Back-Carrying in Children Is Related to Lower Limb Development †
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Procedure
2.3. Statistical Analysis
3. Results
3.1. General Participant Descriptive Data
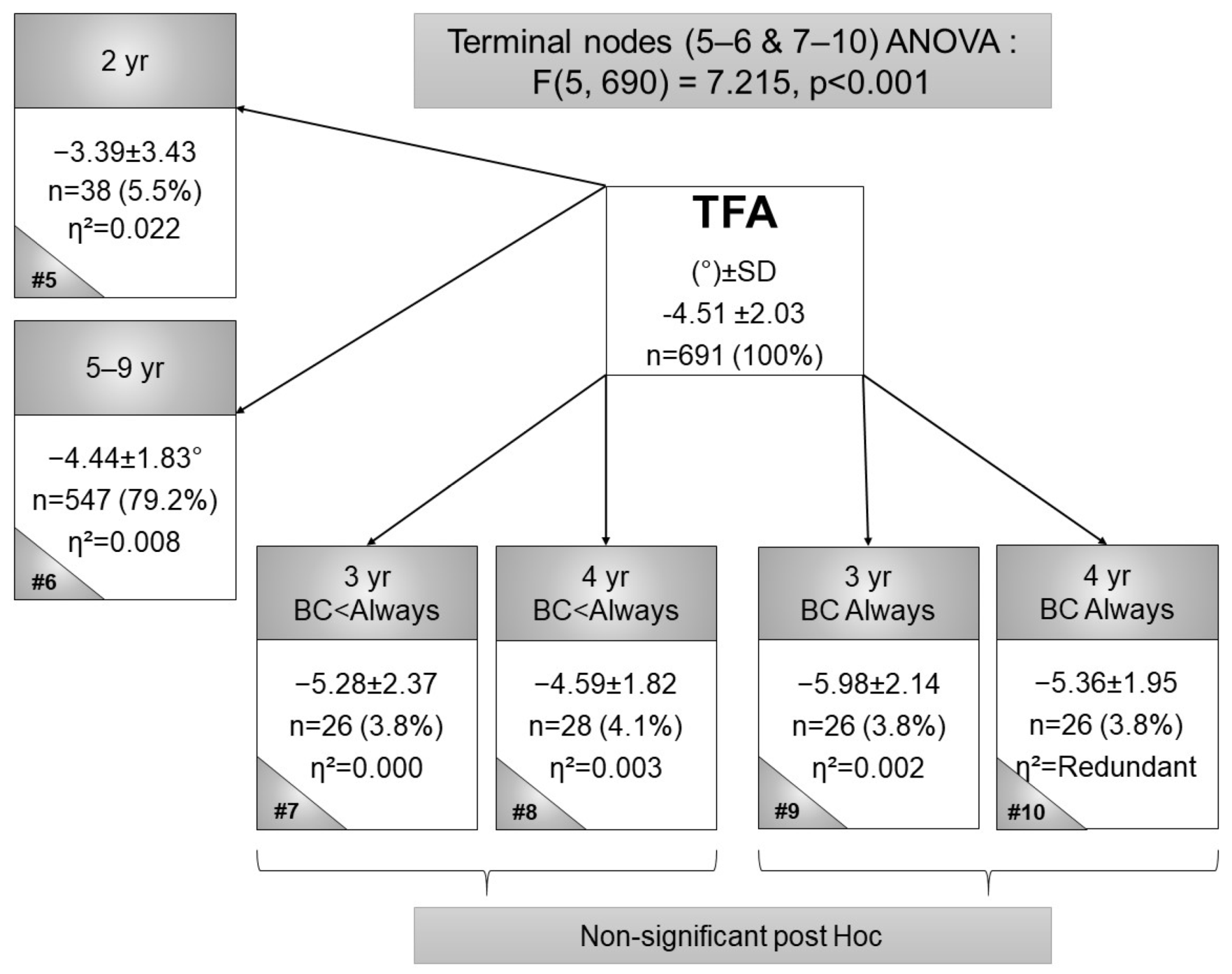
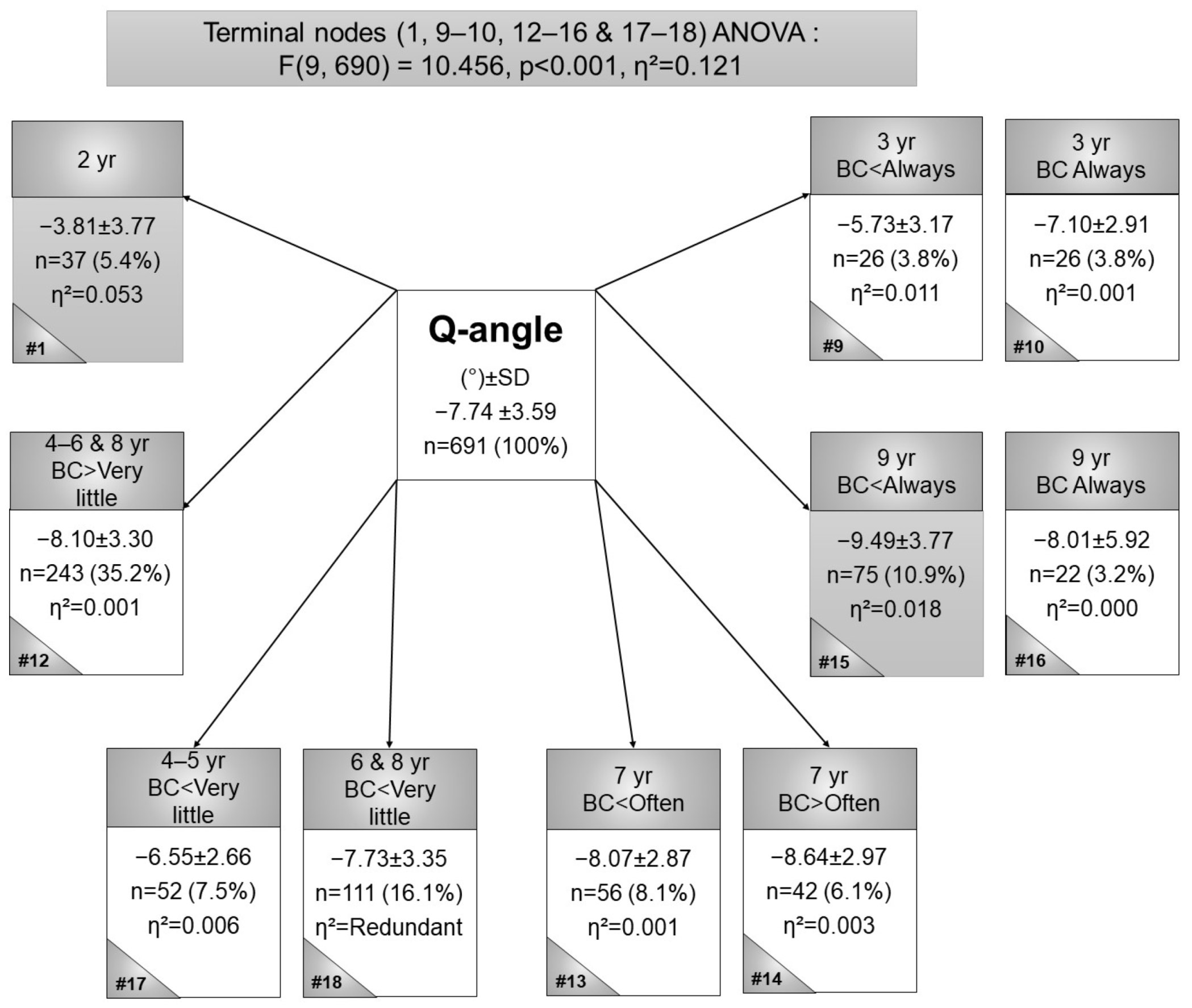
3.2. Frontal Plane Measures: Tibiofemoral Angle, Intermalleolar Distance, and Quadriceps Angle
3.3. Measurement in Transverse Plane: Tibial Torsion and Anteversion
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Pretorius, E.; Naudé, H.; Van Vuuren, C. Can Cultural Behavior have a Negative Impact on the Development of Visual Integration Pathways? Early Child Dev. Care 2002, 172, 173–181. [Google Scholar] [CrossRef]
- Graham, S.M.; Manara, J.; Chokotho, L.; Harrison, W.J. Back-carrying infants to prevent developmental hip dysplasia and its sequelae: Is a new public health initiative needed? J. Pediatric Orthop. 2015, 35, 57–61. [Google Scholar] [CrossRef] [PubMed]
- Pretorius, E.; Naudé, H. Results from an Empirical Study: The impact of carrying a child on the back on the development of visual integration pathways. Early Child Dev. Care 2002, 172, 585–594. [Google Scholar] [CrossRef]
- Golding, J. The mechanical factors which influence bone growth. Eur. J. Clin. Nutr. 1994, 48, S178. [Google Scholar] [PubMed]
- Stroebel, S.; De Ridder, J.H.; Wilders, C.J. Postural deformities in children: A review: Sports medicine. Afr. J. Phys. Health Educ. Recreat. Danc. 2009, 15, 294–330. [Google Scholar]
- Roper, A. Hip dysplasia in the African Bantu. Bone Jt. J. 1976, 58, 155–158. [Google Scholar] [CrossRef]
- van Meerdervoort, H.P. Congenital dislocation of the hip in black patients. S. Afr. Med. J. 1974, 48, 2436–2440. [Google Scholar]
- Griffiths, J. Dislocated hip in East African infants and children. Postgrad. Med. J. 1970, 46, 86. [Google Scholar] [CrossRef]
