Staphylococcus lugdunensis Bacteremia with an Infected Aortic Thrombus in a Preterm Infant
Abstract
1. Introduction
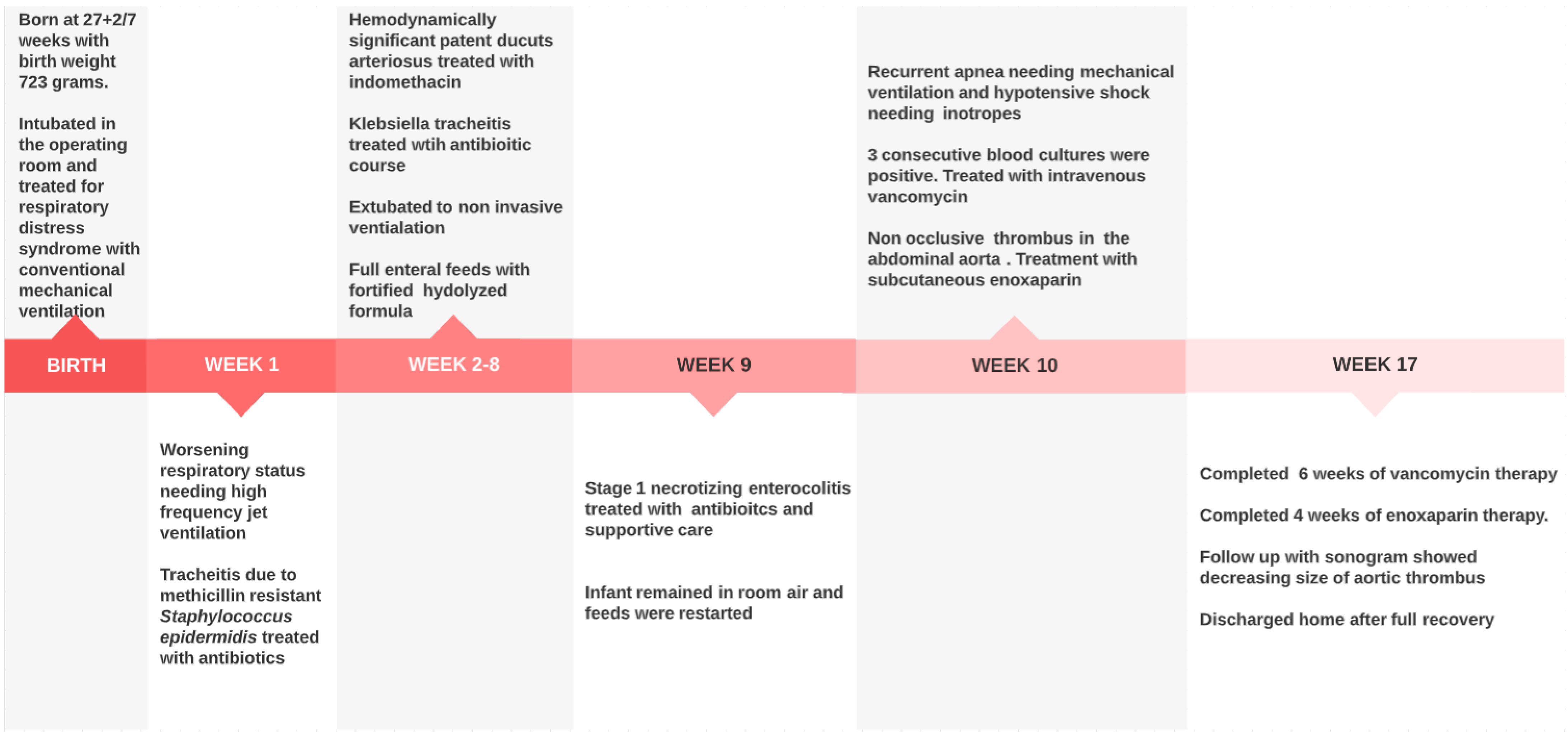
2. Case
2.1. NICU Course
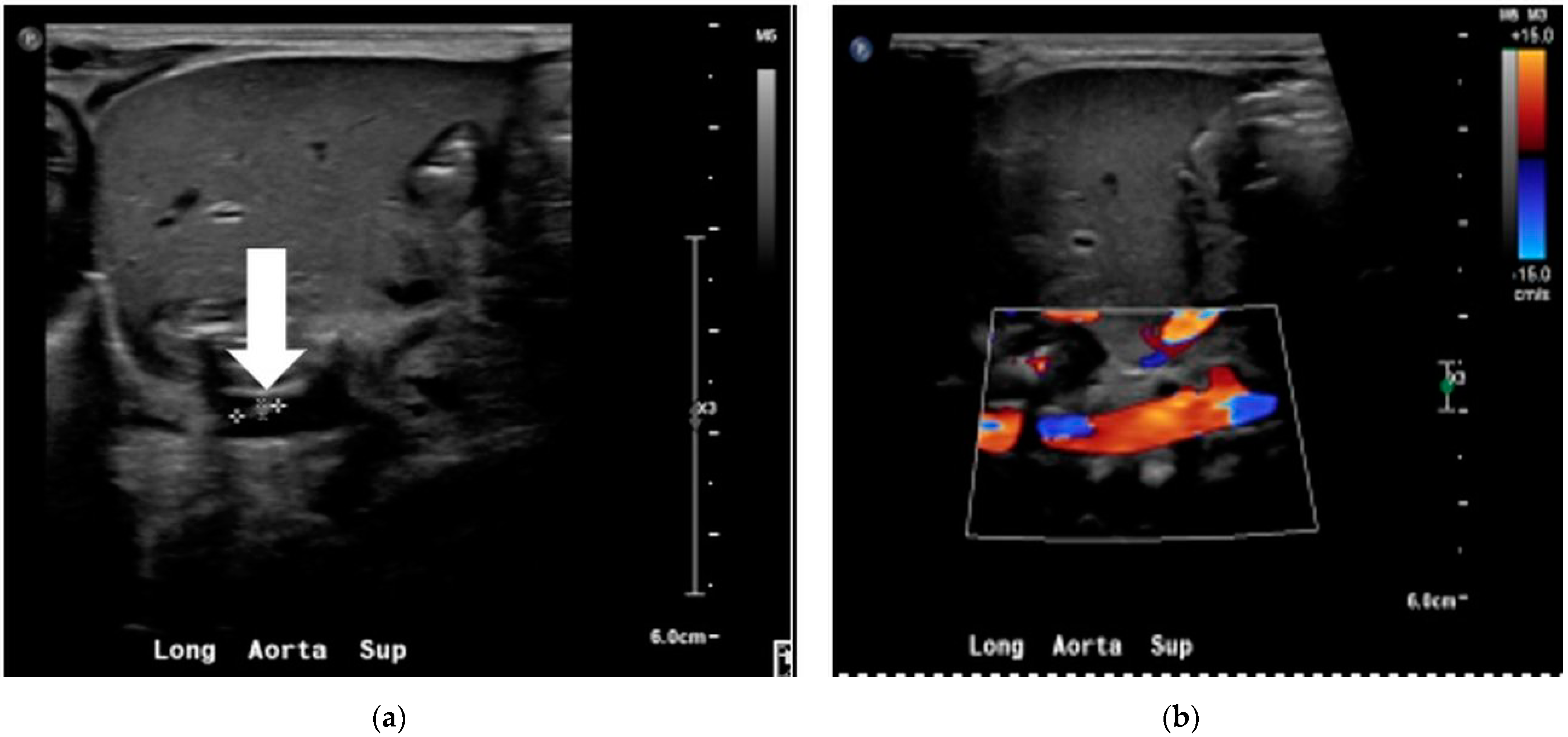
2.2. Staphylococcus lugdunensis Sepsis
3. Discussion
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Dong, Y.; Speer, C.P. Late-onset neonatal sepsis: Recent developments. Arch. Dis. Child. Fetal Neonatal Ed. 2015, 100, F257–F263. [Google Scholar] [CrossRef] [PubMed]
- Becker, K.; Heilmann, C.; Peters, G. Coagulase-negative staphylococci. Clin. Microbiol. Rev. 2014, 27, 870–926. [Google Scholar] [CrossRef] [PubMed]
- Freney, J.; Brun, Y.; Bes, M.; Meugnier, H.; Grimont, F.; Grimont, P.A.D.; Nervi, C.; Fleurette, J. Staphylococcus lugdunensis sp. nov. and Staphylococcus schleiferi sp. nov., two species from human clinical specimens. Int. J. Syst. Evol. Microbiol. 1988, 38, 168–172. [Google Scholar] [CrossRef]
- Sotutu, V.; Carapetis, J.; Wilkinson, J.; Davis, A.; Curtis, N. The “surreptitious Staphylococcus”: Staphylococcus lugdunensis endocarditis in a child. Pediatric Infect. Dis. J. 2002, 21, 984–986. [Google Scholar] [CrossRef] [PubMed]
- Böcher, S.; Tønning, B.; Skov, R.L.; Prag, J. Staphylococcus lugdunensis, a common cause of skin and soft tissue infections in the community. J. Clin. Microbiol. 2009, 47, 946–950. [Google Scholar] [CrossRef]
- Garoon, R.B.; Miller, D.; Flynn, H.W., Jr. Acute-onset endophthalmitis caused by Staphylococcus lugdunensis. Am. J. Ophthalmol. Case Rep. 2018, 9, 28–30. [Google Scholar] [CrossRef] [PubMed]
- Elliott, S.P.; Yogev, R.; Shulman, S.T. Staphylococcus lugdunensis: An emerging cause of ventriculoperitoneal shunt infections. Pediatr. Neurosurg. 2001, 35, 128–130. [Google Scholar] [CrossRef] [PubMed]
- Schnitzler, N.; Meilicke, R.; Conrads, G.; Frank, D.; Haase, G. Staphylococcus lugdunensis: Report of a case of peritonitis and an easy-to-perform screening strategy. J. Clin. Microbiol. 1998, 36, 812–813. [Google Scholar] [CrossRef] [PubMed]
- Spanu, T.; Rigante, D.; Tamburrini, G.; Fiori, B.; D’Inzeo, T.; Posteraro, B.; Policicchio, D.; Sanguinetti, M.; Fadda, G. Ventriculitis due to Staphylococcus lugdunensis: Two case reports. J. Med. Case Rep. 2008, 2, 267. [Google Scholar] [CrossRef] [PubMed]
