The Impact of Mobile Phone Reminders on Perceived Self-Care Levels of Informal Caregivers
Abstract
:1. Introduction
2. Methods
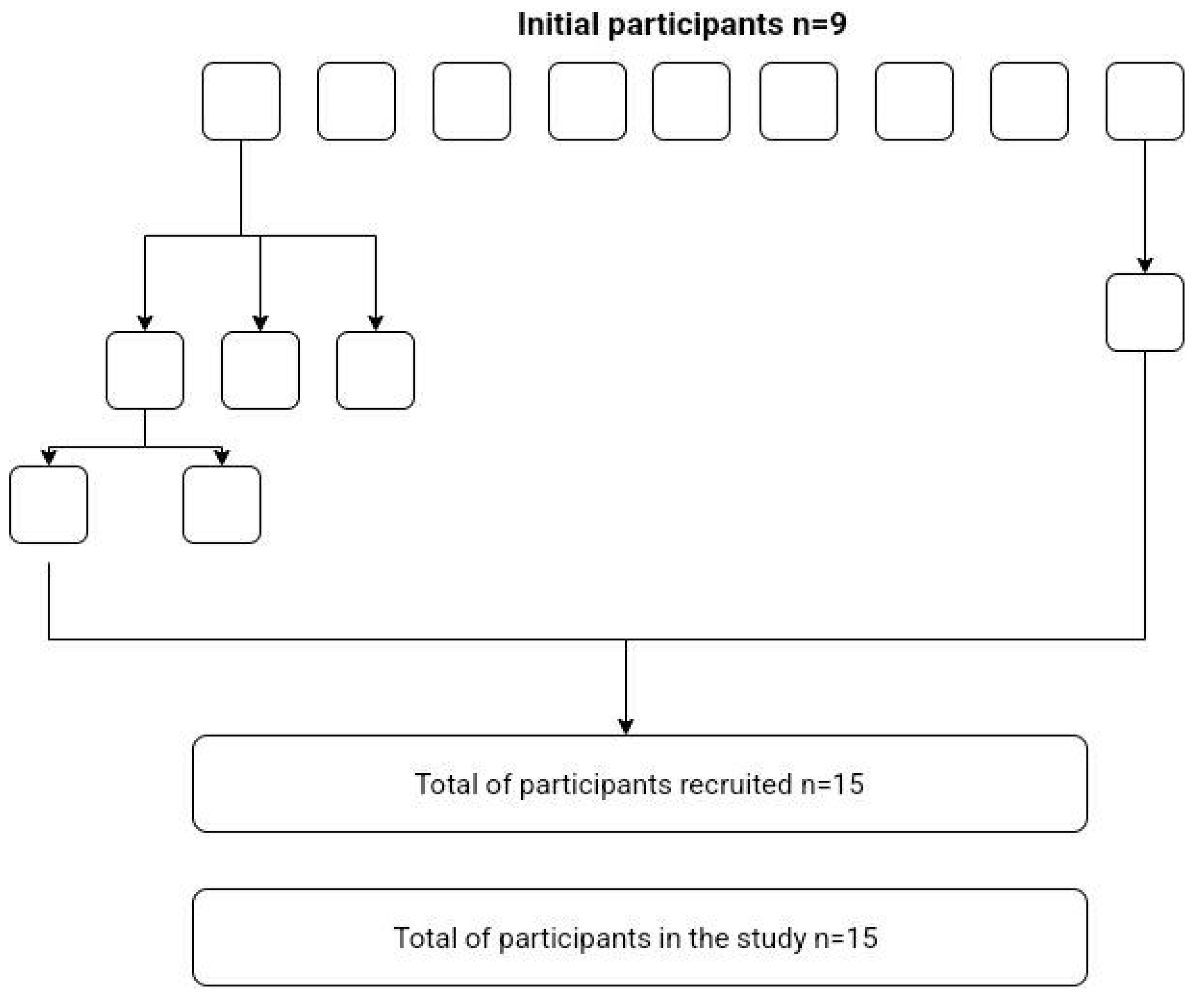
2.1. Sample
2.2. Measurements
2.2.1. Socio-Demographic Characteristics
2.2.2. Mindful Self-Care Scale
2.3. Procedure
3. Results
Differences between Mindful Self-Care Scale Total Score with Reminders and without Reminders
4. Discussion
5. Study Limitations
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Grossman, M.R.; Zak, D.K.; Zelinski, E.M. Mobile Apps for Caregivers of Older Adults: Quantitative Content Analysis. JMIR Mhealth Uhealth 2018, 6, e162. [Google Scholar] [CrossRef]
- Storni, C. Multiple Forms of Appropriation in Self-Monitoring Technology: Reflections on the Role of Evaluation in Future Self-Care. Int. J. Hum. Comput. Interact. 2010, 26, 537–561. [Google Scholar] [CrossRef]
- Fuentes, C.; Hernandez, C.; Escobedo, L.; Herskovic, V.; Tentori, M. Promoting Self-Reflection of Social Isolation through Persuasive Mobile Technologies: The Case of Mother Caregivers of Children with Cancer. Int. J. Hum.-Comput. Interact. 2014, 30, 802–814. [Google Scholar] [CrossRef]
- Park, M.; Choi, S.; Lee, S.J.; Kim, S.H.; Kim, J.; Go, Y.; Lee, D.Y. The roles of unmet needs and formal support in the caregiving satisfaction and caregiving burden of family caregivers for persons with dementia. Int. Psychogeriatr. 2018, 30, 557–567. [Google Scholar] [CrossRef] [PubMed]
- Heynsbergh, N.; Heckel, L.; Botti, M.; Livingston, P. Feasibility, useability and acceptability of technology-based interventions for informal cancer carers: A systematic review. BMC Cancer 2018, 18, 244. [Google Scholar] [CrossRef] [PubMed]
- Boumans, N.P.G.; Dorant, E. Double-duty caregivers: Healthcare professionals juggling employment and informal caregiving. A survey on personal health and work experiences. J. Adv. Nurs. 2014, 70, 1604–1615. [Google Scholar] [CrossRef] [PubMed]
- Mazanec, S.R.; Daly, B.J.; Douglas, S.L.; Lipson, A.R. Work productivity and health of informal caregivers of persons with advanced cancer. Res. Nurs. Health 2011, 34, 483–495. [Google Scholar] [CrossRef] [PubMed]
- Pitsenberger, D.J. Juggling work and elder caregiving: Work-life balance for aging American workers. AAOHN J. 2006, 54, 181–187. [Google Scholar] [CrossRef]
- Black, B.S.; Johnston, D.; Rabins, P.V.; Morrison, A.; Lyketsos, C.; Samus, Q.M. Unmet needs of community-residing persons with dementia and their informal caregivers: Findings from the maximizing independence at home study. J. Am. Geriatr. Soc. 2013, 61, 2087–2095. [Google Scholar] [CrossRef] [PubMed]
