Sociodemographic Characteristics and Stress of People from Spain Confined by COVID-19
Abstract
1. Introduction
1.1. Stress and Confinement
1.2. Stress and Sociodemographic Factors
2. Materials and Methods
2.1. Participants
2.2. Instruments
2.3. Procedure
2.4. Data Analysis
3. Results
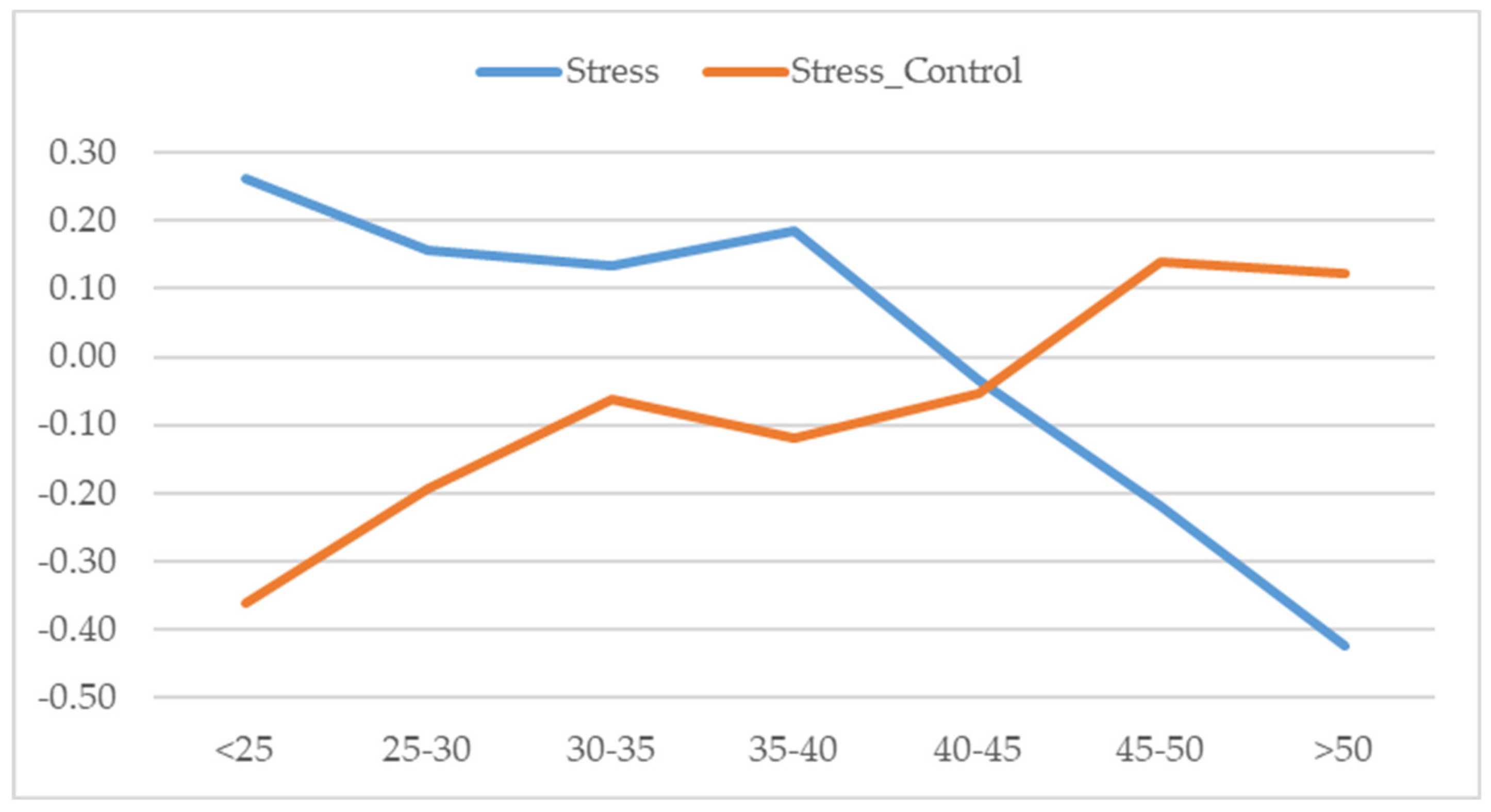
3.1. Differences in Stress According to Gender, Age, and Civil Status
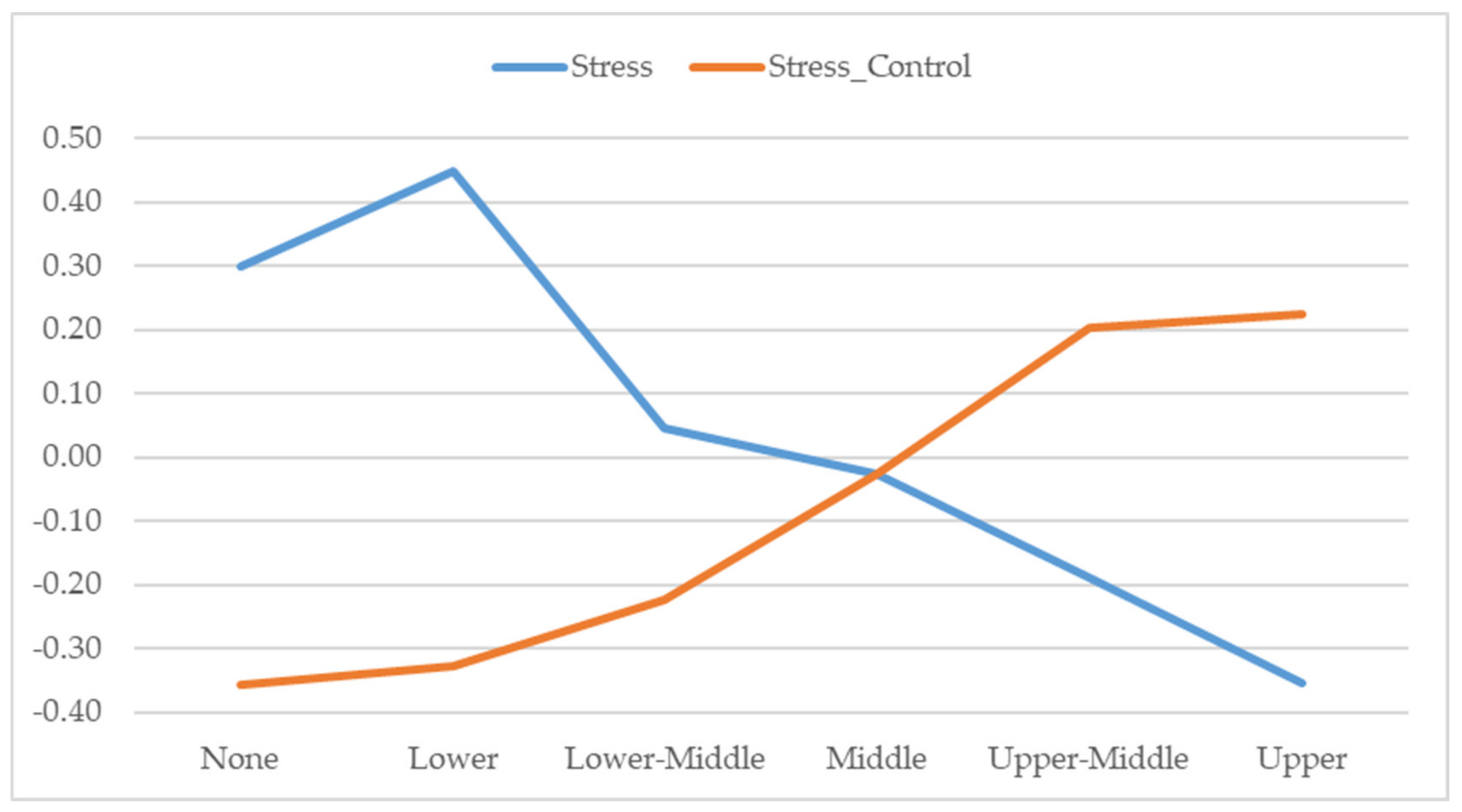