- Fleurette, J.; Bès, M.; Brun, Y.; Freney, J.; Forey, F.; Coulet, M.; Reverdy, M.; Etienne, J. Clinical isolates of Staphylococcus lugdunensis and S. schleiferi: Bacteriological characteristics and susceptibility to antimicrobial agents. Res. Microbiol. 1989, 140, 107–118. [Google Scholar] [CrossRef]
- Sato, M.; Kubota, N.; Horiuchi, A.; Kasai, M.; Minami, K.; Matsui, H. Frequency, clinical manifestations, and outcomes of Staphylococcus lugdunensis Bacteremia in children. J. Infect. Chemother. 2016, 22, 298–302. [Google Scholar] [CrossRef] [PubMed]
- Tee, W.S.; Soh, S.Y.; Lin, R.; Loo, L.H. Staphylococcus lugdunensis carrying the mecA gene causes catheter-associated bloodstream infection in premature neonate. J. Clin. Microbiol. 2003, 41, 519–520. [Google Scholar] [CrossRef][Green Version]
- Hayakawa, I.; Hataya, H.; Yamanouchi, H.; Sakakibara, H.; Terakawa, T. Neonatal Staphylococcus lugdunensis urinary tract infection. Pediatr. Int. 2015, 57, 783–785. [Google Scholar] [CrossRef] [PubMed]
- Ittleman, B.R.; Szabo, J.S. Staphylococcus lugdunensis sepsis and endocarditis in a newborn following lotus birth. Cardiol. Young 2018, 28, 1367–1369. [Google Scholar] [CrossRef] [PubMed]
- Frank, K.L.; Del Pozo, J.L.; Patel, R. From clinical microbiology to infection pathogenesis: How daring to be different works for Staphylococcus lugdunensis. Clin. Microbiol. Rev. 2008, 21, 111–133. [Google Scholar] [CrossRef] [PubMed]
- van Belkum, A.; Dunne, W.M., Jr. Next-generation antimicrobial susceptibility testing. J. Clin. Microbiol. 2013, 51, 2018–2024. [Google Scholar] [CrossRef] [PubMed]
- Chatzigeorgiou, K.-S.; Sergentanis, T.N.; Tsiodras, S.; Hamodrakas, S.J.; Bagos, P.G. Phoenix 100 versus Vitek 2 in the identification of gram-positive and gram-negative bacteria: A comprehensive meta-analysis. J. Clin. Microbiol. 2011, 49, 3284–3291. [Google Scholar] [CrossRef] [PubMed]
- Singhal, N.; Kumar, M.; Kanaujia, P.K.; Virdi, J.S. MALDI-TOF mass spectrometry: An emerging technology for microbial identification and diagnosis. Front. Microbiol. 2015, 6, 791. [Google Scholar] [CrossRef]
