A Pragmatic Approach to Assessment of Chronic and Recurrent Pain in Children with Severe Neurologic Impairment
Abstract
:1. Introduction
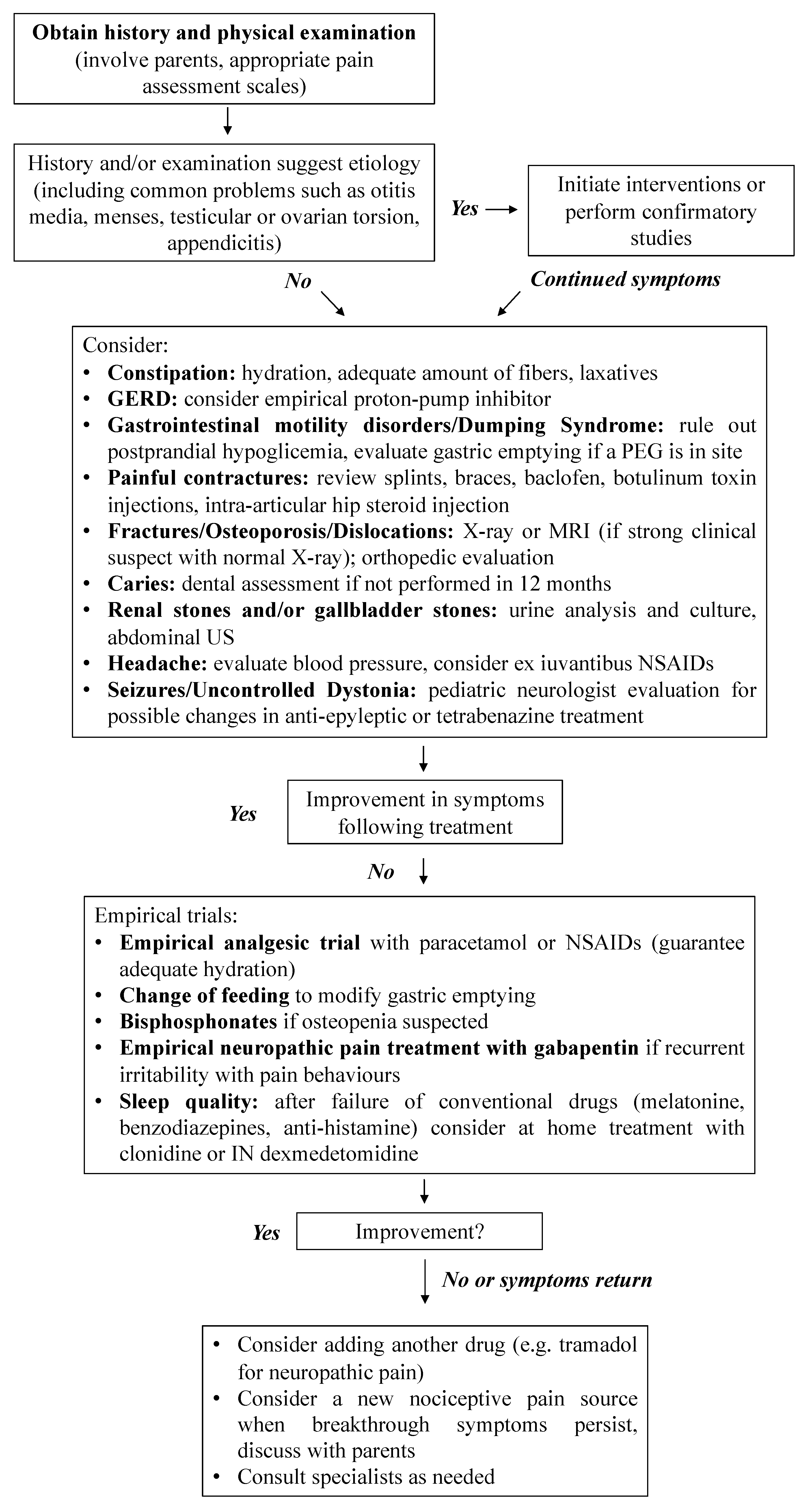
2. Pain Recognition and Measurement
3. Diagnostic Workup for Pain in Patients with Cognitive Impairment
3.1. Gastrointestinal Tract
3.2. Musculoskeletal Pain
3.3. Other Common Source of Pain
3.4. Neurogenic and Other Central Nervous System Causes of Pain
3.5. Do Not Forget: Non-Pharmacological Interventions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Allen, J.; Brenner, M.; Hauer, J.; Molloy, E.; McDonald, D. Severe Neurological Impairment: A delphi consensus-based definition. Eur. J. Paediatr. Neurol. 2020, 29, 81–86. [Google Scholar] [CrossRef]
- Oskoui, M.; Coutinho, F.; Dykeman, J.; Jetté, N.; Pringsheim, T. An update on the prevalence of cerebral palsy: A systematic review and meta-analysis. Dev. Med. Child Neurol. 2013, 55, 509–519. [Google Scholar] [CrossRef]
- Breau, L.M.; Camfield, C.S.; McGrath, P.J.; Finley, G.A. The incidence of pain in children with severe cognitive impairments. Arch. Pediatr. Adolesc. Med. 2003, 157, 1219–1226. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Warlow, T.A.; Hain, R.D.W. ‘Total Pain’ in Children with Severe Neurological Impairment. Children 2018, 5, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breau, L.M.; Camfield, C.S.; McGrath, P.J.; Finley, G.A. Risk factors for pain in children with severe cognitive impairments. Dev. Med. Child Neurol. 2004, 46, 364–371. [Google Scholar] [CrossRef] [PubMed]
- Barbi, E.; Badina, L.; Massaro, M.; Pisciotta, G.; Ventura, A. Paediatricians’ attitudes toward pain in children with severe cognitive impairment. A regional survey. Pediatr. Med. Chir. 2014, 36, 177–180. [Google Scholar] [CrossRef]
- Riquelme, I.; Montoya, P. Developmental changes in somatosensory processing in cerebral palsy and healthy individuals. Clin. Neurophysiol. 2010, 121, 1314–1320. [Google Scholar] [CrossRef]
- Horwood, L.; Li, P.; Mok, E.; Oskoui, M.; Shevell, M.; Constantin, E. Behavioral difficulties, sleep problems, and nighttime pain in children with cerebral palsy. Res. Dev. Disabil. 2019, 95, 103500. [Google Scholar] [CrossRef]
- Lumley, M.A.; Cohen, J.L.; Borszcz, G.S.; Cano, A.; Radcliffe, A.M.; Porter, L.S.; Schubiner, H.; Keefe, F.J. Pain and emotion: A biopsychosocial review of recent research. J. Clin. Psychol. 2011, 67, 942–968. [Google Scholar] [CrossRef] [Green Version]
- Hauer, J.; Houtrow, A.J. Pain Assessment and Treatment in Children With Significant Impairment of the Central Nervous System. Pediatrics 2017, 139, e20171002. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Breau, L.M.; Finley, G.A.; McGrath, P.J.; Camfield, C.S. Validation of the Non-communicating Children’s Pain Checklist-Postoperative Version. Anesthesiology 2002, 96, 528–535. [Google Scholar] [CrossRef]
- Breau, L.M.; McGrath, P.J.; Camfield, C.S.; Finley, G.A. Psychometric properties of the non-communicating children’s pain checklist-revised. Pain 2002, 99, 349–357. [Google Scholar] [CrossRef]