- Loder, R.T.; Shafer, C. The demographics of developmental hip dysplasia in the Midwestern United States (Indiana). J. Child. Orthop. 2015, 9, 93–98. [Google Scholar] [CrossRef]
- Espandar, R.; Mortazavi, S.M.-J.; Baghdadi, T. Angular deformities of the lower limb in children. Asian J. Sports Med. 2010, 1, 46–53. [Google Scholar] [CrossRef]
- Peterson-Kendall, F.; Kendall-McCreary, E.; Geise-Provance, P.; McIntyre-Rodgers, M.; Romani, W. Muscles Testing and Function with Posture and Pain, 5th ed.; Lippincott Williams & Wilkins: Baltimore, MD, USA, 2005. [Google Scholar]
- Knight, R.A. Developmental deformities of the lower extremities. J. Bone Jt. Surg. 1954, 36, 521–558. [Google Scholar] [CrossRef]
- Leveau, B.F.; Bernhardt, D.B. Developmental biomechanics: Effect of forces on the growth, development, and maintenance of the human body. Phys. Ther. 1984, 64, 1874–1882. [Google Scholar] [CrossRef] [PubMed]
- Omololu, B.; Tella, A.; Ogunlade, S.; Adeyemo, A.; Adebisi, A.; Alonge, T.; Salawu, S.; Akinpelu, A. Normal values of knee angle, intercondylar and intermalleolar distances in Nigerian children. West Afr. J. Med. 2003, 22, 301–304. [Google Scholar] [CrossRef] [PubMed]
- van Aswegen, M.; Czyz, S.; Moss, S. The Profile and Development of the Lower limb in Setswana-speaking children between the ages of 2 and 9 years. Int. J. Environ. Res. Public Health 2020, 17, 3245. [Google Scholar] [CrossRef] [PubMed]
- Omololu, B.B.; Ogunlade, O.S.; Gopaldasani, V.K. Normal Q-angle in an adult Nigerian population. Clin. Orthop. Relat. Res. 2009, 467, 2073–2076. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saini, U.C.; Bali, K.; Sheth, B.; Gahlot, N.; Gahlot, A. Normal development of the knee angle in healthy Indian children: A clinical study of 215 children. J. Child. Orthop. 2010, 4, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.C.; Chan, P.; Chiang, S.; Hui, P. Angular and rotational profile of the lower limb in 2630 Chinese children. J. Pediatric Orthop. 1991, 11, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Cahuzac, J.; Vardon, D.; de Gauzy, J.S. Development of the clinical tibiofemoral angle in normal adolescents. A study of 427 normal subjects from 10 to 16 years of age. Bone Jt. J. 1995, 77, 729–732. [Google Scholar] [CrossRef]
