Initial Use of 100% but Not 60% or 30% Oxygen Achieved a Target Heart Rate of 100 bpm and Preductal Saturations of 80% Faster in a Bradycardic Preterm Model
Abstract
1. Introduction
2. Materials and Methods
- (a)
- It will be adjusted by 10% if SpO2 is less than 10% outside the range (e.g., target SpO2 70%, previous minute SpO2 60%, then increase O2 by 10%) or
- (b)
- It will be adjusted by 20% if SpO2 is greater than 10% outside the range (e.g., target SpO2 80%, previous minute SpO2 50%, then increase O2 concentration by 20%).
3. Results
3.1. Primary Outcome
3.2. Time Taken to Achieve an HR ≥ 100 bpm and SpO2 ≥ 80%
3.3. Preductal Saturations, Supplemental Oxygen Use, Oxygenation, and Ventilation
3.3.1. Preductal Saturations
3.3.2. Supplemental Oxygen Use
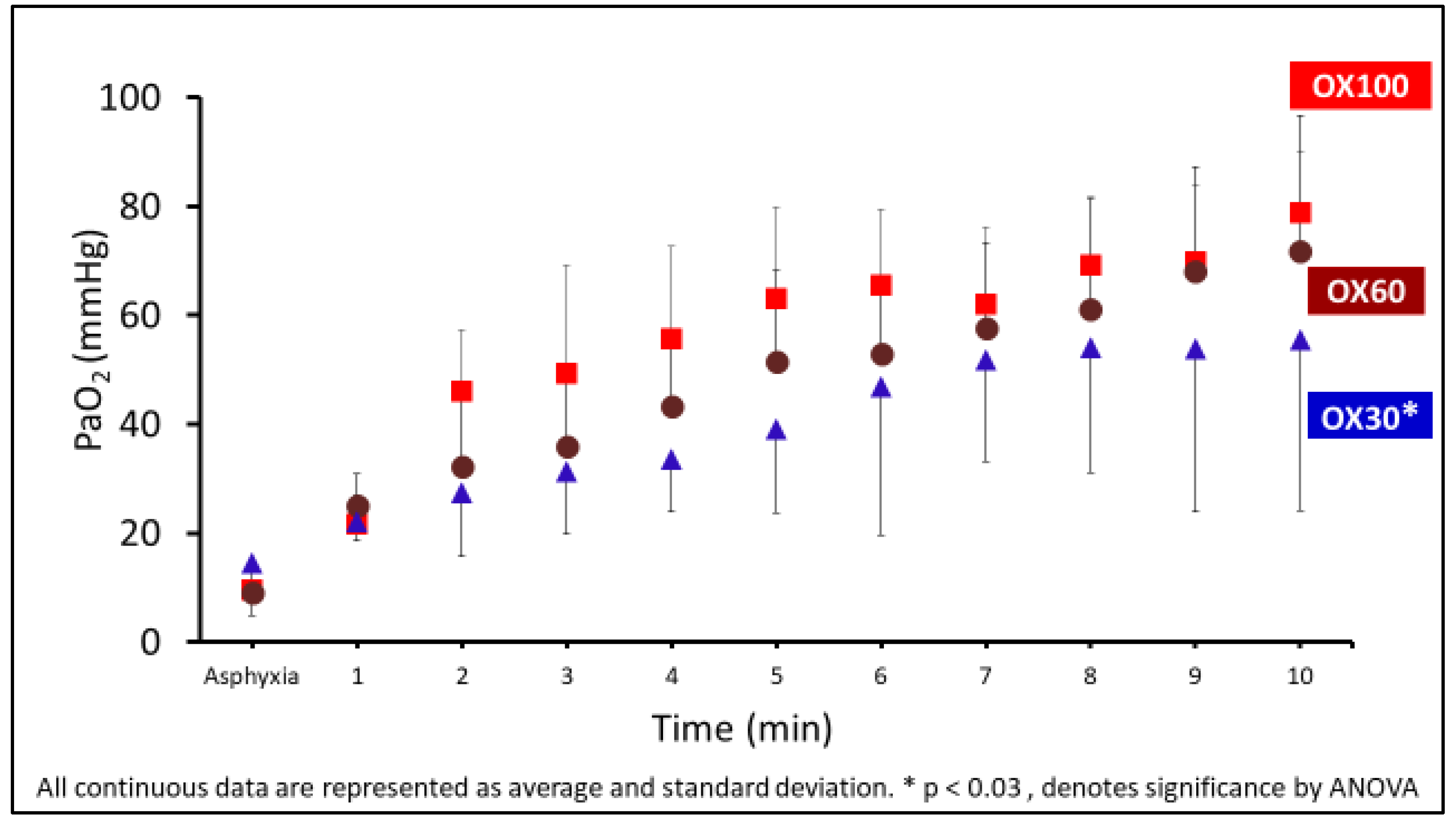
3.3.3. Arterial Oxygenation (PaO2)
3.3.4. Ventilation
3.4. Hemodynamics
3.4.1. Peak Pulmonary Blood Flow
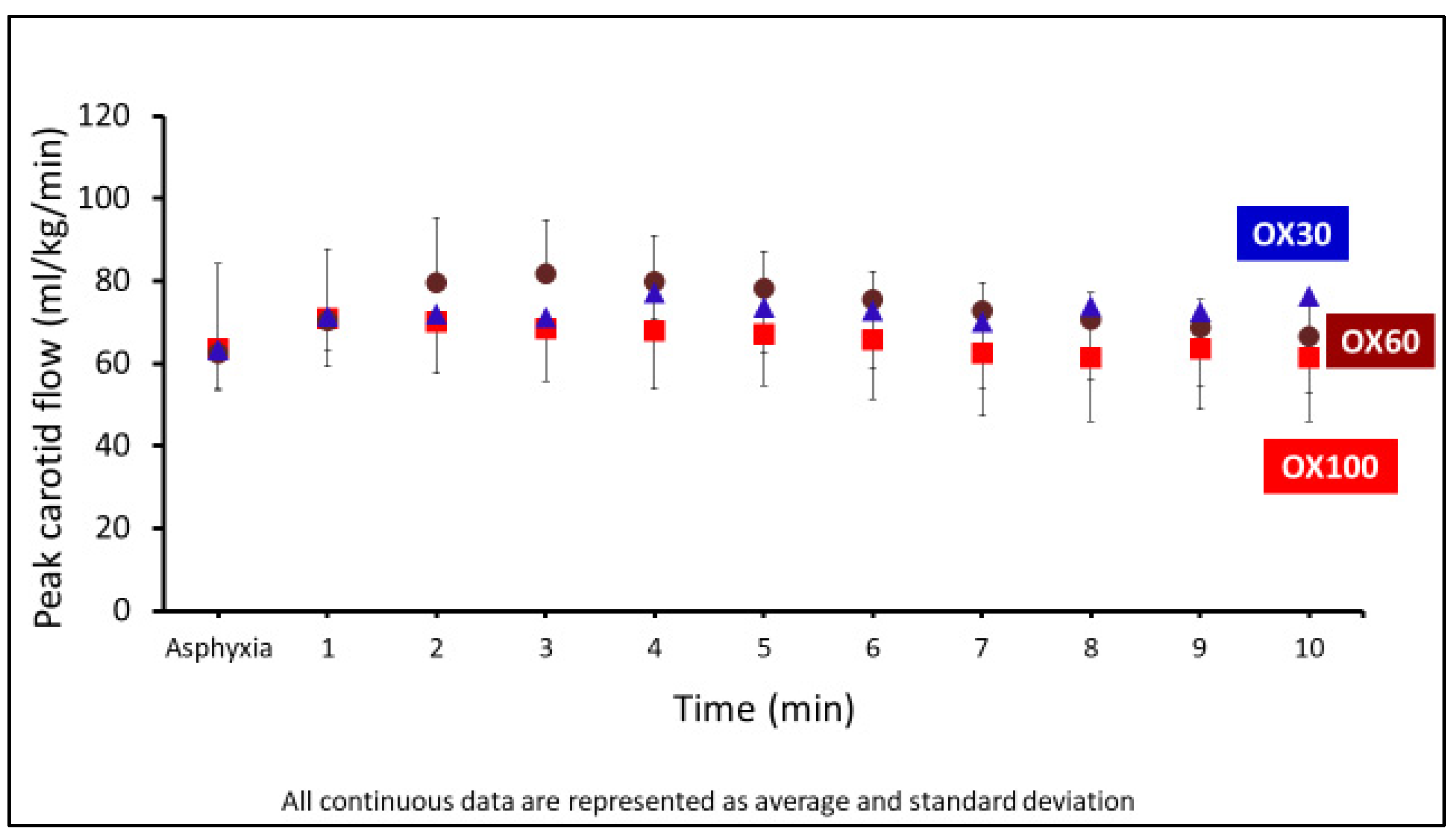
3.4.2. Peak Carotid Blood Flow
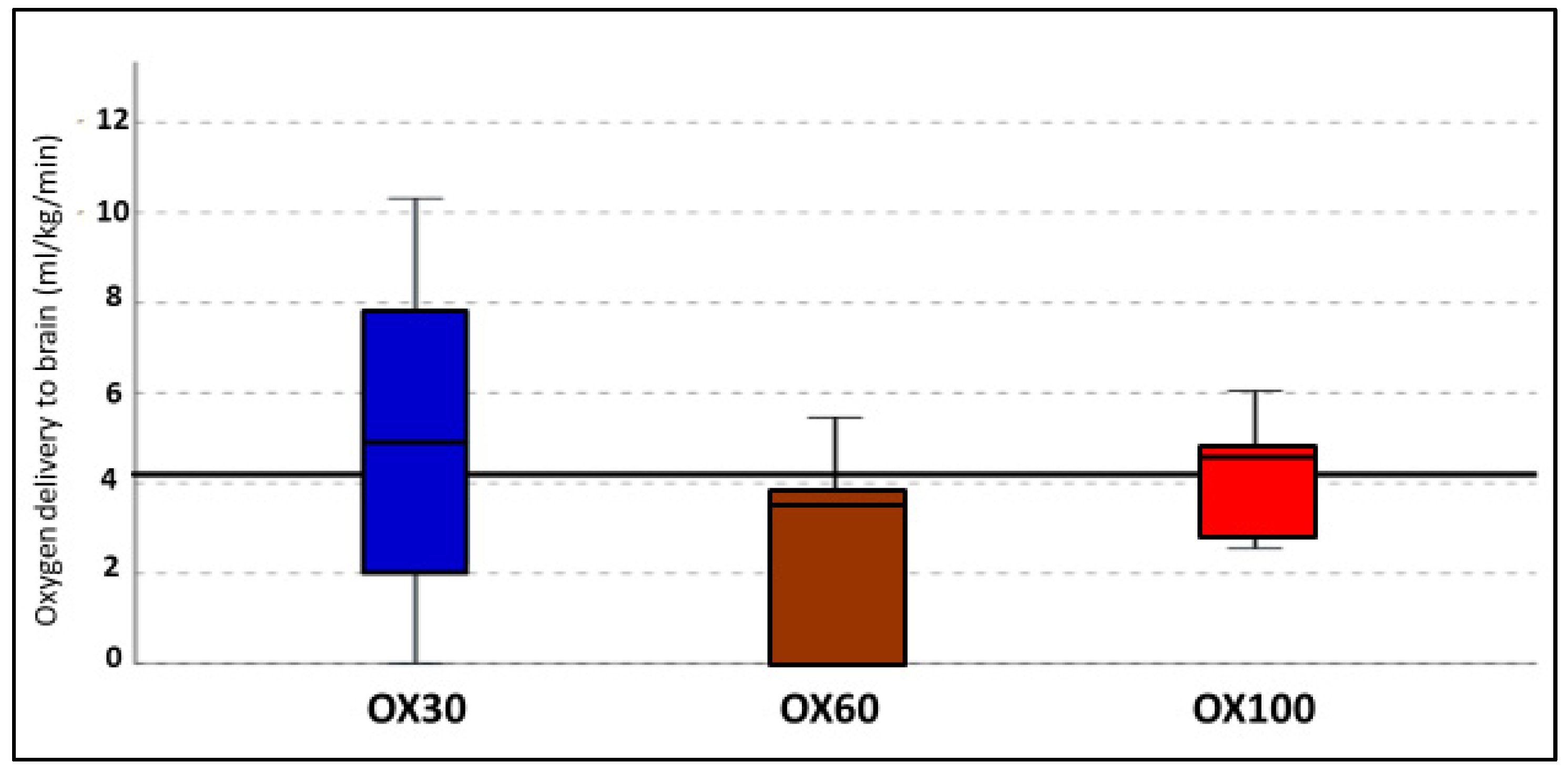
3.5. Oxygen Delivery to the Brain
3.6. Oxidized to Reduced Glutathione Ratio between the Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kapadia, V.; Oei, J.L.; Finer, N.; Rich, W.; Rabi, Y.; Wright, I.M.; Rook, D.; Vermeulen, M.J.; Tarnow-Mordi, W.O.; Smyth, J.P.; et al. Outcomes of delivery room resuscitation of bradycardic preterm infants: A retrospective cohort study of randomised trials of high vs low initial oxygen concentration and an individual patient data analysis. Resuscitation 2021, 167, 209–217. [Google Scholar] [CrossRef] [PubMed]
