J. L., Frohman, N., & Purcell, G. (2015). Intimate partner violence and suicidal ideation in pregnant women. Archives of Women’s Mental Health, 18(4), 573–578. [Google Scholar] [CrossRef]
- Almeida, F. S. J., Coutinho, E. C., Duarte, J. C., Chaves, C. M. B., Nelas, P. A. B., Amaral, O. P., & Parreira, V. C. (2017). Domestic violence in pregnancy: Prevalence and characteristics of the pregnant woman. Journal of Clinical Nursing, 26(15–16), 2417–2425. [Google Scholar] [CrossRef]
- Andreasen, K., Zapata-Calvente, A. L., Martín-de-Las-Heras, S., Bueno-Cavanillas, A., Schei, B., Dokkedahl, S., de León de León, S., Fernandez Lopez, R., Oviedo-Gutiérrez, A., Ankerstjerne, L. B. S., Megías, J. L., Khan, K. S., Rasch, V., & Linde, D. S. (2023). Video consultations and safety App targeting pregnant women exposed to intimate partner violence in Denmark and Spain: Nested cohort intervention study (STOP study). JMIR Formative Research, 7, e38563. [Google Scholar] [CrossRef] [PubMed]
- Antoniou, E., & Iatrakis, G. (2019). Domestic violence during pregnancy in Greece. International Journal of Environmental Research and Public Health, 16(21), 4222. [Google Scholar] [CrossRef] [PubMed]
- Asiimwe, R., Tseng, C. F., Murray, S. M., Ojuka, J. C., Arima, E. G., & Familiar-Lopez, I. (2022). Association of pregnancy-related stigma and intimate partner violence with anxiety and depression among adolescents. Journal of Adolescence, 94(2), 270–275. [Google Scholar] [CrossRef] [PubMed]
- Atilla, R., Yavuz, A., & Kocaöz, S. (2023). Exposure of pregnant women to intimate partner violence during the Pandemic in Turkey and influencing factors. Journal of Community Health Nursing, 40(1), 1–13. [Google Scholar] [CrossRef]
- Avcı, S., Ortabag, T., Ulusal, H., & Taysi, S. (2023). The effect of domestic violence during pregnancy on cortisol hormone release, breastfeeding, and Newborn. Journal of Interpersonal Violence, 38(1–2), NP905–NP930. [Google Scholar] [CrossRef]
- Baǧcioǧlu, E., Vural, M., Karababa, I. F., Akşin, M., & Selek, S. (2014). Decrease in domestic violence during pregnancy: A study from Turkey. Journal of Interpersonal Violence, 29(2), 203–216. [Google Scholar] [CrossRef] [PubMed]
- Bahrami-Vazir, E., Mohammad-Alizadeh-Charandabi, S., Ghelichkhani, F., Mohammadi, A., & Mirghafourvand, M. (2020). Intimate partner abuse among couples during pregnancy and its predictors as reported by pregnant women visiting governmental health care centres in Tabriz, Iran. Journal of Biosocial Science, 52(3), 400–411. [Google Scholar] [CrossRef] [PubMed]
- Belay, S., Astatkie, A., Emmelin, M., & Hinderaker, S. G. (2019). Intimate partner violence and maternal depression during pregnancy: A community-based cross-sectional study in Ethiopia. PLoS ONE, 14(7), e0220003. [Google Scholar] [CrossRef]
- Berg, A. (2016). The importance of the first 1000 days of life. Journal of Child and Adolescent Mental Health, 28(2), iii–vi. [Google Scholar] [CrossRef]
- Bernstein, M., Phillips, T., Zerbe, A., McIntyre, J. A., Brittain, K., Petro, G., Abrams, E. J., & Myer, L. (2016). Intimate partner violence experienced by HIV-infected pregnant women in South Africa: A cross-sectional study. BMJ Open, 6(8), e011999. [Google Scholar] [CrossRef]
- Bikinesi, L. T., Mash, R., & Joyner, K. (2017). Prevalence of intimate partner violence and associated factors amongst women attending antenatal care at Outapi clinic, Namibia: A descriptive survey. African Journal of Primary Health Care and Family Medicine, 9(1). [Google Scholar] [CrossRef] [PubMed]
- Boddy, J., Harris, C., O’Leary, P., Hohenhaus, M., Bond, C., Panagiotaros, C., & Holdsworth, L. (2024). Intersections of intimate partner violence and natural disasters: A systematic review of the quantitative evidence. Trauma, Violence & Abuse, 25(4), 3131–3148. [Google Scholar] [CrossRef]
- Boonnate, N., Tiansawad, S., Chareonsanti, J., & Thungjaroenkul, P. (2015). Factors predicting intimate partner violence during pregnancy among Thai Pregnant Women. Pacific Rim International Journal of Nursing Research, 19, 218–231. [Google Scholar]
- Brunelli, L., Bussolaro, S., Dobrina, R., De Vita, C., Mazzolini, E., Verardi, G., Degrassi, M., Piazza, M., Cassone, A., Starec, A., Ricci, G., Zanchiello, S., & Stampalija, T. (2023). Exploring the needs and expectations of expectant and new parents for an mHealth application to support the first 1000 days of life: Steps toward a co-design approach. International Journal of Environmental Research and Public Health, 20(2), 1227. [Google Scholar] [CrossRef]
- Caprara, G. L., Bernardi, J. R., Bosa, V. L., Da Silva, C. H., & Goldani, M. Z. (2020). Does domestic violence during pregnancy influence the beginning of complementary feeding? BMC Pregnancy and Childbirth, 20(1), 447. [Google Scholar] [CrossRef] [PubMed]
- Chen, P. H., Rovi, S., Vega, M. L., Barrett, T., Pan, K. Y., & Johnson, M. S. (2017). Birth outcomes in relation to intimate partner violence. Journal of the National Medical Association, 109(4), 238–245. [Google Scholar] [CrossRef]
- Debono, C., Borg Xuereb, R., Scerri, J., & Camilleri, L. (2017). Intimate partner violence: Psychological and verbal abuse during pregnancy. Journal of Clinical Nursing, 26(15–16), 2426–2438. [Google Scholar] [CrossRef] [PubMed]
- de Lima, L. H. M., Mattar, R., & Abrahão, A. R. (2016). Domestic violence in pregnant women: A study conducted in the postpartum period of adolescents and adults. Journal of Interpersonal Violence, 34(6), 1183–1197. [Google Scholar] [CrossRef]