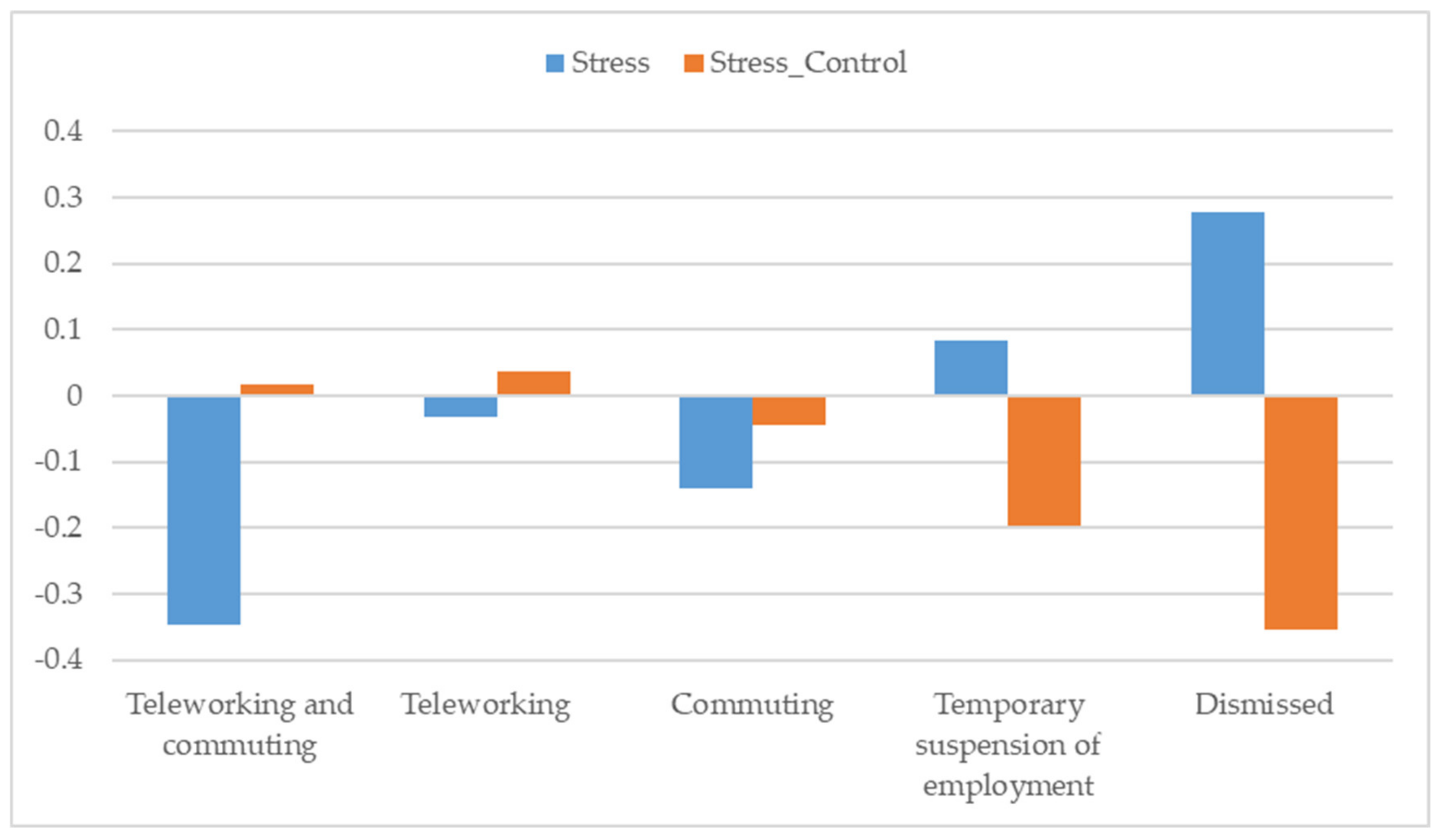
3.2. Differences in Stress by Education Level, Residence, Income, and Work Situation During Confinement
4. Discussion
5. Conclusions
- Although women reported higher levels of stress, probably due to the traditional care roles that they played in the family, they managed that stress in a similar way to men.
- In those who were over 40 years old, levels of stress were lower, and control of stress was better.
- People living in urban and rural areas reported high levels of stress, but those living in semi-urban/suburban or residential areas (with open spaces and accessible resources) reported lower levels.
- The higher the level of income, the lower the stress and the better the control of stress.
- Those who were able to combine teleworking with attending their workplace showed the lowest levels of stress.