- Textbook of Neonatal Resuscitation, 8th ed.; American Academy of Pediatrics: Itasca, IL, USA, 2021. [CrossRef]
- Textbook of Neonatal Resuscitation (NRP), 7th ed.; American Academy of Pediatrics: Itasca, IL, USA, 2016; 326p.
- Oei, J.L.; Finer, N.N.; Saugstad, O.D.; Wright, I.M.; Rabi, Y.; Tarnow-Mordi, W.; Rich, W.; Kapadia, V.; Rook, D.; Smyth, J.P.; et al. Outcomes of oxygen saturation targeting during delivery room stabilisation of preterm infants. Arch. Dis. Child Fetal. Neonatal. Ed. 2017, 103, F446–F454. [Google Scholar] [CrossRef] [PubMed]
- Wyckoff, M.H.; Wyllie, J.; Aziz, K.; de Almeida, M.F.; Fabres, J.; Fawke, J.; Guinsburg, R.; Hosono, S.; Isayama, T.; Kapadia, V.S.; et al. Neonatal Life Support: 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Circulation 2020, 142, S185–S221. [Google Scholar] [CrossRef] [PubMed]
- Wyckoff, M.H.; Wyllie, J.; Aziz, K.; de Almeida, M.F.; Fabres, J.W.; Fawke, J.; Guinsburg, R.; Hosono, S.; Isayama, T.; Kapadia, V.S.; et al. Neonatal Life Support 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Resuscitation 2020, 156, A156–A187. [Google Scholar] [CrossRef] [PubMed]
- Saugstad, O.D.; Kapadia, V.; Oei, J.L. Oxygen in the First Minutes of Life in Very Preterm Infants. Neonatology 2021, 118, 218–224. [Google Scholar] [CrossRef]
- Chandrasekharan, P.; Rawat, M.; Gugino, S.F.; Koenigsknecht, C.; Helman, J.; Nair, J.; Vali, P.; Lakshminrusimha, S. Effect of various inspired oxygen concentrations on pulmonary and systemic hemodynamics and oxygenation during resuscitation in a transitioning preterm model. Pediatr. Res. 2018, 84, 743–750. [Google Scholar] [CrossRef]