- Dinmohammadi, S., Dadashi, M., Ahmadnia, E., Janani, L., & Kharaghani, R. (2021). The effect of solution-focused counseling on violence rate and quality of life of pregnant women at risk of domestic violence: A randomized controlled trial. BMC Pregnancy and Childbirth, 21(1), 221. [Google Scholar] [CrossRef]
- Draper, C. E., Yousafzai, A. K., McCoy, D. C., Cuartas, J., Obradović, J., Bhopal, S., Fisher, J., Jeong, J., Klingberg, S., Milner, K., Pisani, L., Roy, A., Seiden, J., Sudfeld, C. R., Wrottesley, S. V., Fink, G., Nores, M., Tremblay, M. S., & Okely, A. D. (2024). The next 1000 days: Building on early investments for the health and development of young children. The Lancet, 404(10467), 2094–2116. [Google Scholar] [CrossRef]
- Egger, M., Davey Smith, G., Schneider, M., & Minder, C. (1997). Bias in meta-analysis detected by a simple, graphical test. BMJ (Clinical Research Ed.), 315(7109), 629–634. [Google Scholar] [CrossRef]
- Elkhateeb, R., Abdelmeged, A., Ahmad, S., Mahran, A., Abdelzaher, W. Y., Welson, N. N., Al-Zahrani, Y., Alhuwaydi, A. M., & Bahaa, H. A. (2021). Impact of domestic violence against pregnant women in Minia governorate, Egypt: A cross sectional study. BMC Pregnancy and Childbirth, 21(1), 535. [Google Scholar] [CrossRef]
- Farrokh-Eslamlou, H., Sima, O., & Negar, H. (2014). Intimate partner violence during pregnancy in Urmia, Iran in 2012. Journal of Forensic and Legal Medicine, 24, 28–32. [Google Scholar] [CrossRef]
- Fekadu, E., Yigzaw, G., Gelaye, K. A., Ayele, T. A., Minwuye, T., Geneta, T., & Teshome, D. F. (2018). Prevalence of domestic violence and associated factors among pregnant women attending antenatal care service at University of Gondar Referral Hospital, Northwest Ethiopia. BMC Women’s Health, 18(1), 138. [Google Scholar] [CrossRef] [PubMed]
- Ferdos, J., Rahman, M. M., Jesmin, S. S., Rahman, M. A., & Sasagawa, T. (2018). Association between intimate partner violence during pregnancy and maternal pregnancy complications among recently delivered women in Bangladesh. Aggressive Behavior, 44(3), 294–305. [Google Scholar] [CrossRef]
- Field, S., Onah, M., van Heyningen, T., & Honikman, S. (2018). Domestic and intimate partner violence among pregnant women in a low resource setting in South Africa: A facility-based, mixed methods study. BMC Women’s Health, 18(1), 119. [Google Scholar] [CrossRef]
- Fisher, J., Tran, T. D., Biggs, B., Dang, T. H., Nguyen, T. T., & Tran, T. (2013). Intimate partner violence and perinatal common mental disorders among women in rural Vietnam. International Health, 5(1), 29–37. [Google Scholar] [CrossRef]
- Fonseca-Machado, M. de O., Monteiro, J. C. dos S., Haas, V. J., de Vilhena, A. C. F. A., & Gomes-Sponholz, F. (2015). Intimate partner violence and anxiety disorders in pregnancy: The importance of vocational training of the nursing staff in facing them. Revista Latino-Americana de Enfermagem, 23(5), 855–864. [Google Scholar] [CrossRef] [PubMed]
- Gashaw, B. T., Magnus, J. H., & Schei, B. (2019). Intimate partner violence and late entry into antenatal care in Ethiopia. Women and Birth, 32(6), e530–e537. [Google Scholar] [CrossRef]
- Gebrekristos, L. T., Groves, A. K., McNaughton Reyes, L., Moodley, D., Beksinska, M., & Maman, S. (2023). Intimate partner violence victimization during pregnancy increases risk of postpartum depression among urban adolescent mothers in South Africa. Reproductive Health, 20(1), 68. [Google Scholar] [CrossRef] [PubMed]
- Gelaye, B., Do, N., Avila, S., Carlos Velez, J., Zhong, Q. Y., Sanchez, S. E., Lee Peterlin, B., & Williams, M. A. (2016). Childhood abuse, intimate partner violence and risk of migraine among pregnant women: An epidemiologic study. Headache, 56(6), 976–986. [Google Scholar] [CrossRef]
- Gharacheh, M., Azadi, S., Mohammadi, N., Montazeri, S., & Khalajinia, Z. (2015). Domestic violence during pregnancy and women’s health-related quality of life. Global Journal of Health Science, 8(2), 27–34. [Google Scholar] [CrossRef] [PubMed]
- Gómez Aristizábal, L. Y., Confortin, S. C., Batista, R. F. L., de Britto e Alves, M. T. S. S., Simões, V. M. F., & da Silva, A. A. M. (2022). Association between violence and depression during pregnancy with perinatal outcomes: A moderated mediation analysis. BMC Pregnancy and Childbirth, 22(1), 801. [Google Scholar] [CrossRef]
- Gul, S., Zeb, L., & Ruby Faiz, N. (2013). Frequency of different types of domestic violence in antenatal patients. Journal of Postgraduate Medical Institute, 27, 331–335. [Google Scholar]
- Higgins, J. P. T., Thompson, S. G., Deeks, J. J., & Altman, D. G. (2003). Measuring inconsistency in meta-analyses. BMJ (Clinical Research Ed.), 327(7414), 557–560. [Google Scholar] [CrossRef]
- Hooker, L., & Taft, A. (2021). Who is being screened for intimate partner violence in primary care settings? Secondary data analysis of a cluster randomised trial. Maternal and Child Health Journal, 25(10), 1554–1561. [Google Scholar] [CrossRef] [PubMed]
- Ilori, O. R., Olugbenga-Bello, A. I., & Awodutire, P. O. (2023). Is intimate partner violence more common among HIV-positive pregnant women? A comparative study in Oyo State, Nigeria. Journal of the International Association of Providers of AIDS Care, 22, 23259582231151844. [Google Scholar] [CrossRef] [PubMed]
- Islam, M. J., Broidy, L., Mazerolle, P., Baird, K., & Mazumder, N. (2021). Exploring intimate partner violence before, during, and after pregnancy in Bangladesh. Journal of Interpersonal Violence, 36(7–8), 3584–3612. [Google Scholar] [CrossRef]
- Iyengar, R., Bondade, S., & Raj, R. (2021). A cross sectional hospital-based study of intimate partner violence and psychiatric comorbidity in pregnancy. Archives of Psychiatry and Psychotherapy, 22(4), 12–21. [Google Scholar] [CrossRef]
