Promoting Healthy Organizations Through Urban Nature: Psychological and Physiological Effects in Healthcare Workers
Abstract
1. Introduction
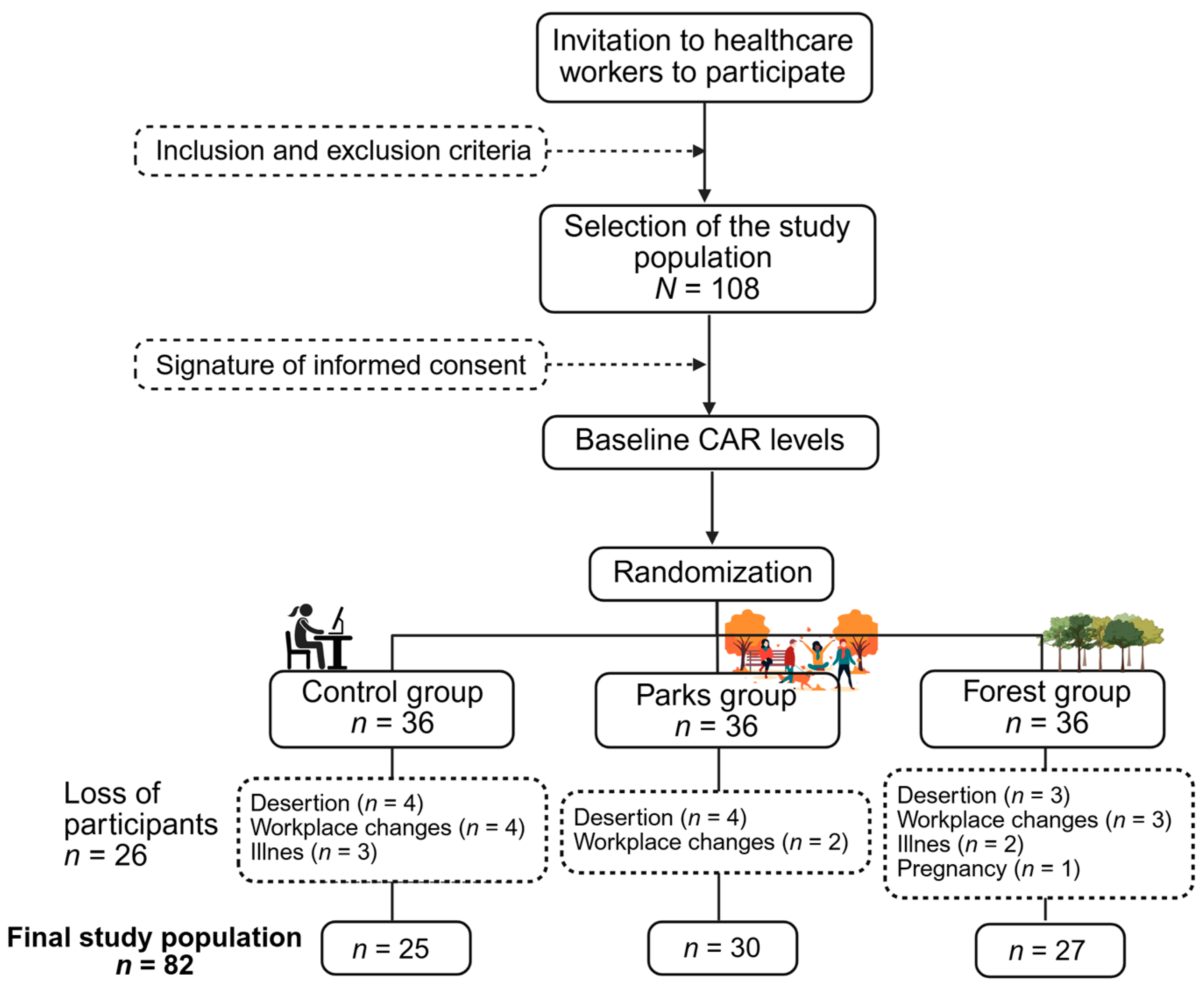
2. Materials and Methods
2.1. Study Design and Population
Eligibility Criteria
2.2. Intervention Development
2.3. Measurement Tools for Psychological Evaluation
2.4. Salivary Cortisol Determination for Physiological Evaluation
2.5. Statistical Analysis
3. Results
3.1. Psychological Effects
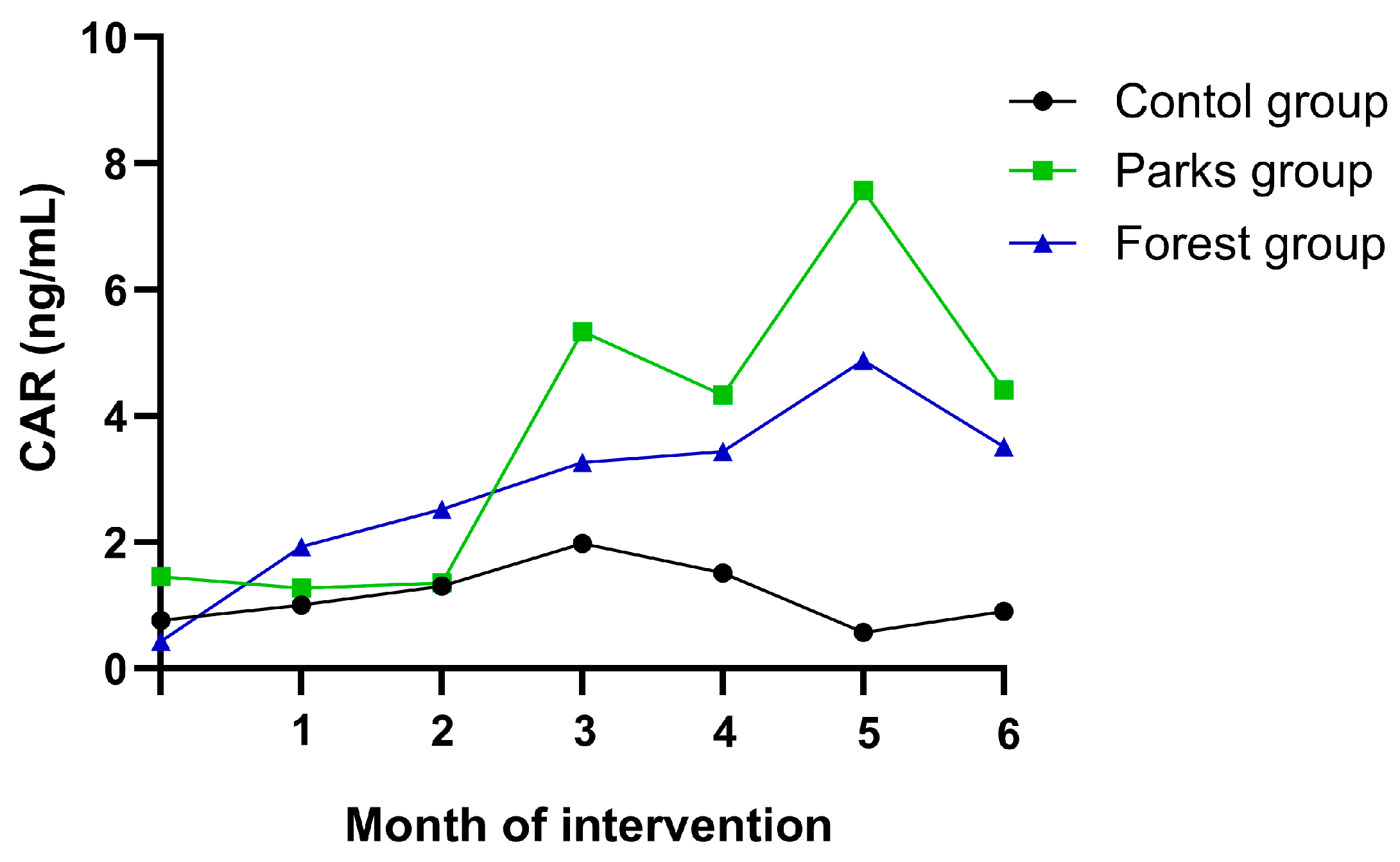
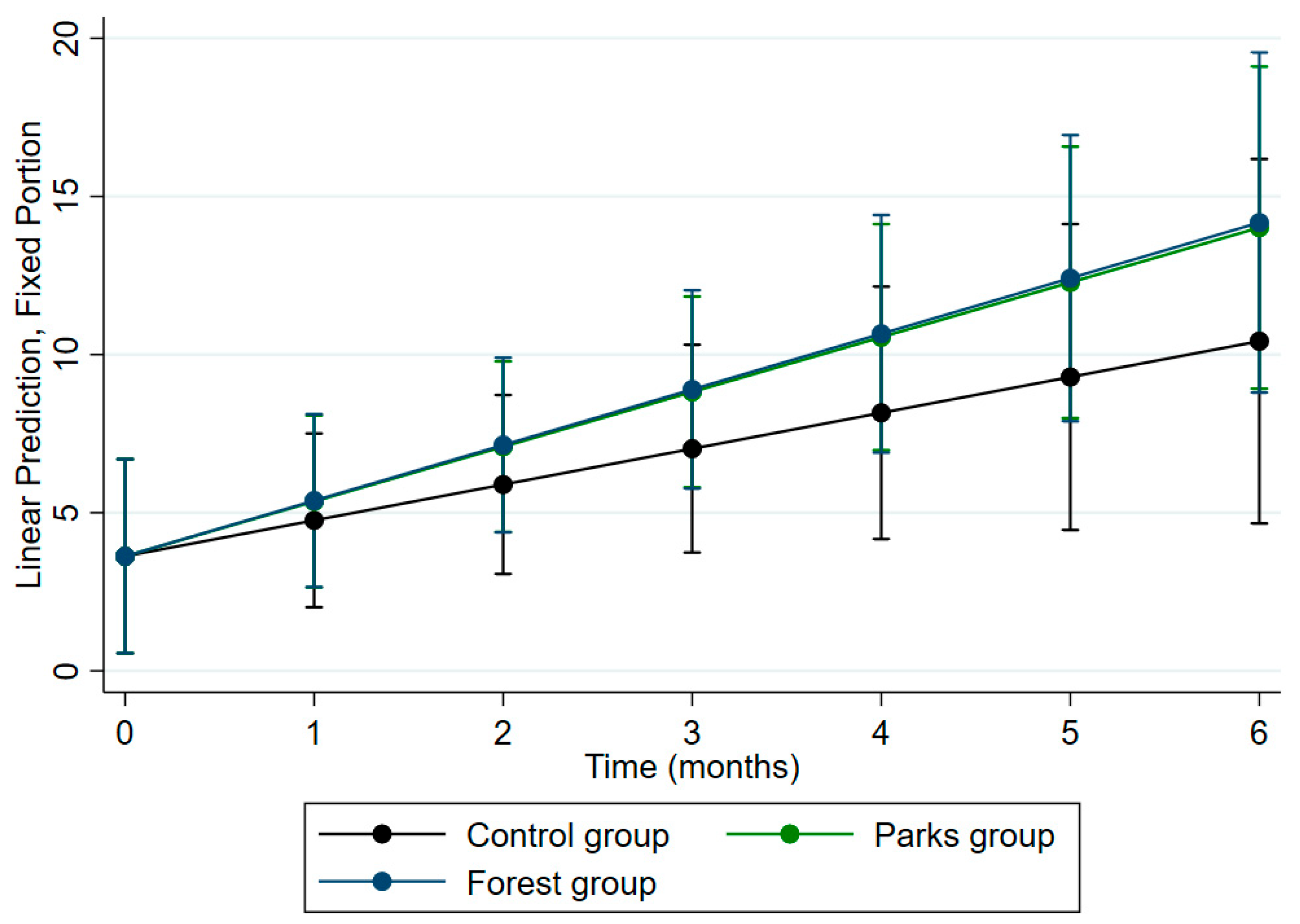
3.2. Physiological Effects
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
| CAR | Cortisol Awakening Response |
| NIH | National Institutes of Health |
| CEMIN | Ethics and Research Methodologies Committee |
| PSS-14 | Perceived Stress Scale |
| STAI | State-Trait Anxiety Inventory |
| PSQI | Pittsburgh Sleep Quality Index |
| MANOVA | Multivariate Analysis of Variance |
| BMI | Body Mass Index |
| HPA | hypothalamic–pituitary–adrenal |
References
- Andersen, L., Corazon, S. S., & Stigsdotter, U. K. (2021). Nature exposure and its effects on immune system functioning: A systematic review. International Journal of Environmental Research and Public Health, 18(4), 1416. [Google Scholar] [CrossRef] [PubMed]
- Anderson, T., & Wideman, L. (2023). The association between the cortisol and cortisone awakening responses. Psychoneuroendocrinology, 152, 106075. [Google Scholar] [CrossRef] [PubMed]
- Bani-Issa, W., Radwan, H., Al Marzooq, F., Al Awar, S., Al-Shujairi, A. M., Samsudin, A. R., Khasawneh, W., & Albluwi, N. (2020). Salivary cortisol, subjective stress and quality of sleep among female healthcare professionals. Journal of Multidisciplinary Healthcare, 13, 125–140. [Google Scholar] [CrossRef] [PubMed]
- Berger, V. W., Bour, L. J., Carter, K., Chipman, J. J., Everett, C. C., Heussen, N., Hewitt, C., Hilgers, R.-D., Luo, Y. A., Renteria, J., Ryeznik, Y., Sverdlov, O., Uschner, D., for the Randomization Innovative Design Scientific Working Group & Beckman, R. A. (2021). A roadmap to using randomization in clinical trials. BMC Medical Research Methodology, 21(1), 168. [Google Scholar] [CrossRef]