- DiZazzo-Miller, R.; Pociask, F.D.; Adamo, D.E. The Role of Confidence in Family Caregiving for People with Dementia. Phys. Occup. Ther. Geriatr. 2020, 38, 355–369. [Google Scholar] [CrossRef]
- Campbell, P.; Wright, J.; Oyebode, J.; Job, D.; Crome, P.; Bentham, P.; Jones, L.; Lendon, C. Determinants of burden in those who care for someone with dementia. Int. J. Geriatr. Psychiatry 2008, 23, 1078–1085. [Google Scholar] [CrossRef] [PubMed]
- Reinhard, S.C.; Given, B.; Petlick, N.H.; Bemis, A. Supporting Family Caregivers in Providing Care. In Patient Safety and Quality: An Evidence-Based Handbook for Nurses; Hughes, R.G., Ed.; Agency for Healthcare Research and Quality: Rockville, MD, USA, 2008. [Google Scholar]
- Caputo, J.; Pavalko, E.K.; Hardy, M.A. The Long-Term Effects of Caregiving on Women’s Health and Mortality. J. Marriage Family 2016, 78, 1382–1398. [Google Scholar] [CrossRef] [PubMed]
- Brown, E.L.; Ruggiano, N.; Page, T.F.; Roberts, L.; Hristidis, V.; Whiteman, K.L.; Castro, J. CareHeroes Web and AndroidTM Apps for Dementia Caregivers: A Feasibility Study. Res. Gerontol. Nurs. 2016, 9, 193–203. [Google Scholar] [CrossRef]
- Price, M.L.; Surr, C.A.; Gough, B.; Ashley, L. Experiences and support needs of informal caregivers of people with multimorbidity: A scoping literature review. Psychol. Health 2020, 35, 36–69. [Google Scholar] [CrossRef] [PubMed]
- Queluz, F.N.F.R.; Kervin, E.; Wozney, L.; Fancey, P.; McGrath, P.J.; Keefe, J. Understanding the needs of caregivers of persons with dementia: A scoping review. Int. Psychogeriatr. 2020, 32, 35–52. [Google Scholar] [CrossRef]
- Vervloet, M.; van Dijk, L.; Santen-Reestman, J.; van Vlijmen, B.; van Wingerden, P.; Bouvy, M.; de Bakker, D. SMS reminders improve adherence to oral medication in type 2 diabetes patients who are real time electronically monitored. Int. J. Med. Inform. 2012, 81, 594–604. [Google Scholar] [CrossRef] [PubMed]
- Oliveira, D.; Zarit, S.H.; Orrell, M. Health-Promoting Self-Care in Family Caregivers of People with Dementia: The Views of Multiple Stakeholders. Gerontologist 2019, 59, e501–e511. [Google Scholar] [CrossRef] [PubMed]
- Jensen, M.; Agbata, I.N.; Canavan, M.; McCarthy, G. Effectiveness of educational interventions for informal caregivers of individuals with dementia residing in the community: Systematic review and meta-analysis of randomised controlled trials. Int. J. Geriatr. Psychiatry 2015, 30, 130–143. [Google Scholar] [CrossRef]
