Management of Enamel Defects with Resin Infiltration Techniques: Two Years Follow Up Retrospective Study
Abstract
:1. Introduction
- -
- Aesthetic results and his stability over time;
- -
- Reduction of hypersensitivity, if present.
2. Materials and Methods
2.1. Sample Description
- -
- Patients subjected to infiltrative treatment with resin (ICON-DMG) from January 2020 to July 2020.
- -
- Elements of anterior sector affected by mild or moderate degree of MIH (according to the classification of Mathu-Muju and Wright) [11].
- -
- Elements of anterior sector with mild or moderate degree of fluorosis (according to the Thylstrup and Ferjerskov index) [12].
- -
- Elements of anterior sector with post-traumatic hypomineralization.
- -
- Elements with conservative treatments;
- -
- Cavitated enamel defects;
- -
- Enamel defects with post-eruptive etiology;
- -
- Severe degree of MIH;
- -
- Severe degree of Fluorosis.
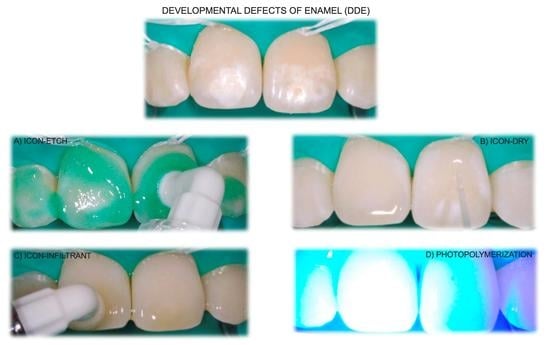
2.2. Infiltrative Resin Treatment Procedure
2.3. Photographic Documentation and Chromatic Evaluation
- 1:
- Clinically excellent/very good (Good color match. No difference in shade and translucency);
- 2:
- Clinically good (minor deviations);
- 3:
- Clinically sufficient/satisfactory (Clear deviation but acceptable. Does not affect aesthetics);
- 4:
- Clinically unsatisfactory (Localized-clinically unsatisfactory but can be corrected by repair);
- 5:
- Clinically poor (Unacceptable. Replacement necessary) [13].
2.4. Dentinal Hypersensitivity
- -
- The Shiff Air Index was used to evaluate the perception of discomfort after the application of air using an air-spray syringe for 3 s at 2 mm of distance and perpendicular to the tooth surface.
- -
- The Wong–Baker Faces Pain Rating Scale was used to characterize pain; this scale uses values ranging from 0 to 10, where 0 represents “no pain” and 10 represents “very strong pain”.
2.5. Statistical Analysis
3. Results
3.1. Study Population
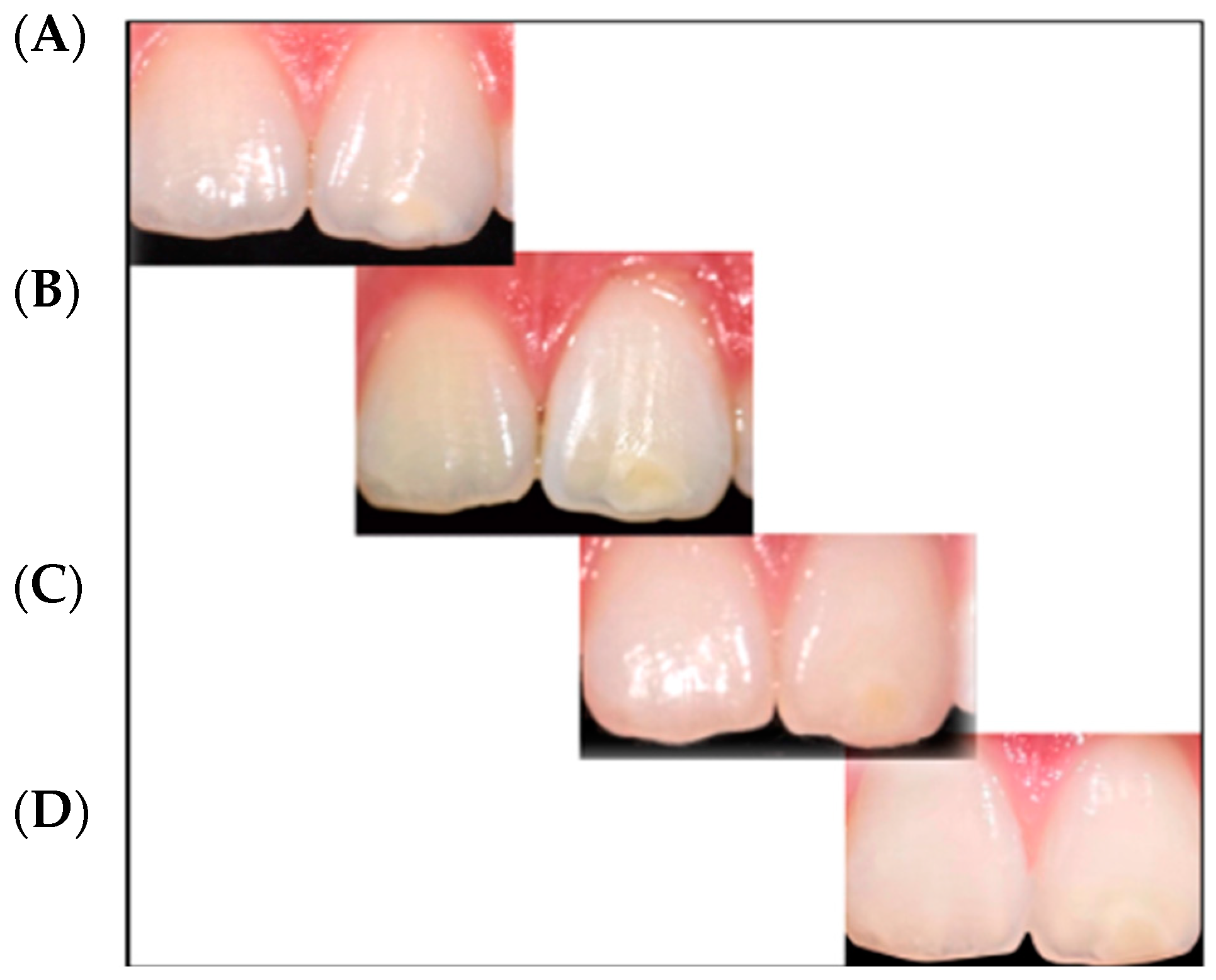
3.2. Qualitative Visual Evaluation
3.3. Dentin Hypersensitivity Assessment
3.4. Statistical Analysis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chankanka, O.; Levy, S.M.; Warren, J.J.; Chalmers, J.M. A literature review of aesthetic perceptions of dental fluorosis and relationships with psychosocial aspects/oral health-related quality of life. Community Dent. Oral Epidemiol. 2010, 38, 97–109. [Google Scholar] [CrossRef]
- Guerra, F.; Mazur, M.; Corridore, D.; Pasqualotto, D.; Nardi, G.; Ottolenghi, L. Evaluation of esthetic properties of developmental defects of enamel: A spectrophotometric clinical study. Sci. World J. 2015, 2015, 878235. [Google Scholar] [CrossRef]