- Solodiuk, J.C.; Scott-Sutherland, J.; Meyers, M.; Myette, B.; Shusterman, C.; Karian, V.E.; Harris, S.K.; Curley, M.A.Q. Validation of the Individualized Numeric Rating Scale (INRS): A pain assessment tool for nonverbal children with intellectual disability. Pain 2010, 150, 231–236. [Google Scholar] [CrossRef]
- Hunt, A.; Goldman, A.; Seers, K.; Crichton, N.; Mastroyannopoulou, K.; Moffat, V.; Oulton, K.; Brady, M. Clinical validation of the paediatric pain profile. Dev. Med. Child Neurol. 2004, 46, 9–18. [Google Scholar] [CrossRef] [PubMed]
- Malviya, S.; Voepel-Lewis, T.; Burke, C.; Merkel, S.; Tait, A.R. The revised FLACC observational pain tool: Improved reliability and validity for pain assessment in children with cognitive impairment. Paediatr. Anaesth. 2006, 16, 258–265. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Voepel-Lewis, T.; Malviya, S.; Tait, A.R.; Merkel, S.; Foster, R.; Krane, E.J.; Davis, P.J. A comparison of the clinical utility of pain assessment tools for children with cognitive impairment. Anesth. Analg. 2008, 106, 72–78. [Google Scholar] [CrossRef]
- Voepel-Lewis, T.; Malviya, S.; Tait, A.R. Validity of parent ratings as proxy measures of pain in children with cognitive impairment. Pain Manag. Nurs. 2005, 6, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Carter, B.; Arnott, J.; Simons, J.; Bray, L. Developing a Sense of Knowing and Acquiring the Skills to Manage Pain in Children with Profound Cognitive Impairments: Mothers’ Perspectives. Pain Res. Manag. 2017. [Google Scholar] [CrossRef]
- Pascolo, P.; Peri, F.; Montico, M.; Funaro, M.; Parrino, R.; Vanadia, F.; Rusalen, F.; Vecchiato, L.; Benini, F.; Congedi, S.; et al. Needle-related pain and distress management during needle-related procedures in children with and without intellectual disability. Eur. J. Pediatr. 2018, 177, 1753–1760. [Google Scholar] [CrossRef]
- Krauss, B.S.; Krauss, B.A.; Green, S.M. Managing Procedural Anxiety in Children. N. Engl. J. Med. 2016, 374, e19. [Google Scholar] [CrossRef]
- Bembich, S.; Morabito, G.; Simeon, V.; Strajn, T.; Rutigliano, R.; Di Rocco, P.; Cont, G.; Risso, F.M.; Peri, F.; Barbi, E. Venipuncture activates the cerebral cortex in children with intellectual disability. Arch. Dis. Child. 2021, 106, 167–172. [Google Scholar] [CrossRef] [PubMed]
- Gfroerer, S.; Rolle, U. Pediatric intestinal motility disorders. World J. Gastroenterol. 2015, 21, 9683–9687. [Google Scholar] [CrossRef] [PubMed]
- Brun, A.C.; Størdal, K.; Johannesdottir, G.B.; Bentsen, B.S.; Medhus, A.W. The effect of protein composition in liquid meals on gastric emptying rate in children with cerebral palsy. Clin. Nutr. 2012, 31, 108–112. [Google Scholar] [CrossRef]
- Di Leo, G.; Pascolo, P.; Hamadeh, K.; Trombetta, A.; Ghirardo, S.; Schleef, J.; Barbi, E.; Codrich, D. Gastrostomy Placement and Management in Children: A Single-Center Experience. Nutrients 2019, 11, 1555. [Google Scholar] [CrossRef] [Green Version]
- Krasaelap, A.; Kovacic, K.; Goday, P.S. Nutrition Management in Pediatric Gastrointestinal Motility Disorders. Nutr. Clin. Pract. 2020, 35, 265–272. [Google Scholar] [CrossRef] [PubMed]