- Kana, M. A., Safiyan, H., Yusuf, H. E., Musa, A. S. M., Richards-Barber, M., Harmon, Q. E., & London, S. J. (2020). Association of intimate partner violence during pregnancy and birth weight among term births: A cross-sectional study in Kaduna, Northwestern Nigeria. BMJ Open, 10(12), e036320. [Google Scholar] [CrossRef]
- Kataoka, Y., & Imazeki, M. (2018). Experiences of being screened for intimate partner violence during pregnancy: A qualitative study of women in Japan. BMC Women’s Health, 18(1), 75. [Google Scholar] [CrossRef] [PubMed]
- Khaironisak, H., Zaridah, S., Hasanain, F. G., & Zaleha, M. I. (2017). Prevalence, risk factors, and complications of violence against pregnant women in a hospital in Peninsular Malaysia. Women and Health, 57(8), 919–941. [Google Scholar] [CrossRef]
- Khatlani, K., Azam, I., Baqir, M., Mehmood, A., & Pasha-Razzak, O. (2023). Exploring the relationship between intimate partner violence during pregnancy and stillbirths. Injury, 54, 110477. [Google Scholar] [CrossRef]
- Kian, F. R., Alikamali, M., Aliei, M. M., & Mehran, A. (2019). Patterns of intimate partner violence: A study of female victims in urban versus rural areas of southeast Iran. Shiraz E Medical Journal, 20(10), e69680. [Google Scholar] [CrossRef]
- Kirk, L., & Bezzant, K. (2020). What barriers prevent health professionals screening women for domestic abuse? A literature review. British Journal of Nursing (Mark Allen Publishing), 29(13), 754–760. [Google Scholar] [CrossRef]
- Kita, S., Haruna, M., Hikita, N., Matsuzaki, M., & Kamibeppu, K. (2017). Development of the Japanese version of the Woman Abuse Screening Tool-Short. Nursing and Health Sciences, 19(1), 35–43. [Google Scholar] [CrossRef]
- Kita, S., Haruna, M., Matsuzaki, M., & Kamibeppu, K. (2016). Associations between intimate partner violence (IPV) during pregnancy, mother-to-infant bonding failure, and postnatal depressive symptoms. Archives of Women’s Mental Health, 19(4), 623–634. [Google Scholar] [CrossRef]
- Koirala, S. (2022). Intimate Partner Violence and Adverse Pregnancy Outcomes. Kathmandu University Medical Journal, 20, 290–294. [Google Scholar] [CrossRef]
- Krishnamurti, T., Davis, A. L., Quinn, B., Castillo, A. F., Martin, K. L., & Simhan, H. N. (2021). Mobile remote monitoring of intimate partner violence among pregnant patients during the COVID-19 shelter-in-place Order: Quality improvement pilot study. Journal of Medical Internet Research, 23(2), e22790. [Google Scholar] [CrossRef]
- Lee, J. Y., June, K. J., Khang, Y. H., Kim, Y. M., & Cho, H. J. (2023). Prevalence of intimate partner violence victimization among Korean perinatal women and associated factors. International Journal of Gynecology and Obstetrics, 161(2), 649–654. [Google Scholar] [CrossRef] [PubMed]
- Lima, L. da S., do Carmo, T. O. A., de Souza Brito Neto, C., & da Cunha Pena, J. L. (2020). Depressive symptoms in pregnant women and intimate partner violence: A cross-sectional study. Enfermeria Global, 19(4), 31–45. [Google Scholar] [CrossRef]
- Luhumyo, L., Mwaliko, E., Tonui, P., Getanda, A., & Hann, K. (2020). The magnitude of intimate partner violence during pregnancy in Eldoret, Kenya: Exigency for policy action. Health Policy and Planning, 35, I7–I18. [Google Scholar] [CrossRef]
- Lukasse, M., Schroll, A. M., Ryding, E. L., Campbell, J., Karro, H., Kristjansdottir, H., Laanpere, M., Steingrimsdottir, T., Tabor, A., Temmerman, M., Van Parys, A. S., Wangel, A. M., & Schei, B. (2014). Prevalence of emotional, physical and sexual abuse among pregnant women in six European countries. Acta Obstetricia et Gynecologica Scandinavica, 93(7), 669–677. [Google Scholar] [CrossRef]
- Mahenge, B., Likindikoki, S., Stöckl, H., & Mbwambo, J. (2013). Intimate partner violence during pregnancy and associated mental health symptoms among pregnant women in Tanzania: A cross-sectional study. BJOG: An International Journal of Obstetrics and Gynaecology, 120(8), 940–947. [Google Scholar] [CrossRef]
- Martin-de-las-Heras, S., Velasco, C., de Dios Luna, J., & Martin, A. (2015). Unintended pregnancy and intimate partner violence around pregnancy in a population-based study. Women and Birth, 28(2), 101–105. [Google Scholar] [CrossRef]
- Martin-de-las-Heras, S., Velasco, C., Luna-del-Castillo, J. D. D., & Khan, K. S. (2019). Breastfeeding avoidance following psychological intimate partner violence during pregnancy: A cohort study and multivariate analysis. BJOG: An International Journal of Obstetrics and Gynaecology, 126(6), 778–783. [Google Scholar] [CrossRef]
- McKelvie, S., Stocker, R., Manwo, M. M., Manwo, A., Sala, T., Leodoro, B., Tran, T., & Fisher, J. (2021). Intimate partner violence and health outcomes experienced by women who are pregnant: A cross-sectional survey in Sanma Province, Vanuatu. The Lancet Regional Health—Western Pacific, 16, 100272. [Google Scholar] [CrossRef] [PubMed]
- Meinhart, M., Seff, I., Troy, K., McNelly, S., Vahedi, L., Poulton, C., & Stark, L. (2021). Identifying the impact of intimate partner violence in humanitarian settings: Using an ecological framework to review 15 years of evidence. International Journal of Environmental Research and Public Health, 18(13), 6963. [Google Scholar] [CrossRef] [PubMed]
- Metreau, E., Young, K. E., & Eapen, S. G. (2024, July 1). World Bank country classifications by income level for 2024–2025. Available online: https://blogs.worldbank.org/en/opendata/world-bank-country-classifications-by-income-level-for-2024-2025 (accessed on 10 May 2025).