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Wang, C.; Pan, R.; Wan, X.; Tan, Y.; Xu, L.; Ho, C.S.; Ho, R.C. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int. J. Environ. Res. Public Health 2020, 17, 1729. [Google Scholar] [CrossRef] [PubMed]
- Shigemura, J.; Ursano, R.J.; Morganstein, J.C.; Kurosawa, M.; Benedek, D.M. Public responses to the novel 2019 coronavirus (2019 – nCoV): Mental health consequences and target populations. Psychiat. Clin. Neuros 2020, 74, 281–282. [Google Scholar] [CrossRef] [PubMed]
- Zandifar, A.; Badrfam, R. Iranian mental health during the COVID-19 epidemic. Asian J. Psychiatr. 2020, 51, 101990. [Google Scholar] [CrossRef] [PubMed]
- Lei, L.; Huang, X.; Zhang, S.; Yang, J.; Yang, L.; Xu, M. Comparison of prevalence and associated factors of anxiety and depression among people affected by versus people unaffected by quarantine during the COVID-19 epidemic in southwestern China. Med. Sci. Monit. 2020, 26, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Huang, Y.; Zhao, N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: A web-based cross-sectional survey. Psychiatry Res. 2020, 288, 1–6. [Google Scholar] [CrossRef]
- Wang, Y.; Di, Y.; Ye, J.; Wei, W. Study on the public psychological states and its related factors during the outbreak of coronavirus disease 2019 (COVID-19) in some regions of China. Psychol. Health Med. 2020, 1–10. [Google Scholar] [CrossRef]
- Trujillo, M.; González-Cabrera, J. Propiedades psicométricas de la versión española de la «Escala de Estrés Percibido» (EEP). Psicol. Conduct. 2007, 15, 457–477. [Google Scholar]
- Bao, Y.; Sun, Y.; Meng, S.; Shi, J.; Lu, L. 2019-nCoV epidemic: Address mental health care to empower society. Lancet 2020, 395, e37–e38. [Google Scholar] [CrossRef]
- Kim, Y.G.; Moon, H.; Kim, S.-Y.; Lee, Y.-H.; Jeong, D.-W.; Kim, K.; Moon, J.Y.; Lee, Y.-K.; Cho, A.; Lee, H.-S.; et al. Inevitable isolation and the change of stress markers in hemodialysis patients during the 2015 MERS-CoV outbreak in Korea. Sci. Rep. 2019, 9, 1–10. [Google Scholar] [CrossRef]
- Park, C.L.; Russell, B.S.; Fendrich, M.; Finkelstein-Fox, L.; Hutchison, M.; Becker, J. Americans’ COVID-19 stress, coping, and adherence to CDC Guidelines. J. Gen. Intern. Med. 2020, 35, 1–8. [Google Scholar] [CrossRef]
- Brooks, S.K.; Webster, R.K.; Smith, L.E.; Woodland, L.; Wessely, S.; Greenberg, N.; Rubin, G.J. The psychological impact of quarantine and how to reduce it: Rapid review of the evidence. Lancet 2020, 395, 912–920. [Google Scholar] [CrossRef]
- Torales, J.; O’Higgins, M.; Castaldelli-Maia, J.M.; Ventriglio, A. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int. J. Soc. Psychiatry 2020, 66, 317–320. [Google Scholar] [CrossRef] [PubMed]
- Rajkumar, R.P. COVID-19 and mental health: A review of the existing literature. Asian J. Psychiatr. 2020, 52, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Dong, L.; Bouey, J. Public mental health crisis during COVID-19 pandemic, China. Emerg. Infect. Dis. 2020, 26, 1616–1618. [Google Scholar] [CrossRef]
- Charles, S.T.; Piazza, J.R.; Mogle, J.; Sliwinski, M.J.; Almeida, D.M. The wear and tear of daily stressors on mental health. Psychol. Sci. 2013, 24, 733–741. [Google Scholar] [CrossRef]
- De Frias, C.M.; Whyne, E. Stress on health-related quality of life in older adults: The protective nature of mindfulness. Aging Ment. Health 2015, 19, 201–206. [Google Scholar] [CrossRef]
