Development, Characterization and In Vitro Evaluation of Paclitaxel and Anastrozole Co-Loaded Liposome
Abstract
:1. Introduction
2. Materials and Methods
2.1. Materials
2.2. Methods
2.2.1. Preparation of PTX and ANA Co-Loaded Liposome
2.2.2. Characterization
2.2.3. Drug Loading and Entrapment Efficiency
2.2.4. In Vitro Drugs Release
2.2.5. Cytotoxicity Study in MCF-7 Cell Line
3. Results and Discussion
3.1. Characterization of Multi-Drug Loaded Liposome
3.2.1. Particle Size and Zeta Potential
3.2.2. Morphology Observation
3.2. Drug Entrapment Efficiency and Loading Capacity
3.3. In Vitro Drug Release of Multi-Drug Loaded Liposome
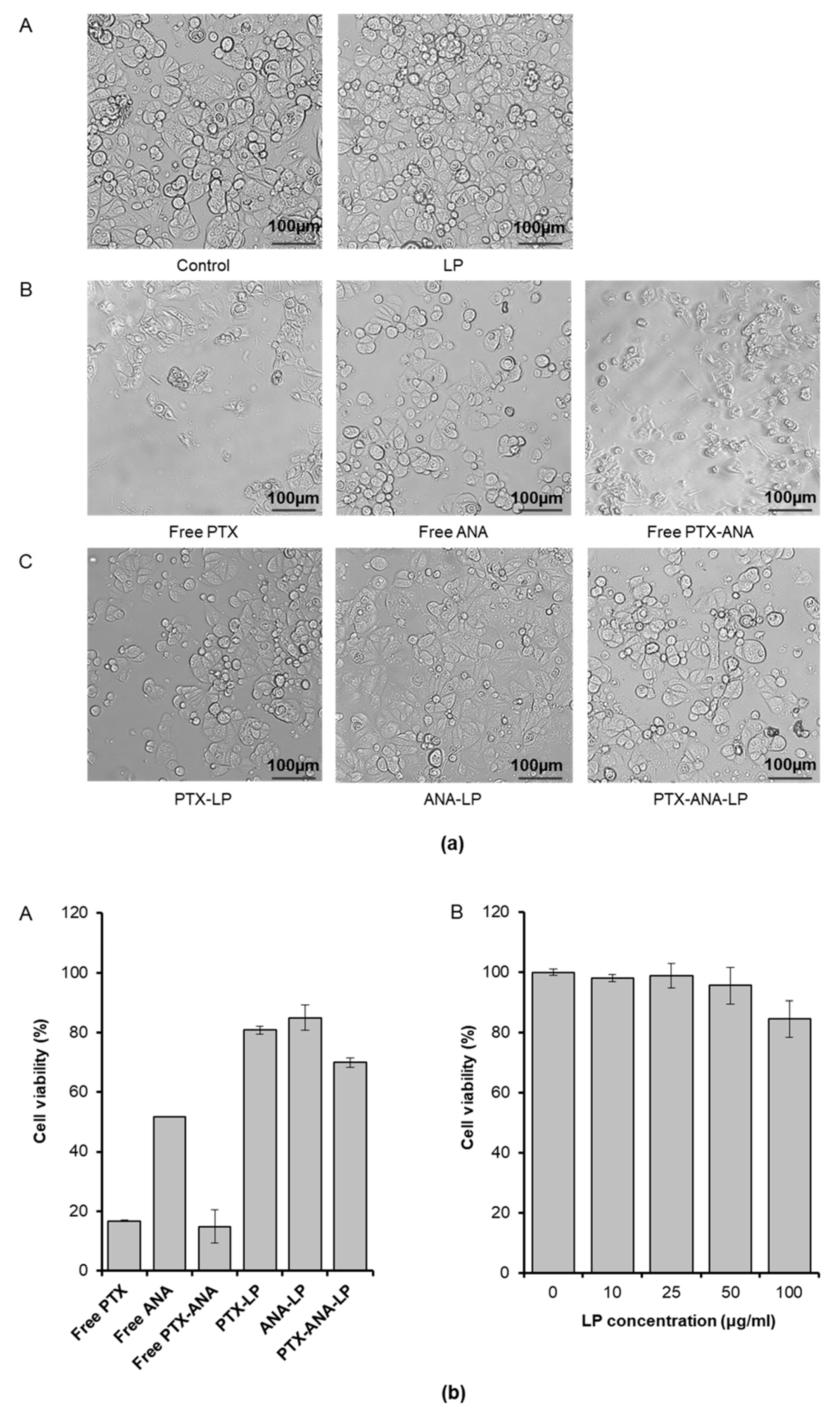
3.4. In Vitro Cytotoxicity
4. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- Semreen, M.H.; Alniss, H.; Cacciatore, S.; El-Awady, R.; Mousa, M.; Almehdi, A.M.; El-Huneidi, W.; Zerbini, L.; Soares, N.C. GC–MS based comparative metabolomic analysis of MCF-7 and MDA-MB-231 cancer cells treated with Tamoxifen and/or Paclitaxel. Biochem. Mol. Biol. 2020, 225, 103875. [Google Scholar] [CrossRef] [PubMed]
- Alqahtani, F.Y.; Aleanizy, F.S.; El Tahir, E.; Alkahtani, H.M.; AlQuadeib, B.T. Paclitaxel. In Profiles of Drug Substances, Excipients and Related Methodology; Elsevier: Amsterdam, The Netherlands, 2019; Volume 44, pp. 205–238. [Google Scholar]
- Crown, J.; O’Leary, M.; Ooi, W.S. Docetaxel and paclitaxel in the treatment of breast cancer: A review of clinical experience. Oncologist 2004, 9, 24–32. [Google Scholar] [CrossRef] [PubMed]
- Paridaens, R.; Biganzoli, L.; Bruning, P.; Klijn, J.; Gamucci, T.; Houston, S.; Coleman, R.; Schachter, J.; Van Vreckem, A.; Sylvester, R. Paclitaxel versus doxorubicin as first-line single-agent chemotherapy for metastatic breast cancer: A European Organization for Research and Treatment of Cancer Randomized Study with cross-over. J. Clin. Oncol. 2000, 18, 724–733. [Google Scholar] [CrossRef] [PubMed]
- Stage, T.B.; Bergmann, T.K.; Kroetz, D.L. Clinical pharmacokinetics of paclitaxel monotherapy: An updated literature review. Clin. Pharmacokinet. 2018, 57, 7–19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- De Weger, V.A.; Beijnen, J.H.; Schellens, J.H. Cellular and clinical pharmacology of the taxanes docetaxel and paclitaxel–A review. Anticancer Drugs 2014, 25, 488–494. [Google Scholar] [CrossRef] [PubMed]
- Smith, I.E.; Dowsett, M. Aromatase inhibitors in breast cancer. New Engl. J. Med. 2003, 348, 2431–2442. [Google Scholar] [CrossRef] [Green Version]
- Geisler, J.; King, N.; Dowsett, M.; Ottestad, L.; Lundgren, S.; Walton, P.; Kormeset, P.; Lønning, PE. Influence of anastrozole (Arimidex), a selective, non-steroidal aromatase inhibitor, on in vivo aromatisation and plasma oestrogen levels in postmenopausal women with breast cancer. Br. J. Cancer 1996, 74, 1286–1291. [Google Scholar] [CrossRef] [Green Version]