- Mohamed, A. A., Mohamed Fahmy, A., Amin Hassan Fahmy El-Sabaa, H., & Abd-Allah Oweedah, N. (2013). Intimate partner violence during pregnancy and its adverse outcomes. Life Science Journal, 10(3), 1097–8135. Available online: https://www.jofamericanscience.org/journals/am-sci/am0908/021_19509am0908_142_150.pdf (accessed on 10 May 2025).
- Musa, A., Chojenta, C., & Loxton, D. (2020). High rate of partner violence during pregnancy in eastern Ethiopia: Findings from a facility-based study. PLoS ONE, 15(6), e0233907. [Google Scholar] [CrossRef]
- Muzrif, M. M., Perera, D., Wijewardena, K., Schei, B., & Swahnberg, K. (2018). Domestic violence: A cross-sectional study among pregnant women in different regions of Sri Lanka. BMJ Open, 8(2), e017745. [Google Scholar] [CrossRef]
- Naghizadeh, S., Mirghafourvand, M., & Mohammadirad, R. (2021). Domestic violence and its relationship with quality of life in pregnant women during the outbreak of COVID-19 disease. BMC Pregnancy and Childbirth, 21(1), 88. [Google Scholar] [CrossRef] [PubMed]
- Nelson, C. A., & Gabard-Durnam, L. J. (2020). Early adversity and critical periods: Neurodevelopmental consequences of violating the expectable environment. Trends in Neurosciences, 43(3), 133–143. [Google Scholar] [CrossRef]
- Nhi, T. T., Hanh, N. T. T., Hinh, N. D., Van Toan, N., Gammeltoft, T., Rasch, V., & Meyrowitsch, D. W. (2019). Intimate partner violence among pregnant women and postpartum depression in Vietnam: A longitudinal study. BioMed Research International, 2019, 4717485. [Google Scholar] [CrossRef]
- Njoku, I. V., Enebe, J. T., & Dim, C. C. (2021). Magnitude and predictors of female domestic abuse in pregnancy in a patriarchal african society: A cross-sectional study of pregnant women in Enugu, South East Nigeria. Pan African Medical Journal, 40. [Google Scholar]
- Nongrum, R., Thomas, E., Lionel, J., & Jacob, K. S. (2014). Domestic violence as a risk factor for maternal depression and neonatal outcomes: A hospital-based cohort study. Indian Journal of Psychological Medicine, 36(2), 179–181. [Google Scholar] [CrossRef]
- Okunola, T. O., Awoleke, J. O., Olofinbiyi, B. A., Rosiji, B. O., Omoya, S., & Olubiyi, A. O. (2021). Adverse birth outcomes among women exposed to intimate partner violence in pregnancy in Ikere-Ekiti, South-west Nigeria: A prospective cohort study. European Journal of Obstetrics and Gynecology and Reproductive Biology, 267, 186–191. [Google Scholar] [CrossRef]
- Omoronyia, O., Ayuk, A., Nwafor, K., & Legogie, A. (2020). Association between Intimate Partner Violence and Mental Health Status During Pregnancy: A Survey among Pregnant Women in Calabar, Nigeria. Indian Journal of Public Health Research & Development, 11(11), 248–254. [Google Scholar] [CrossRef]
- Ottawa Hospital Research Institute. (2000). The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Available online: https://www.ohri.ca/programs/clinical_epidemiology/oxford.asp (accessed on 10 May 2025).
- Page, M. J., McKenzie, J. E., Bossuyt, P. M., Boutron, I., Hoffmann, T. C., Mulrow, C. D., Shamseer, L., Tetzlaff, J. M., Akl, E. A., Brennan, S. E., Chou, R., Glanville, J., Grimshaw, J. M., Hróbjartsson, A., Lalu, M. M., Li, T., Loder, E. W., Mayo-Wilson, E., McDonald, S., … Moher, D. (2021). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. [Google Scholar] [CrossRef]
- Priya, A., Chaturvedi, S., Bhasin, S., Bhatia, M., & Radhakrishnan, G. (2019). Are pregnant women also vulnerable to domestic violence? A community based enquiry for prevalence and predictors of domestic violence among pregnant women. Journal of Family Medicine and Primary Care, 8(5), 1575. [Google Scholar] [CrossRef] [PubMed]
- Pun, K. D., Rishal, P., Darj, E., Infanti, J. J., Shrestha, S., Lukasse, M., Schei, B., Lund, R., Koju, R., Wijewardene, K., Perera, D. C., Muzrif, M. M., Swahnberg, K., & Campbell, J. C. (2019). Domestic violence and perinatal outcomes—A prospective cohort study from Nepal. BMC Public Health, 19(1), 671. [Google Scholar] [CrossRef] [PubMed]
- Pun, K. D., Rishal, P., Infanti, J. J., Bjørngaard, J. H., Koju, R., Schei, B., & Darj, E. (2018). Exposure to domestic violence influences pregnant women’s preparedness for childbirth in Nepal: A cross-sectional study. PLoS ONE, 13(7), e0200234. [Google Scholar] [CrossRef] [PubMed]
- Rasch, V., Van, T. N., Nguyen, H. T. T., Manongi, R., Mushi, D., Meyrowitsch, D. W., Gammeltoft, T., & Wu, C. S. (2018). Intimate partner violence (IPV): The validity of an IPV screening instrument utilized among pregnant women in Tanzania and Vietnam. PLoS ONE, 13(2), e0190856. [Google Scholar] [CrossRef]
- Rees, S., Mohsin, M., Tay, A. K., Soares, E., Tam, N., da Costa, Z., Tol, W., & Silove, D. (2017). Associations between bride price stress and intimate partner violence amongst pregnant women in Timor-Leste. Globalization and Health, 13(1), 66. [Google Scholar] [CrossRef]
- Rees, S. J., Tol, W., Mohammad, M., Tay, A., Tam, N., dos Reis, N., da Costa, E., Soares, C., & Silove, D. (2016). A high-risk group of pregnant women with elevated levels of conflict-related trauma, intimate partner violence, symptoms of depression and other forms of mental distress in post-conflict Timor-Leste. Translational Psychiatry, 6, e725. [Google Scholar] [CrossRef]