- Rawat, M.; Chandrasekharan, P.; Gugino, S.F.; Koenigsknecht, C.; Nielsen, L.; Wedgwood, S.; Mathew, B.; Nair, J.; Steinhorn, R.; Lakshminrusimha, S. Optimal Oxygen Targets in Term Lambs with Meconium Aspiration Syndrome and Pulmonary Hypertension. Am. J. Respir. Cell Mol. Biol. 2020, 63, 510–518. [Google Scholar] [CrossRef]
- Vento, M. Oxygen supplementation in the neonatal period: Changing the paradigm. Neonatology 2014, 105, 323–331. [Google Scholar] [CrossRef]
- Saugstad, O.D.; Lakshminrusimha, S.; Vento, M. Optimizing Oxygenation of the Extremely Premature Infant during the First Few Minutes of Life: Start Low or High? J. Pediatr. 2020, 227, 295–299. [Google Scholar] [CrossRef]
- van Leuteren, R.W.; Scholten, A.W.J.; Dekker, J.; Martherus, T.; de Jongh, F.H.; van Kaam, A.H.; Te Pas, A.B.; Hutten, J. The Effect of Initial Oxygen Exposure on Diaphragm Activity in Preterm Infants at Birth. Front. Pediatr. 2021, 9, 640491. [Google Scholar] [CrossRef]
- Dekker, J.; Hooper, S.B.; Te Pas, A.B. Optimizing oxygenation of the preterm infant directly at birth: Focus of future studies. J. Pediatr. 2021, 229, 309. [Google Scholar] [CrossRef]
- Dekker, J.; Hooper, S.B.; Giera, M.; McGillick, E.V.; Hutten, G.J.; Onland, W.; van Kaam, A.H.; Te Pas, A.B. High vs. Low Initial Oxygen to Improve the Breathing Effort of Preterm Infants at Birth: Study Protocol for a Randomized Controlled Trial. Front. Pediatr. 2019, 7, 179. [Google Scholar] [CrossRef] [PubMed]