- Bernal, J. (2024). El 80% de los trabajadores colombianos padece de estrés laboral: Qué es lo que está pasando. Infobae. Available online: https://www.infobae.com/colombia/2024/10/03/el-80-de-los-trabajadores-colombianos-padece-de-estres-laboral-revelo-informe-internacional/ (accessed on 10 April 2025).
- Campo-Arias, A., Bustos-Leiton, G. J., & Romero-Chaparro, A. (2009). Internal consistency and dimensionality of the perceived stress scale (PSS-10 and PSS-14) in a sample of female university students in Bogotá, Colombia. Aquichan, 9, 271–280. Available online: http://www.scielo.org.co/scielo.php?script=sci_arttext&pid=S1657-59972009000300007&lng=en (accessed on 10 April 2025).
- Canuto, R., Garcez, A., Spritzer, P. M., & Olinto, M. T. A. (2021). Associations of perceived stress and salivary cortisol with the snack and fast-food dietary pattern in women shift workers. Stress, 24(6), 763–771. [Google Scholar] [CrossRef]
- Chae, Y., Lee, S., Jo, Y., Kang, S., Park, S., & Kang, H. (2021). The effects of forest therapy on immune function. International Journal of Environmental Research and Public Health, 18(16), 8440. [Google Scholar] [CrossRef]
- Choi, H., Jeon, Y.-H., Han, J.-W., Moon, J., Kim, S.-Y., & Woo, J.-M. (2022). The effects of a forest therapy on work-related stress for employees in the manufacturing industry: Randomized control study. Global Advances in Health and Medicine, 11, 1–10. [Google Scholar] [CrossRef]
- Clarke, F. J., Kotera, Y., & McEwan, K. (2021). A qualitative study comparing mindfulness and Shinrin-Yoku (forest bathing): Practitioners’ perspectives. Sustainability, 13(12), 6761. [Google Scholar] [CrossRef]
- Conde, C. A., Orozco Vargas, L. C., Báez Rangel, A. M., & Dallos Arenales, M. I. (2009). Physiological contributions to the validity of criterion and construct of the diagnosis of anxiety according to the psychiatric structured interview and the state-trait anxiety inventory (STAI) in a sample of Colombian university students. Revista Colombiana de Psiquiatría, 38(2), 262–278. [Google Scholar]