- Ribeiro, M. R. C., Da Silva, A. A. M., De Britto E Alves, M. T. S. S., Batista, R. F. L., Ribeiro, C. C. C., Schraiber, L. B., Bettiol, H., & Barbieri, M. A. (2017). Effects of socioeconomic status and social support on violence against pregnant women: A structural equation modeling analysis. PLoS ONE, 12(1), e0170469. [Google Scholar] [CrossRef]
- Ribeiro, S. V. O., Batista, R. F. L., Ribeiro, M. R. C., Pessoa, K. C., Simões, V. M. F., De Figueiredo, F. P., & Bettiol, H. (2019). Violence and depressive symptoms during pregnancy in brisa cohort: Using structural equation modeling approach. Revista Brasileira de Saude Materno Infantil, 19(1), 173–184. [Google Scholar] [CrossRef]
- Rishal, P., Pun, K. D., Schei, B., Bhandari, B., Joshi, S. K., Swahnberg, K., Infanti, J. J., Lukasse, M., Bjørngaard, J. H., Darj, E., Lund, R., Koju, R., Wijewardene, K., Perera, D. C., Muzrif, M. M. M., & Campbell, J. C. (2020). Improving safety among pregnant women reporting domestic violence in Nepal—A pilot study. International Journal of Environmental Research and Public Health, 17(7), 2268. [Google Scholar] [CrossRef]
- Samal, S., & Poornesh, S. (2022). Prevalence of Domestic Violence among Pregnant Women: A Cross-sectional Study from a Tertiary Care Centre, Puducherry, India. Journal of Clinical and Diagnostic Research, 16, 6. [Google Scholar] [CrossRef]
- Sapkota, D., Anderson, D., Saito, A., & Baird, K. (2021). Domestic and family violence and its association with mental health among pregnant women attending antenatal care in a tertiary hospital of Eastern Nepal. Journal of Nepal Health Research Council, 19(1), 115–121. [Google Scholar] [CrossRef] [PubMed]
- Sánchez, O. D. R., Tanaka Zambrano, E., Dantas-Silva, A., Bonás, M. K., Grieger, I., Machado, H. C., & Surita, F. G. (2023). Domestic violence: A cross-sectional study among pregnant and postpartum women. Journal of Advanced Nursing, 79(4), 1525–1539. [Google Scholar] [CrossRef] [PubMed]
- Shamu, S., Abrahams, N., Zarowsky, C., Shefer, T., & Temmerman, M. (2013). Intimate partner violence during pregnancy in Zimbabwe: A cross-sectional study of prevalence, predictors and associations with HIV. Tropical Medicine and International Health, 18(6), 696–711. [Google Scholar] [CrossRef]
- Shamu, S., Zarowsky, C., Shefer, T., Temmerman, M., & Abrahams, N. (2014). Intimate partner violence after disclosure of HIV test results among pregnant women in Harare, Zimbabwe. PLoS ONE, 9(10), e109447. [Google Scholar] [CrossRef]
- Shannon, L., Nash, S., & Jackson, A. (2016). Examining intimate partner violence and health factors among rural appalachian pregnant women. Journal of Interpersonal Violence, 31(15), 2622–2640. [Google Scholar] [CrossRef]
- Shrestha, M., Shrestha, S., & Shrestha, B. (2016). Domestic violence among antenatal attendees in a Kathmandu hospital and its associated factors: A cross-sectional study. BMC Pregnancy and Childbirth, 16(1), 360. [Google Scholar] [CrossRef][Green Version]
- Silva, R. de P., & Leite, F. M. C. (2019). Intimate partner violence during pregnancy: Prevalence and associated factors. Revista de Saude Publica, 54(97), 1–11. [Google Scholar] [CrossRef]
- Silva, R. de P., Leite, F. M. C., Dos Santos Netto, E. T., & Deslandes, S. F. (2022). Intimate partner violence during pregnancy: A focus on partner characteristics. In Ciencia e Saude Coletiva (Vol. 27, Issue 5, pp. 1873–1882). Associacao Brasileira de Pos—Graduacao em Saude Coletiva. [Google Scholar] [CrossRef]
- Smith, R., Wight, R., & Homer, C. S. E. (2018). “Asking the hard questions”: Improving midwifery students’ confidence with domestic violence screening in pregnancy. Nurse Education in Practice, 28, 27–33. [Google Scholar] [CrossRef] [PubMed]
- Sobhani, S., Niknami, M., Mirhaghjou, S. N., & Roshan, Z. A. e. (2018). Domestic violence and its maternal and fetal consequences among pregnant women. Journal of Holistic Nursing and Midwifery, 28(2), 143–149. [Google Scholar] [CrossRef]
- Sulaiman, B., Omonua, K. I., Opadiran, O. R., & Yabagi, A. I. (2021). Intimate partner violence among obstetric population at university of Abuja teaching hospital, Abuja, Nigeria. Nigerian Postgraduate Medical Journal, 28(4), 255–258. [Google Scholar] [CrossRef] [PubMed]
- Sussmann, L. G. P. R., Faisal-Cury, A., & Pearson, R. (2020). Depression as a mediator between intimate partner violence and postpartum sexual issues: A structural analysis. Revista Brasileira de Epidemiologia, 23, e200048. [Google Scholar] [CrossRef] [PubMed]
- Suzuki, S., Yamada, F., & Eto, M. (2018). Influence of intimate partner violence on mental status in Japanese women during the first trimester of pregnancy. Journal of Maternal-Fetal and Neonatal Medicine, 31(11), 1524–1526. [Google Scholar] [CrossRef]
- Takelle, G. M., Nakie, G., Rtbey, G., & Melkam, M. (2023). Depressive symptoms and associated factors among pregnant women attending antenatal care at Comprehensive Specialized Hospitals in Northwest Ethiopia, 2022: An institution-based cross-sectional study. Frontiers in Psychiatry, 14, 1148638. [Google Scholar] [CrossRef]
- United Nations. (1994). Declaration on the elimination of violence against women proclaimed by general assembly resolution 48/104 of 20 December. Available online: https://www.un.org/en/genocideprevention/documents/atrocity-crimes/Doc.21_declaration%20elimination%20vaw.pdf (accessed on 12 May 2025).