- Piazza, J.R.; Charles, S.T.; Slwinski, M.J.; Mogle, J.; Almeida, D.M. Affective reactivity to daily stressors and long- term risk of reporting a chronic physical health condition. Ann. Behav. Med. 2003, 45, 110–120. [Google Scholar] [CrossRef]
- Lazarus, R.S. Theory-based stress measurement. Psychol. Inq. 1990, 1, 3–13. [Google Scholar] [CrossRef]
- Wheaton, M.G.; Abramowitz, J.S.; Berman, N.C.; Fabricant, L.E.; Olatunji, B.O. Psychological predictors of anxiety in response to the H1N1 (swine flu) pandemic. Cognit. Ther. Res. 2012, 36, 210–218. [Google Scholar] [CrossRef]
- Cheng, S.K.W.; Wong, C.W.; Tsang, J.; Wong, K.C. Psychological distress and negative appraisals in survivors of severe acute respiratory syndrome (SARS). Psychol. Med. 2004, 34, 1187–1195. [Google Scholar] [CrossRef]
- Asmundson, G.J.G.; Taylor, S. Coronaphobia: Fear and the 2019-nCoV outbreak. J. Anxiety Disord. 2020, 70, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Asmundson, G.J.G.; Taylor, S. How health anxiety influences responses to viral outbreaks like COVID-19: What all decision-makers, health authorities, and health care professionals need to know. J. Anxiety Disord. 2020, 71, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Park, J.-S.; Lee, E.-H.; Park, N.-R.; Choi, Y.H. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: A cross-sectional study. Arch. Psychiat. Nurs. 2018, 32, 2–6. [Google Scholar] [CrossRef] [PubMed]
- Odriozola-González, P.; Planchuelo-Gómez, Á.; Irurtia, M.J.; de Luis-García, R. Psychological effects of the COVID-19 outbreak and lockdown among students and workers of a Spanish university. Psychiatry Res. 2020, 290, 1–8. [Google Scholar]
- Zhang, Y.; Ma, Z.F. Impact of the COVID-19 pandemic on mental health and quality of life among local residents in Liaoning Province, China: A cross-sectional study. Int. J. Environ. Res. Public Health 2020, 17, 2381. [Google Scholar] [CrossRef]
- Qiu, J.; Shen, B.; Zhao, M.; Wang, Z.; Xie, B.; Xu, Y. A nationwide survey of psychological distress among Chinese people in the COVID-19 epidemic: Implications and policy recommendations. Gen. Psychiatr. 2020, 33, 1–3. [Google Scholar] [CrossRef]
- Son, K.; Xu, R.; Stratton, T.D.; Kavcic, V.; Luo, D.; Hou, F.; Bi, F.; Jiao., R.; Yan, S.; Jiang, Y. Sex differences and psychological stress: Responses to the COVID-19 epidemic in China. medRvix 2020, 1–15. [Google Scholar] [CrossRef]
- Yang, Y.; Li, W.; Zhang, Q.; Zhang, L.; Cheung, T.; Xiang, Y.T. Mental health services for older adults in China during the COVID-19 outbreak. Lancet Psychiat. 2020, 7, e19. [Google Scholar] [CrossRef]
- Tsai, J.; Wilson, M. COVID-19: A potential public health problem for homeless populations. Lancet 2020, 5, e186–e187. [Google Scholar] [CrossRef]
- Liem, A.; Wang, C.; Wariyanti, Y.; Latkin, C.A.; Hall, B.J. The neglected health of international migrant workers in the COVID-19 epidemic. Lancet Psychiat. 2020, 7, e20. [Google Scholar] [CrossRef]
- Rashidi Fakari, F.; Simbar, M. Coronavirus pandemic and worries during pregnancy; a letter to the editor. Arch. Acad. Emerg. Med. 2020, 8, e21. [Google Scholar] [PubMed]
- Zhai, Y.; Du, X. Mental health care for international Chinese students affected by the COVID-19 outbreak. Lancet Psychiat. 2020, 7, e22. [Google Scholar] [CrossRef]
- Yao, H.; Chen, J.H.; Xu, Y.F. Rethinking online health services in China during COVID-19 epidemic. Asian J. Psychiatr. 2020, 50, 1. [Google Scholar] [CrossRef] [PubMed]