- De Melo, M. B., Daldegan-Bueno, D., Menezes Oliveira, M. G., & De Souza, A. L. (2022). Beyond ANOVA and MANOVA for repeated measures: Advantages of generalized estimated equations and generalized linear mixed models and its use in neuroscience research. European Journal of Neuroscience, 56(12), 6089–6098. [Google Scholar] [CrossRef] [PubMed]
- Dziurkowska, E., & Wesolowski, M. (2021). Cortisol as a biomarker of mental disorder severity. Journal of Clinical Medicine, 10(21), 5204. [Google Scholar] [CrossRef] [PubMed]
- Escobar-Córdoba, F., & Eslava-Schmalbach, J. (2005). [Colombian validation of the pittsburgh sleep quality index]. Revista De Neurologia, 40(3), 150–155. [Google Scholar] [PubMed]
- Giglberger, M., Peter, H. L., Kraus, E., Kreuzpointner, L., Zänkert, S., Henze, G.-I., Bärtl, C., Konzok, J., Kirsch, P., Rietschel, M., Kudielka, B. M., & Wüst, S. (2022). Daily life stress and the cortisol awakening response over a 13-months stress period—Findings from the LawSTRESS project. Psychoneuroendocrinology, 141, 105771. [Google Scholar] [CrossRef]
- Hansen, M. M., Jones, R., & Tocchini, K. (2017). Shinrin-Yoku (forest bathing) and nature therapy: A state-of-the-art review. International Journal of Environmental Research and Public Health, 14(8), 851. [Google Scholar] [CrossRef]
- Hosmer, D. W., & Lemeshow, S. (2000). Applied logistic regression (1st ed.). Wiley. [Google Scholar] [CrossRef]
- Hu, S., Wang, Y.-G., Drovandi, C., & Cao, T. (2023). Predictions of machine learning with mixed-effects in analyzing longitudinal data under model misspecification. Statistical Methods & Applications, 32(2), 681–711. [Google Scholar] [CrossRef]
- Huang, H., Xia, Y., Zeng, X., & Lu, A. (2022). Prevalence of depression and depressive symptoms among intensive care nurses: A meta-analysis. Nursing in Critical Care, 27(6), 739–746. [Google Scholar] [CrossRef]
- Ipsos. (2024). Informe del Día Mundial de la Salud Mental 2024. Available online: https://www.ipsos.com/en-id/ipsos-world-mental-health-day-report-2024 (accessed on 10 April 2025).