- United Nations. (2015). Transforming our world: The 2030 Agenda for sustainable development: Resolution/adopted by the general assembly. United Nations. [Google Scholar]
- UN Women. (2024). Types of violence against women and girls. Available online: https://www.unwomen.org/en/articles/faqs/faqs-types-of-violence-against-women-and-girls (accessed on 13 May 2025).
- Utaile, M. M., Ahmed, A. A., & Yalew, A. W. (2023). Multilevel analysis of factors for intimate partner violence during pregnancy in Gammo Goffa Zone, South Ethiopia: A community based study. Frontiers in Public Health, 11, 1122041. [Google Scholar] [CrossRef]
- Uzoho, I. C., Baptiste-Roberts, K., Animasahun, A., & Bronner, Y. (2023). The impact of COVID-19 pandemic on Intimate Partner Violence (IPV) against women. International Journal of Social Determinants of Health and Health Services, 53(4), 494–507. [Google Scholar] [CrossRef]
- Velasco, C., Luna, J. D., Martin, A., Caño, A., & Martin-De-las-heras, S. (2014). Intimate partner violence against Spanish pregnant women: Application of two screening instruments to assess prevalence and associated factors. Acta Obstetricia et Gynecologica Scandinavica, 93(10), 1050–1058. [Google Scholar] [CrossRef]
- Wangel, A. M., Ryding, E. L., Schei, B., Östman, M., Lukasse, M., Temmerman, M., Steingrímsdóttir, T., Tabor, A., Karro, H., Van, A. S., Kristjánsdóttir, H., Schroll, A. M., & Laanpere, M. (2016). Emotional, physical, and sexual abuse and the association with symptoms of depression and posttraumatic stress in a multi-ethnic pregnant population in southern Sweden. Sexual and Reproductive Healthcare, 9, 7–13. [Google Scholar] [CrossRef] [PubMed]
- Watson, L. F., & Taft, A. J. (2013). Intimate partner violence and the association with very preterm birth. Birth, 40(1), 17–23. [Google Scholar] [CrossRef]
- Wirtz, A. L., Pham, K., Glass, N., Loochkartt, S., Kidane, T., Cuspoca, D., Rubenstein, L. S., Singh, S., & Vu, A. (2014). Gender-based violence in conflict and displacement: Qualitative findings from displaced women in Colombia. Conflict and Health, 8(1), 10. [Google Scholar] [CrossRef]