- Denis, M.; Atlan, A.; Vennat, E.; Tirlet, G.; Attal, J.P. White defects on enamel: Diagnosis and anatomopathology: Two essential factors for proper treatment (part 1). Int. Orthod. 2013, 11, 139–165. [Google Scholar] [CrossRef]
- Jalevik, B.; Noren, J. Enamel hypomineralization of permanent first molars: A morphological study and survey af possible aetiological factors. Int. Ped. Dent. 2000, 10, 278–289. [Google Scholar] [CrossRef] [PubMed]
- Giuca, M.R.; Cappè, M.; Carli, E.; Lardani, L.; Pasini, M. Investigation of Clinical Characteristics and Etiological Factors in Children with Molar Incisor Hypomineralization. Int. J. Dent. 2018, 2018, 7584736. [Google Scholar] [CrossRef] [PubMed]
- Attal, J.P.; Atlan, A.; Denis, M.; Vennat, E.; Tirlet, G. White spots on enamel: Treatment protocol by superficial or deep infiltration (part 2). Int. Orthod. 2014, 12, 1–31. [Google Scholar] [CrossRef] [PubMed]
- Paglia, L. Molar Incisor Hypomineralization: Paediatricians should be involved as well! Eur. J. Paediatr Dent. 2018, 19, 173. [Google Scholar] [PubMed]
- Paris, S.; Schwendicke, F.; Seddig, S.; Muller, W.D.; Dorfer, C.; Meyer -Lueckel, H. Micro-hardness and mineral loss of enamel lesions after infiltration with various resin: Influence of infiltrant composition and application frequency in vitro. J. Dent. 2013, 41, 543–548. [Google Scholar] [CrossRef] [PubMed]
- Cocco, A.R.; Lund, R.G.; Torre, E.; Martos, J. Treatment of fluorosis spots using a resin infiltration technique: 14- month follow-up. Oral Health Prev. Dent. 2015, 13, 317–322. [Google Scholar] [CrossRef]
- Belli, R.; Rahiotis, C.; Schubert, E.W.; Baratieri, L.N.; Petschelt, A.; Lohabauer, U. Wear and morphology of infiltrated white spot lesions. J. Dent. 2011, 39, 376–385. [Google Scholar] [CrossRef]
- Mathu-Muju, K.; Wright, J.T. Diagnosis and treatment of molar incisor hypomineralization. Compend. Contin. Educ. Dent. 2006, 27, 604–611. [Google Scholar] [PubMed]
- Thylstrup, A.; Fejerskov, O. Clinical appearance of dental fluorosis in permanent teeth in relation to histological changes. Community Dent. Oral Epidemiol. 1978, 6, 315–328. [Google Scholar] [CrossRef] [PubMed]
- Hickel, R.; Peschke, A.; Tyas, M.; Mjör, I.; Bayne, S.; Peters, M.; Hiller Kam Randall, R.; Vanherle, G.; Heintze, S.D. FDI World Dental Federation: Clinical criteria for the evaluation of direct and indirect restorations-update and clinical examples. Clin. Oral Investig. 2010, 14, 349–366. [Google Scholar] [CrossRef] [PubMed]
- Nahsan, F.P.; Da Silva, L.M.; Baseggio, W.; Franco, E.B.; Francisconi, P.A.; Mondelli, R.F.; Wang, L. Conservative approach for a clinical resolution of enamel white spot lesions. Quintessence Int. 2011, 42, 423–426. [Google Scholar]
- Perdigão, J. Resin infiltration of enamel white spot lesions: An ultramorphological analysis. J. Esthet. Restor. Dent. 2020, 32, 317–324. [Google Scholar] [CrossRef]
