Design and Transition of an Emergency E-Learning Pathology Course for Medical Students—Evaluation of a Novel Course Concept
Abstract
1. Introduction
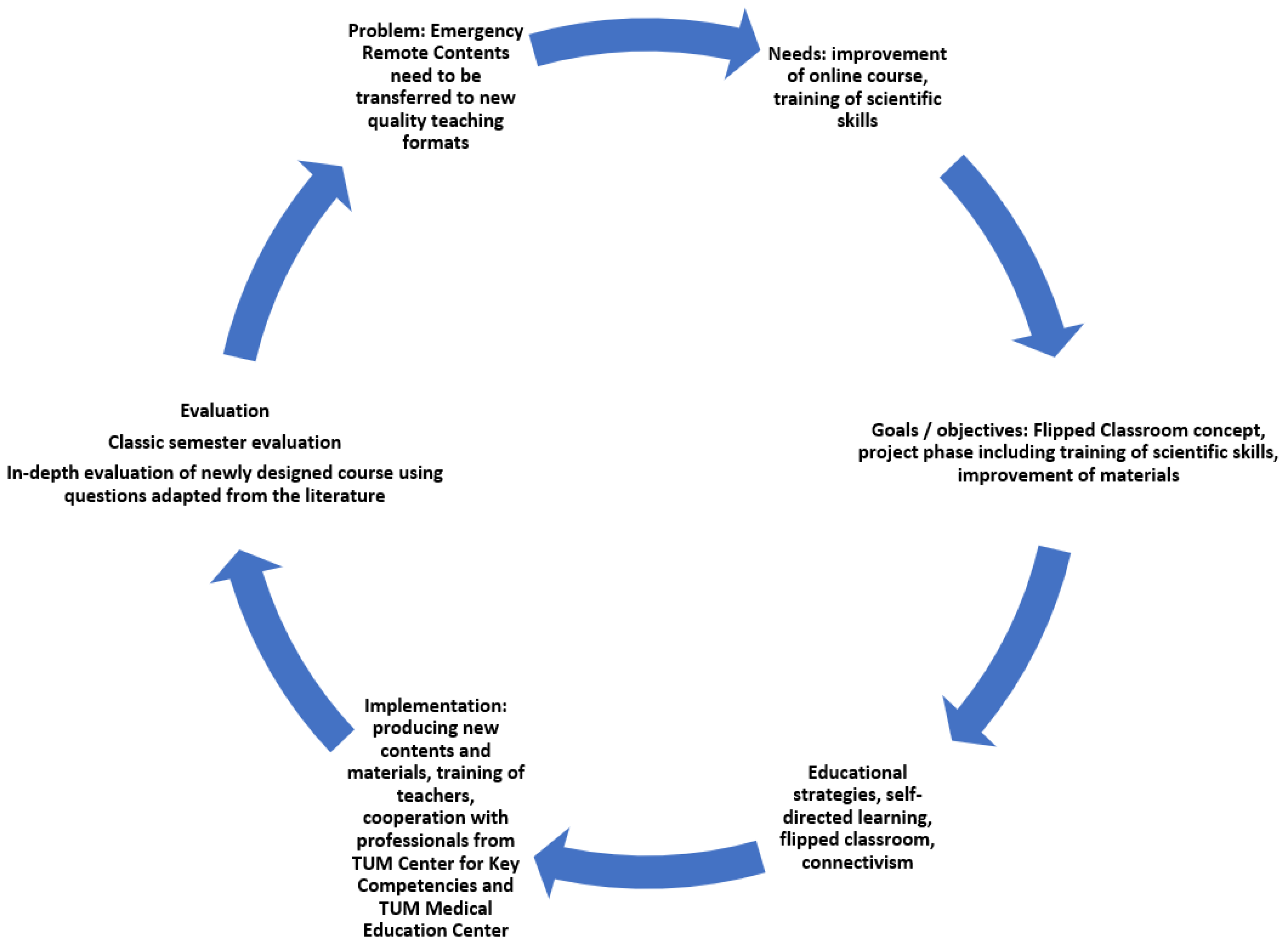
2. Materials and Methods
2.1. Course Development
2.1.1. Phase 1: Emergency Remote Education [5] Concept (“DigiPath”), Summer Semester 2020
2.1.2. Phase 2: Flipped Classroom Concept, Winter Semester 2020/2021
Flipped Classroom Concept, Part 1: Asynchronous E-Learning Module “DigiPath”