- James, K. A., Stromin, J. I., Steenkamp, N., & Combrinck, M. I. (2023). Understanding the relationships between physiological and psychosocial stress, cortisol and cognition. Frontiers in Endocrinology, 14, 1085950. [Google Scholar] [CrossRef]
- Jezova, D., Hlavacova, N., Karailievova, L., Lamatungga, K. E., Halamova, J., Tamatam, D., Pichlerova, M., & Pichler, V. (2024). Reduced hair and salivary cortisol concentrations associated with improved emotional well-being following repeated forest walking: A randomized intervention Trial in older adults. Research Square. [Google Scholar] [CrossRef]
- Kavanaugh, J., Hardison, M. E., Rogers, H. H., White, C., & Gross, J. (2022). Assessing the impact of a Shinrin-Yoku (forest bathing) intervention on physician/healthcare professional burnout: A randomized, controlled trial. International Journal of Environmental Research and Public Health, 19(21), 14505. [Google Scholar] [CrossRef]
- Keller, J., Kayira, J., Chawla, L., & Rhoades, J. L. (2023). Forest bathing increases adolescents’ mental well-being: A mixed-methods study. International Journal of Environmental Research and Public Health, 21(1), 8. [Google Scholar] [CrossRef] [PubMed]
- Kim, J., Jeon, J., & Shin, W. S. (2021). The influence of forest activities in a university campus forest on student’s psychological effects. International Journal of Environmental Research and Public Health, 18(5), 2457. [Google Scholar] [CrossRef]
- Kim, Y., Choi, Y., & Kim, H. (2022). Positive effects on emotional stress and sleep quality of forest healing program for exhausted medical workers during the COVID-19 outbreak. International Journal of Environmental Research and Public Health, 19(5), 3130. [Google Scholar] [CrossRef] [PubMed]
- Knezevic, E., Nenic, K., Milanovic, V., & Knezevic, N. N. (2023). The role of cortisol in chronic stress, neurodegenerative diseases, and psychological disorders. Cells, 12(23), 2726. [Google Scholar] [CrossRef]
- Kotera, Y., Richardson, M., & Sheffield, D. (2022). Effects of Shinrin-Yoku (forest bathing) and nature therapy on mental health: A systematic review and meta-analysis. International Journal of Mental Health and Addiction, 20(1), 337–361. [Google Scholar] [CrossRef]
- Kweon, J., Kim, Y., Choi, H., Im, W., & Kim, H. (2024). Enhancing sleep and reducing occupational stress through forest therapy: A comparative study across job groups. Psychiatry Investigation, 21(10), 1120–1128. [Google Scholar] [CrossRef]
- Law, R., & Clow, A. (2020). Stress, the cortisol awakening response and cognitive function. In International review of neurobiology (Vol. 150, pp. 187–217). Elsevier. [Google Scholar] [CrossRef]
- Lew, T., & Fleming, K. J. (2024). Phytoncides and immunity from forest to facility: A systematic review and meta-analysis. Pharmacological Research-Natural Products, 4, 100061. [Google Scholar] [CrossRef]
- Li, Q. (2022). Effects of forest environment (shinrin-yoku/forest bathing) on health promotion and disease prevention—The establishment of “forest medicine”. Environmental Health and Preventive Medicine, 27, 43. [Google Scholar] [CrossRef]
- Lim, P. Y., Dillon, D., & Chew, P. K. H. (2020). A guide to nature immersion: Psychological and physiological benefits. International Journal of Environmental Research and Public Health, 17(16), 5989. [Google Scholar] [CrossRef]
- Lopresti, A. L., Smith, S. J., & Drummond, P. D. (2022). Modulation of the hypothalamic-pituitary-adrenal (HPA) axis by plants and phytonutrients: A systematic review of human trials. Nutritional Neuroscience, 25(8), 1704–1730. [Google Scholar] [CrossRef]
- McEwan, K., Giles, D., Clarke, F. J., Kotera, Y., Evans, G., Terebenina, O., Minou, L., Teeling, C., Basran, J., Wood, W., & Weil, D. (2021). A pragmatic controlled trial of forest bathing compared with compassionate mind training in the UK: Impacts on self-reported wellbeing and heart rate variability. Sustainability, 13(3), 1380. [Google Scholar] [CrossRef]
- Mikkelsen, S., Forman, J. L., Fink, S., Vammen, M. A., Thomsen, J. F., Grynderup, M. B., Hansen, Å. M., Kaerlev, L., Kolstad, H. A., Rugulies, R., & Bonde, J. P. (2017). Prolonged perceived stress and saliva cortisol in a large cohort of Danish public service employees: Cross-sectional and longitudinal associations. International Archives of Occupational and Environmental Health, 90(8), 835–848. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ministerio de Salud y Protección Social. (2023). Encuesta de Minsalud revela que el 66,3% de los colombianos declara haber enfrentado algún problema de salud mental. Available online: https://www.minsalud.gov.co/Paginas/66-porciento-de-colombianos-declara-haber-enfrentado-algun-problema-de-salud-mental.aspx (accessed on 10 April 2025).