- Arazi, M.; Ögün, T.C.; Memik, R. Normal development of the tibiofemoral angle in children: A clinical study of 590 normal subjects from 3 to 17 years of age. J. Pediatric Orthop. 2001, 21, 264–267. [Google Scholar] [CrossRef]
- Jacquemier, M.; Glard, Y.; Pomero, V.; Viehweger, E.; Jouve, J.-L.; Bollini, G. Rotational profile of the lower limb in 1319 healthy children. Gait Posture 2008, 28, 187–193. [Google Scholar] [CrossRef]
- Sass, P.; Hassan, G. Lower extremity abnormalities in children. Am. Fam. Physician 2003, 68, 461–468. [Google Scholar] [PubMed]
- Magee, D.J. Orthopedic Physical Assessment, 4th ed.; Saunders Elsevier: Philadelphia, PA, USA, 2006. [Google Scholar]
- Lewis, R.J. An Introduction to Classification and Regression Tree (CART) Analysis. In Proceedings of the Annual Meeting of the Society for Academic Emergency Medicine, San Francisco, CA, USA, 22–25 May 2000. [Google Scholar]



| TFA | Q-Angle | IMD | AVA | TTA | |||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Age (years) | Total Mean (°) ± SD(n) | Females Mean (°) ± SD (n) | Males Mean (°) ± SD (n) | Total Mean (°) ± SD (n) | Females Mean (°) ± SD (n) | Males Mean (°) ± SD (n) | Total Mean (cm) ± SD (n) | Females Mean (cm) ± SD (n) | Males Mean (cm) ± SD (n) | Total Mean (°) ± SD (n) | Females Mean (°) ± SD (n) | Males Mean (°) ± SD (n) | Total Mean (°) ± SD (n) | Females Mean (°) ± SD (n) | Males Mean (°) ± SD (n) |
| 2 | −3.39 ± 3.43 (n = 38) | −4.00 ± 3.46 (n = 15) | −2.99 ± 3.43 (n = 23) | −3.81 ± 3.77 (n = 38) | −4.55 ± 3.32 (n = 15) | −3.33 ± 4.03 (n = 23) | −2.09 ± 1.76 (n = 37) | −2.94 ± 1.56 (n = 14) | −1.58 ± 1.70 (n = 23) | 75.82 ± 18.87 (n = 37) | 75.30 ± 15.23 (n = 14) | 76.13 ± 21.10 (n = 23) | 2.03 ± 7.69 (n = 37) | 4.50 ± 7.09 (n = 14) | 0.53 ± 7.79 (n = 23) |