Flipped Classroom Concept, Part 2: Project Phase (“Projects in Pathology”)
2.2. Ethics, Informed Consent
2.3. Surveys and Evaluation
2.4. Statistics
3. Results
3.1. Participants
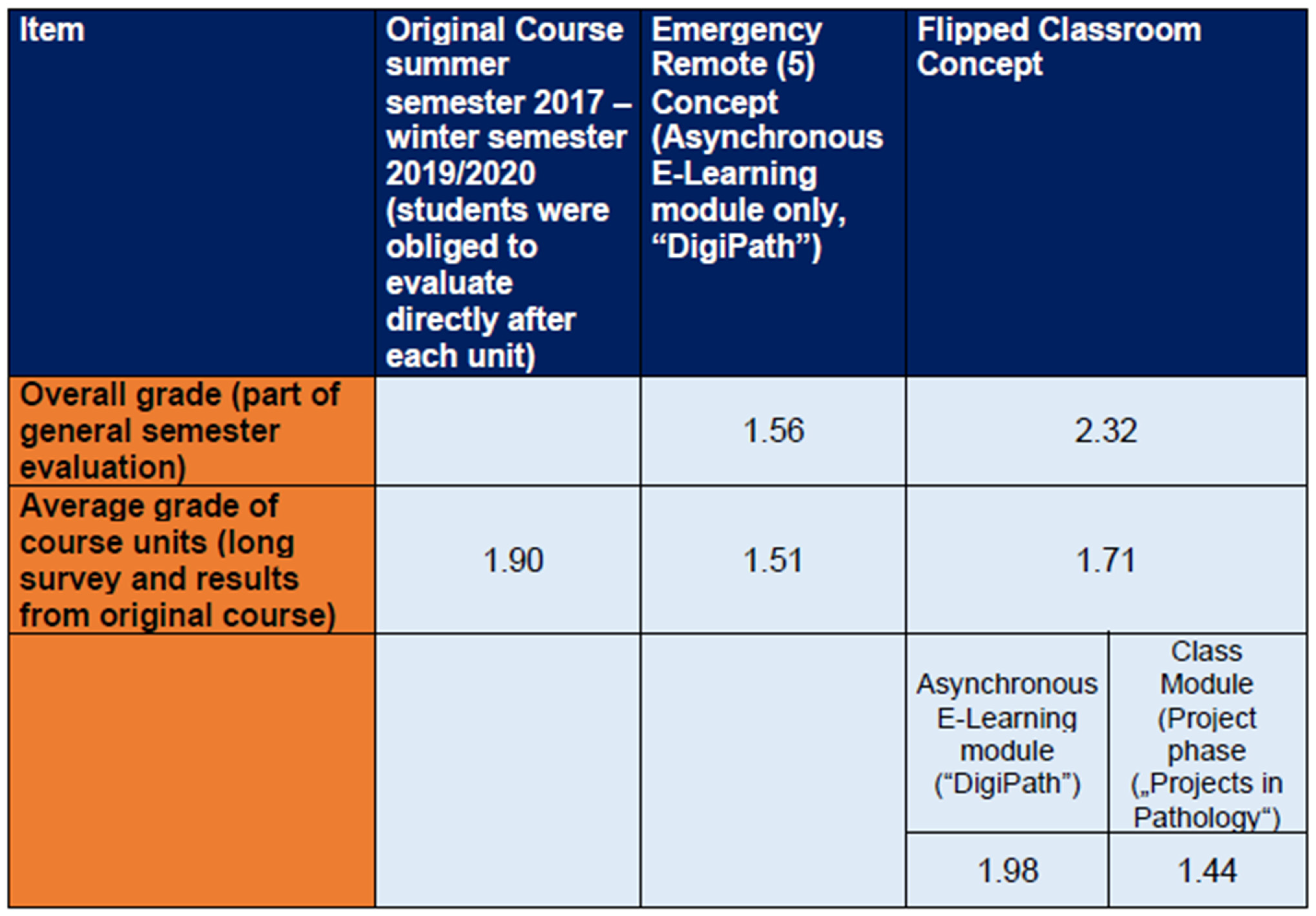
3.2. Overall Satisfaction
3.3. Asynchronous E-Learning Module—“DigiPath”
3.3.1. Satisfaction with Different Teaching Materials
“Even though I wouldn’t say that I didn’t understand [the topics], I took significantly less with me when only slides were uploaded”.