- Wokoma, T. T., Jampala, M., Bexhell, H., Guthrie, K., & Lindow, S. (2014). A comparative study of the prevalence of domestic violence in women requesting a termination of pregnancy and those attending the antenatal clinic. BJOG: An International Journal of Obstetrics and Gynaecology, 121(5), 627–633. [Google Scholar] [CrossRef]
- World Health Organization. (n.d.). Regional offices. Available online: https://www.who.int/about/who-we-are/regional-offices (accessed on 18 March 2025).
- Zapata-Calvente, A. L., Megías, J. L., Velasco, C., Caño, A., Khan, K. S., Rubio, L., & Martín-De-Las-Heras, S. (2022). Screening for intimate partner violence during pregnancy: A test accuracy study. European Journal of Public Health, 32(3), 429–435. [Google Scholar] [CrossRef]
- Zheng, B., Zhu, X., Hu, Z., Zhou, W., Yu, Y., Yin, S., & Xu, H. (2020). The prevalence of domestic violence and its association with family factors: A cross-sectional study among pregnant women in urban communities of Hengyang City, China. BMC Public Health, 20(1), 620. [Google Scholar] [CrossRef] [PubMed]
- Zou, S., Zhang, Y., Cao, Y., & Zhang, Y. (2015). Correlation of maternal abuse during pregnancy with infant temperament and development. Archives of Disease in Childhood, 100(10), 938–943. [Google Scholar] [CrossRef] [PubMed]
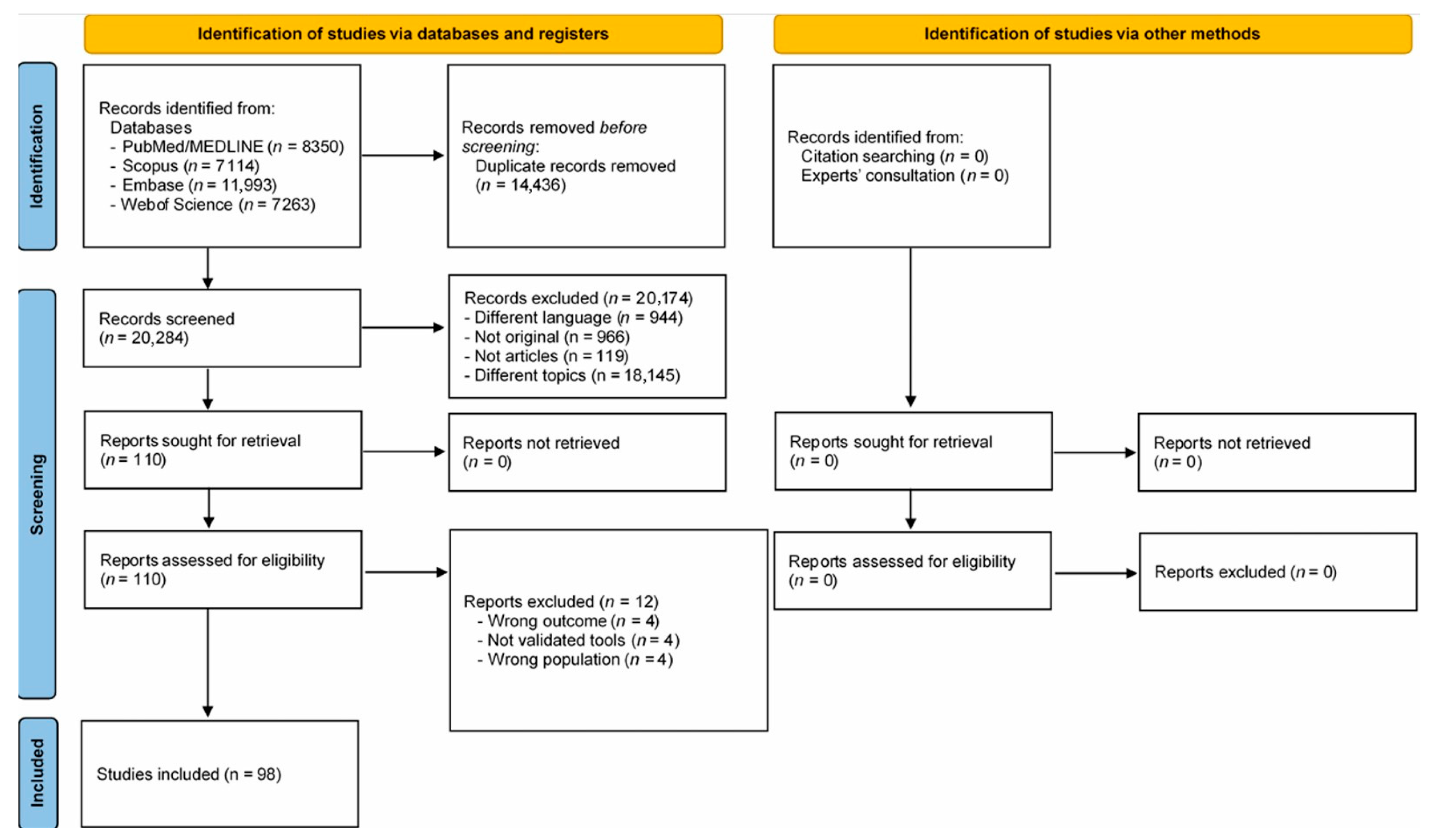
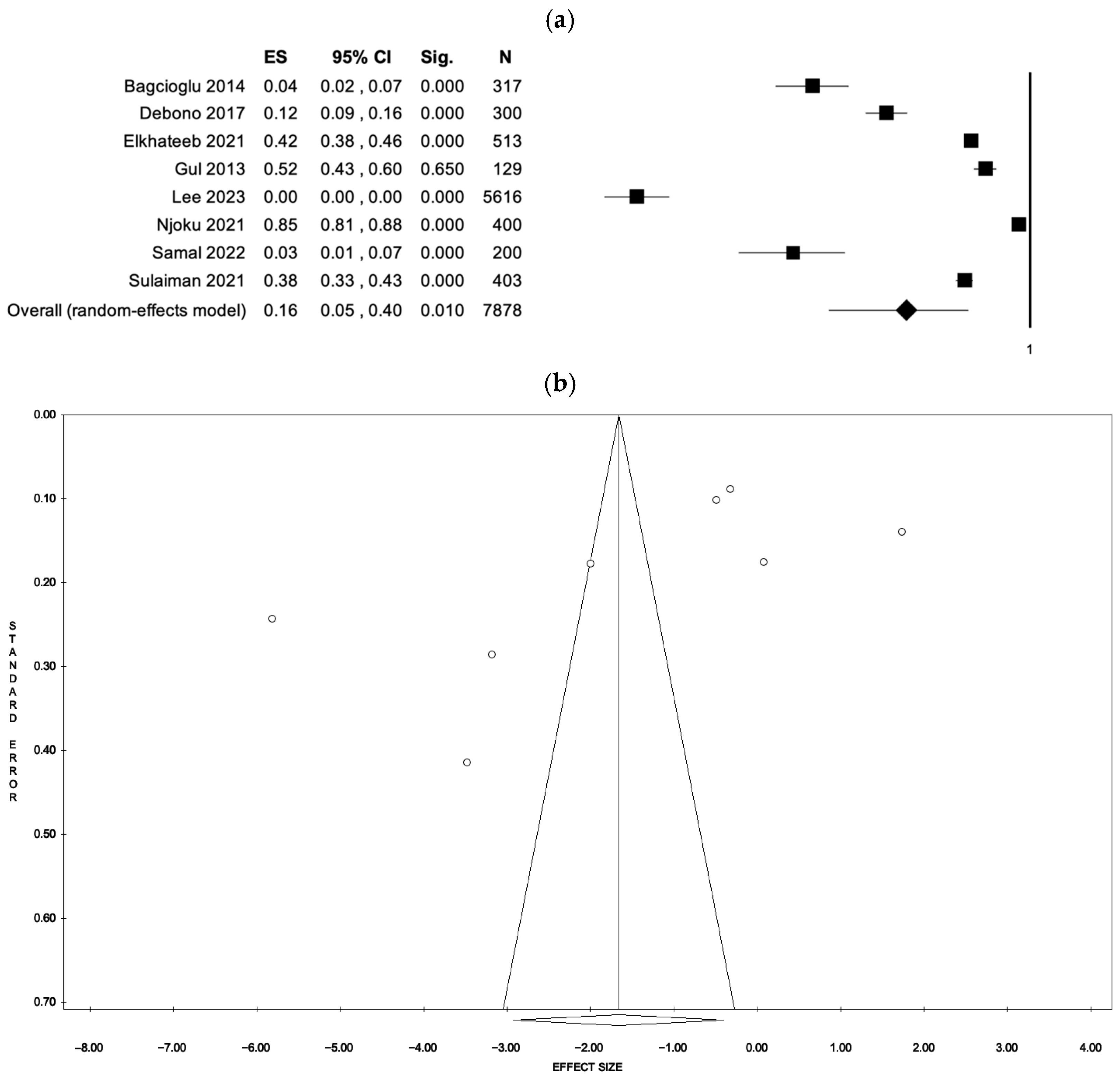
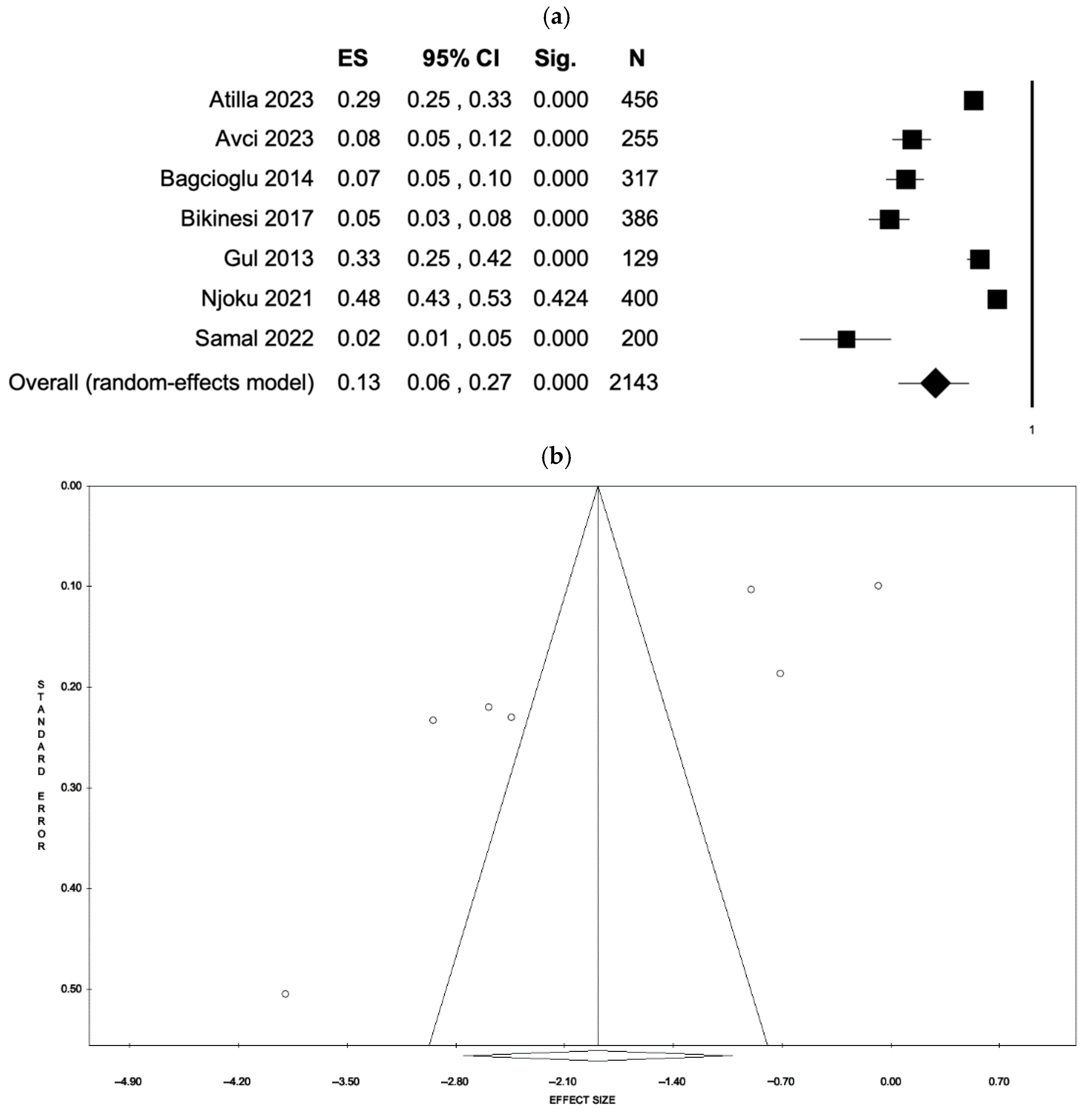
| Search Strategy | Details |
|---|---|
| Inclusion criteria | P: Pregnant women (across all trimesters) or women in the puerperium period. E: Any type of domestic violence perpetrated during pregnancy by an intimate partner. C: Not applicable. O: Prevalence of violence; type of screening tool. S: Original observational studies (including cross-sectional, case–control, or cohort, both prospective and retrospective studies) or interventional studies published as peer-reviewed articles in international scientific journals. |