- Geisler, J.G.; Stubbs, L.J.; Wasserman, W.W.; Mucenski, M.L. Molecular cloning of a novel mouse gene with predominant muscle and neural expression. Mamm. Genome 1998, 9, 274–282. [Google Scholar] [CrossRef]
- Geisler, J.r.; Haynes, B.; Anker, G.; Dowsett, M.; Lønning, P.E. Influence of letrozole and anastrozole on total body aromatization and plasma estrogen levels in postmenopausal breast cancer patients evaluated in a randomized, cross-over study. J. Clin. Oncol. 2002, 20, 751–757. [Google Scholar] [CrossRef]
- Ingle, J.N.; Cairns, J.; j Suman, V.J.; Shepherd, L.E.; Fasching, P.A.; Hoskin, T.L.; Singh, R.J.; Desta, Z.; Kalari, K.R.; Ellis, M.J.; et al. Anastrozole has an association between degree of estrogen suppression and outcomes in early breast cancer and is a ligand for estrogen receptor α. Clin. Cancer Res. 2020, 26, 2986–2996. [Google Scholar] [CrossRef] [Green Version]
- Albain, K.S.; Nag, S.M.; Calderillo-Ruiz, G.; Jordaan, J.P.; Llombart, A.C.; Pluzanska, A.; Rolski, J.; Melemed, A.S.; Reyes-Vidal, J.M.; Sekhon, J.S. Gemcitabine plus paclitaxel versus paclitaxel monotherapy in patients with metastatic breast cancer and prior anthracycline treatment. J. Clin. Oncol. 2008, 26, 3950–3957. [Google Scholar] [CrossRef] [PubMed]
- De Vita, F.; Borg, C.; Farina, G.; Geva, R.; Carton, I.; Cuku, H.; Wei, R.; Muro, K. Ramucirumab and paclitaxel in patients with gastric cancer and prior trastuzumab: Subgroup analysis from RAINBOW study. Future Oncol. 2019, 15, 2723–2731. [Google Scholar] [CrossRef] [PubMed]
- Valery, S.; Chouaid, C.; Rousseau-Bussac, G.; Monnet, I.; Bilger, G.; Boré, P.; Pinsolle, J.; Descourt, R.; Geier, M.; Toffart, A. Efficacy of weekly paclitaxel-bevacizumab combination in advanced non squamous non-small cell lung cancer (NSCLC) progressing after immune checkpoint inhibitors-AVATAX, a retrospective multicentric study: Preliminary data. Ann. Oncol. 2019, 30, xi29. [Google Scholar] [CrossRef]
- Watanabe, N.; Ootawa, Y.; Kodama, K.; Kaide, A.; Ootsuka, N.; Matsuoka, J. Concurrent administration of chemo-endocrine therapy for postmenopausal breast cancer patients. Breast Cancer 2010, 17, 247–253. [Google Scholar] [CrossRef]
- Sato, T.; Nakagawa, T.; Kuwayama, T.; Kubota, K.; Suzuki, S.; Sugihara, K. A case of inflammatory breast cancer responding to anastrozole. Gan Kagaku Ryoho. Cancer Chemother. 2009, 36, 2477–2479. [Google Scholar]
- Mota, L.D.G.; de Barros, A.L.; Fuscaldi, L.L.; de Oliveira, M.C.; Cardoso, V.N. Long-Circulating and pH-Sensitive Liposome Preparation Trapping a Radiotracer for Inflammation Site Detection. J. Nanosci. Nanotechnol. 2015, 15, 4149–4158. [Google Scholar] [CrossRef]