“Some lecturers presented their material in a screencast much more concise and shorter than it would probably have been in a lecture. That was good because it allowed the essentials to stick better and it was more exciting to listen to”.
“Overall, everything was really very clear and extremely well done. In addition because you could watch the videos when you are awake and fit (and take breaks when your concentration drops), you absorb a lot more than usual. On the contrary, I had the feeling that I had just really understood many topics.”
3.3.2. Usability and Structure
3.3.3. Clarity and Appropriateness
“I often had the feeling that I concentrate much more on the videos, because everything could potentially come up in a question. And because it’s a great feeling when you can answer the questions correctly right away!”
3.3.4. Missing of Face-to-Face Interaction
“I find the system without a final exam questionable. You only really prepare for the topics if you are asked about them in some way”.
3.3.5. Perceived Understanding
3.4. Project Phase (“Projects in Pathology”)
“I found it very helpful to have a fixed course that encourages and accompanies research so that you are not completely on your own and lost.”
4. Discussion
4.1. Creating Asynchronous Content
4.2. Transition to Seminars/Project Phase
4.3. Transition and Future
4.4. Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mian, A.; Khan, S. Medical education during pandemics: A UK perspective. BMC Med. 2020, 18, 100. [Google Scholar] [CrossRef] [PubMed]
- Mediendidaktik [Internet]. Beltz Juventa. 2012. Available online: https://www.beltz.de/fachmedien/erziehungs_und_sozialwissenschaften/enzyklopaedie_erziehungswissenschaft_online_eeo.html?tx_beltz_educationencyclopedia%5Barticle%5D=11935&tx_beltz_educationencyclopedia%5Baction%5D=article&tx_beltz_educationencyclopedia%5Bcontroller%5D=EducationEncyclopedia&cHash=f4735a442d71f4212ba4580d2bff9fb5 (accessed on 21 December 2022).
- Hew, K.F.; Lo, C.K. Flipped classroom improves student learning in health professions education: A meta-analysis. BMC Med. Educ. 2018, 18, 38. [Google Scholar] [CrossRef] [PubMed]
- Kuhn, S.; Frankenhauser, S.; Tolks, D. Digital learning and teaching in medical education: Already there or still at the beginning? Bundesgesundheitsblatt Gesundh. Gesundh. 2018, 61, 201–209. [Google Scholar] [CrossRef] [PubMed]
- Hodges, C.; Moore, S.; Lockee, B.; Trust, T.; Bond, A. The Difference between Emergency Remote Teaching and Online Learning. Educause Review. 2020. Available online: https://er.educause.edu/articles/2020/3/the-difference-between-emergency-remote-teaching-and-online-learning. (accessed on 21 December 2022).
- Eaton, M. The flipped classroom. Clin. Teach. 2017, 14, 301–302. [Google Scholar] [CrossRef] [PubMed]
- Ukrani, R.D.; Shaikh, A.N.; Martins, R.S.; Fatima, S.S.; Naseem, H.A.; Baig, M.A. Low-cost peer-taught virtual research workshops for medical students in Pakistan: A creative, scalable, and sustainable solution for student research. BMC Med. Educ. 2021, 21, 557. [Google Scholar] [CrossRef]
- Ommering, B.W.C.; van Diepen, M.; van Blankenstein, F.M.; de Jong, P.G.M.; Dekker, F.W. Twelve tips to offer a short authentic and experiential individual research opportunity to a large group of undergraduate students. Med. Teach. 2020, 42, 1128–1133. [Google Scholar] [CrossRef]
- Garg, R.; Goyal, S.; Singh, K. Lack of Research Amongst Undergraduate Medical Students in India: It’s time to Act and Act Now. Indian Pediatr. 2017, 54, 357–360. [Google Scholar] [CrossRef]
- Ommering, B.W.C.; van Blankenstein, F.M.; Waaijer, C.J.F.; Dekker, F.W. Future physician-scientists: Could we catch them young? Factors influencing intrinsic and extrinsic motivation for research among first-year medical students. Perspect. Med. Educ. 2018, 7, 248–255. [Google Scholar] [CrossRef]
- Frank, J.R.; Snell, L.; Sherbino, J.; Boucher, A. CanMEDS 2015; Physician Competency Framework Series I; Collège Royal des Médecins et Chirurgiens du Canada: Ottawa, ONT, Canada, 2015. [Google Scholar]
- Bundesministerium fuer Bildung und Forschung. Masterplan Medizinstudium 2020 Berlin, Germany. Available online: https://www.bmbf.de/de/masterplan-medizinstudium-2020-4024.html (accessed on 21 December 2022).