- Paris, S.; Schwendicke, F.; Keltsch, J.; Dörfer, C.; Meyer-Lueckel, H. Masking of white spot lesions by resin infiltration in vitro. J. Dent. 2013, 4, 28–34. [Google Scholar] [CrossRef] [PubMed]
- Marouane, O.; Manton, D.J. The influence of lesion characteristics on application time of an infiltrate applied to MIH lesions on anterior teeth: An exploratory in vivo pilot study. J. Dent. 2021, 115, 103814. [Google Scholar] [CrossRef]
- Muñoz, M.A.; Arana-Gordillo, L.A.; Gomes, G.M.; Gomes, O.M.; Bombarda, N.H.; Reis, A.; Loguercio, A.D. Alternative esthetic management of fluorosis and hypoplasia stains: Blending effect obtained with resin infiltration techniques. J. Esthet. Restor. Dent. 2013, 25, 32–39. [Google Scholar] [CrossRef] [PubMed]
- Gençer, M.D.G.; Kirzioğlu, Z. A comparison of the effectiveness of resin infiltration and microabrasion treatments applied to developmental enamel defects in color masking. Dent. Mater. J. 2019, 38, 295–302. [Google Scholar] [CrossRef]
- Saxena, P.; Grewal, M.S.; Agarwal, P.; Kaur, G.; Verma, J.; Chhikara, V. Clinical Efficacy of Resin Infiltration Technique Alone or in Combination with Micro Abrasion and in-Office Bleaching in Adults with Mild-to-Moderate Fluorosis Stains. J. Pharm. Bioallied Sci. 2021, 13, 301–305. [Google Scholar] [CrossRef] [PubMed]
- Mazur, M.; Westland, S.; Ndokaj, A.; Nardi, G.M.; Guerra, F.; Ottolenghi, L. In-vivo colour stability of enamel after ICON treatment at 6 years of follow-up: A prospective single center study. J. Dent. 2022, 122, 103943. [Google Scholar] [CrossRef]
- Almulhim, K.; Khan, A.S.; Alabdulghani, H.; Albasarah, S.; Al-Dulaijan, Y.; Al-Qarni, F.D. Effect of Ageing Process and Brushing on Color Stability and Surface Roughness of Treated White Spot Lesions: An in vitro Analysis. Clin. Cosmet. Investig. Dent. 2021, 13, 413–419. [Google Scholar] [CrossRef]
- Alqahtani, S.; Abusaq, A.; Alghamdi, M.; Shokair, N.; Albounni, R. Colour stability of resin infiltrated white spot lesion after exposure to stain-causing drinks. Saudi J. Biol. Sci. 2022, 29, 1079–1084. [Google Scholar] [CrossRef]
- Shan, D.; He, Y.; Gao, M.; Liu, H.; Zhu, Y.; Liao, L.; Hadaegh, F.; Long, H.; Lai, W. A comparison of resin infiltration and microabrasion for postorthodontic white spot lesion. Am. J. Orthod. Dentofac. Orthop. 2021, 160, 516–522. [Google Scholar] [CrossRef] [PubMed]
- Americano, G.C.; Jacobsen, P.E.; Soviero, V.M.; Haubek, D. A systematic review on the association between molar incisor hypomineralization and dental caries. Int. J. Pead. Dent. 2016, 27, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Nogueira, V.K.C.; Mendes Soares, I.P.; Fragelli, C.M.B.; Boldieri, T.; Manton, D.J.; Bussaneli, D.G.; Cordeiro, R.C.L. Structural integrity of MIH-affected teeth after treatment with fluoride varnish or resin infiltration: An 18-Month randomized clinical trial. J. Dent. 2021, 105, 103570. [Google Scholar] [CrossRef] [PubMed]