- Zhang, H.; Xiao, Y.; Cui, S.; Zhou, Y.; Zeng, K.; Yan, M.; Zhao, C. Novel Galactosylated Poly(ethylene glycol)-Cholesterol for Liposomes as a Drug Carrier for Hepatocyte-Targeting. J. Nanosci. Nanotechnol. 2015, 15, 4058–4069. [Google Scholar] [CrossRef]
- Gunay, M.S.; Ozer, A.Y.; Erdogan, S.; Bodard, S.; Baysal, I.; Gulhan, Z.; Guilloteau, D.; Chalon, S. Development of Nanosized, Pramipexole-Encapsulated Liposomes and Niosomes for the Treatment of Parkinson’s Disease. J. Nanosci. Nanotechnol. 2017, 17, 5155–5167. [Google Scholar] [CrossRef]
- Ahmed, K.S.; Hussein, S.A.; Ali, A.H.; Korma, S.A.; Lipeng, Q.; Jinghua, C. Liposome: Composition, characterisation, preparation, and recent innovation in clinical applications. J. Drug Target. 2019, 27, 742–761. [Google Scholar] [CrossRef]
- Tran, P.; Lee, S.-E.; Kim, D.-H.; Pyo, Y.-C.; Park, J.-S. Recent advances of nanotechnology for the delivery of anticancer drugs for breast cancer treatment. J. Pharm. Investig. 2019, 1–10. [Google Scholar] [CrossRef]
- Chen, S.; Auriat, A.; Koudrina, A.; DeRosa, M.; Cao, X.; Tsai, E.C. Nano-engineering Nanoparticles for Clinical Use in the Central Nervous System: Clinically Applicable Nanoparticles and Their Potential Uses in the Diagnosis and Treatment of CNS Aliments. In Nanoengineering Materials for Biomedical Uses; Springer: New York, NY, USA, 2019; pp. 125–145. [Google Scholar]
- Wesolowski, R.; Ramaswamy, B. Gene expression profiling: Changing face of breast cancer classification and management. Gene Expr. 2011, 15, 105–115. [Google Scholar] [CrossRef] [PubMed]
- Angeloni, S.; Martin, M.; Garcia-Morales, P.; Castro-Galache, M.; Ferragut, J.; Saceda, M. Regulation of estrogen receptor-alpha expression by the tumor suppressor gene p53 in MCF-7 cells. 2004, 180, 497–504. J. Endocrinol. 2004, 180, 497–504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shashni, B.; Nagasaki, Y. Nitroxide radical-containing nanoparticles attenuate tumorigenic potential of triple negative breast cancer. Biomaterials 2018, 178, 48–62. [Google Scholar] [CrossRef] [PubMed]
- Ansari, S.A.; Matricardi, P.; Meo, C.D.; Alhaique, F.; Coviello, T. Evaluation of rheological properties and swelling behaviour of sonicated scleroglucan samples. Molecules 2012, 17, 2283–2297. [Google Scholar] [CrossRef] [PubMed]
- Yang, T.; Cui, F.-D.; Choi, M.-K.; Lin, H.; Chung, S.-J.; Shim, C.-K.; Kim, D.-D. Liposome formulation of paclitaxel with enhanced solubility and stability. Drug Deliv. 2007, 14, 301–308. [Google Scholar] [CrossRef]
- Le, N.T.T.; Pham, L.P.T.; Nguyen, D.H.T.; Le, N.H.; Tran, T.V.; Nguyen, C.K.; Nguyen, D.H. Liposome-Based Nanocarrier System for Phytoconstituents. In Novel Drug Delivery Systems for Phytoconstituents; CRC Press: Boca Raton, FL, USA, 2019; pp. 45–68. [Google Scholar]