| 3 | −5.63 ± 2.26 (n = 52) | −5.70 ± 1.83 (n = 24) | −4.86 ± 1.72 (n = 26) | −6.41 ± 3.09 (n = 52) | −7.08 ± 2.71 (n = 24) | −5.84 ± 3.31 (n = 28) | −2.71 ± 1.76 (n = 52) | −2.29 ± 1.68 (n = 24) | −3.08 ± 1.78 (n = 28) | 77.61 ± 13.75 (n = 52) | 79.53 ± 4.36 (n = 24) | 75.96 ± 18.29 (n = 28) | 8.24 ± 4.74 (n = 52) | 8.38 ± 3.62 (n = 24) | 8.13 ± 5.59 (n = 28) |
| 4 | −4.97 ± 1.90 (n = 54) | −5.01 ± 2.08 (n = 29) | −4.86 ± 1.72 (n = 26) | −7.46 ± 2.92 (n = 54) | −8.16 ± 3.11 (n = 29) | −6.65 ± 2.49 (n = 25) | −2.03 ± 1.28 (n = 53) | −2.04 ± 1.30 (n = 28) | −2.01 ± 1.29 (n = 25) | 75.70 ± 7.02 (n = 52) | 74.96 ± 3.50 (n = 27) | 76.50 ± 9.49 (n = 25) | 11.21 ± 3.94 (n = 51) | 11.14 ± 3.46 (n = 27) | 11.28 ± 4.49 (n = 24) |
| 5 | −4.71 ± 2.02 (n = 112) | −5.13 ± 2.01 (n = 54) | −4.36 ± 2.00 (n = 56) | −7.59 ± 3.40 (n = 112) | −8.09 ± 3.65 (n = 54) | −7.13 ± 3.10 (n = 58) | −1.84 ± 1.51 (n = 112) | −1.79 ± 1.34 (n = 54) | −1.89 ± 1.67 (n = 58) | 75.19 ± 8.24 (n = 111) | 76.41 ± 6.07 (n = 54) | 74.06 ± 9.76 (n = 57) | 11.24 ± 4.73 (n = 111) | 11.40 ± 5.08 (n = 54) | 11.08 ± 4.42 (n = 57) |
| 6 | −4.29 ± 1.61 (n = 113) | −4.43 ± 1.78 (n = 50) | −4.20 ± 1.46 (n = 63) | −7.96 ± 3.29 (n = 113) | −8.68 ± 3.56 (n = 50) | −7.39 ± 2.96 (n = 63) | −1.15 ± 1.18 (n = 113) | −1.22 ± 1.30 (n = 50) | −1.10 ± 1.09 (n = 63) | 70.37 ± 7.96 (n = 113) | 68.73 ± 7.09 (n = 50) | 71.67 ± 8.42 (n = 63) | 9.68 ± 5.62 (n = 112) | 9.66 ± 5.83 (n = 50) | 9.69 ± 5.48 (n = 62) |
| 7 | −4.40 ± 1.60 (n = 98) | −4.67 ± 1.56 (n = 51) | −4.01 ± 1.61 (n = 50) | −8.32 ± 2.91 (n = 98) | −8.44 ± 2.94 (n = 51) | −8.18 ± 2.91 (n = 47) | −1.11 ± 1.21 (n = 98) | −1.25 ± 1.23 (n = 51) | −0.95 ± 1.18 (n = 47) | 70.92 ± 7.85 (n = 97) | 69.91 ± 8.25 (n = 51) | 72.05 ± 7.30 (n = 46) | 11.17 ± 5.88 (n = 98) | 11.11 ± 6.27 (n = 51) | 11.24 ± 5.49 (n = 47) |