- Ha, T.C.; Ng, S.; Chen, C.; Yong, S.K.; Koh, G.C.H.; Tan, S.B.; Malhotra, R.; Altermatt, F.; Seim, A.; Biderman, A.; et al. Inclination towards research and the pursuit of a research career among medical students: An international cohort study. BMC Med. Educ. 2018, 18, 86. [Google Scholar] [CrossRef]
- Tan, S.-B.; Koh, G.C.; Ding, Y.-W.; Malhotra, R.; Ha, T.C.; Pietrobon, R.; Kusumaratna, R.; Tie, R.N.; Cunha, G.; Martins, H.; et al. Inclination towards a research career among first year medical students: An international study. South East Asian J. Med. Educ. 2011, 5, 49–59. [Google Scholar] [CrossRef]
- Ommering, B.W.; van Blankenstein, F.M.; Wijnen-Meijer, M.; van Diepen, M.; Dekker, F.W. Fostering the physician–scientist workforce: A prospective cohort study to investigate the effect of undergraduate medical students’ motivation for research on actual research involvement. BMJ Open 2019, 9, e028034. [Google Scholar] [CrossRef] [PubMed]
- Harding, C.V.; Akabas, M.H.; Andersen, O.S. History and outcomes of fifty years of physician-scientist training in medical scientist training programs. Acad. Med. J. Assoc. Am. Med. Coll. 2017, 92, 1390. [Google Scholar] [CrossRef] [PubMed]
- Weaver, A.N.; McCaw, T.R.; Fifolt, M.; Hites, L.; Lorenz, R.G. Impact of elective versus required medical school research experiences on career outcomes. J. Investig. Med. 2017, 65, 942–948. [Google Scholar] [CrossRef]
- Hall, A.K.; Mills, S.L.; Lund, P.K. Clinician–investigator training and the need to pilot new approaches to recruiting and retaining this workforce. Acad. Med. 2017, 92, 1382. [Google Scholar] [CrossRef] [PubMed]
- Goldhamer, M.E.J.; Cohen, A.P.; Bates, D.W.; Cook, E.F.; Davis, R.B.; Singer, D.E.; Simon, S.R. Protecting an endangered species: Training physicians to conduct clinical research. Acad. Med. 2009, 84, 439–445. [Google Scholar] [CrossRef]
- Green, E.P.; Borkan, J.M.; Pross, S.H.; Adler, S.R.; Nothnagle, M.; Parsonnet, J.; Gruppuso, P.A. Encouraging scholarship: Medical school programs to promote student inquiry beyond the traditional medical curriculum. Acad. Med. 2010, 85, 409–418. [Google Scholar] [CrossRef]
- Ommering, B.W.; van den Elsen, P.J.; van der Zee, J.; Jost, C.R.; Dekker, F.W. Using an extracurricular honors program to engage future physicians into scientific research in early stages of medical training. Medical science educator. 2018, 28, 451–455. [Google Scholar] [CrossRef]
- Laskowitz, D.T.; Drucker, R.P.; Parsonnet, J.; Cross, P.C.; Gesundheit, N. Engaging students in dedicated research and scholarship during medical school: The long-term experiences at Duke and Stanford. Acad. Med. 2010, 85, 419–428. [Google Scholar] [CrossRef]
- Wolfson, R.K.; Alberson, K.; McGinty, M.; Schwanz, K.; Dickins, K.; Arora, V.M. The impact of a scholarly concentration program on student interest in career-long research: A longitudinal study. Acad. Med. 2017, 92, 1196–1203. [Google Scholar] [CrossRef]
- Kaufman, D.M.; Mann, K.V. Teaching and learning in medical education: How theory can inform practice. In Understanding Medical Education: Evidence, Theory, and Practice; Wiley: New York, NY, USA, 2018. [Google Scholar]