- Chandrasekharan, P.; Rawat, M.; Lakshminrusimha, S. How Do We Monitor Oxygenation during the Management of PPHN? Alveolar, Arterial, Mixed Venous Oxygen Tension or Peripheral Saturation? Children 2020, 7, 180. [Google Scholar] [CrossRef] [PubMed]
- Lakshminrusimha, S.; Steinhorn, R.H. Pulmonary vascular biology during neonatal transition. Clin. Perinatol. 1999, 26, 601–619. [Google Scholar] [CrossRef]
- Lakshminrusimha, S.; Vali, P.; Chandrasekharan, P.; Rich, W.; Katheria, A. Differential Alveolar and Systemic Oxygenation during Preterm Resuscitation with 100% Oxygen during Delayed Cord Clamping. Am. J. Perinatol. 2021. [Google Scholar] [CrossRef]
- Markus, T.; Hansson, S.; Amer-Wahlin, I.; Hellstrom-Westas, L.; Saugstad, O.D.; Ley, D. Cerebral inflammatory response after fetal asphyxia and hyperoxic resuscitation in newborn sheep. Pediatr. Res. 2007, 62, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Munkeby, B.H.; Borke, W.B.; Bjornland, K.; Sikkeland, L.I.; Borge, G.I.; Halvorsen, B.; Saugstad, O.D. Resuscitation with 100% O2 increases cerebral injury in hypoxemic piglets. Pediatr. Res. 2004, 56, 783–790. [Google Scholar] [CrossRef]
- Munkeby, B.H.; Borke, W.B.; Bjornland, K.; Sikkeland, L.I.; Borge, G.I.; Lomo, J.; Rivera, S.; Khrestchatisky, M.; Halvorsen, B.; Saugstad, O.D. Resuscitation of hypoxic piglets with 100% O2 increases pulmonary metalloproteinases and IL-8. Pediatr. Res. 2005, 58, 542–548. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Saugstad, O.D.; Ramji, S.; Soll, R.F.; Vento, M. Resuscitation of newborn infants with 21% or 100% oxygen: An updated systematic review and meta-analysis. Neonatology 2008, 94, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Sola, A.; Saldeno, Y.P.; Favareto, V. Clinical practices in neonatal oxygenation: Where have we failed? What can we do? J. Perinatol. 2008, 28 (Suppl. S1), S28–S34. [Google Scholar] [CrossRef]