- Hassall, E.; Kerr, W.; El-Serag, H.B. Characteristics of children receiving proton pump inhibitors continuously for up to 11 years duration. J. Pediatr. 2007, 150, 262–267. [Google Scholar] [CrossRef] [PubMed]
- Grundy, D. Neuroanatomy of visceral nociception: Vagal and splanchnic afferent. Gut 2002, 51, i2. [Google Scholar] [CrossRef] [Green Version]
- Li, J.; Simone, D.A.; Larson, A.A. Windup leads to characteristics of central sensitization. Pain 1999, 79, 75–82. [Google Scholar] [CrossRef]
- Kolasinski, S.L.; Neogi, T.; Hochberg, M.C.; Oatis, C.; Guyatt, G.; Block, J.; Callahan, L.; Copenhaver, C.; Dodge, C.; Felson, D.; et al. 2019 American College of Rheumatology/Arthritis Foundation Guideline for the Management of Osteoarthritis of the Hand, Hip, and Knee. Arthritis Care Res. (Hoboken) 2020, 72, 149–162. [Google Scholar] [CrossRef]
- Henderson, R.C. Bone density and other possible predictors of fracture risk in children and adolescents with spastic quadriplegia. Dev. Med. Child Neurol. 1997, 39, 224–227. [Google Scholar] [CrossRef] [PubMed]
- Henderson, R.C.; Lark, R.K.; Kecskemethy, H.H.; Miller, F.; Harcke, H.T.; Bachrach, S.J. Bisphosphonates to treat osteopenia in children with quadriplegic cerebral palsy: A randomized, placebo-controlled clinical trial. J. Pediatr. 2002, 141, 644–651. [Google Scholar] [CrossRef] [PubMed]
- Hurley, T.; Zareen, Z.; Stewart, P.; McDonnell, C.; McDonald, D.; Molloy, E. Bisphosphonate use in children with cerebral palsy. Cochrane Database Syst. Rev. 2021, 7, CD012756. [Google Scholar]
- Sebestyen, J.F.; Srivastava, T.; Alon, U.S. Bisphosphonates use in children. Clin. Pediatr. (Phila) 2012, 51, 1011–1024. [Google Scholar] [CrossRef]
- Chen, J.J.; Ondo, W.G.; Dashtipour, K.; Swope, D.M. Tetrabenazine for the treatment of hyperkinetic movement disorders: A review of the literature. Clin. Ther. 2012, 34, 1487–1504. [Google Scholar] [CrossRef] [PubMed]
- Cortellazzo Wiel, L.; De Nardi, L.; Magnolato, A.; Sirchia, F.; Bruno, I.; Barbi, E. Beneficial effect of gabapentin in two children with Noonan syndrome and early-onset neuropathic pain. Am. J. Med. Genet. A 2020, 182, 1990–1992. [Google Scholar] [CrossRef] [PubMed]
- Breau, L.M.; Camfield, C.S. Pain disrupts sleep in children and youth with intellectual and developmental disabilities. Res. Dev. Disabil. 2011, 32, 2829–2840. [Google Scholar] [CrossRef]
- Finan, P.H.; Goodin, B.R.; Smith, M.T. The association of sleep and pain: An update and a path forward. J. Pain 2013, 14, 1539. [Google Scholar] [CrossRef] [Green Version]
- De Zen, L.; Del Rizzo, I.; Robazza, M.; Barbieri, F.; Campagna, M.; Vaccher, S.; Barbi, E.; Dall’Amico, R. Home Use of Intranasal Dexmedetomidine in a Child With An Intractable Sleep Disorder. J. Pediatr. Pharmacol. Ther. JPPT 2020, 25, 332. [Google Scholar] [CrossRef]
- De Zen, L.; Della Paolera, S.; Del Rizzo, I.; Taucar, V.; Skabar, A.; Barbi, E. Home Intranasal Dexmedetomidine for Refractory Dystonia in Pediatric Palliative Care. J. Pain Symptom Manag. 2020, 59, e3–e5. [Google Scholar] [CrossRef] [PubMed]