- Thi, N.T.N.; Nguyen, D.H. Hollow mesoporous silica nanoparticles fabrication for anticancer drug delivery. Vietnam J. Sci. Technol. 2020, 58, 39. [Google Scholar]
- Bi, Y.; Lv, B.; Li, L.; Lee, R.J.; Xie, J.; Qiu, Z.; Teng, L. A Liposomal Formulation for Improving Solubility and Oral Bioavailability of Nifedipine. Molecules 2020, 25, 338. [Google Scholar] [CrossRef] [Green Version]
- Nguyen-Thi, N.-T.; Tran, P.; Phuong, L.; Le, N.T.T.; Cao, M.-T.; Nguyen, N.T.; Nguyen, C.H.; Nguyen, D.-H.; Than, V.T.; Le, Q.T. The Engineering of Porous Silica and Hollow Silica Nanoparticles to Enhance Drug-loading Capacity. Processes 2019, 7, 805. [Google Scholar] [CrossRef] [Green Version]
- Yaroslavov, A.; Efimova, A.; Smirnova, N.; Erzunov, D.; Lukashev, N.; Grozdova, I.; Melik-Nubarov, N. A novel approach to a controlled opening of liposomes. Colloids Surf. B Biointerfaces 2020, 190, 110906. [Google Scholar] [CrossRef]
- Sakai-Kato, K.; Yoshida, K.; Izutsu, K.-i. Effect of surface charge on the size-dependent cellular internalization of liposomes. Chem. Phys. Lipids 2019, 224, 104726. [Google Scholar] [CrossRef]
- Ibaraki, H.; Kanazawa, T.; Oogi, C.; Takashima, Y.; Seta, Y. Effects of surface charge and flexibility of liposomes on dermal drug delivery. J. Drug Deliv. Sci. Technol. 2019, 50, 155–162. [Google Scholar] [CrossRef]
- Brandelli, A. The interaction of nanostructured antimicrobials with biological systems: Cellular uptake, trafficking and potential toxicity. Food Sci. Hum. Wellness 2020, 9, 8–20. [Google Scholar] [CrossRef]
- Le, N.T.T.; Cao, V.D.; Nguyen, T.N.Q.; Le, T.T.H.; Tran, T.T.; Hoang Thi, T.T. Soy Lecithin-Derived Liposomal Delivery Systems: Surface Modification and Current Applications. Int. J. Mol. Sci. 2019, 20, 4706. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Le, N.T.T.; Thi, Y.N.N.; Thi, B.L.P.; Hoang, N.L.; Nguyen, C.K.; Nguyen, D.H. Nanoliposomes as an Efficient Drug Carrier System for Paclitaxel Delivery. In Proceedings of the International Conference on the Development of Biomedical Engineering in Vietnam, Ho Chi Minh City, Vietnam, 27–29 June 2018; pp. 193–196. [Google Scholar]
- Drummond, D.C.; Noble, C.O.; Hayes, M.E.; Park, J.W.; Kirpotin, D.B. Pharmacokinetics and in vivo drug release rates in liposomal nanocarrier development. J. Pharm. Sci. 2008, 97, 4696–4740. [Google Scholar] [CrossRef]
- Nguyen, T.L.; Nguyen, T.H.; Nguyen, D.H. Development and in vitro evaluation of liposomes using soy lecithin to encapsulate paclitaxel. Int. J. Biomater. 2017, 2017, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Yan, L.; Dempsey, E.M.; Song, W.; Qi, R.; Li, W.; Huang, Y.; Jing, X.; Zhou, D.; Ding, J. Recent progress in polymer-based platinum drug delivery systems. Prog. Polym. Sci. 2018, 87, 70–106. [Google Scholar] [CrossRef]