| 8 | −4.25 ± 1.77 (n = 127) | −4.53 ± 1.71 (n = 77) | −3.80 ± 1.73 (n = 47) | −7.98 ± 3.30 (n = 127) | −8.29 ± 3.31 (n = 77) | −7.49 ± 3.25 (n = 50) | −1.23 ± 1.63 (n = 127) | −1.49 ± 1.71 (n = 77) | −0.84 ± 1.40 (n = 50) | 69.75 ± 11.02 (n = 126) | 69.30 ± 9.34 (n = 77) | 70.44 ± 13.28 (n = 49) | 12.39 ± 5.39 (n = 127) | 12.26 ± 5.22 (n = 77) | 12.58 ± 5.69 (n = 50) |
| 9 | −4.58 ± 2.09 (n = 97) | −4.95 ± 1.99 (n = 56) | −4.14 ± 2.17 (n = 42) | −9.16 ± 4.36 (n = 97) | −9.66 ± 4.27 (n = 56) | −8.47 ± 4.45 (n = 41) | −0.95 ± 1.40 (n = 97) | −1.09 ± 1.44 (n = 56) | −0.76 ± 1.33 (n = 41) | 70.77 ± 6.92 (n = 96) | 71.30 ± 6.25 (n = 55) | 70.06 ± 7.75 (n = 41) | 12.75 ± 5.54 (n = 97) | 12.31 ± 6.06 (n = 56) | 13.35 ± 4.76 (n = 41) |
| Total | −4.51 ± 2.03 (n = 691) | −4.79 *** ± 1.95 (n = 356) | −4.22 *** ± 2.07 (n = 335) | −7.74 ± 3.59 (n = 691) | −8.30 *** ± 3.58 (n = 356) | −7.14 *** ± 3.51 (n = 335) | −1.48 ± 0.06 (n = 689) | −1.56 ± 1.51 (n = 354) | −1.40 ± 1.55 (n = 335) | 72.42 ± 6.92 (n = 684) | 72.08 ± 8.35 (n = 352) | 72.78 ± 2.07 (n = 332) | 10.67 ± 5.93 (n = 685) | 10.94 ± 5.70 (n = 353) | 10.38 ± 13.71 (n = 332) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
van Aswegen, M.; Czyż, S.H.; Moss, S.J.; Steffens, F. Back-Carrying in Children Is Related to Lower Limb Development. Children 2022, 9, 263. https://doi.org/10.3390/children9020263
van Aswegen M, Czyż SH, Moss SJ, Steffens F. Back-Carrying in Children Is Related to Lower Limb Development. Children. 2022; 9(2):263. https://doi.org/10.3390/children9020263
Chicago/Turabian Stylevan Aswegen, Mariaan, Stanisław H. Czyż, Sarah J. Moss, and Francois Steffens. 2022. "Back-Carrying in Children Is Related to Lower Limb Development" Children 9, no. 2: 263. https://doi.org/10.3390/children9020263
APA Stylevan Aswegen, M., Czyż, S. H., Moss, S. J., & Steffens, F. (2022). Back-Carrying in Children Is Related to Lower Limb Development. Children, 9(2), 263. https://doi.org/10.3390/children9020263