- Mygind, L., Stevenson, M. P., Liebst, L. S., Konvalinka, I., & Bentsen, P. (2018). Stress response and cognitive performance modulation in classroom versus natural environments: A quasi-experimental pilot study with children. International Journal of Environmental Research and Public Health, 15(6), 1098. [Google Scholar] [CrossRef]
- Nasser, A., Ozenne, B., Høgsted, E. S., Jensen, P. S., & Frokjaer, V. G. (2023). Reliability of three versus five saliva sampling times for assessing the cortisol awakening response. Psychoneuroendocrinology, 147, 105950. [Google Scholar] [CrossRef]
- Noushad, S., Ahmed, S., Ansari, B., Mustafa, U.-H., Saleem, Y., & Hazrat, H. (2021). Physiological biomarkers of chronic stress: A systematic review. International Journal of Health Sciences, 15(5), 46–59. [Google Scholar]
- O’Byrne, N. A., Yuen, F., Butt, W. Z., & Liu, P. Y. (2021). Sleep and circadian regulation of cortisol: A short review. Current Opinion in Endocrine and Metabolic Research, 18, 178–186. [Google Scholar] [CrossRef]
- Paredes-Céspedes, D. M., Vélez, N., Parada-López, A., Toloza-Pérez, Y. G., Téllez, E. M., Portilla, C., González, C., Blandón, L., Santacruz, J. C., & Malagón-Rojas, J. (2024). The effects of nature exposure therapies on stress, depression, and anxiety levels: A systematic review. European Journal of Investigation in Health, Psychology and Education, 14(3), 609–622. [Google Scholar] [CrossRef]
- Park, B. J., Tsunetsugu, Y., Kasetani, T., Kagawa, T., & Miyazaki, Y. (2010). The physiological effects of shinrin-yoku (taking in the forest atmosphere or forest bathing): Evidence from field experiments in 24 forests across Japan. Environmental Health and Preventive Medicine, 15(1), 18–26. [Google Scholar] [CrossRef]
- Park, S., Lee, J.-K., & Jee, Y.-S. (2022). Influence of aerobic exercise combined with forest bathing on immunocytes, stress hormones, VO2peak, and body composition in elderly men: A randomized controlled trial. Journal of Men’s Health, 18(7), 1–14. [Google Scholar] [CrossRef]
- Peterfalvi, A., Meggyes, M., Makszin, L., Farkas, N., Miko, E., Miseta, A., & Szereday, L. (2021). Forest bathing always makes sense: Blood pressure-lowering and immune system-balancing effects in late spring and winter in central Europe. International Journal of Environmental Research and Public Health, 18(4), 2067. [Google Scholar] [CrossRef]
- Pratiwi, P., Xiang, Q., & Xie, Z. (2024). Physiological and psychological effects of walking in and viewing autumn forests in urban park in Japanese and Indonesian adults. IOP Conference Series: Earth and Environmental Science, 1384(1), 012014. [Google Scholar] [CrossRef]
- Rajcani, J., Vytykacova, S., Solarikova, P., & Brezina, I. (2021). Stress and hair cortisol concentrations in nurses during the first wave of the COVID-19 pandemic. Psychoneuroendocrinology, 129, 105245. [Google Scholar] [CrossRef] [PubMed]
- Rajoo, K. S., Karam, D. S., & Abdullah, M. Z. (2020). The physiological and psychosocial effects of forest therapy: A systematic review. Urban Forestry & Urban Greening, 54, 126744. [Google Scholar] [CrossRef]
- Ranganathan, P., & Aggarwal, R. (2019). Study designs: Part 3—Analytical observational studies. Perspectives in Clinical Research, 10(2), 91. [Google Scholar] [CrossRef] [PubMed]
- Razai, M. S., Kooner, P., & Majeed, A. (2023). Strategies and interventions to improve healthcare professionals’ well-being and reduce burnout. Journal of Primary Care & Community Health, 14, 21501319231178641. [Google Scholar] [CrossRef]
- Rhee, J. H., Schermer, B., Han, G., Park, S. Y., & Lee, K. H. (2023). Effects of nature on restorative and cognitive benefits in indoor environment. Scientific Reports, 13(1), 13199. [Google Scholar] [CrossRef]
- Rink, L. C., Oyesanya, T. O., Adair, K. C., Humphreys, J. C., Silva, S. G., & Sexton, J. B. (2023). Stressors among healthcare workers: A summative content analysis. Global Qualitative Nursing Research, 10, 23333936231161127. [Google Scholar] [CrossRef]
- Salari, N., Khazaie, H., Hosseinian-Far, A., Khaledi-Paveh, B., Kazeminia, M., Mohammadi, M., Shohaimi, S., Daneshkhah, A., & Eskandari, S. (2020). The prevalence of stress, anxiety and depression within front-line healthcare workers caring for COVID-19 patients: A systematic review and meta-regression. Human Resources for Health, 18(1), 100. [Google Scholar] [CrossRef]
- Santacruz, J. C., & Blandón, L. (2020). El cuidado como estilo de vida para corazones responsables. Fundación Colombiana del Corazón. [Google Scholar]
- Schulz, A., Larra, M. F., Vögele, C., Kölsch, M., & Schächinger, H. (2023). The relationship between self-reported chronic stress, physiological stress axis dysregulation and medically-unexplained symptoms. Biological Psychology, 183, 108690. [Google Scholar] [CrossRef]