- Le, N.T.T.; Nguyen, T.N.Q.; Cao, V.D.; Hoang, D.T.; Ngo, V.C.; Thi, H.; Thanh, T. Recent Progress and Advances of Multi-Stimuli-Responsive Dendrimers in Drug Delivery for Cancer Treatment. Pharmaceutics 2019, 11, 591. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Rodallec, A.; Brunel, J.-M.; Giacometti, S.; Maccario, H.; Correard, F.; Mas, E.; Orneto, C.; Savina, A.; Bouquet, F.; Lacarelle, B. Docetaxel–trastuzumab stealth immunoliposome: Development and in vitro proof of concept studies in breast cancer. Int. J. Nanomed. 2018, 13, 3451. [Google Scholar] [CrossRef] [Green Version]
- Lei, M.; Ma, G.; Sha, S.; Wang, X.; Feng, H.; Zhu, Y.; Du, X. Dual-functionalized liposome by co-delivery of paclitaxel with sorafenib for synergistic antitumor efficacy and reversion of multidrug resistance. Drug Deliv. 2019, 26, 262–272. [Google Scholar] [CrossRef] [Green Version]
- Zidan, A.S.; Sammour, O.A.; Hammad, M.A.; Megrab, N.A.; Hussain, M.D.; Khan, M.A.; Habib, M.J. Formulation of anastrozole microparticles as biodegradable anticancer drug carriers. Aaps Pharmscitech 2006, 7, E38–E46. [Google Scholar] [CrossRef] [Green Version]
- Zhou, D.; Pompon, D.; Chen, S.A. Stable expression of human aromatase complementary DNA in mammalian cells: A useful system for aromatase inhibitor screening. Cancer Res. 1990, 50, 6949–6954. [Google Scholar] [PubMed]



© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Vu, M.T.; Nguyen, D.T.D.; Nguyen, N.H.; Le, V.T.; Dao, T.N.; Nguyen, T.H.; Cong, T.D.; Pham, T.L.-B.; Lam, T.D.; Le, N.T.T. Development, Characterization and In Vitro Evaluation of Paclitaxel and Anastrozole Co-Loaded Liposome. Processes 2020, 8, 1110. https://doi.org/10.3390/pr8091110
Vu MT, Nguyen DTD, Nguyen NH, Le VT, Dao TN, Nguyen TH, Cong TD, Pham TL-B, Lam TD, Le NTT. Development, Characterization and In Vitro Evaluation of Paclitaxel and Anastrozole Co-Loaded Liposome. Processes. 2020; 8(9):1110. https://doi.org/10.3390/pr8091110
Chicago/Turabian StyleVu, Minh Thanh, Dinh Tien Dung Nguyen, Ngoc Hoi Nguyen, Van Thu Le, The Nam Dao, Thi Huong Nguyen, Tien Dung Cong, Truc Le-Buu Pham, Tri Duc Lam, and Ngoc Thuy Trang Le. 2020. "Development, Characterization and In Vitro Evaluation of Paclitaxel and Anastrozole Co-Loaded Liposome" Processes 8, no. 9: 1110. https://doi.org/10.3390/pr8091110
APA StyleVu, M. T., Nguyen, D. T. D., Nguyen, N. H., Le, V. T., Dao, T. N., Nguyen, T. H., Cong, T. D., Pham, T. L.-B., Lam, T. D., & Le, N. T. T. (2020). Development, Characterization and In Vitro Evaluation of Paclitaxel and Anastrozole Co-Loaded Liposome. Processes, 8(9), 1110. https://doi.org/10.3390/pr8091110