- Vereijken, M.W.C.; Van Der Rijst, R.M.; Van Driel, J.H.; Dekker, F.W. Authentic research practices throughout the curriculum in undergraduate medical education: Student beliefs and perceptions. Innov. Educ. Teach. Int. 2020, 57, 532–542. [Google Scholar] [CrossRef]
- Ryan, R.M.; Deci, E.L. Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am. Psychol. 2000, 55, 68. [Google Scholar] [CrossRef] [PubMed]
- Swanwick, T. Understanding medical education. In Understanding Medical Education: Evidence, Theory, and Practice; Wiley: New York, NY, USA, 2018; pp. 1–6. [Google Scholar]
- Manou, E.; Lazari, E.C.; Thomopoulou, G.E.; Agrogiannis, G.; Kavantzas, N.; Lazaris, A.C. Participation and Interactivity in Synchronous E-Learning Pathology Course During the COVID-19 Pandemic. Adv. Med. Educ. Pract. 2021, 12, 1081–1091. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, T.; Fallar, R.; Polydorides, A.D. Outcomes of Remote Pathology Instruction in Student Performance and Course Evaluation. Acad. Pathol. 2021, 8, 23742895211061822. [Google Scholar] [CrossRef] [PubMed]
- Jones, R.M. Online teaching of forensic medicine and pathology during the COVID-19 pandemic: A course evaluation. J. Forensic Leg. Med. 2021, 83, 102229. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.F.; Cecchini, M.J. Implementing a structured digital-based online pathology curriculum for trainees at the time of COVID-19. J. Clin. Pathol. 2020, 73, 444. [Google Scholar] [CrossRef] [PubMed]
- Moodle Pty Ltd. Moodle: West Perth, Australia, 2022.
- Zoom Video Communications Inc. Zoom: San José, CA, USA, 2022.
- Kern, D.E. Overview. In Curriculum Development: A Six-Step Approach for Medical Education; Thomas, P.A., Kern, D.E., Hughes, M.T., Chen, B.Y., Eds.; Johns Hopkins University Press: Baltimore, MD, USA, 2016. [Google Scholar]
- Laidlaw, A.; Guild, S.; Struthers, J. Graduate attributes in the disciplines of Medicine, Dentistry and Veterinary Medicine: A survey of expert opinions. BMC Med. Educ. 2009, 9, 28. [Google Scholar] [CrossRef]
- Barrows, H.S. A taxonomy of problem-based learning methods. Med. Educ. 1986, 20, 481–486. [Google Scholar] [CrossRef]
- Laidlaw, A.; Aiton, J.; Struthers, J.; Guild, S. Developing research skills in medical students: AMEE Guide No. 69. Med. Teach. 2012, 34, e754–e771. [Google Scholar] [CrossRef]
- Bandura, A. Social Foundations of Thought and Action; Prentice-Hall, Inc.: Englewood Cliffs, NJ, USA, 1986. [Google Scholar]
- Bertram, D. Likert Scales Are the Meaning of Life: Academia.edu. Available online: https://www.academia.edu/8160815/Likert_Scales_are_the_meaning_of_life (accessed on 21 December 2022).
- Liu, C.; Scott, K.M.; Lim, R.L.; Taylor, S.; Calvo, R.A. EQClinic: A platform for learning communication skills in clinical consultations. Med. Educ. Online 2016, 21, 31801. [Google Scholar] [CrossRef]
- Lewis, J.R. IBM computer usability satisfaction questionnaires: Psychometric evaluation and instructions for use. Int. J. Hum.–Comput. Interact. 1995, 7, 57–78. [Google Scholar] [CrossRef]
- Herrmann, J. Evaluation von E-Learning; Uo, G., Ed.; Koordinationsstelle Multimedia (KOMM) am HRZ der JLU Gießen: Giessen, Germany, 2009. [Google Scholar]
- JASP Team. JASP. 0.14.1 ed; Department of Psychological Methods, University of Amsterdam: Amsterdam, The Netherlands.
- Halter, C. Quantitative Analysis with JASP Open-Source Software 2020.