- Mowbray, H. In Beijing, coronavirus 2019-nCoV has created a siege mentality. BMJ 2020, 368, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Moghanibashi-Mansourieh, A. Assessing the anxiety level of Iranian general population during COVID-19 outbreak. Asian J. Psychiatr. 2020, 51, 1–5. [Google Scholar]
- Kowal, M.; Coll-Martín, T.; Ikizer, G.; Rasmussen, J.; Eichel, K.; Studzińska, A.; Koszałkowska, K.; Karwowski, M.; Najmussaqib, A.; Pankowski, D.; et al. Who is the most stressed during COVID-19 isolation? Data from 27 countries. PsyArXiv Preprint 2020, 1–23. [Google Scholar] [CrossRef]
- Cortés-Álvarez, N.Y.; Piñeiro-Lamas, R.; Vuelvas-Olmos, C.R. Psychological effects and associated factors of COVID-19 in a Mexican sample. Disaster Med. Public Health Prep. 2020, 1–12. [Google Scholar] [CrossRef]
- Gausman, J.; Langer, A. Sex and gender disparities in the COVID-19 pandemic. J. Women’s Health 2020, 29, 465–466. [Google Scholar] [CrossRef]
- Ozamiz-Etxebarria, N.; Idoiaga Mondragon, N.; Dosil Santamaría, M.; Picaza Gorrotxategi, M. Psychological symptoms during the two stages of lockdown in response to the COVID-19 outbreak: An investigation in a sample of citizens in Northern Spain. Front. Psychol. 2020, 11, 1–9. [Google Scholar]
- Limcaoco, R.S.G.; Mateos, E.M.; Fernandez, J.M.; Roncero, C. Anxiety, worry and perceived stress in the world due to the COVID-19 pandemic. Preliminary results. medRxiv 2020, 1–11. [Google Scholar] [CrossRef]
- Ozamiz-Etxebarria, N.; Dosil-Santamaria, M.; Picaza-Gorrochategui, M.; Idoiaga-Mondragon, N. Stress, anxiety, and depression levels in the initial stage of the COVID-19 outbreak in a population sample in the northern Spain. Cad. Saúde Pública 2020, 36, 1–9. [Google Scholar] [CrossRef]
- Shevlin, M.; McBride, O.; Murphy, J.; Gibson Miller, J.; Hartman, T.K.; Levita, L.; Mason, L.; Martinez, A.; McKay, R.; Stocks, T.; et al. Anxiety, Depression, Traumatic Stress, and COVID-19 Related Anxiety in the UK General Population During the COVID-19 Pandemic. PsyArXiv Preprint 2020, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Organization for Economic Cooperation and Development (OECD). Women at the core of the fight against COVID-19 crisis. OECD Policy Responses to Coronavirus (COVID-19). 2020. Available online: https://www.oecd.org/coronavirus/policy-responses/women-at-the-core-of-the-fight-against-covid-19-crisis-553a8269/ (accessed on 15 June 2020).
- Vicario-Merino, A.; Muñoz-Agustin, N. Analysis of the stress, anxiety and healthy habits in the Spanish COVID-19 confinement. Health Sci. J. 2020, 14, 1–6. [Google Scholar] [CrossRef]
- Rodríguez-Rey, R.; Garrido-Hernansaiz, H.; Collado, S. Psychological impact and associated factors during the initial stage of the Coronavirus (COVID-19) pandemic among the general population in Spain. Front. Psychol. 2020, 11, 1–23. [Google Scholar] [CrossRef] [PubMed]
- Inchausti, F.; MacBeth, A.; Hasson-Ohayon, I.; Dimaggio, G. Psychological intervention and COVID-19: What we know so far and what we can do. J. Contemp. Psychother. 2020, 50, 243–250. [Google Scholar] [CrossRef] [PubMed]
- Cohen, S.; Kamarck, T.; Mermelstein, R. A global measure of perceived stress. J. Health Soc. Behav. 1983, 24, 385–396. [Google Scholar] [CrossRef] [PubMed]
- Campo-Arias, A.; Bustos-Leiton, G.; Romero-Chaparro, A. Consistencia interna y dimensionalidad de la Escala de Estrés Percibido (EEP-10 y EEP-14) en una muestra de universitarias de Bogotá, Colombia. Aquichan 2009, 9, 271–280. [Google Scholar]