- Lök, N.; Bademli, K. Pilot testing of the “First You Should Get Stronger” program among caregivers of older adults with dementia. Arch. Gerontol. Geriatr. 2017, 68, 84–89. [Google Scholar] [CrossRef] [PubMed]
- Losada, A.; Márquez-González, M.; Romero-Moreno, R.; Mausbach, B.T.; Lopez, J.; Fernández-Fernández, V.; Nogales-González, C. Cognitive-behavioral therapy (CBT) versus acceptance and commitment therapy (ACT) for dementia family caregivers with significant depressive symptoms: Results of a randomized clinical trial. J. Consult. Clin. Psychol. 2015, 83, 760–772. [Google Scholar] [CrossRef] [PubMed]
- Sharma, N.; Chakrabarti, S.; Grover, S. Gender differences in caregiving among family-caregivers of people with mental illnesses. World J. Psychiatry 2016, 6, 7. [Google Scholar] [CrossRef]
- Brown, E.L.; Ruggiano, N.; Li, J.; Clarke, P.J.; Kay, E.S.; Hristidis, V. Smartphone-Based Health Technologies for Dementia Care: Opportunities, Challenges, and Current Practices. J. Appl. Gerontol. 2019, 38, 73–91. [Google Scholar] [CrossRef]
- Cook-Cottone, C.P.; Guyker, W.M. The Development and Validation of the Mindful Self-Care Scale (MSCS): An Assessment of Practices that Support Positive Embodiment. Mindfulness 2018, 9, 161–175. [Google Scholar] [CrossRef]
- Nunes, F.; Verdezoto, N.; Fitzpatrick, G.; Kyng, M.; Grönvall, E.; Storni, C. Self-Care Technologies in HCI: Trends, Tensions, and Opportunities. ACM Trans. Comput.-Hum. Interact. 2015, 22, 6. [Google Scholar] [CrossRef]
- Washington, K.T.; Meadows, S.E.; Elliott, S.G.; Koopman, R.J. Information needs of informal caregivers of older adults with chronic health conditions. Patient Educ. Couns. 2011, 83, 37–44. [Google Scholar] [CrossRef]
- Soares, A.C.; Rêgo, A.D.S.; Rodrigues, T.F.C.D.S.; Cardoso, L.C.B.; Rossaneis, M.A.; Carreira, L.; Radovanovic, C.A.T. Construction and validation of self-care educational technology for caregivers. Rev. Bras. Enferm. 2021, 74, e20200215. [Google Scholar] [CrossRef]
- Suwa, S.; Yumoto, A.; Ueno, M.; Yamabe, T.; Hoshishiba, Y.; Sato, M. Practitioners’ identification of informal caregivers’ difficulties with activities of daily living interventions for older people with dementia in Japan. Psychogeriatrics 2021, 21, 466–477. [Google Scholar] [CrossRef]
- Fuller-Tyszkiewicz, M.; Richardson, B.; Little, K.; Teague, S.; Hartley-Clark, L.; Capic, T.; Khor, S.; Cummins, R.A.; Olsson, C.A.; Hutchinson, D. Efficacy of a Smartphone App Intervention for Reducing Caregiver Stress: Randomized Controlled Trial. JMIR Ment. Health 2020, 7, 7. [Google Scholar] [CrossRef]