- Soll, R.F.; Finer, N. Oxygen Redux. Pediatrics 2016, 138, e20163168. [Google Scholar] [CrossRef] [PubMed]
- Vento, M.; Asensi, M.; Sastre, J.; Garcia-Sala, F.; Pallardo, F.V.; Vina, J. Resuscitation with room air instead of 100% oxygen prevents oxidative stress in moderately asphyxiated term neonates. Pediatrics 2001, 107, 642–647. [Google Scholar] [CrossRef]
- Vento, M.; Moro, M.; Escrig, R.; Arruza, L.; Villar, G.; Izquierdo, I.; Roberts, L.J., 2nd; Arduini, A.; Escobar, J.J.; Sastre, J.; et al. Preterm resuscitation with low oxygen causes less oxidative stress, inflammation, and chronic lung disease. Pediatrics 2009, 124, e439–e449. [Google Scholar] [CrossRef]
- Rook, D.; Te Braake, F.W.; Schierbeek, H.; Longini, M.; Buonocore, G.; Van Goudoever, J.B. Glutathione synthesis rates in early postnatal life. Pediatr. Res. 2010, 67, 407–411. [Google Scholar] [CrossRef] [PubMed]




| Parameter | OX30 | OX60 | OX100 |
|---|---|---|---|
| N | 6 | 5 | 7 |
| Gestational age (days) | 127 ± 0.89 | 127 ± 0.84 | 126 ± 0.75 |
| Female (N) | 3 | 3 | 4 |
| Multiplicity | Twins—2 | Twins—3 | Twins—3 |
| pH at asphyxia | 6.92 ± 0.17 | 6.91 ± 0.04 | 6.9 ± 0.18 |
| HR at asphyxia (bpm) | 91 ± 3 | 90 ± 3 | 88 ± 4 |
| Parameter | OX30 | OX60 | OX100 | p-Value |
|---|---|---|---|---|
| Percentage achieving primary outcome (%) | 0 | 40% | 67% | 0.385 |