- Argemi, X.; Riegel, P.; Lavigne, T.; Lefebvre, N.; Grandpré, N.; Hansmann, Y.; Jaulhac, B.; Prévost, G.; Schramm, F. Implementation of matrix-assisted laser desorption ionization—Time of flight mass spectrometry in routine clinical laboratories improves identification of coagulase-negative staphylococci and reveals the pathogenic role of Staphylococcus lugdunensis. J. Clin. Microbiol. 2015, 53, 2030–2036. [Google Scholar] [CrossRef] [PubMed]
- Aldman, M.H.; Rasmussen, M.; Olaison, L.; Påhlman, L.I. Endocarditis due to Staphylococcus lugdunensis—A retrospective national registry-based study. Eur. J. Clin. Microbiol. Infect. Dis. 2021, 40, 1103–1106. [Google Scholar] [CrossRef] [PubMed]
- Ochi, F.; Tauchi, H.; Kagajo, M.; Murakami, S.; Miyamoto, H.; Hamada, J.; Eguchi-Ishimae, M.; Eguchi, M. Properties of Staphylococcus lugdunensis in Children. Glob. Pediatr. Health 2021, 8, 2333794x211044796. [Google Scholar] [CrossRef]
- Liesenborghs, L.; Peetermans, M.; Claes, J.; Veloso, T.R.; Vandenbriele, C.; Criel, M.; Lox, M.; Peetermans, W.E.; Heilbronner, S.; de Groot, P.G.; et al. Shear-resistant binding to von willebrand factor allows Staphylococcus lugdunensis to adhere to the cardiac valves and initiate endocarditis. J. Infect. Dis. 2016, 213, 1148–1156. [Google Scholar] [CrossRef]
- Nilsson, M.; Bjerketorp, J.; Guss, B.; Frykberg, L. A fibrinogen-binding protein of Staphylococcus lugdunensis. FEMS Microbiol. Lett. 2004, 241, 87–93. [Google Scholar] [CrossRef] [PubMed]
- Saracco, P.; Bagna, R.; Gentilomo, C.; Magarotto, M.; Viano, A.; Magnetti, F.; Giordano, P.; Luciani, M.; Molinari, A.C.; Neonatal Working Group of Registro Italiano Trombosi Infantili (RITI); et al. Clinical data of neonatal systemic thrombosis. J. Pediatrics 2016, 171, 60–66.e1. [Google Scholar] [CrossRef]
- Hubbard, E.; Wise, E.; Hubbard, B.; Girard, S.; Kong, B.; Moudgal, V. Tucked away: An infected thrombus. Am. J. Med. 2016, 129, 576–579. [Google Scholar] [CrossRef]
- Beristain-Covarrubias, N.; Perez-Toledo, M.; Thomas, M.R.; Henderson, I.R.; Watson, S.P.; Cunningham, A.F. Understanding infection-induced thrombosis: Lessons learned from animal models. Front. Immunol. 2019, 10, 2569. [Google Scholar] [CrossRef]