- Shirazi, A., Brody, A. L., Soltani, M., & Lang, A. J. (2025). Recovery horizons: Nature-based activities as adjunctive treatments for co-occurring post-traumatic stress disorder and substance use disorders. American Journal of Lifestyle Medicine, 19(4), 626–638. [Google Scholar] [CrossRef]
- Silove, D., Nickerson, A., & Bryant, R. A. (2008). Specific mental health disorders: Trauma and mental disorders. In International encyclopedia of public health (pp. 196–201). Elsevier. [Google Scholar] [CrossRef]
- Smyth, N., Rossi, E., & Wood, C. (2020). Effectiveness of stress-relieving strategies in regulating patterns of cortisol secretion and promoting brain health. In International review of neurobiology (Vol. 150, pp. 219–246). Elsevier. [Google Scholar] [CrossRef]
- Stalder, T., Kirschbaum, C., Kudielka, B. M., Adam, E. K., Pruessner, J. C., Wüst, S., Dockray, S., Smyth, N., Evans, P., Hellhammer, D. H., Miller, R., Wetherell, M. A., Lupien, S. J., & Clow, A. (2016). Assessment of the cortisol awakening response: Expert consensus guidelines. Psychoneuroendocrinology, 63, 414–432. [Google Scholar] [CrossRef]
- Stalder, T., Lupien, S. J., Kudielka, B. M., Adam, E. K., Pruessner, J. C., Wüst, S., Dockray, S., Smyth, N., Evans, P., Kirschbaum, C., Miller, R., Wetherell, M. A., Finke, J. B., Klucken, T., & Clow, A. (2022). Evaluation and update of the expert consensus guidelines for the assessment of the cortisol awakening response (CAR). Psychoneuroendocrinology, 146, 105946. [Google Scholar] [CrossRef] [PubMed]
- Stalder, T., Oster, H., Abelson, J. L., Huthsteiner, K., Klucken, T., & Clow, A. (2025). The Cortisol Awakening Response: Regulation and Functional Significance. Endocrine Reviews, 46(1), 43–59. [Google Scholar] [CrossRef] [PubMed]
- Stier-Jarmer, M., Throner, V., Kirschneck, M., Immich, G., Frisch, D., & Schuh, A. (2021). The psychological and physical effects of forests on human health: A systematic review of systematic reviews and meta-analyses. International Journal of Environmental Research and Public Health, 18(4), 1770. [Google Scholar] [CrossRef] [PubMed]
- Takayama, N., Morikawa, T., Koga, K., Miyazaki, Y., Harada, K., Fukumoto, K., & Tsujiki, Y. (2022). Exploring the physiological and psychological effects of digital shinrin-yoku and its characteristics as a restorative environment. International Journal of Environmental Research and Public Health, 19(3), 1202. [Google Scholar] [CrossRef]
- Tomiko Yamada Da Silveira, L., Carvalho Ferreira, J., & Maria Patino, C. (2023). Mixed-effects model: A useful statistical tool for longitudinal and cluster studies. Jornal Brasileiro de Pneumologia, e20230137. [Google Scholar] [CrossRef]
- Torres, L. H. S. F., Medeiros, Y. K. M., De Sousa, G. M., Vargas, H. Q., De Menezes Galvão, A. C., De Almeida, R. N., Leocadio-Miguel, M., Lobão-Soares, B., Palhano-Fontes, F., De Araujo, D. B., & Galvão-Coelho, N. L. (2024). Use of sleep quality questionary and cortisol awakening response as complementary tools for the evaluation of major depression progression. Current Psychology, 43(22), 19820–19829. [Google Scholar] [CrossRef]
- UTEM. (2020). Guía para la práctica del shinrin yoku en áreas silvestres protegidas del estado. Universidad Tecnológica Metropolitana (UTEM). Available online: https://warnercnr.colostate.edu/wp-content/uploads/sites/2/2021/06/GUIA-PARA-LA-PRACTICA-DE-SHINRIN-YOKU-2020.pdf (accessed on 10 April 2025).
- Vega-Valero, C. Z., Ruíz-Méndez, D., Nava-Quiroz, C. N., Vega-Valero, C. Z., Ruíz-Méndez, D., & Nava-Quiroz, C. N. (2019). Una propuesta de adaptación del cuestionario de síntomas de fatiga laboral. Revista de psicología y ciencias del comportamiento de la Unidad Académica de Ciencias Jurídicas y Sociales, 10(1), 74–86. [Google Scholar] [CrossRef]
- White, M. P., Alcock, I., Grellier, J., Wheeler, B. W., Hartig, T., Warber, S. L., Bone, A., Depledge, M. H., & Fleming, L. E. (2019). Spending at least 120 minutes a week in nature is associated with good health and wellbeing. Scientific Reports, 9(1), 7730. [Google Scholar] [CrossRef]
- WHO. (2022). Occupational health: Health workers. World Health Organization. Available online: https://www.who.int/news-room/fact-sheets/detail/occupational-health--health-workers (accessed on 10 April 2025).
- WIN. (2024). Stress levels rise around the world—Win worldwide independent network of market research and opinion poll. Worldwide Independent Network of Market Research. Available online: https://winmr.com/stress-levels-rise-around-the-world/ (accessed on 10 April 2025).