- Cohen, S.; Janicki-Deverts, D. Who’s stressed? Distributions of psychological stress in the United States in probability samples from 1983, 2006, and 2009. J. App. Soc. Psychol. 2012, 42, 1320–1334. [Google Scholar] [CrossRef]
- Lee, E.-H. Review of the psychometric evidence of the Perceived Stress Scale. Asian Nurs. Res. 2012, 6, 121–127. [Google Scholar] [CrossRef]
- Remor, E. Psychometric properties of a European Spanish version of the Perceived Stress Scale. Span. J. Psychol. 2006, 9, 86–93. [Google Scholar] [CrossRef]
- Taylor, J.M. Psychometric analysis of the Ten-Item Perceived Stress Scale. Psychol. Assess. 2015, 27, 90–101. [Google Scholar] [CrossRef] [PubMed]
- Cohen, J. Statistical power analysis for the behavioral sciences, 2nd ed.; Lawrence Erlbaum Associates: Hillsdale, NJ, USA, 1988. [Google Scholar]
- Rodríguez, S.; Valle, A.; Piñeiro, I.; Rodríguez-Llorente, C.; Guerrero, E.; Martins, L. COVID-19: Sociodemographic characteristics and stress (Version 1). [Data set]. Zenodo 2020. [Google Scholar] [CrossRef]
- Rodríguez, S.; Valle, A.; Piñeiro, I.; Vieites, T.; Díaz, F.; González-Suárez, R. COVID-19 lockdown: Key factors in citizens’ wellbeing. J. Health Psychol. 2020, in press. [Google Scholar]
- Gómez-Salgado, J.; Andrés-Villas, M.; Domínguez-Salas, S.; Díaz-Milanés, D.; Ruiz-Frutos, C. Related health factors of psychological distress during the COVID-19 pandemic in Spain. Int. J. Environ. Res. Public Health 2020, 17, 3947. [Google Scholar] [CrossRef]
- Mantovani, A.; Dalbeni, A.; Beatrice, G. Coronavirus disease 2019 (COVID-19): We don’t leave women alone. Int. J. Public Health 2020, 65, 1–2. [Google Scholar] [CrossRef]
- Mazza, C.; Ricci, E.; Biondi, S.; Colasanti, M.; Ferracuti, S.; Napoli, C.; Roma, P. A nationwide survey of psychological distress among Italian people during the COVID-19 pandemic: Immediate psychological responses and associated factors. Int. J. Environ. Res. Public Health 2020, 17, 3165. [Google Scholar] [CrossRef]
- Nielsen, L.; Curtis, T.; Kristensen, T.S.; Rod Nielsen, N. What characterizes persons with high levels of perceived stress in Denmark? A national representative study. Scand. J. Public Health 2008, 36, 369–379. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rodríguez, S.; Valle, A.; Piñeiro, I.; Rodríguez-Llorente, C.; Guerrero, E.; Martins, L. Sociodemographic Characteristics and Stress of People from Spain Confined by COVID-19. Eur. J. Investig. Health Psychol. Educ. 2020, 10, 1095-1105. https://doi.org/10.3390/ejihpe10040077
Rodríguez S, Valle A, Piñeiro I, Rodríguez-Llorente C, Guerrero E, Martins L. Sociodemographic Characteristics and Stress of People from Spain Confined by COVID-19. European Journal of Investigation in Health, Psychology and Education. 2020; 10(4):1095-1105. https://doi.org/10.3390/ejihpe10040077
Chicago/Turabian StyleRodríguez, Susana, Antonio Valle, Isabel Piñeiro, Carolina Rodríguez-Llorente, Estefanía Guerrero, and Ludmila Martins. 2020. "Sociodemographic Characteristics and Stress of People from Spain Confined by COVID-19" European Journal of Investigation in Health, Psychology and Education 10, no. 4: 1095-1105. https://doi.org/10.3390/ejihpe10040077
APA StyleRodríguez, S., Valle, A., Piñeiro, I., Rodríguez-Llorente, C., Guerrero, E., & Martins, L. (2020). Sociodemographic Characteristics and Stress of People from Spain Confined by COVID-19. European Journal of Investigation in Health, Psychology and Education, 10(4), 1095-1105. https://doi.org/10.3390/ejihpe10040077