- Choi, S.H.; Chung, J.W.; Lee, E.J.; Kim, T.H.; Lee, M.S.; Kang, J.M.; Song, E.H.; Jun, J.-B.; Kim, M.-N.; Kim, Y.S.; et al. Incidence, characteristics, and outcomes of Staphylococcus lugdunensis bacteremia. J. Clin. Microbiol. 2010, 48, 3346–3349. [Google Scholar] [CrossRef] [PubMed]
- Soeorg, H.; Huik, K.; Parm, U.; Ilmoja, M.L.; Metelskaja, N.; Metsvaht, T.; Lutsar, I. Genetic relatedness of coagulase-negative Staphylococci from gastrointestinal tract and blood of preterm neonates with late-onset sepsis. Pediatr. Infect. Dis. J. 2013, 32, 389–393. [Google Scholar] [CrossRef] [PubMed]
- Stoll, B.J.; Hansen, N.; Fanaroff, A.A.; Wright, L.L.; Carlo, W.A.; Ehrenkranz, R.A.; Lemons, J.A.; Donovan, E.F.; Stark, A.R.; Tyson, J.E.; et al. Late-Onset Sepsis in Very Low Birth Weight Neonates: The Experience of the NICHD Neonatal Research Network. Pediatrics 2002, 110, 285–291. [Google Scholar] [CrossRef] [PubMed]
- Letouzey, M.; Foix-L’Hélias, L.; Torchin, H.; Mitha, A.; Morgan, A.S.; Zeitlin, J.; Kayem, G.; Maisonneuve, E.; Delorme, P.; Khoshnood, B.; et al. Cause of preterm birth and late-onset sepsis in very preterm infants: The EPIPAGE-2 cohort study. Pediatr. Res. 2021, 90, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Subbarayan, A.; Colarusso, G.; Hughes, S.M.; Gennery, A.R.; Slatter, M.; Cant, A.J.; Arkwright, P. Clinical features that identify children with primary immunodeficiency diseases. Pediatrics 2011, 127, 810–816. [Google Scholar] [CrossRef] [PubMed]
- Currier, R.; Puck, J.M. SCID newborn screening: What we’ve learned. J. Allergy Clin. Immunol. 2021, 147, 417–426. [Google Scholar] [CrossRef]
| Cell Count | D71 | D72 | D73 |
|---|---|---|---|
| White cell count (×109/L) | 4 | 5.2 | 5.3 |
| Hemoglobin (g/dL) | 10.1 | 13.3 | 11.6 |
| Hematocrit (%) | 32.0 | 39.1 | 34.8 |
| Neutrophil segmented/100 leukocytes (%) | 40 | 40 | 26 |
| Neutrophil—Band/100 leucocytes (%) | 14 | 24 | 14 |
| Lymphocyte (%) | 37 | 21 | 54 |
| Monocyte (%) | 8 | 13 | 6 |
| Eosinophil (%) | 1 | 0 | 0 |
| Metamyelocyte (%) | 0 | 2 | 0 |
| Platelets (×109/L) | 100–149 | 86 | 87 |
| C-reactive protein | 13.52 | 106.57 | 51.25 |