- McLean, S.; Gee, M.; Booth, A.; Salway, S.; Nancarrow, S.; Cobb, M.; Bhanbhro, S. Targeting the Use of Reminders and Notifications for Uptake by Populations (TURNUP): A systematic review and evidence synthesis. Health Serv. Deliv. Res. 2014, 2, 1–184. [Google Scholar] [CrossRef]
- Damgaard, M.T.; Gravert, C. Now or never! The effect of deadlines on charitable giving: Evidence from two natural field experiments. J. Behav. Exp. Econ. 2017, 66, 78–87. [Google Scholar] [CrossRef]
- Damgaard, M.T.; Gravert, C. The hidden costs of nudging: Experimental evidence from reminders in fundraising. J. Public Econ. 2018, 157, 15–26. [Google Scholar] [CrossRef]
- Parker, C.; Scott, S.; Geddes, A. Snowball Sampling. In Research Methods Foundations; Atkinson, P., Delamont, S., Cernat, A., Sakshaug, J.W., Williams, R.A., Eds.; Sage: Newcastle upon Tyne, UK, 2019. [Google Scholar]
| ID | Sex | Age | Time Spend Being a Caregiver (Years) | Caregivers Spend Less Time on Themselves |
|---|---|---|---|---|
| IC1 | female | 47 | 9 | yes |
| IC2 | male | 56 | 1 | yes |
| IC3 | female | 56 | 10 | yes |
| IC4 | female | 26 | 0.4 | yes |
| IC5 | female | 60 | 2 | yes |
| IC6 | female | 76 | 9 | yes |
| IC7 | female | 66 | 3 | yes |
| IC8 | female | 59 | 6 | yes |
| IC9 | female | 46 | 10 | no |
| IC10 | female | 49 | 3 | no |
| IC11 | female | 55 | 5 | yes |
| IC12 | male | 85 | 10 | yes |
| IC13 | female | 59 | 10 | yes |
| IC14 | female | 63 | 9 | yes |
| IC15 | male | 63 | 9 | yes |
| Mindful Self-Care Scale | Condition 1 (without Reminders) | Condition 2 (with Reminders) | Z | r | p |
|---|---|---|---|---|---|
| Median | Median | ||||
| Total score | 20.73 | 20.85 | −2.48 | 0.64 | 0.013 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Peres, B.; Gouveia, É.R.; Campos, P.F. The Impact of Mobile Phone Reminders on Perceived Self-Care Levels of Informal Caregivers. Informatics 2022, 9, 59. https://doi.org/10.3390/informatics9030059
Peres B, Gouveia ÉR, Campos PF. The Impact of Mobile Phone Reminders on Perceived Self-Care Levels of Informal Caregivers. Informatics. 2022; 9(3):59. https://doi.org/10.3390/informatics9030059
Chicago/Turabian StylePeres, Beatriz, Élvio Rúbio Gouveia, and Pedro F. Campos. 2022. "The Impact of Mobile Phone Reminders on Perceived Self-Care Levels of Informal Caregivers" Informatics 9, no. 3: 59. https://doi.org/10.3390/informatics9030059
APA StylePeres, B., Gouveia, É. R., & Campos, P. F. (2022). The Impact of Mobile Phone Reminders on Perceived Self-Care Levels of Informal Caregivers. Informatics, 9(3), 59. https://doi.org/10.3390/informatics9030059