- Julie, M.; Hauer, M.D. Chronic Pain in Children with Severe Impairment of the Central Nervous System: A Framework for Assessment and Initial Management. Complex Care Journal. Available online: http://complexcarejournal.org/2020/03/24/chronic-pain-in-children-with-severe-impairment-of-the-central-nervous-system/ (accessed on 17 October 2021).
- Friedrichsdorf, S.J.; Kang, T.I. The management of pain in children with life-limiting illnesses. Pediatr. Clin. N. Am. 2007, 54, 645–672. [Google Scholar] [CrossRef]

| Face |
| 0 = No particular expression or smile 1 = Occasional grimace/frown; withdrawn or disinterested; appears sad or worried 2 = Consistent grimace or frown; frequent/constant quivering chin, clenched jaw; distressed-looking face; expression of fright or panic Individualized behavior:___________ |
| Legs |
| 0 = Normal position or relaxed; usual tone and motion to limbs 1 = Uneasy, restless, tense; occasional tremors 2 = Kicking, or legs drawn up; marked increase in spasticity, constant tremors or jerking Individualized behavior:___________ |
| Activity |
| 0 = Lying quietly, normal position, moves easily; regular, rhythmic respirations 1 = Squirming, shifting back and forth, tense or guarded movements; mildly agitated (e.g., head back and forth and aggression); shallow, splinting respirations, intermittent sighs 2 = Arched, rigid or jerking; severe agitation; head banging; shivering (not rigors); breath holding, gasping or sharp intake of breaths, severe splinting Individualized behavior:___________ |
| Cry |
| 0 = No cry/verbalization 1 = Moans or whimpers; occasional complaint; occasional verbal outburst or grunt 2 = Crying steadily, screams or sobs, frequent complaints; repeated outbursts, constant grunting Individualized behavior:___________ |
| Consolability |
| 0 = Content and relaxed 1 = Reassured by occasional touching, hugging or being talked to. Distractible 2 = Difficult to console or comfort; pushing away caregiver, resisting care or comfort measures Individualized behavior:___________ |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Benvenuto, S.; Trombetta, A.; Barbi, E. A Pragmatic Approach to Assessment of Chronic and Recurrent Pain in Children with Severe Neurologic Impairment. Children 2022, 9, 45. https://doi.org/10.3390/children9010045
Benvenuto S, Trombetta A, Barbi E. A Pragmatic Approach to Assessment of Chronic and Recurrent Pain in Children with Severe Neurologic Impairment. Children. 2022; 9(1):45. https://doi.org/10.3390/children9010045
Chicago/Turabian StyleBenvenuto, Simone, Andrea Trombetta, and Egidio Barbi. 2022. "A Pragmatic Approach to Assessment of Chronic and Recurrent Pain in Children with Severe Neurologic Impairment" Children 9, no. 1: 45. https://doi.org/10.3390/children9010045
APA StyleBenvenuto, S., Trombetta, A., & Barbi, E. (2022). A Pragmatic Approach to Assessment of Chronic and Recurrent Pain in Children with Severe Neurologic Impairment. Children, 9(1), 45. https://doi.org/10.3390/children9010045