- Taher, N.M.; Alkhamis, H.A.; Dowaidi, S.M. The influence of resin infiltration system on enamel microhardness and surface roughness:an in vistro study. Saudi Dent. J. 2012, 24, 79–84. [Google Scholar] [CrossRef]
- Jia, L.; Stawarczyk, B.; Schmidlin, P.R.; Attin, T.; Wiegand, A. Effect of caries infiltrant application on shear bond strenght of different adhesive system to sound and demineralized enamel. J. Adhes. Dent. 2012, 14, 569–574. [Google Scholar]
- Marouane, O.; Chtioui, F. Transillumination-aided infiltration: A diagnostic concept for treating enamel opacities. J. Esthet. Restor. Dent. 2020, 32, 451–456. [Google Scholar] [CrossRef]
- Pasini, M.; Giuca, M.R.; Scatena, M.; Gatto, R.; Caruso, S. Molar incisor hypomineralization treatment with casein phosphopeptide and amorphous calcium phosphate in children. Minerva. Stomatol. 2018, 67, 20–25. [Google Scholar] [CrossRef]
- Giuca, M.R.; Lardani, L.; Pasini, M.; Beretta, M.; Gallusi, G.; Campanella, V. State-of-the-art on MIH. Part. 1 Definition and aepidemiology. Eur. J. Paediatr. Dent. 2020, 21, 80–82. [Google Scholar] [PubMed]
- Esenlik, E.; Uzer Çelik, E.; Bolat, E. Efficacy of a casein phosphopeptide amorphous calcium phosphate (CPP-ACP) paste in preventing white spot lesions in patients with fixed orthodontic appliances: A prospective clinical trial. Eur. J. Paediatr. Dent. 2016, 17, 274–280. [Google Scholar] [PubMed]
- Sekundo, C.; Frese, C. Underlying Resin Infiltration and Direct Composite Veneers for the Treatment of Severe White Color Alterations of the Enamel: Case Report and 13-Month Follow-Up. Oper. Dent. 2020, 45, 10–18. [Google Scholar] [CrossRef] [PubMed]






| Variable | N (%) |
|---|---|
| DDE Type | |
| 1. Moderate or low-grade MIH | 24 (72.7) |
| 2. Moderate or low-grade Fluorosis | 5 (15.2) |
| 3. Trauma | 4 (12.1) |
| Treated teeth (mean; 95% CI) | 3.5 (2.9–4.0) |
| Age in years (mean; 95% CI) | 11 (10.4–11.6) |
| Index/Variable | Values | |||||
|---|---|---|---|---|---|---|
| FDI | 1 | 2 | 3 | 4 | 5 | |
| Time 0 | 6 (18.2) | 16 (48.5) | 11 (33.3) | |||
| Time 1 | 20 (60.6) | 6 (18.2) | 2 (6.1) | 5 (15.1) | ||
| Time 2 | 20 (60.6) | 7 (21.2) | 4 (12.1) | 2 (6.1) | ||
| Wong Scale | 0 | 2 | 4 | 6 | 8 | 10 |
| Time 0 | 14 (42.4) | 7 (21.2) | 4 (12.1) | 1 (3.1) | 5 (15.1) | 2 (6.1) |
| Time 1 | 26 (78.8) | 4 (12.1) | 3 (9.1) | |||
| Time 2 | 28 (84.9) | 5 (15.1) | ||||
| Shiff Air Index | 0 | 1 | 2 | 3 | ||
| Time 0 | 17 (51.5) | 5 (15.1) | 3 (9.1) | 8 (24.3) | ||
| Time 1 | 27 (81.8) | 4 (12.1) | 2 (6.1) | |||
| Time 2 | 27 (81.8) | 6 (18.2) | ||||