- Yang, Y., Kim, H., Kang, M., Baik, H., Choi, Y., Jang, E.-J., Chang, E.-J., Yun, S., Park, M., Park, E., Yun, H., Lee, T.-J., Kwon, Y.-H., Hong, K.-P., Lee, A.-R., Jung, S., Ahn, T.-H., Jin, H.-Y., & Choi, K.-H. (2023). The effectiveness of nature-based therapy for community psychological distress and well-being during COVID-19: A multi-site trial. Scientific Reports, 13(1), 22370. [Google Scholar] [CrossRef]
- Ye, X., Dou, Z., Jiang, M., Luo, Z., Li, M., Tang, H., Huang, X., Wang, Y., Dong, L., Mao, X., & Feng, Y. (2023). Effects of Linpan nature therapy on health benefits in older women with and without hypertension. Frontiers in Public Health, 11, 1208481. [Google Scholar] [CrossRef]
- Zabini, F., Albanese, L., Becheri, F. R., Gavazzi, G., Giganti, F., Giovanelli, F., Gronchi, G., Guazzini, A., Laurino, M., Li, Q., Marzi, T., Mastorci, F., Meneguzzo, F., Righi, S., & Viggiano, M. P. (2020). Comparative study of the restorative effects of forest and urban videos during COVID-19 lockdown: Intrinsic and benchmark values. International Journal of Environmental Research and Public Health, 17(21), 8011. [Google Scholar] [CrossRef] [PubMed]
- Zhu, J., Sun, L., Zhang, L., Wang, H., Fan, A., Yang, B., Li, W., & Xiao, S. (2020). Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Frontiers in Psychiatry, 11, 386. [Google Scholar] [CrossRef] [PubMed]

| Parameters | Metropolitan Parks Group | Urban Forest Group | Control Group | p | |
|---|---|---|---|---|---|
| Total population | 30 | 27 | 25 | ||
| Sex [n (%)] | Male | 4 (13.33) | 5 (18.52) | 7 (28.00) | 0.39 |
| Female | 26 (86.67) | 22 (81.48) | 18 (72.00) | ||
| Age (years) [mean (SD)] | 43.77 (10.94) | 44.30 (9.50) | 40.04 (9.32) | 0.21 | |
| BMI (kg/m2) [n (%)] | 0.22 | ||||
| Underweight | 1 (3.33) | 1 (3.70) | -- | ||
| Normal weight | 20 (66.67) | 14 (51.85) | 17 (73.91) | ||
| Overweight | 6 (20.00) | 12 (44.44) | 5 (21.74) | ||
| Obese | 3 (10.00) | -- | 1 (4.35) | ||
| Current Smoking [n (%)] | 2 (6.67) | 1 (3.70) | -- | 0.34 | |
| Alcohol consumption [n (%)] | 11 (36.67) | 13 (48.15) | 6 (24.00) | ||
| Current physical activity [n (%)] | 15 (53.57) | 15 (55.56) | 12 (75.00) | ||
| Employer institution [n (%)] | 0.68 | ||||
| Institution A | 14 (46.67) | 10 (37.04) | 12 (48.00) | ||
| Institution B | 16 (53.33) | 17 (62.96) | 13 (52.00) | ||
| Job activity profile [n (%)] | 0.39 | ||||
| Job that primarily involves sitting | 12 (42.86) | 14 (51.85) | 11 (68.75) | ||
| Job that requires a lot of walking | 8 (28.57) | 9 (33.33) | 4 (25.00) | ||
| Job that involves both walking and heavy lifting | 6 (21.43) | 2 (7.41) | -- | ||
| Physically demanding job | 2 (7.14) | 2 (7.41) | 1 (6.25) | ||
| Tenure in the current job [n (%)] | 0.31 | ||||
| 0–6 months | -- | 1 (3.70) | -- | ||
| >6–12 months | 3 (10.71) | -- | 1 (6.25) | ||
| >12–36 months | 1 (3.57) | 3 (11.11) | -- | ||
| >36 months | 24 (85.71) | 23 (85.19) | 15 (93.75) | ||
| Experimental Group Metropolitan Parks | Experimental Group Urban Forest | Control Group | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Scale | Baseline Mean (SD) | Month 3 Mean (SD) | p Value | Month 6 Mean (SD) | p Value | Baseline Mean (SD) | Month 3 Mean (SD) | p Value | Month 6 Mean (SD) | p Value | Baseline Mean (SD) | Month 3 Mean (SD) | p Value | Month 6 Mean (SD) | p Value | |
| PSS-14 | 23.27 (10.03) | 19.40 (10.23) | 0.03 | 18.43 (10.81) | 0.03 | 23.04 (8.56) | 21.38 (8.26) | >0.05 | 17.92 (5.95) | 0.01 | 21.43 (9.50) | 20.84 (8.85) | >0.05 | 19.75 (9.75) | >0.05 | |
| STAI | State | 21.17 (12.12) | 18.00 (10.98) | 0.05 | 17.67 (11.58) | 0.05 | 21.3 (11.59) | 20.50 (9.82) | >0.05 | 14.31 (8.61) | <0.01 | 19.61 (11.90) | 20.6 (12.28) | >0.05 | 18.70 (13.42) | >0.05 |
| Trait | 21.50 (10.06) | 19.70 (9.66) | >0.05 | 18.27 (12.64) | 0.01 | 20.5 (10.23) | 19.35 (10.62) | >0.05 | 14.58 (9.23) | <0.01 | 18.17 (8.87) | 20.0 (11.55) | >0.05 | 17.60 (10.89) | >0.05 | |
| Pittsburgh | Sleep efficiency | 10.00 (10.44) | 10.00 (12.17) | >0.05 | 10.00 (9.84) | >0.05 | 9.00 (9.84) | 8.66 (10.97) | >0.05 | 8.66 (11.55) | >0.05 | 7.66 (8.96) | 6.33 (7.09) | >0.05 | 6.66 (9.07) | >0.05 |
| Sleep duration | 10.00 (9.64) | 10.00 (7.00) | >0.05 | 10.00 (7.93) | >0.05 | 9.00 (6.08) | 8.66 (7.23) | >0.05 | 8.66 (10.79) | >0.05 | 7.66 (6.35) | 6.33 (4.93) | >0.05 | 10.00 (11.31) | >0.05 | |
| Sleep disturbance | 10.00 (14.00) | 10.00 (13.89) | >0.05 | 10.00 (13.89) | >0.05 | 9.00 (13.00) | 8.66 (15.01) | >0.05 | 8.66 (14.15) | >0.05 | 7.66 (10.69) | 6.33 (9.23) | >0.05 | 6.66 (9.81) | >0.05 | |