| Time taken to achieve primary outcome (s) | 600 ± 180 | 480 ± 180 | 360 ± 120 * | 0.04 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bawa, M.; Gugino, S.; Helman, J.; Nielsen, L.; Bradley, N.; Mani, S.; Prasath, A.; Blanco, C.; Mari, A.; Nair, J.; et al. Initial Use of 100% but Not 60% or 30% Oxygen Achieved a Target Heart Rate of 100 bpm and Preductal Saturations of 80% Faster in a Bradycardic Preterm Model. Children 2022, 9, 1750. https://doi.org/10.3390/children9111750
Bawa M, Gugino S, Helman J, Nielsen L, Bradley N, Mani S, Prasath A, Blanco C, Mari A, Nair J, et al. Initial Use of 100% but Not 60% or 30% Oxygen Achieved a Target Heart Rate of 100 bpm and Preductal Saturations of 80% Faster in a Bradycardic Preterm Model. Children. 2022; 9(11):1750. https://doi.org/10.3390/children9111750
Chicago/Turabian StyleBawa, Mausma, Sylvia Gugino, Justin Helman, Lori Nielsen, Nicole Bradley, Srinivasan Mani, Arun Prasath, Clariss Blanco, Andreina Mari, Jayasree Nair, and et al. 2022. "Initial Use of 100% but Not 60% or 30% Oxygen Achieved a Target Heart Rate of 100 bpm and Preductal Saturations of 80% Faster in a Bradycardic Preterm Model" Children 9, no. 11: 1750. https://doi.org/10.3390/children9111750
APA StyleBawa, M., Gugino, S., Helman, J., Nielsen, L., Bradley, N., Mani, S., Prasath, A., Blanco, C., Mari, A., Nair, J., Rawat, M., Lakshminrusimha, S., & Chandrasekharan, P. (2022). Initial Use of 100% but Not 60% or 30% Oxygen Achieved a Target Heart Rate of 100 bpm and Preductal Saturations of 80% Faster in a Bradycardic Preterm Model. Children, 9(11), 1750. https://doi.org/10.3390/children9111750