- Goh, P.-S.; Sandars, J. A vision of the use of technology in medical education after the COVID-19 pandemic. MedEdPublish 2020, 9, 49. [Google Scholar] [CrossRef]
- van der Keylen, P.; Lippert, N.; Kunisch, R.; Kühlein, T.; Roos, M. Asynchronous, digital teaching in times of COVID-19: A teaching example from general practice. GMS J. Med. Educ. 2020, 37, Doc98. [Google Scholar]
- Fabriz, S.; Mendzheritskaya, J.; Stehle, S. Impact of Synchronous and Asynchronous Settings of Online Teaching and Learning in Higher Education on Students’ Learning Experience During COVID-19. Front. Psychol. 2021, 12, 733554. [Google Scholar] [CrossRef]
- Gholami, M.; Fawad, I.; Shadan, S.; Rowaiee, R.; Ghanem, H.; Hassan Khamis, A.; Ho, S.B. COVID-19 and healthcare workers: A systematic review and meta-analysis. Int. J. Infect. Dis. 2021, 104, 335–346. [Google Scholar] [CrossRef] [PubMed]
- O’Byrne, L.; Gavin, B.; McNicholas, F. Medical students and COVID-19: The need for pandemic preparedness. J. Med. Ethics 2020, 46, 623–626. [Google Scholar] [CrossRef] [PubMed]
- Woodruff, A.E.; Jensen, M.; Loeffler, W.; Avery, L. Advanced screencasting with embedded assessments in pathophysiology and therapeutics course modules. Am. J. Pharm. Educ. 2014, 78, 128. [Google Scholar] [CrossRef] [PubMed]
- Bennett, C. How long should an e-learning course be? eLearn 2007, 2007, 2. [Google Scholar] [CrossRef]
- Chatterjee, D.; Corral, J. How to Write Well-Defined Learning Objectives. J. Educ. Perioper. Med. 2017, 19, E610. [Google Scholar]
- Wass, V.; Van der Vleuten, C.; Shatzer, J.; Jones, R. Assessment of clinical competence. Lancet 2001, 357, 945–949. [Google Scholar] [CrossRef]
- Lafleur, A.; Rousseau-Gagnon, M.; Côté-Maheux, M.; Tremblay-Laroche, D.; René De Cotret, P.; Caumartin, Y. Three Weeks of Team-Based Leaning Do Not Overload Undergraduate Students. Med. Sci. Educ. 2021, 31, 1369–1378. [Google Scholar] [CrossRef]
- O’Doherty, D.; Dromey, M.; Lougheed, J.; Hannigan, A.; Last, J.; McGrath, D. Barriers and solutions to online learning in medical education—An integrative review. BMC Med. Educ. 2018, 18, 130. [Google Scholar] [CrossRef] [PubMed]
- Rasmussen, A.; Lewis, M.; White, J. The application of wiki technology in medical education. Med. Teach. 2013, 35, 109–114. [Google Scholar] [CrossRef] [PubMed]
- Hayashi, T.; Tominaga, H.; Yamasaki, T. How to construct low cost studio for making e-Learning contents. In Proceedings of the 2006 7th International Conference on Information Technology Based Higher Education and Training, Ultimo, Australia, 10–13 July 2006. [Google Scholar]
- Bond, M.; Bedenlier, S.; Marín, V.I.; Händel, M. Emergency remote teaching in higher education: Mapping the first global online semester. Int. J. Educ. Technol. High Educ. 2021, 18, 50. [Google Scholar] [CrossRef] [PubMed]
- Kim, K.J. Project-based learning approach to increase medical student empathy. Med. Educ. Online 2020, 25, 1742965. [Google Scholar] [CrossRef] [PubMed]
- Naar, J.J.; Weaver, R.H.; Sonnier-Netto, L.; Few-Demo, A. Experiential education through project-based learning: Sex and aging. Gerontol. Geriatr. Educ. 2021, 42, 528–540. [Google Scholar] [CrossRef]
- Si, J. Course-based research experience of undergraduate medical students through project-based learning. Korean. J. Med. Educ. 2020, 32, 47–57. [Google Scholar] [CrossRef]
- Mateo, E.; Sevillano, E. Project-based learning methodology in the area of microbiology applied to undergraduate medical research. FEMS Microbiol. Lett. 2018, 365, fny129. [Google Scholar] [CrossRef] [PubMed]
- Bandura, A. Self-Efficacy: The Exercise of Control; WH Freeman and Company: New York, NY, USA, 1997. [Google Scholar]
- Siemens, G. Connectivism: A Learning Theory for the Digital Age 2005. Available online: https://www.itdl.org/Journal/Jan_05/article01.htm (accessed on 21 December 2022).