| Sleep latency | 10.00 (14.80) | 10.00 (14.73) | >0.05 | 10.00 (15.59) | >0.05 | 9.00 (12.17) | 8.66 (12.50) | >0.05 | 8.66 (14.15) | >0.05 | 7.66 (11.55) | 6.33 (8.38) | >0.05 | 6.66 (9.81) | >0.05 | |
| Sleep quality | 10.00 (4.00) | 10.00 (5.19) | >0.05 | 10.00 (2.64) | >0.05 | 9.00 (1.00) | 8.66 (3.05) | >0.05 | 8.66 (5.03) | >0.05 | 7.66 (0.57) | 6.33 (3.05) | >0.05 | 6.66 (2.08) | >0.05 | |
| Use of sleep medication | 10.00 (7.93) | 10.00 (7.93) | >0.05 | 10.00 (8.71) | >0.05 | 9.00 (7.81) | 8.66 (7.37) | >0.05 | 8.66 (9.86) | >0.05 | 7.66 (12.42) | 6.33 (9.23) | >0.05 | 6.66 (9.81) | >0.05 | |
| Sleep dysfunction | 10.00 (10.82) | 10.00 (11.36) | >0.05 | 10.00 (10.58) | >0.05 | 9.00 (9.16) | 8.66 (7.09) | >0.05 | 8.66 (10.97) | >0.05 | 7.66 (8.14) | 6.33 (6.02) | >0.05 | 6.66 (4.16) | >0.05 | |
| Yoshitake | General fatigue | 55.67 (26.87) | 43.33 (23.97) | >0.05 | 34.67 (27.76) | <0.01 | 40.00 (27.46) | 34.23 (27.01) | 0.05 | 16.92 (19.55) | <0.01 | 43.48 (28.22) | 40.53 (31.18) | >0.05 | 33.50 (25.60) | >0.05 |
| Physical fatigue | 32.00 (26.31) | 29.33 (27.53) | >0.05 | 24.33 (25.69) | 0.05 | 42.59 (30.83) | 31.15 (27.90) | <0.01 | 15.00 (13.64) | <0.01 | 23.04 (22.04) | 27.89 (26.58) | >0.05 | 19.00 (24.69) | >0.05 | |
| Mental fatigue | 34.00 (21.11) | 26.33 (22.36) | >0.05 | 26.33 (22.36) | >0.05 | 31.85 (22.88) | 18.85 (17.51) | <0.01 | 9.23 (13.24) | <0.01 | 23.04 (20.77) | 23.6 (20.60) | >0.05 | 15.00 (22.59) | >0.05 | |
| Variable | PSS-14 | STAI–State | STAI–Trait | Pittsburgh | Yoshitake | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | β | 95% CI | p | |
| Sex | |||||||||||||||
| Female | 3.60 | −1.85, 9.05 | 0.192 | 6.74 | 0.16, 13.32 | 0.045 | 1.60 | −5.15, 8.35 | 0.638 | 2.26 | 0.15, 4.38 | 0.036 | 12.67 | −1.96, 27.29 | 0.088 |
| Group × Institution | |||||||||||||||
| 1 × 1 | 2.39 | −6.07, 10.84 | 0.575 | −1.12 | −11.33, 9.08 | 0.827 | 2.46 | −8.01, 12.93 | 0.641 | 2.98 | −0.30, 6.26 | 0.074 | −5.90 | −28.58, 16.78 | 0.605 |
| 1 × 2 | 0.80 | −7.47, 9.07 | 0.847 | 3.45 | −6.53, 13.44 | 0.493 | 2.61 | −7.63, 12.85 | 0.613 | 0.43 | −2.77, 3.64 | 0.789 | −7.74 | −29.93, 14.45 | 0.489 |
| 2 × 1 | 2.69 | −6.30, 11.68 | 0.553 | −0.07 | −10.93, 10.78 | 0.989 | 1.31 | −9.82, 12.45 | 0.814 | 2.15 | −1.34, 5.63 | 0.224 | −20.97 | −45.10, 3.16 | 0.087 |
| 2 × 2 | 0.34 | −7.95, 8.63 | 0.935 | −2.63 | −12.63, 7.38 | 0.602 | −2.54 | −12.81, 7.72 | 0.623 | −1.11 | −4.33, 2.10 | 0.491 | −25.70 | −47.93, −3.46 | 0.024 |
| Variable | Coefficient | 95% CI | p |
|---|---|---|---|
| Groupxtime | |||
| Control | 1.20 | 0.11, 2.28 | 0.03 |
| Parks | 1.70 | 072, 2.67 | <0.01 |
| Forest | 1.74 | 0.73, 2.76 | <0.01 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the University Association of Education and Psychology. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vélez, N.; Paredes-Céspedes, D.M.; Cruz-Pérez, A.; López, R.; Parada-López, A.; Téllez-Ávila, E.M.; Rodríguez de Silva, P.; Munevar, A.; Rodríguez González, D.M.; Fuquen, P.; et al. Promoting Healthy Organizations Through Urban Nature: Psychological and Physiological Effects in Healthcare Workers. Eur. J. Investig. Health Psychol. Educ. 2025, 15, 159. https://doi.org/10.3390/ejihpe15080159
Vélez N, Paredes-Céspedes DM, Cruz-Pérez A, López R, Parada-López A, Téllez-Ávila EM, Rodríguez de Silva P, Munevar A, Rodríguez González DM, Fuquen P, et al. Promoting Healthy Organizations Through Urban Nature: Psychological and Physiological Effects in Healthcare Workers. European Journal of Investigation in Health, Psychology and Education. 2025; 15(8):159. https://doi.org/10.3390/ejihpe15080159
Chicago/Turabian StyleVélez, Norida, Diana Marcela Paredes-Céspedes, Angélica Cruz-Pérez, Ronald López, Alejandra Parada-López, Eliana M. Téllez-Ávila, Paola Rodríguez de Silva, Ana Munevar, Diana Marcela Rodríguez González, Paola Fuquen, and et al. 2025. "Promoting Healthy Organizations Through Urban Nature: Psychological and Physiological Effects in Healthcare Workers" European Journal of Investigation in Health, Psychology and Education 15, no. 8: 159. https://doi.org/10.3390/ejihpe15080159
APA StyleVélez, N., Paredes-Céspedes, D. M., Cruz-Pérez, A., López, R., Parada-López, A., Téllez-Ávila, E. M., Rodríguez de Silva, P., Munevar, A., Rodríguez González, D. M., Fuquen, P., Santacruz, J. C., & Malagón-Rojas, J. (2025). Promoting Healthy Organizations Through Urban Nature: Psychological and Physiological Effects in Healthcare Workers. European Journal of Investigation in Health, Psychology and Education, 15(8), 159. https://doi.org/10.3390/ejihpe15080159