| Exclusion criteria | P: Nulliparas, menopausal women, pre-pubertal females. E: Other types of violence not perpetrated during pregnancy and not by an intimate partner. C: Not applicable. O: Any other health outcomes. S: Not original (reviews with or without meta-analysis), not performed among humans, not published as peer-reviewed articles in international scientific journals (book, book chapter, thesis), no full-text papers (abstract, conference paper, letter, commentary, note). |
| Language | English and Italian |
| Time filter | Last 10 years |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brunelli, L.; Pennisi, F.; Pinto, A.; Cella, L.; Parpinel, M.; Brusaferro, S.; Signorelli, C.; Baldo, V.; Gianfredi, V. Prevalence and Screening Tools of Intimate Partner Violence Among Pregnant and Postpartum Women: A Systematic Review and Meta-Analysis. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 161. https://doi.org/10.3390/ejihpe15080161
Brunelli L, Pennisi F, Pinto A, Cella L, Parpinel M, Brusaferro S, Signorelli C, Baldo V, Gianfredi V. Prevalence and Screening Tools of Intimate Partner Violence Among Pregnant and Postpartum Women: A Systematic Review and Meta-Analysis. European Journal of Investigation in Health, Psychology and Education. 2025; 15(8):161. https://doi.org/10.3390/ejihpe15080161
Chicago/Turabian StyleBrunelli, Laura, Flavia Pennisi, Antonio Pinto, Loredana Cella, Maria Parpinel, Silvio Brusaferro, Carlo Signorelli, Vincenzo Baldo, and Vincenza Gianfredi. 2025. "Prevalence and Screening Tools of Intimate Partner Violence Among Pregnant and Postpartum Women: A Systematic Review and Meta-Analysis" European Journal of Investigation in Health, Psychology and Education 15, no. 8: 161. https://doi.org/10.3390/ejihpe15080161
APA StyleBrunelli, L., Pennisi, F., Pinto, A., Cella, L., Parpinel, M., Brusaferro, S., Signorelli, C., Baldo, V., & Gianfredi, V. (2025). Prevalence and Screening Tools of Intimate Partner Violence Among Pregnant and Postpartum Women: A Systematic Review and Meta-Analysis. European Journal of Investigation in Health, Psychology and Education, 15(8), 161. https://doi.org/10.3390/ejihpe15080161