| Variable | Coefficient | 95% C.I. | p-Value |
|---|---|---|---|
| DDE Type | |||
| 1. Moderate or low-grade MIH | Reference | ||
| 2. Moderate or low-grade Fluorosis | 0.6 | (−0.1, −1.3) | 0.09 |
| 3. Trauma | 0.5 | (−0.3, 1.3) | 0.2 |
| Time | |||
| 0 | Reference | ||
| 1 | −2.5 | (−2.8, −2.2) | <0.001 |
| 2 | −2.5 | (−2.8, −2.3) | <0.001 |
| Interaction WSL Type × Time | |||
| 1 × 0 | Reference | ||
| 2 × 1 | −0.9 | (−1.6, −0.2) | 0.009 |
| 2 × 2 | −0.9 | (–1.5, −0.2) | 0.012 |
| 3 × 1 | 2 | (1.3, 2.7) | <0.001 |
| 3 × 2 | 1.3 | (0.6, 2.0) | 0.001 |
| Variable | Coefficient | 95% C.I. | p-Value |
|---|---|---|---|
| DDE Type | |||
| 1. Moderate or low-grade MIH | Reference | ||
| 2. Moderate or low-grade Fluorosis | −0.5 | (−2.5, 1.6) | 0.7 |
| 3. Trauma | −2.3 | (−4.5, 0.1) | 0.052 |
| Time | |||
| 0 | Reference | ||
| 1 | −2.4 | (−3.3, −1.5) | <0.001 |
| 2 | −2.8 | (−3.7, −1.9) | <0.001 |
| Interaction WSL Type × Time | |||
| 1 × 0 | Reference | ||
| 2 × 1 | −0.4 | (−2.6, 1.8) | 0.7 |
| 2 × 2 | 0.1 | (−2.2, 2.2) | 0.9 |
| 3 × 1 | 1.4 | (−1.0, 3.8) | 0.3 |
| 3 × 2 | 1.8 | (−0.6, 4.2) | 0.1 |
| Variable | Coefficient | 95% C.I. | p-Value |
|---|---|---|---|
| DDE Type | |||
| 1. Moderate or low-grade MIH | Reference | ||
| 2. Moderate or low-grade Fluorosis | 0.3 | (−0.5, 1.1) | 0.5 |
| 3. Trauma | −0.6 | (−1.5, 0.3) | 0.2 |
| Time | |||
| 0 | Reference | ||
| 1 | −0.8 | (−1.2, −0.5) | <0.001 |
| 2 | −0.9 | (−1.2, −0.5) | <0.001 |
| Interaction WSL Type × Time | |||
| 1 × 0 | Reference | ||
| 2 × 1 | −0.2 | (−1.0, 0.7) | 0.7 |
| 2 × 2 | −0.3 | (−1.2, 0.5) | 0.4 |
| 3 × 1 | 0.3 | (−0.6, 1.3) | 0.5 |
| 3 × 2 | 0.4 | (−0.5, 1.3) | 0.4 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Brescia, A.V.; Montesani, L.; Fusaroli, D.; Docimo, R.; Di Gennaro, G. Management of Enamel Defects with Resin Infiltration Techniques: Two Years Follow Up Retrospective Study. Children 2022, 9, 1365. https://doi.org/10.3390/children9091365
Brescia AV, Montesani L, Fusaroli D, Docimo R, Di Gennaro G. Management of Enamel Defects with Resin Infiltration Techniques: Two Years Follow Up Retrospective Study. Children. 2022; 9(9):1365. https://doi.org/10.3390/children9091365
Chicago/Turabian StyleBrescia, Alessia Vincenza, Lorenzo Montesani, Dimitri Fusaroli, Raffaella Docimo, and Gianfranco Di Gennaro. 2022. "Management of Enamel Defects with Resin Infiltration Techniques: Two Years Follow Up Retrospective Study" Children 9, no. 9: 1365. https://doi.org/10.3390/children9091365
APA StyleBrescia, A. V., Montesani, L., Fusaroli, D., Docimo, R., & Di Gennaro, G. (2022). Management of Enamel Defects with Resin Infiltration Techniques: Two Years Follow Up Retrospective Study. Children, 9(9), 1365. https://doi.org/10.3390/children9091365