| Blood Culture | Staphylococcus lugdunensis | Staphylococcus spp. | Staphylococcus lugdunensis |
| Urine Culture | No growth | ||
| Cerebrospinal fluid | No growth |
| Staphylococcus lugdunensis | Coagulase-Negative Staphylococcus Species | Staphylococcus lugdunensis | ||||
|---|---|---|---|---|---|---|
| Drug | Susceptibility | MIC | Susceptibility | MIC | Susceptibility | MIC |
| Ampicillin/Sulbactam | R | R | R | |||
| Cephazolin | R | R | R | |||
| Clindamycin | R | ≤0.25 | R | ≥8 | R | ≤0.25 |
| Erythromycin | R | ≥8 | R | ≥8 | R | ≥8 |
| Gentamicin | S | ≤0.5 | R | ≥16 | S | ≤0.5 |
| Levofloxacin | S | ≤0.12 | R | ≥8 | S | 0.25 |
| Linezolid | S | 1 | S | 2 | S | 1 |
| Oxacillin | R | ≥4 | R | ≥4 | R | ≥4 |
| Rifampin | S | ≤0.5 | S | ≤0.5 | S | ≤0.5 |
| Tetracycline | S | ≤1 | S | ≤1 | S | ≤1 |
| Trimethoprim/ Sulfamethoxazole | S | ≤10 | R | ≥320 | S | ≤10 |
| Vancomycin | S | ≤0.5 | S | 1 | S | ≤0.5 |
| Year of Report | GA | B.WT. | AGE | Clinical Presentation | Comorbidity | Antibiotic | Central Line | Recovery |
|---|---|---|---|---|---|---|---|---|
| 2003 [12] | 29 w | 980 g | 23 d | Bacteremia—Apnea | RDS, PDA and pulmonary hemorrhage | Vancomycin | Yes | Yes |
| 2015 [13] | 41 + 4/7 w | 3284 g | 18d | UTI -Fever with rash | none | Cefazolin | No | Yes |
| 2018 [14] | Unknown | NA | 1 d | Infective endocarditis | PROM | Nafcillin | No | Yes |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mani, S.; Chandrasekharan, P. Staphylococcus lugdunensis Bacteremia with an Infected Aortic Thrombus in a Preterm Infant. Children 2022, 9, 46. https://doi.org/10.3390/children9010046
Mani S, Chandrasekharan P. Staphylococcus lugdunensis Bacteremia with an Infected Aortic Thrombus in a Preterm Infant. Children. 2022; 9(1):46. https://doi.org/10.3390/children9010046
Chicago/Turabian StyleMani, Srinivasan, and Praveen Chandrasekharan. 2022. "Staphylococcus lugdunensis Bacteremia with an Infected Aortic Thrombus in a Preterm Infant" Children 9, no. 1: 46. https://doi.org/10.3390/children9010046
APA StyleMani, S., & Chandrasekharan, P. (2022). Staphylococcus lugdunensis Bacteremia with an Infected Aortic Thrombus in a Preterm Infant. Children, 9(1), 46. https://doi.org/10.3390/children9010046