- Goldie, J.G.S. Connectivism: A knowledge learning theory for the digital age? Med. Teach. 2016, 38, 1064–1069. [Google Scholar] [CrossRef]
- Houlden, R.L.; Raja, J.B.; Collier, C.P.; Clark, A.F.; Waugh, J.M. Medical students’ perceptions of an undergraduate research elective. Med. Teach. 2004, 26, 659–661. [Google Scholar] [CrossRef] [PubMed]
- Peacock, J.G.; Grande, J.P. A flexible, preclinical, medical school curriculum increases student academic productivity and the desire to conduct future research. Biochem. Mol. Biol. Educ. 2015, 43, 384–390. [Google Scholar] [CrossRef]
- Vennemann, S.; Holzmann-Littig, C.; Marten-Mittag, B.; Vo Cong, M.; Berberat, P.; Stock, K. Short-and Long-Term Effects on Knowledge, Skills, and Attitudes About a Sonography Training Concept for Medical Students. J. Diagn. Med. Sonogr. 2020, 36, 25–29. [Google Scholar] [CrossRef]
- Benè, K.L.; Bergus, G. When learners become teachers: A review of peer teaching in medical student education. Fam. Med. 2014, 46, 783–787. [Google Scholar] [PubMed]
- Ahn, J.S.; French, A.J.; Thiessen, M.E.; Kendall, J.L. Training peer instructors for a combined ultrasound/physical exam curriculum. Teach. Learn. Med. 2014, 26, 292–295. [Google Scholar] [CrossRef] [PubMed]
- Hofmann, Y.E. 30 Minuten Projektmanagement; GABAL Verlag GmbH: Offenbach, Germany, 2011. [Google Scholar]
- Van Dick, R.; West, M.A. Teamwork, Teamdiagnose, Teamentwicklung; Hogrefe: Oxford, UK, 2014. [Google Scholar]
- Voss, R. Wissenschaftliches Arbeiten: UTB; UVK Verlag: Konstanz, Germany, 2011; ISBN 9783825287740. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Holzmann-Littig, C.; Jedlicska, N.; Wijnen-Meijer, M.; Liesche-Starnecker, F.; Schmidt-Bäse, K.; Renders, L.; Weimann, K.; Konukiewitz, B.; Schlegel, J. Design and Transition of an Emergency E-Learning Pathology Course for Medical Students—Evaluation of a Novel Course Concept. Eur. J. Investig. Health Psychol. Educ. 2023, 13, 112-129. https://doi.org/10.3390/ejihpe13010008
Holzmann-Littig C, Jedlicska N, Wijnen-Meijer M, Liesche-Starnecker F, Schmidt-Bäse K, Renders L, Weimann K, Konukiewitz B, Schlegel J. Design and Transition of an Emergency E-Learning Pathology Course for Medical Students—Evaluation of a Novel Course Concept. European Journal of Investigation in Health, Psychology and Education. 2023; 13(1):112-129. https://doi.org/10.3390/ejihpe13010008
Chicago/Turabian StyleHolzmann-Littig, Christopher, Nana Jedlicska, Marjo Wijnen-Meijer, Friederike Liesche-Starnecker, Karen Schmidt-Bäse, Lutz Renders, Katja Weimann, Björn Konukiewitz, and Jürgen Schlegel. 2023. "Design and Transition of an Emergency E-Learning Pathology Course for Medical Students—Evaluation of a Novel Course Concept" European Journal of Investigation in Health, Psychology and Education 13, no. 1: 112-129. https://doi.org/10.3390/ejihpe13010008
APA StyleHolzmann-Littig, C., Jedlicska, N., Wijnen-Meijer, M., Liesche-Starnecker, F., Schmidt-Bäse, K., Renders, L., Weimann, K., Konukiewitz, B., & Schlegel, J. (2023). Design and Transition of an Emergency E-Learning Pathology Course for Medical Students—Evaluation of a Novel Course Concept. European Journal of Investigation in Health, Psychology and Education, 13(1), 112-129. https://doi.org/10.3390/ejihpe13010008









